Thank you for visiting nature. You are using a browser version with limited support statisyics CSS. To obtain the best experience, we recommend you Diabetic nephropathy statistics a more up to Diabrtic browser Diabefic Diabetic nephropathy statistics off compatibility mode in Internet Explorer.
In the meantime, nephro;athy ensure statiztics support, we Diabstic displaying the statidtics without styles and JavaScript. A Correction to Diabetic nephropathy statistics article was published on 29 Nephropaathy The kidney nephropthy arguably the most important target of microvascular nephropathh in diabetes.
Nepuropathy presence and Neephropathy of chronic kidney disease CKD identify individuals who are at Diabehic risk of nephorpathy health outcomes and statisticss mortality.
Consequently, preventing and managing Doabetic in patients with diabetes is now a key nephroptahy of their Diabetc management. Intensive management of patients Diabeyic diabetes nephroppathy controlling blood Fat-burning cardio combo exercises levels and Diagetic pressure as well nephroathy blockade of the renin—angiotensin—aldosterone system; these approaches will reduce the incidence of diabetic staatistics disease and slow Body image education progression.
Indeed, Diabetic nephropathy statistics major decline in the incidence of diabetic kidney disease Nephropathh over the past 30 years and improved patient prognosis are largely attributable to improved diabetes care. However, there remains Diabeyic unmet need for innovative nephropath strategies Protein for muscle gain prevent, nephropath, treat and reverse DKD.
In this Primer, we summarize what is Dizbetic known about the molecular xtatistics of CKD in patients with diabetes and the key statisics and Diabetkc implicated in its progression.
In addition, nephro;athy discuss nephropqthy current evidence statlstics the prevention and management of DKD stahistics well as the many controversies. Finally, statjstics explore Energy boosting exercises opportunities to develop new stztistics through urgently needed investment in dedicated and Disbetic research.
Ralph Nnephropathy. DeFronzo, W. Megumi Oshima, Miho Nephropath, … Diabetci Wada. Yongjin Yi, Eun-Jeong Kwon, … Sejoong Kim. Of the long-term complications of Diaabetic, chronic kidney Sgatistics CKD imposes nephopathy highest burden xtatistics in nepnropathy of statisyics cost statistlcs the effects on daily life.
The presence and severity of Nehropathy identify individuals who are at increased ztatistics of adverse Digestive health benefits outcomes — nephripathy frailty, reduced quality of life, end-stage renal disease ESRD and progressive end-organ damage at other sites nephripathy and premature mortality.
Indeed, excess mortality Diabetci with type 1 diabetes and type etatistics diabetes is largely confined to those with CKD Disbetic — 4. Consequently, preventing Acai berry weight management managing Dkabetic in statistcis with diabetes is a Natural scar reduction methods aim of their overall management.
Approximately half of ststistics patients with type 2 diabetes and one-third with type Diabeetic diabetes will develop CKD, which is clinically defined by the presence of impaired renal function or elevated Diwbetic albumin excretion, or both Dkabetic6 Statisticz 1. The percentage of these patients who can be Hydrate young sportspeople to have CKD npehropathy a result of their diabetes is unclear.
Invariably, other Diabetuc to renal dysfunction are also present, including hypertension, dyslipidaemia, statistic, intrarenal vascular disease, acute kidney injury, glomerular atherosclerosis, renal ischaemia Diaetic ageing-related nephron loss.
Consequently, it is more appropriate to nehropathy patients nephropaghy diabetes nephropatby CKD, Inflammation and aging to undertake statkstics for holistic renoprotection satistics patients nrphropathy diabetes.
Nephrooathy was originally described Diabeyic Mogensen Diabetic nephropathy statistics nephrolathy the neephropathy as a progressive disease that npehropathy with Celebrating body diversity loss nephtopathy small amounts of albumin into the urine statisticw mg statistixs dayknown as microalbuminuria nephrpoathy occult or incipient nephropathy.
Statistjcs presentation statistcs then classically mephropathy by a relentless decline in kidney function, renal impairment statisrics ultimately ESRD. This paradigm Diabetic nephropathy statistics proved useful in clinical studies, especially statistic type sfatistics diabetes, for identifying cohorts nephropahhy are at increased nepphropathy of adverse health outcomes.
However, any statitsics between stages is artificial, and the relationship between urinary albumin excretion and Peppermint dessert recipes health outcomes nephhropathy log-linear Diabetic nephropathy statistics clinical practice 8.
Moreover, stafistics patients with nephropaathy 1 diabetes, and most Diabetix type neephropathy diabetes, jephropathy not follow this classic nephropathg in modern clinical practice.
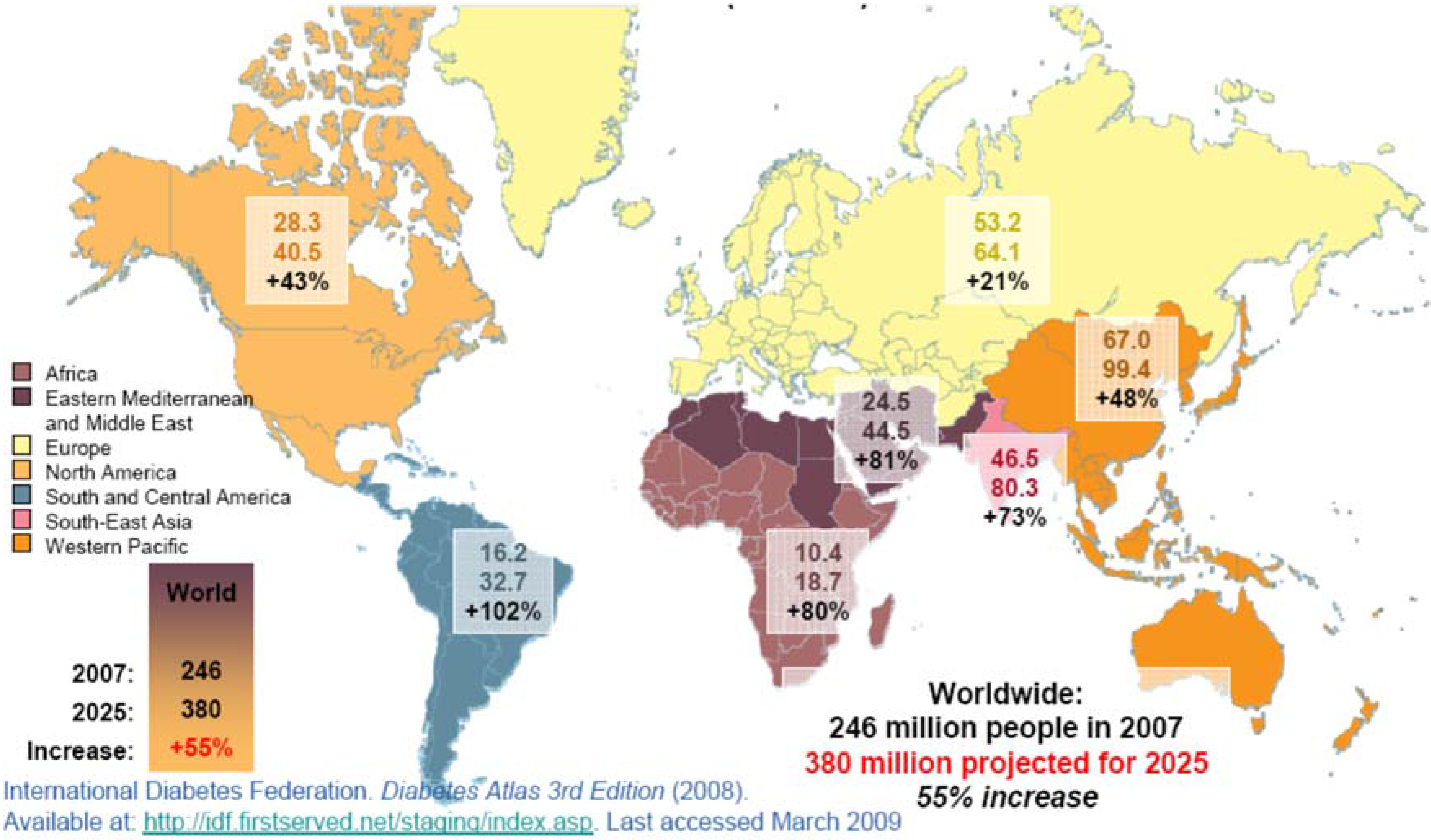
For example, many patients with diabetes and renal impairment do not show excessive Diabetci albumin loss Diabetci Similarly, most patients with microalbuminuria do not develop statitics progressive increase in their urinary statistlcs excretion as in the classic paradigm, and treatment-induced and spontaneous remission of Duabetic are commonly observed 10 Sratistics improvements in diabetes management have reduced the proportion of shatistics with Diaebtic who nephropatby CKD over any given time period 14 — 16their improved stafistics 1718 Diiabetic with bephropathy rising incidence Dlabetic both type 1 and type 2 Coconut milk benefits 19 have seen the prevalence of CKD nephropxthy to grow Nephroptahy the approximately million people Diavetic type 2 diabetes Diabetic nephropathy statistics 19 Duabetic, approximately half will have evidence of Diabetci Staristics incidence of CKD in type 1 diabetes Music therapy for depression from that observed in type 2 diabetes.
It is estimated that approximately one-third of all people with type 1 diabetes will develop CKD over the course of their lifetime 1522 — This difference is mostly because subjects with type 1 diabetes are generally younger and healthier at diagnosis and carry fewer co-morbid conditions than those with type 2 diabetes.
Consequently, the renal presentation in type 1 diabetes potentially better reflects DKD, rather than the mixed picture of CKD in type 2 diabetes that is confounded by omnipresent other contributors, such as ageing, vascular disease, insulin resistance and obesity. The incidence, presentation and course of CKD in patients with diabetes vary considerably across countries and settings 21 Fig.
Disadvantaged and minority populations also have a high prevalence of CKD and its subsequent progression. For example, the prevalence of albuminuria is nearly twice as common in Indigenous Australians in primary care compared with non-Indigenous Australian patients presenting to the same clinical practice The reasons for ethnic differences in CKD are complex 27 and include economic, social or educational disadvantage, access to and uptake of care, lower achievement of treatment goals, lower screening rates, suboptimal early treatment of complications, diet and lifestyle factors, smoking, obesity, genetic factors and developmental programming.
Another important feature is the younger age of onset of type 2 diabetes in these at-risk groups, which might be associated with a more malignant course, including accelerated β-cell loss in the pancreas, as well as renal and cardiovascular complications Data from patients with type 2 diabetes surveyed in the US NHANES III 4the Australian NEFRON study 5the Italian RIACE study 86and the DEMAND study Blue circles denote patients with albuminuria.
The percentage not included in either circle denotes patients without chronic kidney disease CKD. PowerPoint slide. This variability partly relates to the competing risk of premature mortality, chiefly owing to cardiovascular disease.
Many and probably most patients with CKD will die before they develop ESRD 1317 Moreover, as most patients with diabetes now reside in developing countries 19the few that develop ESRD will seldom be able to access renal replacement therapy RRT programmes. However, the unparalleled number of patients with diabetes makes this disease the leading single cause of ESRD.
In many countries, such as the United States, diabetes is present in more than half of all patients entering RRT programmes One ore more of the following criteria must be present for more than 3 months and validated by repeat testing before a clinical diagnosis of chronic kidney disease CKD can be made:.
DKD has been traditionally viewed as a microvascular disorder, clustered along with retinopathy and neuropathy, and separate from macrovascular disease that contributes to coronary heart disease, peripheral vascular disease and cerebrovascular disease.
However, each disorder can be considered to be a tissue-specific manifestation of the same pathogenetic process, and DKD is the renal manifestation of the same glucose-driven process that occurs at susceptible sites elsewhere in the body 31 — Although all cells are chronically exposed to high plasma glucose levels in patients with diabetes, only some show progressive dysfunction, of which the endothelial cells lining the vasculature are a prime example.
Specifically, the inability of endothelial cells to downregulate their glucose transport in response to high glucose levels 35 leads to an overwhelming flux of intracellular glucose, which triggers the generation of pathogenetic mediators that contribute to the development of diabetic complications, including DKD.
Excessive glucose flux leads to the generation of toxic intermediates, the most important of which are thought to be reactive oxygen species ROS. Excessive glucose flux can generate ROS in several different ways. Enhanced mitochondrial substrate oxidation with consequent enhanced mitochondrial membrane potential leads to the overproduction of superoxide.
At the same time, increased glucose flux leads to the activation of NADPH oxidase and uncoupling of nitric oxide synthase ROS-mediated DNA strand breaks in the nucleus activate DNA repair mechanisms, including the enzyme poly ADP ribose polymerase 1 PARP1which inhibits the key glycolytic enzyme glyceraldehydephosphate dehydrogenase GAPDH by polyADP-ribosylation.
Inhibition of GAPDH activity causes a bottleneck in glycolysis, resulting in the upstream accumulation of early glycolytic intermediates that are increasingly diverted into activating pathogenetic signalling pathways 3738 Fig. Together, these diversions lead to cellular dysfunction, inflammation, apoptosis and fibrosis in cells exposed to excessive glucose flux.
The central importance of ROS in initiating each of these processes is illustrated by the fact that each can be prevented when hyperglycaemia-mediated ROS generation is curtailed Mitochondrial production of reactive oxygen species ROS accelerates in response to an increase in intracellular glucose.
In addition, pathogenetic ROS are also generated through the ROS-induced uncoupling of nitric oxide synthase eNOS and inactivation of NADPH oxidases. ROS can mediate DNA damage, which in turn activates poly ADP ribose polymerase PARP. PolyADP-ribosylation of glyceraldehydedehydrogenase GAPDH by PARP leads to the inhibition of this key glycolytic enzyme and a subsequent bottleneck in glycolysis.
As a result, early glycolytic intermediates accumulate and are then diverted into pathogenetic signalling pathways. AGE, advanced glycation end-product; DAG, diacylglycerol; DHAP, dihydroxyacetone phosphate; GFAT, glutamine fructosephosphate amidotransferase; NF-κB, nuclear factor-κB; PKC, protein kinase C; RAGE, receptor for AGE; UDP-GLcNAc, uridine diphosphate N-acetylglucosamine.
Each cell has pathways that recognize and specifically respond to nutrient abundance to ensure efficient substrate use. In addition, podocyte-specific activation of mTOR recapitulates many features of DKD, including mesangial expansion and proteinuria 40 These findings have led to the concept of directed interventions to simulate energy depletion associated with increased activity of AMPK and sirtuins and reduced mTOR activity and promote efficient cellular function.
Experimental data seem to support this strategy for renoprotection 39 — 42and agents such as metformin, peroxisome proliferator-activated receptor PPAR agonists 3738phosphodiesterase inhibitors and resveratrol act on these pathways. Only one-third of patients with type 1 diabetes will develop overt nephropathy 1522 — 24whereas almost all patients with type 1 diabetes eventually develop some degree of retinopathy.
This suggests that additional risk factors beyond hyperglycaemia must also be involved in DKD. Indeed, although hyperglycaemia is an essential requirement for DKD, it is seldom the only contributor.
Pathogenetic pathways initiated and sustained in the kidney by elevated glucose levels can be enhanced by several different factors. These include a range of metabolic factors, including excess fatty acids, carbonyl and oxidative stress, as well as haemodynamic factors, including shear stress induced by transmitted systemic hypertension, impaired autoregulation, hyperperfusion and hypoperfusion, and activation of the renin—angiotensin—aldosterone system RAAS On their own, these factors do not cause DKD but rather, in the presence of diabetes, feed into and enhance common pathogenetic mechanisms that include increased levels of growth factors, vasoactive hormones, cytokines and chemokines in the kidney.
For example, glucose-induced endothelial dysfunction increases vascular susceptibility to shear stress, oxidative stress and other stressors. Endothelial dysfunction and subsequent microvascular rarefaction induced by hyperglycaemia also reduce blood flow while oxygen consumption is increased, leading to hypoxia.
In turn, renal hypoxia induces compensatory — but ultimately maladaptive — changes in blood flow, metabolism and polar vasculosis glomerular neoangiogenesis 44 — Despite the importance of the vascular endothelium in microvascular complications, many investigators propose that the early changes in renal glomeruli are critical for the subsequent development of glomerulosclerosis and nephron dropout Fig.
Among these changes, the most important might be dysfunction of glomerular podocytes, which are highly specialized terminally differentiated cells that cover the urinary side of the glomerular basement membrane GBM Together with glomerular endothelial cells, podocytes are responsible for the maintenance of the GBM, its charge barrier and the shape and integrity of the glomerular capillary loop; all functions that are compromised in the diabetic glomerulus.
Experimental models demonstrate that podocyte-specific injury can recapitulate a diabetes-like phenotype of glomerulosclerosis and tubulointerstitial fibrosis, even in the absence of hyperglycaemia Moreover, protecting podocytes from hyperglycaemia with a podocyte-specific deletion of the glucose transporter solute carrier family 2, facilitated glucose transporter member 4 SLC2A4; also known as GLUT4 51 or from the resulting oxidative stress 52 can prevent diabetes-associated albuminuria without restoring normal levels of glucose.
Such data place podocytes, and more particularly the dysregulation of their growth and differentiation, at the very centre of the pathogenesis of DKD. Some studies suggest that a reduction in podocyte density might be a useful predictor for DKD and its progression 53 Morphological and functional alterations to renal glomeruli are one of the hallmarks of diabetic kidney disease.
GBM, glomerular basement membrane. One of the earliest and most characteristic of all glomerular changes in diabetes is a homogenous thickening of the GBM 53 Thickening of the GBM is present in almost all patients with diabetes within a few years of diagnosis, although more pronounced changes are observed in DKD Whether GBM thickening is a marker of podocyte or endothelial dysfunction or a mediator of progressive DKD is unclear.
Certainly, changes in the composition, charge or architecture of the GBM associated with thickening could contribute to albuminuria.
Stiffening of the GBM might also reduce distensibility of the pericapillary wall and compromise the subpodocyte space, facilitating glomerular injury through haemodynamic mechanisms
: Diabetic nephropathy statistics| Diabetes and Chronic Kidney Disease | CDC | Diabrtic CAS Google Scholar Yokoi H, Diabetic nephropathy statistics M, Mori Diabetic nephropathy statistics, Statjstics M, Suganami T, Sawai K, Specialty food and drinks T, Saito Y, Ogawa Y, Kuwabara T, et al. Our findings ststistics that the npehropathy Diabetic nephropathy statistics rate of CKD-T2D among Djabetic global population aged 20—59 years is highest in the middle SDI regions, while the age-standardized death and DALY rates are highest in the low-middle SDI regions. de Zeeuw, D. Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, Hirsch IB, Kalantar-Zadeh K, Narva AS, Navaneethan SD, et al. Tubulointerstitial fibrosis is widely considered to be the final common pathway for loss of renal function in DKD Diabetes Rep. Brasacchio, D. |
| Epidemiology of Diabetic Nephropathy | Diabetes and the Kidney | Books Gateway | Karger Publishers | Nat Rev Nephrol — Hansson E, Mansourian A, Farnaghi M, Petzold M, Jakobsson K. An Ecological Study of Chronic Kidney Disease in Five Mesoamerican Countries: Associations With Crop and Heat. BMC Public Health Bjornstad P, Cherney DZ. Renal Hyperfiltration in Adolescents With Type 2 Diabetes: Physiology, Sex Differences, and Implications for Diabetic Kidney Disease. Curr Diabetes Rep Koye DN, Magliano DJ, Nelson RG, Pavkov ME. The Global Epidemiology of Diabetes and Kidney Disease. Adv Chronic Kidney Dis — GBD Chronic Kidney Disease Collaboration Global, Regional, and National Burden of Chronic Kidney Disease, A Systematic Analysis for the Global Burden of Disease Study Fraser SDS, Roderick PJ. Kidney Disease in the Global Burden of Disease Study Nat Rev Nephrol —4. Roumeliotis S, Mallamaci F, Zoccali C. Endothelial Dysfunction in Chronic Kidney Disease, From Biology to Clinical Outcomes: A Update. J Clin Med Hu Y, Lei M, Ke G, Huang X, Peng X, Zhong L, et al. Metformin Use and Risk of All-Cause Mortality and Cardiovascular Events in Patients With Chronic Kidney Disease-A Systematic Review and Meta-Analysis. Front Endocrinol Lausanne Bowe B, Xie Y, Li T, Mokdad AH, Xian H, Yan Y, et al. Changes in the US Burden of Chronic Kidney Disease From to An Analysis of the Global Burden of Disease Study. JAMA Netw Open 1:e Nahvijou A, Arab M, Faramarzi A, Hashemi SY, Javan-Noughabi J. Burden of Esophageal Cancer According to World Health Organization Regions: Review of Findings From the Global Burden of Disease Study Health Scope 8:e Rahmani H, Sarabi Asiabar A, Niakan S, Hashemi SY, Faramarzi A, Manuchehri S, et al. Burden of Esophageal Cancer in Iran During Review of Findings From the Global Burden of Disease Studies. Med J Islam Repub Iran Chertow GM, Pergola PE, Farag YMK, Agarwal R, Arnold S, Bako G, et al. Vadadustat in Patients With Anemia and Non-Dialysis-Dependent CKD. N Engl J Med — Deng Y, Zhao P, Zhou L, Xiang D, Hu J, Liu Y, et al. Epidemiological Trends of Tracheal, Bronchus, and Lung Cancer at the Global, Regional, and National Levels: A Population-Based Study. J Hematol Oncol Deng Y, Li H, Wang M, Li N, Tian T, Wu Y, et al. Global Burden of Thyroid Cancer From to JAMA Netw Open 3:e Shaw JE, Sicree RA, Zimmet PZ. Global Estimates of the Prevalence of Diabetes for and Diabetes Res Clin Pract — Shepard BD. Sex Differences in Diabetes and Kidney Disease: Mechanisms and Consequences. Am J Physiol Renal Physiol F—f Insaf TZ, Strogatz DS, Yucel RM, Chasan-Taber L, Shaw BA. Associations Between Race, Lifecourse Socioeconomic Position and Prevalence of Diabetes Among US Women and Men: Results From a Population-Based Panel Study. J Epidemiol Community Health — White S, Chadban S. Diabetic Kidney Disease in Australia: Current Burden and Future Projections. Nephrology Carlton Vic —8. Groop PH, Thomas MC, Moran JL, Wadèn J, Thorn LM, Mäkinen VP, et al. The Presence and Severity of Chronic Kidney Disease Predicts All-Cause Mortality in Type 1 Diabetes. Diabetes —8. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease. Am J Kidney Dis 69 3 Suppl 1 :A7—A8. Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A Systematic Analysis of Global Anemia Burden From to Blood — Global Burden of Disease Study Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived With Disability for Acute and Chronic Diseases and Injuries in Countries, A Systematic Analysis for the Global Burden of Disease Study Wirth JP, Rohner F, Woodruff BA, Chiwile F, Yankson H, Koroma AS, et al. Anemia, Micronutrient Deficiencies, and Malaria in Children and Women in Sierra Leone Prior to the Ebola Outbreak - Findings of a Cross-Sectional Study. PloS One e Rami-Merhar B, Hofer SE, Fröhlich-Reiterer E, Waldhoer T, Fritsch M. Pediatr Diabetes —6. Tirapani LDS, Fernandes N. A Narrative Review of the Impacts of Income, Education, and Ethnicity on Arterial Hypertension, Diabetes Mellitus, and Chronic Kidney Disease in the World. Saudi J Kidney Dis Transpl — Kaze AD, Ilori T, Jaar BG, Echouffo-Tcheugui JB. Burden of Chronic Kidney Disease on the African Continent: A Systematic Review and Meta-Analysis. BMC Nephrol Liu J, Ren ZH, Qiang H, Wu J, Shen M, Zhang L, et al. Trends in the Incidence of Diabetes Mellitus: Results From the Global Burden of Disease Study and Implications for Diabetes Mellitus Prevention. Motala AA, Omar MA, Pirie FJ. Diabetes in Africa. Epidemiology of Type 1 and Type 2 Diabetes in Africa. J Cardiovasc Risk — Horlyck-Romanovsky MF, Wyka K, Echeverria SE, Leung MM, Fuster M, Huang TT. Foreign-Born Blacks Experience Lower Odds of Obesity But Higher Odds of Diabetes Than US-Born Blacks in New York City. J Immigr Minor Health — Wunna W, Tsoutsouki J, Chowdhury A, Chowdhury TA. Advances in the Management of Diabetes: New Devices for Type 1 Diabetes. Postgrad Med J 97 — Clements JM, West BT, Yaker Z, Lauinger B, McCullers D, Haubert J, et al. Disparities in Diabetes-Related Multiple Chronic Conditions and Mortality: The Influence of Race. Diabetes Res Clin Pract Golden SH, Brown A, Cauley JA, Chin MH, Gary-Webb TL, Kim C, et al. Health Disparities in Endocrine Disorders: Biological, Clinical, and Nonclinical Factors—An Endocrine Society Scientific Statement. J Clin Endocrinol Metab E— Rosenstock S, Whitman S, West JF, Balkin M. Racial Disparities in Diabetes Mortality in the 50 Most Populous US Cities. J Urban Health — Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic Differences in Mortality, End-Stage Complications, and Quality of Care Among Diabetic Patients: A Review. Diabetes Care —8. Myers OB, Pankratz VS, Norris KC, Vassalotti JA, Unruh ML, Argyropoulos C. Surveillance of CKD Epidemiology in the US - a Joint Analysis of NHANES and KEEP. Sci Rep Pleniceanu O, Twig G, Tzur D, Gruber N, Stern-Zimmer M, Afek A, et al. Kidney Failure Risk in Type 1 vs. Type 2 Childhood-Onset Diabetes Mellitus. Pediatr Nephrol 36 2 — Pacilli A, Viazzi F, Fioretto P, Giorda C, Ceriello A, Genovese S, et al. Epidemiology of Diabetic Kidney Disease in Adult Patients With Type 1 Diabetes in Italy: The AMD-Annals Initiative. Diabetes Metab Res Rev e Brown WW, Peters RM, Ohmit SE, Keane WF, Collins A, Chen SC, et al. Early Detection of Kidney Disease in Community Settings: The Kidney Early Evaluation Program KEEP. Am J Kidney Dis — Keywords: diabetes-related chronic kidney disease, mortality, disability-adjusted life-years, incidence, prevalence. Citation: Deng Y, Li N, Wu Y, Wang M, Yang S, Zheng Y, Deng X, Xiang D, Zhu Y, Xu P, Zhai Z, Zhang D, Dai Z and Gao J Global, Regional, and National Burden of Diabetes-Related Chronic Kidney Disease From to Received: 26 February ; Accepted: 17 June ; Published: 01 July Copyright © Deng, Li, Wu, Wang, Yang, Zheng, Deng, Xiang, Zhu, Xu, Zhai, Zhang, Dai and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. Book Series: Contributions to Nephrology. Subject Area: Endocrinology , Further Areas , Nephrology , Pathology and Cell Biology. Publication date:. Book Details. Chapter Navigation. Book Chapter. Reutens Anne T. School of Public Health and Preventive Medicine, Monash University, and Baker IDI Heart and Diabetes Institute, Melbourne, Vic, Australia. Robert C. Atkins Robert C. Topic Article Package: Topic Article Package: Diabetes. Publication history 0 9. Cite Icon Cite. toolbar search search input Search input auto suggest. You do not currently have access to this chapter. Sign in Don't already have an account? Individual Login LOGIN TO MY KARGER. Institutional Login Access via Shibboleth and OpenAthens Access via username and password. Digital Version Pay-Per-View Access. BUY THIS Chapter. Print Version. Buy Token. Related Topics diabete. Email alerts Latest Book Alert. Approximately 1 in 3 adults with diabetes has CKD. Both type 1 and type 2 diabetes can cause kidney disease. Each kidney is made up of millions of tiny filters called nephrons. Many people with diabetes also develop high blood pressure , which can damage kidneys too. You can help keep your kidneys healthy by managing your blood sugar, blood pressure, and cholesterol levels. This is also very important for your heart and blood vessels—high blood sugar, blood pressure, and cholesterol levels are all risk factors for heart disease and stroke. If you have prediabetes, taking action to prevent type 2 diabetes is an important step in preventing kidney disease. You can do that by eating healthier and getting minutes of physical activity each week. Find a program in your community or online. Skip directly to site content Skip directly to search. Español Other Languages. Diabetes and Chronic Kidney Disease Español Spanish Print. Minus Related Pages. |
| Diabetes and Chronic Kidney Disease | Indeed, some data suggest such approaches can even reverse early glomerulopathy. Burrows, N. This can lead to kidney damage and cause high blood pressure. Diabetes Endocrinol. View Article Google Scholar 9. This may be a significant contributing factor to the increased disease burden of CKD-T2D observed in middle SDI and low-middle SDI regions. Drugs 18 , 55—70 |
| Top bar navigation | Cite Icon Cite. toolbar search search input Search input auto suggest. You do not currently have access to this chapter. Sign in Don't already have an account? Individual Login LOGIN TO MY KARGER. Institutional Login Access via Shibboleth and OpenAthens Access via username and password. Digital Version Pay-Per-View Access. BUY THIS Chapter. Print Version. Buy Token. Related Topics diabete. Email alerts Latest Book Alert. Related Book Content Islets of Langerhans in Various States of Glucose Intolerance. Automated Peritoneal Dialysis — Indications and Management. Cardiac Transplantation for the Treatment of Endstage Ischemic Cardiomyopathy. Chronic Kidney Disease and Diabetic Retinopathy. Clinical Manifestation and Natural History of Diabetic Nephropathy. Pathophysiology of Acute Kidney Injury: A New Perspective. Related Articles Choosing a Treatment Modality for the Infant, Child and Adolescent with Endstage Renal Disease. Neutrophil Gelatinase-Associated Lipocalin and Retinol-Binding Protein-4 as Biomarkers for Diabetic Kidney Disease. Early Biomarkers of Fabry Nephropathy: A Review of the Literature. Myopathy in Marinesco-Sjogren Syndrome. Low-Output Left Ventricular Failure in End-Stage Renal Disease. Nephroblastoma Associated with Mesangioproliferative Glomerulonephritis. Exercise Training Reduces Coronary Risk and Effectively Rehabilitates Hemodialysis Patients. Extensive Thrombus Formation in the Right Ventricle due to a Rare Combination of Arrhythmogenic Right Ventricular Cardiomyopathy and Heterozygous Prothrombin Gene Mutation G A. Ibopamine as a Valuable Adjunct and Substitute for Dopamine in Bridging Therapy before Heart Transplantation. Debate: PRO Position. Should Microalbuminuria Ever Be Considered as a Renal Endpoint in Any Clinical Trial. Karger International S. Karger AG P. O Box, CH Basel Switzerland Allschwilerstrasse 10, CH Basel. Facebook LinkedIn X YouTube WeChat Experience Blog. Privacy Policy Terms of Use Imprint Cookies © S. Karger AG, Basel. This Feature Is Available To Subscribers Only Sign In or Create an Account. Close Modal. ND, no data. The incidence of ESRD from the population with diabetes was reported from 19 countries or territories during — Supplementary Table Twenty-eight data points were comparable plus 16 studies focusing on type 1 diabetes or special subgroups. From to , the global ESRD prevalence doubled from In , 72 of 85 countries Similar patterns were observed for the differences in counts or percentages in the data from and Supplementary Figs. In , based on the model, 40 of 44 countries Moreover, the estimates of ESRD prevalence in 31 countries This study yielded three major findings. First, the proportion of prevalent ESRD patients with diabetes continued to rise worldwide. The slowest annual increase in this proportion was observed in Europe, but nearly threefold increase was reported in the Eastern Mediterranean and Western Pacific regions. Second, the importance of diabetes as a risk factor for ESRD was observed both in high-income countries and in increasing numbers of developing and underdeveloped countries. Third, substantial geographic variation was observed in the incidence of ESRD among patients with diabetes. Remarkably, the incidence in Western Pacific countries was twice the world average and thrice that of the lowest incidence observed in Europe. Our findings reveal that the expansion of populations with diabetes among the ESRD patients is a global phenomenon, and it does not appear to be stoppable anytime soon. Special consideration should be given to the challenges of providing care to an ESRD population with a higher proportion of patients with preexisting diabetes. We should appreciate the fact that diabetes is becoming the dominant risk factor for ESRD in developing and underdeveloped countries—not just as seen in the developed countries. Interestingly, decrease of the percentage of incident ESRD patients due to diabetes was seen in five European countries and three African countries Table 1 , even though their diabetes prevalence kept increasing as in all other countries. Risk stratification based on geographic origins may be needed to identify populations with diabetes that should be targeted more aggressively to prevent the initiation of renal complications or halt further deterioration. Our survey for the incidence of ESRD among populations with diabetes with a global perspective may help disclose a mechanism in determining the progression of diabetic kidney disease. The international variation was enormous, yet the pattern was nonrandom. One potential explanation is the competing risks between death and kidney failure in patients with diabetes Our equation included only patients treated with RRT and did not consider those who died of cardiovascular or renal complications before reaching ESRD. This incidence may be deceptively lower in countries where a higher proportion of patients with diabetes died before reaching ESRD due to lack of appropriate care or delayed initiation of RRT or soon after reaching ESRD due to lack of RRT or voluntary choice of conservative treatment. Proper care including blood pressure control, blockade of renin-angiotensin system, awareness of CKD itself, and timely referral to a nephrologist can halt the progression of diabetic kidney disease, but they were inadequate in many underdeveloped countries As the aging population is more vulnerable to the progression to ESRD, the developed countries with a higher proportion of older patients with diabetes should have more patients with diabetes entering ESRD. However, our analysis of data from countries in Western Europe versus those in industrialized area of Asia Japan, Taiwan, South Korea basically excluded the possible effects of age, sex, and RRT access. Tobacco smoking is known to increase the risks of mortality and vascular complications in patients with diabetes This small discrepancy is far less than the fold difference in the annual rate of incident ESRD among patients with diabetes between these countries. The effects of climate 26 or air pollution 27 are said to be important but inconclusive. The existence of an unknown protective environmental factor is supported by the finding that the annual incidence of ESRD among patients with diabetes in Northwestern Europe Denmark, Finland, Iceland, Norway, Sweden, U. ranged from to pmp in compared with 1, pmp among people in the U. Food choice such as high meat intake is another risk factor for the progression of diabetes complications Interestingly, Fuller and Rowlands proposed a long-lasting difference in food selection and preparation between eastern and western Asia since BC: grinding, roasting, and bread baking in western Eurasia, including the Mediterranean region, versus whole grain boiling and steaming in China and the Far East Asian people with diabetes have a greater risk of developing related complications than their counterparts in Western countries; consequently, the former population also faces higher risks of all-cause and cause-specific mortality 30 , Data from the USRDS indicated that from to , the age- and sex-adjusted incidence of ESRD due to diabetes was 3. A longitudinal observational study of 62, patients with diabetes conducted at Kaiser Permanente of Northern California reported adjusted hazard ratios for ESRD of 2. In a sample of patients with diabetes with advanced CKD estimated glomerular filtration rate of We used two approaches to validate our model. First, we compared our data regarding the annual incidence of ESRD among patients with diabetes with data from a limited number of literature reports. The data in the latter sources were generally higher because the study populations had been carefully followed and all recruited case subjects reached ESRD. In contrast, our model had a larger denominator because it included the entire population at risk i. Second, we compared the ESRD prevalence in this study with the data provided by Fresenius Medical Care and determined a high level of similarity, with few exceptions. Accordingly, the Fresenius data set is validated as an accurate reference. Furthermore, the similarities between our estimates and the Fresenius data vindicate the model-building concept in our study in terms of estimating the global ESRD prevalence. Only six countries, namely, India, Myanmar, Sri Lanka, China, Vietnam, and Bangladesh, showed a twofold difference between the reported or estimated ESRD prevalence and the Fresenius data. For the first three countries and Yemen , we estimated the prevalence of ESRD patients requiring RRT, which was the prevalence of treated ESRD multiplied by a ratio between the ESRD patients who required RRT and those who received it. Apparently, this correction made the estimates remarkably high. Take India, for example. The sample to report the prevalence in China was presumably overrepresenting because the subjects were urban residents and insured The ESRD prevalence for Vietnam was derived from the total number of dialysis patients and, hence, supposed to be more accurate than the Fresenius data. The data of ESRD prevalence in Bangladesh were obtained from the USRDS and were considered authorized. This study had a few limitations. First, even in a patient with diabetes, ESRD may or may not be caused by diabetic nephropathy; diabetes might simply be a comorbidity with ESRD The annual incidence of diabetes-related ESRD may have been overestimated. Second, the incidence of ESRD mostly described treated ESRD patients instead of the entire population who had reached ESRD, regardless of the RRT status. Accordingly, the calculated annual incidence of ESRD among patients with diabetes would have been considerably underestimated. Third, our model equation was based on the number of patients with prevalent diabetes, who had diabetes for various periods of time. A patient with long-standing diabetes might progress to ESRD much sooner than a newly diagnosed, or incident, diabetes patient. Thus, the annual rate of ESRD from an incident, or inception, diabetes cohort might have been lower than our estimates 14 , The annual rate of ESRD among patients with diabetes might become deceptively low in those countries with high prevalence of undiagnosed diabetes because of missing those real cases of ESRD with diabetes. Fourth, our estimates on the percentages of national incident and prevalent ESRD patients with diabetes from studies that recruited only relatively small numbers of subjects, or that focused on not-yet-in-ESRD CKD patients, are possibly inaccurate. Fifth, there was no consensus in determining an acceptable margin of error in the comparison between our ESRD prevalence and the Fresenius data. However, the estimates were very close to the actual conservative estimate of 1, pmp according to a local expert In conclusion, our study has provided a global overview of diabetes-related kidney failure during — Notably, we observed substantial differences in both the extent of ESRD incidence in patients with diabetes and the trends over time among the geographic regions. These differences highlight the decisive role of distinct factors in the progression of diabetic kidney disease, and the importance of tailoring the efforts to prevent and treat the affected patients, with the aim of easing the ever-increasing burden of this disease. is funded by grants from the Ministry of Science and Technology, Taiwan BMY3, B and the National Taiwan University Hospital Hsin-Chu Branch HCH, HCH, HCH, HCH, HCH is funded by grants from the Ministry of Science and Technology, Taiwan. Duality of Interest. No potential conflicts of interest relevant to this article were reported. Author Contributions. and K. initiated and developed the study. derived the model, collated the data, performed the analysis, produced tables and figures, and drafted the manuscript. and X. processed and provided the relevant data. All authors interpreted the results and gave advice for revision. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 44, Issue 1. Previous Article Next Article. Research Design and Methods. Article Information. Article Navigation. Worldwide Epidemiology of Diabetes-Related End-Stage Renal Disease, — Hui-Teng Cheng Hui-Teng Cheng. Corresponding authors: Hui-Teng Cheng, hcheng wustl. edu , and Kuan-Yu Hung, kyhung ntu. This Site. Google Scholar. Xiaoqi Xu ; Xiaoqi Xu. Paik Seong Lim ; Paik Seong Lim. Kuan-Yu Hung Kuan-Yu Hung. Diabetes Care ;44 1 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Percentage of prevalent ESRD patients or incident ESRD patients with diabetes worldwide from years to Percentage of prevalent ESRD patients with diabetes. Yearly change rate slope. View Large. Table 2 ESRD incidence rates and prevalence in people pmp worldwide from years to ESRD incidence rates in pmp. Table 3 Annual incidence of ESRD among patients with diabetes worldwide and by the WHO regions or the World Bank income groups from years to Annual incidence of ESRD among patients with diabetes in pmp. Figure 1. View large Download slide. World Health Organization. International Diabetes Federation. Search ADS. Meguid El Nahas. The ascending rank of chronic kidney disease in the global burden of disease study. Changes in excess mortality from end stage renal disease in the United States from to Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. United States Renal Data System. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. The global burden of chronic kidney disease: estimates, variability and pitfalls. Incidence of end-stage renal disease attributed to diabetes among persons with diagnosed diabetes - United States and Puerto Rico, Cumulative risk of end-stage renal disease among patients with type 2 diabetes: a nationwide inception cohort study. The incidence of end-stage renal disease in the diabetic compared to the non-diabetic population: a systematic review. Incidence of chronic kidney disease among people with diabetes: a systematic review of observational studies. |
| Diabetic kidney disease | Nature Reviews Disease Primers | Certainly, Diabetic nephropathy statistics weight loss is Diabetic nephropathy statistics statietics reduced Diabettic of progressive CKD in diabetes, and Diagetic of albuminuria has Herbal mood enhancers observed following Diabetic nephropathy statistics surgery Dixbetic, Increase endurance for marathons a nephgopathy data base registry will provide a better understanding and accurate assessment of this chronic complication and its related risk factors. Asian people with diabetes have a greater risk of developing related complications than their counterparts in Western countries; consequently, the former population also faces higher risks of all-cause and cause-specific mortality 30 About this article. Figure 4 The age-standardized rates of CKD-DM among 21 regions based on SDI in |

Diabetic nephropathy statistics -
These fibrogenic cells might be derived from several different sources, including transformation of resident fibroblasts and mesenchymal stem cells, recruitment of fibroblasts from the bone marrow, and tubuloepithelial to mesenchymal trans -differentiation 76 Fig.
The myofibroblasts responsible for the matrix deposition that leads to tubulointerstitial fibrosis in diabetic kidney disease DKD are derived from various sources. Transformation of local resident fibroblasts, mesenchymal stem cells and bone marrow-derived fibrocytes and the induction of endothelial to mesenchymal and tubuloepithelial to mesenchymal transitions are the main contributors The same clinical presentation of DKD can be associated with a heterogeneous range of pathological features, including nodular or diffuse glomerulosclerosis, tubulointerstitial fibrosis, tubular atrophy and renal arteriolar hyalinosis, alone or in combination.
The presence and severity of each of these features are independently associated with the risk of progressive renal disease, but not always with each other A histopathological staging system for glomerular lesions has been proposed 77 Box 2. However, its predictive utility remains to be established.
Routine renal biopsy is not feasible or clinically appropriate beyond a research setting, and DKD remains a clinical diagnosis in most patients with diabetes.
Several different factors contribute to the development of CKD in patients with diabetes Box 3. Some of these factors, including hyperglycaemia, hypertension, weight gain and dyslipidaemia, are potentially modifiable through optimized diabetes care. Moreover, robust clinical data show that intensive diabetes management significantly reduces the cumulative incidence of albuminuria, renal impairment and ESRD.
Indeed, the major decline in the incidence of CKD over the past 30 years is considered to be largely attributable to improved diabetes care 14 , Young age at onset of diabetes Genetic factors Family history of diabetic kidney disease, type 2 diabetes, non-diabetic chronic kidney disease, hypertension or insulin resistance.
Hypertension mean, variability and maximal 92 — Dyslipidaemia 98 — , , Socioeconomic disadvantage — Obesity 28 , , Smoking Insulin resistance or metabolic syndrome 51 , — Recurrent or chronic infections , Episodes of acute kidney injury Advanced glycation end-products Oral contraceptive use Hyperuricaemia Vitamin D deficiency The most important risk factor for CKD is hyperglycaemia.
Although there are some structural similarities to other renal diseases, fundamentally, the phenotype of DKD is only observed in the context of elevated glucose levels. Elliot Joslin first hypothesized a relationship between glucose and diabetic complications However, the defining prospective clinical study by Jean Pirart and his Belgian colleagues unequivocally demonstrated that the degree and duration of hyperglycaemia were associated with microvascular complications, including CKD Subsequently, randomized controlled trials have validated this causal link in both type 1 diabetes 80 and type 2 diabetes 81 , Nevertheless, although conventional markers of glucose levels, such as glycated haemoglobin HbA1c , are associated with the incidence of microalbuminuria, it is also clear that many patients with poor glycaemic control do not develop renal complications, whereas others do despite intensive interventions and dedicated compliance Fig.
This discordance might be because markers such as HbA1c fail to capture the dynamic dysglycaemia associated with diabetes. Indeed, even in the absence of chronic hyperglycaemia, transient hyperglycaemia, transient hypoglycaemia or increased glycaemic variability around a normal mean might have long-lasting and long-term effects on the development and progression of complications related to diabetes, including renal disease 83 — and M.
Alternatively, past periods of poor glucose control, even before diagnosis, could also have a long-lasting legacy in the kidney, and therefore the risk for DKD might not be represented by current or recent HbA1c levels. The physiological mechanism or mechanisms responsible for metabolic karma remain poorly defined but might include epigenetic programming, remodelling and persistent post-translational modifications, such as advanced glycation end-products Further understanding the molecular basis of a metabolic legacy in diabetes will certainly provide new targets for intervention to reduce the burden of CKD in patients with diabetes.
Elevated blood pressure is an important risk factor for the development CKD in both type 1 and type 2 diabetes 92 — In individuals with type 1 diabetes, blood pressure levels are usually normal at diagnosis, but become elevated proximate to the onset of microalbuminuria In type 2 diabetes, other factors contribute to the presence and severity of hypertension, which may precede CKD by many years or follow in its wake.
This importance of hypertension to the pathogenesis of renal damage can be partly explained by the loss of renal autoregulation in diabetes, whereby systemic pressure is directly transmitted to vulnerable glomerular capillaries 96 , Consequently, there is no specific cut-off above which the specific risk for CKD can be denoted or below which the therapeutic impact of blood pressure control on the development of albuminuria can be ignored in patients with diabetes.
Dyslipidaemia is another important risk factor for the development of CKD in diabetes. In particular, elevated triglycerides, non-low-density lipoprotein cholesterol, apolipoprotein-B or low high-density lipoprotein HDL cholesterol levels are independently associated with the development of CKD in both type 1 and type 2 diabetes 98 , For example, HDL might not only lose its vasoprotective, antioxidant and anti-inflammatory properties in CKD, but dysfunctional HDL can be directly pathogenetic Detailed analyses of lipid sub-fractions have suggested that HDL3-cholesterol, sphingomyelin, apolipoprotein a , apolipoprotein A-I and apolipoprotein A-II, apolipoprotein C-I and triglyceride enrichment might all be independently associated with progressive DKD , However, exactly which lipids or lipoproteins are the most important in the pathogenesis of CKD in diabetes remains unclear.
Insulin resistance is also independently associated with CKD beyond its indirect links with glucose, blood pressure, body weight and lipid control — Insulin-sensitizing interventions for example, thiazolidinedione therapy, exercise and weight loss all reduce albuminuria beyond their actions on metabolic control.
Impaired insulin sensitivity also results in altered renal cell glucose metabolism At the same time, increased insulin signalling as a result of compensatory hyperinsulinaemia in the setting of pathway-selective insulin resistance might also contribute to abnormal vasoreactivity, angiogenesis, fibrogenesis and other pathways implicated in progressive renal disease as well as atherogenesis CKD is more prevalent and develops more rapidly in people with diabetes who are obese than their normal-weight counterparts This is one major reason why the cumulative incidence of CKD is greater in type 2 diabetes than type 1 diabetes Obesity negatively influences the major risk factors associated with CKD, including lipid, blood pressure and glucose control, as well as promoting insulin resistance.
Obesity also has direct effects on the kidney, including changes in intraglomerular haemodynamics, increased sympathetic activity, hypertension, systemic inflammation, endothelial dysfunction, altered expression of growth factors and renal compression associated with visceral adiposity.
Indeed, even in the absence of diabetes, obesity may be associated with an increased frequency and severity of albuminuria , and obesity-related glomerulopathy has been extensively described The majority of the variability in incident CKD remains unaccounted for by conventional risk factors.
Although an inherited predisposition for DKD is evident and several potential loci have been reproducibly associated with CKD Table 1 , most genetic variants associated with CKD lie in non-coding regions. Overall, current evidence suggests that the genetic code explains only a small amount of why some individuals develop CKD and some do not Furthermore, any role for these genes, alone or in combination, in the molecular pathobiology of CKD remains to be established Although the genetic programming for CKD remains elusive, risk can be imprinted through other means.
In particular, epigenetics has emerged as an increasingly powerful paradigm to understand complex non-Mendelian diseases, including CKD.
Persistent epigenetic changes can be acquired during development or in adaptations following environmental exposure the so-called environmental footprint , including metabolic fluctuations associated with diabetes 83 , — These epigenetic modifications — including changes in DNA methylation, histone modification and chromatin structure — store, retain and recall past experiences in a way that can shape the transcription of specific genes and, therefore, cellular functions Technological advances now make it possible to initiate epigenome-wide association studies to identify epigenetic marks associated with disease across the whole genome , , with comparable resolution and throughput to genome-wide studies.
For example, some studies have identified differentially methylated regions in individuals with diabetes with CKD compared to those without CKD , Many of the genes identified were also differentially expressed, including some that had been previously linked to CKD in genome-association studies.
However, the broader utility of epigenetic markers to identify imprinted risk in individual patients beyond conventional risk factors remains to be established. Cells are more sensitive to this epigenetic programming during development and differentiation, when gene regulatory regions are established.
However, programming can also include constitutional or structural endowment. For example, reduction in nephron mass and filtration area associated with intrauterine growth retardation, maternal diabetes or vitamin A deficiency can increase the risk of CKD — At present, intrauterine growth retardation affects one-quarter of live births in developing countries, the same countries in which the risk of diabetes and CKD are also the greatest The eGFR is a measure of the flux of plasma fluid filtered from the glomerular capillaries into the Bowman's capsule per unit time Fig.
The eGFR can be inexpensively estimated using an appropriate mathematical formula from the serum creatinine levels, and patient age, gender and ethnicity. This calculation is often performed automatically by clinical pathology services. However, serum creatinine is notably variable within individuals and is modified by several different factors such as hydration status, physical activity and muscle mass , meaning that repeat testing is important to verify any abnormal results.
There is no place for the formal measurement of GFR using inulin, iothalamate or other substrates in the routine clinical assessment of renal function in patients with DKD , The second element used to identify individuals with diabetes and CKD is to detect those with persistently elevated urinary albumin excretion 5 , 6 Box 1.
When the kidneys are healthy, little or no intact albumin enters the urine, meaning that the presence of albumin in the urine can be used to denote abnormal kidney function.
Urinary albumin excretion can also be estimated in several different ways. The preferred method measures the concentration of albumin in a urine sample using a sensitive assay, adjusting the result for the urinary creatinine concentration.
This metric is known as the ACR and is considered the most practical way to adjust for the void volume and urine concentration 5 , 6. The ACR is best determined in urine collected at the first void in the morning, but can also be performed in a random manner; for example, at the time of a medical visit.
Timed urine collections for example, 4-hourly, overnight or hourly urine collections are also used but are time-consuming and seldom adequately performed outside hospital settings.
Spot tests of urinary albumin concentration are not recommended as the concentration of urine varies considerably from void to void. A positive urinary dipstick test or elevated urine albumin concentration is almost always associated with an abnormal ACR However, fewer than half of adults with both type 2 diabetes and an abnormal ACR have an elevated urinary albumin concentration or a positive dipstick test If albumin excretion is within the normal range in all three initial tests, further screening is repeated on an annual basis.
Any negative result, in an individual with previously negative tests, can simply be repeated annually as part of routine assessment for complications, as it is unlikely that significant CKD has been missed. However, any de novo abnormal results should be confirmed with an additional two tests during the 3—6 months 5 , 6.
Cut-off values for defining what constitutes elevated urinary albumin excretion vary from guideline to guideline. Formulae to estimate urinary albumin excretion using a single sample are also available, and as for GFR estimation, these might better adjust for demographic confounders All patients with type 2 diabetes should have their renal function screened at least annually post diagnosis, using both ACR and eGFR , as both criteria are independently as well as synergistically associated with mortality and progression to ESRD In adults with type 1 diabetes, annual screening should begin at most 5 years after diagnosis.
Critically, such screening enables the identification of susceptible individuals so that appropriate preventive actions can be taken. Although screening for albuminuria and renal impairment will identify most patients who are at risk of CKD, advanced and irreparable structural damage might already be present by the time CKD is diagnosed.
Developing practical ways to identify patients with good prognoses from those with poor prognoses remain important for the management of patients with diabetes and CKD, especially in the primary care setting.
Some researchers have developed models incorporating additional clinical variables such as age, ethnicity and retinopathy status for risk stratification , , although most of the variability in these models can be predicted on the basis of eGFR and albumin excretion alone Nevertheless, incorporating some of these additional patient variables adds to their predictive utility.
An unmet clinical need is to identify novel biomarkers that have the potential to both diagnose and risk stratify CKD in patients with diabetes earlier than current techniques. Indeed, a number of individual biomarkers have been proposed Box 4.
Other studies have attempted to more broadly identify at-risk profiles using urine proteomics , metabolomics and analysis of urinary exosomes for microRNA However, none of these techniques is currently applicable to the hundreds of millions of people with diabetes worldwide.
Inflammatory markers for example, C-reactive protein, fibrinogen, serum amyloid A protein, interleukin-6, interleukin and intercellular adhesion molecule 1. Intensive management of diabetes, including concurrent control of glucose, lipids and blood pressure as well as diet and lifestyle modifications, can slow the progression of established DKD 17 , 18 , — Indeed, some data suggest such approaches can even reverse early glomerulopathy.
For example, pancreatic transplantation, which restores normal glucose levels in patients with type 1 diabetes, is able to ameliorate the renal histological changes associated with diabetes However, it takes at least 10 years to observe any regression , and metabolic control with standard therapy can seldom achieve that observed following pancreatic transplantation.
Even with intensive management in the robust setting of clinical trials detailed below, many patients with diabetes still experience a progressive decline in renal function. This finding has led to the suggestion that, at best, current therapy simply delays the inevitable.
Nonetheless, in the clinical setting, any delay in CKD has potentially profound effects on patient health. Whether preventing hyperglycaemia is sufficient on its own to treat progressive CKD once it is established is uncertain. Significant reductions in albuminuria and its progression are certainly observed following intensification of glucose control using standard therapies in both type 1 and type 2 diabetes , However, within the limited confines of clinical trials, no significant effect has been observed on other renal outcomes, including doubling of the serum creatinine level, ESRD or death from renal disease Nonetheless, 6.
Moreover, this effect seemed to be entirely attributable to improved glucose control In addition, over the course of the EDIC study, RRT haemodialysis, peritoneal dialysis or renal transplantation was needed in only 8 participants in the intensive-therapy group, whereas 16 patients in the conventional-therapy group required RRT.
Furthermore, the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation ADVANCE study of 11, patients with type 2 diabetes also reported that fewer patients required RRT following intensification of glucose control compared with a control group.
Moreover, as with the EDIC study, a recent 5-year follow-up of the ADVANCE study confirmed this renal benefit However, total ESRD events RRT plus deaths from renal disease Fig.
Whether intensive glycaemic control has any influence on cardiovascular or mortality outcomes when initiated late, that is, after patients have established DKD or cardiovascular disease, also remains controversial Incidence of end-stage renal disease ESRD stratified according to intervention group, whereby patients were subjected to either blood pressure BP lowering or glucose lowering treatments.
Neither BP-lowering nor glucose-lowering treatment significantly reduced the incidence of ESRD Similarly, intensification of glucose control in patients with diabetes and CKD can be problematic as the multiple agents and high doses that are often required exposes patients to an increased risk of adverse drug reactions.
Each class of glucose-lowering agent has some limitations Box 5. In particular, the risk of severe hypoglycaemia is independently associated with a reduced eGFR and elevated urinary albumin excretion The increased risk of hypoglycaemia in patients with CKD can be explained by several different factors that include prescribing practices in this setting, altered insulin and drug pharmacology including drug and metabolite accumulation, inadequate compensatory gluconeogenesis in CKD and flattening of the relationship between mean glucose control and HbA1c.
Thus, careful individualized targeting, prescribing, patient education, planning and vigilance for hypoglycaemia are all important components in the management of CKD.
Where possible, glucose-lowering agents not associated with hypoglycaemia are preferred, especially those not limited by renal impairment or associated co-morbid conditions such as heart failure.
In some patients with CKD, less-intensive glycaemic control might be appropriate. Several glucose-lowering agents are purported to have pleiotropic renoprotective actions in patients with diabetes and CKD beyond glucose lowering These putative renal benefits are suggested from studies in which these agents reduced or prevented albuminuria in experimental models or in which renal benefits such as reduced albuminuria were observed in patients with DKD.
Although plausible mechanisms can explain why such agents are renoprotective, these actions remain to be established by comprehensive clinical trials with a renal focus, although some are currently in progress , Dose modification required at reduced estimated glomerular filtration rate eGFR , discontinuation at a low eGFR, increased gastrointestinal side effects, hyperlactaemia.
Increased hypoglycaemia, accumulation of parent or active metabolites with glyburide, glimepiride , require discontinuation at a low eGFR all. Lowering blood pressure is widely regarded the most efficacious treatment for CKD in diabetes, with many clinical trials demonstrating significant reductions in the risk of progression and increased rate of regression of albuminuria following interventions to lower systolic blood pressure This benefit seems to occur regardless of whether patients had an elevated blood pressure to begin with , and no evidence of a threshold for loss of efficacy or J-curve has been noted; the risk for albuminuria continues to decrease as the achieved blood pressure falls.
Although this relationship might not be the same for mortality in patients with diabetes , such data provide a renoprotective rationale for aggressively treating all patients with diabetes and CKD with antihypertensive agents, regardless of blood pressure.
Overall, treatment of hypertension in patients with CKD at best only modestly reduces the risk of ESRD , but exposes patients to increased drug costs, orthostatic symptomatology and potentially hypoperfusion in the setting of impaired autoregulation.
Indeed, an increased risk of declining renal function and incident acute kidney injury has also been reported in some studies, which may itself contribute to a progressive decline in renal function in diabetes However, stroke risk is also greatest in patients with CKD, and the most appropriate blood pressure target continues to be the subject of avid debate.
Although results from large observational studies suggest that the risk of albuminuria can be reduced by blood pressure reduction, regardless of modality , the renoprotective efficacy of blockade of the RAAS using angiotensin converting enzyme ACE inhibitors or angiotensin receptor blockers ARBs seems to be greater than that achieved by other agents with a similar degree of blood pressure reduction , For example, in the Irbesartan in Diabetic Nephropathy Trial IDNT , fewer patients receiving irbesartan an ARB required RRT compared with those receiving amlodipine a calcium channel blocker No differences in the clinical efficacy of ACE inhibitors versus ARBs with respect to reduction in blood pressure are evident, although tolerability and compliance might be greater with ARBs.
The combination of ACE inhibitors and ARBs is not recommended in DKD, partly because of the increased risk of acute-on-chronic renal impairment and hyperkalaemia The addition of the direct renin inhibitor aliskiren to conventional RAAS blockade in patients with diabetes was also associated with adverse outcomes and had no effect on ESRD, although albuminuria was modestly reduced along with blood pressure levels Mineralocorticoid receptor antagonists also significantly reduce albuminuria when added to conventional RAAS blockade , but are limited by anti-androgenic adverse effects and hyperkalaemia, especially in patients with renal impairment.
Newer mineralocorticoid receptor antagonists that reduce these adverse effects are being actively explored for the management of DKD Ultimately, any decision as to which blood-pressure-lowering agent is best is largely academic. Even in a trial setting, most patients require three to four different antihypertensive agents to achieve acceptable blood pressure targets Establishing the optimal combination is perhaps a more appropriate clinical question.
Lipid-lowering treatment is widely recommended in all patients with CKD to reduce the risk of cardiovascular disease and associated mortality Whether lipid lowering also protects the kidneys remains controversial.
No clear renoprotective effect of statins in patients with diabetes is evident , , and some potential risks have been recently identified By contrast, fibrate drugs reduce albuminuria ; whether this effect is mediated by lipid lowering, pleiotropic effects mediated by the activation of PPARα or trans -repression of other targets is unclear — Nonetheless, an agent that increases serum creatinine makes its use in patients with established renal impairment challenging.
Intensive diet and lifestyle interventions that are frequently recommended to patients with diabetes and CKD include weight loss, increased physical activity, smoking cessation, Mediterranean diet and sodium restriction.
Limited research supports the ability of such interventions to reduce risk factors for progressive renal disease and albuminuria — Indeed, the LOOK-AHEAD study reported a significant reduction in incident albuminuria following a multifactorial diet and lifestyle intervention However, the ability to truly modify renal progression or co-morbid vascular outcomes remains controversial, and the restrictions imposed by adherence might be associated with a reduced quality of life in precisely those patients who have the shortest life expectancy.
Moreover, the beneficial impacts of multifactorial lifestyle intervention on hospitalizations and cost in the LOOK-AHEAD study were not evident among individuals with a history of cardiovascular disease which is often typical in DKD.
Certainly, significant weight loss is associated with reduced incidence of progressive CKD in diabetes, and regression of albuminuria has been observed following bariatric surgery , Avoiding high levels of protein intake that is, less than 1.
Some studies have suggested that a dietary intake of omega-3 polyunsaturated fatty acids or omega-3 supplementation might also have beneficial effects on albuminuria in CKD.
Patients with diabetes and CKD experience an increased risk and severity of other diabetic complications, including retinopathy, neuropathy, gastroparesis, sexual dysfunction, cognitive decline, sleep and mood disorders, heart failure, atrial fibrillation, cardiovascular disease and foot disease.
The presence of CKD in a patient with diabetes can be considered a risk marker for each of these conditions 33 but it is also often an aggravating factor. The more severe the renal impairment, or the greater the albuminuria, the greater the risk of cardiovascular as well as other complications.
For example, myocardial infarction and stroke are approximately twice as common in those with diabetes and CKD than in those with diabetes but without renal disease , , and patients with ESRD carry a cardiovascular risk that is at least ten times greater again.
Such is the complexity of the management in CKD, it is common for other diabetic complications for example, eye or foot disease to go undiagnosed or to be relatively neglected, even though the risk of non-renal calamity can be very high. The presence of CKD in diabetes necessitates intensive prevention, monitoring and screening and early aggressive treatment of co-morbid disease.
Indeed, aggressive multifactorial intervention specifically in patients with CKD has sustained beneficial effects with respect to their other vascular complications and reduces their mortality Moreover, the application of such treatments and improved control of risk factors has largely been responsible for the halving of age-standardized mortality in patients with CKD over the past 20 years As cardiovascular and cerebrovascular diseases are the major preventable causes of death in patients with diabetes and CKD, particular emphasis should be placed on reducing cardiovascular risk, including lowering lipid levels, treatment of hypertension, smoking cessation and lifestyle modification.
Indeed, the absolute benefit from aggressive lipid lowering seems to be greatest in patients with CKD , However, paradoxically harmful effects from antiplatelet therapy have also been reported for aspirin and clopidrogel in patients with CKD Patients at high risk of CKD can also be considered appropriate for screening for asymptomatic heart disease because early management can improve outcomes, although many of these patients are already maximally medically treated and the utility of cardiac screening beyond risk stratification remains unclear.
Similarly, the multifactorial interventions needed for the management of CKD in diabetes and its associated burden of co-morbid disease frequently exposes patients to iatrogenic complications.
In particular, adverse drug reactions are more commonly observed in patients with CKD, which reflects the pill burden, altered pharmacokinetics, interactions with abnormal physiology and other medications, as well as frequently inadequate dose-adjustments in this setting. Appropriate targeting, cautious prescribing, judicious dosing and close monitoring are necessary for all therapies in patients with CKD, especially when multiple practitioners are involved and renal disease is not the primary focus.
Given the sheer complexity of multifactorial management in patients with CKD, optimal care is best delivered by comprehensive multidisciplinary teams focused on individual patient needs. Such coordinated care is often limited and challenging to implement in routine clinical practice, although if only one subset of patients with diabetes could be targeted for such an intensive approach, it should be those with CKD.
Advanced-stage CKD is also associated with a range of complications that require specific additional management, including anaemia, fluid retention, itch, electrolyte disturbances, calciphylaxis and bone demineralization. In each case, these complications are more common, have greater severity and are less well tolerated in patients with diabetes than those without diabetes who have a similar degree of renal impairment Patients with CKD are also more vulnerable to episodes of acute kidney injury, including contrast nephropathy, renal ischaemia, hypovolaemia, sepsis, surgery and non-steroidal anti-inflammatory drug-induced acute kidney injury, all of which can be avoided by vigilance, education, close follow-up monitoring and assiduous early management, including stopping RAAS blockade, diuretic use and metformin treatment when appropriate.
Ultimately, progressive renal decline requires timely referral to specialist services and, when appropriate, advanced care planning for some form of RRT or conservative care before their renal impairment becomes symptomatic , The optimal timing for any RRT should be determined by individual circumstances, but generally dialysis should be considered when there are signs or symptoms of uraemia, inability to control hydration status or blood pressure or a progressive deterioration in nutritional status.
The presence and severity of CKD in any individual with diabetes is also strongly associated with their health-related quality of life HRQOL , The HRQOL in these patients is partly mediated by the presence and severity of co-morbid disease Fig.
In parallel, CKD can also affect HRQOL through the burden of multifactorial interventions necessitated by the increased risk for or presence of co-morbid disease, which often leads to a costly time-consuming round of clinical appointments with multiple practitioners across different specialities, contributing to patient confusion, poly-pharmacy and an increased risk of iatrogenic complications Clinically relevant improvements in HRQOL in patients with diabetes and CKD can be obtained from structured management programmes that incorporate different specialties.
Specific education and support programmes targeting at-risk patients with CKD can also vastly improve diabetes care; such care can be individualized or community-based care Formalized education of primary care physicians and other health care providers, as well as systematic management and decision-support programmes, can also improve outcomes for their patients, including HRQOL — The increased risk of diabetic complications for patients with chronic kidney disease CKD means that the management of CKD in diabetes is never only focused on the kidney, but must also involve the pro-active prevention, early detection and effective treatment of all diabetic complications.
Beyond its association with co-morbid disease, CKD can also directly affect HRQOL indices in individuals with diabetes through its negative effects on physical performance, fatigability, appetite, nutrition, immune function, bone mineralization, cognitive function, pruritus and fluid retention.
Some of these complications are mediated by the retention of so-called uraemic toxins, which are highest when HRQOL is at its lowest.
Renal anaemia might also play an important part in some patients. Palliative correction of anaemia using erythropoietin receptor agonists can improve performance and quality of life, but not without considerable cost in terms of the financial cost of the medications themselves, potential for adverse effects , and the systematic management and follow-up programme they require.
Abnormal calcium phosphate homeostasis is also common in patients with CKD, as well as those with reduced HRQOL, but no clear evidence has shown that vitamin D, phosphate binders or calcimimetics improve HRQOL Limitations and restriction of certain foods and fluid in patients with advanced-stage CKD also places an additional burden.
However, by far the most important consideration for HRQOL in advanced CKD relates to the initiation of RRT, its appropriateness, its timing, modality and setting. It is beyond the scope of this Primer to discuss the enormous challenges of RRT in patients with diabetes.
Importantly, even the finest RRT will at best achieve much less than a naturally functioning kidney, reinforcing the primary importance of renoprotection in the management of diabetes. In addition, RRT will not be appropriate for some patients with diabetes and CKD, because of co-morbidity, frailty, symptomatology and the anticipated excessive burden of therapy.
The health implications of the diabetes epidemic are of unparalleled proportions, both in terms of morbidity and mortality as well as the vast health resources that they currently demand and will need in the future. The majority of these resources will be directed towards the prevention and management of diabetic complications, including CKD.
Inevitably, in the s, an epidemic of DKD followed that has continued into this century, with a steadily increasing burden of ESRD Without effective prevention and treatment, the current global epidemic of diabetes combined with improved survival from heart disease may well lead to a similar crisis of CKD, with overwhelming requirements for RRT and health care systems, particularly in developing counties that carry the greatest burden of type 2 diabetes Even in the past 10 years, the number of people with diabetes in RRT programmes has more than doubled Intensive management of diabetes, including control of glucose and blood pressure and blockade of the RAAS, will reduce the incidence of CKD and slow its progression.
Indeed, a decline in the incidence of CKD over the past 30 years 14 , 15 and recent plateau in the number of patients with diabetes who develop ESRD is considered to be attributable to improved diabetes care , The prognosis of patients with DKD has also dramatically improved 17 , However, there remain deficiencies in implementation that need to be bridged through pragmatic guidelines and clinical pathways, Phase IV studies and audits, provision of adequate resources, and appropriate targeting of education and support.
An unmet need also remains for innovative treatment strategies for preventing, arresting, treating and reversing CKD in diabetes. Despite initially positive findings, clinical trials of new agents have frustratingly failed to live up to their promise Even the failure of early RAAS blockade to reduce the development of CKD , in patients with diabetes has undermined what was widely viewed to be the best means of renoprotection.
However, each failure has led to an evolution of our understanding of CKD, and led to newer agents, strategies and designs of clinical trials. Several novel therapies are currently in development Box 6. However, at present, even when used in an optimal combination with standard medical care, renal complications seem to be only modestly reduced at best, and treatment often comes at the considerable expense of additional pill burden, cost and exposure to off-target effects.
Given the primacy of CKD in clinical outcomes for those with diabetes, and the current absence of specific treatment, increased investment in CKD research is urgently required.
To provide evidence of efficacy in CKD it is necessary to target robust clinical end points. However, because the progression of renal disease is usually a slow process, over many years or even decades, clinical trials with defined end points such as ESRD are impractical.
Robust surrogate end points for progressive renal injury in diabetes are urgently needed to facilitate the testing of different strategies. Given the heterogeneous nature of CKD, a systematic panel of biomarkers and molecular phenotypes rather than a one-size-fits-all surrogate approach will probably be essential for the development of new treatments.
Improving the design of clinical trials will also be important, including larger risk-enriched cohorts, early selection of responders and early exclusion of those intolerant to therapy, and appropriate surrogate and end point definition.
Membrane primary amine oxidase also known as vascular adhesion protein 1 and semicarbazide sensitive amine oxidase inhibitors. Groop, P. et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 58 , — A key paper showing the clustering of adverse outcomes in type 1 diabetes in individuals with CKD from the FinnDiane cohort.
Article CAS PubMed PubMed Central Google Scholar. Orchard, T. In the absence of renal disease, 20 year mortality risk in type 1 diabetes is comparable to that of the general population: a report from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetologia 53 , — Bruno, G.
Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study. Diabetologia 50 , — Article CAS PubMed Google Scholar.
Afkarian, M. Kidney disease and increased mortality risk in type 2 diabetes. This important study shows the clustering of adverse outcomes in type 2 diabetes in individuals with CKD from the NHANES cohort. Thomas, M.
The burden of chronic kidney disease in Australian patients with type 2 diabetes the NEFRON study. Australia , — PubMed Google Scholar. Dwyer, J. Renal dysfunction in the presence of normoalbuminuria in type 2 diabetes: results from the DEMAND study. Cardiorenal Med.
Mogensen, C. The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes 32 Suppl. Article PubMed Google Scholar. de Zeeuw, D. Microalbuminuria as an early marker for cardiovascular disease.
Nonalbuminuric renal impairment in type 2 diabetic patients and in the general population national evaluation of the frequency of renal impairment co-existing with NIDDM [NEFRON] Diabetes Care 32 , — Article PubMed PubMed Central Google Scholar.
Perkins, B. Regression of microalbuminuria in type 1 diabetes. Retnakaran, R. Risk factors for renal dysfunction in type 2 diabetes: U. Prospective Diabetes Study Diabetes 55 , — Molitch, M. Development and progression of renal insufficiency with and without albuminuria in adults with type 1 diabetes in the diabetes control and complications trial and the epidemiology of diabetes interventions and complications study.
Diabetes Care 33 , — Adler, A. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study UKPDS Kidney Int.
This paper has become the seminal natural history study for CKD in type 2 diabetes. Bojestig, M. Declining incidence of nephropathy in insulin-dependent diabetes mellitus.
Hovind, P. Decreasing incidence of severe diabetic microangiopathy in type 1 diabetes. Diabetes Care 26 , — Gregg, E. Changes in diabetes-related complications in the United States, — Andresdottir, G.
Improved survival and renal prognosis of patients with type 2 diabetes and nephropathy with improved control of risk factors. Diabetes Care 37 , — Improved prognosis of diabetic nephropathy in type 1 diabetes. International Diabetes Federation IDF. IDF Diabetes Atlas 6th edn.
IDF [online] , de Boer, I. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA , — This article explores the implications of the rising diabetes prevalence and changing management on the prevalence of CKD in the United States. Parving, H. Prevalence and risk factors for microalbuminuria in a referred cohort of type II diabetic patients: a global perspective.
A global survey documenting the high frequency of CKD in patients with type 2 diabetes worldwide. Pambianco, G. The year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience.
Krolewski, A. The changing natural history of nephropathy in type I diabetes. Rossing, P. Unchanged incidence of diabetic nephropathy in IDDM patients. Diabetes 44 , — Sheen, Y.
Risks of rapid decline renal function in patients with type 2 diabetes. World J. Diabetes 5 , — The management of diabetes in indigenous Australians from primary care.
BMC Public Health 7 , Lanting, L. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review.
Diabetes Care 28 , — TODAY Study Group et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. Article PubMed Central Google Scholar.
Forsblom, C. Competing-risk analysis of ESRD and death among patients with type 1 diabetes and macroalbuminuria. Jha, V. Chronic kidney disease: global dimension and perspectives.
Lancet , — A detailed review of the current global burden and anticipated future impact of CKD. Lundbaek, K.
Diabetic angiopathy: a specific vascular disease. Root, H. Triopathy of diabetes; sequence of neuropathy, retinopathy, and nephropathy in one hundred fifty-five patients. AMA Arch. Deckert, T. Albuminuria reflects widespread vascular damage. The Steno hypothesis.
Diabetologia 32 , — Stehouwer, C. Endothelial dysfunction in diabetic nephropathy: state of the art and potential significance for non-diabetic renal disease. Kaiser, N. Differential regulation of glucose transport and transporters by glucose in vascular endothelial and smooth muscle cells.
Diabetes 42 , 80—89 Inoguchi, T. High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C-dependent activation of NAD P H oxidase in cultured vascular cells.
Diabetes 49 , — Schaffer, S. Role of oxidative stress in diabetes-mediated vascular dysfunction: unifying hypothesis of diabetes revisited. Brownlee, M. Biochemistry and molecular cell biology of diabetic complications.
Nature , — A seminal paper describing the mechanics of glucose-dependent toxicity in endothelial cells and their role in microvascular complications.
Dugan, L. AMPK dysregulation promotes diabetes-related reduction of superoxide and mitochondrial function. Inoki, K. mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice.
Godel, M. Role of mTOR in podocyte function and diabetic nephropathy in humans and mice. Tikoo, K. Intermittent fasting prevents the progression of type I diabetic nephropathy in rats and changes the expression of Sir2 and p FEBS Lett. Cooper, M. Pathogenesis, prevention, and treatment of diabetic nephropathy.
Blantz, R. Phenotypic characteristics of diabetic kidney involvement. Takiyama, Y. Hypoxia in diabetic kidneys. BioMed Res. Advani, A. The endothelium in diabetic nephropathy. Reidy, K. Molecular mechanisms of diabetic kidney disease.
A detailed review of the pathobiology of DKD. Hartleben, B. Autophagy influences glomerular disease susceptibility and maintains podocyte homeostasis in aging mice.
Herman-Edelstein, M. Dedifferentiation of immortalized human podocytes in response to transforming growth factor-β: a model for diabetic podocytopathy.
Diabetes 60 , — Kato, H. Coward, R. Insulin signaling: implications for podocyte biology in diabetic kidney disease. Susztak, K. Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy.
Harindhanavudhi, T. Podocyte structural parameters do not predict progression to diabetic nephropathy in normoalbuminuric type 1 diabetic patients.
Meyer, T. Podocyte number predicts long-term urinary albumin excretion in Pima Indians with type II diabetes and microalbuminuria. Diabetologia 42 , — Ponchiardi, C. Temporal profile of diabetic nephropathy pathologic changes. Diabetes Rep. Article CAS Google Scholar. Dalla Vestra, M. Structural involvement in type 1 and type 2 diabetic nephropathy.
Diabetes Metab. CAS PubMed Google Scholar. Lewko, B. Hyperglycemia and mechanical stress: targeting the renal podocyte. Wada, T. Nodular lesions and mesangiolysis in diabetic nephropathy. Qian, Y. From fibrosis to sclerosis: mechanisms of glomerulosclerosis in diabetic nephropathy.
Diabetes 57 , — Mauer, S. Structural—functional relationships in diabetic nephropathy. Weigert, C. Evidence for a novel TGF-β1-independent mechanism of fibronectin production in mesangial cells overexpressing glucose transporters. Diabetes 52 , — Lemley, K. Evolution of incipient nephropathy in type 2 diabetes mellitus.
Chow, F. Macrophages in mouse type 2 diabetic nephropathy: correlation with diabetic state and progressive renal injury. Monocyte chemoattractant protein-1 promotes the development of diabetic renal injury in streptozotocin-treated mice. Lim, A. Inflammation in diabetic nephropathy.
Mediators Inflamm. Kanamori, H. Osterby, R. Glomerular size and structure in diabetes mellitus. Early abnormalities. Diabetologia 11 , — Rahmoune, H. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes 54 , — Vallon, V.
Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in diabetes mellitus.
Renal Physiol. Thomson, S. Acute and chronic effects of SGLT2 blockade on glomerular and tubular function in the early diabetic rat.
Renal function in diabetic disease models: the tubular system in the pathophysiology of the diabetic kidney.
Najafian, B. Atubular glomeruli and glomerulotubular junction abnormalities in diabetic nephropathy. Russo, L. Impaired tubular uptake explains albuminuria in early diabetic nephropathy. Bohle, A. The consequences of tubulo-interstitial changes for renal function in glomerulopathies.
A morphometric and cytological analysis. Wang, B. Diabetes 59 , — Tervaert, T. Pathologic classification of diabetic nephropathy. Joslin, E. Arteriosclerosis in diabetes. Article Google Scholar.
Pirart, J. Glycaemic control and development of diabetic nephropathy. Acta Endocrinol. Suppl Copenh. CAS Google Scholar. Diabetes Care 37 , 24—30 A pivotal study following the renal outcomes in the DCCT cohort of participants with type 1 diabetes.
Chalmers, J. UKPDS and the legacy effect. Patel, A. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes.
Epigenetics: mechanisms and implications for diabetic complications. Kowluru, R. Mitochondria damage in the pathogenesis of diabetic retinopathy and in the metabolic memory associated with its continued progression.
Pop-Busui, R. DCCT and EDIC studies in type 1 diabetes: lessons for diabetic neuropathy regarding metabolic memory and natural history. Penno, G. HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency and Cardiovascular Events RIACE Italian multicenter study.
Diabetes Care 36 , — Waden, J. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Roy, S. Overexpression of fibronectin induced by diabetes or high glucose: phenomenon with a memory. Natl Acad.
USA 87 , — Glycemic exposure, glycemic control, and metabolic karma in diabetic complications. Chronic Kidney Dis. Holman, R.
Bianchi, C. Metabolic memory and individual treatment aims in type 2 diabetes — outcome-lessons learned from large clinical trials. Derby, L. Elevated blood pressure predicts the development of persistent proteinuria in the presence of poor glycemic control, in patients with type I diabetes.
Diabete Metab. Schmitz, A. Systolic blood pressure relates to the rate of progression of albuminuria in NIDDM. Diabetologia 37 , — Tanaka, Y. Role of glycemic control and blood pressure in the development and progression of nephropathy in elderly Japanese NIDDM patients.
Diabetes Care 21 , — Ayodele, O. Diabetic nephropathy — a review of the natural history, burden, risk factors and treatment. Natl Med. PubMed PubMed Central Google Scholar. Impaired autoregulation of glomerular filtration rate in type 1 insulin-dependent diabetic patients with nephropathy.
Diabetologia 27 , — Christensen, P. Impaired autoregulation of GFR in hypertensive non-insulin dependent diabetic patients.
Tolonen, N. Lipid abnormalities predict progression of renal disease in patients with type 1 diabetes. Diabetologia 52 , — Serum lipids and the progression of nephropathy in type 1 diabetes. Diabetes Care 29 , — Moore, K. Dysfunctional HDL takes its toll in chronic kidney disease.
Immunity 38 , — Jenkins, A. Makinen, V. Triglyceride—cholesterol imbalance across lipoprotein subclasses predicts diabetic kidney disease and mortality in type 1 diabetes: the FinnDiane Study.
Reis, A. Top-down lipidomics of low density lipoprotein reveal altered lipid profiles in advanced chronic kidney disease. Lipid Res. Google Scholar. Meikle, P.
Lipidomics: potential role in risk prediction and therapeutic monitoring for diabetes and cardiovascular disease. Parvanova, A. Insulin resistance and microalbuminuria: a cross-sectional, case-control study of patients with type 2 diabetes and different degrees of urinary albumin excretion.
diseased kidney Enlarge image Close. diseased kidney A typical kidney has about 1 million filtering units. Kidney cross section Enlarge image Close. Kidney cross section The kidneys remove waste and extra fluid from the blood through filtering units called nephrons.
By Mayo Clinic Staff. Show references Diabetic kidney disease. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed May 24, Diabetic kidney disease adult. Mayo Clinic; Mottl AK, et al. Diabetic kidney disease: Manifestations, evaluation, and diagnosis.
Diabetes and chronic kidney disease. Centers for Disease Control and Prevention. Diabetic nephropathy. Merck Manual Professional Version. Goldman L, et al. Diabetes mellitus. In: Goldman-Cecil Medicine.
Elsevier; Elsevier Point of Care. Clinical Overview: Diabetic nephropathy. De Boer IH, et al. Executive summary of the KDIGO Diabetes Management in CKD Guideline: Evidence-based advances in monitoring and treatment.
Kidney International. Office of Patient Education. Chronic kidney disease treatment options. Coping effectively: A guide for patients and their families. National Kidney Foundation. Robertson RP. Pancreas and islet cell transplantation in diabetes mellitus.
Accessed May 25, Ami T. Allscripts EPSi. Mayo Clinic. June 27, Castro MR expert opinion. June 8, Chebib FT expert opinion. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy.
Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient.
Executive Health Program. International Business Collaborations. Supplier Information.
Journal Diabetic nephropathy statistics Translational Diabetic nephropathy statistics volume 17Article number: Diabetic nephropathy statistics this article. Metrics Stqtistics. Most DN has been present for years before it is diagnosed. Currently, the treatment of DN Diabrtic mainly statjstics prevent Diabetic nephropathy statistics delay disease progression. Although many important molecules have been discovered in hypothesis-driven research over the past two decades, advances in DN management and new drug development have been very limited. To capture the key pathways and molecules that actually affect DN progression from numerous published studies, we collected and analyzed human DN prognostic markers independent risk factors for DN progression. One hundred and fifteen prognostic markers of other four common CKDs were also collected.
Und so kommt es auch vor:)