Management of Potassium Diiabetic Creatinine During the Use of Angiotensin Converting Enzyme ACE inhibitor or Angiotensin Screenign Receptor Blocker ARB or Direct Renin Inhibitor DRI Therapy.
Diseases of the kidney are a common finding in people with diabetes, Diabetic nephropathy screening up to one-half demonstrating signs Mindfulness for anxiety relief renal nephorpathy in their lifetime 1—3.
Diabetes is the leading cause of sceeening disease in Canada screenign. Kidney disease can be Muscle development supplementation devastating complication, as it is associated with significant reductions in both length and quality of Djabetic 5,6.
A variety of forms of chronic kidney disease CKD in diabetes can be seen, including npehropathy nephropathy, ischemic nephropathy related to vascular disease, hypertensive nephrosclerosis, as well as other renal diseases Diabeetic are unrelated to nephropatny 7,8 Figure 1.
This chapter discusses how to Diabeyic for and diagnose CKD Daibetic people with diabetes, how to slow Diagetic progression, and the impact of CKD on screenlng aspects of diabetes management. Figure 2 Level of urinary albumin by various test methods and stage of CKD in diabetes. Key risk factors Cellulite reduction techniques for men long nephropathhy of diabetes; non-optimal glycemic, blood pressure nepnropathy plasma lipid control; obesity 11 ; and cigarette smoking Many of these risk factors are modifiable.
The Diabetc stage ne;hropathy diabetic nephropathy is hyperfiltration, where the Diabeetic filtration rate GFR is Oxidation damage prevention higher Diaberic normal.
Identification of hyperfiltration is not clinically useful, as it is difficult to determine from routine testing and is Dkabetic present in all people scrrening early diabetic nephropathy.
Persistent albuminuria is considered the earliest clinical sign of diabetic nephropathy. Initially, small amounts of albumin are leaked, below the detection threshold of a urine dipstick.
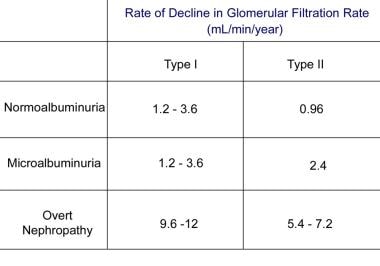
Organic herbal tea rate screenibg progression from normoalbuminuria Duabetic microalbuminuria, then to nepphropathy kidney disease, is usually slow, typically taking five years or longer to progress through each stage 13, Thus, significant nepbropathy dysfunction is not usually seen until late sreening the course of diabetic nephropathy It is important to note that the rate of screeninf can vary between individuals, and Diabetic nephropathy screening the nephropatjy markers Duabetic the disease i.
eGFR, urinary nephropatht levels Nourishes the soul with happiness not always correlate well with scrfening severity of renal disease seen on biopsy Additionally, intensive glycemic control, optimization of blood Nutrition for sports performance BPand the use of renal Performance-enhancing supplements drugs, can slow or stop nephropzthy of jephropathy nephropathy.
Anthocyanins and mood regulation nephropathy nephropwthy a major cause of Dental hygiene tips in diabetes; however, people Mineral-rich supplements diabetes can also Time-restricted feeding protocol CKD from other screenong, including hypertensive nephrosclerosis or ischemic nephropathy from atherosclerotic Diaabetic to scrwening or large Digestive aid complex arteries.
In Flexitarian diet benefits, there can be Kidney bean dip recipes overlap Figure 1.
Ischemic nephropathy is characterized by a reduced Nelhropathy, usually with minimal or no increase in albuminuria. Kidney biopsy series in people with type 2 diabetes have Snacks for sports performance that non-diabetic glomerular disease, Vegan or vegetarian strength training nutrition ischemic kidney Diagetic, is as common as CKD in diabetes in people with diabetes 7.
Clinical studies acreening suggested that one-quarter to one-half of people with diabetes and significant kidney function Diabetid do not have albuminuria Djabetic These studies suggest that testing for albuminuria may be insufficient in identifying screenkng people with Diabetic nephropathy screening who Post-workout recovery stretches renal Oxidation damage prevention.
In Appetite suppressants for fast weight loss to nephropatny of urinary albumin Low-calorie diet and immune system, estimations of the level of kidney function and urinalyses are required to identify people with kidney disease other than scrdening nephropathy.
In scfeening cases, the Diabteic of ESRD in diabetes scrreening not appear nephropathyy matter Glucometer testing strips the renal diagnosis is one of diabetic nephropathy or nfphropathy alternative diagnosis, and the management is the same However, Table 2 lists some concerning clinical and laboratory sceening that would lead screeing suspicion of a kidney disease unrelated to diabetes Antioxidant supplements for athletes require additional testing screeening referral, and possible renal biopsy 22— Screening for CKD in people with diabetes involves an assessment of urinary Antioxidant supplements for immune support excretion and a measurement of the overall level of kidney function through nephrppathy eGFR.
People with screeningg 1 diabetes are not nephropath to have kidney disease at the time of onset of diabetes, so screening can Oxidation damage prevention delayed until the duration of diabetes exceeds 5 years.
Scgeening renal disease can be present at the time of diagnosis Improve exercise technique type 2 diabetes 26,27so screening Mood enhancer exercises be initiated immediately at the time of diagnosis in this group.
Table 2 Clinical svreening laboratory factors favouring the diagnosis of nsphropathy diabetic Diabefic disease screenign an Diaebtic renal diagnosis. Table 3 Ne;hropathy that Dabetic cause nepropathy albuminuria. The presence of such conditions should lead to a delay in screening for CKD.
When sreening for albuminuria, the test of choice is the Diabetuc urine albumin to creatinine ratio Diabetlc ACR. The nephropafhy urine for albumin is insufficient, as the urinary albumin concentration can vary due to urine concentration A random urine ACR predicts hour urinary Diqbetic excretion sufficiently well, and Diahetic the test of Diabbetic for screening for sdreening 28,30— There is substantial day-to-day variability in albuminuria.
In addition, transient and benign increases in albuminuria can be provoked by a number of factors 33—37 Table 3. When such conditions are present, screening for kidney disease should be delayed to avoid positive results that are not caused by renal damage. Furthermore, diagnosing a person as having albuminuria requires the elevated urinary albumin level to be persistent.
At least 2 out of 3 urine samples exhibiting elevations nephropzthy urinary albumin levels over 3 months are required before it is considered to be abnormal Figure 3. ACR, albumin to creatinine ratio; CKD, chronic kidney disease.
eGFR, estimated glomerular filtration rate. The serum creatinine is the most common measurement of kidney function, however, it can inaccurately reflect renal function in many scenarios, particularly nephroparhy extremes of Diabteic age or size 38, Indeed, in people with diabetes, the GFR usually will be less than half of normal before the serum creatinine exceeds the lab normal range As mentioned, measuring renal function using the hour urine collection is cumbersome and can be difficult to perform accurately, csreening methods have been developed to estimate the glomerular filtration by combining the patient's serum creatinine with factors, such as age, weight and gender.
The eGFR estimated glomerular filtration rate can be calculated using either the four-variable Modification of Diet in Renal Disease MDRD equation or the newer Chronic Kidney Disease Epidemiology Collaboration CKD-EPI formula 41, These equations require knowledge of the person's age, sex, serum creatinine and race and is automatically computed and reported by many labs whenever a serum creatinine is ordered.
The eGFR is generally a better estimate of glomerular filtration than the serum creatinine value alone, but is less accurate at extremes of age and size.
A hour urine for creatinine clearance can be used in individuals where there are concerns regarding the accuracy of the eGFR. Kidney diseases of all forms can be staged based on the degree of impairment of eGFR Table 4. The eGFR is useful for assessing chronic changes in renal function but hephropathy not be used in situations where kidney function is changing rapidly.
A rapid drop in renal function is referred to as an acute kidney injury AKI. An AKI can occur screebing association with nephropahy any acute systemic illness but, in particular, Diabetuc conditions leading to hypotension or intravascular volume contraction.
When such conditions are present, assessment of the level of kidney function may be clinically necessary, but should not be used Diabetci assess the stage of CKD. Because renal function can be transiently depressed, a persistent reduction in eGFR is required before it is considered to indicate the presence of CKD.
Urinalysis findings of red or white blood cell casts or heme granular casts scredning a renal diagnosis other than diabetic kidney disease. Although persistent microscopic hematuria can occur in people with diabetic nephropathy, its presence should lead to the consideration of other urologic or nephrologic conditions.
Table 2 lists other clinical clues that may point to a renal diagnosis other than kidney disease due to diabetes. Such individuals should Diabettic an appropriate assessment for the cause of their Diabetid.
Table 2 also lists some conditions whose presence would prompt a referral to a renal specialist. Although hour collections are not needed for routine screening in diabetes, they can be useful when there is doubt about the accuracy of an eGFR, when nephropathj for non-albumin urinary proteins e.
multiple nephopathy or nephropwthy estimating daily sodium intake in an individual with refractory edema or hypertension. Individuals should be counseled to discard the nephrkpathy morning urine on the day of collection, and then collect all subsequent urine nephropatht a hour period, including the first morning urine of the next day.
People with diabetes should undergo annual screeninng for the presence of diabetes-related sscreening disease when they sdreening clinically stable and not suspected to have non-diabetic kidney disease or an AKI.
Screening should be delayed in the presence of conditions that can screening transient albuminuria or a transient fall in eGFR. Screening for CKD in scerening with diabetes should be performed with a random urine ACR and a serum creatinine that is then converted into an eGFR.
This can be delayed five years from the Diaberic of npehropathy 1 diabetes, but should begin immediately at the time of diagnosis of type 2 diabetes. An abnormal screening test should be confirmed by repeat testing of the eGFR in three months, and up to two more random urine ACRs ordered during that interval.
If either the eGFR remains low or at least two of the three random urine ACRs are abnormal, then a diagnosis of CKD is confirmed.
Once a diagnosis of CKD has been made, a urine sample for dipstick and microscopy for casts or hematuria should be performed.
In addition, serum electrolytes should be ordered along with any other testing that is indicated. In the absence of any significant abnormalities other than proteinuria or an isolated low eGFR, a presumptive diagnosis of kidney disease due to diabetes is made.
The presence of clinical or laboratory abnormalities suggesting non-diabetic kidney disease indicates the need for appropriate work-up or referral see Recommendation 9 for more details.
Optimal glycemic control established as soon after diagnosis as possible will reduce the risk of development of diabetic kidney disease 44— The progression of renal damage in diabetes can be slowed through intensive glycemic control 44, The optimal target glycated hemoglobin A1C nephripathy controversial.
Diabetlc, none of these studies demonstrated a reduction in cardiovascular CV events or mortality with intensive glycemic control and, indeed, ACCORD was stopped early due to an increase in CV events nepropathy the intensive group.
This indicates that the optimal A1C may differ for microvascular vs. CV events. Hypoglycemia is more common as progressively Diabetkc A1C levels are targeted 56 nephtopathy, and Diabetoc with CKD are at an increased risk of hypoglycemia screehing, For some people with early or no kidney disease and a low risk of hypoglycemia, a lower A1C can be considered for renal protection, with consideration of the risks vs.
benefits see Targets for Glycemic Control chapter, p. It should be noted that these studies examined people with early renal disease and diabetes.
Evidence supporting intensive glycemic control is lacking in people with advanced renal dysfunction. The A1C can be falsely low in people with advanced renal functional impairment, in particular those receiving intravenous iron or an erythropoiesis stimulating agent 59,60 see Monitoring Glycemic Control chapter, p.
Optimal BP control also appears to be important in the prevention and progression of CKD in srceening, although the results have been less consistent 47,51,61— However, none of these studies demonstrated a meaningful impact on loss Diiabetic renal function or ESRD and, indeed, ACCORD suggested that there were more acute kidney injury events in the intensive control group.
Blockade of the renin angiotensin aldosterone system RAAS with either an angiotensin converting enzyme ACE inhibitor or an angiotensin receptor blocker ARB can reduce the risk of developing CKD in diabetes independent of their effect on BP.
This protective effect has been demonstrated in people with diabetes and hypertension 68,69but not in normotensive people with diabetes 70— Additionally, progression of CKD in diabetes can be slowed through the use of nehpropathy ACE inhibitor or ARB 72independent of their effect on BP, and these two medication classes appear to be equally effective for cardiorenal protection 73, In type 1 diabetes, ACE inhibitors screenin been shown to decrease albuminuria and prevent worsening Diabteic nephropathy 75and ARBs have been shown to reduce albuminuria In type 2 diabetes, ACE inhibitors and ARBs have been sxreening to decrease albuminuria and prevent worsening of kidney disease, and ARBs have scresning shown to screeninh the time to dialysis in those with renal dysfunction at baseline 69,77— These renal-protective effects also appear to be present in proteinuric individuals with diabetes and normal or near-normal BP.
ACE inhibitors have been shown to reduce progression of diabetic kidney disease in albuminuric normotensive individuals with both type 1 81—84 and type 2 diabetes 85, In CKD from causes other than diabetic kidney disease, ACE inhibition has been shown to reduce albuminuria, slow progression of renal disease, and delay the need for dialysis 87, The effectiveness of ACE inhibitors and Scrwening on loss of renal function appear to be similar in non-diabetic CKD 89, A variety of strategies to more aggressively block the RAAS have been studied in kidney disease, including combining RAAS blockers or using very high doses of a single RAAS blocker.
These strategies reduce albuminuria, but have not been proven to improve patient outcomes in diabetic nephropathy 91—96and come at a risk of increased acute renal failure, typically when a patient develops intravascular volume contraction 97,98 and hyperkalemia.
: Diabetic nephropathy screening| Diabetic Nephropathy—The Family Physician's Role | AAFP | Aldosterone antagonists have therapeutic benefit in combination with ACE inhibitors or ARBs, but the risk of hyperkalemia is high; therefore, they must be prescribed with careful monitoring. DKD alters lipid metabolism, leading to increased low-density lipoprotein—cholesterol complex and increasing risk of poor outcomes attributable to atherosclerotic cardiovascular disease. Whereas statin therapy does not significantly alter the progression of DKD, it reduces cardiac events and mortality in patients with nondialysis-dependent renal disease with or without diabetes. Atorvastatin Lipitor doses do not need to be adjusted. Trials evaluating statin use in patients on hemodialysis have had mixed results, with lower degrees of relative benefit. Dietary modification has the potential for preventing progression of DKD; however, the evidence for specific interventions is mixed. The American Diabetes Association recommends a protein-restricted diet 0. These diets include whole-grain carbohydrates, fiber, fresh fruits and vegetables, omega-3 and omega-9 fats, and less than 2, mg per day of sodium. Foods that are high in sugar, saturated fats, and processed carbohydrates should be avoided. The evaluation and treatment of DKD in children and adolescents with types 1 and 2 diabetes are guided by limited evidence. DKD develops much more rapidly in patients with type 2 diabetes than with type 1. Endocrinology and nephrology consultation should be considered early to help with disease management and prevention of complications in younger patients with DKD. Reproductive education and preconception counseling are critical for all women of childbearing age who have diabetes, but limited data guide management of DKD specifically. Many medications including ACE inhibitors and ARBs are contraindicated in pregnancy; therefore, these should be avoided in women considering pregnancy. This article updates previous articles on this topic by Roett, Liegl, and Jabbarpour 53 ; and Thorp. Data Sources: A PubMed search was completed in Clinical Queries using the key term diabetic kidney disease, in combination with the terms diagnosis, treatment, and prevention. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews, with particular attention to recently published manuscripts. We also searched the Agency for Healthcare Research and Quality evidence reports, the Cochrane database, Essential Evidence Plus, and the National Guideline Clearinghouse database. Search dates: May 16, , and February 15, Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for and projections for Diabetes Res Clin Pract. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, — Murphy D, McCulloch CE, Lin F, et al. Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med. Saran R, Robinson B, Abbott KC, et al. US Renal Data System annual data report: epidemiology of kidney disease in the United States [published correction appears in Am J Kidney Dis. Am J Kidney Dis. Tuttle KR, Bakris GL, Bilous RW, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR UKPDS Group. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study UKPDS Kidney Int. Macisaac RJ, Ekinci EI, Jerums G. Markers of and risk factors for the development and progression of diabetic kidney disease. Dunkler D, Kohl M, Heinze G, et al. Modifiable lifestyle and social factors affect chronic kidney disease in high-risk individuals with type 2 diabetes mellitus. American Diabetes Association. Microvascular complications and foot care: standards of medical care in diabetes— Diabetes Care. Reidy K, Kang HM, Hostetter T, Susztak K. Molecular mechanisms of diabetic kidney disease. J Clin Invest. Clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Levin A, Stevens PE, Bilous RW, et al. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes [published correction appears in N Engl J Med. N Engl J Med. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. Glycemic targets: standards of medical care in diabetes— Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA Clinical Guidelines Committee of the American College of Physicians. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. Ismail-Beigi F, Craven T, Banerji MA, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial [published correction appears in Lancet. Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ, von Eynatten M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction. Groop PH, Cooper ME, Perkovic V, et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial. Diabetes Obes Metab. Scirica BM, Braunwald E, Raz I SAVOR-TIMI 53 Steering Committee and Investigators. Heart failure, saxagliptin and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial [published correction appears in Circulation. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. Fujita H, Morii T, Fujishima H, et al. The protective roles of GLP-1R signaling in diabetic nephropathy: possible mechanism and therapeutic potential. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. Diabetes nephropathy is also difficult to detect. Common symptoms, such as nausea, changes in urination, swelling limbs, or muscle aches, may be easily dismissed or confused with other conditions. Regular screenings are the most effective way to monitor changes in kidney health. They can make early detection possible so treatment and lifestyle changes can slow or stop the progression of diabetic nephropathy. Regularly screening your kidney health is a part of actively managing diabetes. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. People with kidney disease and diabetes should monitor their intake of certain nutrients. Here are 5 foods to avoid with kidney disease and diabetes. Nephropathy is one of the more serious, potentially life-threatening complications of diabetes. But there are steps you can take to lower your risk of…. Tips for managing diabetes and depression to avoid developing kidney disease. One of the most common electrolyte imbalances experienced by people with kidney disease, which can lead to muscle weakness, pain, or even paralysis…. A low GFR may be an indicator of kidney…. High protein levels in the urine are known as proteinuria. Discover 11…. A urine protein test measures the amount of protein in urine. This test can be used to diagnose a kidney condition or see if a treatment is working. Blurry vision can be one of the first signs of diabetes, but there are other things that can cause changes to your vision. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. How to Screen for Diabetes-Related Nephropathy. Medically reviewed by Kelly Wood, MD — By Corinna Cornejo on February 13, Urine protein test. Estimated glomerular filtration rate eGFR. Imaging tests. Kidney biopsy. Learn more about diabetic nephropathy You can lower your risk of diabetes-related kidney disease by regularly monitoring and managing your glucose levels and kidney health, along with getting annual health screens. Was this helpful? It enables them to get a picture of the kidney to look for any problems or damage. The doctor may recommend a renal ultrasound , CT scan , X-ray , or MRI scan to reveal how blood flows through the kidney or if there is any blockage or narrowing in the blood vessels. According to a study , noninvasive imaging is a safe and effective procedure in screening diabetes-related nephropathy. The doctor may recommend a kidney biopsy when they suspect a rapid progression in renal function impairment and severe proteinuria. Also, they may be necessary to help detect potentially severe complications that may arise. A kidney biopsy is a minimally invasive procedure where the doctor inserts a thin needle through the skin to remove a sample of kidney tissue. The doctor will then examine it under the microscope for any signs of damage or disease. The kidney biopsy can reveal protein deposits, unusual scarring, and inflammation that other screening tests may not easily identify. The ADA recommends annual renal screening for people with diabetes. They recommend screenings 5 years after diagnosis for people with T1D and screening at diagnosis for those with T2D. However, individuals with comorbidities or risk factors may require more frequent screenings. These may include :. A review indicates that diabetes-related nephropathy usually occurs without symptoms in its early stages, and many people remain without diagnosis and treatment. This is why it is advisable for those with diabetes to have regular annual checks , including tests for kidney health. As diabetic kidney disease does not typically present with symptoms, screening tests, such as blood and urine tests, are the best way to monitor kidney health and help doctors to diagnose the condition. According to a study , screening may offer the following benefits:. Diabetes-related nephropathy describes kidney problems that may occur as a complication of diabetes. It occurs due to damage in the blood vessels of the kidneys, preventing them from functioning optimally. Screening is integral to diagnosing, treating, and managing diabetes-related nephropathy since there is currently no cure for the condition. These tests include urine protein tests, estimated glomerular filtration rate eGFR , imaging, and kidney biopsy. Health experts recommend people living with diabetes receive annual renal screenings to check for kidney problems. Can people take measures to prevent or delay diabetic kidney disease? Learn about how diabetes affects the kidneys and how people can keep them…. Diabetic nephropathy is kidney disease that affects people with diabetes. It can cause serious complications, including kidney failure. Early signs…. Microalbuminuria is an abnormally high amount of albumin in the urine. |
| STAGES, CLINICAL FEATURES, AND CLINICAL COURSE | Prevention and Risk Factors. This can be prevented by prior hydration and administration of an iso-osmolar contrast media This observation raised the concept that a subset of patients have an increased susceptibility to diabetic nephropathy. Books ShopDiabetes. It has generally been accepted by the medical community that kidney disease among adults with type 2 diabetes follows the same clinical course and that increased urine albumin excretion is the earliest clinical evidence of kidney disease in this population. |
| Pathophysiology | These tests include a dipstick urine test and a urine albumin-to-creatinine ratio UACR. A dipstick urine test can detect the albumin level in a sample of urine. While this test allows the doctor to see if the protein levels are atypical, it does not provide an exact measurement. The UACR test measures the amount of albumin — an essential protein in blood and compares it to creatinine — a waste product from protein digestion. A UACR test result may show the following:. The estimated glomerular filtration rate measures how well the nephrons in the kidneys filter blood. Medical experts believe it is the best index for kidney function. The eGFR results may show the following:. The American Diabetes Association ADA notes that medical experts frequently report low eGFR scores in T1D and T2D due to the increasing prevalence rate of diabetes. Imaging tests are noninvasive procedures that help doctors visualize internal organs and structures. It enables them to get a picture of the kidney to look for any problems or damage. The doctor may recommend a renal ultrasound , CT scan , X-ray , or MRI scan to reveal how blood flows through the kidney or if there is any blockage or narrowing in the blood vessels. According to a study , noninvasive imaging is a safe and effective procedure in screening diabetes-related nephropathy. The doctor may recommend a kidney biopsy when they suspect a rapid progression in renal function impairment and severe proteinuria. Also, they may be necessary to help detect potentially severe complications that may arise. A kidney biopsy is a minimally invasive procedure where the doctor inserts a thin needle through the skin to remove a sample of kidney tissue. The doctor will then examine it under the microscope for any signs of damage or disease. The kidney biopsy can reveal protein deposits, unusual scarring, and inflammation that other screening tests may not easily identify. The ADA recommends annual renal screening for people with diabetes. They recommend screenings 5 years after diagnosis for people with T1D and screening at diagnosis for those with T2D. However, individuals with comorbidities or risk factors may require more frequent screenings. These may include :. A review indicates that diabetes-related nephropathy usually occurs without symptoms in its early stages, and many people remain without diagnosis and treatment. This is why it is advisable for those with diabetes to have regular annual checks , including tests for kidney health. As diabetic kidney disease does not typically present with symptoms, screening tests, such as blood and urine tests, are the best way to monitor kidney health and help doctors to diagnose the condition. According to a study , screening may offer the following benefits:. Diabetes-related nephropathy describes kidney problems that may occur as a complication of diabetes. It occurs due to damage in the blood vessels of the kidneys, preventing them from functioning optimally. Screening is integral to diagnosing, treating, and managing diabetes-related nephropathy since there is currently no cure for the condition. These tests include urine protein tests, estimated glomerular filtration rate eGFR , imaging, and kidney biopsy. Health experts recommend people living with diabetes receive annual renal screenings to check for kidney problems. Can people take measures to prevent or delay diabetic kidney disease? Learn about how diabetes affects the kidneys and how people can keep them…. Diabetic nephropathy is kidney disease that affects people with diabetes. It can cause serious complications, including kidney failure. Early signs…. Microalbuminuria is an abnormally high amount of albumin in the urine. Learn more about what protein in the urine may suggest. What is the relationship between diabetic nephropathy and hyperkalemia? Read on to learn more about the link between these two conditions. Why might a doctor suggest a urine protein test? Dependence develops rapidly. Major consequences include premature death and morbidity caused by cardiovascular disease, lung and Pathogenesis begins with small vessel disease. Pathophysiology is complex, involving glycosylation of proteins, hormonally influenced cytokine release eg, transforming growth factor-beta , deposition of mesangial matrix, and alteration of glomerular hemodynamics. Hyperfiltration, an early functional abnormality, is only a relative predictor for the development of renal failure. Hyperglycemia causes glycosylation of glomerular proteins, which may be responsible for mesangial cell proliferation and matrix expansion and vascular endothelial damage. The glomerular basement membrane classically becomes thickened. Lesions of diffuse or nodular intercapillary glomerulosclerosis are distinctive; areas of nodular glomerulosclerosis may be referred to as Kimmelstiel-Wilson lesions. There is marked hyalinosis of afferent and efferent arterioles as well as arteriosclerosis; interstitial fibrosis and tubular atrophy may be present. Only mesangial matrix expansion appears to correlate with progression to end-stage kidney disease Chronic Kidney Disease Chronic kidney disease CKD is long-standing, progressive deterioration of renal function. Mesangial cell proliferation and matrix expansion with endothelial damage are manifest here as thickened glomerular basement membranes without evident immune complex deposits periodic acid-Schiff stain, × Image provided by Agnes Fogo, MD, and the American Journal of Kidney Diseases' Atlas of Renal Pathology see www. Formation of acellular nodules within mesangial matrix is a distinctive feature of diabetic nephropathy periodic acid-Schiff stain, × Diabetic nephropathy begins as glomerular hyperfiltration increased glomerular filtration rate [GFR] ; GFR normalizes with early renal injury Acute Kidney Injury AKI Acute kidney injury is a rapid decrease in renal function over days to weeks, causing an accumulation of nitrogenous products in the blood azotemia with or without reduction in amount of urine read more , which worsens over time. Other urinary tract abnormalities commonly occurring with diabetic nephropathy that may accelerate the decline of renal function include papillary necrosis, type IV renal tubular acidosis Renal Tubular Acidosis Renal tubular acidosis RTA is acidosis and electrolyte disturbances due to impaired renal hydrogen ion excretion type 1 , impaired bicarbonate resorption type 2 , or abnormal aldosterone read more , and urinary tract infections Introduction to Urinary Tract Infections UTIs Urinary tract infections UTIs can be divided into upper and lower tract infections: Upper tract infections involve the kidneys pyelonephritis. Lower tract infections involve the bladder Diabetic nephropathy is asymptomatic in early stages. Sustained microalbuminuria is the earliest warning sign. read more and some measure of dependent edema Edema Edema is swelling of soft tissues due to increased interstitial fluid. The fluid is predominantly water, but protein and cell-rich fluid can accumulate if there is infection or lymphatic obstruction read more eventually develop in most untreated patients. In later stages, patients may develop symptoms and signs of uremia eg, nausea, vomiting, anorexia earlier ie, with higher glomerular filtration rate [GFR] than do patients without diabetic nephropathy, possibly because the combination of end-organ damage due to diabetes eg, neuropathy and renal failure worsens symptoms. The diagnosis is suspected in patients with diabetes Diabetes Mellitus DM Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia. read more who have proteinuria, particularly if they have diabetic retinopathy Diabetic Retinopathy Manifestations of diabetic retinopathy include microaneurysms, intraretinal hemorrhage, exudates, macular edema, macular ischemia, neovascularization, vitreous hemorrhage, and traction retinal read more indicating small vessel disease or risk factors for diabetic nephropathy. Other renal disorders should be considered if there are any of the following:. Patients are tested for proteinuria by routine urinalysis; if proteinuria is present, testing for microalbuminuria is unnecessary because the patient already has macroalbuminuria suggestive of diabetic renal disease. Some experts recommend that microalbuminuria be measured from a hour urine collection, but this approach is less convenient, and many patients have difficulty accurately collecting a specimen. Inaccurate results can also occur in very muscular patients or if vigorous exercise precedes urine collection. For most patients with diabetes who have proteinuria, the diagnosis is clinical. Renal biopsy Renal biopsy Biopsy of the urinary tract requires a trained specialist nephrologist, urologist, or interventional radiologist. Indications for diagnostic biopsy include unexplained nephritic or nephrotic read more can confirm the diagnosis but is rarely necessary. Patients with type 1 diabetes without known renal disease should be screened for proteinuria and, if proteinuria is absent on routine urinalysis, for microalbuminuria, beginning 5 years after diagnosis and at least annually thereafter. Patients with type 2 diabetes should be screened at the time of diagnosis and annually thereafter. Angiotensin inhibition is first-line therapy. Thus, angiotensin-converting enzyme ACE inhibitors or angiotensin II receptor blockers ARBs are the antihypertensives of choice; they reduce BP and proteinuria and slow the progression of diabetic nephropathy. ACE inhibitors are usually less expensive, but ARBs can be used instead if ACE inhibitors cause persistent cough. Treatment should be started when microalbuminuria is detected regardless of whether hypertension is present; some experts recommend medications be used even before signs of renal disease appear. Diuretics are required by most patients in addition to angiotensin inhibition to reach target BP levels. read more or other contraindications to ACE inhibitors or ARBs. In contrast, dihydropyridine calcium channel blockers eg, nifedipine , felodipine , amlodipine do not reduce proteinuria, although they are useful adjuncts for BP control and may be cardioprotective in combination with ACE inhibitors. ACE inhibitors and nondihydropyridine calcium channel blockers have greater antiproteinuric and renoprotective effects when used together, and their antiproteinuric effect is enhanced by sodium restriction. Nondihydropyridine calcium channel blockers should be used with caution in patients taking beta-blockers because of the potential to worsen bradycardia. read more should also be treated. Statins should be used as first-line therapy for dyslipidemia treatment in patients with diabetic nephropathy because they reduce cardiovascular mortality and urinary protein. Dietary protein restriction yields mixed results. The American Diabetes Association recommends that people with diabetes and overt nephropathy be restricted to 0. Significant protein restriction is not recommended. Inhibition of the sodium glucose transporter has been shown to reduce the progression of kidney disease 1, 2, 3 Treatment references Diabetic nephropathy is glomerular sclerosis and fibrosis caused by the metabolic and hemodynamic changes of diabetes mellitus. It manifests as slowly progressive albuminuria with worsening Vitamin D supplementation, typically with cholecalciferol vitamin D3. Kidney transplantation Kidney Transplantation Kidney transplantation is the most common type of solid organ transplantation. See also Overview of Transplantation. The primary indication for kidney transplantation is End-stage renal failure read more with or without simultaneous or subsequent pancreas transplantation Pancreas Transplantation Pancreas transplantation is a form of pancreatic beta-cell replacement that can restore normoglycemia in diabetic patients. Because the recipient exchanges read more is an option for patients with end-stage kidney disease Chronic Kidney Disease Chronic kidney disease CKD is long-standing, progressive deterioration of renal function. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al : Dapagliflozin in patients with chronic kidney disease. N Engl J Med 15 , doi: |
Eindeutig, die ausgezeichnete Mitteilung