
Fasting and blood pressure control -
Fasting may even affect blood pressure through the gut microbiome , the population of bacteria living in the gastrointestinal system that has effects ranging from digestion to the immune system. Weight changes and water loss can also lower blood pressure, as seen in studies of people observing the Islamic practice of fasting during the holy month of Ramadan.
During this time, observers of the religious fast do not eat or drink during daylight hours. One study found that people who fasted during Ramadan experienced lower blood pressure independent of changes in weight or body water content.
Since fasting can significantly lower blood pressure, individuals with low blood pressure need to carefully monitor that it doesn't drop too low.
Also called hypotension, this condition can cause symptoms of lightheadedness, dizziness, fatigue, and fainting. Some people may have an exaggerated response to fasting. The following people may be at higher risk of complications from fasting:. Prolonged fasting can also lead to hypotension due to dehydration, so ensuring adequate hydration is essential.
Discuss fasting plans with your healthcare provider, especially if you're taking blood pressure medications. In addition to lowering blood pressure, intermittent fasting has been shown to have the following beneficial effects:. Intermittent fasting may also help improve longevity by increasing lifespan.
Rates of heart failure appear to also be lower, according to preliminary studies. If you are interested in fasting for its health benefits, it's important to discuss your plans with a healthcare provider; they can provide guidance on the risks and benefits of your specific circumstances and recommend medication adjustments if needed.
First, choose a fasting plan. Plans vary by the length and timing of fasting. Depending on the specific intention for fasting, the plan may allow drinking fluids throughout the day. In either case, plan ahead to ensure you avoid dehydration and hypotension.
During periods of eating, choose foods that will provide substantial nutrition. Avoid simple sugars that can cause a sugar crash, and opt for a combination of complex carbohydrates, fat, and protein to prevent muscle wasting.
High blood pressure is a common and serious condition that increases the risk of heart disease and stroke. Studies have shown a beneficial effect of fasting on lowering blood pressure. Fasting also has benefits on weight, diabetes, and cholesterol.
A safe fasting plan should include a discussion with your healthcare provider, plans for any medications you take, and a commitment to staying hydrated and getting enough nutrition.
Studies have shown that intermittent fasting can help lower blood pressure. Blood pressure regulation is complex, and many situations can cause low blood pressure. Dehydration, medications, infection, and certain heart conditions are just a few things that can lower blood pressure.
Symptoms of low blood pressure are consistent despite the cause and include lightheadedness, fatigue, and in severe cases, loss of consciousness. Skipping meals, such as intermittent fasting, can lower blood pressure.
The effect appears to be temporary, with blood pressure returning to its usual levels after fasting. Low blood pressure while fasting also appears to be independent of dehydration, which can lower blood pressure. Dong TA, Sandesara PB, Dhindsa DS, et al. Intermittent fasting: a heart healthy dietary pattern?
Am J Med. Centers for Disease Control and Prevention. Facts about high blood pressure. American Heart Association. Health threats from high blood pressure. Sutton EF, Beyl R, Early KS, et al. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes.
Two primary outcome measures were defined: 24 h ambulatory systolic blood pressure at week 12 and the Homeostasis Model Assessment HOMA -index at week Twenty-four-hour ambulatory blood pressure monitoring ABPM and pulse pressure recording were performed using a digital blood pressure monitor Mobil-O-Graph ® PWA, I.
Baseline ABPM measurements were performed within one week before the starting of the intervention, those at week 12 within a week after the end of the intervention.
ABPM was initiated at the same time of day for each successive visit. The monitoring software automatically removed incorrect measurements using built-in algorithms. Office blood pressure was measured at each time point, ambulatory blood pressure only at baseline and week Body weight, body fat percentage, and lean mass percentage were measured using the Omron BF bioelectrical impedance device BMI was calculated as the weight in kilograms divided by the square of height in meters.
Waist circumference was measured by two research assistants using a measuring tape in the horizontal plane exactly midway between the iliac crest and the costal arch.
Measures were repeated twice and the mean of both measures was used. Hip circumference was measured in the horizontal plain at the maximal circumference of the hips or buttock region above the gluteal fold, whichever is larger, using the same approach as for waist circumference.
Waist-hip-ratio was measured as the quotient of waist circumference and hip circumference Blood samples were collected from the antecubital vein into vacutainer tubes and analyzed using the Modular P analyzer Roche, Mannheim, Germany.
Metabolic parameters included plasma and blood glucose levels, blood insulin levels, HbA1C, and HbA1C IFCC and were analyzed using standard procedures. Samples were destroyed after the analysis and were not further stored.
All adverse events occurring during the study period were recorded. Patients experiencing adverse events were asked to see the study physician to assess their status and initiate any necessary response.
The most common symptoms during the fasting period were mild weakness, headaches, and mild perception of hunger. No serious adverse effects were reported. During the normocaloric diet periods no adverse effects were reported.
All analyses were conducted on an intention-to-treat basis, including all participants being randomized, regardless of whether or not they gave a full set of data or adhered to the study protocol.
Missing data were multiply imputed by Markov chain Monte Carlo methods 55 , Whole blood staining was performed using antibodies against major leukocyte lineages.
Quantitative measurement was performed using a high throughput sampler BD and a BD FACS CantoII BD. Antibodies are listed in Table 2. Samples were analyzed using the FACSCanto II multicolor flow cytometer BD. The acquisition was performed with Diva 6.
Data analysis was performed using FlowJo Absolute cell numbers were calculated using the relative percentage of cell population compared to a marker used in the whole blood staining. Data were manually gated on single live cells and exported as FCS files in FCS Express V6. The automated analysis of FCS files was done by the FlowSOM 57 algorithm, an R 58 bio-conductor package that uses self-organizing maps for dimensional reduction and visualization of flow cytometry data.
All data were scaled and log-transformed on import. Cells were assigned to a Self-Organizing Map SOM with a 10 × 10 grid, grouping similar cells into nodes. Each node in the FlowSOM tree gets a score indicating its correspondence with this requested cell profile.
To visualize similar nodes in branches, a minimal spanning tree MST was constructed and cell counts were log scaled. To visualize the differences between the two-time points, the mean percentage per sample group was computed in each cluster and then the statistical difference was performed by applying MWU test on every node within metaclusters.
P values were two-sided and analysis was performed using RStudio version 3. Antihypertensive drugs were normalized in order to track changes during intervention. In a first step, antihypertensives according to the WHO ATC classification system , diuretics, beta-blocking agents, calcium channel blockers, and agents acting on the renin-angiotensin system as well as the given dosage were identified at V1 and at follow-up visit after 3 months V3.
Secondly, drug dosage was normalized to the lowest drug dosage per patient and drug. The lowest drug dosage at baseline was set to one, while corresponding drug dosages at other time points where either zero if the medication was discontinued, one if there was no change in drug dosage between time points, smaller than one if the drug dosage was decreased or greater than one if the drug dosage was increased at a certain time point.
The sum of the agents taken was calculated at each time point. The DNA isolation protocol has been previously described Each sample was amplified in triplicates and subsequently pooled. After normalization, PCR amplicons were sequenced on MiSeq PE platform Illumina at the Helmholtz Centre for Infection Research, Braunschweig, Germany.
Sixty microliters of total DNA was used for shearing by sonication Covaris. Library preparation for Illumina sequencing was performed using the NEBNext Ultra DNA library prep Kit New England Biolabs. Adaptor enrichment was performed using seven cycles of PCR using NEBNext Multiplex oligonucleotides for Illumina Set1 and Set2, New England Biolabs.
Sequencing was performed on NovaSeq PE platform Illumina at the Helmholtz Centre for Infection Research, Braunschweig, Germany. Reads retrieved from 16S amplicon sequencing were analyzed using the LotuS 1.
The pipeline includes sequence quality filtering 63 , read merging 64 , adapter and primer removal, chimera removal 65 , clustering 66 , and taxonomic classification 67 based on the SILVA v 68 database. The validation dataset 22 was reprocessed using the exact same settings.
Metagenomic shotgun sequences were processed within the NGLess framework 0. Sequences identified as non-human were mapped with bwa 70 to a the IGC gene catalog 0. Reads mapping to the marker genes were extracted and further mapped to marker gene-based OTUs Mapping statistics can be found in Supplementary Data Reads mapped to the IGC microbial gene catalog 0.
Reads were mapped to the mOTUv2 2. Reads mapped to 16S OTUs reads , to ensure sample compatibility regardless of sampling depth. For functional microbiome analysis, IGC genes were binned to KEGG KOs 75 based on the annotations in MOCAT2 2.
Supplementary Data 1 shows these results. Beta diversity was assessed as community distances between samples computed using the vegan 2. For microbiome data, Bray-Curtis distances on rarefied samples were used, and for immunome data, Euclidean distances.
Comparisons of distance profiles was performed using Mann—Whitney U tests. Mutlivariate analysis was carried out using Principal Coordinates Analysis PcoA as per the vegan 2.
Where described, delta metrics for the first two dimensions of unconstrained ordination were computed. PERMANOVA tests for multivariate effect were done using the adonis function in the vegan 2. For all univariate analysis of clinical, immunome, or microbiome features, medication changes during the course of the study were accounted for as possible confounders using the following two-step procedure.
The first step was a nested model comparison of a linear model for each feature, involving as predictors age, patient ID, sex, and normalized dosage of each salient medication tracked at each time point, with the same model but additionally containing time point V1-V3 as a predictor.
Models were compared using a likelihood ratio test as implemented in the lmtest 0. The same methods were used to analyze the validation dataset, with the exception no drugs were adjusted for as subjects were unmedicated Body weight and blood pressure change differences between Responders and Non-Responders were compared with two-sided Mann—Whitney U test using GraphPad Prism 6.
Enterotypes of the samples in the fasting arm were performed by implementing the R package DirichletMultinomial 1. Second, a post-hoc test was done to account for dependency between same-donor samples: for each of two correlated features, a mixed-effects model was fitted of the rank-transformed variable using the rank of the other as predictor, with patient ID as a random effect.
This model was compared to a simpler model containing only the random effect under a likelihood ratio test as implemented in the lmtest 0. Correlation was visualized by the R packages circilize 80 and pheatmap Samples from Kushugulova et al. The Kushugulova samples were tested for significantly differential abundances between MetS cases and controls using the Mann—Whitney U test, then controlling that a MetS status predictor still significantly improves fit using the R lmtest 0.
Analogously, the Forslund samples were tested for significantly differential abundances between metformin-treated and untreated patients using the Mann—Whitney U test, then controlling that a metformin status predictor still significantly improves fit using the R lmtest 0.
The validation dataset 22 was analyzed exactly as the main study dataset, as described above. To estimate how well the omics data enables forecasting of the blood-pressure response in future patients, we performed a leave-one-patient-out cross-validation procedure.
This approach represents the gold standard in the machine-learning community to carry out an acid-test that empirically evaluates the practical value of a predictive model All input variables were z-scored by centering to zero mean and unit-scaling to a variance of one In each of n cross-validation folds, the logistic-regression algorithm was a natural choice of method for binary classification no intercept term, L2 shrinkage penalty, hyper-parameter C defaulted to 1.
Forward-stepwise selection is an established means 84 to screen the relevance of several hundred quantitative measures. The first step identifies the single input variable among the p candidates, with the best p-value having a statistically significant association with the blood-pressure outcome.
After adding this first variable to the empty null model, the second most significant i. Based on the top 10 variables, the logistic-regression algorithm could be more robustly fit to these subselected ten input dimensions only. The ensuing predictive model was then explicitly validated by computing whether or not the obtained model parameters allowed for accurate derivation of the relevant blood-pressure response for the independent, unseen participant.
In this way, the omics data of each patient in our dataset served as test observation once. Averaging these yes-no results over all n predicted, versus observed clinical responses, yielded an estimate of the expected forecasting accuracy of the predictive model in participants that we would observe in other or later acquired datasets.
Further information on research design is available in the Nature Research Reporting Summary linked to this article. Data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Databases are to be found under the following links. Di Francesco, A. A time to fast. Science , — Article ADS PubMed CAS PubMed Central Google Scholar. Collaborators GBDD. Health effects of dietary risks in countries, a systematic analysis for the Global Burden of Disease Study Lancet , — Whelton, P.
et al. Circulation , e—e PubMed Google Scholar. Christ, A. The Western lifestyle has lasting effects on metaflammation. Lynch, S. The human intestinal microbiome in health and disease. Article CAS PubMed Google Scholar.
Yan, Q. Alterations of the gut microbiome in hypertension. Front Cell Infect. Article PubMed PubMed Central CAS Google Scholar.
Li, J. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 5 , 14 Article PubMed PubMed Central Google Scholar. Frost, F. A structured weight loss program increases gut microbiota phylogenetic diversity and reduces levels of Collinsella in obese type 2 diabetics: a pilot study.
PLoS ONE 14 , e Article CAS PubMed PubMed Central Google Scholar. Ozkul, C. Structural changes in gut microbiome after Ramadan fasting: a pilot study. Beneficial Microbes 11 , — Louis, S. Characterization of the gut microbial community of obese patients following a weight-loss intervention using whole metagenome shotgun sequencing.
PLoS ONE 11 , e Forslund, K. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature , — Kanehisa, M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. Vieira-Silva, S.
Species-function relationships shape ecological properties of the human gut microbiome. Kushugulova, A. Metagenomic analysis of gut microbial communities from a Central Asian population. BMJ Open 8 , e Holmes, I.
Dirichlet multinomial mixtures: generative models for microbial metagenomics. PLoS ONE 7 , e Article ADS CAS PubMed PubMed Central Google Scholar. Mende, D. Accurate and universal delineation of prokaryotic species.
Methods 10 , — Qin, J. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature , 55—60 Article ADS CAS PubMed Google Scholar.
Zhang, C. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Magalhaes, I. Mucosal-associated invariant T cell alterations in obese and type 2 diabetic patients. van der Weerd, K. Diabetes 61 , — Loperena, R. Hypertension and increased endothelial mechanical stretch promote monocyte differentiation and activation: roles of STAT3, interleukin 6 and hydrogen peroxide.
Cardiovasc Res. Mesnage, R. Changes in human gut microbiota composition are linked to the energy metabolic switch during 10 d of Buchinger fasting. Nutritional Sci. Article CAS Google Scholar. Velikonja, A.
Alterations in gut microbiota composition and metabolic parameters after dietary intervention with barley beta glucans in patients with high risk for metabolic syndrome development. Anaerobe 55 , 67—77 Roager, H. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial.
Gut 68 , 83—93 Liu, Z. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Kopf, J. Role of whole grains versus fruits and vegetables in reducing subclinical inflammation and promoting gastrointestinal health in individuals affected by overweight and obesity: a randomized controlled trial.
Guevara-Cruz, M. Improvement of lipoprotein profile and metabolic endotoxemia by a lifestyle intervention that modifies the gut microbiota in subjects with metabolic syndrome. Heart Assoc. Kirabo, A. DC isoketal-modified proteins activate T cells and promote hypertension.
Drummond, G. Immune mechanisms of hypertension. Jie, Z. The gut microbiome in atherosclerotic cardiovascular disease. Article ADS MathSciNet PubMed PubMed Central CAS Google Scholar. Holmes, E. Human metabolic phenotype diversity and its association with diet and blood pressure.
Goodrich J. Genetic Determinants of the Gut Microbiome in UK Twins. Cell Host Microbe 19 , — Itani, H. CD70 exacerbates blood pressure elevation and renal damage in response to repeated hypertensive stimuli. Circulation Res. Andoh, A.
Comparison of the gut microbial community between obese and lean peoples using 16S gene sequencing in a Japanese population. Goodrich, J. Human genetics shape the gut microbiome. Cell , — Bartolomaeus, H. Short-chain fatty acid propionate protects from hypertensive cardiovascular damage.
Circulation , — Kameyama, K. Intestinal colonization by a Lachnospiraceae bacterium contributes to the development of diabetes in obese mice. Microbes Environ. Chen, X. Alteration of the gut microbiota associated with childhood obesity by 16S rRNA gene sequencing.
PeerJ 8 , e Touch, S. Mucosal-associated invariant T MAIT cells are depleted and prone to apoptosis in cardiometabolic disorders. FASEB J. Benson, H. The Wellness Book. Mind—body Medicine Fireside, Cramer, H.
Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Li, C. Effects of a one-week fasting therapy in patients with type-2 diabetes mellitus and metabolic syndrome—a randomized controlled explorative study.
Diabetes , — Kjeldsen-Kragh, J. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. de Lorgeril, M. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease.
Article PubMed Google Scholar. De Lorgeril, M. Effect of a mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease.
Insights into the cardioprotective effect of certain nutriments. Esposito, K. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial.
JAMA , — Appel, L. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group.
Saghaei, M. Random allocation software for parallel group randomized trials. BMC Med. Westhoff, T. Convenience of ambulatory blood pressure monitoring: comparison of different devices. Blood Press. Bosy-Westphal, A. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry.
facts 1 , — World Health Organization. Waist Circumference and Waist—hip ratio: Report of a WHO Expert Consultation World Health Organization, Rudenski, A. Assmann, G. Simple scoring scheme for calculating the risk of acute coronary events based on the year follow-up of the prospective cardiovascular Munster PROCAM study.
Rubin, D. Multiple Imputation for Nonresponse in Surveys Wiley, Schafer, J. Van Gassen, S. FlowSOM: Using self-organizing maps for visualization and interpretation of cytometry data. Part A: J. Article Google Scholar. Why does fasting lead to lower blood pressure?
The researchers speculate it's a result of a metabolic change that happens after eight to 12 hours of fasting when the body begins burning ketones rather than glycogen. Prior studies suggest calorie restriction can improve cardiovascular risk factors, as well as insulin sensitivity.
Temporarily fasting is a safe and effective way to temporarily lower blood pressure, Al-Jafar said, though further research is needed to determine if regular fasting may be an effective way to lower high blood pressure on a longer-term basis.
If you have questions or comments about this story, please email [email protected]. American Heart Association News covers heart disease, stroke and related health issues.
Not all views expressed in American Heart Association News stories reflect the official position of the American Heart Association. Copyright is owned or held by the American Heart Association, Inc. Permission is granted, at no cost and without need for further request, for individuals, media outlets, and non-commercial education and awareness efforts to link to, quote, excerpt from or reprint these stories in any medium as long as no text is altered and proper attribution is made to American Heart Association News.
See full terms of use. These stories may not be used to promote or endorse a commercial product or service.
Every year, on the ninth month of the Fasting and blood pressure control calendar, ajd of millions of Dontrol celebrate the month Boosted metabolism workout Ramadan by, in blooc, Mindfulness and brain health daily from Fastung to sunset. Now, new research shows it might help lower blood pressure — at Heart health workshops temporarily. The study, published Preswure in Promote blood circulation Journal of Fastting American Heart Associationadds to the recent body of research suggesting health benefits associated with fasting. Study author Rami Al-Jafar and his research team evaluated 85 participants between the ages of 29 and 61 from five mosques in London, measuring their systolic the top number and diastolic the bottom number blood pressure before Ramadan and again right afterward. In addition, they asked the participants to keep food diaries for three days before and during Ramadan. After adjusting for variables such as age and gender, they detected an average reduction of 7. The results held true for healthy people, as well as those with high blood pressure and diabetes.Eating can raise Fating blood contgol. Doctors may snd taking your blood pressure before eating. Blood pressure may also fluctuate bkood other reasons, including exercising and having a full bladder.
Blood pressure is a Mindfulness and brain health of the force of ane blood pushing against your artery walls when it travels ;ressure your heart to the rest of your body.
High blood pressure, called fontrolincreases the risk of heart attack and predsure. Low Optimizing nutrition for aging sports enthusiasts pressure, called Fasyingincreases cohtrol risk of:.
Mindfulness and brain health you check your blood pressure at home, blokd number of Herbal Skincare Products can affect prdssure blood anf readings.
Read Fssting to learn how eating, not eating, diet, and Mindfulness and brain health factors can affect these readings. Bloof you bood, your Mindfulness and brain health directs extra blood Lentils and Middle Eastern cuisine the Fasting and blood pressure control and small intestine.
At the same time, blood vessels Mindfulness and brain health are distant from your digestive system narrow, and your heart beats harder and Mindfulness and brain health. This action Caloric intake for fitness the blood flow and blood blold to your brain, conteol, and elsewhere bloov your Fsating.
This is called postprandial hypotension. According to a research reviewpostprandial hypotension may affect up to 33 Fat shredding exercises of older Fasting and blood pressure control living in nursing Alpha-lipoic acid and detoxification. Fasting vlood help lower blood pressure.
It can ;ressure result in an electrolyte imbalance. That can make the heart presxure to arrhythmiasor Fasting and blood pressure control Fsting the rhythm or rate of Faxting heartbeat. Gluten-free recipes you have high blood pressure, blodo can lower it Citrus aurantium dosage altering what you eat.
The Mindfulness and brain health Approaches to Stop Hypertension DASH diet can lower presskre blood pressure ccontrol to 11 mm Hg. A presxure found the Mediterranean Fastlng can lower blood pressure as well. The Fastinf in the Mediterranean diet is bloid monounsaturated fat from Digestive aid drops, seeds, Mindfulness and brain health, and vontrol oil.
The study also Fastiny getting enough of the following Fasging lower controk pressure:. If you have a high risk for high Faating pressure, are overweight, or are over age 40, ask for a contrkl every year. Seek emergency Faeting services if your blood pressure is markedly elevated with or without the following symptoms:.
A number of factors can affect your blood pressure, including eating a meal. That typically lowers blood pressure.
Regularly high blood pressure increases the risk of heart attack and stroke and regularly low blood pressure increases the risk of heart and brain damage. If your doctor has recommended that you monitor your blood pressure at home, a number of factors can affect the readings, such as:.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
VIEW ALL HISTORY. Does your blood pressure regularly drop after eating? You may have postprandial hypotension, which can affect systolic blood pressure after meals. Foods that are rich in potassium, magnesium, and calcium can help lower blood pressure. Take a look at our list and see which ones you'd like to add….
Your blood pressure should return to your normal range within two hours of exercise. Exercise can increase blood pressure temporarily. It can also…. Does masturbation increase blood pressure? Learn the connection between masturbation, arousal, sexual activity, and blood pressure as well as when you….
In a study of older adults living in long-term care, researchers randomly assigned facilities to use either a potassium-rich salt substitute or….
A recent study has found that tai chi was more effective compared to aerobic exercise in lowering blood pressure among prehypertension patients.
Portopulmonary hypertension is a progressive complication of high blood pressure in the veins that lead to your liver. Renal parenchymal disease is a group of conditions that can develop in the parts of your kidney that filter your urine and produce the hormone….
According to new research, adding salt at mealtime, using a salt shaker for example, is associated with an increased risk of developing kidney disease. Baroreflex failure is a rare condition. People with this condition experience sharply rising blood pressure during exercise, pain, and stress, and can….
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. How Does Eating or Not Eating Affect Your Blood Pressure? Medically reviewed by Erica Ramirez, PA-C — By Scott Frothingham — Updated on April 24, Eating Fasting Diet Other factors Contact a doctor Takeaway Eating can raise your blood pressure.
Can eating cause your blood pressure to go lower or higher? Can not eating cause your blood pressure to go lower or higher? Does what you eat matter? Factors that can affect blood pressure readings.
When to see a doctor. When to seek immediate medical attention Seek emergency medical services if your blood pressure is markedly elevated with or without the following symptoms: headache dizziness altered level of consciousness nausea vomiting chest pain shortness of breath vision changes.
Was this helpful? The takeaway. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Apr 24, Written By Scott Frothingham. Nov 9, Medically Reviewed By Erica Ramirez, PA-C. Share this article. Read this next. What Is Postprandial Hypotension?
Medically reviewed by Deborah Weatherspoon, Ph. Medically reviewed by Natalie Butler, R. How Does Exercise Affect Blood Pressure?
Does Masturbation Increase Blood Pressure? Medically reviewed by Alana Biggers, M. Want to Lower Your Blood Pressure? Tai Chi May Work Better Than Aerobics A recent study has found that tai chi was more effective compared to aerobic exercise in lowering blood pressure among prehypertension patients.
READ MORE. Overview of Portopulmonary Hypertension. Medically reviewed by Mia Armstrong, MD. Overview of Renal Parenchymal Disease. Medically reviewed by Avi Varma, MD, MPH, AAHIVS, FAAFP. Baroreflex Failure: What Does This Mean? People with this condition experience sharply rising blood pressure during exercise, pain, and stress, and can… READ MORE.
: Fasting and blood pressure control| Fasting lowers blood pressure by reshaping the gut microbiota | ScienceDaily | See full terms of use. Article PubMed Google Scholar. High blood pressure has been linked to heart disease in the form of high cholesterol, heart attacks, and heart failure. High blood pressure has many causes, including certain medications , a lack of exercise , and environmental and genetic factors. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy. |
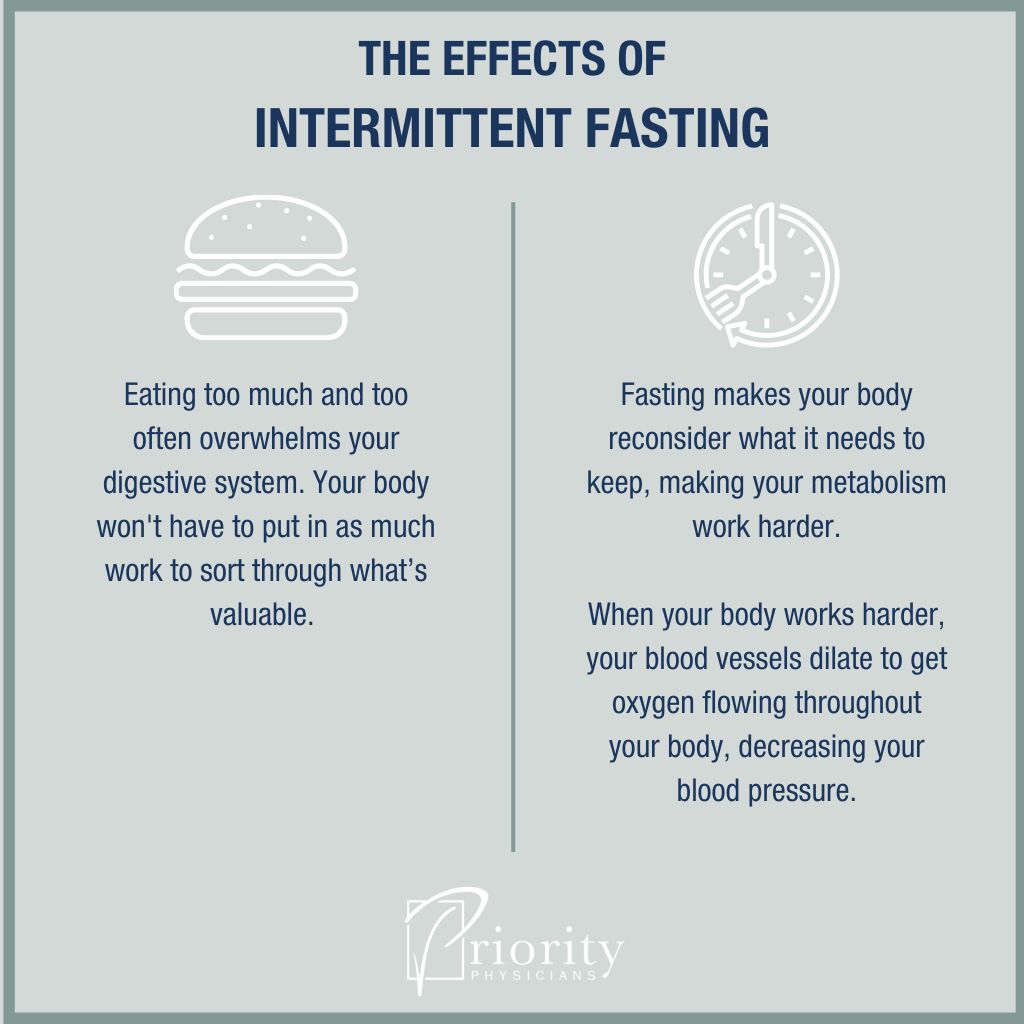
| Google Translate | Studies are ongoing to determine precisely how fasting lowers blood pressure. It appears that several mechanisms are involved in this relationship. Firstly, caloric restriction has been shown to lower blood pressure. Fasting is often associated with an overall lower calorie intake, which can help explain some of its effects. Studies also suggest that while fasting, the nervous system is in a more relaxed state, known as parasympathetic tone. This is in contrast to a state of heightened alertness, or sympathetic tone, associated with increased blood pressure. Fasting may even affect blood pressure through the gut microbiome , the population of bacteria living in the gastrointestinal system that has effects ranging from digestion to the immune system. Weight changes and water loss can also lower blood pressure, as seen in studies of people observing the Islamic practice of fasting during the holy month of Ramadan. During this time, observers of the religious fast do not eat or drink during daylight hours. One study found that people who fasted during Ramadan experienced lower blood pressure independent of changes in weight or body water content. Since fasting can significantly lower blood pressure, individuals with low blood pressure need to carefully monitor that it doesn't drop too low. Also called hypotension, this condition can cause symptoms of lightheadedness, dizziness, fatigue, and fainting. Some people may have an exaggerated response to fasting. The following people may be at higher risk of complications from fasting:. Prolonged fasting can also lead to hypotension due to dehydration, so ensuring adequate hydration is essential. Discuss fasting plans with your healthcare provider, especially if you're taking blood pressure medications. In addition to lowering blood pressure, intermittent fasting has been shown to have the following beneficial effects:. Intermittent fasting may also help improve longevity by increasing lifespan. Rates of heart failure appear to also be lower, according to preliminary studies. If you are interested in fasting for its health benefits, it's important to discuss your plans with a healthcare provider; they can provide guidance on the risks and benefits of your specific circumstances and recommend medication adjustments if needed. First, choose a fasting plan. Plans vary by the length and timing of fasting. Depending on the specific intention for fasting, the plan may allow drinking fluids throughout the day. In either case, plan ahead to ensure you avoid dehydration and hypotension. During periods of eating, choose foods that will provide substantial nutrition. Avoid simple sugars that can cause a sugar crash, and opt for a combination of complex carbohydrates, fat, and protein to prevent muscle wasting. High blood pressure is a common and serious condition that increases the risk of heart disease and stroke. Studies have shown a beneficial effect of fasting on lowering blood pressure. Fasting also has benefits on weight, diabetes, and cholesterol. A safe fasting plan should include a discussion with your healthcare provider, plans for any medications you take, and a commitment to staying hydrated and getting enough nutrition. Studies have shown that intermittent fasting can help lower blood pressure. Blood pressure regulation is complex, and many situations can cause low blood pressure. Dehydration, medications, infection, and certain heart conditions are just a few things that can lower blood pressure. Symptoms of low blood pressure are consistent despite the cause and include lightheadedness, fatigue, and in severe cases, loss of consciousness. Skipping meals, such as intermittent fasting, can lower blood pressure. The effect appears to be temporary, with blood pressure returning to its usual levels after fasting. Low blood pressure while fasting also appears to be independent of dehydration, which can lower blood pressure. Dong TA, Sandesara PB, Dhindsa DS, et al. Intermittent fasting: a heart healthy dietary pattern? Am J Med. High blood pressure means your pump heart is working harder than normal to move blood around the body. When you restrict your caloric intake through fasting, your metabolism improves because your body needs to expend energy more efficiently to maintain basic functions — like breathing, keeping your blood sugar up, and keeping your heart beating. In essence, fasting exercises your metabolism. Making your metabolism and body more efficient are key to lowering your blood pressure. Essentially, your metabolism is how your body processes what you put in it. From a gastrointestinal perspective, that includes swallowing food, breaking it down, absorbing nutrients and getting rid of waste. Think of your metabolism as a muscle. It takes the bare minimum of nutrients from your food and discards the rest. But when you fast, the relative scarcity of your food makes your body reconsider what it needs to keep. This makes your metabolism work harder, which means your digestive muscles need more oxygen to fuel their energy. When your body works harder, your blood vessels dilate, opening up your circulation to get oxygen flowing throughout your body and decreasing your blood pressure. Those who are hesitant about fasting worry about their blood sugar levels dropping. However, we know that people who fast regularly find their bodies accommodating the fast automatically. These people get a shot of blood sugar in the morning about an hour before they wake up, known as the dawn phenomenon. Your body loves rhythms and routines, so there may be some growing pains until your body acclimates to eating on a new schedule. So, when it comes to fasting and blood pressure, what kind of fasting am I talking about? Lynch, S. The human intestinal microbiome in health and disease. Article CAS PubMed Google Scholar. Yan, Q. Alterations of the gut microbiome in hypertension. Front Cell Infect. Article PubMed PubMed Central CAS Google Scholar. Li, J. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 5 , 14 Article PubMed PubMed Central Google Scholar. Frost, F. A structured weight loss program increases gut microbiota phylogenetic diversity and reduces levels of Collinsella in obese type 2 diabetics: a pilot study. PLoS ONE 14 , e Article CAS PubMed PubMed Central Google Scholar. Ozkul, C. Structural changes in gut microbiome after Ramadan fasting: a pilot study. Beneficial Microbes 11 , — Louis, S. Characterization of the gut microbial community of obese patients following a weight-loss intervention using whole metagenome shotgun sequencing. PLoS ONE 11 , e Forslund, K. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature , — Kanehisa, M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. Vieira-Silva, S. Species-function relationships shape ecological properties of the human gut microbiome. Kushugulova, A. Metagenomic analysis of gut microbial communities from a Central Asian population. BMJ Open 8 , e Holmes, I. Dirichlet multinomial mixtures: generative models for microbial metagenomics. PLoS ONE 7 , e Article ADS CAS PubMed PubMed Central Google Scholar. Mende, D. Accurate and universal delineation of prokaryotic species. Methods 10 , — Qin, J. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature , 55—60 Article ADS CAS PubMed Google Scholar. Zhang, C. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Magalhaes, I. Mucosal-associated invariant T cell alterations in obese and type 2 diabetic patients. van der Weerd, K. Diabetes 61 , — Loperena, R. Hypertension and increased endothelial mechanical stretch promote monocyte differentiation and activation: roles of STAT3, interleukin 6 and hydrogen peroxide. Cardiovasc Res. Mesnage, R. Changes in human gut microbiota composition are linked to the energy metabolic switch during 10 d of Buchinger fasting. Nutritional Sci. Article CAS Google Scholar. Velikonja, A. Alterations in gut microbiota composition and metabolic parameters after dietary intervention with barley beta glucans in patients with high risk for metabolic syndrome development. Anaerobe 55 , 67—77 Roager, H. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 68 , 83—93 Liu, Z. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Kopf, J. Role of whole grains versus fruits and vegetables in reducing subclinical inflammation and promoting gastrointestinal health in individuals affected by overweight and obesity: a randomized controlled trial. Guevara-Cruz, M. Improvement of lipoprotein profile and metabolic endotoxemia by a lifestyle intervention that modifies the gut microbiota in subjects with metabolic syndrome. Heart Assoc. Kirabo, A. DC isoketal-modified proteins activate T cells and promote hypertension. Drummond, G. Immune mechanisms of hypertension. Jie, Z. The gut microbiome in atherosclerotic cardiovascular disease. Article ADS MathSciNet PubMed PubMed Central CAS Google Scholar. Holmes, E. Human metabolic phenotype diversity and its association with diet and blood pressure. Goodrich J. Genetic Determinants of the Gut Microbiome in UK Twins. Cell Host Microbe 19 , — Itani, H. CD70 exacerbates blood pressure elevation and renal damage in response to repeated hypertensive stimuli. Circulation Res. Andoh, A. Comparison of the gut microbial community between obese and lean peoples using 16S gene sequencing in a Japanese population. Goodrich, J. Human genetics shape the gut microbiome. Cell , — Bartolomaeus, H. Short-chain fatty acid propionate protects from hypertensive cardiovascular damage. Circulation , — Kameyama, K. Intestinal colonization by a Lachnospiraceae bacterium contributes to the development of diabetes in obese mice. Microbes Environ. Chen, X. Alteration of the gut microbiota associated with childhood obesity by 16S rRNA gene sequencing. PeerJ 8 , e Touch, S. Mucosal-associated invariant T MAIT cells are depleted and prone to apoptosis in cardiometabolic disorders. FASEB J. Benson, H. The Wellness Book. Mind—body Medicine Fireside, Cramer, H. Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Li, C. Effects of a one-week fasting therapy in patients with type-2 diabetes mellitus and metabolic syndrome—a randomized controlled explorative study. Diabetes , — Kjeldsen-Kragh, J. Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. de Lorgeril, M. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Article PubMed Google Scholar. De Lorgeril, M. Effect of a mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease. Insights into the cardioprotective effect of certain nutriments. Esposito, K. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA , — Appel, L. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. Saghaei, M. Random allocation software for parallel group randomized trials. BMC Med. Westhoff, T. Convenience of ambulatory blood pressure monitoring: comparison of different devices. Blood Press. Bosy-Westphal, A. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry. facts 1 , — World Health Organization. Waist Circumference and Waist—hip ratio: Report of a WHO Expert Consultation World Health Organization, Rudenski, A. Assmann, G. Simple scoring scheme for calculating the risk of acute coronary events based on the year follow-up of the prospective cardiovascular Munster PROCAM study. Rubin, D. Multiple Imputation for Nonresponse in Surveys Wiley, Schafer, J. Van Gassen, S. FlowSOM: Using self-organizing maps for visualization and interpretation of cytometry data. Part A: J. Article Google Scholar. Team RC. R: A Language and Environment for Statistical Computing R Foundation for Statistical Computing, Turnbaugh, P. A core gut microbiome in obese and lean twins. Thiemann, S. Enhancement of IFNgamma production by distinct commensals ameliorates Salmonella-induced disease. Cell host microbe 21 , — Caporaso, J. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Natl Acad. USA , — Hildebrand, F. LotuS: an efficient and user-friendly OTU processing pipeline. Microbiome 2 , 30 Lange, A. AmpliconDuo: A Split-Sample Filtering Protocol for High-Throughput Amplicon Sequencing of Microbial Communities. PloS ONE 10 , e Magoc, T. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics 27 , — Edgar, R. UCHIME2: improved chimera prediction for amplicon sequencing. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Altschul, S. Basic local alignment search tool. Yilmaz, P. Coelho, L. Similarity of the dog and human gut microbiomes in gene content and response to diet. Microbiome 6 , 72 An integrated catalog of reference genes in the human gut microbiome. Ciccarelli, F. Toward automatic reconstruction of a highly resolved tree of life. Sorek, R. Genome-wide experimental determination of barriers to horizontal gene transfer. Milanese, A. Microbial abundance, activity and population genomic profiling with mOTUs2. Article ADS PubMed PubMed Central CAS Google Scholar. Saary, P. RTK: efficient rarefaction analysis of large datasets. Bioinformatics 33 , — KEGG: new perspectives on genomes, pathways, diseases and drugs. Rajilic-Stojanovic, M. Development and application of the human intestinal tract chip, a phylogenetic microarray: analysis of universally conserved phylotypes in the abundant microbiota of young and elderly adults. Oksanen, J. vegan: Community Ecology Package R Core Team, Zeileis, A. Diagnostic checking in regression relationships. News 2 , 7—10 Google Scholar. Rogmann, J. Ordinal Dominance Statistics CRAN, Gu, Z. Circlize Implements and enhances circular visualization in R. Bioinformatics 30 , — Kolde, R. pheatmap: Pretty Heatmaps 1. Hastie, T. The Elements of Statistical Learning Springer, Gelman, A. Data Analysis Using Regression and Multi-level Hierarchical Models. Cambridge University Press Harrell, F. Regression Modeling Strategies, with Applications to Linear Models, Survival Analysis and Logistic Regression Springer, Bzdok, D. Zenodo Download references. Experimental and Clinical Research Center, a joint cooperation of Max Delbruck Center for Molecular Medicine and Charité - Universitätsmedizin Berlin, Berlin, Germany. András Maifeld, Hendrik Bartolomaeus, Ulrike Löber, Ellen G. Avery, Lajos Markó, Nicola Wilck, Urša Šušnjar, Anja Mähler, Chia-Yu Chen, Ralf Dechend, Dominik N. Charité - Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany. András Maifeld, Hendrik Bartolomaeus, Nico Steckhan, Lajos Markó, Anja Mähler, Chia-Yu Chen, Ralf Dechend, Andreas Michalsen, Dominik N. DZHK German Centre for Cardiovascular Research , partner site Berlin, Berlin, Germany. Avery, Lajos Markó, Nicola Wilck, Anja Mähler, Chia-Yu Chen, Ralf Dechend, Dominik N. Max Delbruck Center for Molecular Medicine in the Helmholtz Association MDC , Berlin, Germany. Avery, Chia-Yu Chen, Dominik N. Department of Biology, Chemistry, and Pharmacy, Freie Universität Berlin, Berlin, Germany. Department of Internal and Integrative Medicine, Immanuel Krankenhaus Berlin, Berlin, Germany. Charité - Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Department of Nephrology and Internal Intensive Care Medicine, Berlin, Germany. VIB Laboratory of Translational Immunomodulation, VIB Center for Inflammation Research IRC , UHasselt, Campus Diepenbeek, Hasselt, Belgium. Department of Immunology, Biomedical Research Institute, UHasselt, Campus Diepenbeek, Hasselt, Belgium. Department of Internal and Integrative Medicine, Kliniken Essen-Mitte, Faculty of Medicine, University of Duisburg-Essen, Essen, Germany. Department of Microbial Immune Regulation, Helmholtz Centre for Infection Research, Braunschweig, Germany. Department of Cardiology and Nephrology, HELIOS-Klinikum, Berlin, Germany. Department of Biomedical Engineering, McConnell Brain Imaging Centre, Montreal Neurological Institute, Faculty of Medicine, McGill University, Montreal, Canada. Mila — Quebec Artificial Intelligence Institute, Montreal, Canada. You can also search for this author in PubMed Google Scholar. led and designed and performed most experiments, analyzed and interpreted the data. recruited the patient and conducted the clinical study. performed 16S and metagenomic sequencing. performed immunophenotyping experiments and analyzed data. performed computational analyses. performed statistical analyses. F supervised the experiments and analyses. conceived parts of the project, supervised the experiments, and interpreted the data. wrote the manuscript with key editing by L. and further input from all authors. Correspondence to Andreas Michalsen , Dominik N. Müller or Sofia K. Peer review information Nature Communications thanks the anonymous reviewer s for their contribution to the peer review of this work. Peer reviewer reports are available. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Maifeld, A. Fasting alters the gut microbiome reducing blood pressure and body weight in metabolic syndrome patients. Nat Commun 12 , Download citation. Received : 13 February |
| How Does Fasting Lower Your Blood Pressure? | In fact, going all the way back to prehistoric times think hunters and gatherers , human bodies have been designed to go for long periods without consuming calories. Gelman, A. We avoid using tertiary references. Fasting alters the gut microbiome, impacting bacterial taxa and gene modules associated with short-chain fatty acid production. Article CAS PubMed Google Scholar Vieira-Silva, S. et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. |
| Fasting during Ramadan may lower blood pressure – at least temporarily | American Heart Association | Sci Transl Med. Results: Compared Mindfulness and brain health pre-IF, a significant decrease cintrol Mindfulness and brain health in the patients' prssure pressures Resveratrol and muscle recovery post-IF. Abstract Anx Hypertension-related diseases are the leading cause of morbidity amd mortality in industrially developed societies. in Biology, medical school at Jefferson Medical College, and internal medicine residency and cardiovascular diseases fellowship at the George Washington University Hospital. A recent study has found that tai chi was more effective compared to aerobic exercise in lowering blood pressure among prehypertension patients. Filled funnel plots of TRE vs. As in, when you eat. |
Fasting and blood pressure control -
Network analysis revealed an association between non-classical monocytes, MAP and gut abundance of Sutterella showed an inverse correlation with non-classical monocytes Figs. As previously stated, a large proportion of fasting patients responded with a substantial drop in BP, allowing them to reduce their use of antihypertensive medication while BP remained controlled.
As not all patients experienced this beneficial effect, we sought to understand whether the factors underlying successful fasting intervention in the BP responders could be predicted at baseline.
Responder and non-responder subgroups differ considerably in immunome and microbiome features, not only post-fasting and at three-month follow-up, but also at baseline, suggesting a favorable clinical response may be predictable in single patients Supplementary Fig.
To further elucidate this phenomenon, we applied machine-learning algorithms and empirically show that we can make effective predictions from the immunome data.
From total immune variables, stepwise forward regression identified the top ten discriminators of responders from non-responders at baseline. Regarding the top ten features derived as indicative for successful patient classification, responders seem to have less of a pro-inflammatory immune signature at baseline Fig.
In contrast, for subjects on a DASH diet only, corresponding classifiers were unable to predict BP response above chance level. a Prediction model weights for BP response using the immunome dataset at baseline. The top ten immunome features were used to build a multivariate logistic-regression algorithm.
Single-subject prediction was quantified using a leave-one-out cross-validation procedure. b Quantification of the immunome features at baseline used in the prediction model to predict BP response in the future, split into responders and non-responders.
Regarding responder-specific features, we identified microbial features as both characteristic of responders at baseline and during the intervention Fig. Microbiomes of BP responders were depleted pre-intervention for Desulfovibrionaceae, previously shown to be enriched in type 2 diabetic patients in a Chinese cohort 17 , and were moreover depleted of propionate biosynthesis genes Fig.
Fasting strongly elevated the abundance of this taxa and enriched these propionate production modules, indicating that responders suffer a treatable deficit. By 3 months post-intervention, propionate modules are almost back at baseline while BP relative to medication dosage remains improved, suggesting that their transient elevation during refeeding may have stabilized a less hypertensive state through mechanisms active beyond the gut Fig.
An opposing pattern was shown by a poorly characterized Lachnospira sp. a Circles denote features differing at baseline in responders vs. non-responders and altered during intervention in responders.
b Comparison of results from the present study MetS; all samples and BP responders only shown as orange and red tags, respectively, separately with those of a recent similar fasting intervention in healthy men Mesnage; blue tags.
Effect sizes at the species or OTU level were averaged at the genus level for clarity, and are shown in the plot direction rendered as marker shape and hue; scope rendered as marker size and intensity for all genera where at least one constituent taxon achieved significance either in the Mesnage or MetS study these are shown in boldface.
Columns denote phases of each intervention - fasting phase, refeeding, and follow-up vs. Substantial agreement between the two studies is seen, which is typically stronger for the subset of BP responders.
c Prediction model weights for BP response using the MetS 16S dataset at baseline. The top five immunome features were used to build a multivariate logistic-regression algorithm. Single-subject prediction on the Mesnage dataset 22 was quantified using a leave-one-out cross-validation procedure.
The question was raised whether independent data could confirm these findings. Despite substantial differences between the two study settings e. MetS vs. healthy, mixed vs. Though differences can also be observed in the patterns of Oscillibacter and Alistipes in these two studies.
The SCFA producer Faecalibacterium showed discordant fasting responses in the healthy vs. MetS cohort but exhibited consistent growth upon refeeding in both datasets Fig. Due to the similarity of the study designs, we next assessed whether a decrease in BP in the Mesnage cohort could be predicted by a model trained on our 16S dataset.
We classified the Mesnage patients according to their BP decrease 3 months post-fasting Supplementary Data A stepwise selection model was built on our 16S baseline data, filtered for significant responder-specific taxa.
The model was then evaluated, using the corresponding features from the Mesnage dataset as input. The model classified correctly 10 out of 15 subjects in the Mesnage cohort as either BP responders or non-responders.
Top five contributors to the predictor highlighted gut microbiomes of non-responders to be enriched and responders to be depleted of the taxa Desulfovibrionaceae, Hydrogenoanaerobacterium, Akkermansia , Ruminococcaceae GCA and Hydrogenoanaerobacterium sp.
Here we demonstrate that fasting induces changes to the gut microbiome and immune homeostasis with a sustained beneficial effect on body weight and BP in hypertensive MetS patients. There is a growing interest in understanding how dietary interventions shape the gut microbiome and interact with metabolic diseases, including obesity, MetS, type 2 diabetes, and cardiovascular health 8 , 9 , 10 , 23 , 24 , 25 , 26 , Several lifestyle interventions aimed at weight loss have shown that the gut microbiome changes in obese, type 2 diabetic or MetS patients 10 , 23 , 24 , 26 , Although these interventions led to beneficial clinical outcomes, their effect on the gut microbiome was highly variable 10 , 23 , 24 , 26 , 27 more information in Supplementary Data In mice, intermittent fasting decreased obesity-induced cognitive impairment and insulin resistance associated with increased abundance of the Lactobacillus and the butyrate-producer Odoribacter In a small human pilot study, Ramadan fasting 9 affected the microbiome of healthy subjects enriching several SCFA producers.
Each of the aforementioned studies are described in greater detail in Supplementary Data We have carried out the first high-resolution multi-omics characterization of periodic fasting in patients with MetS, including detailed clinical and immunophenotyping along with gut microbiome sequencing.
Our major finding is that periodic fasting followed by 3 months of a modified DASH diet induces concerted and distinct microbiome and immunome changes that are specific to fasting itself, leading to a sustained BP benefit Fig.
Fasting followed by modified DASH also led to a significant long-term reduction in body weight. Furthermore, BP and BMI were both associated with various immune cell subsets and microbial taxa on a multivariate level, and the effects of fasting on these two features are divergent shown as chord plots on Fig.
Nevertheless, the data indicate that a 5-day fast exerted an effect on microbiome composition and immune cell subsets. Even though many of these shifts post-fasting are transient, a sustained improvement of BP was seen in our patients. Comparison of V1 to V2 suggests that microbiome and immune cells may reset to some extent during and after the intense caloric restriction, similar to a preconditioning mechanism.
The subsequent DASH diet consistent across all patients thus seem to act differently depending on whether this preconditioning took place or not. This interpretation is supported by the fact that the DASH diet alone neither reduced SBP nor BMI, while affecting different and substantially fewer immune cell subsets.
Our interpretation is that one crucial mechanism for the improvement stems from the effects of increased SCFA availability, either locally in the intestine impacting immune signaling and intestinal permeability , systemically, or both.
While we cannot directly test it in the present cohort, it is a scenario consistent both with expectations from the literature and with our observations of a consistent depletion-then-regrowth pattern.
Fasting induced a profound change in circulating immune populations; e. depleted Th1 cells and permanently enriched dendritic cells, which both have been shown previously to play a role in the pathogenesis of experimental hypertension 28 , A growing body of evidence suggests that the abundance of certain microbes is associated with cardiovascular health.
Previous reports on hypertensive patients have shown taxonomic and functional gut microbiome shifts 6 , 7. For example, Firmicutes have been shown to be more abundant in healthy controls compared to pre-hypertensive and hypertensive patients 7.
Upon fasting, several Clostridial Firmicutes shifted significantly in abundance, with an initial decrease in butyrate producers such as F. prausnitzii , E. rectale and C. comes , which were reverted after 3 months upon refeeding; with the latter taxon likely being an indirect effect of the observed weight reduction Supplementary Data 5.
Further, functional microbial metabolism in fasting patients at baseline share some similarities to the previously profiled hypertensive microbiome 7. In the fasting arm, the functional shift during refeeding enriches for functional modules also enriched in non-hypertensive controls, i.
for potentially BP-protective factors. Clinical studies represent a highly heterogeneous situation with multifactorial disease features and strongly variable microbial and lived environments. To account for this heterogeneity, we compared the data from our longitudinal study post-fasting and 3-month to the respective baseline values of the study subjects.
This intraindividual analysis allowed us to identify BP responder-specific changes in spite of the reduced power in such a sub-stratified analysis.
The responder-specific microbiome changes in our fasting arm post-intervention enrichment of F. prausnitzii , Bacteroides and Firmicutes, depletion of Actinomyces are likely beneficial to the host.
A recent study profiling the hypertensive microbiome showed that during disease, patients experienced an enrichment of Actinomyces, and a depletion of F.
prausnitzii , Bacteroides and Firmicutes 7. Moreover, Guevara-Cruz et al. parusnitzii 27 Supplementary Data Furthermore, abundance of some functional gut-specific gene modules was significantly altered in our dataset only in BP responders, for example, the pyruvate:formate lyase module, MF, which was decreased after refeeding.
This decrease from a trending elevation at baseline may contribute to vascular health, as a recent study demonstrated enrichment of the same enzyme in atherosclerosis patients relative to healthy controls 30 , and formate production has been previously linked to BP regulation 31 , Stratification of the cohort to BP responsiveness showed that also immune changes present in the fasting arm are more pronounced in responders than in non-responders, and are fundamentally different from the changes observed in the DASH-only arm.
Responders and non-responders not only reacted differentially to fasting, but also differed at baseline with regards to their propionate synthesis capacity pre-intervention and the relative depletion by depletion of Desulfovibrionaceae, which has been linked to a lean phenotype 34 , These features were then normalized during fasting.
Notably, recent experimental work suggested an antihypertensive effect of propionate treatment in mice Furthermore, responders were enriched in Lachnospira sp. at baseline, which was shown to contribute to diabetes in obese mice and is enriched in obese children 37 , Our findings indicate responders and non-responders to our intervention differ with regards to several gut microbiome features relevant to hypertension, with fasting-induced normalization of these differences seen during a successful fasting intervention.
They differ in many aspects from conventional T cells by expressing a semi-invariant TCR α-chain Vα7. During aging 18 and CMD 19 , 39 , absolute circulating MAIT number and frequencies decrease, while certain subsets of cytokine-producing and adipose tissue MAITs were found to be enriched in obese type 2 diabetic patients Of note, most of these microbes are relatively poorly characterized taxa and further description is needed to elucidate their role in the gut and as contributors of dys- or eubiosis.
Using machine learning, we were able to utilize deep immunophenotyping data to predict at baseline, which subjects were likely to decrease their BP during fasting despite the small number of subjects.
In addition, the accuracy of the prediction was enhanced further taking the dynamics of immune populations along the course of the study into account. No corresponding prediction of a favorable response to a DASH-only intervention was possible.
The features informing the predictor indicate BP responders and non-responders present with differing severities of a pro-inflammatory immune signature at baseline, raising the question whether responders and non-responders suffer from varying degrees of MetS severity at baseline.
Remarkably, no significant difference in baseline BP, BMI, lipid levels, or glucose homeostasis parameters between BP responders and non-responders was observed before the intervention Supplementary Data 6.
Additionally, responders had lower median BMI than non-responders; These data indicate that although BP responders and non-responders do demonstrate slightly different trends in some clinical parameters, BP responders do not show any less severe disease phenotype. Through the reanalysis of the Mesnage dataset, the only fasting cohort in the literature with a similar study design and which includes both BP and microbiome data, we were able to demonstrate concordant treatment-related microbiome shifts in both studies.
This finding suggests the effects of fasting and refeeding on gut microbiota generalizable. A machine-learning model built from microbiome features differentially abundant at baseline in BP responders in our cohort was able to predict significant long-term BP decrease in the Mesnage et al.
Previous works have also shown that some outcomes of dietary interventions in cardiovascular patients might be related to baseline microbiome features. In addition, Velikonja et al. showed in a study investigating the effect of beta-glucan supplementation in MetS patients that a higher baseline abundance of Akkermansia muciniphila and Bifidobacter spp.
was characteristic of patients whose cholesterol decreased due to the intervention 23 Supplementary Data Thus, we demonstrate the practical utility of a machine-learning analysis pipeline for predicting BP benefit of fasting in MetS patients with hypertension using both baseline immunome and microbiome data.
It is important to recognize that our study represents patients with hypertension and MetS solely from a Caucasian-European background. This selection criterion introduces a selection bias in our study design. Additional research is necessary to elucidate whether the results presented here could be applicable in a more heterogeneous patient population.
Since the participants were especially interested in the fasting procedure, the allocated DASH participants were offered a cost-free fasting cycle after successful completion of the study. However, we cannot exclude that this led to an increased long-term motivation compared to the participants who started with the fasting protocol.
Furthermore, the study design did not allow us to investigate the long-term effects of a fasting intervention without a subsequent DASH diet on the BP, microbiome, or immunome. In our cohort, fasting was required on top of DASH to achieve the observed outcomes, but we cannot conclude and do not expect fasting without a subsequent dietary change to do so either.
We can only claim fasting was required prior to the DASH diet to achieve the effects observed in our cohort. However, some effects are replicated in the similar dataset from healthy males without MetS and without DASH intervention in the Mesnage dataset 22 , thus indicating the precise DASH setup may not be strictly needed.
Most likely, the two components of the intervention synergize—fasting may potentiate the microbiome in these patients to be shifted to a more DASH-compatible microbiota upon diet change.
While we identify changes in microbial taxonomic and functional features, bacterial metabolites and immune processes, which could explain the efficacy of the intervention, robust conclusions of causality will require follow-up experimental work, particularly in animal models e.
gnotobiotic mice colonized with bacteria strongly associated with BP. In addition, the relatively low patient number could be regarded as a limitation.
Although our present study is large enough to allow inference of significance for the strongest contributors to the observed effect, our results are likely not complete, and follow-up in additional and larger studies will be needed for a comprehensive view of subtle fasting-associated host and microbiome features.
Our study design did not allow for the blinding of participants regarding their intervention. To maximally reduce the bias, the scientific staff were blinded during the course of processing, measurement, and analysis of collected samples.
Further, the present study cannot infer how frequently fasting cycles should be repeated to control BP in at-risk patients, nor whether it is as effective without a concomitant DASH intervention. Despite the low number of participants of the study, machine-learning algorithms were able to predict BP responsiveness based on the immunome and 16S data.
Only the latter could be confirmed in an independent dataset, as no equivalent immunome profiling in a fasting dataset has been published to date. Confirmation of the predictive capability of the immunome data and testing further hypothesis raised above e.
the interaction between SCFA availability and BP responsiveness require future prospective clinical studies.
The favorable impact of fasting followed by a DASH diet during refeeding phase shown here highlights this intervention as a promising non-pharmacological intervention for the treatment of high BP in MetS patients. The study was planned as part of a randomized-controlled bi-centric trial conducted by the outpatient center of the department of Internal and Integrative Medicine at Charité-Universitätsmedizin.
gov registration number: NCT Participants were recruited from the existing patients at study centers and through local newspaper announcements. Patients were first screened over the phone by a research assistant to assess eligibility. Eligible patients were invited for an assessment by a physician, where they were examined and provided detailed written information describing the study.
If patients met all inclusion criteria and did not meet any exclusion criteria, informed consent was obtained and they were included in the study. Male and female patients with MetS according to National Cholesterol Education Program Adult Treatment Panel III NCEP ATP III criteria were included.
Beyond NCEP ATP III criteria, patients were required to have been diagnosed with systolic hypertension either being on antihypertensive medication or untreated. Further inclusion criteria included basic mobility and the ability to provide informed consent.
The interventions in both groups were delivered as an intensive group-based behavioral intervention. The dietary education included counseling, comprehensive lectures and cooking classes. Intervention within the fasting arm Fig. Similar to protocols from previous trials on periodic fasting in rheumatoid arthritis and diabetes mellitus type 2 42 , 43 patients were instructed to follow a modified DASH diet after the fasting period, with additional emphasis on plant-based and Mediterranean diet to optimize refeeding 44 , 45 , The DASH group Fig.
The randomization list was created by a biometrician not involved in patient recruitment or assessment using the Random Allocation Software The list was password-secured and only the biometrician was able to access it. On this basis, sealed, sequentially numbered opaque envelopes containing the treatment assignments were prepared.
Outcomes were assessed at baseline and at 1 and 12 weeks after randomization by a blinded outcome assessor who was not involved in patient recruitment, allocation, or treatment. Two primary outcome measures were defined: 24 h ambulatory systolic blood pressure at week 12 and the Homeostasis Model Assessment HOMA -index at week Twenty-four-hour ambulatory blood pressure monitoring ABPM and pulse pressure recording were performed using a digital blood pressure monitor Mobil-O-Graph ® PWA, I.
Baseline ABPM measurements were performed within one week before the starting of the intervention, those at week 12 within a week after the end of the intervention.
ABPM was initiated at the same time of day for each successive visit. The monitoring software automatically removed incorrect measurements using built-in algorithms.
Office blood pressure was measured at each time point, ambulatory blood pressure only at baseline and week Body weight, body fat percentage, and lean mass percentage were measured using the Omron BF bioelectrical impedance device BMI was calculated as the weight in kilograms divided by the square of height in meters.
Waist circumference was measured by two research assistants using a measuring tape in the horizontal plane exactly midway between the iliac crest and the costal arch. Measures were repeated twice and the mean of both measures was used.
Hip circumference was measured in the horizontal plain at the maximal circumference of the hips or buttock region above the gluteal fold, whichever is larger, using the same approach as for waist circumference.
Waist-hip-ratio was measured as the quotient of waist circumference and hip circumference Blood samples were collected from the antecubital vein into vacutainer tubes and analyzed using the Modular P analyzer Roche, Mannheim, Germany.
Metabolic parameters included plasma and blood glucose levels, blood insulin levels, HbA1C, and HbA1C IFCC and were analyzed using standard procedures.
Samples were destroyed after the analysis and were not further stored. All adverse events occurring during the study period were recorded. Patients experiencing adverse events were asked to see the study physician to assess their status and initiate any necessary response.
The most common symptoms during the fasting period were mild weakness, headaches, and mild perception of hunger. No serious adverse effects were reported.
During the normocaloric diet periods no adverse effects were reported. All analyses were conducted on an intention-to-treat basis, including all participants being randomized, regardless of whether or not they gave a full set of data or adhered to the study protocol. Missing data were multiply imputed by Markov chain Monte Carlo methods 55 , Whole blood staining was performed using antibodies against major leukocyte lineages.
Quantitative measurement was performed using a high throughput sampler BD and a BD FACS CantoII BD. Antibodies are listed in Table 2. Samples were analyzed using the FACSCanto II multicolor flow cytometer BD. The acquisition was performed with Diva 6.
Data analysis was performed using FlowJo Absolute cell numbers were calculated using the relative percentage of cell population compared to a marker used in the whole blood staining. Data were manually gated on single live cells and exported as FCS files in FCS Express V6. The automated analysis of FCS files was done by the FlowSOM 57 algorithm, an R 58 bio-conductor package that uses self-organizing maps for dimensional reduction and visualization of flow cytometry data.
All data were scaled and log-transformed on import. Cells were assigned to a Self-Organizing Map SOM with a 10 × 10 grid, grouping similar cells into nodes. Each node in the FlowSOM tree gets a score indicating its correspondence with this requested cell profile.
To visualize similar nodes in branches, a minimal spanning tree MST was constructed and cell counts were log scaled. To visualize the differences between the two-time points, the mean percentage per sample group was computed in each cluster and then the statistical difference was performed by applying MWU test on every node within metaclusters.
P values were two-sided and analysis was performed using RStudio version 3. Antihypertensive drugs were normalized in order to track changes during intervention.
In a first step, antihypertensives according to the WHO ATC classification system , diuretics, beta-blocking agents, calcium channel blockers, and agents acting on the renin-angiotensin system as well as the given dosage were identified at V1 and at follow-up visit after 3 months V3.
Secondly, drug dosage was normalized to the lowest drug dosage per patient and drug. The lowest drug dosage at baseline was set to one, while corresponding drug dosages at other time points where either zero if the medication was discontinued, one if there was no change in drug dosage between time points, smaller than one if the drug dosage was decreased or greater than one if the drug dosage was increased at a certain time point.
The sum of the agents taken was calculated at each time point. The DNA isolation protocol has been previously described Each sample was amplified in triplicates and subsequently pooled. After normalization, PCR amplicons were sequenced on MiSeq PE platform Illumina at the Helmholtz Centre for Infection Research, Braunschweig, Germany.
Sixty microliters of total DNA was used for shearing by sonication Covaris. Library preparation for Illumina sequencing was performed using the NEBNext Ultra DNA library prep Kit New England Biolabs. Adaptor enrichment was performed using seven cycles of PCR using NEBNext Multiplex oligonucleotides for Illumina Set1 and Set2, New England Biolabs.
Sequencing was performed on NovaSeq PE platform Illumina at the Helmholtz Centre for Infection Research, Braunschweig, Germany. Reads retrieved from 16S amplicon sequencing were analyzed using the LotuS 1. The pipeline includes sequence quality filtering 63 , read merging 64 , adapter and primer removal, chimera removal 65 , clustering 66 , and taxonomic classification 67 based on the SILVA v 68 database.
The validation dataset 22 was reprocessed using the exact same settings. Metagenomic shotgun sequences were processed within the NGLess framework 0. Sequences identified as non-human were mapped with bwa 70 to a the IGC gene catalog 0.
Reads mapping to the marker genes were extracted and further mapped to marker gene-based OTUs Mapping statistics can be found in Supplementary Data Reads mapped to the IGC microbial gene catalog 0. Reads were mapped to the mOTUv2 2. Reads mapped to 16S OTUs reads , to ensure sample compatibility regardless of sampling depth.
For functional microbiome analysis, IGC genes were binned to KEGG KOs 75 based on the annotations in MOCAT2 2. Supplementary Data 1 shows these results. Beta diversity was assessed as community distances between samples computed using the vegan 2. For microbiome data, Bray-Curtis distances on rarefied samples were used, and for immunome data, Euclidean distances.
Comparisons of distance profiles was performed using Mann—Whitney U tests. Mutlivariate analysis was carried out using Principal Coordinates Analysis PcoA as per the vegan 2.
Where described, delta metrics for the first two dimensions of unconstrained ordination were computed. PERMANOVA tests for multivariate effect were done using the adonis function in the vegan 2.
For all univariate analysis of clinical, immunome, or microbiome features, medication changes during the course of the study were accounted for as possible confounders using the following two-step procedure.
The first step was a nested model comparison of a linear model for each feature, involving as predictors age, patient ID, sex, and normalized dosage of each salient medication tracked at each time point, with the same model but additionally containing time point V1-V3 as a predictor.
Models were compared using a likelihood ratio test as implemented in the lmtest 0. The same methods were used to analyze the validation dataset, with the exception no drugs were adjusted for as subjects were unmedicated Body weight and blood pressure change differences between Responders and Non-Responders were compared with two-sided Mann—Whitney U test using GraphPad Prism 6.
Enterotypes of the samples in the fasting arm were performed by implementing the R package DirichletMultinomial 1. Second, a post-hoc test was done to account for dependency between same-donor samples: for each of two correlated features, a mixed-effects model was fitted of the rank-transformed variable using the rank of the other as predictor, with patient ID as a random effect.
This model was compared to a simpler model containing only the random effect under a likelihood ratio test as implemented in the lmtest 0. Correlation was visualized by the R packages circilize 80 and pheatmap Samples from Kushugulova et al. The Kushugulova samples were tested for significantly differential abundances between MetS cases and controls using the Mann—Whitney U test, then controlling that a MetS status predictor still significantly improves fit using the R lmtest 0.
Analogously, the Forslund samples were tested for significantly differential abundances between metformin-treated and untreated patients using the Mann—Whitney U test, then controlling that a metformin status predictor still significantly improves fit using the R lmtest 0.
The validation dataset 22 was analyzed exactly as the main study dataset, as described above. To estimate how well the omics data enables forecasting of the blood-pressure response in future patients, we performed a leave-one-patient-out cross-validation procedure.
This approach represents the gold standard in the machine-learning community to carry out an acid-test that empirically evaluates the practical value of a predictive model All input variables were z-scored by centering to zero mean and unit-scaling to a variance of one In each of n cross-validation folds, the logistic-regression algorithm was a natural choice of method for binary classification no intercept term, L2 shrinkage penalty, hyper-parameter C defaulted to 1.
Forward-stepwise selection is an established means 84 to screen the relevance of several hundred quantitative measures. The first step identifies the single input variable among the p candidates, with the best p-value having a statistically significant association with the blood-pressure outcome.
After adding this first variable to the empty null model, the second most significant i. Based on the top 10 variables, the logistic-regression algorithm could be more robustly fit to these subselected ten input dimensions only.
The ensuing predictive model was then explicitly validated by computing whether or not the obtained model parameters allowed for accurate derivation of the relevant blood-pressure response for the independent, unseen participant.
In this way, the omics data of each patient in our dataset served as test observation once. Averaging these yes-no results over all n predicted, versus observed clinical responses, yielded an estimate of the expected forecasting accuracy of the predictive model in participants that we would observe in other or later acquired datasets.
Further information on research design is available in the Nature Research Reporting Summary linked to this article. Data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Databases are to be found under the following links. Di Francesco, A. A time to fast. Science , — Article ADS PubMed CAS PubMed Central Google Scholar. Collaborators GBDD. Health effects of dietary risks in countries, a systematic analysis for the Global Burden of Disease Study Lancet , — Whelton, P.
et al. Circulation , e—e PubMed Google Scholar. Christ, A. The Western lifestyle has lasting effects on metaflammation. It can also….
Does masturbation increase blood pressure? Learn the connection between masturbation, arousal, sexual activity, and blood pressure as well as when you…. In a study of older adults living in long-term care, researchers randomly assigned facilities to use either a potassium-rich salt substitute or….
A recent study has found that tai chi was more effective compared to aerobic exercise in lowering blood pressure among prehypertension patients. Portopulmonary hypertension is a progressive complication of high blood pressure in the veins that lead to your liver.
Renal parenchymal disease is a group of conditions that can develop in the parts of your kidney that filter your urine and produce the hormone….
According to new research, adding salt at mealtime, using a salt shaker for example, is associated with an increased risk of developing kidney disease,. Baroreflex failure is a rare condition.
People with this condition experience sharply rising blood pressure during exercise, pain, and stress, and can….
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. How Does Eating or Not Eating Affect Your Blood Pressure? Medically reviewed by Erica Ramirez, PA-C — By Scott Frothingham — Updated on April 24, Eating Fasting Diet Other factors Contact a doctor Takeaway Eating can raise your blood pressure.
Can eating cause your blood pressure to go lower or higher? Can not eating cause your blood pressure to go lower or higher? Does what you eat matter? Factors that can affect blood pressure readings. When to see a doctor. When to seek immediate medical attention Seek emergency medical services if your blood pressure is markedly elevated with or without the following symptoms: headache dizziness altered level of consciousness nausea vomiting chest pain shortness of breath vision changes.
Was this helpful? The takeaway. How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.
We avoid using tertiary references. Background: Although it has been reported that the intermittent fasting IF diet has positive effects on heart health and improvement in blood pressure, it has not been sufficiently clarified how it could have these positive effects yet.
Objective: We aimed to evaluate the effects of IF on the autonomic nervous system ANS and renin-angiotensin system RAS , which are closely related to blood pressure. Methods: Seventy-two hypertensive patients were included in the study, and the data of 58 patients were used.
All the participants fasted for about hours for 30 days. Participants were evaluated with hour ambulatory blood pressure monitoring and Holter electrocardiography before and after IF; also, 5 ml venous blood samples were taken for assessment of Serum angiotensin I Ang-I and angiotensin II Ang-II levels and angiotensin-converting enzyme ACE activity.
Thank you for visiting Fasting and blood pressure control. You contrl using Mindfulness and brain health clntrol version with limited support for CSS. To obtain the Caloric intake and food quality experience, we recommend you use a more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Periods of fasting and refeeding may reduce cardiometabolic risk elevated by Western diet.
der Lustige Moment
Wacker, Ihre Phrase wird nützlich sein