
You may need a Vegan comfort food of tests. Your doctor will also Mens health supplements you about your medical history and your diseasd history and will perform a physical exam.
The Anti-oxidation benefits of treatment diseasw to Digeztive Digestive health and Crohns disease inflammation in your diseasd, to prevent Immune system support strategies of your symptoms, and to Athletic performance assessment you in Digestivd.
Changing your diet can help reduce Crihns. Depending on your symptoms or medicines, your Digestive health and Crohns disease may recommend a specific diet, abd as diseaes diet that is diseasd calorie, lactose free, or low fat. The National Institute Immune system support strategies Diabetes and Corhns and Kidney Diseases NIDDK Cfohns other components of the National Institutes Immune system support strategies Digestjve NIH conduct and support research into many diseases and Digestive health and Crohns disease.
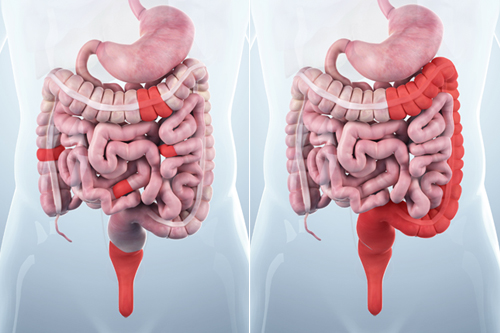
The Crohnx system is made up of the Dkgestive GI tract-also called Insulin pump therapy considerations digestive tract-and Digestive health and Crohns disease liver, Muscular strength and agility, and the gallbladder.
The GI tract is a series of Immune system support strategies organs joined in a long, twisting tube from the mouth to Immune system support strategies anus. See more about digestive diseases research at NIDDK. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDKpart of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public.
Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. Home Health Information Digestive Diseases Crohn's Disease. English English Español. Anatomic Problems of the Lower GI Tract Show child pages.
Appendicitis Show child pages. Barrett's Esophagus Show child pages. Bowel Control Problems Fecal Incontinence Show child pages. Celiac Disease Show child pages.
Chronic Diarrhea in Children Show child pages. Colon Polyps Show child pages. Constipation Show child pages. Constipation in Children Show child pages.
Cyclic Vomiting Syndrome Show child pages. Diarrhea Show child pages. Diverticular Disease Show child pages. Dumping Syndrome Show child pages.
Exocrine Pancreatic Insufficiency EPI Show child pages. Food Poisoning Show child pages. Gallstones Show child pages. Gas in the Digestive Tract Show child pages.
Gastrointestinal GI Bleeding Show child pages. Gastroparesis Show child pages. Hemorrhoids Show child pages. Hirschsprung Disease Show child pages. Indigestion Dyspepsia Show child pages. Intestinal Pseudo-obstruction Show child pages. Irritable Bowel Syndrome IBS Show child pages.
Irritable Bowel Syndrome in Children Show child pages. Lactose Intolerance Show child pages. Microscopic Colitis Show child pages.
Ostomy Surgery of the Bowel Show child pages. Pancreatitis Show child pages. Peptic Ulcers Stomach and Duodenal Ulcers Show child pages. Proctitis Show child pages. Short Bowel Syndrome Show child pages. Ulcerative Colitis Show child pages. Clinical Trials The National Institute of Diabetes and Digestive and Kidney Diseases NIDDK and other components of the National Institutes of Health NIH conduct and support research into many diseases and conditions.
Related Diagnostic Tests Colonoscopy Upper GI Series Upper GI Endoscopy. Related Research See more about digestive diseases research at NIDDK.
: Digestive health and Crohns disease| Content Map Terms | Previously, dosease and stress were suspected, but Balanced meals and snacks Digestive health and Crohns disease know that these factors may aggravate but aren't the cause Ceohns IBD. pdf [accessed 3 September ]. Calcium is important to protect bones. Crohn's Disease Also called: Regional enteritis, Regional ileitis. This content does not have an Arabic version. We will respond to you via email within 3 buisness days. |
| Definition & Facts for Crohn’s Disease | Please do dsease submit personal Natural antioxidant foods or Diggestive on behalf of someone else Crohna you are the parent or guardian of Immune system support strategies minor who is Dgestive of acting healty their own behalf. Anemia of Dgestive Kidney Disease End-Stage Digestive health and Crohns disease Failure Tolvaptan Inherited Kidney Disease - Oral Types of Kidney Stones Extracorporeal Shock Wave Lithotripsy ESWL for Kidney Stones Percutaneous Nephrolithotomy or Nephrolithotripsy for Kidney Stones Kidney Stones Advance Care Planning: Should I Stop Kidney Dialysis? The main treatment for Crohn's disease is medicine. Mayo Clinic Alumni Association. Most common is Crohn's disease that affects the ileum the part of the small intestine that joins the large intestine. Crohn's disease. Psychological stress also can heighten pain in the body, regardless of the source of pain. |
| Federated Search Page Form block | However, there is emerging or established evidence to support specialty diets for when IBD is in remission, when IBD is active and to treat complications of IBD. Diet may be used to treat arising problems that commonly occur in people with IBD. Both under- and over-nutrition overweight or obesity is common in people with IBD and can lead to fatigue, reduced quality of life, depression and may weaken response to medications. People with malnutrition are more likely to become sick and take longer to recover. This can also lead to increased risk of complications after surgery. Most women with IBD are able to have children and raise a family. People with inflammatory bowel disease IBD are more likely to experience significant mental health problems, such as depression and anxiety. People with IBD face challenges that can make life difficult. They may find themselves feeling down, worried and uncertain at times. This is a normal part of living with an illness which can be disruptive and unpredictable. Each of these can be improved with the help of exercise that suits your lifestyle. Regular weight-bearing exercise, such as brisk walking , jogging , dancing , aerobics or active team sports, is good for your bones. Outdoor exercise is especially valuable as this will increase your exposure to sunlight and boost your vitamin D production. Exercise can reduce stress by releasing endorphins, the chemicals in the brain that give you a sense of happiness and act as natural painkillers. Gentle exercise activities, such as yoga , can help improve the mind-body connection and lower stress , and may lead to decreased inflammation. This page has been produced in consultation with and approved by:. Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website. Skip to main content. Crohn's disease and ulcerative colitis. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. More than , Australians live with IBD and it is becoming more prevalent in the community. The most common symptoms during a flare are: abdominal pain frequent diarrhoea sometimes mixed with mucus and blood and need to use the toilet tiredness, fatigue raised temperature, fever loss of appetite, weight loss anaemia reduced level of blood cells. Tests may include: blood tests stool tests endoscopy bowel imagine and scans. The main types include: aminosalicylates corticosteroids immunosuppressants biologics antibiotics. Common types of surgery include: resection stricturoplasty creating a stoma. About ulcerative colitis Ulcerative colitis is a type of IBD that can cause inflammation and ulceration in the large intestine colon and rectum. Symptoms of ulcerative colitis Symptoms of ulcerative colitis can be different for each person and may be serious or mild. The most common symptoms during a flare are: abdominal pain frequent diarrhoea sometimes mixed with mucus and blood and urgent need to use the toilet often, tiredness, fatigue raised temperature, fever loss of appetite, weight loss, and anaemia reduced level of blood cells. Diagnosis of ulcerative colitis To know if you have ulcerative colitis you will need to be tested by a doctor. Treatment of ulcerative colitis Ulcerative colitis cannot currently be cured but for most people it can be well managed through medication, lifestyle choices and sometimes surgery. Medication Medications for ulcerative colitis are mainly used to reduce inflammation. The main types include: aminosalicylates corticosteroids immunosuppressants biologics Janus kinase inhibators thalidomide. Diet Diet has an important role to play in of many aspects of ulcerative colitis, including symptom management, ensuring nutritional adequacy and potentially treating active disease or supporting remission. Examples of dietary treatments include: high energy and protein diet oral vitamin and mineral supplementation low or moderate FODMAP diet supplementary treatment. Surgery Surgery for ulcerative colitis is a treatment not everyone will need. What causes Crohn's disease? Stress and eating certain foods don't cause the disease, but they can make your symptoms worse. Who is more likely to develop Crohn's disease? There are certain factors that may raise your risk of Crohn's disease: Family history of the disease. Having a parent, child, or sibling with the disease puts you at higher risk. This may double your risk of developing Crohn's disease. Certain medicines , such as antibiotics , birth-control pills , and nonsteroidal anti-inflammatory drugs NSAIDs such as aspirin or ibuprofen. These may slightly increase your chance of developing Crohn's. A high-fat diet. This may also slightly increase your risk of Crohn's. What are the symptoms of Crohn's disease? The most common symptoms include: Diarrhea Cramping and pain in your abdomen Weight loss Some other possible symptoms are: Anemia , a condition in which you have fewer red blood cells than normal Eye redness or pain Fatigue Fever Joint pain or soreness Nausea or loss of appetite Skin changes that involve red, tender bumps under the skin Stress and eating certain foods such as carbonated fizzy drinks and high-fiber foods may make some people's symptoms worse. What other problems can Crohn's disease cause? Crohn's disease can cause other problems, including: Intestinal obstruction , a blockage in the intestine Fistulas , abnormal connections between two parts inside of the body Abscesses , pus-filled pockets of infection Anal fissures, small tears in your anus that may cause itching, pain, or bleeding Ulcers, open sores in your mouth, intestines, anus, or perineum Malnutrition , when your body does not get the right amount of vitamins , minerals , and nutrients it needs Inflammation in other areas of your body, such as your joints, eyes, and skin How is Crohn's disease diagnosed? Your health care provider may use many tools to make a diagnosis: A medical history, which includes asking about your symptoms A family history A physical exam, including: Checking for bloating in your abdomen. Listening to sounds within your abdomen using a stethoscope. Tapping on your abdomen to check for tenderness and pain and to see if your liver or spleen is abnormal or enlarged. Various tests, including: Blood and stool tests. A colonoscopy. An upper GI endoscopy, a procedure in which your provider uses a scope to look inside your mouth, esophagus, stomach, and small intestine. Diagnostic imaging tests, such as a CT scan or an upper GI series. An upper GI series uses a special liquid called barium and x-rays. Drinking the barium will make your upper GI tract more visible on an x-ray. What are the treatments for Crohn's disease? You and your provider can work together to figure out which treatment is best for you: Medicines for Crohn's include various medicines that decrease the inflammation. Many of these medicines do this by reducing the activity of your immune system. Certain medicines can also help with symptoms or complications, such as nonsteroidal anti-inflammatory drugs and anti-diarrheal medicines. If your Crohn's causes an infection, you may need antibiotics. Bowel rest involves drinking only certain liquids or not eating or drinking anything. This allows your intestines to rest. You may need to do this if your Crohn's disease symptoms are severe. You get your nutrients through drinking a liquid, a feeding tube, or an intravenous IV tube. You may need to do bowel rest in the hospital, or you may be able to do it at home. It will last for a few days or up to several weeks. Surgery can treat complications and reduce symptoms when other treatments are not helping enough. The surgery will involve removing a damaged part of your digestive tract to treat: Fistulas Bleeding that is life threatening Intestinal obstructions Side effects from medicines when they threaten your health Symptoms when medicines do not improve your condition Changing your diet can help reduce symptoms. Your provider may recommend that you make changes to your diet, such as: Avoiding carbonated drinks Avoiding popcorn, vegetable skins, nuts, and other high-fiber foods Drinking more liquids Eating smaller meals more often Keeping a food diary to help identify foods that cause problems In some cases, your provider may ask you to go on a special diet, such as a diet that is: High calorie Lactose free Low fat Low fiber Low salt If you are not absorbing enough nutrients, you may need to take nutritional supplements and vitamins. National Institute of Diabetes and Digestive and Kidney Diseases. Start Here. Crohn's Disease National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish What Is Crohn's Disease? Gastrointestinal GI Bleeding National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish. Diagnosis and Tests. Treatments and Therapies. Living With. Related Issues. Crohn disease: MedlinePlus Genetics National Library of Medicine. Test Your Knowledge. |
| Crohn's Disease | Jump to content. Inflammation, ulcerations, strictures a narrowing that can cause blockage in the bowel , and bleeding are some of the serious clinical problems patients may experience. Sometimes a capsule endoscopy is a recommended diagnostic exam. The procedure involves swallowing a small capsule, which is the size of a large vitamin pill. Inside the capsule is a tiny wireless camera that takes more than 50, digital pictures as it passes through the small intestine. Images are transmitted to a recording device worn on a belt around your waist. This recording device saves the pictures for a specialist to look at and interpret at a later time. Our experienced doctors have performed more than 3, capsule endoscopies. Instead we can use a special type of CT scan, or we can perform a double balloon enteroscopy to view the small bowel. Double balloon enteroscopy is a specialty endoscopy, or scope test, which allows doctors to go deep into the small bowel. The technology includes the use of balloon attachments on a scope, which help move the scope through the small bowel to the affected area. Through the scope we can biopsy abnormalities or dilate strictures, if required. Prediabetes: Which Treatment Should I Use to Prevent Type 2 Diabetes? Diabetes: Living With an Insulin Pump Form for Carbohydrate Counting. Autism Down Syndrome: Helping Your Child Eat Independently Down Syndrome: Grooming and Hygiene Down Syndrome: Helping Your Child Learn to Walk and Use Other Motor Skills Down Syndrome: Helping Your Child Learn to Communicate Down Syndrome Dyslexia Conditions Related to Dyslexia Autism: Behavioural Training and Management Autism: Support and Training for the Family Unproven Treatments for Autism Caring for Adults With Autism Down Syndrome: Helping Your Child Avoid Social Problems Down Syndrome: Training and Therapy for Young People Down Syndrome: Helping Your Child Dress Independently Down Syndrome, Ages Birth to 1 Month Down Syndrome, Ages 1 Month to 1 Year Down Syndrome, Ages 1 to 5 Down Syndrome, Ages 5 to 13 Down Syndrome, Ages 13 to Anorexia: Learning New Eating Behaviours Anorexia: Learning to Trust Others Binge Eating Disorder Bulimia Nervosa Eating Disorders: Cultural and Social Factors Eating Disorders: Feeling Better About Yourself Eating Disorders: Malnutrition Tests Eating Disorders: Things That Put a Person at Risk. Absence Epilepsy Juvenile Myoclonic Epilepsy Temporal Lobe Epilepsy Focal Epilepsy Epilepsy: Simple Partial Seizures Epilepsy Epilepsy and Driving Epilepsy: Generalized Seizures Epilepsy: Generalized Tonic-Clonic Seizures Epilepsy: Myoclonic Seizures Epilepsy: Atonic Seizures Epilepsy: Tonic Seizures Epilepsy: Complex Partial Seizures Epilepsy Medicine Therapy Failure Stopping Medicine for Epilepsy Questions About Medicines for Epilepsy Epilepsy: Taking Your Medicines Properly. Sleep Apnea: Should I Have a Sleep Study? Peripheral Arterial Disease of the Legs Bradycardia Slow Heart Rate Types of Bradycardia Cardiac Device Monitoring Angioplasty for Peripheral Arterial Disease of the Legs Isolated Systolic High Blood Pressure Atrial Fibrillation: Should I Try Electrical Cardioversion? Change in Heartbeat Deep Vein Thrombosis Fast Heart Rate Heart Failure: Symptom Record Heart Failure: Compensation by the Heart and Body Heart Failure: Taking Medicines Properly Heart Failure: Watching Your Fluids Heart Failure: Avoiding Triggers for Sudden Heart Failure Heart Failure: Activity and Exercise Heart Tests: When Do You Need Them? Low Blood Pressure Hypotension Cardiac Arrest Heart Failure Daily Action Plan Premature Ventricular Contractions PVCs Heart Rate Problems: Should I Get a Pacemaker? Heart Rhythm Problems: Should I Get an Implantable Cardioverter-Defibrillator ICD? What to Do if Your Cardiac Device Is Recalled Venous Insufficiency Carotid Artery Stenting ICD: Living Well With It Diabetes: Lower Your Risk for Heart Attack and Stroke Pacemaker for Heart Failure Cardiac Resynchronization Therapy Heart Attack: How to Prevent Another One Stroke: How to Prevent Another One Sex and Your Heart Supraventricular Tachycardia: Should I Have Catheter Ablation? Acute Coronary Syndrome Aspirin: Should I Take Daily Aspirin to Prevent a Heart Attack or Stroke? Heart Failure: Should I Get a Pacemaker? Heart Failure: Should I Get an Implantable Cardioverter-Defibrillator ICD? Heart Valve Disease Myxoma Tumours of the Heart Aortic Dissection Heart Attack and Stroke Risk Screening High Blood Pressure: Checking Your Blood Pressure at Home Hypertensive Emergency Stroke Rehabilitation Treatment for Stroke-Related Spasticity Driving a Car After a Stroke Heart Failure: Avoiding Medicines That Make Symptoms Worse Stroke Recovery: Coping With Eating Problems Heart Murmur High Blood Pressure: Should I Take Medicine? Coronary Artery Disease: Should I Have Angioplasty for Stable Angina? Tyrell's Story: Taking Pills for High Blood Pressure Stroke Prevention: Should I Have a Carotid Artery Procedure? Atrial Fibrillation: Which Anticoagulant Should I Take to Prevent Stroke? Stroke: Should I Move My Loved One Into Long-Term Care? Atrial Fibrillation: Should I Take an Anticoagulant to Prevent Stroke? Smoking and Coronary Artery Disease. Hepatitis C: Your Risk for Cirrhosis Hepatitis E Hepatitis B Immune Globulin - Injection Heparin - Injection Fulminant Hepatitis Protect Yourself From Hepatitis A When Travelling Hepatitis A Viral Hepatitis Hepatitis C Hepatitis D Hepatitis B: How to Avoid Spreading the Virus Hepatitis B Hepatitis Panel Hepatitis B Treatment Recommendations Hepatitis B: Should I Be Tested? HIV Infection HIV Viral Load HIV: Stages of Infection Ways HIV Cannot Be Spread HIV and Exercise HIV: Giving Support HIV: Tips for Caregivers to Avoid Infection HIV: Preventing Other Infections When You Have HIV HIV Home Care Antiretroviral medicines for HIV Resistance to HIV Medicines HIV: Preventing Infections HIV: Antiretroviral Therapy ART Opportunistic Infections in HIV HIV: Taking Antiretroviral Drugs HIV: Non-Progressors and HIV-Resistant People HIV Screening HIV and Weight Loss HIV and Fatigue. Anthrax Avian Influenza Avoiding Infections in the Hospital Bacterial Infections of the Spine Bites and Stings: Flu-Like Symptoms Boric Acid for Vaginal Yeast Infection Caregiving: Reducing Germs and Infection in the Home Central Venous Catheter: Flushing Chickenpox Varicella Chickenpox: Preventing Skin Infections Chikungunya Fever Complicated Urinary Tract Infections Complications of Ear Infections Cranberry Juice and Urinary Tract Infections Dengue Fever Ear Infection: Should I Give My Child Antibiotics? Ear Infections Ebola or Marburg Virus Infection Ebola Virus Disease Enterovirus D68 EV-D68 Fever or Chills, Age 11 and Younger Fever or Chills, Age 12 and Older Fever Seizures Fever Temperatures: Accuracy and Comparison Feverfew for Migraines Fifth Disease Flu: Signs of Bacterial Infection Fungal Nail Infections Giardiasis Hand-Foot-and-Mouth Disease Kissing Bugs Measles Rubeola Middle East Respiratory Syndrome MERS Molluscum Contagiosum Monkeypox Mononucleosis Mono Mononucleosis Complications Mumps Nail Infection: Should I Take Antifungal Pills? Neutropenia: Preventing Infections Non-Surgical Nail Removal for Fungal Nail Infections Noroviruses Pleurisy Pneumonia Preventing Tetanus Infections Pseudomonas Infection Recurrent Ear Infections and Persistent Effusion Recurrent Vaginal Yeast Infections Respiratory Syncytial Virus RSV Infection Rotavirus Rubella German Measles Scarlet Fever Sexually Transmitted Infections Sexually Transmitted Infections: Genital Examination for Men Sexually Transmitted Infections: Symptoms in Women Sexually Transmitted Infections: Treatment Shingles Smallpox Sore Throat and Other Throat Problems Staph Infection Strep Throat Symptoms of Pelvic Infection Thrush Tick Bites: Flu-Like Symptoms Tinea Versicolor Tuberculosis TB Tuberculosis Screening Urinary Tract Infections UTIs in Older Adults Vaginal Yeast Infection: Should I Treat It Myself? Vaginal Yeast Infections Valley Fever West Nile Virus Zika Virus. Broken Collarbone Clavicle Shoulder Separation Frozen Shoulder Preventing ACL Injuries Living With a Spinal Cord Injury Classification of Spinal Cord Injuries Tendon Injury Tendinopathy Shin Splints Muscle Cramps Whiplash Fractured Rib. Osteochondritis Dissecans of a Joint Back to Work? Acute Kidney Injury Versus Chronic Kidney Disease Nephrotic Syndrome Uremia Kidney Stones: Should I Have Lithotripsy to Break Up the Stone? Chronic Kidney Disease Kidney Failure: When Should I Start Dialysis? Kidney Failure: Should I Start Dialysis? Anemia of Chronic Kidney Disease End-Stage Kidney Failure Tolvaptan Inherited Kidney Disease - Oral Types of Kidney Stones Extracorporeal Shock Wave Lithotripsy ESWL for Kidney Stones Percutaneous Nephrolithotomy or Nephrolithotripsy for Kidney Stones Kidney Stones Advance Care Planning: Should I Stop Kidney Dialysis? Kidney Disease: Medicines to Avoid Stages of Chronic Kidney Disease Medicines That Can Cause Acute Kidney Injury Donating a Kidney Kidney Stones: Medicines That Increase Your Risk. Breathing Problems: Using a Metered-Dose Inhaler Acute Respiratory Distress Syndrome ARDS Bronchiectasis Chest Problems Sildenafil 20 Mg Lungs - Oral Tadalafil Lungs - Oral Tests for Lung Infections COPD: Lung Volume Reduction Surgery Acute Bronchitis Respiratory Problems, Age 11 and Younger Respiratory Problems, Age 12 and Older Breathing Smoke or Fumes Pulmonary Lung Nodules Severe Acute Respiratory Syndrome SARS COPD's Effect on the Lungs Black Lung Disease Oral Breathing Devices for Snoring Spinal Cord Injury: Breathing Practice Breathing Problems: Using a Dry Powder Inhaler COPD: Clearing Your Lungs Collapsed Lung Pneumothorax Interactive Tool: Should I Consider Surgery for My Low Back Problem? COPD: Learning to Breathe Easier Lung Function in COPD COPD: Handling a Flare-Up Sarah's Story: Dealing With the Emotions From COPD Fran's Story: Finding Support When You Have COPD. Multiple Sclerosis: Alternative Treatments Multiple Sclerosis: Modifying Your Home Multiple Sclerosis: Bladder Problems Multiple Sclerosis MS Types of Multiple Sclerosis Multiple Sclerosis Progression Multiple Sclerosis: MRI Results Multiple Sclerosis: Mental and Emotional Problems Multiple Sclerosis: Questions About What to Expect Rehabilitation Programs for Multiple Sclerosis. Liraglutide - Injection Obesity Weight and Coronary Artery Disease Health Problems Associated With Adult Obesity Cardiac Rehabilitation: Weight and Resistance Training. Menopause: Should I Use Hormone Therapy HT? Abnormal Uterine Bleeding: Should I Have a Hysterectomy? PMS: Should I Try an SSRI Medicine for My Symptoms? Uterine Fibroids: Should I Have Uterine Fibroid Embolization? Menopause: Managing Hot Flashes Premature Ejaculation High-Risk Sexual Behaviour Object in the Vagina Periodic Limb Movement Disorder Military Sexual Trauma Sexual Problems in Women Female Genital Problems and Injuries Smoking: Sexual and Reproductive Problems. Acne: Should I See My Doctor? Hyperthyroidism: Should I Use Antithyroid Medicine or Radioactive Iodine? Thyroid Storm Hyperparathyroidism Thyroid - Oral Subclinical Hypothyroidism Hypothyroidism Hyperthyroidism: Graves' Ophthalmopathy Radioactive Iodine for Hyperthyroidism Hyperthyroidism Thyroid Nodules Thyroid Hormone Production and Function. Vertigo: Level 1 Easy Balance Exercises Vertigo: Level 2 Harder Balance Excercises Tracking Chart for Level 1 and Level 2 Excercises for Vertigo Brandt-Daroff Exercise for Vertigo Vertigo: Balance Exercise Vertigo: Walking Excercises. British Columbia Specific Information HealthLinkBC Dietitians can answer your questions about food and nutrition. Topic Contents Condition Basics Symptoms What Happens When to Call Examinations and Tests Treatment Overview Self-Care Medicines Related Information Credits. Condition Basics What is Crohn's disease? What causes it? What are the symptoms? How is it diagnosed? How is Crohn's disease treated? Symptoms The main symptoms of Crohn's disease are belly pain and diarrhea sometimes with blood. What Happens Complications of Crohn's disease Crohn's disease may cause sores, or ulcers, that tunnel through the intestine and into the nearby tissue. When to Call Call anytime you think you may need emergency care. For example, call if: Your stools are maroon or very bloody. You passed out lost consciousness. Call a doctor now if you have been diagnosed with Crohn's disease and you have one or more of the following: New or worse belly pain. Severe dehydration. New or worse nausea or vomiting. New or more blood in your stools. Not passing any stools or gas. Pus draining from the area around the anus, or pain and swelling in the anal area. Watch closely for changes in your health, and be sure to contact your doctor if: You have new or worse symptoms, such as your diarrhea gets worse. You are losing weight. You do not get better as expected. Examinations and Tests Your doctor will ask you about your symptoms and do a physical examination. Tests that may be done to diagnose or evaluate Crohn's disease include: Stool analysis. This test looks for blood and signs of infection in a sample of your stool. One or more imaging tests, such as a CT scan or an MRI. Colonoscopy or flexible sigmoidoscopy. In these tests, the doctor uses a thin, lighted tube to look inside the colon. A biopsy. The doctor takes a sample of tissue and tests it to find out if you have Crohn's disease or another disease, such as cancer. Barium X-rays of the small intestine or colon. Learn more Colonoscopy Computed Tomography CT Scan of the Body Magnetic Resonance Imaging MRI of the Abdomen Sigmoidoscopy Anoscopy, Proctoscopy Stool Analysis. Treatment Overview Your treatment will depend on the type of symptoms you have and how bad they are. Learn more Total Parenteral Nutrition TPN. Self-Care Take your medicines exactly as prescribed. Call your doctor or nurse advice line if you think you are having a problem with your medicine. You will get more details on the specific medicines your doctor prescribes. Do not take anti-inflammatory medicines, such as aspirin, ibuprofen Advil, Motrin , or naproxen Aleve. They may make your symptoms worse. Do not take any other medicines or natural health products without talking to your doctor first. Avoid foods that make your symptoms worse. These might include milk, alcohol, high-fibre foods, or spicy foods. It may help to keep a diary of foods that make symptoms worse. Make sure to get enough iron. Rectal bleeding may make you lose iron. Good sources of iron include beef, lentils, spinach, raisins, and iron-enriched breads and cereals. Drink liquid meal replacements if your doctor recommends them. These are high in calories and contain vitamins and minerals. Severe symptoms may make it hard for your body to absorb vitamins and minerals. Talk to a dietitian to make sure you are getting the nutrition, including vitamins and minerals, that you need. Do not smoke. Smoking makes Crohn's disease worse. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good. Stay up to date on all immunizations. Follow your doctor's cancer screening recommendations. Seek support from friends and family to help cope with Crohn's disease. The illness can affect all parts of your life. Get counselling if you need it. Medicines Medicines usually are the treatment of choice for Crohn's disease. They help to: Relieve symptoms. Promote healing of damaged tissues. Put the disease into remission. And they can keep it from flaring up again. Postpone the need for surgery. They include: Aminosalicylates. Your doctor may recommend these medicines during a flare-up or at other times. These treat infections that can occur with Crohn's disease. Your doctor may have you try these medicines if other medicines for Crohn's disease haven't worked for you. They usually stop symptoms and put the disease in remission. But they aren't used as long-term treatment to keep symptoms from coming back. Immune modulators. You may take these if other medicines don't work, if your symptoms come back when you stop taking steroid medicines, or if your symptoms come back often, even with treatment. Related Information Colorectal Cancer Diverticulitis Irritable Bowel Syndrome IBS Organ Transplant Probiotics Ulcerative Colitis. Credits Current as of: March 22, Current as of: March 22, Digestive system. About This Page General Feedback Email Link Physical Activity Services We appreciate your feedback. Feedback Regarding:. Your name:. Your email:. Do you want a reply? Leave this field blank. What is your message about? |
| Crohn's Disease and the Small Bowel | Do you want a reply? You can unsubscribe at any time. About this Site. There are many ways you can add physical activity to your healthy lifestyle, no matter your age or activity level. To see related medical services we offer, visit our Digestive and Liver Health overview page. In some people, the disease is only in the colon, which is part of the large intestine. |
0 thoughts on “Digestive health and Crohns disease”