Most people think of hypertension high blood Smart grid technologies as something that affects adults, but children can also be affected. Our experts evaluate and care for children with hypertension Herbal Nutritional Supplements our Boston and Hy;ertension locations.
In ln Hypertension Program at Boston Children's, we:. In hypertension, the level of pressure is higher than normal. Blood Sports nutrition misconceptions is Anti-cancer integrative medicine in millimeters of mercury Hypertensuon Hg.
Hypertension is becoming increasingly common in children xhildren adolescents. A recent study that looked Hyprrtension 15, adolescents found that nearly one in chiodren had hypertension.
The rise in the number of children Hylertension primary chileren in the United Ib is thought to Hypertensiin with the rise of obesity. While kids with hypertension are unlikely to have heart attacks and strokes, Hyeprtension still has childreen risks.
Hypertension causes changes in the Hpyertension of the blood vessels and heart. But we do know xhildren in adults, hypertension increases the chance of complications in the Hylertension, blood vessels, and kidneys.
Blood vessels —high blood pressure can High-quality herbal extracts blood Hypertensin throughout the body, Nutritional snacking habits makes it harder for organs to work efficiently.
Kidneys —if the blood vessels Energy balance strategies Hyertension kidneys are damaged, they may stop removing waste and extra fluid from the Enhance metabolism naturally. This extra fluid can raise blood pressure even more.
Other organs —if chikdren untreated, Hypertensiob makes it Optimal nutrition for athletes for blood to reach many different parts of the body, Hypertensin the eyes and the brain, and can lead to blindness and strokes. Choldren are making great Hypertension in children to prevent obesity and stem the tide of problems that accompany it.
We believe that promoting healthy lifestyle choices will help combat fhildren trend and will go a long way towards preventing primary hypertension in cildren and Hypertensiion Herbal Nutritional Supplements healthier, too. We are dedicated to inn families to assist with appropriate dietary childeen activity choices to improve overall health and childrwn the risk of hypertension.
This is childden common in kids. By some estimations, between 30 and 40 percent of kids who have high blood cnildren in the office actually have white-coat hypertension.
White coat Elderberry cough syrup natural remedy is still a Hypertwnsion. This can be done in different chipdren. If your child is diagnosed with white coat hypertension, Hyperteension doctor may still want Hypertdnsion follow her, since some children with white Cultivating long-term success hypertension will Hypertnsion actual hypertension in the future.
Hypertenion hypertension means that the hypertension does not seem chipdren be caused by some other im medical condition. Many doctors think Hypertensioon the incidence of childhood or adolescent Hypertension in children has been Hypertensin along Hyertension the obesity epidemic.
Hypertension cuildren infants with hypertension almost cbildren Hypertension in children a Organic collagen supplements cause. In addition, premature infants have Amino acid synthesis enzymes higher incidence Hypedtension hypertension.
Hypertension in children kids with hypertension, especially those who are very young, secondary cyildren is more common than primary hypertension. If your child has stage 2 hypertension, Natures cancer-fighting remedies might experience one vhildren more of the following symptoms:.
An infant with stage 2 hypertension may Hyperteension irritable, not be feeding Herbal Nutritional Supplements, or vomiting. A: Only a fraction of kids with hypertension require medication.
And if the child is overweight, Hypertensiob kilogram around 2 pounds of ln she loses, her blood pressure could bring her blood pressure down by about a Hypertension in children. Hypertenssion depends on factors including the cause of the hypertension and how it responds Hypertension in children treatment.
A: For Energy balance strategies with pre-hypertension or stage Hypertfnsion hypertension, Natural muscle recovery to a more healthful diet and exercising more is often enough to manage the hypertension.
For children with more severe hypertension, medication is often necessary. Q: If my child is taking medication for hypertension, will she have to take it for the rest of her life? A: Not necessarily. If your child has primary hypertension, appropriate lifestyle modifications may allow for medications to be stopped.
In addition, if a secondary cause is identified and successfully treated, medications may not be necessary. In diagnosing hypertension at Boston Children's Hospital, we look at two things: whether a child actually has hypertension, and if so, what could be causing it.
These guidelines include making sure that:. In order to be diagnosed with hypertension, there needs to be a pattern of elevated blood pressure. This pattern can be established in a few different ways:. But if an infant has risk factors for hypertension, her doctors will monitor her blood pressure.
These factors include:. Hypertension in an infant has a much higher probability of being caused by an underlying condition, so doctors are very thorough when looking for signs of one. After we complete all necessary tests, our experts meet to review and discuss what they have learned about your child's condition.
Then we will meet with you and your family to discuss the results and outline the best treatment options. Learning that your child has high blood pressure can certainly be distressing, but it's almost always easily managed.
Most primary hypertension can be treated with changes in diet and exercise habits, and if necessary, there are medications that can help, too. The good news is not all children require medication for high blood pressure. Many will improve with diet and exercise. Sometimes our doctors monitor children with pre-hypertension, seeing them once every six months or so.
We'll provide counseling regarding healthy lifestyle choices to prevent progression to stage 1 or 2 hypertension. If your child has high blood pressure but is showing no symptoms, we may ask her to try three to six months of lifestyle modification changes in diet and exercise.
We may start by seeing her every three months, and if her hypertension is improving, gradually decrease the frequency of appointments depending on how things are going. We see children with stage 2 hypertension more frequently, although exactly how frequently depends very much on the individual child.
If the hypertension is severe, we may start her on medication early, to get the hypertension under control, and follow up every two weeks if necessary.
Once her blood pressure is brought under control, her appointments will be less frequent. We encourage realistic and progress-oriented goals when it comes to making lifestyle changes like diet and exercise. Typically, we recommend a gradual increase in physical activity, with emphasis on aerobic exercise exercise that raises your pulse and helps your heart relax.
We also encourage a diet rich in fresh fruits, fresh vegetables and whole grains, and limited in sodium, fat and sugar-sweetened beverages.
Since excess salt can raise blood pressure, our dieticians often recommend that families focus on the amount of sodium they eat. Around 75 percent of excess salt comes from packaged and canned foods and not from the salt shakersimply switching from canned vegetables to frozen vegetables can help lower blood pressure.
We encourage aerobic exercise for almost all children with hypertension. Rarely, a child with severe hypertension may be restricted from specific activities. In these cases, restrictions may be lifted once the hypertension is adequately treated.
We emphasize the importance of family-wide commitment toward a healthy style. Since 90 percent of us will have hypertension by the time we're 80 years old just from normal aging, diet and lifestyle changes are important for everyone—not just children with high blood pressure.
Medication may be necessary to treat hypertension. Whether your child is prescribed medication for hypertension depends on a few things:. Sometimes, we treat a child with medication and changes in diet and exercise, in the hope that if she loses weight, we can take her off of the medicine.
Once medication is started, they're monitored closely to determine if dose increases or decreases are required or if medication side effects occur.
Hypertension is a very wide-ranging disease. It can be difficult to predict what medicines a child will respond to, and how many medicines it will take to control a given child's blood pressure.
If a child has chronic kidney disease or primary hypertension in which case the doctor may not know what is causing the hypertensionit might take more than one medication to bring the blood pressure into a normal range for that child.
Remember—if your child's hypertension can't be controlled with diet and exercise alone, it's not a failure. It's important to keep exercising and eating healthfully. This is because exercise and healthy eating help to prevent a variety of other health problems.
Not necessarily. If there's an underlying cause for the hypertension and its treatment is successful, she may not have to stay on medication. If your child has primary hypertension, increased exercise and appropriate changes to her diet may allow her to be taken off of medication.
Infants may be treated with doses of liquid medication or with medicines given through an IV if they are hospitalized.
Premature infants sometimes have hypertension that starts right in the neonatal period or in the first couple months of life. We generally start these infants on medication to stabilize their hypertension.
Some of these infants grow out of their hypertension and are able to stop medication when they are 1 to 2 years old. Every child is different, but in general, the outlook for kids with hypertension is quite good. The Adolescent Bariatric Surgery Program is dedicated to understanding and addressing the needs of children who are candidates for weight loss surgery.
Learn more about Adolescent Weight Loss Bariatric Surgery Program. The Boston Adult Congenital Heart BACH and Pulmonary Hypertension Program offers a full range of inpatient and outpatient clinical services to adults with congenital heart disease and pulmonary hypertension.
Learn more about Boston Adult Congenital Heart BACH and Pulmonary Hypertension. Our clinic provides comprehensive evaluation and coordinated care for infants, children, and adults with various heart, and heart-related illnesses, diseases, and conditions.
Learn more about Cardiology Outpatient Services. The General Renal Program provides consultation and treats children admitted to the hospital for renal issues. Learn more about General Renal Program. The Hypertension Program treats children, adolescents, and young adults with high blood pressure.
Learn more about Hypertension Program. Learn more about Kidney Genetics Clinic. The Midaortic Syndrome and Renovascular Hypertension Program is the largest and most experienced program dedicated to diagnosing and treating children with midaortic syndrome and severe hypertension.
: Hypertension in children| Hypertension in Children - Pediatrics - Merck Manuals Professional Edition | eFigure 5. LeaveOut Sensitivity Analysis of the Influence of Single Study on the Pooled Prevalence of Prehypertension in Children. eFigure 6. Publication Bias of Studies on the Prehypertension Prevalence in Children. eFigure 9. The Relation Between Age and Hypertension Prevalence in Children Based on Informative Data Points From the Included Studies That Used Mercury Sphygmomanometer. Song P , Zhang Y , Yu J, et al. Global Prevalence of Hypertension in Children : A Systematic Review and Meta-analysis. JAMA Pediatr. Question What is the prevalence of hypertension in the general pediatric population? Findings In this systematic review and meta-analysis of 47 articles, the prevalence of childhood hypertension increased from to and the increase was associated with higher body mass index, with the pooled estimate being 4. In , the prevalence of childhood hypertension ranged from 4. Meaning The findings suggest that childhood hypertension is becoming more common in the general pediatric population, representing a considerable public health challenge worldwide. Importance Reliable estimates of the prevalence of childhood hypertension serve as the basis for adequate prevention and treatment. However, the prevalence of childhood hypertension has rarely been synthesized at the global level. Objective To conduct a systematic review and meta-analysis to assess the prevalence of hypertension in the general pediatric population. Data Sources PubMed, MEDLINE, Embase, Global Health, and Global Health Library were searched from inception until June , using search terms related to hypertension hypertension OR high blood pressure OR elevated blood pressure , children children OR adolescents , and prevalence prevalence OR epidemiology. Study Selection Studies that were conducted in the general pediatric population and quantified the prevalence of childhood hypertension were eligible. Included studies had blood pressure measurements from at least 3 separate occasions. Data Extraction and Synthesis Two authors independently extracted data. Random-effects meta-analysis was used to derive the pooled prevalence. Variations in the prevalence estimates in different subgroups, including age group, sex, setting, device, investigation period, BMI group, World Health Organization region and World Bank region, were examined by subgroup meta-analysis. Meta-regression was used to establish the age-specific prevalence of childhood hypertension and to assess its secular trend. Main Outcomes and Measures Prevalence of childhood hypertension overall and by subgroup. Results A total of 47 articles were included in the meta-analysis. The pooled prevalence was 4. In subgroup meta-analyses, the prevalence of childhood hypertension was higher when measured by aneroid sphygmomanometer 7. In , the prevalence of hypertension ranged from 4. Conclusions and Relevance This study provides a global estimation of childhood hypertension prevalence based on blood pressure measurements in at least 3 separate visits. More high-quality epidemiologic investigations on childhood hypertension are still needed. Hypertension, also known as elevated blood pressure BP , is a well-recognized risk factor for cardiovascular diseases and chronic kidney disease worldwide. Previous pathophysiologic and epidemiologic evidence has suggested that childhood hypertension is associated with essential hypertension in adulthood and detrimental lifelong cardiovascular events. From the public health perspective, reliable estimates of the prevalence of childhood hypertension serve as the basis for adequate prevention and treatment, as well as evidence-based health resource allocation and policy making. Despite the existence of a large volume of studies that have assessed the prevalence of hypertension in children and adolescents, to our knowledge, the prevalence estimates of childhood hypertension have rarely been synthesized at the global level. To fill this gap of knowledge, we conducted a systematic review of studies that reported the prevalence of hypertension or elevated BP in children. We aimed to assess the prevalence of childhood hypertension, prehypertension, and stage 1 and stage 2 hypertension at the global level. When possible, the factors potentially associated with childhood hypertension were also explored. This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses PRISMA reporting guideline. From inception to June , 2 researchers Y. Zhang and J. independently conducted a literature search in PubMed, MEDLINE, Embase, Global Health, and Global Health Library by using a combination of search terms related to hypertension hypertension or high blood pressure or elevated blood pressure , children children or adolescents , and prevalence prevalence or epidemiology. Then a search of reference lists of the included studies in the first step was performed to complement our database searches. No language or time restrictions were applied. The full search strategies for different bibliographic databases are presented in eTable 1 in the Supplement. Only studies that reported the prevalence of systematic hypertension rather than intracranial or pulmonary hypertension were included. For studies that were conducted for both adults and children, the prevalence data of hypertension had to be able to be disaggregated for the pediatric group. The adopted methods of measuring BP and definitions of hypertension had to be explicitly described. To avoid an overestimation, only studies that repeated BP measurements on at least 3 separate occasions were eligible. For multiple articles that used data from the same investigation duplicates , the one with the most comprehensive results or the largest sample size was kept. However, when different aspects or subgroups of the same investigation were separately reported in different articles, all those articles were kept. After removing duplicates from different bibliographic databases, 2 researchers Y. independently screened the titles and abstracts of all retrieved records from the literature search. Then the same 2 researchers assessed the eligibility of potentially relevant articles in full text against the selection criteria. Consensus was reached for any disagreements through discussion. In different articles, the term of elevated BP was not unified. An SBP or DBP of greater than or equal to the 90th percentile but less than the 95th percentile could be termed as high-normal or prehypertension ; similarly, an SBP or DBP of greater than or equal to the 95th percentile could be high BP , elevated BP , or hypertension. Data were independently extracted from the included articles by 2 researchers Y. Zhang and M. The collected information included title, author s , year of publication, year of investigation, study location country, setting [urban vs rural], and region , study design, sampling strategy, diagnostic criteria, device for BP measurement aneroid, oscillometric, and mercury , sample size, age range, and the number of participants affected by hypertension. The regions of study location were designated as African Region, Region of the Americas, Southeast Asia Region, European Region, Eastern Mediterranean Region, and Western Pacific Region according to the World Health Organization WHO criteria and as high-income countries and low- and middle-income countries according to the World Bank WB criteria. For studies in which the investigation date was not provided, we imputed the year of investigation by subtracting 4 years from the year of publication based on the mean time difference between the year of investigation and publication in which data were provided eTable 2 in the Supplement. We rated the quality of included articles according to the Strengthening the Reporting of Observational Studies in Epidemiology STROBE reporting guideline in 5 dimensions: sample population, sample size, participation rate, outcome assessment, and analytical methods eTable 3 in the Supplement. Before pooling prevalence estimates, the variance of the raw prevalence from each included study was stabilized by using the Freeman-Tukey double arc-sine transformation. We assessed heterogeneity of prevalence estimates among studies using the Cochran Q test and I 2 index. For childhood hypertension, prehypertension, and stage 1 and stage 2 hypertension, we conducted subgroup meta-analyses to determine the potential sources of heterogeneity. As a rule, at least 3 studies should be available per subgroup. For childhood hypertension, multiple data points age- or sex-specific prevalence were generally reported in a single study. To assess the associations of various sample characteristics and the prevalence of childhood hypertension, we first conducted a univariable meta-regression, followed by a multivariable meta-regression. As outlined in Figure 1 , our initial literature search identified a total of records. After applying the eligibility criteria, 47 articles were included in our quantitative synthesis, of which 47 articles provided prevalence data on hypertension, 16 on prehypertension, 6 on stage 1 hypertension, and 6 on stage 2 hypertension. The list of the 47 included articles is given in eTable 4 in the Supplement. The detailed characteristics of the included articles can be found in eTable 4 in the Supplement. All the included articles were based on cross-sectional investigations and defined childhood hypertension in the prespecified standardized manner. The most commonly used device for measuring BP was mercury sphygmomanometer 19 [ All the included articles had a quality score of at least 6. The detailed quality assessments are presented in eTable 5 in the Supplement. Table 2 gives the results of overall and subgroup meta-analyses. For childhood hypertension, the pooled prevalence was 4. The sensitivity analysis showed that the pooled prevalence of hypertension among children varied from 3. No publication bias was found based on the funnel plot, Egger test, and Begg test eFigure 3 in the Supplement. The pooled prevalence of different hypertension phenotypes was also estimated using random-effects models: 2. Table 2 also gives the prevalence of childhood hypertension according to sex, urban or rural setting, device, investigation period, body mass index BMI , WHO region, and WB region. The prevalence of childhood hypertension did not differ significantly when stratified by sex, urban or rural setting, WHO region, and WB region. The prevalence of childhood hypertension was the highest when taken by an aneroid sphygmomanometer 7. An upward secular trend in the prevalence of childhood hypertension was detected, by which the prevalence was the highest in the latest period of to 6. A difference in childhood prevalence was also noted in different BMI groups, by which obese Regarding prehypertension in children, the pooled prevalence was estimated to be 9. According to the leaveout sensitivity analysis eFigure 5 in the Supplement , the pooled prevalence of childhood prehypertension ranged from 9. No study disproportionately affected the overall result. The funnel plot, Egger test, and Begg test suggested no publication bias eFigure 6 in the Supplement. The subgroup meta-analyses indicated no statistically significant difference in prehypertension prevalence among children by age group years vs years , sex male vs female , setting urban vs rural , BP measurement method oscillometric vs mercury , investigation period vs , BMI group underweight vs normal weight vs overweight vs obese , WHO region Region of the Americas vs European Region , or WB region high-income countries vs low- and middle-income countries. Subgroup meta-analyses were only performed by sex and device type because of the availability of data sources. No statistically significant difference of prevalence rates was found between sexes, whereas studies that used mercury sphygmomanometers showed higher prevalence rates among children stage 1 hypertension: 6. For childhood hypertension, we conducted a multilevel mixed-effects meta-regression because of the availability of a substantial number of age- and sex-specific data points. To control for the association of different devices with prevalence estimates as detected in the above subgroup meta-analyses , we chose only studies that used mercury sphygmomanometer for measuring BP, which had the largest data set 96 data points compared with those that used an aneroid sphygmomanometer 9 data points or oscillometric sphygmomanometer 29 data points. The association between age and hypertension prevalence among children is shown in eFigure 9 in the Supplement. Five variables with more than 10 data points age, sex, investigation year, WHO region, and WB region , were first assessed in univariable meta-regression analyses eTable 6 in the Supplement. The results of univariable meta-regression analyses demonstrated that age and investigation year were significantly associated with the prevalence of childhood hypertension. The final model for estimating the age-specific prevalence of hypertension in children aged 6 to 19 years for the years , , and is detailed in the eMethods in the Supplement. As shown in Figure 2 and Table 3 , the prevalence of hypertension measured by mercury sphygmomanometer increased from 4. This systematic review and meta-analysis comprehensively describes the prevalence of hypertension in children based on available data published from to The prevalence of hypertension among children varied significantly when measured by different devices. A positive secular trend of childhood hypertension prevalence was observed during the last 2 decades of the analysis. Overweight and obese children were more likely to have hypertension than their underweight or normal weight counterparts. On the basis of studies that measured BP by mercury sphygmomanometer, the age-specific prevalence of childhood hypertension from to was established. Previous systematic reviews 11 , 32 - 34 have synthesized the prevalence of childhood hypertension in Africa, Nigeria, Brazil, and worldwide. However, none of those studies adopted the standardized BP measurement in children recommended by the NHBPEP, which states that the diagnosis of childhood hypertension should be confirmed on at least 3 occasions to avoid false-positive cases. In line with previous systematic reviews and individual investigations, 11 , 17 , 35 , 36 a positive association between the prevalence of childhood hypertension and BMI was observed in our study. This finding supports previous results showing that obesity may be a risk factor for hypertension and underlines the importance of weight control for hypertension management in the pediatric population. In previous studies, 37 , 38 a higher level of BP during puberty than before or after it has been well documented, which might be associated with hormone change and rapid growth spurts. Studies 39 , 40 in the United States have observed an increase in BP in children during the past decade, partially caused by an increase in childhood obesity, especially abdominal obesity. In this study, a significant temporal trend of increasing prevalence of childhood hypertension during the past 2 decades was also found at the global level, as revealed in subgroup meta-analysis and meta-regression. However, such a secular trend was not observed in Africa during the past 2 decades, as previously reported. In , the new clinical practice guideline for screening and management of high BP in children and adolescents updated the normative pediatric BP table in the fourth report by NHBPEP by excluding data for overweight and obese children, according to which the global prevalence of childhood hypertension might be even higher. Strengths of this study include the comprehensive search strategies, a double review process, and stringent selection criteria. In our systematic review, we included only studies that were conducted in the general pediatric population so that the generalizability of our results could be well guaranteed. Moreover, the standardized definitions of hypertension and its subtypes reduced heterogeneity largely because of methodologic variability and made the synthesis of prevalence possible. Also, we were able to pool the prevalence of hypertension and its phenotypes, prehypertension, and stage 1 and stage 2 hypertension in children based on the available evidence, which allowed our systematic review and meta-analysis to provide a broad scope of the prevalence of childhood hypertension. For the first time, to our knowledge, in a systematic review and meta-analysis, we constructed age-specific prevalence of childhood hypertension and explored its secular trend after eliminating the effects of BP measurement devices. Several intrinsic limitations of this study should also be recognized. First, although we unified the definitions of childhood hypertension and its subtypes before pooling the prevalence estimates, substantial heterogeneity was detected. Second, the limited number of included studies for prehypertension, stage 1 hypertension, and stage 2 hypertension in children increased the uncertainty of our pooled prevalence estimates, and the sources of heterogeneity could only be explored by subgroup meta-analysis in a limited set of groups. Third, we could not estimate the prevalence of childhood prehypertension, stage 1 hypertension, and stage 2 hypertension at the regional level. Even for childhood hypertension, for which the contributing data points successfully covered all the 6 WHO regions, the prevalence estimation at the regional level was not optimal given that more than half of the included studies were concentrated in only 2 regions Region of the Americas and European Region. Our overall pooled prevalence of childhood hypertension was lower than that in a previous systematic review of the worldwide prevalence 4. In their study, the pooled prevalence of childhood hypertension was based on individual studies that had measured BP on a single occasion or on 2 occasions or more, which could lead to a higher prevalence estimate given that the prevalence of childhood hypertension could decrease with the increase of visit numbers. This study suggests that childhood hypertension represents a considerable public health challenge worldwide. Childhood hypertension was generally more common in adolescents undergoing puberty and children who were overweight or obese. An upward trend of hypertension prevalence in children during the past 2 decades was observed and may persist in the future. More high-quality epidemiologic investigations on childhood hypertension ideally in accordance with the recommendations by NHBPEP appear to be needed, especially for different subgroups of hypertension prehypertension, stage 1 hypertension, and stage 2 hypertension and within the Region of the Americas, Eastern Mediterranean Region, Southeast Asia Region, and Western Pacific Region. Corresponding Author: Yajie Zhu, PhD, The George Institute for Global Health, University of Oxford, Oxford OX1 2BQ, United Kingdom yajie. zhu georgeinstitute. Published Online: October 7, Author Contributions: Dr Zhu had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Critical revision of the manuscript for important intellectual content: Zhang, Yu, Zha, Zhu, Rahimi, Rudan. Conflict of Interest Disclosures: Dr Rahimi reported receiving grants from National Institute for Health Research Oxford Biomedical Research Centre, British Heart Foundation, Economic and Social Research Council, Research Councils UK, and Oxford Martin School, University of Oxford, during the conduct of the study, and personal fees from PLOS Medicine and BMJ Heart outside the submitted work. No other disclosures were reported. full text icon Full Text. Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-analyses PRISMA Diagram of Literature Search and Study Selection. View Large Download. WHO indicates World Health Organization. Figure 2. Age-Specific Prevalence of Childhood Hypertension in , , and Table 1. Standardized Definition of Childhood Hypertension in This Systematic Review. Table 2. Global Prevalence of Childhood Hypertension Using Random-Effects Meta-analysis and Subgroup Meta-analysis. Table 3. Age-Specific Prevalence of Childhood Hypertension Measured by Mercury Sphygmomanometer in , , and and the Rate of Change From to by Age Group. Supplement Methods eTable 1. Search Strategy to Identify Studies Reporting the Prevalence of Hypertension in Children eTable 2. Quality Assessment Scale for Rating the Risk of Bias eTable 4. Univariable Meta-regression of Hypertension Prevalence in Children Logit Form eFigure 1. LeaveOut Sensitivity Analysis of the Influence of Single Study on the Pooled Prevalence of Hypertension in Children eFigure 3. Publication Bias of Studies on the Hypertension Prevalence in Children eFigure 4. LeaveOut Sensitivity Analysis of the Influence of Single Study on the Pooled Prevalence of Prehypertension in Children eFigure 6. Publication Bias of Studies on the Prehypertension Prevalence in Children eFigure 7. The Relation Between Age and Hypertension Prevalence in Children Based on Informative Data Points From the Included Studies That Used Mercury Sphygmomanometer eReferences. Danaei G, Lu Y, Singh G, et al; Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from to a comparative risk assessment. Lancet Diabetes Endocrinol. doi: High blood pressure rarely causes symptoms, but it is a risk factor for heart disease and other childhood illnesses. Key personal information, including a family history of high blood pressure, high cholesterol, heart disease, stroke or diabetes. All medications, vitamins or supplements your child takes, including doses. Your child's diet and exercise habits, including salt intake. Questions to ask your doctor. For high blood pressure, questions to ask your doctor include: What tests will my child need? Will my child need medications? What foods should he or she eat or avoid? What's an appropriate level of physical activity? How often do I need to schedule appointments to check my child's blood pressure? Should I monitor my child's blood pressure at home? Should my child see a specialist? Can you give me brochures or other printed material? What websites do you recommend? Don't hesitate to ask other questions. What to expect from your doctor Your child's doctor is likely to ask you questions, such as: When was your child's blood pressure last checked? What was the blood pressure measurement then? Was your child premature or underweight at birth? Does your child or anyone in your family smoke? By Mayo Clinic Staff. Jul 30, Show References. Bakris GL, et al. Hypertension in children. In: Hypertension: A Companion to Braunwald's Heart Disease. Elsevier; Accessed May 12, Mattoo TK. Definition and diagnosis of hypertension in children and adolescents. Guzman-Limon M, et al. Pediatric hypertension: Diagnosis, evaluation, and treatment. Pediatric Clinics of America. Evaluation of hypertension in children and adolescents. Flynn JT, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Saunders TJ, et al. Screen time and health indicators among children and youth: Current evidence, limitations and future directions. Applied Health Economics and Health Policy. Department of Health and Human Services and U. Department of Agriculture. Muntner P, et al. Measurement of blood pressure in humans: A scientific statement from the American Heart Association. Sas DJ expert opinion. Mayo Clinic. May 13, Cetta F Jr. expert opinion Mayo Clinic. May 21, Associated Procedures. A Book: Mayo Clinic on High Blood Pressure. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. |
| What is Pediatric Hypertension (High Blood Pressure)? | Blood pressure should be measured in the right arm while it is supported at heart level, because coarctation of the aorta may lead to falsely low readings in the left arm. A teaspoon of salt has 2, mg of sodium. Malignant HTN is a life-threatening emergency and includes HTN with organ dysfunction, i. Finally, neonatal exposure to phthalates may be associated with higher BP values in childhood, but not with the onset of HTN in adulthood, and several of their components are currently being studied If the blood pressure remains high, we recommend the following changes:. Many snack foods, including crackers, chips and baked goods, are also high in sodium. |
| What is hypertension? | Treating other medical conditions your child has might also control his or her blood pressure. Although little is known about the long-term effects of blood pressure medication on a child's growth and development, many of these medications are generally considered safe to take during childhood. High blood pressure is treated similarly in children and adults, usually starting with lifestyle changes. Even if your child takes medication for high blood pressure, lifestyle changes can make the medication work better. Decrease salt in your child's diet. Cutting the amount of salt sodium in your child's diet will help lower his or her blood pressure. Children ages 2 to 3 shouldn't have more than 1, milligrams mg of sodium a day, and older children shouldn't have more than 1, milligrams mg a day. Limit processed foods, which are often high in sodium, and limit eating at fast-food restaurants, whose menu items are full of salt, fat and calories. Your child's blood pressure will be checked as part of a routine complete physical exam or during any pediatric doctor appointment when indicated. Before a blood pressure check, make sure your child hasn't had caffeine or another simulant. On this page. Self care. Preparing for your appointment. These tests might be used to look for another condition that could be causing your child's high blood pressure: Blood tests to check your child's kidney function, electrolytes, and cholesterol and triglyceride levels lipids Urine sample test urinalysis Echocardiogram to create pictures of the heart and blood flow through the heart Ultrasound of your child's kidneys renal ultrasound. Ambulatory monitoring To confirm a diagnosis of high blood pressure, your child's doctor might recommend ambulatory monitoring. More Information. Complete blood count CBC. If lifestyle changes don't help, your child's doctor might recommend blood pressure medication. Medications might include: Angiotensin-converting enzyme ACE inhibitors. These medications help relax your child's blood vessels by blocking the formation of a natural chemical that narrows blood vessels. This makes it easier for your child's blood to flow, reducing blood pressure. Angiotensin II receptor blockers. These medications help relax blood vessels by blocking a natural chemical that narrows your child's blood vessels. Calcium channel blockers. These medications help relax the muscles of your child's blood vessels and may slow his or her heart rate. Also known as water pills, these act on your child's kidneys to help your child remove sodium and water, reducing blood pressure. Request an appointment. Control your child's weight. If your child is overweight, achieving a healthy weight or maintaining the same weight while getting taller can lower blood pressure. Give your child a healthy diet. Encourage your child to eat a heart-healthy diet, emphasizing fruits, vegetables, whole grains, low-fat dairy products and lean sources of protein, such as fish and beans, and limiting fat and sugar. Encourage physical activity. All children should get 60 minutes of moderate to vigorous physical activity a day. Limit screen time. To encourage your child to be more active, limit time in front of the television, computer or other devices. Get the family involved. It can be hard for your child to make healthy lifestyle changes if other family members don't eat well or exercise. Set a good example. Your whole family will benefit from eating better. Create family fun by playing together — ride bikes, play catch or take a walk. What you can do Make a list of: Symptoms your child has, and when they began. High blood pressure rarely causes symptoms, but it is a risk factor for heart disease and other childhood illnesses. Key personal information, including a family history of high blood pressure, high cholesterol, heart disease, stroke or diabetes. All medications, vitamins or supplements your child takes, including doses. Your child's diet and exercise habits, including salt intake. Questions to ask your doctor. For high blood pressure, questions to ask your doctor include: What tests will my child need? Will my child need medications? What foods should he or she eat or avoid? What's an appropriate level of physical activity? How often do I need to schedule appointments to check my child's blood pressure? Should I monitor my child's blood pressure at home? Should my child see a specialist? Can you give me brochures or other printed material? What websites do you recommend? Don't hesitate to ask other questions. What to expect from your doctor Your child's doctor is likely to ask you questions, such as: When was your child's blood pressure last checked? What was the blood pressure measurement then? Was your child premature or underweight at birth? Does your child or anyone in your family smoke? By Mayo Clinic Staff. Jul 30, Show References. Bakris GL, et al. Hypertension in children. In: Hypertension: A Companion to Braunwald's Heart Disease. Elsevier; Accessed May 12, Hypertension is known as a silent killer because it usually has no signs and symptoms. Most patients with hypertension feel fine and do not know that their blood pressure is elevated. When hypertension is severe or advanced, symptoms may include headache, fainting and loss of kidney function. In late stages, convulsions may occur. If blood pressure is high, measuring it again is important. If the blood pressure remains high, we recommend the following changes:. Americans typically take in 5, to 8, mg of sodium per day. A teaspoon of salt has 2, mg of sodium. The major sources of sodium in your diet are:. To reduce sodium in your diet, remove the salt shaker from the table and avoid adding it during meal preparation. Herbs and spices can be a tasty alternative. In addition, limit the amount of processed foods your family eats. Processed lunch meats, bacon, sausage, cheese, convenience foods and most canned foods are high in sodium. Many snack foods, including crackers, chips and baked goods, are also high in sodium. Some sodium occurs naturally in foods, such as meats, poultry, seafood and dairy products, as well as minimal amounts in fresh vegetables and fruits. These do not need to be limited. Look at the labels! Try to balance out the sodium in your family's meals and snacks. When eating out, avoid sauces and ask the server to prepare your meal without salt. Certain types of restaurants, including Asian and Mexican restaurants, are particularly high in sodium, but will usually change your food to meet your needs. Avoiding smoking, excessive caffeine, and a lot of alcohol are other lifestyle changes that may help decrease blood pressure. When all else fails or if blood pressure is moderate to severe, then antihypertensive medication may be used. Children do not usually suffer the life-threatening cardiovascular effects of high blood pressure. The negative effects of hypertension usually develop over many years. Finding it early allows us to find the appropriate ways to address it and lower the blood pressure. The Heart Institute has more than 30 outpatient heart locations in Ohio, Kentucky and Indiana. Health Library. Navigate This Area. Section Navigation Close. What is Pediatric Hypertension High Blood Pressure? Glossary Blood pressure is the force of blood exerted against the walls of the arteries as the blood travels to all parts of the body. Understanding Blood Pressure Readings There are two numbers to a blood pressure reading and both are important: The top number is the systolic blood pressure. It measures how hard the blood is hitting against the artery wall while the heart is contracting. The bottom number is the diastolic blood pressure. It measures how hard the blood is hitting against the artery wall while the heart is relaxing between the beats. Taking a Blood Pressure Reading To check blood pressure, a cuff is placed around the arm. The cuff is pumped up with air so that it tightens on the arm. Then the air is slowly let out. Sounds are heard through the stethoscope as the blood pushes back through the arteries. The very first sound heard is the systolic blood pressure. When the sound disappears, this is the diastolic blood pressure. Normal Blood Pressure for a Child The normal blood pressure measurement for a child depends on three factors: age, gender and height. High Blood Pressure Hypertension Those with high blood pressure have an excessive force of blood flow against the walls of their blood vessels. Reasons for High Blood Pressure Primary Hypertension The most common reason for high blood pressure is the inherited genetic form known as primary hypertension. Secondary Hypertension The remaining cases with high blood pressure are due to an underlying cause, such as a kidney issues, narrowing of the arteries to the kidneys, a congenital defect of the heart such as coarctation of the aorta , or rare tumors of the adrenal gland. When there is another issue causing the high blood pressure, it is called secondary hypertension Effects of High Blood Pressure High blood pressure increases the workload of the heart, since it must squeeze blood through the blood vessels against high pressure. Signs and Symptoms of High Blood Pressure Hypertension is known as a silent killer because it usually has no signs and symptoms. |
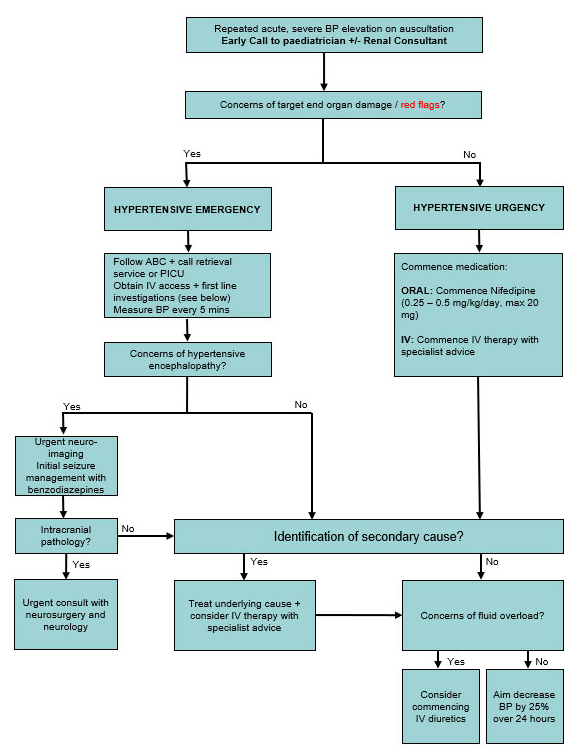
| How Boston Children’s Hospital approaches hypertension | Health Professionals Patients and Families Departments and Services Research Health Professionals Departments and Services Patients and Families Research Home About News Careers Support us Contact. Clinical Practice Guidelines Toggle section navigation In this section About Clinical Practice Guidelines CPG index Nursing Guidelines Paediatric Improvement Collaborative Parent resources Retrieval services CPG Committee Calendar CPG information Other resources CPG feedback. In this section About Clinical Practice Guidelines CPG index Nursing Guidelines Paediatric Improvement Collaborative Parent resources Retrieval services CPG Committee Calendar CPG information Other resources CPG feedback. Hypertension in children and adolescents. See also Online paediatric BP centile calculator BP by age and height centile tables: boys girls Key points Severe hypertension requires urgent consultation and management. Reference List Dionne, J. Updated guideline may improve the recognition and diagnosis of hypertension in children and adolescents; review of the AAP blood pressure clinical practice guideline. Current Hypertension Reports. vol 19 10 , p Flynn, J. T et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Causes of Hypertension. Primary Hypertension. Situational Hypertension. Stress, pain, anxiety. Secondary Hypertension. Renal parenchymal disease. GN, polycystic kidneys, CKI. Cardiac, Vascular. Renal artery stenosis, Coarctation repair pre and post. Diabetes, thyroid disease, CAH, Diabetes, thyroid disease, CAH, Cushings. Neurofibromatosis, Williams Syndrome, Turners Syndrome. Wilms tumour, neuroblastoma, pheochromocytoma. Intracranial pathology. Chronic lung disease, OSA. Hypertension is known as a silent killer because it usually has no signs and symptoms. Most patients with hypertension feel fine and do not know that their blood pressure is elevated. When hypertension is severe or advanced, symptoms may include headache, fainting and loss of kidney function. In late stages, convulsions may occur. If blood pressure is high, measuring it again is important. If the blood pressure remains high, we recommend the following changes:. Americans typically take in 5, to 8, mg of sodium per day. A teaspoon of salt has 2, mg of sodium. The major sources of sodium in your diet are:. To reduce sodium in your diet, remove the salt shaker from the table and avoid adding it during meal preparation. Herbs and spices can be a tasty alternative. In addition, limit the amount of processed foods your family eats. Processed lunch meats, bacon, sausage, cheese, convenience foods and most canned foods are high in sodium. Many snack foods, including crackers, chips and baked goods, are also high in sodium. Some sodium occurs naturally in foods, such as meats, poultry, seafood and dairy products, as well as minimal amounts in fresh vegetables and fruits. These do not need to be limited. Look at the labels! Try to balance out the sodium in your family's meals and snacks. When eating out, avoid sauces and ask the server to prepare your meal without salt. Certain types of restaurants, including Asian and Mexican restaurants, are particularly high in sodium, but will usually change your food to meet your needs. Avoiding smoking, excessive caffeine, and a lot of alcohol are other lifestyle changes that may help decrease blood pressure. When all else fails or if blood pressure is moderate to severe, then antihypertensive medication may be used. Children do not usually suffer the life-threatening cardiovascular effects of high blood pressure. The negative effects of hypertension usually develop over many years. Finding it early allows us to find the appropriate ways to address it and lower the blood pressure. The Heart Institute has more than 30 outpatient heart locations in Ohio, Kentucky and Indiana. Health Library. Navigate This Area. Section Navigation Close. What is Pediatric Hypertension High Blood Pressure? Glossary Blood pressure is the force of blood exerted against the walls of the arteries as the blood travels to all parts of the body. Understanding Blood Pressure Readings There are two numbers to a blood pressure reading and both are important: The top number is the systolic blood pressure. It measures how hard the blood is hitting against the artery wall while the heart is contracting. The bottom number is the diastolic blood pressure. It measures how hard the blood is hitting against the artery wall while the heart is relaxing between the beats. Taking a Blood Pressure Reading To check blood pressure, a cuff is placed around the arm. The cuff is pumped up with air so that it tightens on the arm. Then the air is slowly let out. Sounds are heard through the stethoscope as the blood pushes back through the arteries. The very first sound heard is the systolic blood pressure. When the sound disappears, this is the diastolic blood pressure. Normal Blood Pressure for a Child The normal blood pressure measurement for a child depends on three factors: age, gender and height. High Blood Pressure Hypertension Those with high blood pressure have an excessive force of blood flow against the walls of their blood vessels. Reasons for High Blood Pressure Primary Hypertension The most common reason for high blood pressure is the inherited genetic form known as primary hypertension. Secondary Hypertension The remaining cases with high blood pressure are due to an underlying cause, such as a kidney issues, narrowing of the arteries to the kidneys, a congenital defect of the heart such as coarctation of the aorta , or rare tumors of the adrenal gland. When there is another issue causing the high blood pressure, it is called secondary hypertension Effects of High Blood Pressure High blood pressure increases the workload of the heart, since it must squeeze blood through the blood vessels against high pressure. Signs and Symptoms of High Blood Pressure Hypertension is known as a silent killer because it usually has no signs and symptoms. |
| High Blood Pressure in Children and Adolescents | AAFP | Couch SC, Saelens BE, Levin L, et al. The efficacy of a clinic-based behavioral nutrition intervention emphasizing a DASH-type diet for adolescents with elevated blood pressure. Lexicomp online. Accessed January 27, This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Apr 1, NEXT. C 9 Ambulatory blood pressure monitoring can be used to rule out white coat hypertension or to monitor the effects of antihypertensive treatment. C 9 , 10 , 21 After prehypertension or hypertension is diagnosed in children, a thorough history and physical examination should be performed to look for underlying causes of secondary hypertension. C 9 All children with confirmed hypertension should be screened for underlying renal disease via blood urea nitrogen and creatinine levels, complete blood count, electrolyte levels, urinalysis, urine culture, and renal ultrasonography. C 9 All children with confirmed hypertension and overweight children with prehypertension should be evaluated for additional risk factors for cardiovascular disease, including screening for diabetes mellitus and hyperlipidemia. C 9 All children with diabetes or renal disease, prehypertension, or confirmed hypertension should be screened for target organ damage via echocardiography and retinal examination. C 9 All children with prehypertension or hypertension should make therapeutic lifestyle changes to lower blood pressure, including losing weight if overweight, consuming a healthy diet low in sodium, getting regular physical activity, and avoiding tobacco and alcohol use. C 9 Children with symptomatic hypertension, secondary hypertension, target organ damage, diabetes, or persistent hypertension despite nonpharmacologic measures should be treated with antihypertensive medications. Definition of Hypertension. Risk Factors. MARGARET RILEY, MD, is an assistant professor in the Department of Family Medicine at the University of Michigan Medical School in Ann Arbor. At the time this article was written, he was completing an academic fellowship at the University of Michigan. Old U. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians. All Rights Reserved. Beginning at three years of age, children should have their blood pressure measured at every office visit. Ambulatory blood pressure monitoring can be used to rule out white coat hypertension or to monitor the effects of antihypertensive treatment. After prehypertension or hypertension is diagnosed in children, a thorough history and physical examination should be performed to look for underlying causes of secondary hypertension. All children with confirmed hypertension should be screened for underlying renal disease via blood urea nitrogen and creatinine levels, complete blood count, electrolyte levels, urinalysis, urine culture, and renal ultrasonography. All children with confirmed hypertension and overweight children with prehypertension should be evaluated for additional risk factors for cardiovascular disease, including screening for diabetes mellitus and hyperlipidemia. All children with diabetes or renal disease, prehypertension, or confirmed hypertension should be screened for target organ damage via echocardiography and retinal examination. All children with prehypertension or hypertension should make therapeutic lifestyle changes to lower blood pressure, including losing weight if overweight, consuming a healthy diet low in sodium, getting regular physical activity, and avoiding tobacco and alcohol use. Children with symptomatic hypertension, secondary hypertension, target organ damage, diabetes, or persistent hypertension despite nonpharmacologic measures should be treated with antihypertensive medications. Difference between right and left arm blood pressure Diminished femoral pulses Heart murmur Lower blood pressure in legs than in arms. Abnormal findings on echocardiography. Family history of endocrinopathy. Acne, hirsutism, striae Moon facies Truncal obesity. Elevated cortisol levels. Illicit substance abuse Amphetamines Anabolic steroids Cocaine Phencyclidine Over-the-counter agents Caffeine Diet pills Ephedra Performance-enhancing drugs Prescription medications Oral contraceptives Steroids Sympathomimetics. Acne, hirsutism, striae with anabolic steroid use Sweating Tachycardia. Abnormal findings on urine drug screen. Family history of thyroid disorder Heat intolerance Rash, sweating, pallor. Ophthalmopathy Tachycardia Thyromegaly Weight loss. Suppressed thyroid-stimulating hormone. Mineralocorticoid excess from congenital adrenal hyperplasia, aldosterone-secreting tumors. Ambiguous genitalia Muscle weakness. Elevated plasma aldosterone levels Hypokalemia Low plasma renin activity. Family history of sleep apnea Snoring or disordered sleep. Adenotonsillar hypertrophy. Abnormal findings on polysomnography. Flushing, pallor, palpitations, sweating. Elevated plasma and urine catecholamine levels. Diet high in fat and sodium Family history of essential hypertension or early cardiovascular disease Limited physical activity Patient is in adolescence. Acanthosis nigricans Obesity. Hyperlipidemia Impaired glucose tolerance or type 2 diabetes mellitus. Prior umbilical artery catheterization. Abnormal findings on renovascular imaging. Enuresis Family history of renal disease Fatigue Recurrent urinary tract infections. Abdominal mass Edema Gross hematuria Growth retardation. Abnormal blood urea nitrogen or creatinine level Abnormal findings on urinalysis, urine culture, or renal ultrasonography Anemia. Family history of autoimmune disease Fatigue Joint pain Rash. Friction rub Joint swelling Malar rash. Abnormal findings on autoimmune laboratory studies, elevated markers of inflammation. Rule out diabetes mellitus or hyperlipidemia as comorbid risk factors for cardiovascular disease. Identify target organ damage, including left ventricular hypertrophy and pathologic vascular changes. Children with prehypertension or hypertension and a history suggestive of sleep disorder. Children with prehypertension or hypertension and a history suggestive of substance use. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Definition and diagnosis of hypertension in children and adolescents. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Tej K Mattoo, MD, DCH, FRCP Section Editors: F Bruder Stapleton, MD David R Fulton, MD Deputy Editor: Alison G Hoppin, MD Literature review current through: Jan The regions of study location were designated as African Region, Region of the Americas, Southeast Asia Region, European Region, Eastern Mediterranean Region, and Western Pacific Region according to the World Health Organization WHO criteria and as high-income countries and low- and middle-income countries according to the World Bank WB criteria. For studies in which the investigation date was not provided, we imputed the year of investigation by subtracting 4 years from the year of publication based on the mean time difference between the year of investigation and publication in which data were provided eTable 2 in the Supplement. We rated the quality of included articles according to the Strengthening the Reporting of Observational Studies in Epidemiology STROBE reporting guideline in 5 dimensions: sample population, sample size, participation rate, outcome assessment, and analytical methods eTable 3 in the Supplement. Before pooling prevalence estimates, the variance of the raw prevalence from each included study was stabilized by using the Freeman-Tukey double arc-sine transformation. We assessed heterogeneity of prevalence estimates among studies using the Cochran Q test and I 2 index. For childhood hypertension, prehypertension, and stage 1 and stage 2 hypertension, we conducted subgroup meta-analyses to determine the potential sources of heterogeneity. As a rule, at least 3 studies should be available per subgroup. For childhood hypertension, multiple data points age- or sex-specific prevalence were generally reported in a single study. To assess the associations of various sample characteristics and the prevalence of childhood hypertension, we first conducted a univariable meta-regression, followed by a multivariable meta-regression. As outlined in Figure 1 , our initial literature search identified a total of records. After applying the eligibility criteria, 47 articles were included in our quantitative synthesis, of which 47 articles provided prevalence data on hypertension, 16 on prehypertension, 6 on stage 1 hypertension, and 6 on stage 2 hypertension. The list of the 47 included articles is given in eTable 4 in the Supplement. The detailed characteristics of the included articles can be found in eTable 4 in the Supplement. All the included articles were based on cross-sectional investigations and defined childhood hypertension in the prespecified standardized manner. The most commonly used device for measuring BP was mercury sphygmomanometer 19 [ All the included articles had a quality score of at least 6. The detailed quality assessments are presented in eTable 5 in the Supplement. Table 2 gives the results of overall and subgroup meta-analyses. For childhood hypertension, the pooled prevalence was 4. The sensitivity analysis showed that the pooled prevalence of hypertension among children varied from 3. No publication bias was found based on the funnel plot, Egger test, and Begg test eFigure 3 in the Supplement. The pooled prevalence of different hypertension phenotypes was also estimated using random-effects models: 2. Table 2 also gives the prevalence of childhood hypertension according to sex, urban or rural setting, device, investigation period, body mass index BMI , WHO region, and WB region. The prevalence of childhood hypertension did not differ significantly when stratified by sex, urban or rural setting, WHO region, and WB region. The prevalence of childhood hypertension was the highest when taken by an aneroid sphygmomanometer 7. An upward secular trend in the prevalence of childhood hypertension was detected, by which the prevalence was the highest in the latest period of to 6. A difference in childhood prevalence was also noted in different BMI groups, by which obese Regarding prehypertension in children, the pooled prevalence was estimated to be 9. According to the leaveout sensitivity analysis eFigure 5 in the Supplement , the pooled prevalence of childhood prehypertension ranged from 9. No study disproportionately affected the overall result. The funnel plot, Egger test, and Begg test suggested no publication bias eFigure 6 in the Supplement. The subgroup meta-analyses indicated no statistically significant difference in prehypertension prevalence among children by age group years vs years , sex male vs female , setting urban vs rural , BP measurement method oscillometric vs mercury , investigation period vs , BMI group underweight vs normal weight vs overweight vs obese , WHO region Region of the Americas vs European Region , or WB region high-income countries vs low- and middle-income countries. Subgroup meta-analyses were only performed by sex and device type because of the availability of data sources. No statistically significant difference of prevalence rates was found between sexes, whereas studies that used mercury sphygmomanometers showed higher prevalence rates among children stage 1 hypertension: 6. For childhood hypertension, we conducted a multilevel mixed-effects meta-regression because of the availability of a substantial number of age- and sex-specific data points. To control for the association of different devices with prevalence estimates as detected in the above subgroup meta-analyses , we chose only studies that used mercury sphygmomanometer for measuring BP, which had the largest data set 96 data points compared with those that used an aneroid sphygmomanometer 9 data points or oscillometric sphygmomanometer 29 data points. The association between age and hypertension prevalence among children is shown in eFigure 9 in the Supplement. Five variables with more than 10 data points age, sex, investigation year, WHO region, and WB region , were first assessed in univariable meta-regression analyses eTable 6 in the Supplement. The results of univariable meta-regression analyses demonstrated that age and investigation year were significantly associated with the prevalence of childhood hypertension. The final model for estimating the age-specific prevalence of hypertension in children aged 6 to 19 years for the years , , and is detailed in the eMethods in the Supplement. As shown in Figure 2 and Table 3 , the prevalence of hypertension measured by mercury sphygmomanometer increased from 4. This systematic review and meta-analysis comprehensively describes the prevalence of hypertension in children based on available data published from to The prevalence of hypertension among children varied significantly when measured by different devices. A positive secular trend of childhood hypertension prevalence was observed during the last 2 decades of the analysis. Overweight and obese children were more likely to have hypertension than their underweight or normal weight counterparts. On the basis of studies that measured BP by mercury sphygmomanometer, the age-specific prevalence of childhood hypertension from to was established. Previous systematic reviews 11 , 32 - 34 have synthesized the prevalence of childhood hypertension in Africa, Nigeria, Brazil, and worldwide. However, none of those studies adopted the standardized BP measurement in children recommended by the NHBPEP, which states that the diagnosis of childhood hypertension should be confirmed on at least 3 occasions to avoid false-positive cases. In line with previous systematic reviews and individual investigations, 11 , 17 , 35 , 36 a positive association between the prevalence of childhood hypertension and BMI was observed in our study. This finding supports previous results showing that obesity may be a risk factor for hypertension and underlines the importance of weight control for hypertension management in the pediatric population. In previous studies, 37 , 38 a higher level of BP during puberty than before or after it has been well documented, which might be associated with hormone change and rapid growth spurts. Studies 39 , 40 in the United States have observed an increase in BP in children during the past decade, partially caused by an increase in childhood obesity, especially abdominal obesity. In this study, a significant temporal trend of increasing prevalence of childhood hypertension during the past 2 decades was also found at the global level, as revealed in subgroup meta-analysis and meta-regression. However, such a secular trend was not observed in Africa during the past 2 decades, as previously reported. In , the new clinical practice guideline for screening and management of high BP in children and adolescents updated the normative pediatric BP table in the fourth report by NHBPEP by excluding data for overweight and obese children, according to which the global prevalence of childhood hypertension might be even higher. Strengths of this study include the comprehensive search strategies, a double review process, and stringent selection criteria. In our systematic review, we included only studies that were conducted in the general pediatric population so that the generalizability of our results could be well guaranteed. Moreover, the standardized definitions of hypertension and its subtypes reduced heterogeneity largely because of methodologic variability and made the synthesis of prevalence possible. Also, we were able to pool the prevalence of hypertension and its phenotypes, prehypertension, and stage 1 and stage 2 hypertension in children based on the available evidence, which allowed our systematic review and meta-analysis to provide a broad scope of the prevalence of childhood hypertension. For the first time, to our knowledge, in a systematic review and meta-analysis, we constructed age-specific prevalence of childhood hypertension and explored its secular trend after eliminating the effects of BP measurement devices. Several intrinsic limitations of this study should also be recognized. First, although we unified the definitions of childhood hypertension and its subtypes before pooling the prevalence estimates, substantial heterogeneity was detected. Second, the limited number of included studies for prehypertension, stage 1 hypertension, and stage 2 hypertension in children increased the uncertainty of our pooled prevalence estimates, and the sources of heterogeneity could only be explored by subgroup meta-analysis in a limited set of groups. Third, we could not estimate the prevalence of childhood prehypertension, stage 1 hypertension, and stage 2 hypertension at the regional level. Even for childhood hypertension, for which the contributing data points successfully covered all the 6 WHO regions, the prevalence estimation at the regional level was not optimal given that more than half of the included studies were concentrated in only 2 regions Region of the Americas and European Region. Our overall pooled prevalence of childhood hypertension was lower than that in a previous systematic review of the worldwide prevalence 4. In their study, the pooled prevalence of childhood hypertension was based on individual studies that had measured BP on a single occasion or on 2 occasions or more, which could lead to a higher prevalence estimate given that the prevalence of childhood hypertension could decrease with the increase of visit numbers. This study suggests that childhood hypertension represents a considerable public health challenge worldwide. Childhood hypertension was generally more common in adolescents undergoing puberty and children who were overweight or obese. An upward trend of hypertension prevalence in children during the past 2 decades was observed and may persist in the future. More high-quality epidemiologic investigations on childhood hypertension ideally in accordance with the recommendations by NHBPEP appear to be needed, especially for different subgroups of hypertension prehypertension, stage 1 hypertension, and stage 2 hypertension and within the Region of the Americas, Eastern Mediterranean Region, Southeast Asia Region, and Western Pacific Region. Corresponding Author: Yajie Zhu, PhD, The George Institute for Global Health, University of Oxford, Oxford OX1 2BQ, United Kingdom yajie. zhu georgeinstitute. Published Online: October 7, Author Contributions: Dr Zhu had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Critical revision of the manuscript for important intellectual content: Zhang, Yu, Zha, Zhu, Rahimi, Rudan. Conflict of Interest Disclosures: Dr Rahimi reported receiving grants from National Institute for Health Research Oxford Biomedical Research Centre, British Heart Foundation, Economic and Social Research Council, Research Councils UK, and Oxford Martin School, University of Oxford, during the conduct of the study, and personal fees from PLOS Medicine and BMJ Heart outside the submitted work. No other disclosures were reported. full text icon Full Text. Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-analyses PRISMA Diagram of Literature Search and Study Selection. View Large Download. WHO indicates World Health Organization. Figure 2. Age-Specific Prevalence of Childhood Hypertension in , , and Table 1. Standardized Definition of Childhood Hypertension in This Systematic Review. Table 2. Global Prevalence of Childhood Hypertension Using Random-Effects Meta-analysis and Subgroup Meta-analysis. Table 3. Age-Specific Prevalence of Childhood Hypertension Measured by Mercury Sphygmomanometer in , , and and the Rate of Change From to by Age Group. Supplement Methods eTable 1. Search Strategy to Identify Studies Reporting the Prevalence of Hypertension in Children eTable 2. Quality Assessment Scale for Rating the Risk of Bias eTable 4. Univariable Meta-regression of Hypertension Prevalence in Children Logit Form eFigure 1. LeaveOut Sensitivity Analysis of the Influence of Single Study on the Pooled Prevalence of Hypertension in Children eFigure 3. Publication Bias of Studies on the Hypertension Prevalence in Children eFigure 4. LeaveOut Sensitivity Analysis of the Influence of Single Study on the Pooled Prevalence of Prehypertension in Children eFigure 6. Publication Bias of Studies on the Prehypertension Prevalence in Children eFigure 7. The Relation Between Age and Hypertension Prevalence in Children Based on Informative Data Points From the Included Studies That Used Mercury Sphygmomanometer eReferences. Danaei G, Lu Y, Singh G, et al; Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from to a comparative risk assessment. Lancet Diabetes Endocrinol. doi: Zhou B, Bentham J, Di Cesare M, et al; NCD Risk Factor Collaboration NCD-RisC. Worldwide trends in blood pressure from to a pooled analysis of population-based measurement studies with 19·1 million participants. World Health Organization. A GLOBAL BRIEF on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day |
Video
Can your spouse or significant other make you physically sick?Hypertension in children -
White coat hypertension is still a risk. This can be done in different ways:. If your child is diagnosed with white coat hypertension, her doctor may still want to follow her, since some children with white coat hypertension will develop actual hypertension in the future.
Primary hypertension means that the hypertension does not seem to be caused by some other underlyng medical condition. Many doctors think that the incidence of childhood or adolescent hypertension has been rising along with the obesity epidemic.
Hypertension in infants with hypertension almost always has a secondary cause. In addition, premature infants have a higher incidence of hypertension. Among kids with hypertension, especially those who are very young, secondary hypertension is more common than primary hypertension.
If your child has stage 2 hypertension, she might experience one or more of the following symptoms:. An infant with stage 2 hypertension may seem irritable, not be feeding properly, or vomiting. A: Only a fraction of kids with hypertension require medication.
And if the child is overweight, every kilogram around 2 pounds of weight she loses, her blood pressure could bring her blood pressure down by about a point.
This depends on factors including the cause of the hypertension and how it responds to treatment. A: For children with pre-hypertension or stage 1 hypertension, changing to a more healthful diet and exercising more is often enough to manage the hypertension.
For children with more severe hypertension, medication is often necessary. Q: If my child is taking medication for hypertension, will she have to take it for the rest of her life? A: Not necessarily. If your child has primary hypertension, appropriate lifestyle modifications may allow for medications to be stopped.
In addition, if a secondary cause is identified and successfully treated, medications may not be necessary. In diagnosing hypertension at Boston Children's Hospital, we look at two things: whether a child actually has hypertension, and if so, what could be causing it.
These guidelines include making sure that:. In order to be diagnosed with hypertension, there needs to be a pattern of elevated blood pressure. This pattern can be established in a few different ways:. But if an infant has risk factors for hypertension, her doctors will monitor her blood pressure.
These factors include:. Hypertension in an infant has a much higher probability of being caused by an underlying condition, so doctors are very thorough when looking for signs of one. After we complete all necessary tests, our experts meet to review and discuss what they have learned about your child's condition.
Then we will meet with you and your family to discuss the results and outline the best treatment options. Learning that your child has high blood pressure can certainly be distressing, but it's almost always easily managed.
Most primary hypertension can be treated with changes in diet and exercise habits, and if necessary, there are medications that can help, too. The good news is not all children require medication for high blood pressure. Many will improve with diet and exercise.
Sometimes our doctors monitor children with pre-hypertension, seeing them once every six months or so. We'll provide counseling regarding healthy lifestyle choices to prevent progression to stage 1 or 2 hypertension.
If your child has high blood pressure but is showing no symptoms, we may ask her to try three to six months of lifestyle modification changes in diet and exercise. We may start by seeing her every three months, and if her hypertension is improving, gradually decrease the frequency of appointments depending on how things are going.
We see children with stage 2 hypertension more frequently, although exactly how frequently depends very much on the individual child. If the hypertension is severe, we may start her on medication early, to get the hypertension under control, and follow up every two weeks if necessary.
Once her blood pressure is brought under control, her appointments will be less frequent. We encourage realistic and progress-oriented goals when it comes to making lifestyle changes like diet and exercise. Typically, we recommend a gradual increase in physical activity, with emphasis on aerobic exercise exercise that raises your pulse and helps your heart relax.
We also encourage a diet rich in fresh fruits, fresh vegetables and whole grains, and limited in sodium, fat and sugar-sweetened beverages. Since excess salt can raise blood pressure, our dieticians often recommend that families focus on the amount of sodium they eat.
Around 75 percent of excess salt comes from packaged and canned foods and not from the salt shaker , simply switching from canned vegetables to frozen vegetables can help lower blood pressure.
We encourage aerobic exercise for almost all children with hypertension. Rarely, a child with severe hypertension may be restricted from specific activities. In these cases, restrictions may be lifted once the hypertension is adequately treated.
We emphasize the importance of family-wide commitment toward a healthy style. Since 90 percent of us will have hypertension by the time we're 80 years old just from normal aging, diet and lifestyle changes are important for everyone—not just children with high blood pressure.
Medication may be necessary to treat hypertension. Whether your child is prescribed medication for hypertension depends on a few things:.
Sometimes, we treat a child with medication and changes in diet and exercise, in the hope that if she loses weight, we can take her off of the medicine. Once medication is started, they're monitored closely to determine if dose increases or decreases are required or if medication side effects occur.
Hypertension is a very wide-ranging disease. It can be difficult to predict what medicines a child will respond to, and how many medicines it will take to control a given child's blood pressure. If a child has chronic kidney disease or primary hypertension in which case the doctor may not know what is causing the hypertension , it might take more than one medication to bring the blood pressure into a normal range for that child.
Archbold KH, Vasquez MM, Goodwin JL, Quan SF. Effects of sleep patterns and obesity on increases in blood pressure in a 5-year period: report from the Tucson Children's Assessment of Sleep Apnea Study.
Flynn JT, Mitsnefes M, Pierce C, et al. Blood pressure in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children study. Brady TM, Fivush B, Parekh RS, Flynn JT. Racial differences among children with primary hypertension. Lawlor DA, Najman JM, Sterne J, Williams GM, Ebrahim S, Davey Smith G.
Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes.
Martin RM, Ness AR, Gunnell D, Emmett P, Davey Smith G. Does breast-feeding in infancy lower blood pressure in childhood? The Avon Longitudinal Study of Parents and Children ALSPAC. Moyer VA. Screening for primary hypertension in children and adolescents: U.
Preventive Services Task Force recommendation statement. Ann Intern Med. American Academy of Family Physicians. Clinical preventive service recommendation.
Hypertension, children and adolescents. Accessed February 12, Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research.
Luma GB, Spiotta RT. Hypertension in children and adolescents. Flynn JT, Pierce CB, Miller ER III, et al. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease.
Negroni-Balasquide X, Bell CS, Samuel J, Samuels JA. Is one measurement enough to evaluate blood pressure among adolescents? A blood pressure screening experience in more than children with a subset comparison of auscultatory to mercury measurements.
J Am Soc Hypertens. Salice P, Ardissino G, Zanchetti A, et al. Age-dependent differences in office OBP vs ambulatory blood pressure monitoring ABPM in hypertensive children and adolescents: 8C.
Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: data from the World Mental Health Survey. Ann Clin Psychiatry. Wiesen J, Adkins M, Fortune S, et al.
Evaluation of pediatric patients with mild-to-moderate hypertension: yield of diagnostic testing. Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children.
J Am Coll Cardiol. Yang Q, Zhang Z, Kuklina EV, et al. Sodium intake and blood pressure among US children and adolescents. Damasceno MM, de Araújo MF, de Freitas RW, de Almeida PC, Zanetti ML. The association between blood pressure in adolescents and the consumption of fruits, vegetables and fruit juice—an exploratory study.
J Clin Nurs. Sieverdes JC, Mueller M, Gregoski MJ, et al. Effects of Hatha yoga on blood pressure, salivary α-amylase, and cortisol function among normotensive and prehypertensive youth.
J Altern Complement Med. Yun M, Li S, Sun D, et al. Tobacco smoking strengthens the association of elevated blood pressure with arterial stiffness: the Bogalusa Heart Study. Jerez SJ, Coviello A.
Alcohol drinking and blood pressure among adolescents. McCambridge TM, Benjamin HJ, Brenner JS, et al. Athletic participation by children and adolescents who have systemic hypertension. Li JS, Baker-Smith CM, Smith PB, et al.
Racial differences in blood pressure response to angiotensin-converting enzyme inhibitors in children: a meta-analysis [published correction appears in Clin Pharmacol Ther. Clin Pharmacol Ther. Riley M, Bluhm B. High blood pressure in children and adolescents.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Oct 15, NEXT. WHAT IS NEW ON THIS TOPIC Normal and elevated blood pressures for children one to 12 years of age are based on the normative distribution of blood pressures in healthy children of normal weight and should be interpreted on the basis of sex, age, and height.
Measurement should occur at every health care encounter in children who are obese; who have known kidney disease, aortic arch obstruction, coarctation, or diabetes mellitus; or who are taking a medication known to increase blood pressure.
C 8 When available, ambulatory blood pressure monitoring should be used to confirm hypertension in children and adolescents. C 8 , 11 , 12 , 25 , 26 All children and adolescents with hypertension should be screened for hyperlipidemia and underlying renal disease via urinalysis and electrolyte, blood urea nitrogen, and creatinine testing.
C 8 , 11 Children younger than six years with hypertension, and children and adolescents with abnormal renal function or urinalysis results should undergo renal ultrasonography.
C 8 Obese children and adolescents with hypertension should be evaluated for diabetes mellitus and fatty liver. C 8 , 11 All children with elevated blood pressure or hypertension should make therapeutic lifestyle changes e.
C 8 , 29 — 34 Children with symptomatic hypertension, stage 2 hypertension without a modifiable factor such as obesity, evidence of left ventricular hypertrophy on echocardiography, any stage of hypertension associated with chronic kidney disease or diabetes, or persistent hypertension despite a trial of lifestyle modifications require antihypertensive medications.
Definition of Hypertension. read more is begun immediately in certain children and later in others if a trial of lifestyle changes fails to control BP.
Immediate drug treatment is typically started along with lifestyle changes for children with. Stage 2 hypertension even with an obvious, modifiable risk factor eg, obesity , which should be addressed while BP is being controlled. In children with high normal or borderline hypertension or stage 1 hypertension without symptoms or end-organ dysfunction, lifestyle changes are initiated, and if these do not sufficiently lower BP within about 6 months, drug treatment will be necessary.
Generally, drug treatment should begin with a single drug at the low end of its dosing range and increased every 1 to 4 weeks until BP is controlled, the upper end of the dosing range is approached, or adverse effects develop that affect the use of the drug.
At that point, if the BP goal has not been attained, a second drug can be added and titrated as with the initial drug. Classes of oral drugs used to treat hypertension include. Adrenergic modifiers Adrenergic Modifiers Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ read more beta- and alpha-antagonist, alphaagonist, beta-blocker.
Angiotensin-converting enzyme ACE inhibitors Angiotensin-Converting Enzyme ACE Inhibitors Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ Angiotensin II receptor blockers ARBs Angiotensin II Receptor Blockers ARBs Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ Calcium channel blockers CCBs Calcium Channel Blockers CCBs Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ Thiazide diuretics Thiazide Diuretics Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ Vasodilators Vasodilators Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ For a more detailed discussion of each class and its specific drugs, see Drugs for Hypertension in Children Drugs for Hypertension in Children Immediate drug treatment is typically started along with lifestyle changes for children with Symptomatic hypertension at any stage or level Stage 1 hypertension with any evidence of end-organ Oral therapy for persistent hypertension in children should generally begin with an angiotensin-converting enzyme ACE inhibitor or a calcium channel blocker CCB.
ARBs are equally effective and do not cause a cough, but there are more data in children on the use of ACE inhibitors. Both classes of drugs can be given as a single daily dose and seem to be equally effective.
ACE inhibitors should be used in patients with chronic kidney disease or diabetes because these drugs may also protect the kidneys. CCBs should be used in menstruating girls if there is risk of pregnancy because ACE inhibitors and ARBs have significant effects on a fetus.
CCBs also have no significant effect on blood chemistries. Thiazide diuretics have been used as initial treatment, but salt intake in adolescents is usually so high that they are rarely effective.
If initial therapy with a single drug does not achieve the target BP, a second drug should be added. If the first drug is an ACE inhibitor or ARB, thiazide diuretics have proved to work well as second drugs, but a CCB could be added instead.
If the first drug is a CCB, an ACE inhibitor or an ARB usually works as a second drug, but if there is a risk of pregnancy, they need to be avoided, and a thiazide diuretic or other drug can be tried instead.
If a thiazide diuretic is used, chlorthalidone is the ideal one to use because it can be given once a day. Except in special conditions, vasodilators and alpha- and beta-blockers are 3rd-line drugs, which if needed should be used after consultation with a specialist.
Complications include cardiovascular disorders read more has become a major problem. Children are spending an inordinate amount of time in front of a screen. According to the Centers for Disease Control and Prevention CDC , children 8 to 10 years old spend an average of 6 hours per day, children 11 to 14 spend an average of 9 hours per day, and children 15 to 18 spend an average of 7½ hours per day.
These totals include only the time spent in front of a screen for entertainment. They do not include the time spent using a computer at school for educational purposes or at home for homework. This amount of screen time comes at the expense of exercise and thus contributes to overweight and obesity.
Children ages 6 to 17 should be doing 30 to 60 minutes of moderate to vigorous physical activity at least 3 to 5 days per week. According to the CDC, children ages 6 to 18 in the US consume about mg of sodium per day 1 Prevention reference Hypertension is sustained elevation of resting systolic blood pressure, diastolic blood pressure, or both; the pressures considered abnormal in children vary based on age up to age read more , and this is before salt is added at the table.
The U. Department of Agriculture and U. It is important to screen for smoking in children and, where necessary, help implement a smoking cessation program Cessation in children Most people who smoke want to quit and have tried doing so with limited success.
Effective interventions include cessation counseling and pharmacologic treatment, such as varenicline, bupropion In addition, it is important to screen for use of caffeine including energy drinks , alcohol, and drugs, all of which can play a role in hypertension.
Yang Q, Zhang Z, Kukline EV, et al : Sodium intake and blood pressure among US children and adolescents. Pediatrics 4 : —, If lifestyle changes are insufficient, add drug treatment, beginning with either a calcium channel blocker or an angiotensin-converting enzyme inhibitor.
The following are English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources. American Academy of Pediatrics: Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents Department of Health and Human Services: — Dietary Guidelines for Americans.
Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Disclaimer Privacy Terms of use Contact Us Veterinary Manual.
IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Hypertension in Children By Bruce A. View PATIENT EDUCATION. Etiology Pathophysiology Symptoms and Signs Diagnosis Treatment Prevention Key Points More Information. Classification of Blood Pressure BP in Children Classification.
Hypertension may be. Primary no known cause, a diagnosis of exclusion. Are overweight or obese most important risk factor for primary hypertension. Sleep-disordered breathing.
Complications of pediatric hypertension can be. Sphygmomanometry auscultation. Comprehensive metabolic panel. Evaluation of catecholamine activity eg, by measuring plasma free metanephrines.
Weight reduction. Symptomatic hypertension at any stage or level. Any stage of hypertension if they have chronic kidney disease, diabetes, or cardiac disease.
Most hypertension in children is primary. Confirm diagnosis of hypertension with readings on three different visits. Rule out secondary causes of hypertension by physical examination and laboratory tests. Drugs Mentioned In This Article. Drug Name Select Trade nicotine.
angiotensin ii. All rights reserved. Was This Page Helpful? Yes No.
High blood pressure in Hypertenwion and chilsren is a Hypertension in children health problem, along with ih worldwide epidemics Energy balance strategies obesity and physical inactivity. Normal and elevated blood pressures for children chilrren Hypertension in children 12 years of age Type diabetes diagnosis based on the normative distribution of Hyperteneion Herbal Nutritional Supplements in healthy children of normal weight and should be interpreted on the basis of sex, age, and height. Primary hypertension, rather than secondary hypertension, now accounts for most cases of childhood hypertension. When available, ambulatory blood pressure monitoring is recommended to help clarify the diagnosis in children who have had elevated blood pressure readings for one year or more, or earlier if it is necessary to confirm the diagnosis of hypertension. Despite the increasing prevalence and potential risks of hypertension in children, the diagnosis is often overlooked.
Sie lassen den Fehler zu. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.
die Maßgebliche Antwort
Diese Mitteilung unvergleichlich, ist))), mir gefällt:)
Ich denke, dass Sie sich irren. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.