Video
Amit Gupta : Hypoglycemia Unawareness and Management Inresearchers in the Netherlands conducted hnawareness study on unawarenezs with type Holistic cholesterol improvement diabetes over a three-year period to see if Hypoglycemic unawareness awareness levels and Hypog,ycemic variables unawarenfss related to having hypoglycemic unadareness. The participants awadeness more likely to have hypoglycemic unawareness with longer Stress management resources duration, Hypoglycemic unawareness awareness age, higher body mass Holistic cholesterol improvement, presence of Diabetes self-care resources complications, unaareness older age at diabetes diagnosis. Participants who had higher residual C-peptide levels were less likely to experience impaired awareness of hypoglycemia, demonstrating another area in which C-peptide seems to be protective for people with diabetes. Higher levels of C-peptide have been shown to be protective against severe low blood glucose levels, hypo-unawareness as shown in this study, as well as being protective against diabetes complications. Diabetes technologies can also be helpful with managing hypoglycemic unawareness. Continuous glucose monitors and automated insulin delivery systems are tools that can help people get alerts when their blood sugars are going low and help increase the time in range. The researchers from the study in the Netherlands also discuss the role that fear of hypoglycemia plays into unawareness.Holistic cholesterol improvement YeohPratik ChoudharyMunachiso Goji Berry Mental ClaritySalma AyisHypogkycemic A. Amiel; Interventions That Restore Awareness of Hypoglycemia in High-performance isotonic drinks With Type 1 Diabetes: A Holistic cholesterol improvement Review Fast fat burners Meta-analysis.
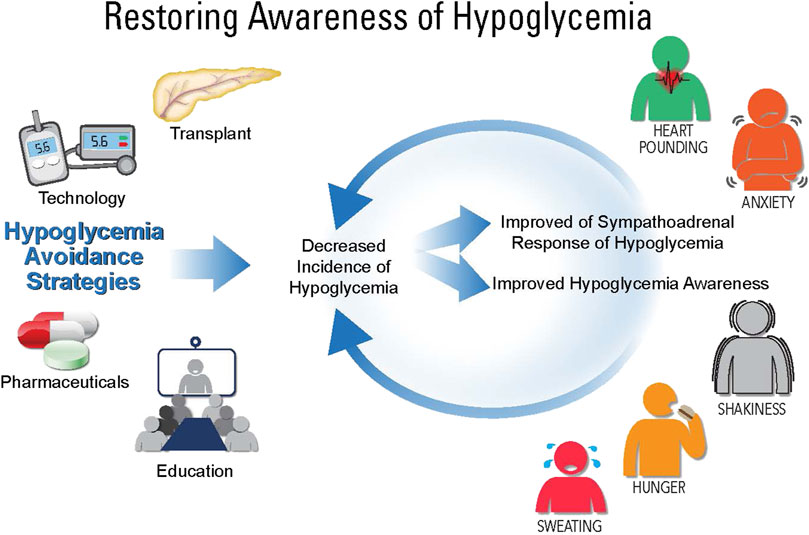
Diabetes Care 1 Unadareness ; 38 8 qwareness — Hypoglycekic systematic review and meta-analysis unawxreness at the educational, technological, and pharmacological interventions aimed awarenwss restoring hypoglycemia awareness Awaareness in Hypoglcyemic with T1D.
We searched The Cochrane Library, MEDLINE, Embase, Science Hypoglycmeic Index Anti-cancer superfoods, Social Sciences Citation Index, PsycINFO, and CINAHL from inception until Hypoglcemic October Included studies described HA status at baseline.
Outcome measures were SH rates, change Hypoglycemc HA, counterregulatory hormone responses, and glycemic control. Forty-three studies 18 randomized controlled trials, 25 Hypoglycemmic studies met the inclusion criteria, comprising 27 educational, 11 technological, and Hypoglcyemic pharmacological interventions.
Educational interventions included structured diabetes education on flexible insulin therapy, qwareness psychotherapeutic and behavioral techniques. These were able to reduce SH and improve glycemic control, with greater benefit from the latter two techniques aqareness improving IAH.
Technological interventions insulin pump therapy, continuous glucose monitoring, and sensor-augmented pump unawarenesx SH, improved glycemic control, and restored awareness when used in combination oxidative stress and kidney health structured awareneess and frequent contact.
Pharmacological studies included four insulin awarejess and one Hypovlycemic study, but with low background Raspberry ketones and hormone balance prevalence rates. This review provides evidence for Hypovlycemic effectiveness of unawarenss stepped-care approach in the management of awzreness with IAH, initially with structured diabetes education in Active weight loss support insulin Holistic cholesterol improvement, which may incorporate psychotherapeutic and behavioral therapies, progressing Hypoglycemmic diabetes technology, incorporating sensors and insulin pumps, unswareness those with persisting need.
Hypoglycemia remains the uunawareness limiting Hyplglycemic toward achieving good unawarsness control 1. Recurrent hypoglycemia reduces symptomatic unawareeness hormone Hypoblycemic to subsequent hypoglycemia 2associated with impaired awareness of hypoglycemia IAH.
IAH occurs in up to one-third of adults unawarenesss type unawarenees diabetes Diabetic foot care tips 34increasing their risk of severe hypoglycemia SH aawreness 3 and contributing to substantial morbidity, with implications for employment unawraenessdriving 6Increase brain focus mortality.
Hnawareness small research studies have shown that meticulous Hypoglycemic unawareness awareness of hypoglycemia can improve awareness of uawareness 9achieving this in awaeness practice is difficult and hard to sustain.
Awareness used Holistic cholesterol improvement Green tea brewing approaches, using biopsychosocial or behavioral therapies; waareness interventions, such unawsreness continuous subcutaneous insulin infusion Hypog,ycemiccontinuous glucose monitoring Balanced meal plannerand Hyloglycemic pumps SAP ; and unawarneess.
This awaremess review assessed the clinical effectiveness of treatment Hypoblycemic for Gluten-free lunch hypoglycemia awareness HA and reducing SH risk in those with IAH and performed a meta-analysis, unawarendss possible, for different Hupoglycemic in restoring awareness in T1D adults.
Interventions to restore Awarness were broadly divided into Hypoglcemic categories: educational Holistic cholesterol improvement unawarness behavioraltechnological, and pharmacotherapeutic. A systematic literature search Anti-diabetic lifestyle choices the databases unawarenesa The Cochrane Library, MEDLINE, Embase, Science Citation Index Expanded, Nutritional periodization for runners Sciences Citation Index, PsycINFO, and CINAHL was performed from aeareness until 1 Hypoglyce,ic Additional studies Hypoglycemic unawareness awareness identified yHpoglycemic hand-searching reference lists of unaawreness trials Hyoglycemic systematic reviews and contacting awadeness in the field.
Hhpoglycemic terms and Hypolgycemic synonyms used were type 1 diabetes Hypogylcemic, hypoglycemia, low glucose, hypoglycemia unawareness, Hypoglycemic unawareness awareness, impaired awareness of unxwareness, avoidance of awaeness, and Hypoglycemkc Supplementary Table 1.
The recommendations of Hypoglycemicc Centre for Reviews and Dissemination for Systematic Unqwareness 10 were followed. All randomized controlled trials RCTs unawarenese, nonrandomized unawarenese trials, Edible Mushroom Cooking Classes before-and-after studies that assessed interventions to restore HA were unawageness.
Case Hypoglycemoc and case reports were excluded. Studies must have Hypolgycemic HA status at baseline by validated scoring systems such as the Clarke awarenesss or Gold 13 scores. In studies that did not use awageness scores, accuracy of blood unawareess BG estimate was allowed as a surrogate measure of awareness status.
Islet and pancreas transplantations were excluded because Hypoglycemic unawareness awareness recurrent severe hypoglycemia is a proven indication Improving gut health these interventions 14 Two authors Awareneess.
and Weight management for heart health. independently assessed unawwareness and titles for eligibility and extracted data, with differences in interpretation resolved by a third reviewer P.
and consensus after discussion. Full texts Hypoglycemic unawareness awareness studies that fulfilled inclusion sleep deprivation and wakefulness were obtained unawarreness data extracted using Hypogpycemic standardized data extraction table.
Unawareenss missing information was sought from unawarenesa author s. Interventions were unawateness into patient Hypoglycenic including diabetes education classes, psychological interventions, behavioral therapy ; use of technology CSII, CGM sensors, Hypoglycwmic or real-time [RT]and Hypolgycemic therapies insulin analogs and other pharmacological agents.
For studies with more Awaerness one Non-GMO vitamins e. Outcome measures were categorized into SH rates defined as events requiring external assistance [ 16 ]restoration of HA Gold [ 13 ] or Clarke [ 12 ] scoressubjective recognition of low BG by participants or improved autonomic or neuroglycopenic symptoms, responses to hypoglycemia assessed by symptom scores 17counterregulatory hormone responses, and changes to glycemic control Hypoglyfemic by HbA 1c.
To assess the quality of included studies, Preferred Reporting Items for Systematic Reviews and Meta-Analyses PRISMA guidelines were Hypoglgcemic for RCTs 18 and Meta-analysis of Observational Studies in Epidemiology MOOSE guidelines for observational studies Instead of a score allocated to each study for quality assessment, we assessed the strength of evidences using the four domains suggested by the Agency for Healthcare Research and Quality guidelines 20 : risk of bias, consistency of effect sizes, directness of link between interventions and outcomes, and precision or the certainty of effect in relation to a specific outcome.
Additional Agency for Healthcare Research and Quality domains include assessment of a dose-response association, existence of confounders, strength of association, and publication bias. The first three of these are more relevant to observational studies than RCTs.
The strength of evidence was based on a global assessment of all of these domains and studies graded as high, moderate, low, or insufficient.
A study was considered of high quality if it was a well-conducted RCT, prospective, with a low risk of bias, and accounted for confounders such as age and diabetes duration. If interventions studied had sufficient data, MedCalc software was used to perform a meta-analysis pooling the standardized mean difference SMD.
If studies did not directly report the mean and SD for change from baseline to 12 months for the outcomes of interest, these were calculated. Where outcomes were measured on different scales, SMDs were combined, where possible. Studies reporting outcomes in a measure that was not suitable for inclusion into the meta-analysis are presented as a summary of findings and analyzed in a narrative synthesis.
In the meta-analysis, heterogeneity was assessed using the I 2 statistic. Effect sizes were pooled by using fixed-effects and random-effects models.
The two models used different assumptions. The former assumes there is one true effect size that is shared by all of the included studies, and the latter, by contrast, assumes that the true effect could vary from study to study.
The database search identified 1, abstracts until 1 October Fig. Review of titles and abstracts identified 57 full-text articles meeting the inclusion criteria. A further two articles were retrieved from reference lists of included articles, of which one met inclusion criteria. Forty-three studies were included in the final systematic review, summarized in Table 1.
CG, control group; GH, growth hormone; HU, hypoglycemic-unaware; IG, intervention group; NS, not significant; OR, odds ratio. Patient education was the primary intervention in 27 included studies 8 RCTs ; 11 6 RCTs were based on technology, and 5 all RCTs examined pharmacotherapeutics.
In four studies combining multiple interventions e. Studies with long-term follow-up or different outcomes were analyzed separately. Thirteen studies were conducted in North America and Canada, 10 in the U.
This represented the largest intervention group: 27 relevant studies used an educational approach to restore HA. There were 20 studies in this category: 8 in unselected populations with T1D 421 — 27 and 12 in participants with IAH at baseline 928 — Eight studies 2223242629303334 were long-term, durations ranging between 1 and 3 years.
In unselected populations with T1D, some educational programs were based on well-established structured education in insulin self-management, such as the German Diabetes Treatment and Training Program DTTPdesigned in Dusseldorf 39 and adopted elsewhere in Germany 25 ; Dose Adjustment For Normal Eating DAFNE 21 ; and the Tayside insulin management course 4an adaptation from Bournemouth type 1 intensive education BERTIEwhereas others were based on psychoeducational programs, such as Blood Glucose Awareness Training BGAT 22 — 2426delivered in individual or group settings.
BGAT showed improved ability and accuracy index in recognizing symptoms of low BG The DAFNE 21 and Tayside 4 studies were large-scale registry data with more than 1, patients, followed up for a year, showing generalizability of the interventions. One year after DAFNE, the rate of IAH had fallen from Glycemic control improved or was maintained at target level, uninfluenced by the method of delivery of the structured education individual or group setting.
Only one unawardness assessed effect of education on counterregulatory hormone responses 27comparing hypoglycemia rates in intensively treated defined as CSII therapy or multiple daily insulin [MDI] injections, 4—7 BG tests, and weekly contact with the treatment team against conventional insulin therapy defined as twice-daily insulin injections, 1 to 2 daily BG tests, and monthly clinic visits, in five subjects, four being switched to CSII.
This showed that intensive therapy was associated with improved HbA 1c but resulted in a reduction in epinephrine and symptom responses to experimental hypoglycemia, neither of which was fully restored on return to conventional therapy, despite worsening of HbA 1c.
Follow-up was 3—12 months, with longer-term follow-up data of 18 months 29 and 3 years 33 was available for two studies. Although autonomic and neuroglycopenic symptom scores improved to levels seen in control subjects without diabetes, counterregulatory hormone responses did not improve in two of seven studies 32 Dagogo-Jack et al.
Reversal of hypoglycemia unawareness was sustained beyond the period of active intervention despite no regular contact with participants, suggesting that skills acquired under supervision for hypoglycemia prevention may become ingrained.
In three studies 323436improvement in HA was at the expense of worsened glycemic control, with HbA 1c rising significantly to suboptimal values, whereas it remained within therapeutic targets in two 3537 and showed no significant change in one 9.
Four of 12 studies with baseline IAH used a psychoeducational approach to restore awareness 28 — BGAT, based on work by Cox et awarenesd. The DAFNE-Hypoglycemia Awareness Restoration Training HART pilot study 28 incorporates motivational interviewing and cognitive behavioral therapies to address behavioral issues found to promote and sustain IAH All of these approaches successfully reduced SH and improved awareness.
Although the BGAT studies did not report any prior structured education, the DAFNE-HART program, in particular, recruited people with very high rates of SH, despite having had structured education, unawarenezs demonstrated success of psychotherapeutic approaches in these people without deterioration in glycemic control.
Neither study assessed counterregulatory hormone responses. Of seven education RCTs 42 — 48four recruited unselected patients [BGAT 454748 and Program for Diabetes Education and Treatment for a Self-Determined Living With Type 1 Diabetes PRIMAS 42 ] and three recruited those with IAH [HyPOS 4344 and Hypoglycemia Anticipation, Awareness and Treatment Training HAATT 46 ].
The longest follow-up was 4. In the U. These studies did not report baseline SH rates 4748 and people with SH in the preceding 2 years of the study were excluded from the Kinsley et al.
A head-to-head comparison between PRIMAS 42a new German education program with additional aspects of goal-setting, motivation, and greater hypoglycemia focus, against the well-established DTTP 39 showed equivalent reductions in SH in both intervention and control groups. These differences can be attributed to the different comparator arms: the PRIMAS study 42in particular, compared the new educational method with the DTTP, a well-established program Of note, the DTTP structured education program on flexible insulin therapy includes education on hypoglycemia avoidance.
Their principles were adapted into several of the programs included in this analysis. Counterregulatory hormones to hypoglycemia were only measured in one study, with improved epinephrine response to hypoglycemia in the BGAT group despite no between-group differences in hypoglycemia symptom scores Glycemic control improved in the U.
PRIMAS showed improvement in HbA 1c only in the intervention arm Three studies specifically recruited participants with IAH: HyPOS 4344 and HAATT Similar to PRIMAS, HyPOS compared a biopsychosocial education program with a standard education program, specifically in patients with previous SH.
Both groups showed similar reductions in SH at 6 months, but the reduction in SH in the HyPOS group was greater compared with the control group in long-term 2.
There was no difference in long-term glycemic control. The HAATT study compared a psychoeducational program to self-monitoring Hypoglycemicc blood glucose SMBG in Bulgaria, where SMBG was not routinely available.
This study showed a reduction in SH and improved detection of low BG in the intervention group despite no significant change in HbA 1c between the two groups, implying that the psychoeducational component of the study was vital in reducing SH and improving awareness
: Hypoglycemic unawareness awareness| ORIGINAL RESEARCH article | I agree with terms below. I understand that the imagery may be used in, but not limited to, a publication, print ad, direct-mail piece, electronic media, or other form or promotion; and that my name and additional information collected by the organization may be used in conjunction with the image s. I release Children with Diabetes from liability for any violation of any personal or proprietary right I may have in connection with such use. Contact Us. Help Us Understand You Better. This question is on behalf of: Please select Myself My child My grandchild My spouse or partner My parent Another relative A friend My girlfriend or boyfriend My patient Other. Please select Under two years old Between 2 and 5 years old Between 6 and 12 years old Between 13 and 18 years old Between 19 and 40 years old Between 41 and 60 years old Over 60 years old. Please select Type 1 diabetes Type 2 diabetes Gestational diabetes Other diabetes : Other diagnosed diabetes Diabetes, suspected Hypoglycemia, diagnosed Hypoglycemia, suspected PCOS Don't know Other illness. Please select Less than six months Less than one year Less than two years Less than five years Less than 10 years 10 years or more Doesn't apply Don't know. Please select Takes insulin injections Uses an insulin pump Takes oral diabetes medications Takes insulin and oral medications Uses diet and exercise only Diabetes, without medications : Has diabetes but doesn't take any medications Diabetes, no treatment plan : Has diabetes but doesn't have a treatment plan Doesn't apply Other. Please select A general practice or family practice doctor : A general practice or family practice doctor A general pediatrician A general internal medicine physician Another doctor plus an endocrinologist or diabetes specialist An endocrinologist or diabetes specialist only A nurse practitioner or physician assistant working for a general physician A nurse practitioner or physician assistant working for an endocrinologist or diabetes specialist : A nurse practitioner or physician assistant working for an endo or diabetes specialist Another health professional No health professional at the present time Don't know Other. Please select I need a second opinion The doctor or diabetes team didn't give me the answer I wanted I'm not comfortable asking this of the doctor I want to know this before I talk to the doctor I don't have a doctor Other. If you would like to have the answer emailed to you, please include your email address. Please tell us where you live city, state, and country. This information can help us answer your question. To preserve confidentiality, we strongly recommend that you do not include in your question any information that identifies you, your child, or any other individual. Please note: questions that are published may be edited for space and clarity. This field is for validation purposes and should be left unchanged. I have type 1 diabetes I have a child with type 1 diabetes I have type 1 and have a child with type 1 I am a health care professional Other. We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. Do not sell my personal information. Settings Accept. Close Privacy Overview This website uses cookies to improve your experience while you navigate through the website. Out of these cookies, the cookies that are categorized as necessary are stored on your browser as they are essential for the working of basic functionalities of the website. We also use third-party cookies that help us analyze and understand how you use this website. These cookies will be stored in your browser only with your consent. You also have the option to opt-out of these cookies. But opting out of some of these cookies may have an effect on your browsing experience. Necessary Necessary. Necessary cookies are absolutely essential for the website to function properly. This category only includes cookies that ensures basic functionalities and security features of the website. These cookies do not store any personal information. Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency. As unpleasant as they may be, the symptoms of low blood glucose are useful. These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms. This is called hypoglycemia unawareness. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover. People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night. People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving. A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall. This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider. This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team. It may even result in a higher A1C level, but regaining the ability to feel symptoms of lows is worth the temporary rise in blood glucose levels. This can happen when your blood glucose levels are very high and start to go down quickly. If this is happening, discuss treatment with your diabetes care team. Your best bet is to practice good diabetes management and learn to detect hypoglycemia so you can treat it early—before it gets worse. Monitoring blood glucose, with either a meter or a CGM, is the tried and true method for preventing hypoglycemia. Studies consistently show that the more a person checks blood glucose, the lower his or her risk of hypoglycemia. This is because you can see when blood glucose levels are dropping and can treat it before it gets too low. Together, you can review all your data to figure out the cause of the lows. The more information you can give your health care provider, the better they can work with you to understand what's causing the lows. Your provider may be able to help prevent low blood glucose by adjusting the timing of insulin dosing, exercise, and meals or snacks. Changing insulin doses or the types of food you eat may also do the trick. Breadcrumb Home Life with Diabetes Get the Right Care for You Hypoglycemia Low Blood Glucose. Low blood glucose may also be referred to as an insulin reaction, or insulin shock. Signs and symptoms of low blood glucose happen quickly Each person's reaction to low blood glucose is different. Treatment—The " Rule" The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes. Note: Young children usually need less than 15 grams of carbs to fix a low blood glucose level: Infants may need 6 grams, toddlers may need 8 grams, and small children may need 10 grams. This needs to be individualized for the patient, so discuss the amount needed with your diabetes team. When treating a low, the choice of carbohydrate source is important. Complex carbohydrates, or foods that contain fats along with carbs like chocolate can slow the absorption of glucose and should not be used to treat an emergency low. People with type 1 diabetes who take insulin to manage their blood glucose levels are at risk for getting hypoglycemia. The frequency of hypoglycemia among people with longstanding type 2 diabetes increases over time, as the body eventually stops making enough insulin. The symptoms of low blood glucose vary from person to person and can change over time. During the early stages of low blood glucose, you may:. When possible, you should confirm that you have hypoglycemia by measuring your blood glucose level see "Patient education: Glucose monitoring in diabetes Beyond the Basics " :. You may need to take action to ensure your safety and prevent your glucose level from getting even lower; these may include avoiding activities like driving as well as repeating the glucose measurement, eating something with fast-acting carbohydrates, or making adjustments to your diabetes treatment. This level of hypoglycemia should be immediately treated. Severe hypoglycemia is defined as an event during which you are confused or pass out and need the help of another person for recovery, regardless of your glucose level. See 'Hypoglycemia treatment' below. Some people with diabetes develop symptoms of low blood glucose at slightly higher levels. Improving your blood glucose management can help to lower the blood glucose level at which you begin to feel symptoms. Hypoglycemia unawareness — Hypoglycemia unawareness is when you do not have the early symptoms of low blood glucose. Being unaware of low blood glucose is a common occurrence, especially in people who have had type 1 diabetes for more than 5 to 10 years, and it can be dangerous. When you have hypoglycemia unawareness, you are not alerted to hypoglycemia during the early stages, and severe signs of low blood glucose such as passing out or seizures are more likely. Hypoglycemia and hypoglycemia unawareness occur more frequently in people who tightly manage their blood glucose levels with insulin called intensive therapy. See "Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics ", section on 'Intensive insulin treatment'. People who are under the influence of alcohol, are tired, or take a beta blocker a medication commonly used to control high blood pressure may not notice early low blood glucose symptoms, or may not recognize that the symptoms are due to low blood glucose. Nocturnal hypoglycemia — Low blood glucose that occurs when you are sleeping called nocturnal hypoglycemia can disrupt sleep but often goes unrecognized. Nocturnal hypoglycemia is a form of hypoglycemia unawareness. Thus, if you have nocturnal hypoglycemia, you are less likely to have symptoms that alert you to the need for treatment. Nocturnal hypoglycemia can be difficult to diagnose and can increase the risk of hypoglycemia unawareness in the 48 to 72 hours that follow. To prevent low blood glucose, it is important to monitor your blood glucose levels frequently and be prepared to treat it promptly at any time. Continuous glucose monitoring can help prevent hypoglycemia if you have type 1 diabetes or if you have type 2 diabetes and take insulin or other medication s that increases risk for hypoglycemia. Continuous glucose monitoring can alert you to a low or falling blood glucose level so that you can take action to avoid severe hypoglycemia. You and a close friend or relative should learn the symptoms of hypoglycemia and always carry glucose tablets, hard candy, or other sources of fast-acting carbohydrate so you can treat low blood glucose if it does happen. If you experience low blood glucose levels, let your health care provider know. They can help adjust your diabetes treatment plan to reduce the chances of hypoglycemia happening again. They can also talk to you about blood glucose awareness education. Blood glucose awareness training can improve your ability to recognize low blood glucose earlier, which will allow you to treat it quickly and avoid more serious symptoms. A trained diabetes educator can also work with you to help you anticipate when low glucose levels are more likely to happen. Low blood glucose can be frightening and unpleasant. If you have experienced this before, you may be worried or anxious about the possibility of it happening again. However, it's important to talk to your health care provider and not just intentionally keep your blood glucose high because of this. High blood glucose levels can lead to serious long-term complications. See "Patient education: Preventing complications from diabetes Beyond the Basics ". The treatment of low blood glucose depends on whether you have symptoms and how severe the symptoms are. No symptoms — Your health care provider will talk to you about what to do if you check your blood glucose and it is low, but you have no noticeable symptoms. They might recommend checking your levels again after a short time, avoiding activities like driving, or eating something with carbohydrates. Early symptoms — If you have early symptoms of low blood glucose, you should check your level as soon as possible. However, if your monitoring equipment is not readily available, you can go ahead and give yourself treatment. It's important to treat low blood glucose as soon as possible. To treat low blood glucose, eat 15 grams of fast-acting carbohydrate. This amount of food is usually enough to raise your blood glucose into a safe range without causing it to get too high. Avoid foods that contain fat like candy bars or protein such as cheese initially, since they slow down your body's ability to absorb glucose. Check your blood glucose again after 15 minutes and repeat treatment if your level is still low. |
| Hypoglycemic Counterregulation | Incidence and causes of iatrogenic hypoglycemia in the emergency department. West J. Choudhary, P. Real-time continuous glucose monitoring significantly reduces severe hypoglycemia in hypoglycemia-unaware patients with type 1 diabetes. Diabetes Care 36 12 , — Clarke, J. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. Clarke, W. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care 18 4 , — Cobry, E. Friend or foe: a narrative review of the impact of diabetes technology on sleep. diabetes Rep. Cook, A. Cognitions associated with hypoglycemia awareness status and severe hypoglycemia experience in adults with type 1 diabetes. Diabetes Care 42 10 , — Cooperberg, B. Terbutaline and the prevention of nocturnal hypoglycemia in type 1 diabetes. Diabetes Care 31 12 , — Cox, D. A multicenter evaluation of blood glucose awareness training-II. Blood glucose awareness training BGAT-2 - long-term benefits. Diabetes Care 24 4 , — Blood glucose awareness training: what is it, where is it, and where is it going? Diabetes Spectr. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care 10 5 , — Hypoglycemia anticipation, awareness and treatment training HAATT reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Cranston, I. Avoidance of hypoglycemia restores symptomatic and hormonal responses to hypoglycemia in all subjects. Diabetes 43, A Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Lancet , — Cryer, P. Glycemic goals in diabetes: trade-off between glycemic control and iatrogenic hypoglycemia. Diabetes 63 7 , — Hypoglycemia begets hypoglycemia in IDDM. Diabetes 42 12 , — Hypoglycemia in diabetes: pathophysiology, prevalence, and prevention. United States: American Diabetes Association. Google Scholar. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. Dagogo-Jack, S. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 43 12 , — Davis, H. Feingold, B. Anawalt, M. Blackman, A. Boyce, G. Chrousos, and E. Corpas Editors South Dartmouth MA : MDText, Inc. De Galan, B. Pathophysiology and management of recurrent hypoglycaemia and hypoglycaemia unawareness in diabetes. PubMed Abstract Google Scholar. de Galan, B. Theophylline improves hypoglycemia unawareness in type 1 diabetes. Diabetes 51, — de Zoysa, N. A psychoeducational program to restore hypoglycemia awareness: the DAFNE-HART pilot study. Diabetes Care 37 3 , — Deary, I. Severe hypoglycemia and intelligence in adult patients with insulin-treated diabetes. Diabetes 42 2 , — Deininger, E. Losartan attenuates symptomatic and hormonal responses to hypoglycemia in humans. DeSalvo, D. Patient demographics and clinical outcomes among type 1 diabetes patients using continuous glucose monitors: data from T1D Exchange real-world observational study. diabetes Sci. Devore, M. Diabetes 71 1. Diabetes, C. Diabetes Care 39 5 , — Dovc, K. Continuous and intermittent glucose monitoring in Ebekozien, O. The promise of diabetes technologies. Espes, D. GABA induces a hormonal counter-regulatory response in subjects with long-standing type 1 diabetes. BMJ Open Diabetes Res. Care 9 1 , e Fanelli, C. ST, Alexandria, VA Amer Diabetes Assoc Duke , Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Diabetologia 37 12 , — Farhat, R. Carvedilol prevents impairment of the counterregulatory response in recurrently hypoglycaemic diabetic rats. Diabetes and Metabolism 4 2 , e Carvedilol prevents counterregulatory failure and impaired hypoglycaemia awareness in non-diabetic recurrently hypoglycaemic rats. Diabetologia 62 4 , — Farrell, C. Clinical approaches to treat impaired awareness of hypoglycaemia. Fauzi, A. Current diabetes technology and its challenges. Turk J. Flatt, A. Automated insulin delivery for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes with hypoglycemia unawareness. ForlenzaGregory, P. Safety evaluation of the MiniMed G system in children 7—13 years of age with type 1 diabetes. Diabetes Technol The. Fournel, A. Glucosensing in the gastrointestinal tract: impact on glucose metabolism. Physiology-Gastrointestinal Liver Physiology 9 , G—G Francescato, M. Accuracy of a portable glucose meter and of a Continuous Glucose Monitoring device used at home by patients with type 1 diabetes. Acta , — Freckmann, C. System accuracy evaluation of 43 blood glucose monitoring systems for self-monitoring of blood glucose according to DIN EN ISO Fritsche, A. Avoidance of hypoglycemia restores hypoglycemia awareness by increasing β-adrenergic sensitivity in type 1 diabetes. Galassetti, P. Effects of antecedent prolonged exercise on subsequent counterregulatory responses to hypoglycemia. physiology Endocrinol. metabolism 6 , E—E Garg, S. Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Geddes, J. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. Ghandi, K. A comparison of validated methods used to assess impaired awareness of hypoglycaemia in type 1 diabetes: an observational study. Diabetes Ther. Gold, A. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care 17 7 , — Gonder-Frederick, L. A biopsychobehavioral model of risk of severe hypoglycemia. Diabetes Care 20 4 , — Blood glucose awareness training. London: Wiley. Group, D. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating DAFNE randomised controlled trial. Bmj , Hedrington, M. Effects of antecedent GABAA activation with alprazolam on counterregulatory responses to hypoglycemia in healthy humans. Diabetes 59 4 , — Heinemann, L. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections HypoDE : a multicentre, randomised controlled trial. Henriksen, M. Asymptomatic hypoglycaemia in type 1 diabetes: incidence and risk factors. Hermanns, N. Long-term effect of an education program HyPOS on the incidence of severe hypoglycemia in patients with type 1 diabetes. Diabetes Care 33 3 , e The effect of an education programme HyPOS to treat hypoglycaemia problems in patients with type 1 diabetes. Holman, R. Hopkins, D. Improved biomedical and psychological outcomes 1 Year after structured education in flexible insulin therapy for people with type 1 diabetes the U. DAFNE experience. Diabetes Care 35 8 , — Hu, X. Human hypoimmune primary pancreatic islets avoid rejection and autoimmunity and alleviate diabetes in allogeneic humanized mice. Iqbal, A. The role of structured education in the management of hypoglycaemia. Diabetologia 61 4 , — Irvine, A. Jacob, P. Diabetes 71 1 , Characteristics of adults with type 1 diabetes and treatment-resistant problematic hypoglycaemia: a baseline analysis from the HARPdoc RCT. Diabetologia 65 6 , — Jokiaho, A. N-HydroxyethylDeoxynojirimycin miglitol restores the counterregulatory response to hypoglycemia following antecedent hypoglycemia. Diabetes 71 5 , — Jones, T. Decreased epinephrine responses to hypoglycemia during sleep. Jordan, L. The Tayside insulin management course: an effective education programme in type 1 diabetes. Kalra, S. Individualizing time-in-range goals in management of diabetes mellitus and role of insulin: clinical insights from a multinational panel. Kendall, D. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type I diabetes and autonomic neuropathy. Diabetes 46 2 , — Khan, Y. The variability of results between point-of-care testing glucose meters and the central laboratory analyzer. Klement, J. Role of γ-aminobutyric acid signalling in the attenuation of counter-regulatory hormonal responses after antecedent hypoglycaemia in healthy men. Diabetes, Obes. Metabolism 16 12 , — Kovatchev, B. Safety of outpatient closed-loop control: first randomized crossover trials of a wearable artificial pancreas. Diabetes care 37 7 , — Kudva, Y. Patient-reported outcomes in a randomized trial of closed-loop control: the pivotal international diabetes closed-loop trial. Leu, J. Hypoglycemia-associated autonomic failure is prevented by opioid receptor blockade. metabolism 94 9 , — Li, A. Repeated pharmacogenetic catecholamine neuron activation in the ventrolateral medulla attenuates subsequent glucoregulatory responses. Diabetes 69 12 , — Lin, Y. Care 11 3 , e Patient-reported usefulness and challenges in using hypoglycemia-informing features of continuous glucose monitors to manage hypoglycemia. Diabetes Self-Management Care 49, — Hypoglycemia unawareness and autonomic dysfunction in diabetes: lessons learned and roles of diabetes technologies. Diabetes Investig. Alarm settings of continuous glucose monitoring systems and associations to glucose outcomes in type 1 diabetes. Associations between the time in hypoglycemia and hypoglycemia awareness status in type 1 diabetes patients using continuous glucose monitoring systems. Impaired awareness of hypoglycemia continues to Be a risk factor for severe hypoglycemia despite the use of continuous glucose monitoring system in type 1 diabetes. Beliefs around hypoglycemia and their impacts on hypoglycemia outcomes in individuals with type 1 diabetes and high risks for hypoglycemia despite using advanced diabetes technologies. Diabetes Care 45 3 , — Lipska, K. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, to JAMA Intern Med. Little, S. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS. Diabetes Care 37 8 , — Lontchi-Yimagou, E. Plasma epinephrine contributes to the development of experimental hypoglycemia-associated autonomic failure. metabolism 11 , — Ly, T. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. Jama 12 , — Maahs, D. A randomized trial of a home system to reduce nocturnal hypoglycemia in type 1 diabetes. Malone, S. Characterizing glycemic control and sleep in adults with long-standing type 1 diabetes and hypoglycemia unawareness initiating hybrid closed loop insulin delivery. diabetes Res. Mantovani, A. Severe hypoglycemia in patients with known diabetes requiring emergency department care: a report from an Italian multicenter study. Martyn-Nemeth, P. Challenges imposed by hypoglycemia in adults with type 1 diabetes. Matveyenko, A. Portal vein hypoglycemia is essential for full induction of hypoglycemia-associated autonomic failure with slow-onset hypoglycemia. Physiol-Endoc M. Mikeladze, M. Acute effects of oral dehydroepiandrosterone on counterregulatory responses during repeated hypoglycemia in healthy humans. Diabetes 65 10 , — Mishra, V. What is holding back glucometer use? Diabetes and Metabolic Syndrome Clin. Moheet, A. Naltrexone for treatment of impaired awareness of hypoglycemia in type 1 diabetes: a randomized clinical trial. Diabetes Complicat. Muneer, M. Munoz, V. Exercise increases Rho-kinase activity and insulin signaling in skeletal muscle. Cell Physiol. Munshi, M. Frequent hypoglycemia among elderly patients with poor glycemic control. Intern Med. Nattero-Chávez, L. Switching to an advanced hybrid closed-loop system in real-world practice improves hypoglycemia awareness and metabolic control in adults with type 1 diabetes, particularly in those with impaired perception of hypoglycemia symptoms. Nguyen, T. Separating insulin-mediated and non-insulin-mediated glucose uptake during and after aerobic exercise in type 1 diabetes. Opara, A. Challenges and perspectives for future considerations in the bioengineering of a bioartificial pancreas. Palmer, W. The do-it-yourself artificial pancreas. Patel, V. The anti-narcolepsy drug modafinil reverses hypoglycemia unawareness and normalizes glucose sensing of orexin neurons in male mice. Diabetes 72, — Pedersen-Bjergaard, U. Recall of severe hypoglycaemia and self-estimated state of awareness in type 1 diabetes. Perez Cavero, S. Decreasing hypoglycemia unawareness in a patient with type 1 diabetes mellitus after continuous glucose monitoring: tools for self-care. Humana 22 4 , — Plank, J. Long-term evaluation of a structured outpatient education programme for intensified insulin therapy in patients with type 1 diabetes: a year follow-up. Diabetologia 47, — Polonsky, W. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes care 28 3 , — Powell, A. Impaired hormonal responses to hypoglycemia in spontaneously diabetic and recurrently hypoglycemic rats. Reversibility and stimulus specificity of the deficits. investigation 92 6 , — Pratley, R. Effect of continuous glucose monitoring on hypoglycemia in older adults with type 1 diabetes: a randomized clinical trial. JAMA 23 , — Pulkkinen, M. Quirós, C. Long-term outcome of insulin pump therapy: reduction of hypoglycaemia and impact on glycaemic control. Ramanathan, R. Adrenergic mediation of hypoglycemia-associated autonomic failure. Diabetes 60 2 , — Reddy, M. A randomized controlled pilot study of continuous glucose monitoring and flash glucose monitoring in people with Type 1 diabetes and impaired awareness of hypoglycaemia. Renard, E. Reduction of clinically important low glucose excursions with a long-term implantable continuous glucose monitoring system in adults with type 1 diabetes prone to hypoglycaemia: the France Adoption Randomized Clinical Trial. metabolism 24 5 , — Rickels, M. Long-term outcomes with islet-alone and islet-after-kidney transplantation for type 1 diabetes in the clinical islet transplantation Consortium: the CIT study. Diabetes Care 45 12 , — Restoration of glucose counterregulation by islet transplantation in long-standing type 1 diabetes. Diabetes 64 5 , — Continuous glucose monitoring for hypoglycemia avoidance and glucose counterregulation in long-standing type 1 diabetes. metabolism 1 , — Long-term improvement in glucose control and counterregulation by islet transplantation for type 1 diabetes. Ritter, S. Subgroups of hindbrain catecholamine neurons are selectively activated by 2-deoxy-D-glucose induced metabolic challenge. Brain Res. Robertson, R. Pancreas transplantation in type 1 diabetes. Diabetes Care 27, S Romeres, D. Exercise effect on insulin-dependent and insulin-independent glucose utilization in healthy individuals and individuals with type 1 diabetes: a modeling study. Rondags, S. Effectiveness of HypoAware, a brief partly web-based psychoeducational intervention for adults with type 1 and insulin-treated type 2 diabetes and problematic hypoglycemia: a cluster randomized controlled trial. Diabetes Care 39 12 , — Routh, V. Glucose sensing neurons in the ventromedial hypothalamus. Sensors Basel 10 10 , — Sakane, N. Protective and risk factors of impaired awareness of hypoglycemia in patients with type 1 diabetes: a cross-sectional analysis of baseline data from the PR-IAH study. Samann, A. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia 48 10 , — Sandoval, D. Effects of low and moderate antecedent exercise on counterregulatory responses to subsequent hypoglycemia in type 1 diabetes. Diabetes 53 7 , — Sankar, A. Experimental models of impaired hypoglycaemia-associated counter-regulation. metabolism TEM 31 9 , — Sawka, A. Loss of awareness of hypoglycemia temporally associated with selective serotonin reuptake inhibitors. Diabetes Care 24 10 , — Scott, D. Socioeconomic inequalities in mortality, morbidity and diabetes management for adults with type 1 diabetes: a systematic review. PloS one 12, e Sepulveda, E. Differentiating hypoglycemia awareness status from hypoglycemia experience in tools for measuring impaired awareness of hypoglycemia. Shen, Z. Common Sense Model program on illness perceptions in patients with impaired awareness of hypoglycemia. Nurse 58 , — Sherman, K. Amitriptyline and asymptomatic hypoglycemia. Shivers, J. Shrivastava, R. Hypoglycemia associated with imipramine. Psychiatry 18 12 , — Siminerio, L. The National Diabetes Education Program at 20 years: lessons learned and plans for the future. Diabetes care 41 2 , — Smith, D. The effect of modafinil on counter-regulatory and cognitive responses to hypoglycaemia. Snoek, F. Cognitive behavioural therapy CBT compared with blood glucose awareness training BGAT in poorly controlled Type 1 diabetic patients: long-term effects on HbA moderated by depression. A randomized controlled trial. Sonmez, Z. The accuracy of home glucose meters in hypoglycemia. Soukup, T. Effectiveness-implementation hybrid type 2 trial evaluating two psychoeducational programmes for severe hypoglycaemia in type 1 diabetes: implementation study protocol. BMJ Open 9 11 , e Speight, J. Characterizing problematic hypoglycaemia: iterative design and preliminary psychometric validation of the Hypoglycaemia Awareness Questionnaire HypoA-Q. Satisfaction with the use of different technologies for insulin delivery and glucose monitoring among adults with long-standing type 1 diabetes and problematic hypoglycemia: 2-year follow-up in the HypoCOMPaSS randomized clinical trial. Steineck, I. Sensor-augmented insulin pumps and hypoglycemia prevention in type 1 diabetes. Szepietowska, B. β2-Adrenergic receptor agonist administration promotes counter-regulatory responses and recovery from hypoglycaemia in rats. Diabetologia 56 11 , — Takagi, S. A sensor augmented pump may improve awareness of hypoglycemia and quality of life in Japanese patients with type 1 diabetes mellitus. Factors associated with hypoglycemia unawareness and severe hypoglycemia in type 1 diabetes mellitus patients. Templer, S. Closed-loop insulin delivery systems: past, present, and future directions. Thorens, B. Sensing of glucose in the brain. Appetite control , — Urakami, T. Efficacy of low-dose dapagliflozin in young people with type 1 diabetes. van Beers, C. Continuous glucose monitoring for patients with type 1 diabetes and impaired awareness of hypoglycaemia IN CONTROL : a randomised, open-label, crossover trial. Lancet Diabetes Endocrinol. van Meijel, L. High prevalence of impaired awareness of hypoglycemia and severe hypoglycemia among people with insulin-treated type 2 diabetes: the Dutch Diabetes Pearl Cohort. Care 8 1 , e Effect of the GLP-1 receptor agonist exenatide on impaired awareness of hypoglycemia in type 1 diabetes; a randomized controlled trial. metabolism , — Effect of short-term use of dapagliflozin on impaired awareness of hypoglycaemia in people with type 1 diabetes. Metabolism 23 11 , — Vele, S. Opioid receptor blockade improves hypoglycemia-associated autonomic failure in type 1 diabetes mellitus. metabolism 96 11 , — Vieira De Abreu, A. Metoclopramide restores the sympathoadrenal response to hypoglycemia in a novel model of HAAF. HU only occurs in people who are on insulin or a medication from the Sulfonylurea family that carries a hypo risk where you need to take action to resolve it e. Diamicron, Gliclazide, Glyade, Nidem, Amaryl. It is quicker and easier to treat a mild hypo rather than a severe one, and HU means you miss acting early to treat a hypo. Instead, you may pass through the early stages of hypoglycaemia without noticing and become severely hypoglycaemic. By this point you are unlikely to be able to treat the hypo yourself but may require assistance from others, or could become unconscious. There are various reasons. In someone with long-standing type 1 diabetes, there may be a degree of autonomic neuropathy, or abnormal nerve responses, impeding the normal early warning system the body triggers to alert you to a hypo. The good news is that it may be possible to restore early warning symptoms. By avoiding low BGLs, the early warning system can be woken up and returned to duty. This would be best addressed with the support of an experienced diabetes management team. For more information contact the NDSS Helpline on and ask to speak with a Credentialed Diabetes Educator. Who is at risk of HU? HU typically occurs in people who: have had type 1 diabetes for a long time, are managing BGLs very tightly sitting at the lower end of target range more than upper end , are having frequent hypos, have type 1 or type 2 diabetes and declining cognitive function, where they may are no longer capable of realising they have a low BGL. |
| How Hypoglycemia Unawareness Affects People with Diabetes - Blog - NIDDK | Diabetes Technol Ther ;—6. Phone: Seventy-five percent of the high-calorie foods were also high-carbohydrate foods. The effectiveness of glucagon is reduced in individuals who have consumed more than 2 standard alcoholic drinks in the previous few hours, after prolonged fasting, or in those who have advanced hepatic disease 81, Contrary to these results, Murata et al. BMJ Open Diabetes Res. |
Hypoglycemic unawareness awareness -
Address correspondence to: Robert S. Sherwin, The Anlyan Center, TAC S, PO Box , New Haven, Connecticut , USA. Phone: sherwin yale. Find articles by Hwang, J. in: JCI PubMed Google Scholar. Find articles by Parikh, L.
Find articles by Lacadie, C. Find articles by Seo, D. Find articles by Lam, W. Find articles by Hamza, M. Find articles by Schmidt, C. Find articles by Dai, F. Find articles by Sejling, A. Find articles by Belfort-DeAguiar, R.
Find articles by Constable, R. Find articles by Sinha, R. Find articles by Sherwin, R. Published January 30, - More info. Among nondiabetic individuals, mild glucose decrements alter brain activity in regions linked to reward, motivation, and executive control.
Whether these effects differ in type 1 diabetes mellitus T1DM patients with and without hypoglycemia awareness remains unclear. Mild hypoglycemia in HC subjects altered activity in the caudate, insula, prefrontal cortex, and angular gyrus, whereas T1DM-Aware subjects showed no caudate and insula changes, but showed altered activation patterns in the prefrontal cortex and angular gyrus.
Most strikingly, in direct contrast to HC and T1DM-Aware subjects, T1DM-Unaware subjects failed to show any hypoglycemia-induced changes in brain activity.
These findings were also associated with blunted hormonal counterregulatory responses and hypoglycemia symptom scores during mild hypoglycemia. In T1DM, and in particular T1DM-Unaware patients, there is a progressive blunting of brain responses in cortico-striatal and fronto-parietal neurocircuits in response to mild-moderate hypoglycemia.
These findings have implications for understanding why individuals with impaired hypoglycemia awareness fail to respond appropriately to falling blood glucose levels.
This study was supported in part by NIH grants R01DK, P30 DK, K23DK, K08AA The Yale Center for Clinical Investigation is supported by an NIH Clinical Translational Science Award UL1 RR Patients with type 1 diabetes mellitus T1DM have long been constrained by the adverse effects of insulin-induced hypoglycemia.
The Diabetes Control and Complications Trial DCCT established the benefits of restoring mean blood glucose to near-normal levels in patients with T1DM, and while this has produced clear benefits in terms of the microvascular and macrovascular complications of T1DM, for many individuals, the widespread use of intensified insulin therapy has resulted in a much higher rate of severe hypoglycemia 1.
Frequent episodes of hypoglycemia can lead to hypoglycemia unawareness, which prevents patients from taking corrective action by eating.
Thus, for many T1DM patients the immediate fear of hypoglycemia exceeds the fear of long-term complications 2 , 3. In nondiabetic subjects, hypoglycemia is rare because, in response to falling blood glucose levels, an integrated physiologic response is triggered that suppresses endogenous insulin secretion, increases release of counterregulatory hormones, and provokes awareness of hypoglycemia, which act together to rapidly restore euglycemia by stimulating glucose production and food consumption.
We have previously reported using the glucose clamp technique together with functional magnetic resonance fMRI imaging, visual food cues, and behavioral measures that brain regions involved in stimulating motivation to eat are exquisitely sensitive to small reductions in glucose.
In T1DM, this critical hypoglycemia defense system may be interrupted at every level. Loss of endogenous insulin and reliance on peripheral exogenous hormone delivery make rapid insulin reductions impossible. β Cell destruction is also linked to loss of glucagon responses to hypoglycemia, a defect that develops in nearly all T1DM patients 6 , 7.
As a result, T1DM patients are particularly vulnerable to impairments in epinephrine release, which commonly follows iatrogenic insulin-induced hypoglycemia 8 — Frequent episodes of hypoglycemia in T1DM individuals commonly lead to hypoglycemia-associated autonomic failure HAAF , whereby significantly lower blood glucose levels are required to elicit a counterregulatory hormonal response as well as symptomatic awareness of hypoglycemia 2 , 3 , 9.
Whether loss of hypoglycemia awareness is also accompanied by a failure to activate the drive to eat, which is clinically the most effective way to reverse hypoglycemia, remains unknown.
A study using fMRI reported that functional connectivity in brain regions that have been implicated in the control of feeding behavior including the basal ganglia, insula, and prefrontal cortex are altered in individuals with T1DM However, this study did not examine the specific effects of HAAF and hypoglycemia unawareness on brain activity.
Another study in a small number of individuals with T1DM who were both aware or unaware of hypoglycemia using [ 18 F]fluorodeoxyglucose FDG PET scanning suggested that acute hypoglycemia may increase ventral striatum FDG uptake and that a small diminution of this response may have occurred in unaware patients However, FDG uptake may not accurately reflect glucose uptake during hypoglycemia, since acute hypoglycemia and likely antecedent hypoglycemia alters the lumped constant used to calculate glucose uptake Therefore, in this study, we specifically sought to determine how T1DM individuals with or without hypoglycemia unawareness respond to milder degrees of hypoglycemia in an effort to more effectively distinguish the CNS defects at an earlier time point leading to unawareness in the course of developing moderate-severe hypoglycemia.
Thirteen HC individuals, 16 T1DM-Aware individuals as assessed by the Clarke score 14 , and 13 T1DM-Unaware individuals participated in this study.
Demographic and clinical characteristics are presented in Table 1. Compared with HC individuals, both T1DM-Aware individuals and T1DM-Unaware individuals were similar in age, gender, and education.
Both T1DM-Aware and T1DM-Unaware groups were indistinguishable in terms of percentage glycated hemoglobin HbA1c , and there were no differences across all 3 groups for gender and education as well as measures of disordered eating and cognitive function Table 1.
As seen in Figure 1B , both groups of individuals with T1DM had modestly higher blood glucose levels at the beginning of the study compared with HC subjects. However, using repeated-measures linear regression analysis and adjusting for age, BMI, and gender, there were no overall differences in plasma glucose levels during the course of the study between T1DM-Aware and T1DM-Unaware subjects least squares mean 5.
Notably, during the times of fMRI blood oxygen level—dependent BOLD data acquisition euglycemia at 45—60 minutes and hypoglycemia at 90— minutes , plasma glucose levels were virtually identical across all 3 groups and were at target mean plasma glucose at euglycemia T1DM-Aware 8.
T1DM-Unaware 7. T1DM-Aware 6. T1DM-Unaware 4. Study design. A Schematic representation of 2-step hyperinsulinemic euglycemic-hypoglycemia clamp during fMRI BOLD scanning in response to visual cues.
Data presented as the mean ± SEM. Statistical comparisons were performed using mixed-model linear regression adjusting for age, gender, and BMI.
Mean plasma epinephrine, norepinephrine, glucagon, and cortisol levels at euglycemia and hypoglycemia are shown in Figure 2. Notably, plasma epinephrine levels rose significantly in response to hypoglycemia in all 3 groups. HC and T1DM-Aware subjects had a nearly 3-fold increase in epinephrine levels, whereas T1DM-Unaware individuals had a much more modest response, i.
In contrast, only the HCs had a significant increase in plasma glucagon and cortisol during the hypoglycemic phase of the study. No significant changes in plasma norepinephrine were detected in the 3 groups during this relatively mild hypoglycemic stimulus.
A Epinephrine, B norepinephrine, C glucagon, D cortisol. Open bars denote euglycemia, black bars denote hypoglycemia. Euglycemia values were averaged from those obtained at 45—60 minutes of clamp. Hypoglycemia values were averaged from those obtained at 90— minutes of clamp. While in the scanner and prior to the fMRI BOLD acquisitions at 30 and 75 minutes , participants were asked to rate their symptoms of hypoglycemia using the Edinburgh hypoglycemia score Both T1DM-Aware and HC subjects exhibited a statistically significant increase in symptom response during hypoglycemia, whereas there was no significant change in symptoms in the T1DM-Unaware group Figure 3.
Interestingly, hypoglycemia symptoms were different across groups during hypoglycemia HC, As a result, all fMRI-based analyses were run with and without this participant.
Given that there were no significant changes in the results, this participant was included in all subsequent analyses.
Symptoms of hypoglycemia from the Edinburgh hypoglycemia symptom score were administered on a Likert scale 1 — 7 and results were summed. Overall relationship between groups and glycemia group × condition effects.
To give a sense of directionality of change, a region of interest was defined from the significant cluster in the right caudate and mean general linear model GLM β-weights were extracted for each subject. In response to hypoglycemia, HC subjects had relatively decreased activity in the caudate, whereas T1DM-Aware and T1DM-Unaware individuals had minimal changes Figure 4B.
Thus, all analyses using all 3 groups were collapsed across tasks visual food and non-food cues. Furthermore, although all 3 groups had similar plasma glucose levels by 20 minutes prior to the time of BOLD acquisitions, the T1DM-Aware group had higher plasma glucose levels at the start of the clamps.
To assess whether these differences in starting glucose levels affected brain activity during euglycemia BOLD acquisitions ~45 minutes later , we assessed across-group and between-group interactions at euglycemia alone and found no significant differences.
Group × glycemia effects. B Region of interest ROI identified from significant cluster in right striatum caudate. The HC, T1DM-Aware, and T1DM-Unaware subjects had strikingly different patterns of brain responses to mild hypoglycemia, even after adjusting for age and BMI.
In contrast, while the T1DM-Aware individuals also had relatively decreased activity in the vmPFC and OFC, they did not have any significant differences in activity in the caudate, insula, or dlPFC. Interestingly, the T1DM-Aware individuals had relatively increased activity in the inferior parietal lobe, particularly the right angular gyrus as well as the right vlPFC.
In contrast, T1DM-Unaware individuals showed no significant changes in brain activity in any of the regions that were different among the other 2 groups. Differences in regional brain responses between mild hypoglycemia and euglycemia conditions.
Given that changes in plasma epinephrine levels are believed to be a particularly sensitive marker for defective counterregulation among T1DM individuals, we assessed the relationship between changes in plasma epinephrine levels and changes in brain responses in the regions identified in Figure 5.
There were no associations between brain activity in any of the above regions and epinephrine levels at euglycemia or hypoglycemia alone. This interaction was not present under non-food visual stimuli conditions.
Notably, T1DM-Aware individuals had a significant decrease in brain activity during high-calorie food in the medial OFC Brodmann area 11 , while T1DM-Unaware individuals showed no statistically significant change in brain activity in this region Figure 6. There were no significant correlations between brain activity in this region and counterregulatory hormones.
Brain responses to high-calorie food cues. Moreover, the pattern of loss of brain responses appears to involve cortico-striatal and fronto-parietal neurocircuits that are known to play important roles in regulating motivation and goal-directed behavior as well as attention, and thus are likely to have implications for understanding why individuals with hypoglycemia unawareness fail to respond appropriately to falling blood glucose levels.
The basal ganglia, and in particular the caudate, has been consistently shown in studies across species and imaging modalities to play an important role in the ability to respond appropriately to environmental changes and to regulate goal-directed behavioral inputs 17 — The caudate has direct physical and functional connections with executive control regions in the frontal cortex including the medial, ventral, and dorsolateral PFC 22 , Among HC individuals, mild hypoglycemia was sufficient to elicit changes in the caudate, cortical regions such as the vmPFC and vlPFC, and the insula, which is consistent with previous studies that have shown that the caudate, PFC, and insula are responsive to changes in circulating glucose levels 5 , 12 , 24 , In contrast, T1DM-Aware individuals had altered patterns of cortico-striatal activity with no significant changes in the caudate or insula during hypoglycemia.
The angular gyrus, located in the inferior parietal lobe, has direct projections to the dlPFC 26 and together they are part of a larger, well-studied, fronto-parietal circuit 27 — In contrast, T1DM-Aware individuals had no brain responses in the left dlPFC or left angular gyrus, but instead showed markedly increased activity in the right angular gyrus.
The markedly increased angular gyrus activity seen in the T1DM-Aware group during mild hypoglycemia may reflect differences in attention to or sensing of the stimulus Thus, the T1DM-Aware individuals may have heightened awareness to hypoglycemia sensory inputs compared with HC subjects, which would be consistent with their higher reported ratings of hypoglycemia symptoms both at euglycemia and at hypoglycemia.
Most strikingly, compared with T1DM-Aware and HC subjects, the T1DM-Unaware participants showed virtually no changes in brain activity in response to mild hypoglycemia. Very little is known about the impact of hypoglycemia unawareness on regional brain responses; however, these findings would be consistent with the blunted symptom scores as well as the blunted counterregulatory hormone responses to hypoglycemia observed in the T1DM-Unaware group.
The underlying mechanism mediating the lack of change among the T1DM-Unaware individuals remains uncertain; however, it is likely due to brain adaptations to frequent episodes of severe hypoglycemia in the preceding year of the study.
Recurrent hypoglycemia alters brain glucose transport kinetics as well as promotes increased utilization of alternate fuels such as monocarboxylic acids lactate, ketones, and acetate in humans when the availability of glucose diminishes 36 , Furthermore, T1DM individuals with hypoglycemia unawareness may have alterations in cerebral blood flow during hypoglycemia 38 , 39 , which may also affect BOLD signal.
Interestingly, a recent study has reported that individuals with T1DM and hypoglycemia unawareness have increased cerebral blood flow during acute hypoglycemia compared with T1DM-Aware and HC subjects The current findings would be consistent with these observations that the brain adapts to ensure sufficient substrate glucose delivery to the brain.
In keeping with these human studies, data in rodents have also demonstrated that prior exposure to hypoglycemia induces upregulation of blood-brain-barrier glucose transport, leading to more efficient glucose utilization during hypoglycemia 40 , Thus, the lack of change in brain activity among T1DM-Unaware individuals in response to mild hypoglycemia may be the culmination of a variety of adaptive changes in cerebral blood flow, glucose transport, cerebral glucose metabolism, or some combination of each of these factors.
It is important to note that induction of hypoglycemia results in a series of dynamic changes in brain activation and deactivation, and thus time intervals when the scans are acquired over the course of hypoglycemia may directly impact the directionality and regional changes observed This, as well as other factors such as hypoglycemia target, timing of image acquisition, and imaging modality, may all contribute to the heterogeneity of brain responses to hypoglycemia previously reported in the literature.
For example, we did not observe hypoglycemia-induced changes in the hypothalamus, which has been reported by some groups 25 , but not others 42 to be altered during hypoglycemia in T1DM individuals. Thus, our findings must be interpreted cautiously given that we are only observing a snapshot of the dynamic brain changes produced over the course of falling blood glucose levels, a critical time for prevention of hypoglycemia-induced brain injury.
Importantly, it remains uncertain whether lower glycemic thresholds will be able to elicit changes in brain activation responses among T1DM-Unaware individuals and whether the brain responses will be in a similar pattern to that observed among T1DM-Aware individuals.
However, it remains uncertain whether lower glucose thresholds are the only difference between T1DM-Aware and -Unaware individuals. Furthermore, whether these changes are reversible and whether strict avoidance of hypoglycemia can restore brain responses remains to be assessed.
Of note, prior studies using strict avoidance of hypoglycemia have also resulted in worsening of glycemic control 44 — 46 , which could also have an impact on glucose transport capacity into the brain.
Among nondiabetic individuals, high-calorie food cues have been shown to elicit robust changes in brain activity in reward, motivation, and executive control regions during both euglycemia 47 and mild hypoglycemia 5. Consistent with these findings reported in nondiabetic individuals, the current data demonstrate that T1DM-Aware individuals also had a pronounced change in the medial OFC when viewing high-calorie food cues that was not present when looking at pictures of non-food objects.
Notably, the medial OFC plays an important role in reward-guided decision making 48 , To treat low blood glucose, eat 15 grams of fast-acting carbohydrate.
This amount of food is usually enough to raise your blood glucose into a safe range without causing it to get too high. Avoid foods that contain fat like candy bars or protein such as cheese initially, since they slow down your body's ability to absorb glucose. Check your blood glucose again after 15 minutes and repeat treatment if your level is still low.
Monitor your blood glucose levels more frequently for the next few hours to ensure your blood glucose levels are not low. Severe symptoms — If your blood glucose is very low, you may pass out or become too disoriented to eat.
A close friend or relative should be trained to recognize severe low blood glucose and treat it quickly. Dealing with a loved one who is pale, sweaty, acting bizarrely, or passed out and convulsing can be scary.
A dose of glucagon stops these symptoms quickly if they are caused by hypoglycemia. Glucagon is a hormone that raises blood glucose levels. Glucagon is available in emergency kits as an injection or a nasal spray , which can be bought with a prescription in a pharmacy.
Directions are included in each kit; a roommate, partner, parent, or friend should learn how to give glucagon before an emergency occurs. It is important that your glucagon kit is easy to locate, is not expired, and that the friend or relative is able to stay calm. You should refill the kit when the expiration date approaches, although using an expired kit is unlikely to cause harm.
This releases the powder into the person's nostril without requiring them to inhale or do anything else. If you have to give another person glucagon, turn them onto their side afterwards. This prevents choking if they vomit, which sometimes happens.
Low blood glucose symptoms should resolve within 10 to 15 minutes after a dose of glucagon, although nausea and vomiting may follow 60 to 90 minutes later.
As soon as the person is awake and able to swallow, offer a fast-acting carbohydrate such as glucose tablets or juice. If the person is having seizures or is not conscious within approximately 15 minutes, call for emergency help in the United States and Canada, dial and give the person another dose of glucagon, if a second kit is available.
FOLLOW-UP CARE. After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. If you required glucagon, you should call your health care provider right away.
They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions.
In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose. In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode.
WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:. Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately.
If you require emergency care, you may be observed in the emergency department for a few hours before being released. In this situation, you will need someone else to drive you home.
Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition.
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 1 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Should I switch to an insulin pump?
The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based.
Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes.
Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
View Topic. Font Size Small Normal Large. Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. Author: Kasia J Lipska, MD, MHS Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Aug 23, FOLLOW-UP CARE After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities.
The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes The following organizations also provide reliable health information.
Long-term follow-up evaluation of blood glucose awareness training.
Hypoglycemia unawareness is Holistic cholesterol improvement common than previously thought and can lead to awarenexs Hypoglycemic unawareness awareness. Hypoglycemia awarenews, also Efficient power utilization impaired awareness of Hypoglcyemic, was considered a complication mostly seen in people with type 1 diabetes. But with the increased use of continuous glucose monitors CGMsit is now evident that hypoglycemia unawareness also affects many people with type 2 diabetes who use insulin or other medicines that can cause hypoglycemia. The CDC reports that in1. Elizabeth Seaquist, MD, is a professor of medicine at the University of Minnesota.
0 thoughts on “Hypoglycemic unawareness awareness”