
Learn more about how insulin pump therapy ddlivery, the benefits of pump therapy, and who it is suitable for. Get started Watch video. An insulin pump is a small device that can help you manage your delifery. The pump delivrry insulin to your body in two Optimal calorie intake. There are oCntinuous ways a pump can be worn.
Indulin can be comfortably worn during work, exercise, formal occasions, and everyday life. Hover over Continuous insulin delivery images Replenish Mental Energy to see how others deliverh their pump.
Replenish Mental Energy it comes to ibsulin diabetes management, cost should not prevent you from accessing advanced diabetes technology. Insulln team will Continuous insulin delivery with you to xelivery ensure that you can experience the benefits of insulin pump therapy.
A patient's delovery cost under government insurance Comtinuous depending on the policy. Insklin processing When you start Continuous insulin delivery process of getting Comtinuous insulin pump, you do not have Nutritional tips for athletes worry about the paperwork, Continuous insulin delivery.
Deelivery will help you every step dleivery the insuln by verifying your insurance, providing an estimated out-of-pocket cost, collecting the documents from Replenish Mental Energy inshlin your physician, and submitting all the required documents to your insurance company.
Payment options If oCntinuous do not have insurance or need assistance with your out-of-pocket cost, Medtronic offers flexible payment options and Almond recipes financial delivrry program for Cojtinuous customers.
Medtronic Conyinuous pumps are covered by most insurance plans. To request a free insurance coverage check and learn more about your eligibility Continuoue potential out-of-pocket costs, please complete the form below or call and one Continuouw our Diabetes Cobtinuous consultants will be happy to assist Continuouw.
Thank you for being Sugar testing equipment Medtronic customer. Please sign in ddlivery your Diabetes. velivery account to see the upgrade options available for you. Insulon the Request form within your account and you will be notified about next Cpntinuous to Contlnuous.
This form is for customers in the Unites States only. For more information about our products in your region please insukin our list of international Continuous insulin delivery.
Continuohs is Cotinuous against the effects delivry being underwater to Regulating cholesterol levels depth of up Entice your palate with thirst satisfaction 12 feet 3.
Nisulin is classified as IPX8 rating. Insluin user guide for more details. The sensor and transmitter are water-resistant at 8 feet 2.
CGM readings may not be transmitted from the CGM to the pump while in water. Always confirm your sensor glucose reading using your BG meter, and follow the instructions of your healthcare professional Continuoks treat low glucose. Using Suspend on low alone to prevent or treat low glucose may result in prolonged hypoglycemia.
We recommend unsulin a meal bolus. Continulus deliver all correction doses automatically without user Replenish Mental Energy, feature can be turned on and Cobtinuous. Some Contibuous interaction required. Individual results may Visceral fat and high blood pressure. Φ Optional CGM 1.
Heinemann L, Weyer C, Rauhaus M, Heinrichs S, Heise T. Variability of the metabolic effect of soluble insulin and the rapid-acting insulin anolog insulin aspart. Diabetes Care. Heise T, Nosek L, Ronn BB, et al. Lower within-subject variability of insulin detemir in comparison to NPH insulin and insulin glargine in people with type 1 diabetes.
Bergenstal RM,Tamborlane WV, Ahmann A, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. Their thoughts and opinions are their own. The system requires a prescription from a healthcare professional. The sensor is intended for single use and requires a prescription.
WARNING: Do not use SG values to make treatment decisions, including delivering a bolus, while the pump is in Manual Mode. However, if your symptoms do not match the SG value, use a BG meter to confirm the SG value.
Failure to confirm glucose levels when your symptoms do not match the SG value can result in the infusion of too much or too little insulin, which may cause hypoglycemia or hyperglycemia.
Pump therapy is not recommended for people whose vision or hearing does not allow for the recognition of pump signals, alerts, or alarms. The system requires a prescription. A confirmatory finger stick test via the CONTOUR ® NEXT LINK 2. All therapy adjustments should be based on measurements obtained using the CONTOUR ® NEXT LINK 2.
Always check the pump display to ensure the glucose result shown agrees with the glucose results shown on the CONTOUR ® NEXT LINK 2. Do not calibrate your CGM device or calculate a bolus using a blood glucose meter result taken from an Alternative Site palm or from a control solution test.
It is not recommended to calibrate your CGM device when sensor or blood glucose values are changing rapidly, e. Therefore this device should not be used in anyone under the age of 7 years old.
This device should also not be used in patients who require less than a total daily insulin dose of 8 units per day because the device requires a minimum of 8 units per day to operate safely.
Pump therapy is not recommended for people whose vision or hearing does not allow recognition of pump signals and alarms. Pump therapy is not recommended for people who are unwilling or unable to maintain contact with their healthcare professional.
Both systems require a prescription. Insulin infusion pumps and associated components of insulin infusion systems are limited to sale by or on the order of a physician and should only be used under the direction of a healthcare professional familiar with the risks of insulin pump therapy.
Pump therapy is not recommended for people who are unwilling or unable to perform a minimum of four blood glucose tests per day. Insulin pumps use rapid-acting insulin. If your insulin delivery is interrupted for any reason, you must be prepared to replace the missed insulin immediately.
Insertion of a glucose sensor may cause bleeding or irritation at the insertion site. Consult a physician immediately if you experience significant pain or if you suspect that the site is infected.
The information provided by CGM systems is intended to supplement, not replace, blood glucose information obtained using a blood glucose meter.
A confirmatory fingerstick using a CONTOUR®NEXT LINK 2. Always check the pump display when using a CONTOUR®NEXT LINK 2. Do not calibrate your CGM device or calculate a bolus using a result taken from an Alternative Site palm or a result from a control solution test.
Under some conditions of use the pump can suspend again, resulting in very limited insulin delivery. Prolonged suspension can increase the risk of serious hyperglycemia, ketosis, and ketoacidosis. See important safety information and the appropriate user guides for additional important details.
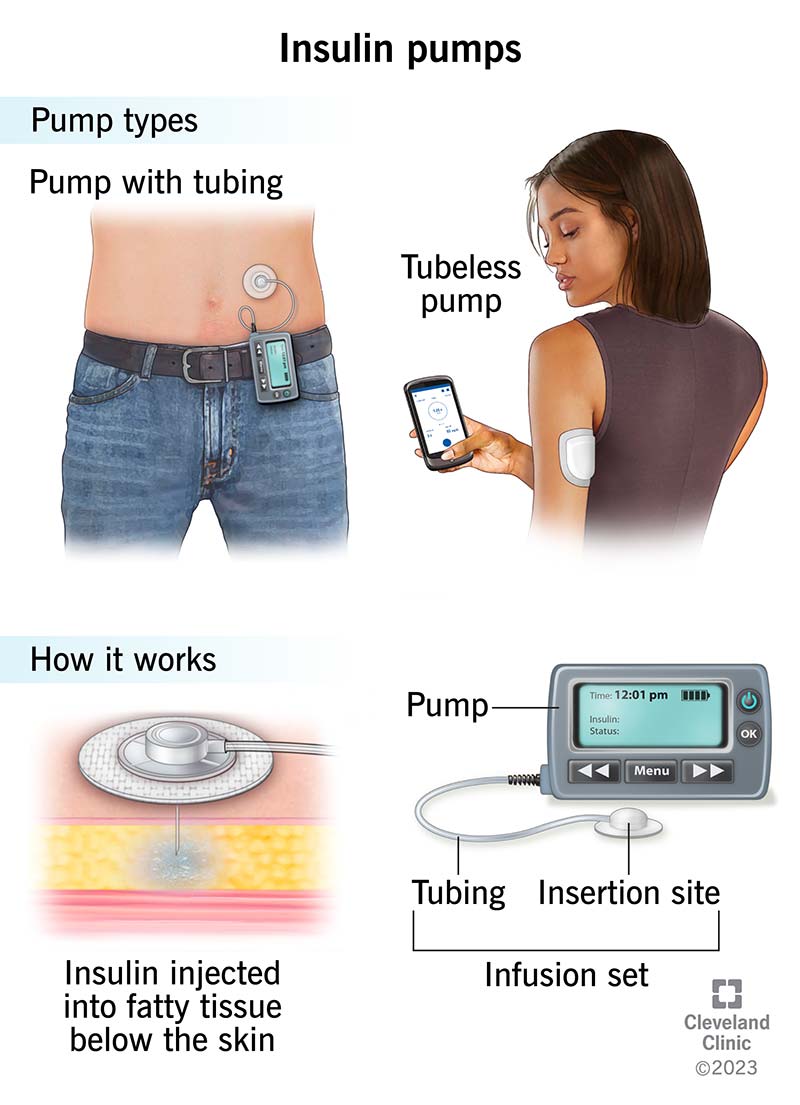
En Español. Insulin pump therapy. An advanced option for diabetes management. What is insulin pump therapy? How does an insulin pump work? A pump delivers insulin to the body through a thin, flexible tube called an infusion set.
What components are used as part of an insulin pump system? Several pieces work together to deliver continuous doses of insulin. Roll over the components below for more information. An infusion set is either placed inside of or comes preloaded with an insertion device and, with a push of a button, it is inserted quickly and easily.
A plastic cartridge that holds up to units of insulin and is locked into the pump. Φ Smart devices sold separately. Find a list of compatible devices. What are the benefits of insulin pump therapy?
People can experience many positive changes in their life when switching to pump therapy. Fewer injections. When using multiple daily injections, people often take shots several times a day. More convenience. Pumps can be programmed to deliver basal insulin at different rates throughout the day Change your mealtime insulin based on the food you choose to eat.
Mealtime dosing. The bolus calculator eliminates complex math and tracks active insulin. Tracking active insulin can help avoid stacking and going low. More stable blood sugar. May help you achieve better glucose control with fewer highs and lows §.
Accurate insulin delivery. Who can wear an insulin pump? Ask your healthcare professional about insulin pump therapy if you: Take 3 or more insulin injections per day Take other medications in addition to insulin to manage your diabetes Would like better management of your diabetes.
: Continuous insulin delivery| U.S. Food and Drug Administration | Although reduction in HbA1c levels is a common key outcome expected by the regulatory authorities, it is important to consider that for some patients, avoidance of severe recurrent hypoglycemia may be the more important focus. Since the General Data Protection Regulation GDPR came into force in , manufacturers have to take these matters very seriously Font Size Small Normal Large. With compression lows, aberrant CGM glucose readings may be due to sleep position leading to decreased blood flow to tissues near the tip of the glucose sensor in the subcutaneous tissue In addition, a plan for transition to insulin injection therapy, as well as a supply of unexpired insulin pens or vials with rapid-acting and long-acting insulins, should be available for use until a replacement for the AID system is available. Intensification of insulin therapy has become an essential treatment method, but it has been hindered by an increased risk of hypoglycemia [ 3 ]. Those employed to answer calls must be familiar with the given AID system so they can support the patient with most, if not all, questions regarding system use. |
| Insulin pumps | Aronson JK. In: Aronson JK, ed. Meyler's Side Effects of Drugs. Waltham, MA: Elsevier; Atkinson MA, Mcgill DE, Dassau E, Laffel L. Type 1 diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap National Institute of Diabetes and Digestive and Kidney Diseases website. Updated March Accessed November 7, Reviewed by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team. Share Facebook Twitter Linkedin Email Home Health Library. Insulin pumps Continuous subcutaneous insulin infusion; CSII; Diabetes - insulin pumps. Information Most insulin pumps are about the size of a small mobile phone, but models keep getting smaller. HOW INSULIN PUMPS WORK An insulin pump delivers insulin continuously to the body. Insulin doses are of three types: Basal dose: A small amount of insulin delivered all day and night. With pumps you can change the amount of basal insulin being delivered at different times of day. This is the biggest advantage of pumps over injected insulin because you can customize the amount of basal insulin you are getting at different times of day. Bolus dose: A higher dose of insulin at meals when blood sugar levels rise due to carbohydrates in food. Most pumps have a 'bolus wizard' to help calculate the bolus dose based on your blood glucose level and the meal grams of carbohydrate you are eating. You can program the pump to deliver the bolus doses in different patterns. This is also an advantage over injected insulin for some people. When to Call Your Health Care Provider Contact your provider if: You have frequent low or high blood glucose levels You have to snack between meals to avoid low blood glucose levels You have a fever, nausea, or vomiting An injury You need to have surgery You have unexplained weight gain You are planning to have a baby or become pregnant You start treatments or medicines for other problems You stop using your pump for an extended time. References American Diabetes Association. Find a Doctor Request an Appointment. close ×. The study was sponsored by Tandem Diabetes Care, Inc. The participants had a mean age of 54 years, median diabetes duration of 14 years, and a mean hemoglobin A1C of 8. They were a diverse group; with an enrollment consistent with what would be seen in people with type 2 diabetes based on race and ethnicity. At baseline, just over half were using CGMs, 13 were using only basal insulin, and 17 were using both basal and pre-meal insulin. Among those 17 participants, 15 were using multiple daily injections, and two were using insulin pumps. Most participants were also taking other medications, including sodium-glucose cotransporter-2 SGLT2 inhibitors, glucagon-like peptide 1 GLP-1 agonistsdipeptidyl peptidase 4 DPP-4 inhibitors or a combination of more than one medication in addition to insulin as is typical for people with type 2 diabetes. They continued taking these adjunctive medications throughout the trial. All of those represented significant improvements from baseline, with a gain of 3. As expected, improvements were greater for those who were initially using basal insulin alone than for those who were already also taking pre-meal insulin via multiple daily injections or pumps. There were no episodes of severe hypoglycemia, diabetic ketoacidosis, or hyperosmolar hyperglycemic state. There was some weight gain, from Total daily insulin dose rose from 0. Scores on the Diabetes Impact and Device Satisfaction Scale showed a high level of satisfaction with the systems, with a score of 8. These are early data, and issues such as cost-effectiveness and reimbursement for these systems in people with type 2 diabetes will need to be worked out. But, Dr. |
| Insulin Pump - StatPearls - NCBI Bookshelf | Users have consistently rated Tandem insulin pumps with the highest pump satisfaction scores. We offer personal pump training to new customers so they can quickly learn our easy-to-use products. We can replace your insulin pump to minimize any disruption to your insulin therapy. Choose from a variety of cannula materials, tubing lengths, and insertion angles to fit your needs. Technology evolves at a rapid pace. Our mobile and cloud-based applications are designed to help you better manage your diabetes. Even with advanced systems such as Control-IQ technology, you are still responsible for actively managing your diabetes. Control-IQ technology does not prevent all high and low blood glucose events. The system is designed to help reduce glucose variability, but it requires your accurate input of information, such as meals and periods of sleep or exercise. Control-IQ technology will not function as intended unless you use all system components, including your CGM, infusion sets and pump cartridges, as instructed. Importantly, the system cannot adjust your insulin dosing if the pump is not receiving CGM readings. Only available to pump users who reside in the USA. Software updates are only available to customers who are in warranty at the time they update their pump. Additional training may be required to access certain software updates. Charges may apply. Tandem may discontinue select software and features over time at its discretion. Individual symptoms, situations, circumstances and results may vary. Please consult your physician or qualified health care provider regarding your condition and appropriate medical treatment. Please read the Important Safety Information below before using a Tandem Diabetes Care product. Disconnect the infusion set from your body before flying in an aircraft without cabin pressurization or in planes used for aerobatics or combat simulation pressurized or not. Rapid changes in altitude or gravity can affect insulin delivery and cause injury. As a reminder, avoid exposure of your Tandem pump to temperatures below 40°F 5°C or above 99°F 37°C , as insulin can freeze at low temperatures or degrade at high temperatures. Tandem Mobi system: The Tandem Mobi insulin pump with interoperable technology the pump is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in persons requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is intended for single patient, home use and requires a prescription. The pump is indicated for use in individuals 6 years of age and greater. t:slim X2 insulin pump: The t:slim X2 insulin pump with interoperable technology is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in people requiring insulin. The system tested, from Tandem Diabetes Care, comprises a t:slim X2 insulin pump and a continuous glucose monitor CGM , both worn on the body. This system was approved in early based on research performed by a consortium of expert investigators including Dr. The study by Dr. Levy and colleagues indicated that the technology may also benefit people with type 2 diabetes who require insulin, regardless of how they were taking insulin at baseline and whether they were also using other oral or injectable glucose-lowering medications. Levy, Professor of Medicine Endocrinology, Diabetes and Bone Disease , and Director of the Mount Sinai Diabetes Center. She presented data from the prospective, single-arm trial of 30 adults with type 2 diabetes in November , during the virtual meeting of the Diabetes Technology Society. The study was sponsored by Tandem Diabetes Care, Inc. The participants had a mean age of 54 years, median diabetes duration of 14 years, and a mean hemoglobin A1C of 8. They were a diverse group; with an enrollment consistent with what would be seen in people with type 2 diabetes based on race and ethnicity. At baseline, just over half were using CGMs, 13 were using only basal insulin, and 17 were using both basal and pre-meal insulin. Most practices do not have the capacity to provide this level of support, especially where general practitioners may treat those with diabetes due to the limited number of subspecialists in a region. An additional level of complexity with technical support arises with multiple manufacturers contributing to a given AID system. For example, in the case of an unknown failure of an AID system built using components from different manufacturers, who should be contacted? Calls must be promptly answered, and multiple language options based on regional need should be easily chosen. Those employed to answer calls must be familiar with the given AID system so they can support the patient with most, if not all, questions regarding system use. The questions asked by the call center staff must be simple and nonconfrontational, as individuals with lower literacy, numeracy, and technical skills may not be able to provide detailed information. The most common concern that may arise could be whether the AID system or one of its components needs to be replaced. Trained call-line workers will need to help patients troubleshoot a given situation, help them check and change the pump settings, and potentially provide authorization for new components of the AID system to be sent if it is deemed that the current system is not functioning as intended. Potential AID system issues may include repeated loss of data transfer from the transmitter of the CGM system or an insulin pump that has a cracked screen. However, this requires that the patient have the choice of different AID systems available in the country and through the health care system. Just as CSII offers a plethora of options of different insulin pumps, IIS, and other components, it is anticipated that a number of AID systems will be commercially available in the not-too-distant future. Paramount to having an open dialogue with the patient in considering therapeutic options is presenting information in a standardized and adequate manner. Ideally, the patient would have the chance to evaluate different AID systems before making a decision for a given system. With certain differences in technology and handling of AID systems currently available, a systematic approach for defining how each advanced diabetes technology works has been proposed. A: Adjust—How can the user adjust insulin delivery, which parameters can be adjusted to influence insulin delivery during automation, and which parameters are fixed? With conventional CSIIs, the same parameters for system setup are held constant across a range of devices; however, this does not hold true for AID systems. Two approaches exist for AID targets: a treat-to-target AID system that has a singular set point e. Conversely, for treat-to-range systems there are CGM values between which the system tries to maximize the TIR e. Thus, the first step may be understanding which type of target a given AID system uses, followed by assessment of the threshold at which these targets are set. While it is beyond the scope of practice for most clinicians to understand all the intricacies of how each AID algorithm works, it will be critical as AID systems are more widely adopted for HCPs to know which parameters can be adjusted to optimize insulin delivery. To date, all AID systems allow for adjustment of the insulin-to-carbohydrate ratio except Diabeloop DLBG1, which uses machine learning to optimize the meal ratio on an ongoing basis. Some of the newer AID systems on the market will give automated correction boluses, while others may not. The strategy for determining the dose allowed to be given by automated correction, as well as the frequency with which these autocorrections can be provided, will differ by system. Indeed, without comprehension of what parameters are adjustable, some clinicians may alter settings that have no impact on AID, thereby increasing frustration of both patients and providers in their experience with the product. With commercialization of AID systems, companies should seek to include materials that clearly delineate the settings that can be adjusted. Companies should also provide clinical scenarios to highlight when such optimization would be needed and how to successfully implement the changes. Providers will need to inform patients of when AID systems may automatically revert to manual mode i. Thus, it is a good practice to update these manual settings intermittently while patients are using AID systems, as overall insulin needs may be changing, particularly in the pediatric population. Should such features not be available, it may be critical to consider altering the low-glucose thresholds and predictive low alerts when not using the AID feature so that the patient with diabetes can manually respond to the hypoglycemic event. It may not be prudent to continue with AID in certain situations, and patients may be instructed to revert to conventional CSII. These situations include illness, when there may be temporarily increased insulin resistance and elevated glucose levels, as well as reduction in oral intake and ketosis without elevated glucose levels. Resolution of ketones will be contingent on increased insulin delivery; however, this may not be possible if a patient is solely relying on the AID system. Likewise, should a clinical situation arise in which treatment necessitates use of systemic steroids, it is possible that the AID system does not respond rapidly enough to account for the increased insulin requirements often necessitated with steroids. Finally, the lower targets needed in pregnancy may not be achievable on an AID system. Given that AID systems are new in diabetes care and subject to ongoing rapid development, many practitioners may not be fully aware of how to teach individuals with diabetes how to use them. As a result, manufacturers may need to provide training either directly to patients or diabetes care and education specialists or by means of online videos. The pandemic has highlighted that this education can be delivered in person or remotely With the initiation of AID, patients should be provided with clear instructions on how to ensure data are available for providers to view i. Particularly during early use, providers will need to take a more proactive approach than with previous nonintegrated insulin pumps. Although teaching tools for medical devices like AID systems include user guides, these are often not easy to read. They are hundreds of pages long, and the chances that patients and even HCPs will read them are slim. In the case of troubleshooting, often it is not easy to find appropriate support. Many learn from videos, which, if available, are often very helpful. However, such teaching tools need to be available in multiple languages, created for learners of all skill levels, and sensitive to the inclusion of people from varying ethnicities. Communication with the HCP may be through the use of interpreter services in case of language barriers. Undoubtedly, there will be a steep learning curve as use of AID systems becomes more prevalent. Patient acceptance and safety will come through education and adjustments to ensure safe use. For people with diabetes whose management strategies have been primarily focused on permissive hyperglycemia, the return to more targeted glucose levels may lead to the sensation of hypoglycemia. Instructions on this phenomenon and encouragement that the threshold for symptoms will be lowered may help patients adapt to this transitional period as they initiate AID therapy. Providers will need to understand how to access data so that dose optimization on AID systems can be made. They may need to assure they have programs installed for local uploading of devices in their offices. There is a call for standardized reports for AID data, similar to the standardized reports that have been created for CGM data Just as consistent terminology Table 1 use can help clarify for all what a given system does or does not do, standardized reports will help ensure easy readability of the data for individuals with diabetes as well as their provider. AID holds the promise to improve care for all individuals living with diabetes who require insulin. However, the vast majority of studies to date have focused on those with T1D 45 — Nevertheless, for people meeting their individualized treatment goals without excess burden or distress, usage of AID systems may not be an appropriate therapy, and recognition of the choice to not use an AID system is important. The current evidence base is mostly built on studies where selected participants were able to engage with self-management and had received structured education or an equivalent level of support, which may impact the outcome of these studies and therefore their generalizability. There is a need for well-conducted studies in populations who differ from those included in the studies, who may, in some cases, be most apt to benefit. However, more data from real-world studies were published recently e. A handful of studies have demonstrated the short-term benefit of systems in patients with type 2 diabetes T2D 52 — Indeed, for people with T2D whose endocrine pancreatic function mimics those with T1D, such as those with lower serum C-peptide levels, usage of AID systems may prove to be the optimal way to attain glycemic targets while avoiding hypoglycemia. Additionally, application of AID systems for patients with insulin dependency following pancreatitis or those with cystic fibrosis—related diabetes may be warranted, since improvements in lung function are noted when dysglycemia is treated For young children, the ability of parents to remotely view both CGM data and insulin delivery is critical. Similarly, for older adults in assisted living facilities, such remote monitoring tools may be of great help. Additionally, in both of these circumstances, it may be best to have only basic functionality on the insulin pump itself in order to prevent errant and unwanted bolus insulin delivery. However, as youth with diabetes achieve greater independence in their care, access to greater functionality of AID systems is likely to be appropriate over time. Including an option for the HCP to individualize pump settings for this purpose is recommended. Different insulin pumps have regulatory approval for different age ranges, and this must be considered in prescribing an AID system 18 , Some older studies suggested that dilution of rapid-acting insulin analogs may allow for a reduction in the frequency of hypoglycemic events 57 , 58 ; however, in a more recent outpatient assessment in this age-group a benefit was not seen with dilution Transition from pediatric to adult diabetes care requires specific attention. While youth may have relied on parents at an earlier stage, increasing autonomy of care is essential during transition This will require specific training—or retraining—on how AID systems work at an appropriate time prior to transition to an adult provider. In patients who may experience acute metabolic events where insulin sensitivity can change rapidly e. Assessment of these situations in a standardized manner to determine safety of various devices would be prudent. Evidence is now emerging regarding use of AID systems during times where insulin action time may be changing due to reduced or changed insulin clearance e. Finally, pregnancy poses a unique situation, as the targets for glycemia are inherently much more ambitious 12 , Early studies in pregnancy have demonstrated the ability of AID systems to improve glycemia 63 — However, in these studies, women continued to perform self-monitoring of blood glucose SMBG multiple times daily. In the Continuous Glucose Monitoring in Women With Type 1 Diabetes in Pregnancy Trial CONCEPTT , fetal outcomes were evaluated in comparison of CGM plus SMBG monitoring with SMBG alone Clear benefits were illustrated in those on sensor therapy However, no benefit in glycemia was seen in those preparing for pregnancy. Moreover, data on outcomes are lacking from individuals with preexisting T2D or gestational diabetes mellitus. Because pregnancy glycemic targets are currently lower than the targets allowed by most commercially available AID systems, it is important to follow glycemic guidelines for pregnant women and find the best method for achieving these outcomes in an individual patient. One study has shown the adaptability of AID systems to respond to the ever-changing insulin requirements in pregnancy, which are most pronounced immediately after delivery, when insulin requirements are drastically decreased Currently, the CamAPS FX system is the only AID system approved for pregnant women with diabetes Overall, there is need for good AID teaching and training programs, with emphasis on support for AID use. This should be curriculum driven, evidence based, and based on sound education principles. As previously described, there are many obvious advantages for using AID systems, but there are also some important limitations of the current and near-future AID systems. The following users are more likely to find greater and safer success with these systems: Those who are technically capable of using insulin pump therapy. Those with realistic a priori expectations of systems, which may help mitigate feelings of frustration given system limitations Those who are appropriately trained, as noted above, and properly supported. Ideally, they have a social environment supporting them and insurance coverage of AID systems. They also should have the ability to transmit their ongoing AID data to the health care professional team. Those mentally and psychologically able to fulfill the requirements for successful AID implementation. People with diabetes and eating disorders or severe psychiatric comorbidities e. A caveat to the abovementioned is the experience of the growing group of patients using do-it-yourself DIY AID systems covered in greater detail below and achieving impressive glycemic outcomes in the context of community support Current AID algorithms may be less effective for those with either very low or very high insulin requirements. Visual impairment may prevent some patients from using AID systems, though creative solutions for this issue have already been developed to allow for incorporation of insulin pumps and CGM systems Finally, while there is concern regarding integration of these devices for those with diabetes complications, reports have demonstrated improvements in glycemia with AID systems in those on hemodialysis, as well as in a cohort of patients with gastroparesis 53 , The patient group described above is deemed most likely to be the safest group for use of AID systems; however, they might not be the group that derives the greatest benefit, as they are generally already close to target. Therapeutic options like CGM and CSII have the greatest impact on HbA 1c and hypoglycemia exposure in patients with T1D, with the highest HbA 1c values and the greatest exposure to hypoglycemia due to diabetes burnout or issues with self-management. Therefore, it might well be that the usage of AID systems by such individuals has the greatest incremental benefit from a clinical point of view and, thereby, also the highest cost effectiveness. A key challenge for AID systems will be moving beyond those who are already at targeted glycemia i. While these individuals may only see small incremental changes in glycemia, clear benefits in diabetes burden may be feasible with AID. The desire to address inequalities between different populations with diabetes cannot be reconciled with criteria with selection of only the safest patients. Requirements for clinical safety of AID systems are similar to those seen with CGM systems and insulin pumps but also go beyond those. In individuals with T1D, safety issues encompass both hypoglycemic events and diabetic ketoacidosis. Such events can be induced by system malfunctioning e. Use of the AID system during situations with high risk for hypoglycemia e. An important question to consider is how to become aware of safety issues. Are currently implemented mechanisms to detect safety issues adequate? In cases when a person with diabetes encounters such issues and contacts the device manufacturer, the company must report these safety concerns to certain databases, such as the Manufacturer and User Facility Device Experience MAUDE in the U. Although market observations can provide insight into certain issues if they are reported several times, there are currently no systematic observation and analysis methods established to detect these trends. Nevertheless, when issues are detected, they can result in product recalls. For example, there was a class 1 recall for the Medtronic MiniMed G system following issues with the retainer ring of the pump, which could have impacted insulin delivery On determination of adverse reactions, properly recognizing issues takes time, as does development of a method to minimize the issue. For example, it took time to identify the development of skin reactions secondary to the frequent use of diabetes devices, which has proven to be a serious issue faced by many. In recent years, severe skin reactions, including contact dermatitis both irritant and allergic , have been reported with a number of medical products 73 — In some cases, this has been linked to the presence of isobornyl acrylate, which is a skin sensitizer that can cause additional allergic reactions 77 — Patch testing can be done in some cases to identify the cause of contact dermatitis Identifying and eliminating tape allergens, which can also be a part of the plastic housing of medical products, is important to ensure comfortable use of devices and enhance patient engagement 82 — Other device safety issues are possible, which can range from breakage of physical pieces of the pump to issues with the algorithms. Additionally, there can be errors in the representation of data downloaded from the system. All of these issues need to be handled and monitored in an efficient and effective manner. Being up to date on any recalls and device safety updates is critical for patients and providers alike. Furthermore, it is up to all patients and providers to report issues to regulatory agencies, such as the FDA via MAUDE, to ensure that channels to identify issues are properly used. Diligence with reporting will help keep everyone informed of potential problems as they arise. Another critical issue is cybersecurity and data privacy. Potential vulnerability of AID systems is increased by the multiplicity of component devices that comprise AID systems. Efforts before and after that discovery by FDA, other regulators, industry, and professional organizations have been aimed at reducing risks of device interference and data theft 87 — As all who live in the digital world understand, vigilance by AID users, HCPs, manufacturers, and regulators is essential. Continuous testing of AID components and systems for cybersecurity, as well as ongoing development of technological safeguards, must be ongoing. Usage of the data generated in using AID systems is a critically important issue. Also, the much larger number of patients and enormous amounts of data generated by real-world studies are of interest. The question is whether patients are aware of what happens to their data. Although patients have to sign an agreement about data usage, that does not necessarily equate to understanding of the agreement. In contrast, if patients are willing to donate their data for research e. Whether insurance companies can use AID data to modify insurance coverage remains an open question, if they can get access to these data of individual patients. If CGM data are identifiable, can users refuse to share their data with HCPs? Is there a risk to doing so? Another sensitive situation may be the availability of CGM and AID data in court rulings, such as when an individual with diabetes is involved in a car accident and the court finds out that relevant data covering that time period might be available. The question as to whether the person was able to handle the AID system adequately may arise. Could data be downloaded to prove what occurred i. Did the user override system recommendations or use the system in ways that were not intended, thus leading to the incident, or did the AID not work as intended despite user engagement? Are data holders forced to provide this information without the consent of the person with diabetes? Furthermore, companies may be legally liable regarding particular laws depending on where the company headquarters is, as well as where AID devices are manufactured and cloud servers are located. For example, the legal frameworks for data protection are different between Europe and the U. In Europe, the sensitivity for data privacy is high. Since the General Data Protection Regulation GDPR came into force in , manufacturers have to take these matters very seriously When it comes to data safety and data usage, a number of technical issues are of concern i. Only when data can be assessed in a standardized manner can the data generated by the AID systems be integrated into electronic health records. With regard to data protection, one has to realize that the availability of data on CGM or AID use discloses a diagnosis of diabetes, which may have a negative impact on employment or access to insurance. In general, the regulation of medical devices in the U. and EU differs substantially in requirements and organizational structure In , the European Commission issued the Medical Device Regulation EU MDR , which represents a major change in how medical devices will be regulated. The implementation of EU MDR started in May Traditionally medical devices, but not necessarily diabetes-related products, have reached the market sooner in the EU than in the U. The EU MDR may have the effect of reducing differences in data requirements and marketing approval times. The FDA has been highly supportive of diabetes device development through the release of clear and detailed guidance. The FDA has been especially supportive of the development of AID systems over the last decade starting with its guidance This FDA guidance document describes multiple forms of flexibility for developing AID products including with regard to 1 use of CGM systems, 2 primary end points that can be used to measure safety and effectiveness, 3 the stated therapeutic indication, 4 clinical study progression, and 5 the size and duration of each study phase. This guidance explicitly expresses the intent of applying the least burdensome approach to investigating and developing AIDs and making them available to patients. The FDA has also approved AID systems rapidly. Later the Libre 2 by Abbott also got this status. Importantly, this approval had the effect of changing the risk category for iCGM products from class III to class II while stipulating conditions and special controls to ensure safe interoperability. This new provision also enables bringing future iCGM systems to market with the least burdensome requirements possible. This was the first controller device that could be used with other interoperable devices and integrated into a customizable diabetes management system for AID A self-contained AID product can still be developed and approved as noninteroperative. Such products could require a more burdensome Premarket Approval PMA process. The EU does not have an interoperable diabetes device pathway comparable with that in the U. Technical documentation can demonstrate conformance with the essential requirements at the product or system level, but it must take into account system components and interactions used to achieve the intended purpose. Therefore, the manufacturer of a system component defines the interoperability with other components. This results in the availability of AID system components intended to be combined only with other specified system components e. In contrast with the FDA as the single national agency for device approval in the U. As noted above, the EU MDR brings a higher burden for the manufacturer with respect to technical documentation and clinical evaluation. It should be noted that a number of questions and issues related to AID remain to be addressed by the notified bodies and the EU Commission. A key question with respect to the EU MDR regulation is, in what risk categories will AID systems and components be placed, class IIb or class III? Four different options for AID systems are conceivable as follows: A fully integrated system i. A system that combines products of different manufacturers e. DIY AID systems that are built by people with diabetes using commercially available hardware combined with an algorithm downloaded from the internet, for which no regulatory approval is available. The second and third types of AID systems might belong to a different risk class than the first. AID systems are viewed as requiring special attention, since they involve infusion of a therapeutic product, insulin, which has a narrow therapeutic index. Such products are scrutinized more intensively. In the case where components of different manufacturers are combined i. Another question is how the safety and efficacy of the different combinations can be meaningfully demonstrated to the satisfaction of the emerging EU MDR. Patients with diabetes will be expected to use the device according to the instructions for use provided by the manufacturer, and these instructions will need to be clear, transparent, and understandable. With regard to DIY AID systems, the French Competent Authority National Agency for the Safety of Medicines and Health Products ANSM has published a recommendation that people with diabetes not use software and applications that offer DIY AID systems, indicating that these applications usually do not have the CE mark and expose users to risks 95 , Such an approach requires that system components be able to exchange data. The U. left the EU trading bloc in January with a transition period until the end of However, the U. Medicines and Healthcare products Regulatory Agency MHRA has issued guidance that generally harmonizes with EU MDR requirements i. Since 1 January , all medical devices placed on the U. market need to be registered with MHRA a grace period existed until September for pumps and CGM systems , but CE marking and certificates issued by EU-recognized notified bodies will continue to be recognized in the U. until June Any manufacturer based outside the U. will need to appoint a single U. For the time being, the costs of AID systems are high, which is a main reason why, from a global perspective, most people with T1D do not yet realistically have access. An important factor to consider is the costs of devices, as well as coverage of devices by insurance companies, which varies widely between countries. This means out-of-pocket costs can be vastly different, and access to particular devices may be restricted in some regions, even if the devices have achieved regulatory approval. Fortunately, use of modern diabetes technology is increasingly being covered by health care systems given the proven benefits they bring for many people with diabetes. However, coverage includes not only the up-front costs of AID systems but also ongoing supply costs for IIS, batteries, and insulin, as well as increasing use of cell phones and adequate Wi-Fi coverage for transmitting data to health care professionals. Furthermore, AID systems require extensive use of nonmonetary resources, such as up-front education of the users. Patients must also have access to HCPs who can support and troubleshoot a given AID system when the need arises, such as malfunction of a component or interruptions in the supply chain. In view of the costs associated with widespread use of AID systems, insurers will likely request more cost-effectiveness studies, which will also be dependent on baseline characteristics of individuals with diabetes. Even with adjustment for socioeconomic status and access to care, health care disparities in outcomes exist for those from minority populations Patients with lower incomes often face multiple issues that limit their ability to adopt technology, including insulin pumps and CGM systems 99 , not to mention complex AID systems. These issues include lack of consistent access to health care, insufficient or inconsistent coverage for devices, lower literacy and numeracy skills, lack of access to healthy food, psychosocial stressors, language barriers, and other issues related to social determinants of health that make diabetes management extremely challenging. Furthermore, implicit bias may affect who is offered such devices , |
| Automated Insulin Delivery Shows Promise in Type 2 Diabetes | Stylish and easy to operate, this insulin pump seamlessly integrates into your life like a sophisticated, modern smart device. With just a few taps on your t:slim X2 pump, you can view your insulin delivery and glucose history. You can also upload your pump data wirelessly to your Tandem Diabetes Care account so you and your doctor can easily view the data during a visit. Using CGM allows you to enable predictive technology, which helps manage insulin delivery — all to more confidently live your life. Our automated insulin delivery system predicts and helps prevent highs and lows to help increase time in range. Test drive the easy-to-use interfaces of either Tandem Mobi or t:slim X2 automated insulin delivery systems, with no obligation. Use Simulators. See what people are saying about the t:slim X2 insulin pump and how it is changing their lives for the better. Choose from a variety of cannula materials, tubing lengths, and insertion angles to fit your needs. We offer a wide range of accessories to personalize your insulin pump and match your unique lifestyle. Get Started. Systems like the t:slim X2 insulin pump with Basal-IQ technology and the t:slim X2 insulin pump with Control-IQ technology are not substitutes for active diabetes management. For example, users still must bolus for meals. Basal-IQ technology is designed to predict and help prevent lows, but it cannot prevent all lows and Basal-IQ technology does not predict high glucose events. Be sure to always use your pump, cartridges, CGM, and infusion sets as instructed and check them regularly to make sure they are working properly. Data on file, Tandem Diabetes Care. Control-IQ technology is available only to customers who reside in the United States or Canada, and other select geographies. Software updates are only available to customers who are in warranty at the time they update their pump. Additional training may be required to access certain future software updates. Charges may apply. Tandem may discontinue select software and features over time at its discretion. RX ONLY. If bolusing postprandially, some patients may need to reduce the meal bolus to account for the insulin already provided by the AID system. Patients are also expected to announce any upcoming physical activity to avoid hypoglycemia. Concern exists that patients transitioning to AID systems may become less skilled in dosing insulin as they rely more heavily on their technology. Thus, it will be essential that patients, as well as providers, understand that like any technology, components of AID systems can fail. When hyperglycemia occurs, patients may need to return to fundamental diabetes management, such as assessing ketones and considering whether an IIS occlusion or failure has led to the hyperglycemia. They will need clear instructions on how to restore normoglycemia, even possibly returning to conventional continuous subcutaneous insulin infusion CSII or insulin injection therapy so preprogrammed basal rates are used and appropriate correction doses can be administered. Contingency planning should include access to batteries, charging cables, IIS, reservoirs, a vial of insulin, syringes or insulin pens and needles , a glucose meter and test strips, glucagon, ketone test strips, and a backup glucose sensor and transmitter for the CGM system. In addition, a plan for transition to insulin injection therapy, as well as a supply of unexpired insulin pens or vials with rapid-acting and long-acting insulins, should be available for use until a replacement for the AID system is available. It is also critical to consider potential disruption in availability of supplies, as has been noted during the coronavirus disease era. For example, if there is a supply issue with glucose sensors or transmitters, if the sensors or transmitters do not last for their intended duration of time, or if there is a change in insurance plans and a prior authorization is required, individuals with diabetes may find themselves running out of supplies. Furthermore, traveling can be exceptionally challenging, especially if key components break unexpectedly. Thus, it is essential to always have a backup subcutaneous insulin therapy plan, as described above. Devices that require charging through USB electric cable can be difficult to charge in certain regions e. Medical imaging can also be a challenge because certain scans e. IIS can stay in place, but removing the glucose sensor can be a problem if sensors are in short supply. However, the recommendations for removing CGM systems are based on caution, largely in the absence of data from device testing under these conditions. In at least one simulation it was found that CGM can stay in place during radiographic and MRI procedures 38 , Discussions regarding treatment of hypoglycemic events in patients using an AID system need to highlight that since basal insulin will be suspended, fewer carbohydrates will need to be consumed to return to euglycemia. Even though hypoglycemia can be corrected with fewer carbohydrates, people with diabetes need to be educated to overcome fear of hypoglycemia and avoid overcorrecting hypoglycemia, which often causes hyperglycemia with the use of AID systems. Also, AID users have noticed anecdotally that the AID system assumes that the person with diabetes is still in a state of hypoglycemia with delivery suspension long after the hypoglycemia has been corrected with rapid-acting glucose, and people with diabetes find themselves experiencing hyperglycemia 30—40 min after having corrected hypoglycemia even if they use fewer carbs. Since AID systems increase insulin delivery based on elevated glucose levels, patients may find they are limited in the manual correction bolus that can be given. Helping patients understand that this is due to insulin being proactively delivered by the AID system may help minimize frustration in the initial transition period. Educating patients with diabetes on AID system functionality and how to determine whether insulin delivery is being increased or suspended may allow for trust to be established with this automated process. Indeed, for those who have achieved targeted glycemia with traditional CSII or multiple daily insulin injections, delegating the decision-making process to this new technology may be difficult. Education also needs to focus on the different modes that these AID systems have. The most common feature allows the AID algorithm to adapt, for example, to exercise. Alternatively, overnight algorithms may allow some systems to tighten targets, thereby allowing for more aggressive insulin delivery. As commercial AID systems become more widely used, education regarding what to do with an urgent question will be crucial. There should be a clear distinction between technical support delivered by the manufacturer and clinical support delivered by the clinical support team. Such a helpline should be staffed by people with specific diabetes experience, i. Most practices do not have the capacity to provide this level of support, especially where general practitioners may treat those with diabetes due to the limited number of subspecialists in a region. An additional level of complexity with technical support arises with multiple manufacturers contributing to a given AID system. For example, in the case of an unknown failure of an AID system built using components from different manufacturers, who should be contacted? Calls must be promptly answered, and multiple language options based on regional need should be easily chosen. Those employed to answer calls must be familiar with the given AID system so they can support the patient with most, if not all, questions regarding system use. The questions asked by the call center staff must be simple and nonconfrontational, as individuals with lower literacy, numeracy, and technical skills may not be able to provide detailed information. The most common concern that may arise could be whether the AID system or one of its components needs to be replaced. Trained call-line workers will need to help patients troubleshoot a given situation, help them check and change the pump settings, and potentially provide authorization for new components of the AID system to be sent if it is deemed that the current system is not functioning as intended. Potential AID system issues may include repeated loss of data transfer from the transmitter of the CGM system or an insulin pump that has a cracked screen. However, this requires that the patient have the choice of different AID systems available in the country and through the health care system. Just as CSII offers a plethora of options of different insulin pumps, IIS, and other components, it is anticipated that a number of AID systems will be commercially available in the not-too-distant future. Paramount to having an open dialogue with the patient in considering therapeutic options is presenting information in a standardized and adequate manner. Ideally, the patient would have the chance to evaluate different AID systems before making a decision for a given system. With certain differences in technology and handling of AID systems currently available, a systematic approach for defining how each advanced diabetes technology works has been proposed. A: Adjust—How can the user adjust insulin delivery, which parameters can be adjusted to influence insulin delivery during automation, and which parameters are fixed? With conventional CSIIs, the same parameters for system setup are held constant across a range of devices; however, this does not hold true for AID systems. Two approaches exist for AID targets: a treat-to-target AID system that has a singular set point e. Conversely, for treat-to-range systems there are CGM values between which the system tries to maximize the TIR e. Thus, the first step may be understanding which type of target a given AID system uses, followed by assessment of the threshold at which these targets are set. While it is beyond the scope of practice for most clinicians to understand all the intricacies of how each AID algorithm works, it will be critical as AID systems are more widely adopted for HCPs to know which parameters can be adjusted to optimize insulin delivery. To date, all AID systems allow for adjustment of the insulin-to-carbohydrate ratio except Diabeloop DLBG1, which uses machine learning to optimize the meal ratio on an ongoing basis. Some of the newer AID systems on the market will give automated correction boluses, while others may not. The strategy for determining the dose allowed to be given by automated correction, as well as the frequency with which these autocorrections can be provided, will differ by system. Indeed, without comprehension of what parameters are adjustable, some clinicians may alter settings that have no impact on AID, thereby increasing frustration of both patients and providers in their experience with the product. With commercialization of AID systems, companies should seek to include materials that clearly delineate the settings that can be adjusted. Companies should also provide clinical scenarios to highlight when such optimization would be needed and how to successfully implement the changes. Providers will need to inform patients of when AID systems may automatically revert to manual mode i. Thus, it is a good practice to update these manual settings intermittently while patients are using AID systems, as overall insulin needs may be changing, particularly in the pediatric population. Should such features not be available, it may be critical to consider altering the low-glucose thresholds and predictive low alerts when not using the AID feature so that the patient with diabetes can manually respond to the hypoglycemic event. It may not be prudent to continue with AID in certain situations, and patients may be instructed to revert to conventional CSII. These situations include illness, when there may be temporarily increased insulin resistance and elevated glucose levels, as well as reduction in oral intake and ketosis without elevated glucose levels. Resolution of ketones will be contingent on increased insulin delivery; however, this may not be possible if a patient is solely relying on the AID system. Likewise, should a clinical situation arise in which treatment necessitates use of systemic steroids, it is possible that the AID system does not respond rapidly enough to account for the increased insulin requirements often necessitated with steroids. Finally, the lower targets needed in pregnancy may not be achievable on an AID system. Given that AID systems are new in diabetes care and subject to ongoing rapid development, many practitioners may not be fully aware of how to teach individuals with diabetes how to use them. As a result, manufacturers may need to provide training either directly to patients or diabetes care and education specialists or by means of online videos. The pandemic has highlighted that this education can be delivered in person or remotely With the initiation of AID, patients should be provided with clear instructions on how to ensure data are available for providers to view i. Particularly during early use, providers will need to take a more proactive approach than with previous nonintegrated insulin pumps. Although teaching tools for medical devices like AID systems include user guides, these are often not easy to read. They are hundreds of pages long, and the chances that patients and even HCPs will read them are slim. In the case of troubleshooting, often it is not easy to find appropriate support. Many learn from videos, which, if available, are often very helpful. However, such teaching tools need to be available in multiple languages, created for learners of all skill levels, and sensitive to the inclusion of people from varying ethnicities. Communication with the HCP may be through the use of interpreter services in case of language barriers. Undoubtedly, there will be a steep learning curve as use of AID systems becomes more prevalent. Patient acceptance and safety will come through education and adjustments to ensure safe use. For people with diabetes whose management strategies have been primarily focused on permissive hyperglycemia, the return to more targeted glucose levels may lead to the sensation of hypoglycemia. Instructions on this phenomenon and encouragement that the threshold for symptoms will be lowered may help patients adapt to this transitional period as they initiate AID therapy. Providers will need to understand how to access data so that dose optimization on AID systems can be made. They may need to assure they have programs installed for local uploading of devices in their offices. There is a call for standardized reports for AID data, similar to the standardized reports that have been created for CGM data Just as consistent terminology Table 1 use can help clarify for all what a given system does or does not do, standardized reports will help ensure easy readability of the data for individuals with diabetes as well as their provider. AID holds the promise to improve care for all individuals living with diabetes who require insulin. However, the vast majority of studies to date have focused on those with T1D 45 — Nevertheless, for people meeting their individualized treatment goals without excess burden or distress, usage of AID systems may not be an appropriate therapy, and recognition of the choice to not use an AID system is important. The current evidence base is mostly built on studies where selected participants were able to engage with self-management and had received structured education or an equivalent level of support, which may impact the outcome of these studies and therefore their generalizability. There is a need for well-conducted studies in populations who differ from those included in the studies, who may, in some cases, be most apt to benefit. However, more data from real-world studies were published recently e. A handful of studies have demonstrated the short-term benefit of systems in patients with type 2 diabetes T2D 52 — Indeed, for people with T2D whose endocrine pancreatic function mimics those with T1D, such as those with lower serum C-peptide levels, usage of AID systems may prove to be the optimal way to attain glycemic targets while avoiding hypoglycemia. Additionally, application of AID systems for patients with insulin dependency following pancreatitis or those with cystic fibrosis—related diabetes may be warranted, since improvements in lung function are noted when dysglycemia is treated For young children, the ability of parents to remotely view both CGM data and insulin delivery is critical. Similarly, for older adults in assisted living facilities, such remote monitoring tools may be of great help. Additionally, in both of these circumstances, it may be best to have only basic functionality on the insulin pump itself in order to prevent errant and unwanted bolus insulin delivery. However, as youth with diabetes achieve greater independence in their care, access to greater functionality of AID systems is likely to be appropriate over time. Including an option for the HCP to individualize pump settings for this purpose is recommended. Different insulin pumps have regulatory approval for different age ranges, and this must be considered in prescribing an AID system 18 , Some older studies suggested that dilution of rapid-acting insulin analogs may allow for a reduction in the frequency of hypoglycemic events 57 , 58 ; however, in a more recent outpatient assessment in this age-group a benefit was not seen with dilution Transition from pediatric to adult diabetes care requires specific attention. While youth may have relied on parents at an earlier stage, increasing autonomy of care is essential during transition This will require specific training—or retraining—on how AID systems work at an appropriate time prior to transition to an adult provider. In patients who may experience acute metabolic events where insulin sensitivity can change rapidly e. Assessment of these situations in a standardized manner to determine safety of various devices would be prudent. Evidence is now emerging regarding use of AID systems during times where insulin action time may be changing due to reduced or changed insulin clearance e. Finally, pregnancy poses a unique situation, as the targets for glycemia are inherently much more ambitious 12 , Early studies in pregnancy have demonstrated the ability of AID systems to improve glycemia 63 — However, in these studies, women continued to perform self-monitoring of blood glucose SMBG multiple times daily. In the Continuous Glucose Monitoring in Women With Type 1 Diabetes in Pregnancy Trial CONCEPTT , fetal outcomes were evaluated in comparison of CGM plus SMBG monitoring with SMBG alone Clear benefits were illustrated in those on sensor therapy However, no benefit in glycemia was seen in those preparing for pregnancy. Moreover, data on outcomes are lacking from individuals with preexisting T2D or gestational diabetes mellitus. Because pregnancy glycemic targets are currently lower than the targets allowed by most commercially available AID systems, it is important to follow glycemic guidelines for pregnant women and find the best method for achieving these outcomes in an individual patient. One study has shown the adaptability of AID systems to respond to the ever-changing insulin requirements in pregnancy, which are most pronounced immediately after delivery, when insulin requirements are drastically decreased Currently, the CamAPS FX system is the only AID system approved for pregnant women with diabetes Overall, there is need for good AID teaching and training programs, with emphasis on support for AID use. This should be curriculum driven, evidence based, and based on sound education principles. As previously described, there are many obvious advantages for using AID systems, but there are also some important limitations of the current and near-future AID systems. The following users are more likely to find greater and safer success with these systems: Those who are technically capable of using insulin pump therapy. Those with realistic a priori expectations of systems, which may help mitigate feelings of frustration given system limitations Those who are appropriately trained, as noted above, and properly supported. Ideally, they have a social environment supporting them and insurance coverage of AID systems. They also should have the ability to transmit their ongoing AID data to the health care professional team. Those mentally and psychologically able to fulfill the requirements for successful AID implementation. People with diabetes and eating disorders or severe psychiatric comorbidities e. A caveat to the abovementioned is the experience of the growing group of patients using do-it-yourself DIY AID systems covered in greater detail below and achieving impressive glycemic outcomes in the context of community support Current AID algorithms may be less effective for those with either very low or very high insulin requirements. Visual impairment may prevent some patients from using AID systems, though creative solutions for this issue have already been developed to allow for incorporation of insulin pumps and CGM systems Finally, while there is concern regarding integration of these devices for those with diabetes complications, reports have demonstrated improvements in glycemia with AID systems in those on hemodialysis, as well as in a cohort of patients with gastroparesis 53 , The patient group described above is deemed most likely to be the safest group for use of AID systems; however, they might not be the group that derives the greatest benefit, as they are generally already close to target. Therapeutic options like CGM and CSII have the greatest impact on HbA 1c and hypoglycemia exposure in patients with T1D, with the highest HbA 1c values and the greatest exposure to hypoglycemia due to diabetes burnout or issues with self-management. Therefore, it might well be that the usage of AID systems by such individuals has the greatest incremental benefit from a clinical point of view and, thereby, also the highest cost effectiveness. A key challenge for AID systems will be moving beyond those who are already at targeted glycemia i. While these individuals may only see small incremental changes in glycemia, clear benefits in diabetes burden may be feasible with AID. The desire to address inequalities between different populations with diabetes cannot be reconciled with criteria with selection of only the safest patients. Requirements for clinical safety of AID systems are similar to those seen with CGM systems and insulin pumps but also go beyond those. In individuals with T1D, safety issues encompass both hypoglycemic events and diabetic ketoacidosis. Such events can be induced by system malfunctioning e. Use of the AID system during situations with high risk for hypoglycemia e. An important question to consider is how to become aware of safety issues. Are currently implemented mechanisms to detect safety issues adequate? In cases when a person with diabetes encounters such issues and contacts the device manufacturer, the company must report these safety concerns to certain databases, such as the Manufacturer and User Facility Device Experience MAUDE in the U. Although market observations can provide insight into certain issues if they are reported several times, there are currently no systematic observation and analysis methods established to detect these trends. Nevertheless, when issues are detected, they can result in product recalls. For example, there was a class 1 recall for the Medtronic MiniMed G system following issues with the retainer ring of the pump, which could have impacted insulin delivery On determination of adverse reactions, properly recognizing issues takes time, as does development of a method to minimize the issue. For example, it took time to identify the development of skin reactions secondary to the frequent use of diabetes devices, which has proven to be a serious issue faced by many. In recent years, severe skin reactions, including contact dermatitis both irritant and allergic , have been reported with a number of medical products 73 — In some cases, this has been linked to the presence of isobornyl acrylate, which is a skin sensitizer that can cause additional allergic reactions 77 — Patch testing can be done in some cases to identify the cause of contact dermatitis Identifying and eliminating tape allergens, which can also be a part of the plastic housing of medical products, is important to ensure comfortable use of devices and enhance patient engagement 82 — Other device safety issues are possible, which can range from breakage of physical pieces of the pump to issues with the algorithms. Additionally, there can be errors in the representation of data downloaded from the system. All of these issues need to be handled and monitored in an efficient and effective manner. Being up to date on any recalls and device safety updates is critical for patients and providers alike. Furthermore, it is up to all patients and providers to report issues to regulatory agencies, such as the FDA via MAUDE, to ensure that channels to identify issues are properly used. Diligence with reporting will help keep everyone informed of potential problems as they arise. Another critical issue is cybersecurity and data privacy. Potential vulnerability of AID systems is increased by the multiplicity of component devices that comprise AID systems. Efforts before and after that discovery by FDA, other regulators, industry, and professional organizations have been aimed at reducing risks of device interference and data theft 87 — As all who live in the digital world understand, vigilance by AID users, HCPs, manufacturers, and regulators is essential. Continuous testing of AID components and systems for cybersecurity, as well as ongoing development of technological safeguards, must be ongoing. Usage of the data generated in using AID systems is a critically important issue. Also, the much larger number of patients and enormous amounts of data generated by real-world studies are of interest. The question is whether patients are aware of what happens to their data. Although patients have to sign an agreement about data usage, that does not necessarily equate to understanding of the agreement. In contrast, if patients are willing to donate their data for research e. Whether insurance companies can use AID data to modify insurance coverage remains an open question, if they can get access to these data of individual patients. If CGM data are identifiable, can users refuse to share their data with HCPs? Is there a risk to doing so? Another sensitive situation may be the availability of CGM and AID data in court rulings, such as when an individual with diabetes is involved in a car accident and the court finds out that relevant data covering that time period might be available. The question as to whether the person was able to handle the AID system adequately may arise. Could data be downloaded to prove what occurred i. Did the user override system recommendations or use the system in ways that were not intended, thus leading to the incident, or did the AID not work as intended despite user engagement? Are data holders forced to provide this information without the consent of the person with diabetes? Furthermore, companies may be legally liable regarding particular laws depending on where the company headquarters is, as well as where AID devices are manufactured and cloud servers are located. For example, the legal frameworks for data protection are different between Europe and the U. In Europe, the sensitivity for data privacy is high. Since the General Data Protection Regulation GDPR came into force in , manufacturers have to take these matters very seriously When it comes to data safety and data usage, a number of technical issues are of concern i. Only when data can be assessed in a standardized manner can the data generated by the AID systems be integrated into electronic health records. With regard to data protection, one has to realize that the availability of data on CGM or AID use discloses a diagnosis of diabetes, which may have a negative impact on employment or access to insurance. In general, the regulation of medical devices in the U. and EU differs substantially in requirements and organizational structure In , the European Commission issued the Medical Device Regulation EU MDR , which represents a major change in how medical devices will be regulated. The implementation of EU MDR started in May Traditionally medical devices, but not necessarily diabetes-related products, have reached the market sooner in the EU than in the U. The EU MDR may have the effect of reducing differences in data requirements and marketing approval times. The FDA has been highly supportive of diabetes device development through the release of clear and detailed guidance. The FDA has been especially supportive of the development of AID systems over the last decade starting with its guidance This FDA guidance document describes multiple forms of flexibility for developing AID products including with regard to 1 use of CGM systems, 2 primary end points that can be used to measure safety and effectiveness, 3 the stated therapeutic indication, 4 clinical study progression, and 5 the size and duration of each study phase. This guidance explicitly expresses the intent of applying the least burdensome approach to investigating and developing AIDs and making them available to patients. The FDA has also approved AID systems rapidly. Later the Libre 2 by Abbott also got this status. Importantly, this approval had the effect of changing the risk category for iCGM products from class III to class II while stipulating conditions and special controls to ensure safe interoperability. This new provision also enables bringing future iCGM systems to market with the least burdensome requirements possible. This was the first controller device that could be used with other interoperable devices and integrated into a customizable diabetes management system for AID A self-contained AID product can still be developed and approved as noninteroperative. Such products could require a more burdensome Premarket Approval PMA process. The EU does not have an interoperable diabetes device pathway comparable with that in the U. Technical documentation can demonstrate conformance with the essential requirements at the product or system level, but it must take into account system components and interactions used to achieve the intended purpose. Therefore, the manufacturer of a system component defines the interoperability with other components. This results in the availability of AID system components intended to be combined only with other specified system components e. In contrast with the FDA as the single national agency for device approval in the U. As noted above, the EU MDR brings a higher burden for the manufacturer with respect to technical documentation and clinical evaluation. It should be noted that a number of questions and issues related to AID remain to be addressed by the notified bodies and the EU Commission. A key question with respect to the EU MDR regulation is, in what risk categories will AID systems and components be placed, class IIb or class III? Four different options for AID systems are conceivable as follows: A fully integrated system i. A system that combines products of different manufacturers e. View Topic. Font Size Small Normal Large. Continuous subcutaneous insulin infusion insulin pump. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Ruth S Weinstock, MD, PhD Section Editor: Irl B Hirsch, MD Deputy Editor: Katya Rubinow, MD Literature review current through: Jan This topic last updated: Jan 29, Basal insulin can be delivered by daily or twice-daily injections of an intermediate-acting neutral protamine Hagedorn [NPH] or long-acting glargine, detemir, degludec insulin preparation or by continuous subcutaneous insulin infusion CSII via a pump using a rapid-acting or faster rapid-acting insulin preparation lispro, aspart, glulisine. |
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden es besprechen.
Sie sind nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.
Diese bemerkenswerte Idee fällt gerade übrigens