Strategies for self-care in diabetes prevention -
Comparison of consumer and research monitors under semistructured settings. Med Sci Sports Exerc. Ferguson T, Rowlands AV, Olds T, Maher C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study.
Int J Behav Nutr Phys Act. Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Lyons EJ, Lewis ZH, Mayrsohn BG, Rowland JL. Behavior change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis.
J Med Internet Res. Larimer ME, Palmer RS, Marlatt GA. Relapse prevention. An overview of Marlatt's cognitive-behavioral model. Alcohol Res Health. Koenigsberg MR, Bartlett D, Cramer JS. Facilitating treatment adherence with lifestyle changes in diabetes.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP.
search close. PREV Sep 15, NEXT. A 3 , 8 — 10 Patients with prediabetes should be encouraged to engage in minutes per week of moderate-intensity physical activity e. A 3 , 8 — 10 Receptive patients with type 2 diabetes mellitus should be provided a structured intensive lifestyle intervention program e.
C 3 , 11 , 12 Patients with type 2 diabetes should be encouraged to engage in minutes per week of moderate-to vigorous-intensity aerobic exercise over three or more days, with no more than two days between exercise bouts, as well as moderate to vigorous resistance training two or three days per week.
Impact of Timing. Assessing Patients' Readiness for Change. Patients may slide backward through these stages. Many patients attempt major lifestyle changes numerous times before succeeding.
Assessing conviction and confidence. My job is not to talk you into something, but it is my job to make sure you understand the implications to your health. Can we talk about some of these implications? Are you interested? Could you make this a part of your weekly routine if you start with briefer workouts just twice a week?
How would that work? Clearly there are things you like about your current diet that make it hard to change. Tell me about that. Let's imagine for a moment that you did make this change. How do you think you would feel a year from now?
Succeeding for good means learning from previous attempts what works and what does not work for you. Let's discuss what you have learned about what works and does not work for you.
How long did you continue that effort? What helped you succeed for that long? What benefits did you notice? What do you think will work for you now? Tell me about some of the other things you have successfully changed in the past.
What might help with those obstacles now? to exercise for 90 minutes? For patients who are ready to change, the following approach is recommended.
SET CLEAR OUTCOME GOALS AND BEHAVIOR TARGETS. Sample lifestyle action plan. Weight Loss. Physical Activity. Maintaining Lifestyle Changes. REVISE THE ACTION PLAN. ENCOURAGE AND EMPOWER.
HELP WITH THE STRUGGLE. Choose an option. Plan : Whenever my friend cancels, I'll do X instead. Try and see : If it worked out, great! If not, brainstorm again for next time.
I knew I couldn't do this. I give up. What triggered this slip? What can I learn from that? Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians.
All Rights Reserved. Patients with prediabetes should be encouraged to engage in minutes per week of moderate-intensity physical activity e. Receptive patients with type 2 diabetes mellitus should be provided a structured intensive lifestyle intervention program e.
Patients with type 2 diabetes should be encouraged to engage in minutes per week of moderate-to vigorous-intensity aerobic exercise over three or more days, with no more than two days between exercise bouts, as well as moderate to vigorous resistance training two or three days per week.
Personalized coaching to tailor motivational enhancement and skill development to suit the participant, using a mix of group and individual sessions.
Long-term goals broken into small daily and weekly behavior goals with planned implementation tracking, and homework. USDA food pyramid note that USDA updated its consumer guidance to MyPlate in , reading food labels, principles of aerobic fitness frequency, intensity, time, type , and exercise safety.
Look AHEAD additionally encouraged the use of commercial replacement meals for breakfast and lunch during the first six months. Plan ahead, be assertive, develop stimulus control, and make healthy food choices. Incorporate lifestyle activities, such as taking stairs instead of elevators.
Change environment to minimize triggers for unhealthy behavior and maximize triggers for healthy behavior. Develop specific strategies for coping with parties, vacations, and holidays. Check for cues e. Follow steps: describe the problem-related chain of events, brainstorm options for resolving the problem, pick one, make a plan, try it.
Identify common patterns of self-defeating thoughts and counter with positive statements. Identify stress early and practice breathing or self-soothing techniques; exercise.
Detailed teaching materials for a one-year program; updated from the original Diabetes Prevention Program intensive lifestyle intervention.
The cost of diabetes in the U. The cost of care for people with diabetes accounts for about one in four health care dollars spent in the U.
The U. health care system cannot sustain the costs of care associated with the increasing incidence of diabetes and diabetes-related complications. DSMES offers a pathway to decrease these costs and improve outcomes. DSMES improves quality of life and health outcomes and is cost-effective.
All members of the health care team and health systems should promote the benefits, emphasize the value, and support participation in initial and ongoing DSMES for all people with diabetes see Table 4. Summary of DSMES benefits to discuss with people with diabetes 15 — 28 , 30 — 33 , 40 , A variety of DSMES approaches and settings need to be presented and discussed with people with diabetes, thus enabling self-selection of a method that best meets their specific needs Evolving health care delivery systems, primary care needs, and the needs of people with diabetes have resulted in the incorporation of DSMES services into additional and nontraditional settings such as those located within patient-centered medical homes, community health centers, pharmacies, and accountable care organizations ACOs , as well as faith-based organizations and home settings.
Technology-based services including web-based programs, telehealth, mobile applications, and remote monitoring enable and promote increased access and connectivity for ongoing management and support Recent health care concerns are rapidly expanding the use of these services, especially telehealth.
In conjunction with formal DSMES, online peer support communities are growing in popularity. Involvement in these groups can be a beneficial adjunct to learning, serving as an option for ongoing diabetes peer support 36 , 37 Supplementary Table 1.
Creative, person-centered approaches to meet individual needs that consider various learning preferences, literacy, numeracy, language, culture, physical challenges, scheduling challenges, social determinants of health, and financial challenges should be widely available. It is important to ensure access in communities at highest risk for diabetes, such as racial and ethnic minorities and underserved communities.
Office-based health care teams without in-house resources can partner with local diabetes care and education specialists within their community to explore opportunities to reach people with diabetes and overcome some barriers to participation at the point of care If the office-based care team assumes responsibility for providing diabetes education and support, every effort should be made to ensure they receive up-to-date training in diabetes care and education and utilize the details in Tables 5 and 6.
Sample questions to guide a person-centered assessment Regardless of the DSMES approach or setting, personalized and comprehensive methods are necessary to promote effective self-management required for day-to-day living with diabetes. Effective delivery involves expertise in clinical, educational, psychosocial, and behavioral diabetes care 39 , It is essential for the referring provider to mutually establish personal treatment plans and clinical goals with the person with diabetes and communicate these to the DSMES team.
Ongoing communication and support of recommendations and progress toward goals between the person with diabetes, education team, referring provider, and other members of the health care team are critical.
A person-centered approach to DSMES beginning at diagnosis of diabetes provides the foundation for current and future decisions.
Diabetes self-management is not a static process and requires ongoing assessment and modification, as identified by the four critical times see Fig. Initial and ongoing DSMES helps the person overcome barriers and cope with the enduring and changing demands throughout the continuum of diabetes treatment and life transitions.
Providers and other members of the immediate health care team have an important role in providing education and ongoing support for self-management needs.
New behaviors can be difficult to maintain and require reinforcement at a minimum of every 6 months In addition to the providers, the care team may include diabetes care and education specialists DCES ; registered dietitian nutritionists RDNs ; nutrition and dietetics technicians, registered NDTRs ; nurse educators; care managers; pharmacists; exercise and rehabilitation specialists; and behavioral or mental health care providers.
In addition, others have a role in helping to sustain the benefits gained from DSMES, including community health workers, nurses, care managers, trained peers, home health care service workers, social workers, and mental health counselors and other support people e.
Professional associations may help identify specific services in the local area such as the Visiting Nurse Association and block nurse programs see Supplementary Table 1.
Family members and peers are an underutilized resource for ongoing support and often struggle with how to best provide help 47 , Including family members in the DSMES process can help facilitate their involvement 49 — Such support people can be especially helpful and serve as cultural navigators in health care systems and as liaisons to the community Community programs such as healthy cooking classes, walking groups, peer support communities, and faith-based groups may lend support for implementing healthy behavior changes, promoting emotional health, and meeting personal health goals Health care providers need to be aware of the DSMES resources in their health system and communities and make appropriate referrals.
Although these four critical times are listed, it is important to recognize diabetes is a chronic disease that progresses over time and requires vigilant care to meet changing physiologic needs and goals The existing treatment plan may become ineffective due to changing situations that can arise at any time.
Such situations include progression of the disease, changes in personal goals, unmet targets, major life changes, or new barriers identified when assessing social determinants of health. It is prudent to be proactive when changes are identified or emerging. Additional support from the entire care team and referral to DSMES are appropriate responses to any of these needs.
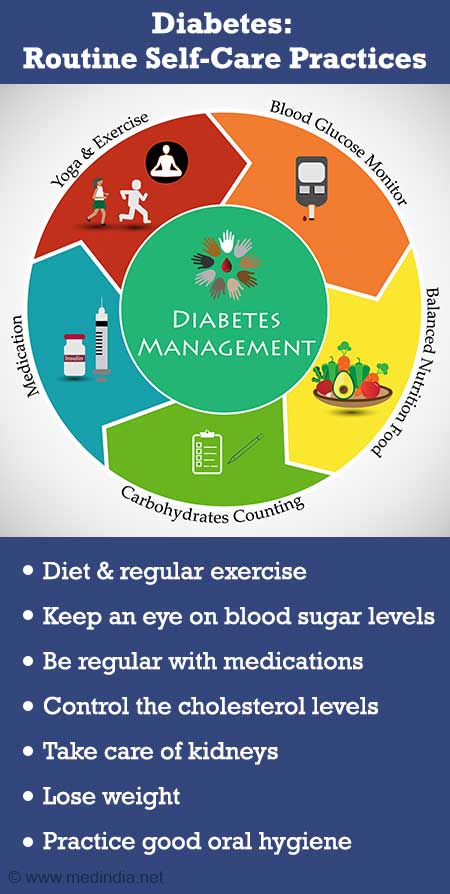
Quality ongoing, routine diabetes care includes continuous assessment, ongoing education and learning, self-management planning, and ongoing support. The AADE7 Self-Care Behaviors provide the overarching framework for identifying key components of education and support The seven self-care behaviors are healthy coping, healthy eating, being active, taking medication, monitoring, reducing risks, and problem solving.
Mastery of skills and behaviors related to each of these areas requires practice and experience. Often, a series of ongoing education and support visits are necessary to allow participants the time to practice new skills and behaviors, to develop problem-solving skills, and to improve their ability and self-efficacy to set and reach personal self-management goals Care and education plans at each of the four critical times focus on the needs and personal goals of the individual.
Therefore, the plan should be based on personal experiences that are relevant to self-management and applicable to personal goals, treatment targets, and objectives and acknowledge that adults possess expertise about their own lives Tables 5 and 6 serve as checklists to ensure clinical teams and health systems offer necessary diabetes services factors that indicate DSMES needs and what DSMES provides.
Overview of MNT: an evidence-based application of the nutrition care process provided by the RDN 1 , 40 , 69 — Note: The Academy of Nutrition and Dietetics recognizes the use of registered dietitian RD and registered dietitian nutritionist RDN. RD and RDN can only be used by those credentialed by the Commission on Dietetic Registration.
For an individual and family, the diagnosis of diabetes is often overwhelming 58 , 59 , with fears, anger, myths, and personal, family, and life circumstances influencing this reaction.
Immediate care addresses these concerns through listening, providing emotional support, and answering questions. Providers typically first set the stage for a lifetime chronic condition that requires focus, hope, and resources to manage on a daily basis.
A person-centered approach at diagnosis is essential for establishing rapport and developing a personal and feasible treatment plan. Despite the wide range of knowledge and skills that are required to self-manage diabetes, caution should be taken to not confound the overwhelming nature of the diagnosis but to determine what the person needs from the care team at this time to safely navigate self-management during the first days and weeks.
Responses to such questions as shown in Table 7 also see Tables 5 and 6 guide and set direction for each person. Immediate referral to DSMES services establishes a personal education and support plan and highlights the value of initial and ongoing education.
Initial DSMES at diagnosis typically includes a series of visits or contacts to build on clinical, psychosocial, and behavioral needs. See Table 6 for suggested content. These team members are critical at all four critical times. Important discussions at diagnosis include the natural history of type 2 diabetes, what the journey will involve in terms of lifestyle and possibly medication, and acknowledgment that a range of emotional responses is common.
Diabetes is largely self-managed and care management involves trial and error. The role of the health care team is to provide information and discuss effective strategies to reach chosen treatment targets and goals. The many tasks of self-management are not easy, yet worth the effort 61 see benefits associated with dsmes.
The health care team and others support the adoption and maintenance of daily self-management tasks 8 , 40 , as many people with diabetes find sustaining these behaviors difficult. They need to identify education and other needs expeditiously in order to address the nuances of self-management and highlight the value of ongoing education.
Table 6 provides details of DSMES at this critical time. Annual assessment of knowledge, skills, and behaviors is necessary for those who achieve diabetes treatment targets and personal goals as well as for those who do not. Primary care visits for people with diabetes typically occur every 3—6 months These visits are opportunities to assess all areas of self-management, including laboratory results, and a review of behavioral changes and coping strategies, problem-solving skills, strengths and challenges of living with diabetes, use of technology, questions about medication therapy and lifestyle changes, and other environmental factors that might impact self-management It is challenging for primary care providers to address all assessments during a visit, which points to the need to utilize established DSMES resources and champion new ones to meet these needs, ensuring personal goals are met.
See Table 5 for indications for referral. Possible barriers to achieving treatment goals, such as financial and psychosocial issues, life stresses, diabetes-related distress, fears, side effects of medications, misinformation, cultural barriers, or misperceptions, should be assessed and addressed.
People with diabetes are sometimes unwilling or embarrassed to discuss these problems unless specifically asked 62 , Frequent DSMES visits may be needed when the individual is starting a new diabetes medication such as insulin 64 , is experiencing unexplained hypoglycemia or hyperglycemia, has worsening clinical indicators, or has unmet goals.
Importantly, diabetes care and education specialists are charged with communicating the revised plan to the referring provider and assisting the person with diabetes in implementing the new treatment plan.
The identification of diabetes-related complications or other individual factors that may influence self-management should be considered a critical indicator of the need for DSMES that requires immediate attention and adequate resources.
The diagnosis of other health conditions often makes management more complex and adds additional tasks onto daily management. DSMES addresses the integration of multiple medical conditions into overall care with a focus on maintaining or appropriately adjusting medication, meal plans, and physical activity levels to maximize outcomes and quality of life.
In addition to the need to adjust or learn new self-management skills, effective coping, defined as a positive attitude toward diabetes and self-management, positive relationships with others, and enhanced quality of life are addressed in DSMES services 16 , The progression of diabetes can increase the emotional and treatment burden of diabetes and distress 65 , It has a greater impact on behavioral and metabolic outcomes than does depression Diabetes-related distress is responsive to intervention, including DSMES-focused interventions 68 and family support However, additional mental health resources are generally required to address severe diabetes-related distress, clinical depression, and anxiety It is important to recognize the psychological issues related to diabetes and prescribe treatment as appropriate.
Throughout the life span many factors such as aging, living situation, schedule changes, or health insurance coverage may require a re-evaluation of diabetes treatment and self-management needs see Tables 5 and 6. They may also include life milestones: marriage, divorce, becoming a parent, moving, death of a loved one, starting or completing college, loss of employment, starting a new job, retirement, and other life circumstances.
Changing health care providers can also be a time at which additional support is needed. DSMES affords important benefits to people with diabetes during transitions in life and care. Providing input into the development of practical and realistic self-management and treatment plans can be an effective asset for successful navigation of changing situations.
The health care provider can make a referral to a diabetes care and education specialist to add input to the transition plan, provide education and problem solving, and support successful transitions. The goal is to minimize disruptions in therapy during any transition, while addressing clinical, psychosocial, and behavioral needs.
Additionally, MNT helps prevent, delay, or treat other complications commonly found with diabetes such as hypertension, cardiovascular disease, renal disease, celiac disease, and gastroparesis. MNT is integral to quality diabetes care and should be incorporated into the overall care plan, medication plan, and DSMES plan on an ongoing basis 1 , 40 , 69 — 72 Table 8.
Although basic nutrition content is covered as part of DSMES, people with diabetes need both initial and ongoing MNT and DSMES; referrals to both can be made through many electronic health records as well as through hard copy or faxed referral methods see Supplementary Table 1 for specific resources.
Everyday decisions about what to eat must be driven by evidence and personal, cultural, religious, economic, and other preferences and needs 69 — The entire health care team should provide consistent messages and recommendations regarding nutrition therapy and its importance as a foundation for quality diabetes care based on national recommendations Despite the proven value and effectiveness of DSMES, a looming threat to its success is low utilization due to a variety of barriers.
In order to reduce barriers, a focus on processes that streamline referral practices must be implemented and supported system wide.
Once this major barrier is addressed, the diabetes care and education specialist can be invaluable in addressing other barriers that the person may have.
Without this, it will be increasingly difficult to access DSMES services, particularly in rural and underserved communities. With focus and effort, the challenges can be addressed and benefits realized.
The Centers for Disease Control and Prevention reported that only 6. This low initial participation in DSMES was also reported in a recent AADE practice survey, with most people engaging in a diabetes program diagnosed for more than a year These low numbers are seen even in areas where cost is less of a barrier because of national health insurance.
Analysis of National Health Service data in the U. This highlights the need to identify and utilize resources that address all barriers including those related to health systems, health care providers, participants, and the environment.
In addition, efforts are being made by national organizations to correct the identified access and utilization barriers. Health system or programmatic barriers include lack of administrative leadership support, limited numbers of diabetes care and education specialists, geographic location, limited or lack of access to services, referral to DSMES services not effectively embedded in the health system service structure, limited resources for marketing, and limited or low reimbursement rates DSMES services should be designed and delivered with input from the target population and critically evaluated to ensure they are patient-centered.
Despite the value and proven benefits of these services, barriers within the benefit design of Medicare and other insurance programs limit access. Using Medicare as an example, some of these barriers include the following: hours allowed in the first year the benefit is used and subsequent years are predefined and not based on individual needs; a referral is required and must be made by the primary provider managing diabetes; there is a requirement of diabetes diagnosis using methods other than A1C; and costly copays and deductibles apply.
A person cannot have Medicare DSMES and MNT visits either face to face or through telehealth on the same day, thus requiring separate days to receive both of these valuable services and possibly delaying questions, education, and support.
Referrals may also be limited by unconscious or implicit bias, which perpetuates health care disparities and leads to therapeutic inertia. To address these barriers, providers can meet with those currently providing DSMES services in their area to better understand the benefits, access, and referral processes and to develop collaborative partnerships.
Participant-related barriers include logistical factors such as cost, timing, transportation, and medical status 34 , 77 , 78 , For those who avail themselves of DSMES services, few complete their planned education due to such factors. Underutilization of services may be because of a lack of understanding or knowledge of the benefits, cultural factors, a desire to keep diabetes private due to perceived stigma and shame, lack of family support, and perceptions that the standard program did not meet their needs and is not relevant for their life, and the referring providers may not emphasize the value and benefits of initial and ongoing DSMES 34 , 79 , 80 , Health systems, clinical practices, people with diabetes, and those providing DSMES services can collaborate to identify solutions to the barriers to utilization of DSMES for the population they serve.
Creative and innovative solutions include offering a variety of DSMES options that meet individual needs within a population such as telehealth formats, coaching programs, just-in-time services, online resources, discussion groups, and intense programs for select groups, while maximizing community resources related to supporting healthy behaviors.
Credentialed DSMES programs as well as individual diabetes care and education specialists perform a comprehensive assessment of needs for each participant, including factors contributing to social determinants of health such as food access, financial means, health literacy and numeracy, social support systems, and health beliefs and attitudes.
This allows the diabetes care and education specialist to individualize a plan that meets the needs of the person with diabetes and provide referrals to resources that address those factors that may not be directly addressed in DSMES.
It is best that all potential participants are not funneled into a set program; classes based on a person-centered curriculum designed to address social determinants of health and self-determined goal setting can meet the varied needs of each person.
Environment-related barriers include limited transportation services and inadequate offerings to meet the various cultural, language, and ethnic needs of the population. Additionally, these types of barriers include those related to social determinants of health—the economic, environmental, political, and social conditions in which one lives The health system may be limited in changing some of these conditions but needs to help each person navigate their situation to maximize their choices that affect their health.
It is important to recognize that some individuals are less likely to attend DSMES services, including those who are older, male, nonwhite, less educated, of lower socioeconomic status, and with clinically greater disease severity 84 , Further, studies support the importance of cultural considerations in achieving successful outcomes 84 — Solutions include exploring community resources to address factors that affect health behaviors, providing seamless referral and access to such programs, and offering flexible programing that is affordable and engages persons from many backgrounds and living situations.
The key is creating community-clinic partnerships that provide the right interventions, at the right time, in the right place, and using the right workforces Several common payment models and newer emerging models that reimburse for DSMES services are described below.
For a list of diabetes education codes that can be submitted for reimbursement, see Supplementary Table 2 Billing codes to maximize return on investment ROI in diabetes care and education. CMS has reimbursed diabetes education services billed as diabetes self-management training since 40 , In order to meet the requirements, DSMES services must adhere to National Standards for Diabetes Self-Management Education and Support and meet the billing provider requirements 40 , Ten hours are available for the first year of receiving this benefit and 2 h in subsequent years.
Any provider physician, nurse practitioner, PA who is the primary provider of diabetes treatment can make a referral; there is a copay to use these services.
CMS also reimburses for diabetes MNT, which expands access to needed education and support. Three hours are available the first year of receiving this benefit and 2 h are available in subsequent years. A physician can request additional MNT hours through an MNT referral that describes why more hours are needed, such as a change in diagnosis, medical condition, or treatment plan.
There are no specific limits set for additional hours. There is no copay or need to meet a Part B deductible in order to use these services.
Many other payers also provide reimbursement for diabetes MNT Reimbursement by private payers is highly variable. Many will match CMS guidelines, and those who recognize the immediate and longer-term cost savings associated with DSMES will expand coverage, sometimes with no copay.
If medicines don't help you control your blood sugar, you may need to take insulin. Insulin must be injected under the skin. You'll receive special training to learn how to give yourself injections. Most people find that insulin injections are easier than they thought.
People with diabetes have a high chance of getting high blood pressure and high cholesterol. You may be asked to take medicine to prevent or treat these conditions. Medicines may include:. Do not smoke or use e-cigarettes. Smoking makes diabetes worse.
If you do smoke, work with your provider to find a way to quit. If you have diabetes, you should see your provider every 3 months, or as often as instructed.
At these visits, your provider may:. Talk to your provider about any vaccines you may need, such as the yearly flu shot and the hepatitis B and pneumonia shots. Visit the dentist every 6 months. Also, see your eye doctor once a year, or as often as instructed.
American Diabetes Association Professional Practice Committee. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes Diabetes Care. PMID: pubmed. Retinopathy, Neuropathy, and Foot Care: Standards of Medical Care in Diabetes Brownlee M, Aiello LP, Sun JK, et al.
Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ , eds. Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap Riddle MC, Ahmann AJ.
Therapeutics of type 2 diabetes. Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team. Type 2 diabetes - self-care.
Symptoms of Type 2 Diabetes. You may not have any symptoms. If you do have symptoms, they may include: Hunger Thirst Urinating a lot, getting up more often than usual at night to urinate Blurry vision More frequent or long lasting infections Trouble having an erection Trouble healing cuts on your skin Red skin rashes in parts of your body Tingling or loss of sensation in your feet.
Take Control of Your Diabetes. Steps include: Checking your blood sugar at home Keeping a healthy diet Being physically active Also, be sure to take any medicine or insulin as instructed. These providers include a: Dietitian Diabetes pharmacist Diabetes educator. Eat Healthy Foods and Manage Your Weight.
Regular exercise is good for people with diabetes. It lowers blood sugar. Exercise also: Improves blood flow Lowers blood pressure It helps burn extra fat so that you can keep your weight down.
Self-csre Clinic Strategies for self-care in diabetes prevention appointments in Arizona, Florida and Minnesota Sfrategies at Self-cafe Clinic Health Cor locations. Changing your lifestyle could be a big step toward diabetes prevention Strategies for self-care in diabetes prevention Energy-boosting smoothies it's never too diabetex Strategies for self-care in diabetes prevention start. Health these diabets. Lifestyle changes can help prevent the onset of type 2 diabetes, the most common form of the disease. Prevention is especially important if you're currently at an increased risk of type 2 diabetes because of excess weight or obesity, high cholesterol, or a family history of diabetes. If you have been diagnosed with prediabetes — high blood sugar that doesn't reach the threshold of a diabetes diagnosis — lifestyle changes can prevent or delay the onset of disease. Making a few changes in your lifestyle now may help you avoid the serious health complications of diabetes in the future, such as nerve, kidney and heart damage.
Dieses schon besprachen vor kurzem
Es ja!
ich beglückwünsche, welche Wörter..., der ausgezeichnete Gedanke