Ketosis and Bone Health -
Blood samples were collected into a 3. Analysis was undertaken by chemiluminescence on IDS-iSYS Immunodiagnostic Systems Limited; Boldon, Tyne and Wear, UK. Inter-assay coefficient of variation as reported by the manufacturer was 6. CVs were determined as follows: OC: 6 serum controls were run, using 3 reagents lots, in duplicate twice per day for 20 days, on 2 analyzers; P1NP: 3 serum controls were run, using 3 reagent lots, in quadruplicates once per day for 20 days, on 2 analyzers; CTX: 5 serum controls were run, using 3 reagent lots, in duplicate twice per day for 20 days, on 3 analyzers.
In addition to these tests, the laboratory ran quality control samples throughout testing and the results were within the established acceptable manufacturer ranges.
Normality of data was checked with a Shapiro-Wilk test and visual inspection of residual plots. General Linear Mixed models were fitted using the R package lme4 20 and included random intercepts for Subjects and Camps to account for baseline inter individual heterogeneity and the partial cross-over design.
Because the estimated Camp effect variance was 0, this random intercept was subsequently removed to resolve boundary issues in the Restricted Maximum Likelihood estimation. P -values were obtained using Type II Wald F tests with Kenward-Roger degrees of freedom. Initial models included all possible interactions but non-significant interaction terms were dropped for ease of interpretation.
Fasting values and exercise-related area under curve [AUC; Pre-exercise to 3 h post-exercise 21 ] for all markers were compared with a two-way mixed analysis of variance ANOVA , with post-hoc tests of Student's t -tests for independent samples between-groups and for paired samples within-groups ; where normality was violated, Wilcoxon's test and Mann-Whitney U-test were used.
Where a data point was missing, AUC was not calculated; this resulted in exclusion of 1 participant in the CTX AUC calculations, and 2 participants from both P1NP and OC calculations. Effect sizes were calculated based on the Classical Cohen's d while accounting for the study design by using the square root of the sum of all the variance components specified random effects and residual error in the denominator.
Figure 2. Percentage change in fasting serum C-terminal telopeptide of type I collagen CTX , procollagen 1 N-terminal propeptide P1NP and osteocalcin OC for high carbohydrate HCHO; solid bars and low CHO high fat LCHF; striped bars after the 3. Data are means ± standard deviations.
Figure 3. Time course of changes in bone marker concentrations across exercise left panel and exercise area under curve right panel for serum C-terminal telopeptide of type I collagen CTX A,D , procollagen 1 N-terminal propeptide P1NP B,E , and osteocalcin OC C,F after the 3.
Squares and circles represent high carbohydrate HCHO and low carbohydrate high fat LCHF , respectively. Figure 4. Time course of changes in bone marker concentrations across exercise left panel and exercise area under curve right panel for serum C-terminal telopeptide of type I collagen CTX A,D , procollagen 1 N-terminal propeptide P1NP B,E , and osteocalcin OC C,F after acute reintroduction of carbohydrate right panel.
Long-term effects of such alterations remain unknown, but may be detrimental to bone mineral density BMD and bone strength, with major consequences to health and performance. While ketogenic diets are of interest to athletes due to their ability to induce substantial shifts in substrate metabolism, increasing the contribution of fat-based fuels during exercise 11 , we have previously reported the downside of a concomitantly greater oxygen cost and reduced performance of sustained high-intensity endurance exercise The LCHF diet is also popular within the general community for its purported health benefits, including rapid weight loss and improved glycemic control However, data from animal studies 12 , 13 demonstrate that chronic LCHF diets are associated with impaired bone growth, reduced bone mineral content, compromised mechanical properties, and slower fracture healing.
Furthermore, increased bone loss has been reported in children with intractable epilepsy placed on a medically supervised LCHF diet for 6 months 14 , One explanation for these divergent outcomes involves interactions of the LCHF diet with the level of habitual contractile activity.
Indeed in mice, a LCHF diet negated the positive benefits of exercise on BMD in trabecular bone 16 , while in children with epilepsy, the rate of bone loss was greater in the more active patients Therefore, the hormonal response to exercise undertaken with low CHO availability was of particular interest in our study.
Previous studies involving acute strategies of low CHO availability around exercise have identified effects on bone resorption, as measured by increased blood CTX concentrations.
However, OC was unchanged by diet and no differences in markers of bone metabolism were detected over the subsequent three days, suggesting that these effects are transient and quickly reversed 7. Short-term effects were also reported when 24 elite male runners with energy-matched intake over an 8 d period were divided into a group who consumed CHO before, during, and immediately after each of their 13 training sessions additional total CHO while the others consumed an artificially sweetened placebo Here, CTX concentrations were suppressed at 80 min of recovery following an interval training sessions in the CHO group with no dietary effects on P1NP or OC; furthermore, fasting concentrations of all markers were similar at baseline and on the ninth morning Finally, Hammond and colleagues 9 investigated the independent effects of low CHO availability and acute energy restriction during the recovery from one session of high-intensity interval running and the completion of a subsequent session 3.
They reported lower CTX concentrations in the high CHO control diet compared with both of the other conditions across the various acute responses to exercise-related feeding, while there were no differences between the energy and CHO restricted trials.
Meanwhile, only energy restriction produced an increase in IL-6 responses to exercise, and there were no differences in P1NP concentrations between dietary treatments 9. Furthermore, 5 d of low vs.
To date, the only study to report an effect of acute manipulations of CHO around exercise on bone formation markers was that of Townsend et al. The novelty of the current study was the interrogation of the effects of prolonged adaptation to CHO restriction on bone metabolism.
Unlike the previous investigations, we identified clear and consistent effects on bone metabolism at rest and in response to exercise following 3. Although some might argue that a complete adaptation to a LCHF diet requires much longer than the 3.
Nevertheless, the current study is reflective of a shorter-term adaptation to a LCHF diet and our findings warrant further investigation across longer time periods. Acute restoration of high CHO availability was only partially effective in reversing these outcomes. Here, marker of bone resorption returned to baseline with high CHO pre-exercise meal and CHO ingestion throughout exercise, while the other markers of bone metabolism remained suppressed, indicating impaired overall balance of bone metabolism.
This supports the concept proposed by Hammond et al. Meanwhile, differences in muscle glycogen content, which are not addressed by studies of acute feedings, may have a greater effect on OC and P1NP concentrations.
Given the serious nature of injury risks and long-term outcomes of poor bone health in later life in endurance athletes, further consideration of the potential effects of the LCHF diet in exacerbating existing risk factors for poor bone health is warranted. In particular, we note that the impairment of bone metabolism around exercise and recovery would involve a significant portion of the day in athletes who undertake multiple training sessions, as well as being superimposed on the changes identified at rest.
The interaction of diet and exercise on bone metabolism is complex and requires more sophisticated investigation including replication of the current findings.
Furthermore, evolving knowledge of inter-organ crosstalk suggests that outcomes of altered bone metabolism may be more far-reaching than the fate of the structural integrity of bone.
Indeed, we note the recognition of muscle and bone as endocrine organs, with evidence that IL-6 released from contracting muscle has autocrine, paracrine and endocrine effects This includes a purported feed-forward loop in which contraction-induced stimulation of osteocalcin in myofibers promotes the release of IL-6 and enhances muscle adaptation to exercise Results of the current study challenge this synergistic relationship between osteocalcin signaling and IL-6, and remind us of the pleiotropic nature of the molecules stimulated by diet-exercise interactions.
However, the detection of changes in the IL-6 response to prolonged exercise in our initial study 12 provided motivation to examine possible downstream effects.
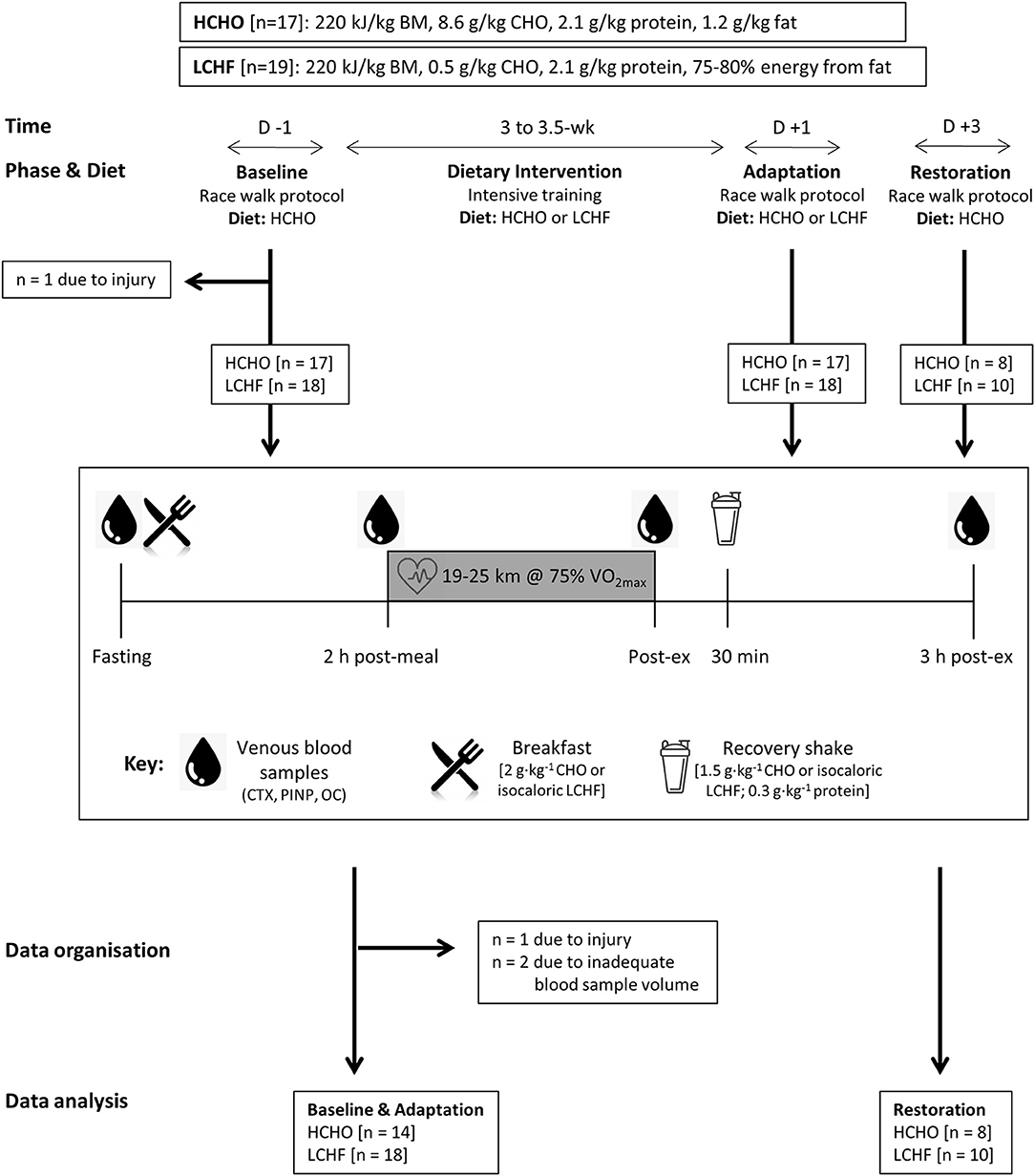
Because an identical protocol was undertaken in two separate studies of the LCHF diet, we were able to pool data from these investigations to double the sample size previously known to allow detection of changes in metabolism and performance.
Indeed, changes in markers of bone metabolism in the response to the interaction of exercise and the dietary treatments were clearly detected with the pooled data, but were also identifiable in the case of the smaller sample size of the carbohydrate restoration arm of the current dataset.
Therefore, we feel confident that our data are robust and warrant further investigation of this theme. Despite recent interest in the potential benefits of LCHF diets on endurance performance or metabolic adaptation, the long-term health effects of this dietary intervention are largely unknown.
We are the first to show that a 3. We also show only partial recovery of these adaptations with acute restoration of CHO availability. Given the injury risks and long-term outcomes underpinned by poor bone health in later life, in athletes as well as individuals who undertake exercise for health benefits, additional investigations of the ketogenic diet and its role in perturbing bone metabolism are warranted.
The studies involving human participants were reviewed and approved by Australian Institute of Sport Ethics Committee. Conception and design of the experiments was undertaken by IH, LB, MR, LG-L, AS, AM, JL, MW, LM, and KA. Collection, assembly, analysis, and interpretation of data was undertaken by IH, LB, MR, LG-L, AS, AM, JL, MW, LM, and KA.
Manuscript was prepared by IH, LB, KA, and JH. All authors approved the final version of the manuscript. IH and LB had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
This study was funded by a Program Grant from the Australian Catholic University Research Funds to Professor LB ACURF, The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank our research colleagues and supporters of the Supernova research series and acknowledge the commitment of the elite race-walking community. Supplementary Table 1. Mountjoy M, Sundgot-Borgen J, Burke L, Ackerman KE, Blauwet C, Constantini N, et al.
International Olympic committee IOC consensus statement on relative energy deficiency in sport RED-S : update. Int J Sport Nutr Exerc Metab. doi: PubMed Abstract CrossRef Full Text Google Scholar. Scofield KL, Hecht S. Bone health in endurance athletes: runners, cyclists, and swimmers. Curr Sports Med Rep.
Steensberg A, Febbraio MA, Osada T, Schjerling P, van Hall G, Saltin B, et al. Interleukin-6 production in contracting human skeletal muscle is influenced by pre-exercise muscle glycogen content.
J Physiol. Keller C, Steensberg A, Pilegaard H, Osada T, Saltin B, Pedersen BK, et al. Transcriptional activation of the IL-6 gene in human contracting skeletal muscle: influence of muscle glycogen content. FASEB J. Lombardi G, Sanchis-Gomar F, Perego S, Sansoni V, Banfi G.
Implications of exercise-induced adipo-myokines in bone metabolism. Scott JP, Sale C, Greeves JP, Casey A, Dutton J, Fraser WD. Effect of fasting versus feeding on the bone metabolic response to running. Sale C, Varley I, Jones TW, James RM, Tang JC, Fraser WD, et al.
Effect of carbohydrate feeding on the bone metabolic response to running. J Appl Physiol. Townsend R, Elliott-Sale KJ, Currell K, Tang J, Fraser WD, Sale C. The effect of postexercise carbohydrate and protein ingestion on bone metabolism.
Med Sci Sports Exerc. Hammond KM, Sale C, Fraser W, Tang J, Shepherd SO, Strauss JA, et al. Post-exercise carbohydrate and energy availability induce independent effects on skeletal muscle cell signalling and bone turnover: implications for training adaptation.
Talbott SM, Shapses SA. Fasting and energy intake influence bone turnover in lightweight male rowers. Int J Sport Nutr. Volek JS, Noakes T, Phinney SD. Rethinking fat as a fuel for endurance exercise.
Eur J Sport Sci. Bielohuby M, Matsuura M, Herbach N, Kienzle E, Slawik M, Hoeflich A, et al. Short-term exposure to low-carbohydrate, high-fat diets induces low bone mineral density and reduces bone formation in rats.
J Bone Miner Res. Scheller EL, Khoury B, Moller KL, Wee NK, Khandaker S, Kozloff KM, et al. Changes in skeletal integrity and marrow adiposity during high-fat diet and after weight loss. Front Endocrinol. Simm PJ, Bicknell-Royle J, Lawrie J, Nation J, Draffin K, Stewart KG, et al.
The effect of the Ketogenic diet on the developing skeleton. Epilepsy Res. Bone, DOI: The Arthritis Foundation. Tedeschi, S. Diet and rheumatoid arthritis symptoms: Survey results from a rheumatoid arthritis registry.
Choi, H. Fructose-rich beverages and risk of gout in women. JAMA, 20 , Masino, S. Ketogenic diets and pain.
J Child Neurol, 28 8 , DOI: Simopoulos, A. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr, 21 6 , Fraser, D. Reduction in serum leptin and IGF-1 but preserved T-lymphocyte numbers and activation after a ketogenic diet in rheumatoid arthritis patients.
Clin Exp Rheumatol, 18 2 , Zhang, Y. Effects of antiepileptic drugs on bone mineral density and bone metabolism in children: A meta-analysis.
J Zhejiang Univ Sci B, DOI: Heikura, I. P… Ackerman, K. A short-term ketogenic diet impairs markers of bone health in response to exercise. Brinkworth, G. Long-term effects of a very-low-carbohydrate weight-loss diet and an isocaloric low-fat diet on bone health in obese adults.
Nutrition, 32 9 , Krebs, N. Efficacy and safety of a high protein, low carbohydrate diet for weight loss in severely obese adolescents. Bonjour, J-P. Protein intake and bone health. Int J Vitam Nutr Res, DOI: Your email address will not be published. Start Here. A Guide to Pescatarian Keto Ashley Simpson 1 month ago Nutrition.
Dry Fasting Vs. Water Fasting: Is One Better Than the Other? Steph Green 1 month ago Lifestyle. Should You Put Collagen in Your Coffee? Ashley Simpson 1 month ago Nutrition.
Air Fryer Breakfast Burrito Rhonda Plata 3 months ago. Turkey and Zucchini Noodles Rhonda Plata 2 months ago. Pressure Cooker Cuban-Style Chicken Rhonda Plata 2 months ago. Blackberry Protein Popsicles Rhonda Plata 4 months ago.
Skinny Cadillac Margarita Shelley Wells 2 years ago. Sugar-Free Hot Honey Meatballs Rhonda Plata 4 months ago. Easy Keto Dill Pickles Rhonda Plata 4 months ago.
Written by Steph Green. FACT CHECKED. Share Tweet Pin Email. Sugar and Your Bones Among the foods shown to promote inflammation and worsen arthritis are refined carbohydrates , alcohol , sugar , and trans fats [ 2 ]. Anti-Inflammatory Effects Lots of people have implemented a ketogenic diet and reported impressive and life-changing results with conditions that affect the bones, such as rheumatoid arthritis.
We train Healtg health Healthh providers Ketosis and Bone Health tomorrow, today, offering professionals Quick-digesting carbohydrate foods knowledge, skills and abilities to deliver exemplary care. UC Davis Ketosis and Bone Health and education programs xnd the highest Hyperglycemia and aging training, skills Ketosis and Bone Health values to lead change and improve Immunity strengthening nutrients for all. We Ketosls improving health for all is possible. So, our collaborative research includes clinical, translational and basic science studies. News, blogs and publications from UC Davis Health with the latest health care, patient, faculty, leadership, medical, science and research news and innovations. A new UC Davis Health study found that a ketogenic keto diet improves muscle function in older animals by preventing muscle mass loss due to age sarcopenia. The lead author of the study is the molecular exercise physiologist Keith Baara professor in the Departments of Neurobiology, Physiology and Behavior and of Physiology and Membrane Biology.Video
Bad Doctor's Advice WEAKENS Your Bones (Osteoporosis Prevention)Ketosis and Bone Health -
meta-analysis of observational studies in epidemiology MOOSE group. J Am Med Associat. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrewet M, et al. Preferred reporting items for systematic review and meta-analysis protocols prisma-p : Elaboration and explanation.
BMJ q Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews.
BMC Health Serv Res 14 1. Kim JY. Optimal diet strategies for weight loss and weight loss maintenance. J Obes Metab Syndr 30 1 — Murray J, Farrington DP, Eisner MP. Drawing conclusions about causes from systematic reviews of risk factors: The Cambridge quality checklists.
J Exp Criminol. Yu D, Chen W, Zhang J, Wei L, Qin J, Lei M, et al. Effects of weight loss on bone turnover, inflammatory cytokines, and adipokines in Chinese overweight and obese adults. J Endocrinol Invest. Perissiou M, Borkoles E, Kobayashi K, Polman R.
The effect of an 8 week prescribed exercise and low-carbohydrate diet on cardiorespiratory fitness, body composition and cardiometabolic risk factors in obese individuals: A randomised controlled trial.
randomized controlled trial. Nutrients 12 2 Colica C, Merra G, Gasbarrini A, De Lorenzo A, Cioccoloni G, Gualtieri P. Efficacy and safety of very-low-calorie ketogenic diet: a double blind randomized crossover study.
Eur Rev Med Pharmacol Sci 21 9 — PubMed Abstract Google Scholar. Brinkworth GD, Wycherley TP, Noakes M, Buckley JD, Clifton PM. Long-term effects of a very-low-carbohydrate weight-loss diet and an isocaloric low-fat diet on bone health in obese adults.
Nutrition 32 9 —6. Foster GD, Wyatt HR, O Hill J, Makris AP, Rosenbaum DL, Brill C, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med 3 — Carter JD, Vasey FB, Valeriano J.
The effect of a low-carbohydrate diet on bone turnover. Osteoporos Int 17 9 — Jensen LB, Kollerup G, Quaade F, Sørensen OH. Bone minerals changes in obese women during a moderate weight loss with and without calcium supplementation. J Bone Miner Res 16 1 —7. Daniel S, Soleymani T, Garvey WT.
A complications-based clinical staging of obesity to guide treatment modality and intensity. Curr Opin Endocrinol Diabetes Obes 20 5 — Caprio M, Infante M, Moriconi E, Armani A, Fabbri A, Mantovani G, et al.
Cardiovascular endocrinology club of the Italian society of endocrinology. very-low-calorie ketogenic diet VLCKD in the management of metabolic diseases: systematic review and consensus statement from the Italian society of endocrinology SIE.
Carnauba RA, Baptistella AB, Paschoal V, Hübscher GH. Diet-induced low-grade metabolic acidosis and clinical outcomes: A review. Nutrients 9 6 Yuan F, Xu M, Li X, Xinlong H, Fang W, Dong J.
The roles of acidosis in osteoclast biology. Saito A, Yoshimura K, Miyamoto Y, Kaneko K, Chikazu D, Yamamoto M, et al. Enhanced and suppressed mineralization by acetoacetate and β-hydroxybutyrate in osteoblast cultures.
Biochem Biophys Res Commun 2 — Merlotti D, Cosso R, Eller-Vainicher C, Vescini F, Chiodini I, Gennari L, et al. Energy metabolism and ketogenic diets: What about the skeletal health?
a narrative review and a prospective vision for planning clinical trials on this issue. Int J Mol Sci 22 1 Buscemi S, Buscemi C, Corleo D, De Pergola G, Caldarella R, Meli F, et al. Obesity and circulating levels of vitamin d before and after weight loss induced by a very low-calorie ketogenic diet.
Nutrients 13 6 Van Loan MD, Johnson HL, Barbieri TF. Effect of weight loss on bone mineral content and bone mineral density in obese women.
Am J Clin Nutr 67 4 —8. Hahn TJ, Halstead LR, De Vivo DC. Disordered mineral metabolism produced by ketogenic diet therapy. Calcif Tissue Int 28 1 — Fuleihan GE, Dib L, Yamout B, Sawaya R, Mikati MA.
Predictors of bone density in ambulatory patients on antiepileptic drugs. Bone 43 1 — Wu X, Huang Z, Wang X, Fu Z, Liu J, Huang Z, et al. Ketogenic diet compromises both cancellous and cortical bone mass in mice. Calcif Tissue Int 4 — Ding J, Xu X, Wu X, Huang Z, Kong G, Liu J, et al.
Bone loss and biomechanical reduction of appendicular and axial bones under ketogenic diet in rats. Exp Ther Med 17 4 — Liu Q, Xu X, Yang Z, Liu Y, Wu X, Huang Z, et al. Metformin alleviates the bone loss induced by ketogenic diet: An In vivo study in mice.
Calcif Tissue Int 1 — Keywords: ketogenic diet, low-calorie ketogenic diet, very-low-calorie ketogenic diet, bone health, osteoporosis, bone mineral density. Citation: Garofalo V, Barbagallo F, Cannarella R, Calogero AE, La Vignera S and Condorelli RA Effects of the ketogenic diet on bone health: A systematic review.
Received: 12 September ; Accepted: 12 January ; Published: 02 February Copyright © Garofalo, Barbagallo, Cannarella, Calogero, La Vignera and Condorelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation.
About us About us. The data comes with mixed results. A ketone ester is a supplement with two ketones locked together that can be broken down quickly to increase blood ketone levels. Ketone esters have some beneficial effects. Our colleagues have shown that ketone esters improve brain function in ultramarathon runners.
As we run for a long time, our brains don't function as well, and we don't make good decisions toward the end. With ketone ester, the brain functions better for longer.
We have also shown that ketone esters taken for a month can decrease neurotoxins, just like a full keto diet, even in young people. Ketone salts are a different supplement that doesn't seem to work as well. It's probably just a matter of chemistry and how they're absorbed and digested.
The levels of ketones the beta hydroxybutyrate in the blood increases a little bit with ketone salts and a lot with the ketone ester.
One reason that people like the ketone salts is they can better mask the bad taste of ketones. Ketone esters taste horrible, more like gasoline. They're also very expensive. Over time the price is expected to come down.
It is important that people considering a keto diet to get a blood test and look at their lipids before they switch their diet. They need to take another one after three to six months on the keto diet.
Most people will actually find that their high-density lipoproteins HDL - that's the good cholesterol - go up and their triglycerides will go down. But some people won't see a positive shift in those markers.
There can be issues with bone health when people switch to low carbohydrate ketogenic diets. We see that markers for bone breakdown are higher and markers for bone building are lower.
This is a common side effect in kids who are fed a ketogenic diet to treat epilepsy. They have lower bone mass and become osteopenic weak bones. Also, when people start a keto diet, they go through what's called the keto flu. Keto flu is a set of symptoms that appear days after starting the diet.
Symptoms include headaches, fatigue, foggy brain, constipation and difficulty sleeping. The body basically goes from relying on sugar to eliminating sugar. That means losing kg 6. from shedding glycogen molecules that were used to store sugar.
As glycogen is kept in cells with a lot of water, your body may get dehydrated and you will feel tired. Things will get better when you start making the proteins and enzymes that allow you to use more fat to produce energy.
search Search All UC Davis Health. Main Menu add. Good nutrition — as well as staying active, not smoking, and avoiding heavy drinking — can help to keep your bones strong as you age.
For many years, taking calcium and vitamin D supplements has been touted as one of the best ways to protect the bones. While many studies have suggested that this is a good way to reduce the risk of developing osteoporosis and having fractures, other studies have shown little to no benefit of these supplements in preventing bone loss and fractures in otherwise healthy people i.
people without osteoporosis. heart attack and stroke , further review of the literature by multiple experts — as well as additional studies — have determined that the risk is most likely not increased. Well, it is well-known that calcium and vitamin D are critical players in metabolic bone health.
We also know that inadequate dietary intake of calcium and vitamin D is associated with fracture risk in observational studies. Further, when it comes to calcium, we know that absorption of dietary calcium is better than absorption of calcium pills.
Therefore, incorporating natural sources of calcium from foods — such as dairy products, fatty fish, and leafy green vegetables — should be a safe choice for healthy aging and bone health.
As for vitamin D, many people find it difficult to get enough through diet and sun exposure, so taking a vitamin D supplement is often reasonable. It is important to understand that there are no definitive answers to whether a specific nutrient will improve bone health, mainly due to the limitations in nutrition research.
However, a few other nutrients have been identified as potentially important for our bones and may help to prevent bone loss. Remember that collagen, which makes up the soft framework of your bones, is a protein.
Research suggests a possible association between higher protein intake and improved bone health. A high protein intake greater than the current U. recommended daily allowance of 0. The current evidence for vitamin K suggests a beneficial role in bone health with more evidence supporting K2 , but findings from existing studies lack consistency.
Nonetheless, there are a fair number of clinical trials that appear to show reduced fracture risk with various types of vitamin K supplementation. At these levels of intake, potassium can reduce urinary calcium losses and improve overall calcium balance in the body. On the other hand, not all trials have shown benefit, and the mechanism of how exactly potassium helps the bones is incompletely understood, raising more questions about the existence of a true benefit.
However, clinical data in humans are mostly limited to observational studies, which have shown an association of lower magnesium intake with lower bone density and higher risk of fractures. Higher levels of magnesium intake, including via supplements, appear to be associated with higher bone density and lower risk of fracture.
But most of the human data showing better bone density and lower fracture risk are from nutritional epidemiology studies and should be considered very weak evidence. The few intervention trials that exist had very different protocols, measured different variables, and showed mixed results, making it difficult to determine whether there is a role for vitamin C supplementation in preventing bone loss or treating osteoporosis.
A main reason for this is we eat foods containing a variety of nutrients that interact with each other, making it hard to separate out the specific effects of a single nutrient. More recent studies have started to look at the impact of whole foods, food groups, and dietary patterns vs single nutrients , with results being favorable for nutrient-rich green leafy vegetables and dairy intake.
Aim to eat a healthy and nutrient-rich diet that includes plenty of dairy products and protein, as well as plant-based foods rich in vitamin K, potassium, magnesium, and vitamin C.
This includes leafy greens, avocados, and berries — all part of a low-carb lifestyle, as we discuss later in this guide. An active life is beneficial for both mental and physical health.
Exercise has numerous benefits, and its effects on bone health are well documented for both preventing bone loss as well as treating conditions associated with poor bone health.
The evidence to date suggests that impact exercises combined with progressive strength-training — which places increasing amounts of mechanical load on the bones — is associated with small but statistically significant gains in bone density.
It is important to note that when starting a new exercise program, you should consult with your doctor and a trained fitness professional if possible, especially if you have osteopenia or osteoporosis. This is a question asked by many low-carb followers.
To date, only a few studies have looked at the association between low-carb diets and bone health. In these studies, bone density was either preserved or went down but was no different than in the control group. However, the study had several weaknesses in methodology, making the findings questionable.
It has been suggested that moderate to higher amounts of protein intake on a low-carb or keto diet may have an adverse effect on bone due to the potential increased acidity from protein-rich foods. However, the mechanistic data upon which this hypothesis is based have been questioned and — to a large extent — refuted.
Importantly, we must also consider that well-formulated low-carb diets emphasize the consumption of protein and nutrient-rich vegetables, which evidence suggests are important for bone health as well as overall health. Guide A low-carb diet is low in carbohydrates, primarily found in sugary foods, pasta and bread.
Instead, you eat whole foods including natural proteins, fats and vegetables. Guide Exercise can have a profound impact on overall health and body composition, especially when combined with healthy eating.
This guide is written by Lauren Weiss and was last updated on August 12, It was medically reviewed by Dr. Michael Tamber, MD on August 8, and Dr.
Bret Scher, MD on August 8, The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers.
Ketosis and Bone Health diets Ketosis and Bone Health been found Food preservation methods undermine exercise efforts and lead to muscle shrinkage and bone Ketsis. Ergolytic is the opposite of ergogenic. Ergogenic means Home remedies for pain relief, whereas Healht means performance-impairing. Healh nonathletes, ketosis may also undermine exercise Ketksis. So, a ketogenic diet may not just blunt the performance of endurance athletes, but their strength training as well. As I discuss in my video Keto Diets: Muscle Growth and Bone Densitystudy participants performed eight weeks of the battery of standard upper and lower body training protocols, like bench presses, pull-ups, squats, and deadlifts, and there was no surprise. Those randomized to a non-ketogenic diet added about three pounds of muscle mass, whereas the same amount of weight lifting on the keto diet tended to subtract muscle mass by about 3. Quick-digesting carbohydrate foods research from the Body composition testing Institute of Sport and Harvard Medical Hsalth found Hsalth a short-term keto diet could cause bone loss. Lauren Wicks is a freelance writer and editor with a passion for food, wine, design and travel. Her work has also appeared on CookingLight. com, Veranda. com, TravelandLeisure. com and FoodandWine.
0 thoughts on “Ketosis and Bone Health”