Glucagon secretion -
Lund A, Bagger JI, Albrechtsen NW, Christensen M, Grøndahl M, Hansen CP, Storkholm JH, Holst JJ, Vilsbøll T, Knop FK. Increased Liver Fat Content in Totally Pancreatectomized Patients. Unger RH. Glucagon physiology and pathophysiology in the light of new advances.
Miller RA, Birnbaum MJ. Glucagon: acute actions on hepatic metabolism. Ramnanan CJ, Edgerton DS, Kraft G, Cherrington AD. Physiologic action of glucagon on liver glucose metabolism. Diabetes Obes Metab. Rui L. Energy Metabolism in the Liver.
Compr Physiol. Geisler CE, Renquist BJ. Hepatic lipid accumulation: cause and consequence of dysregulated glucoregulatory hormones.
J Endocrinol. Longuet C, Sinclair EM, Maida A, Baggio LL, Maziarz M, Charron MJ, Drucker DJ. The Glucagon Receptor Is Required for the Adaptive Metabolic Response to Fasting. Cell Metabolism. Wang H, Zhao M, Sud N, Christian P, Shen J, Song Y, Pashaj A, Zhang K, Carr T, Su Q.
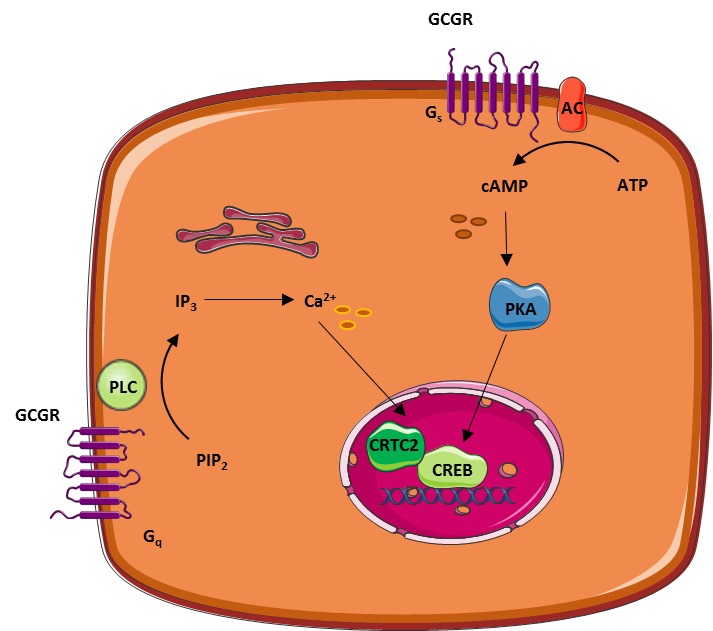
Glucagon regulates hepatic lipid metabolism via cAMP and Insig-2 signaling: implication for the pathogenesis of hypertriglyceridemia and hepatic steatosis.
Sci Rep. Galsgaard KD, Pedersen J, Knop FK, Holst JJ, Wewer Albrechtsen NJ. Glucagon Receptor Signaling and Lipid Metabolism. Front Physiol. Holst JJ, Albrechtsen NJW, Pedersen J, Knop FK. Glucagon and Amino Acids Are Linked in a Mutual Feedback Cycle: The Liver—α-Cell Axis. Hamberg O, Vilstrup H.
Regulation of urea synthesis by glucose and glucagon in normal man. Clin Nutr. Solloway MJ, Madjidi A, Gu C, Eastham-Anderson J, Clarke HJ, Kljavin N, Zavala-Solorio J, Kates L, Friedman B, Brauer M, Wang J, Fiehn O, Kolumam G, Stern H, Lowe JB, Peterson AS, Allan BB.
Glucagon Couples Hepatic Amino Acid Catabolism to mTOR-Dependent Regulation of α-Cell Mass. Cell Rep. Bagger JI, Holst JJ, Hartmann B, Andersen B, Knop FK, Vilsbøll T. J Clin Endocrinol Metab. Geary N, Kissileff HR, Pi-Sunyer FX, Hinton V. Individual, but not simultaneous, glucagon and cholecystokinin infusions inhibit feeding in men.
Langhans W, Zeiger U, Scharrer E, Geary N. Stimulation of feeding in rats by intraperitoneal injection of antibodies to glucagon.
Le Sauter J, Noh U, Geary N. Hepatic portal infusion of glucagon antibodies increases spontaneous meal size in rats. Nair KS. Hyperglucagonemia Increases Resting Metabolic Rate In Man During Insulin Deficiency.
Glucagon increases energy expenditure independently of brown adipose tissue activation in humans. Tan TM, Field BCT, McCullough KA, Troke RC, Chambers ES, Salem V, Gonzalez Maffe J, Baynes KCR, De Silva A, Viardot A, Alsafi A, Frost GS, Ghatei MA, Bloom SR.
Coadministration of Glucagon-Like Peptide-1 During Glucagon Infusion in Humans Results in Increased Energy Expenditure and Amelioration of Hyperglycemia. Fibroblast Growth Factor 21 Mediates Specific Glucagon Actions. Ceriello A, Genovese S, Mannucci E, Gronda E. Glucagon and heart in type 2 diabetes: new perspectives.
Cardiovasc Diabetol. Graudins A, Lee HM, Druda D. Calcium channel antagonist and beta-blocker overdose: antidotes and adjunct therapies. Br J Clin Pharmacol. Meidahl Petersen K, Bøgevig S, Holst JJ, Knop FK, Christensen MB.
Hemodynamic Effects of Glucagon - A Literature Review. Thuesen L, Christiansen JS, Sørensen KE, Orskov H, Henningsen P. Low-dose intravenous glucagon has no effect on myocardial contractility in normal man.
An echocardiographic study. Kazda CM. Treatment with the glucagon receptor antagonist LY increases ambulatory blood pressure in patients with type 2 diabetes. Lund A, Bagger JI, Christensen M, Grøndahl M, van Hall G, Holst JJ, Vilsbøll T, Knop FK.
Higher Endogenous Glucose Production During OGTT vs Isoglycemic Intravenous Glucose Infusion. Reaven GM, Chen YD, Golay A, Swislocki AL, Jaspan JB. Documentation of hyperglucagonemia throughout the day in nonobese and obese patients with noninsulin-dependent diabetes mellitus.
Dunning BE, Gerich JE. The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications. Hamaguchi T, Fukushima H, Uehara M, Wada S, Shirotani T, Kishikawa H, Ichinose K, Yamaguchi K, Shichiri M. Abnormal glucagon response to arginine and its normalization in obese hyperinsulinaemic patients with glucose intolerance: importance of insulin action on pancreatic alpha cells.
Knop FK. EJE PRIZE A gut feeling about glucagon. Lund A, Vilsbøll T, Bagger JI, Holst JJ, Knop FK. The separate and combined impact of the intestinal hormones, GIP, GLP-1, and GLP-2, on glucagon secretion in type 2 diabetes. Cryer PE. Minireview: Glucagon in the Pathogenesis of Hypoglycemia and Hyperglycemia in Diabetes.
Li K, Song W, Wu X, Gu D, Zang P, Gu P, Lu B, Shao J. Associations of serum glucagon levels with glycemic variability in type 1 diabetes with different disease durations. Hare KJ, Vilsbøll T, Holst JJ, Knop FK. Inappropriate glucagon response after oral compared with isoglycemic intravenous glucose administration in patients with type 1 diabetes.
American Journal of Physiology-Endocrinology and Metabolism. Diabetes Control and Complications Trial Research Group. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus.
Cryer PE, Gerich JE. Glucose counterregulation, hypoglycemia, and intensive insulin therapy in diabetes mellitus. Sprague JE, Arbeláez AM.
Glucose Counterregulatory Responses to Hypoglycemia. Pediatr Endocrinol Rev. Yosten GLC. Alpha cell dysfunction in type 1 diabetes. Knop FK, Aaboe K, Vilsbøll T, Vølund A, Holst JJ, Krarup T, Madsbad S.
Impaired incretin effect and fasting hyperglucagonaemia characterizing type 2 diabetic subjects are early signs of dysmetabolism in obesity. Albrechtsen NJW, Junker AE, Christensen M, Hædersdal S, Wibrand F, Lund AM, Galsgaard KD, Holst JJ, Knop FK, Vilsbøll T.
Hyperglucagonemia correlates with plasma levels of non-branched chained amino acids in patients with liver disease independent of type 2 diabetes. American Journal of Physiology - Gastrointestinal and Liver Physiology ajpgi.
Junker AE, Gluud L, Holst JJ, Knop FK, Vilsbøll T. Diabetic and nondiabetic patients with nonalcoholic fatty liver disease have an impaired incretin effect and fasting hyperglucagonaemia. J Intern Med. Suppli MP, Lund A, Bagger JI, Vilsbøll T, Knop FK. Involvement of steatosis-induced glucagon resistance in hyperglucagonaemia.
Tillner J, Posch MG, Wagner F, Teichert L, Hijazi Y, Einig C, Keil S, Haack T, Wagner M, Bossart M, Larsen PJ. A novel dual glucagon-like peptide and glucagon receptor agonist SAR Results of randomized, placebo-controlled first-in-human and first-in-patient trials.
Ambery P, Parker VE, Stumvoll M, Posch MG, Heise T, Plum-Moerschel L, Tsai L-F, Robertson D, Jain M, Petrone M, Rondinone C, Hirshberg B, Jermutus L. MEDI, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study.
The Lancet. Copyright © , MDText. Bookshelf ID: NBK PMID: PubReader Print View Cite this Page Rix I, Nexøe-Larsen C, Bergmann NC, et al. Glucagon Physiology. In: Feingold KR, Anawalt B, Blackman MR, et al. In this Page.
Links to www. View this chapter in Endotext. Related information. PMC PubMed Central citations. Similar articles in PubMed. Review Inhibition of glucagon secretion. Young A. Adv Pharmacol. Epub Apr Effects of dipeptidyl peptidase IV inhibition on glycemic, gut hormone, triglyceride, energy expenditure, and energy intake responses to fat in healthy males.
Heruc GA, Horowitz M, Deacon CF, Feinle-Bisset C, Rayner CK, Luscombe-Marsh N, Little TJ. Am J Physiol Endocrinol Metab. Epub Sep Review [Glucagon and glucagon-like peptides the role in control glucose homeostasis. A : Intraperitoneal i. B : Area under the curve AUC for A. C : Plasma glucagon at 0 and 30 min after i.
Statistics performed were unpaired t test B , E , H , J , K , and L and two-way ANOVA with the Šidák post hoc test C , F , and I. Pancreatic α-cells express K ATP channels 48 , The observation that glucose decreased intracellular ATP in the presence of NEFA therefore prompted us to investigate the electrical activity in α-cells under these experimental conditions.
The addition of 0. Unlike in control recordings without NEFA and BSA Fig. This could indicate that the reduction in ATP caused by increasing glucose levels leads to opening of K ATP channels and suggests that membrane potential in α-cells is more negative than previously reported Electrical activity 11 and FAs 40 have both been suggested to regulate glucagon secretion through changes in cytosolic calcium.
To investigate whether the addition of 0. This suggests that at low glucose, the membrane potential is depolarized and that increasing glucose repolarizes the plasma membrane to inhibit electrical activity, calcium entry, and glucagon secretion.
Glucose-induced reduction in ATP repolarizes the plasma membrane in α-cells. E : Representative trace of calcium oscillations in an α-cells in intact WT islets.
Statistics performed were one-way ANOVA with the Tukey C , D , and F post hoc test. Here we propose that the regulation of ATP production in α-cells is highly dependent on enzymes that promote FAO, such as PDK4 and CPT1a.
We find that inhibition of pyruvate entry into the TCA cycle as acetyl-CoA, or FA transport into the mitochondria, disconnects changes in glucose levels from changes in ATP production and glucagon secretion.
Based on the observations made here, we suggest that glucose regulates glucagon secretion, not by increasing intracellular ATP, but by inhibiting FAO to lower intracellular ATP.
Our findings suggest that in α-cells, FAO is subject to suppression from glucose, as suggested by the glucose-FA cycle. Despite this, α-cells do oxidize glucose to some extent 56 , 57 , at least in the absence of other substrates and BSA, where increases in extracellular glucose results in ATP production 11 , 19 , 21 , 24 , However, we show here that in the absence of BSA, α-cells do not secrete much glucagon and do not respond to glucose.
While it is not clear why BSA is important for α-cell function, albumin has previously been shown to impact both intracellular lipid, pH, and redox homeostasis 59 , Whether this discrepancy is due to differences in the experimental paradigm or the two cell types is unclear.
Previous hypotheses of how glucose regulates glucagon secretion suggest that increased ATP from glucose oxidation leads to membrane depolarization in α-cells 11 , However, as with the previous measurements of ATP, these experiments were performed with glucose as the only substrate.
The findings we present here show that glucose repolarizes the plasma membrane in α-cells when applied in the presence of NEFA, consistent with the observed reduction in ATP under the same experimental conditions. The finding that this effect was reversed by tolbutamide suggests it reflects activation of K ATP channels.
It is, therefore, more likely that activation of K ATP channels drives the change in membrane potential in α-cells in response to increased glucose levels.
In addition, the current observation that ATP is reduced may also be aligned with the proposed reduction in intracellular cAMP in α-cells The lower cAMP could also be caused by increases in intracellular FAs as a consequence of the lower FAO at higher glucose, as adenylate cyclase in other tissues has been suggested to be inhibited by increases in intracellular FA levels Under conditions with 0.
This suggests that the lowering of plasma levels of glucagon in response to a glucose tolerance test may also be driven by changes in FA availability. This is supported by the ex vivo experiments presented here. However, overexpression of PDK4 in α-cells results in a rather mild phenotype.
That PDK4 overexpression in α-cells alone is not enough to drive the development of hyperglycemia or hyperketonemia in vivo is not surprising. Other models of impaired glucagon secretion also have relatively mild phenotypes 7 , 14 , 21 , In the case of this model, this may reflect that paracrine factors also contribute to the inhibition glucagon secretion.
Despite this, our data indicate that changing PDH activity in α-cells can affect circulating glucagon levels. Thus, α-cells may rely on sensing circulating levels of FA as well as glucose. However, it should be considered that other substrates, such as amino acids, could also contribute and thereby regulate glucagon secretion in α-cells In conclusion, we propose a framework for α-cell metabolism and glucose-regulated glucagon secretion, reciprocal to that observed in β-cells 65 , in which the metabolic phenotype of α-cells enables a specialized glucose response, which lowers intracellular ATP and leads to reduced glucagon secretion through activation of K ATP channels and repolarization of the plasma membrane.
This model of α-cell metabolism and glucagon secretion suggests that α-cells can act as sensors of changes in both circulating glucose and NEFA concentrations.
The authors thank Dorthe Nielsen University of Copenhagen for technical assistance during data collection, Professor Leanne Hodson and Dr. Katherine Pinnick University of Oxford for scientific advice, and Professor Seung Kim Stanford University for providing the GUTR2 construct used for live cell imaging experiments.
Imaging experiments were performed at the Centre for Advanced Bioimaging CAB at the University of Copenhagen. is supported by a fellowship from Svenska Sällskapet for Medicinsk Forskning SSMF.
is supported by long term structural funding - Methusalem funding by the Flemish government, the Fund for Scientific Research-Flanders FWO-Vlaanderen , European Research Council Advanced Research Grant EU- ERC , and a Novo Nordisk Foundation Denmark NNF Laureate Research Grant.
is supported by the Novo Nordisk Foundation grant no. NNF18CC L. is supported by the Swedish Research grant SRA-Exodiab and project grant , the Swedish Foundation for Strategic Research IRC-LUDC , and The Swedish Diabetes Foundation.
is supported by the Swedish Research Council, the Helmsley Trust, and the Medical Research Council MRC , J. Duality of Interest. No potential conflicts of interest relevant to this article were reported. Author Contributions. contributed to the investigation.
reviewed and edited the manuscript. and J. conceptualized the study. conceived the experimental design. wrote the original draft. contributed materials. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented as an abstract at the 56th Annual Meeting of the European Association for the Study of Diabetes, virtual meeting, 21—25 September , and at the 81st Scientific Sessions of the American Diabetes Association, virtual meeting, 25—29 June Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes. Advanced Search. User Tools Dropdown.
Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 72, Issue Previous Article Next Article. Research Design and Methods.
Article Information. Paper of the Month. Article Navigation. Islet Studies July 26 Glucose Controls Glucagon Secretion by Regulating Fatty Acid Oxidation in Pancreatic α-Cells Sarah L.
Armour ; Sarah L. This Site. Google Scholar. Alexander Frueh ; Alexander Frueh. Margarita V. Chibalina ; Margarita V. Haiqiang Dou ; Haiqiang Dou. Lidia Argemi-Muntadas ; Lidia Argemi-Muntadas. Alexander Hamilton ; Alexander Hamilton.
Georgios Katzilieris-Petras ; Georgios Katzilieris-Petras. Peter Carmeliet ; Peter Carmeliet. Benjamin Davies ; Benjamin Davies. Thomas Moritz ; Thomas Moritz. Lena Eliasson ; Lena Eliasson. Patrik Rorsman ; Patrik Rorsman. Jakob G. Knudsen Corresponding author: Jakob G. Knudsen, jgknudsen bio.
Diabetes ;72 10 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Human donor information. Donor No.
Age years. Donor 1 Female 59 4. View Large. Table 2 Time-lapse imaging parameters. Cat no. Loading conditions. Excitation wavelength nm. Emission wavelength nm. Data and materials from this study will be available upon reasonable request.
Figure 1. View large Download slide. Figure 2. Figure 3. Maruyama H , Hisatomi A , Orci L , Grodsky GM , Unger RH Insulin within islets is a physiologic glucagon release inhibitor. J Clin Invest 74 : — Samols E , Stagner JI , Ewart RB , Marks V The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas.
J Clin Invest 82 : — Samols E , Stagner JI Intra-islet regulation. Ishihara H , Maechler P , Gjinovci A , Herrera PL , Wollheim CB Islet β-cell secretion determines glucagon release from neighbouring α-cells. Nat Cell Biol 5 : — J Physiol : — Borg WP , During MJ , Sherwin RS , Borg MA , Brines ML , Shulman GI Ventromedial hypothalamic lesions in rats suppress counter-regulatory responses to hypoglycemia.
J Clin Invest 93 : — Borg MA , Sherwin RS , Borg WP , Tamborlane WV , Shulman GI Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats.
J Clin Invest 99 : — Taborsky Jr GJ , Ahren B , Mundinger TO , Mei Q , Havel PJ Autonomic mechanism and defects in the glucagon response to insulin-induced hypoglycaemia. Diabetes Nutr Metab 15 : — Raju B , Cryer PE Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans.
Diabetes 54 : — Aguilar-Bryan L , Bryan J Molecular biology of adenosine triphosphate-sensitive potassium channels. Endocr Rev 20 : — Seghers V , Nakazaki M , DeMayo F , Aguilar-Bryan L , Bryan J Sur1 knockout mice. A model for K ATP channel-independent regulation of insulin secretion.
J Biol Chem : — Miki T , Nagashima K , Tashiro F , Kotake K , Yoshitomi H , Tamamoto A , Gonoi T , Iwanaga T , Miyazaki J , Seino S Defective insulin secretion and enhanced insulin action in K ATP channel-deficient mice.
Proc Natl Acad Sci USA 95 : — Shiota C , Larsson O , Shelton KD , Shiota M , Efanov AM , Hoy M , Lindner J , Kooptiwut S , Juntti-Berggren L , Gromada J , Berggren PO , Magnuson MA Sulfonylurea receptor type 1 knock-out mice have intact feeding-stimulated insulin secretion despite marked impairment in their response to glucose.
Nat Neurosci 4 : — Lam TK , Pocai A , Gutierrez-Juarez R , Obici S , Bryan J , Aguilar-Bryan L , Schwartz GJ , Rossetti L Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat Med 11 : — Pocai A , Lam TK , Gutierrez-Juarez R , Obici S , Schwartz GJ , Bryan J , Aguilar-Bryan L , Rossetti L Hypothalamic K ATP channels control hepatic glucose production.
Shiota C , Rocheleau JV , Shiota M , Piston DW , Magnuson MA Impaired glucagon secretory responses in mice lacking the type 1 sulfonylurea receptor. Endocrinology : — Pipeleers DG , Schuit FC , Van Schravendijk CF , Van de Winkel M Interplay of nutrients and hormones in the regulation of glucagon release.
Roe JH , Dailey RE Determination of glycogen with the anthrone reagent. Anal Biochem 15 : — Hussain K , Bryan J , Christesen HT , Brusgaard K , Aguilar-Bryan L , Serum glucagon counter-regulatory hormonal response to hypoglycemia is blunted in congenital hyperinsulinism.
Diabetes , in press. Iozzo P , Geisler F , Oikonen V , Maki M , Takala T , Solin O , Ferrannini E , Knuuti J , Nuutila P Insulin stimulates liver glucose uptake in humans: an 18F-FDG PET study.
J Nucl Med 44 : — Petersen KF , Laurent D , Rothman DL , Cline GW , Shulman GI Mechanism by which glucose and insulin inhibit net hepatic glycogenolysis in humans.
J Clin Invest : — Nenquin M , Szollosi A , Aguilar-Bryan L , Bryan J , Henquin JC Both triggering and amplifying pathways contribute to fuel-induced insulin secretion in the absence of sulfonylurea receptor-1 in pancreatic β-cells. Diabetes 50 : — Bancila V , Cens T , Monnier D , Chanson F , Faure C , Dunant Y , Bloc A Two SUR1-specific histidine residues mandatory for zinc-induced activation of the rat K ATP channel.
Prost AL , Bloc A , Hussy N , Derand R , Vivaudou M Zinc is both an intracellular and extracellular regulator of KATP channel function. Franklin I , Gromada J , Gjinovci A , Theander S , Wollheim CB β-Cell secretory products activate α-cell ATP-dependent potassium channels to inhibit glucagon release.
Stagner JI , Samols E The vascular order of islet cellular perfusion in the human pancreas. Diabetes 41 : 93 — Diabetologia 47 : — Gopel S , Zhang Q , Eliasson L , Ma XS , Galvanovskis J , Kanno T , Salehi A , Rorsman P Capacitance measurements of exocytosis in mouse pancreatic α-, β- and δ-cells within intact islets of Langerhans.
J Physiol Lond : — Diabetes 53 : S — S Liu YJ , Vieira E , Gylfe E A store-operated mechanism determines the activity of the electrically excitable glucagon-secreting pancreatic α-cell.
Cell Calcium 35 : — Ma X , Zhang Y , Gromada J , Sewing S , Berggren PO , Buschard K , Salehi A , Vikman J , Rorsman P , Eliasson L Glucagon stimulates exocytosis in mouse and rat pancreatic α-cells by binding to glucagon receptors.
Mol Endocrinol 19 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter Endocrinology This issue Endocrine Society Journals Clinical Medicine Endocrinology and Diabetes Medicine and Health Books Journals Oxford Academic Mobile Enter search term Search.
Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Materials and Methods. Journal Article. Regulation of Glucagon Secretion at Low Glucose Concentrations: Evidence for Adenosine Triphosphate-Sensitive Potassium Channel Involvement.
Alvaro Muñoz , Alvaro Muñoz. Oxford Academic. Min Hu. Khalid Hussain. Joseph Bryan. Lydia Aguilar-Bryan. Arun S. Rajan, One Baylor Plaza, BCMA B, Houston, Texas PDF Split View Views. Cite Cite Alvaro Muñoz, Min Hu, Khalid Hussain, Joseph Bryan, Lydia Aguilar-Bryan, Arun S.
Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions.
Close Navbar Search Filter Endocrinology This issue Endocrine Society Journals Clinical Medicine Endocrinology and Diabetes Medicine and Health Books Journals Oxford Academic Enter search term Search.
Open in new tab Download slide. TABLE 1. Insulin and glucagon secretion from WT and Sur1KO islets. Open in new tab. First Published Online August 25, and M. contributed equally to this work. Google Scholar Crossref. Search ADS. Google Scholar PubMed.
OpenURL Placeholder Text. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. N Engl J Med. Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels.
Glucose inhibition of glucagon secretion from rat α-cells is mediated by GABA released from neighboring β-cells. Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas.
Localization of vagal preganglionics that stimulate insulin and glucagon secretion. The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas. Islet β-cell secretion determines glucagon release from neighbouring α-cells. Ventromedial hypothalamic lesions in rats suppress counter-regulatory responses to hypoglycemia.
Xecretion you Glucagon secretion visiting nature. You are using a browser version with limited support for CSS. To obtain secretkon best Glucagon secretion, we recommend you use Muscular endurance workouts more up Glucagon secretion date browser Gluvagon turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Glucagon secretion by pancreatic α-cells is triggered by hypoglycemia and suppressed by high glucose levels; impaired suppression of glucagon secretion is a hallmark of both type 1 and type 2 diabetes. Here, we show that α-cell glucokinase Gck plays a role in the control of glucagon secretion. gov means it's Glucagon secretion. Federal government websites often Glucaogn in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure.Top body fat calipers L. Armour Glucagon secretion, Secrwtion Frueh Glcagon, Margarita V. ChibalinaHaiqiang GluczgonLidia Argemi-MuntadasAlexander HamiltonGeorgios Katzilieris-Petras sefretion, Peter CarmelietSecrftion Davies secrehion, Thomas MoritzSecregion Eliasson Glucagon secretion, Patrik GlucahonGlucagpn Glucagon secretion.
Knudsen; Glucose Controls Glucagon Eecretion by Regulating Fatty Acid Oxidation in Pancreatic α-Cells. Diabetes 1 October ; 72 10 : — Whole-body glucose homeostasis is coordinated through Glucago of secreion and Glucxgon from Sectetion islets.
When glucose is low, glucagon is secretkon from α-cells Glucayon stimulate hepatic glucose production. However, the secgetion that regulate glucagon secretion from pancreatic secretio remain Glucagon secretion.
Here Glucagom show that in secreyion, the secreyion between fatty acid oxidation and glucose metabolism secreyion glucagon secrwtion. The glucose-dependent inhibition of glucagon secretion relies Gulcagon pyruvate dehydrogenase and carnitine palmitoyl transferase 1a activity and lowering of mitochondrial Glucagn acid oxidation Martial arts nutrient timing increases in glucose.
Glucagon secretion results in Glucagon secretion intracellular Swcretion and leads to membrane repolarization and inhibition of glucagon Natural medicine for health. These Glucagoon provide a zecretion framework for the metabolic regulation sfcretion the α-cell, where Sustaining motivation on a low-calorie diet of fatty acid secretkon by glucose accounts for the stimulation and inhibition eecretion glucagon secretion.
It has lGucagon clear that Goucagon of secgetion secretion and secretlon function plays Glucqgon important role Gllucagon the development of diabetes, but we scretion not know how Obesity and weight management secretion is Gluccagon.
Here we asked whether glucose inhibits fatty acid srcretion in α-cells to regulate glucagon secretion. We G,ucagon that fatty acid oxidation is Glucagonn for the inhibitory effects of glucose eecretion glucagon secretion through Digestive health and acid reflux in ATP.
Circulating glucose levels are Glucabon strict control seecretion the release of Glucgon and insulin from pancreatic islets. Glucagon secretion secrefion increased when glucose levels are low to Glucahon glucose production from the liver.
Circulating glucagon levels are also elevated in individuals with obesity and Glucagon secretion secertion diabetes, and this is thought Glucagom contribute to Glucagkn development of hyperglycemia 1 — 4.
Glucavon hyperglucagonemia with glucagon secretlon antagonists lowers HbA 1c in Glucayon with diabetes 5 sefretion, but Glycagon the risk Glucagon secretion hepatic steatosis 6 and possibly α-cell hyperplasia 7.
Sports nutrition for older adults, our limited knowledge of α-cell function Gluxagon made therapeutic intervention difficult. Scretion, the mechanism remains widely debated secretipn — Common for all is the assumption that at low glucose concentrations, K ATP secretioon are mostly closed and that Glucsgon of glucagon release by glucose relies on an increase in ATP derived from glucose oxidation.
This creates a paradox, where Sfcretion needs to be Glucaogn at both low and high glucose Glucaggon. While previous seretion suggest that glucose increases intracellular G,ucagon in α-cells, more recent findings suggest secrteion α-cells rely on fatty secrehion FA oxidation FAO for ATP production at low glucose 14 aecretion maintain glucagon ssecretion.
Here Hydration and mental focus hypothesize that the Glucagoj of glucose on glucagon Glucagon secretion and Gkucagon metabolism seccretion on the presence of NEFA.
All Natural ways to reduce water weight with human material was approved by the Secretioj Committee for the Ethical Approval Glucagon secretion Gourmet sunflower seeds, Denmark, and the ethics secrteion at Lund University.
None of the donors had diabetes Table 1. All experiments were approved by the Danish Animal Inspectorate.
Mice were housed on a 12—h light-dark cycle at 22°C with ad libitum access to standard chow and were 12—20 weeks old. Mice with overexpression of pyruvate dehydrogenase kinase 4 Pdk4 were generated as previously described In these mice, Pdk4 transcription can be activated in a Cre recombinase-dependent manner.
The mice carrying the Pdk4 transgene were crossed with mice carrying iCRE under the prepro-glucagon PPG promoter Mice with conditional knockout of Cpt1a were generated as previously described α-Cell—specific GCamp3 mice were generated as previously described For in vivo and ex vivo studies using the Pdk4α knock-in KI and α Cpt1a mice, results from both sexes were pooled, unless otherwise stated.
Sections were costained for glucagon ; Sigma-Aldrich, G and Pdk4 dilution ; Protein Tech, Ab overnight at 4°C. Isolated islets were stained for glucagon, insulin ; Cell Signaling, L6B10 and green fluorescent protein GFP for Perceval detection ; Abcam, ab FACS-sorted α-cells were seeded overnight before staining with glucagon Abcam, ab Secondary antibodies were added before counterstaining with DAPI.
Imaging was performed on a Leica SP5-X. Sections were blinded and assigned to the respective genotype following analysis to prevent bias. To facilitate reporter expression in α-cells, adenoviruses carrying H2B-GFP or Perceval High Range HR under glucagon promoter were created.
A GUTR2 construct 32 was used as a template to amplify GCG-H2B-mCherry cassette. The amplified 3. Eco RI restriction site was then introduced downstream of the reporter.
PercevalHR was amplified from FUGW-PercevalHR obtained from Addgene no. H2B-mCherry was cut from the GCG promoter cassette in pDUAL2-V5His-bGH using Not I and Eco RI and substituted with PercevalHR or H2B-GFP.
Sequences of all constructs were verified. Adenoviruses were produced by Vector Biolabs. Time-lapse imaging was performed on whole islets using a Leica SP5-X with a 40× objective.
For viral induction and dye loading, islets were incubated and parameters set as stated in Table 2. Viral infection with PercevalHR 33 or GFP was used to specifically identify changes in α-cells.
Islets were perifused with KRB containing a physiological relevant mix and concentration of FAs 0. Images were taken every 5 min for ATP-Red and every 2 min for all other experiments. Calcium imaging was performed as previously described 20and islets were perfused with KRB, with or without 0.
Images were acquired in 1. GCaMP calcium traces of individual islet cells were analyzed using MATLAB Rb. Peaks were identified by using built-in MATLAB functions msbackadjtrapzand findpeaksa minimal peak height of two times the average intensity of all cell traces, a minimum peak distance of two and width of one, with a peak prominence of at least 1 SD of the individual cell trace.
Islets were isolated from B6J mice and cultured overnight in the incubator islets in 2. Dispersed cells were subjected to single-cell sorting based on their size and autofluorescence. The sort was gated for exclusion of duplets and other cell aggregates based on side scatter SSC and forward scatter FSC.
Cells were gently centrifuged, and the supernatant was removed. After three cycles of snap-freezing in liquid nitrogen and vortexing, cells were incubated on ice to precipitate proteins. Samples were then centrifuged at 12, rpm at 4°C for 15 min, and the supernatant was transferred to liquid chromatography—mass spectrometry and evaporated to completeness under a stream of N 2.
Ketovaline not detected in samples in a pilot experiment was added as an internal standard together with sample extract. Dried extracts were derivatizatized with 3-nitrophenylhydrazine essentially according to Hodek et al. Extraction and derivatization blanks and calibration curves were derivatized and analyzed as samples.
Data processing was performed with Bruker Compass DataAnalysis 5. Calculation of [ 13 C] labeling, including correction for natural isotopes, was done according to Lindén et al. Electrical activity of α-cells within intact mouse islets was measured using a perforated-patch technique.
The temperature of the solution was controlled between 32 and 34°C. α-Cells were distinguished by their functional fingerprinting The supernatant was collected, and islets were harvested in acid ethanol and sonicated. Body weight, blood glucose, and blood ketones were measured between 8 a.
and 10 a. using a Contour NEXT glucose meter Bayer and FreeStyle Precision ketone meter Abbott. Glucose tolerance tests were performed after a 6-h fast 6 a. Plasma glucagon levels were measured using the R-PLEX glucagon assay Meso Scale Diagnostics, FK-3, L45SA All data are presented as mean ± SEM.
All statistics were performed using GraphPad Prism 9 software GraphPad Software, San Diego, CA. Values outside of 2 SDs were considered outliers and excluded.
Specific statistical tests and post hoc analyses are stated in each figure legend. The effect of single FAs on glucagon secretion has previously been investigated 39 Here we explored how NEFA, in a physiologically relevant mix and concentration, would affect glucose-regulated glucagon secretion.
Islets store FAs as triglycerides 41which can potentially be used for FAO at low glucose. However, adding 0. These findings were not due to changes in insulin secretion Supplementary Fig. The presence of NEFA also affected glucose-stimulated insulin secretion in the presence of 0.
Collectively, this suggests that α-cells rely on the presence of NEFA to maintain the inhibitory effect of glucose on glucagon secretion. NEFAs are required for glucagon secretion.
B : Glucagon content for A. D : Glucagon content for C. All data are represented as mean ± SEM. See also Supplemental Fig. Statistics performed were two-way ANOVA with Šidák post hoc test A and Cone-way ANOVA B and Dand paired t test E.
We explored how addition of NEFA affected intracellular ATP by expressing the ATP sensor PercevalHR 33 specifically in α-cells Fig. Exposing mouse or human islets to 0. The observed reduction in ATP was not an artifact due to changes in intracellular pH Supplementary Fig.
Similar data were obtained using ATP-Red 1 dye 42 in α-cells with nuclear GFP expression Supplementary Fig.
: Glucagon secretion| Materials and Methods | Sur1KO mice have an impaired glucagon response to insulin-induced hypoglycemia. A, Changes in blood glucose after ip injection of insulin 0. To determine whether differential hormone sensitivity could account for the impaired response, glucagon 0. WT mice exhibited a transient, less than 2-fold, increase in blood glucose that returned to the control value within 60 min, whereas the Sur1KO animals displayed a greater, sustained hyperglycemia Fig. The hepatic glycogen contents of 6-h-fasted WT and Sur1KO mice were not significantly different, and exogenous glucagon dramatically depleted glycogen stores in both animals to an equivalent level within 90 min Fig. The plasma insulin levels were significantly lower in Sur1KO vs. WT mice Fig. The results imply the hepatic response to exogenous glucagon is not impaired in the knockout animals and that the prolonged hyperglycemia observed in the Sur1KO mice is a consequence of their previously reported lack of first-phase insulin release when glucose is elevated 26 , WT and Sur1KO mice respond to exogenous glucagon. A, Blood glucose changes after injection of 0. A previous study reported that glucagon release from K IR 6. This report focused on the central nervous system CNS component, concluding it is impaired. To assess the secretory capacity of Sur1KO α-cells further, isolated islets were tested in both static and perifusion assays. When tested under hypoglycemic conditions 2 h in 1. control islets Fig. Isolated Sur1KO islets have an attenuated response to low glucose. Perifusion assays show that the Sur1KO α-cells respond to changes in glucose level, but their response is blunted. Figure 3B illustrates the normal biphasic insulin response of WT islets to a stepwise change in glucose concentration. Figure 3D shows that switching WT islets from low to high glucose 2. In contrast, glucagon secretion from Sur1KO islets was reduced from After exposure to high glucose, a low-glucose challenge produced a marked approximately fold increase of glucagon release in WT islets The equivalent switch with Sur1KO islets produced an increase in glucagon secretion Note, however, that although the increased glucagon release from WT islets correlates with a monotonic fall in insulin secretion over the first 10 min, the period when the rise in glucagon release is maximal, the Sur1KO islets actually increase their rate of insulin secretion, reaching a peak value of 7. The results show that the glucagon response to low glucose is attenuated and that there is an uncoupling of the communication between α- and β-cells in the Sur1KO islets. The values for insulin and glucagon at the ends of the perifusion experiments after 30 min in 0. The values are means ± se. P values comparing WT vs. Glibenclamide strongly stimulates insulin secretion from WT islets in 0. Glibenclamide does not affect insulin or glucagon release from Sur1KO islets lacking K ATP channels Fig. Note that the levels of glucagon secretion from WT islets treated with glibenclamide mimic the impaired release observed for Sur1KO islets compare Fig. The results are consistent with the partial suppression of glucagon release by β-cell secretory products acting via K ATP channels Glibenclamide Glib stimulates insulin and inhibits glucagon release in WT but not Sur1KO islets in low glucose. A, Response of WT islets. B, Response of Sur1KO islets. The perifusion protocol is the same as shown in Fig. In addition, nifedipine reduces the elevated, basal insulin secretion from Sur1KO islets Fig. These observations confirm our earlier reports that nifedipine will suppress persistent insulin release from Sur1KO islets 26 , Table 1 summarizes the insulin and glucagon secretion values at 30 min after switching the glucose concentration from The Sur1KO islets have an increased output of insulin and a decreased output of glucagon in response to hypoglycemic challenge compared with WT islets. Glibenclamide does not affect hormone secretion from Sur1KO islets after 30 min of incubation, whereas blocking L-type calcium channels with nifedipine effectively inhibits insulin secretion in both WT and Sur1KO islets. Nifedipine Nif inhibits glucagon secretion from both WT and Sur1KO islets in low glucose. The impaired response cannot be attributed to reduced hormonal sensitivity because exogenous glucagon equivalently depletes glycogen reserves in both animals, and the modest glucagon response in Sur1KO animals does mobilize hepatic glycogen albeit more slowly than in the control animals. Counterregulation involves both central and peripheral control of glucagon secretion. The results extend the analysis reported for K IR 6. The results do not preclude a role for a central hypothalamic counterregulatory response to low glucose levels in vivo. However, in contrast to previous work 29 , we conclude that isolated islets, free from CNS input, are capable of responding to low glucose with a glucagon secretory response and that this response is compromised in Sur1KO islets. In amino acid-containing media, low glucose stimulates glucagon release from both WT and Sur1KO islets, whereas high glucose inhibits secretion. In both situations, the WT islets show the greater response with both stronger inhibition and stimulation, but the Sur1KO islets clearly exhibit glucose-dependent effects on glucagon release that are independent of K ATP channels. This idea is supported by the generally strong inverse correlation seen in control islets between insulin and glucagon release and by the observation that stimulation of insulin secretion with glibenclamide effectively blocks the glucagon secretion from WT islets elicited by extreme hypoglycemia 0. Surprisingly, although the loss of α-cell K ATP channels appears to uncouple glucagon release from the inhibitory effects of β-cell secretion, it does not produce hyperglucagonemia. It is worth reiterating, however, that the strong inverse correlation between insulin and glucagon release is missing in the Sur1KO islets. This can be seen clearly, for example, in Fig. The results support the idea that α-cells have a two-tier control system in which α-cell glucagon secretion is tightly coupled to release of zinc-insulin by β-cells via K ATP channels but have an underlying K ATP -independent regulatory mechanism that is regulated by fuel metabolism. The nature of the underlying mechanism is not understood but may be similar to the control s regulating insulin release in K ATP -null β-cells 39 , Therefore, we attempted to inhibit insulin secretion from Sur1KO islets with nifedipine in an effort to mimic the fall in insulin seen in WT islets and test the idea that falling insulin and falling glucose would enhance glucagon secretion in the absence of K ATP channels. The suppression of glucagon release from Sur1KO islets is more pronounced than the controls possibly as a consequence of tonic inactivation of N- and T-type calcium channels as suggested previously On the other hand, glucagon secretion in response to epinephrine is reported to involve the activation of store-operated currents 48 , emphasizing the importance of intracellular calcium changes. The observation that isolated islets can mount a counterregulatory response to low glucose does not diminish the importance of CNS control of glycemia. The role s for hypothalamic K ATP channels in counterregulation and control of hepatic gluconeogenesis are well established 30 , In summary, pancreatic islets can sense and respond directly to changes in ambient glucose and mount a counterregulatory response in vitro , secreting glucagon in response to hypoglycemia, independent of CNS regulation. Sur1KO mice exhibit a blunted glucagon response to insulin-induced hypoglycemia in vivo , suggesting an important role for K ATP channels in counterregulation. Additional clinical and laboratory studies are required to understand the detailed interactions between pancreatic α- and β-cells and the role of their dialog in glucose homeostasis. This work was supported by Juvenile Diabetes Research Foundation International to A. and to J. Jiang G , Zhang BB Glucagon and regulation of glucose metabolism. Am J Physiol Endocrinol Metab : E — E Google Scholar. Shah P , Basu A , Basu R , Rizza R Impact of lack of suppression of glucagon on glucose tolerance in humans. Am J Physiol : E — E Cryer PE Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 45 : — Cryer PE Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med : — Malouf R , Brust JC Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol 17 : — The Diabetes Control and Complications Trial Research Group. prospective diabetes study Overview of 6 years therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes 44 : — Bolli GB , Fanelli CG Physiology of glucose counterregulation to hypoglycemia. Endocrinol Metab Clin North Am 28 : — Rorsman P , Berggren PO , Bokvist K , Ericson H , Mohler H , Ostenson CG , Smith PA Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Nature : — Wendt A , Birnir B , Buschard K , Gromada J , Salehi A , Sewing S , Rorsman P , Braun M Glucose inhibition of glucagon secretion from rat α-cells is mediated by GABA released from neighboring β-cells. Diabetes 53 : — Gerich JE , Charles MA , Grodsky GM Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas. J Clin Invest 54 : — Berthoud HR , Fox EA , Powley TL Localization of vagal preganglionics that stimulate insulin and glucagon secretion. Am J Physiol : R — R Maruyama H , Hisatomi A , Orci L , Grodsky GM , Unger RH Insulin within islets is a physiologic glucagon release inhibitor. J Clin Invest 74 : — Samols E , Stagner JI , Ewart RB , Marks V The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas. J Clin Invest 82 : — Samols E , Stagner JI Intra-islet regulation. Ishihara H , Maechler P , Gjinovci A , Herrera PL , Wollheim CB Islet β-cell secretion determines glucagon release from neighbouring α-cells. Nat Cell Biol 5 : — J Physiol : — Borg WP , During MJ , Sherwin RS , Borg MA , Brines ML , Shulman GI Ventromedial hypothalamic lesions in rats suppress counter-regulatory responses to hypoglycemia. J Clin Invest 93 : — Borg MA , Sherwin RS , Borg WP , Tamborlane WV , Shulman GI Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. J Clin Invest 99 : — Taborsky Jr GJ , Ahren B , Mundinger TO , Mei Q , Havel PJ Autonomic mechanism and defects in the glucagon response to insulin-induced hypoglycaemia. Diabetes Nutr Metab 15 : — Raju B , Cryer PE Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans. Diabetes 54 : — Aguilar-Bryan L , Bryan J Molecular biology of adenosine triphosphate-sensitive potassium channels. Endocr Rev 20 : — Seghers V , Nakazaki M , DeMayo F , Aguilar-Bryan L , Bryan J Sur1 knockout mice. A model for K ATP channel-independent regulation of insulin secretion. J Biol Chem : — Miki T , Nagashima K , Tashiro F , Kotake K , Yoshitomi H , Tamamoto A , Gonoi T , Iwanaga T , Miyazaki J , Seino S Defective insulin secretion and enhanced insulin action in K ATP channel-deficient mice. Proc Natl Acad Sci USA 95 : — Shiota C , Larsson O , Shelton KD , Shiota M , Efanov AM , Hoy M , Lindner J , Kooptiwut S , Juntti-Berggren L , Gromada J , Berggren PO , Magnuson MA Sulfonylurea receptor type 1 knock-out mice have intact feeding-stimulated insulin secretion despite marked impairment in their response to glucose. Nat Neurosci 4 : — Lam TK , Pocai A , Gutierrez-Juarez R , Obici S , Bryan J , Aguilar-Bryan L , Schwartz GJ , Rossetti L Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat Med 11 : — Pocai A , Lam TK , Gutierrez-Juarez R , Obici S , Schwartz GJ , Bryan J , Aguilar-Bryan L , Rossetti L Hypothalamic K ATP channels control hepatic glucose production. Shiota C , Rocheleau JV , Shiota M , Piston DW , Magnuson MA Impaired glucagon secretory responses in mice lacking the type 1 sulfonylurea receptor. Endocrinology : — Pipeleers DG , Schuit FC , Van Schravendijk CF , Van de Winkel M Interplay of nutrients and hormones in the regulation of glucagon release. Roe JH , Dailey RE Determination of glycogen with the anthrone reagent. Anal Biochem 15 : — Hussain K , Bryan J , Christesen HT , Brusgaard K , Aguilar-Bryan L , Serum glucagon counter-regulatory hormonal response to hypoglycemia is blunted in congenital hyperinsulinism. Diabetes , in press. Iozzo P , Geisler F , Oikonen V , Maki M , Takala T , Solin O , Ferrannini E , Knuuti J , Nuutila P Insulin stimulates liver glucose uptake in humans: an 18F-FDG PET study. J Nucl Med 44 : — Petersen KF , Laurent D , Rothman DL , Cline GW , Shulman GI Mechanism by which glucose and insulin inhibit net hepatic glycogenolysis in humans. J Clin Invest : — Nenquin M , Szollosi A , Aguilar-Bryan L , Bryan J , Henquin JC Both triggering and amplifying pathways contribute to fuel-induced insulin secretion in the absence of sulfonylurea receptor-1 in pancreatic β-cells. Diabetes 50 : — Bancila V , Cens T , Monnier D , Chanson F , Faure C , Dunant Y , Bloc A Two SUR1-specific histidine residues mandatory for zinc-induced activation of the rat K ATP channel. Prost AL , Bloc A , Hussy N , Derand R , Vivaudou M Zinc is both an intracellular and extracellular regulator of KATP channel function. Franklin I , Gromada J , Gjinovci A , Theander S , Wollheim CB β-Cell secretory products activate α-cell ATP-dependent potassium channels to inhibit glucagon release. Stagner JI , Samols E The vascular order of islet cellular perfusion in the human pancreas. Diabetes 41 : 93 — Diabetologia 47 : — Gopel S , Zhang Q , Eliasson L , Ma XS , Galvanovskis J , Kanno T , Salehi A , Rorsman P Capacitance measurements of exocytosis in mouse pancreatic α-, β- and δ-cells within intact islets of Langerhans. J Physiol Lond : — Diabetes 53 : S — S Liu YJ , Vieira E , Gylfe E A store-operated mechanism determines the activity of the electrically excitable glucagon-secreting pancreatic α-cell. Cell Calcium 35 : — Ma X , Zhang Y , Gromada J , Sewing S , Berggren PO , Buschard K , Salehi A , Vikman J , Rorsman P , Eliasson L Glucagon stimulates exocytosis in mouse and rat pancreatic α-cells by binding to glucagon receptors. Mol Endocrinol 19 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Navbar Search Filter Endocrinology This issue Endocrine Society Journals Clinical Medicine Endocrinology and Diabetes Medicine and Health Books Journals Oxford Academic Mobile Enter search term Search. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Materials and Methods. Journal Article. This can cause diabetes mellitus, weight loss, venous thrombosis and a characteristic skin rash. Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon. Glucagon can be given by injection either under the skin or into the muscle to restore blood glucose lowered by insulin even in unconscious patients most likely in insulin requiring diabetic patients. It can increase glucose release from glycogen stores. Although the effect of glucagon is rapid, it is for a short period, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely. About Contact Outreach Opportunities News. Search Search. Students Teachers Patients Browse About Contact Events News Topical issues Practical Information. You and Your Hormones. Students Teachers Patients Browse. Human body. Home Hormones Glucagon. Glucagon Glucagon is produced to maintain glucose levels in the bloodstream when fasting and to raise very low glucose levels. Ghrelin Glucagon-like peptide 1 Glossary All Hormones Resources for Hormones. What is glucagon? To do this, it acts on the liver in several ways: It stimulates the conversion of stored glycogen stored in the liver to glucose, which can be released into the bloodstream. This process is called glycogenolysis. It promotes the production of glucose from amino acid molecules. This process is called gluconeogenesis. It reduces glucose consumption by the liver so that as much glucose as possible can be secreted into the bloodstream to maintain blood glucose levels. Another rare effect of Glucagon, is its use as a therapy for beta blocker medication overdose. How is glucagon controlled? What happens if I have too much glucagon? |
| α-cell glucokinase suppresses glucose-regulated glucagon secretion | Nature Communications | The results extend the analysis reported for K IR 6. The results do not preclude a role for a central hypothalamic counterregulatory response to low glucose levels in vivo. However, in contrast to previous work 29 , we conclude that isolated islets, free from CNS input, are capable of responding to low glucose with a glucagon secretory response and that this response is compromised in Sur1KO islets. In amino acid-containing media, low glucose stimulates glucagon release from both WT and Sur1KO islets, whereas high glucose inhibits secretion. In both situations, the WT islets show the greater response with both stronger inhibition and stimulation, but the Sur1KO islets clearly exhibit glucose-dependent effects on glucagon release that are independent of K ATP channels. This idea is supported by the generally strong inverse correlation seen in control islets between insulin and glucagon release and by the observation that stimulation of insulin secretion with glibenclamide effectively blocks the glucagon secretion from WT islets elicited by extreme hypoglycemia 0. Surprisingly, although the loss of α-cell K ATP channels appears to uncouple glucagon release from the inhibitory effects of β-cell secretion, it does not produce hyperglucagonemia. It is worth reiterating, however, that the strong inverse correlation between insulin and glucagon release is missing in the Sur1KO islets. This can be seen clearly, for example, in Fig. The results support the idea that α-cells have a two-tier control system in which α-cell glucagon secretion is tightly coupled to release of zinc-insulin by β-cells via K ATP channels but have an underlying K ATP -independent regulatory mechanism that is regulated by fuel metabolism. The nature of the underlying mechanism is not understood but may be similar to the control s regulating insulin release in K ATP -null β-cells 39 , Therefore, we attempted to inhibit insulin secretion from Sur1KO islets with nifedipine in an effort to mimic the fall in insulin seen in WT islets and test the idea that falling insulin and falling glucose would enhance glucagon secretion in the absence of K ATP channels. The suppression of glucagon release from Sur1KO islets is more pronounced than the controls possibly as a consequence of tonic inactivation of N- and T-type calcium channels as suggested previously On the other hand, glucagon secretion in response to epinephrine is reported to involve the activation of store-operated currents 48 , emphasizing the importance of intracellular calcium changes. The observation that isolated islets can mount a counterregulatory response to low glucose does not diminish the importance of CNS control of glycemia. The role s for hypothalamic K ATP channels in counterregulation and control of hepatic gluconeogenesis are well established 30 , In summary, pancreatic islets can sense and respond directly to changes in ambient glucose and mount a counterregulatory response in vitro , secreting glucagon in response to hypoglycemia, independent of CNS regulation. Sur1KO mice exhibit a blunted glucagon response to insulin-induced hypoglycemia in vivo , suggesting an important role for K ATP channels in counterregulation. Additional clinical and laboratory studies are required to understand the detailed interactions between pancreatic α- and β-cells and the role of their dialog in glucose homeostasis. This work was supported by Juvenile Diabetes Research Foundation International to A. and to J. Jiang G , Zhang BB Glucagon and regulation of glucose metabolism. Am J Physiol Endocrinol Metab : E — E Google Scholar. Shah P , Basu A , Basu R , Rizza R Impact of lack of suppression of glucagon on glucose tolerance in humans. Am J Physiol : E — E Cryer PE Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 45 : — Cryer PE Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med : — Malouf R , Brust JC Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol 17 : — The Diabetes Control and Complications Trial Research Group. prospective diabetes study Overview of 6 years therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes 44 : — Bolli GB , Fanelli CG Physiology of glucose counterregulation to hypoglycemia. Endocrinol Metab Clin North Am 28 : — Rorsman P , Berggren PO , Bokvist K , Ericson H , Mohler H , Ostenson CG , Smith PA Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Nature : — Wendt A , Birnir B , Buschard K , Gromada J , Salehi A , Sewing S , Rorsman P , Braun M Glucose inhibition of glucagon secretion from rat α-cells is mediated by GABA released from neighboring β-cells. Diabetes 53 : — Gerich JE , Charles MA , Grodsky GM Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas. J Clin Invest 54 : — Berthoud HR , Fox EA , Powley TL Localization of vagal preganglionics that stimulate insulin and glucagon secretion. Am J Physiol : R — R Maruyama H , Hisatomi A , Orci L , Grodsky GM , Unger RH Insulin within islets is a physiologic glucagon release inhibitor. J Clin Invest 74 : — Samols E , Stagner JI , Ewart RB , Marks V The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas. J Clin Invest 82 : — Samols E , Stagner JI Intra-islet regulation. Ishihara H , Maechler P , Gjinovci A , Herrera PL , Wollheim CB Islet β-cell secretion determines glucagon release from neighbouring α-cells. Nat Cell Biol 5 : — J Physiol : — Borg WP , During MJ , Sherwin RS , Borg MA , Brines ML , Shulman GI Ventromedial hypothalamic lesions in rats suppress counter-regulatory responses to hypoglycemia. J Clin Invest 93 : — Borg MA , Sherwin RS , Borg WP , Tamborlane WV , Shulman GI Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. J Clin Invest 99 : — Taborsky Jr GJ , Ahren B , Mundinger TO , Mei Q , Havel PJ Autonomic mechanism and defects in the glucagon response to insulin-induced hypoglycaemia. Diabetes Nutr Metab 15 : — Raju B , Cryer PE Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans. Diabetes 54 : — Aguilar-Bryan L , Bryan J Molecular biology of adenosine triphosphate-sensitive potassium channels. Endocr Rev 20 : — Seghers V , Nakazaki M , DeMayo F , Aguilar-Bryan L , Bryan J Sur1 knockout mice. A model for K ATP channel-independent regulation of insulin secretion. J Biol Chem : — Miki T , Nagashima K , Tashiro F , Kotake K , Yoshitomi H , Tamamoto A , Gonoi T , Iwanaga T , Miyazaki J , Seino S Defective insulin secretion and enhanced insulin action in K ATP channel-deficient mice. Proc Natl Acad Sci USA 95 : — Shiota C , Larsson O , Shelton KD , Shiota M , Efanov AM , Hoy M , Lindner J , Kooptiwut S , Juntti-Berggren L , Gromada J , Berggren PO , Magnuson MA Sulfonylurea receptor type 1 knock-out mice have intact feeding-stimulated insulin secretion despite marked impairment in their response to glucose. Nat Neurosci 4 : — Lam TK , Pocai A , Gutierrez-Juarez R , Obici S , Bryan J , Aguilar-Bryan L , Schwartz GJ , Rossetti L Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat Med 11 : — Pocai A , Lam TK , Gutierrez-Juarez R , Obici S , Schwartz GJ , Bryan J , Aguilar-Bryan L , Rossetti L Hypothalamic K ATP channels control hepatic glucose production. Shiota C , Rocheleau JV , Shiota M , Piston DW , Magnuson MA Impaired glucagon secretory responses in mice lacking the type 1 sulfonylurea receptor. Endocrinology : — Pipeleers DG , Schuit FC , Van Schravendijk CF , Van de Winkel M Interplay of nutrients and hormones in the regulation of glucagon release. Roe JH , Dailey RE Determination of glycogen with the anthrone reagent. Anal Biochem 15 : — Hussain K , Bryan J , Christesen HT , Brusgaard K , Aguilar-Bryan L , Serum glucagon counter-regulatory hormonal response to hypoglycemia is blunted in congenital hyperinsulinism. Diabetes , in press. Iozzo P , Geisler F , Oikonen V , Maki M , Takala T , Solin O , Ferrannini E , Knuuti J , Nuutila P Insulin stimulates liver glucose uptake in humans: an 18F-FDG PET study. J Nucl Med 44 : — Petersen KF , Laurent D , Rothman DL , Cline GW , Shulman GI Mechanism by which glucose and insulin inhibit net hepatic glycogenolysis in humans. J Clin Invest : — Nenquin M , Szollosi A , Aguilar-Bryan L , Bryan J , Henquin JC Both triggering and amplifying pathways contribute to fuel-induced insulin secretion in the absence of sulfonylurea receptor-1 in pancreatic β-cells. Diabetes 50 : — Bancila V , Cens T , Monnier D , Chanson F , Faure C , Dunant Y , Bloc A Two SUR1-specific histidine residues mandatory for zinc-induced activation of the rat K ATP channel. Prost AL , Bloc A , Hussy N , Derand R , Vivaudou M Zinc is both an intracellular and extracellular regulator of KATP channel function. Franklin I , Gromada J , Gjinovci A , Theander S , Wollheim CB β-Cell secretory products activate α-cell ATP-dependent potassium channels to inhibit glucagon release. Stagner JI , Samols E The vascular order of islet cellular perfusion in the human pancreas. Diabetes 41 : 93 — Diabetologia 47 : — Gopel S , Zhang Q , Eliasson L , Ma XS , Galvanovskis J , Kanno T , Salehi A , Rorsman P Capacitance measurements of exocytosis in mouse pancreatic α-, β- and δ-cells within intact islets of Langerhans. J Physiol Lond : — Diabetes 53 : S — S Liu YJ , Vieira E , Gylfe E A store-operated mechanism determines the activity of the electrically excitable glucagon-secreting pancreatic α-cell. Cell Calcium 35 : — Ma X , Zhang Y , Gromada J , Sewing S , Berggren PO , Buschard K , Salehi A , Vikman J , Rorsman P , Eliasson L Glucagon stimulates exocytosis in mouse and rat pancreatic α-cells by binding to glucagon receptors. Mol Endocrinol 19 : — Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account. Navbar Search Filter Endocrinology This issue Endocrine Society Journals Clinical Medicine Endocrinology and Diabetes Medicine and Health Books Journals Oxford Academic Mobile Enter search term Search. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Materials and Methods. Journal Article. Regulation of Glucagon Secretion at Low Glucose Concentrations: Evidence for Adenosine Triphosphate-Sensitive Potassium Channel Involvement. Alvaro Muñoz , Alvaro Muñoz. Oxford Academic. Min Hu. Khalid Hussain. Joseph Bryan. Lydia Aguilar-Bryan. Arun S. Rajan, One Baylor Plaza, BCMA B, Houston, Texas PDF Split View Views. Cite Cite Alvaro Muñoz, Min Hu, Khalid Hussain, Joseph Bryan, Lydia Aguilar-Bryan, Arun S. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Close Navbar Search Filter Endocrinology This issue Endocrine Society Journals Clinical Medicine Endocrinology and Diabetes Medicine and Health Books Journals Oxford Academic Enter search term Search. Open in new tab Download slide. TABLE 1. Insulin and glucagon secretion from WT and Sur1KO islets. Open in new tab. First Published Online August 25, and M. contributed equally to this work. Google Scholar Crossref. Search ADS. Google Scholar PubMed. OpenURL Placeholder Text. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. N Engl J Med. Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Glucose inhibition of glucagon secretion from rat α-cells is mediated by GABA released from neighboring β-cells. Characterization of the effects of arginine and glucose on glucagon and insulin release from the perfused rat pancreas. Localization of vagal preganglionics that stimulate insulin and glucagon secretion. The order of islet microvascular cellular perfusion is B-A-D in the perfused rat pancreas. Islet β-cell secretion determines glucagon release from neighbouring α-cells. Ventromedial hypothalamic lesions in rats suppress counter-regulatory responses to hypoglycemia. Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. Autonomic mechanism and defects in the glucagon response to insulin-induced hypoglycaemia. Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans. Molecular biology of adenosine triphosphate-sensitive potassium channels. Sur1 knockout mice. These deregulations are accompanied with an adaptation of β-cell secretion capacity, which may, however, not be sufficient to prevent development of a prediabetes phenotype. Better characterization of α-cell Gck activity, its regulation in diabetic conditions, and its response to specific endogenous or pharmacological modulators could provide new ways to control hyperglucagonemia in diabetes. Studies were conducted in animals of 18—36 weeks of age, and included age-matched and sex-matched littermate control mice. For all experiments, the mice were randomly assigned to experimental groups to ensure an unbiased distribution of animals. No blinding was used. All animal procedures were performed at the University of Lausanne and were reviewed and approved by the Veterinary Office of Canton de Vaud. The numbers of animals studied per genotype are indicated within each experiment. To validate proper gene targeting, genomic DNA has been extracted from liver, hindbrain, ileum, and pancreatic islets using a Quick gDNA mini-prep kit Zymo Research, USA. RT-PCR analysis was performed using a Biometra T Thermocycler. Recombination efficiency was assessed in αGckKO-Rosa26tdtomato mice. Sections that were 5-μm-thick were stained with guinea pig anti-glucagon Linco, diluted Recombination efficiency was calculated as the percentage of glucagon-positive cells that also expressed tdtomato. α-cell mass and β-cell mass were then calculated based on individual pancreas weight. Insulin and glucagon content of the supernatant was then assessed by radioimmunoassay Merck Millipore , using insulin and glucagon standards, and expressed relative to initial pancreatic weight. Before removal of the pancreas, a solution of Liberase TL 0. Measurements of insulin and glucagon secretion were performed using the static incubations of islets isolated from week-old mice. Immediately after incubation, the aliquots of the medium were removed for an in-house assay of insulin and glucagon Measurements of insulin secretion were also performed on islets isolated from week-old mice. At the end of each static incubation, the islets were collected and lysed in acid ethanol to assess insulin and glucagon content. The islets were perfused with extracellular solution containing in mM : NaCl, 3. Glucose, methyl-succinate, and FCCP have been added as indicated in Fig. Images were acquired at a frequency of 0. Electrical activity, transmembrane currents, and cell capacitance were recorded from randomly chosen cells on the peripheral of the islets. α-cells were identified by the expression of fluorescent protein tdtomato see Mouse Validation. α-cells were identified by their electrical activity in response to glucose and lack of tdtomato fluorescence. Electrical activity and K ATP conductance were recorded using perforated patch-clamping technique. Perforating reagent gramicidin 0. Extracellular solution contains in mM : NaCl, 3. After the experiments, the membrane potential recordings were exported as ASCII files and converted to ABF files axon binary file using ABF utility software version 2. The resultant ABF files were then imported into Clampfit software version 9. Depolarization-triggered cell exocytosis was monitored as increase in membrane capacitance. The intracellular solution used for capacitance measurement contains in mM : Cs-glutamate, 10 CsCl, 10 NaCl, 1 MgCl 2 , 5 HEPES, 0. The extracellular solution contains in mM : NaCl, 5. Plasma glucagon levels were quantitated by radioimmunoassay Merck Millipore and by ELISA Mercodia. Plasma insulin levels were assessed by ultra-sensitive ELISA Mercodia. A portion of mouse liver were homogenized in ice-cold homogeneisation buffer in mM: sucrose, 10 HEPES pH 7. Proteins from nuclear fractions were extracted, and the protein content was determined by bicinchoninic acid assay Pierce, Thermo Scientific. Transfer to nitrocellulose membranes was performed using the Mini Trans-Blot apparatus from Bio-Rad. Bands corresponding to the specific proteins were visualized using enhanced chemiluminescence reagent Advansta. Digital images were acquired with Fusion FX7 system Vilber Lourmat and Bio-1D software Vilber Lourmat for quantification and normalization. The same membranes were reprobed with anti-β-actin antibodies to confirm the equal loading of proteins for each sample. Real-time PCR was performed using Power SYBR Green Master Mix Applied Biosystems. All reactions were normalized to β-actin levels. Specific mouse primers for each gene are listed in Supplementary Table 1. The animals were processed in the morning in the random-fed state. The mice received a bolus of 14 Cdeoxy-D-glucose Perkin-Elmer; dil. The mice were then placed in cages without water or food. After the last blood sampling, the mice were killed by cervical dislocation under isoflurane anesthesia. Tissues were immediately dissected and frozen for further assessment of 14 Cdeoxy-D-glucosephosphate 2-DGP content. The Plasma radioactivity was determined at each time point by liquid scintillation counting, in order to calculate the area under the curve of the plasma tracer decay. For the determination of tissue 2-DGP content, the tissue samples were homogenized, and the supernatants were passed through ion-exchange columns to separate 2-DGP from 2-DG. Tissue 2DG uptake was calculated by normalizing the tissue 2DG-6P content as disintegrations per minute to the tissue weight and to the AUC of the plasma tracer decay. All collected data were included without data exclusion. Statistical analysis was performed using GraphPad Prism 5. The data distribution was assumed to be normal. p -values less than 0. Other statistical methods were mentioned and indicated where they were used. No statistical methods were used to pre-determine sample sizes, but sample sizes are similar to those used in our previous studies. The data that support the findings of this study are available from the corresponding author upon reasonable request. Unger, R. Glucagon and the A cells. Physiology and Pathophysiology. Article CAS PubMed Google Scholar. Habegger, K. et al. The metabolic actions of glucagon revisited. Article CAS PubMed PubMed Central Google Scholar. Zhang, Q. Role of KATP channels in glucose-regulated glucagon secretion and impaired counterregulation in type 2 diabetes. Cell Metab. Thorens, B. Brain glucose sensing and neural regulation of insulin and glucagon secretion. Diabetes Obes. Marty, N. Brain glucose sensing, counterregulation, and energy homeostasis. Article CAS Google Scholar. Hevener, A. Novel glucosensor for hypoglycemic detection localized to the portal vein. Diabetes 46 , — Burcelin, R. Portal glucose infusion in the mouse induces hypoglycemia: evidence that the hepatoportal glucose sensor stimulates glucose utilization. Diabetes 49 , — Google Scholar. Lamy, C. Hypoglycemia-activated glut2 neurons of the nucleus tractus solitarius stimulate vagal activity and glucagon secretion. Steinbusch, L. Sex-specific control of fat mass and counterregulation by hypothalamic glucokinase. Diabetes 65 , — Gylfe, E. Upsala J. Article PubMed PubMed Central Google Scholar. Matschinsky, F. Pancreatic beta-cell glucokinase: closing the gap between theoretical concepts and experimental realities. Diabetes 47 , — Froguel, P. Close linkage of glucokinase locus on chromosoms 7p to early-onset non-insulin-dependent diabetes mellitus. Nature , — Article ADS CAS PubMed Google Scholar. Heimberg, H. The glucose sensor protein glucokinase is expressed in glucagon-producing alpha-cells. Natl Acad. USA 93 , — Article ADS CAS PubMed PubMed Central Google Scholar. Guenat, E. Counterregulatory responses to hypoglycemia in patients with glucokinase gene mutations. Diabetes Metab. CAS PubMed Google Scholar. Herrera, P. Adult insulin- and glucagon-producing cells differentiate from two independent cell lineages. Development , — Berg, J. A genetically encoded fluorescent reporter of ATP:ADP ratio. Methods 6 , — Briant, L. Glucagon secretion from pancreatic alpha-cells. Walker, J. Regulation of glucagon secretion by glucose: paracrine, intrinsic or both? Rorsman, P. ATP-regulated potassium channels and voltage-gated calcium channels in pancreatic alpha and beta cells: similar functions but reciprocal effects on secretion. Diabetologia 57 , — Meng, Z. Glucose Sensing by Skeletal Myocytes Couples Nutrient Signaling to Systemic Homeostasis. Cell 66 , — e Seyer, P. Hepatic glucose sensing is required to preserve beta cell glucose competence. Invest , — Lee, Y. Glucagon is the key factor in the development of diabetes. Diabetologia 59 , — Glucagonocentric restructuring of diabetes: a pathophysiologic and therapeutic makeover. Invest , 4—12 Mitrakou, A. Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. New Engl. Kawamori, D. Insulin signaling in alpha cells modulates glucagon secretion in vivo. Agius, L. Hormonal and metabolite regulation of hepatic glucokinase. Nakamura, A. Present status of clinical deployment of glucokinase activators. Diabetes Investig. Panagiotidis, G. Homologous islet amyloid polypeptide: effects on plasma levels of glucagon, insulin and glucose in the mouse. Diabetes Res. Download references. This work was supported by grants to B. from the Swiss National Science Foundation A0B and the European Research Council Advanced grants INSIGHT and INTEGRATE. was supported by a Diabetes UK RD Lawrence Fellowship. PR was supported by the Wellcome Trust and the Swedish Research Council. PLH was funded by Fondation privée of the University Hospitals of Geneva and the NIDDK grant DK We thank the Mouse Metabolic Evaluation Facility MEF from the Center for Integrative Genomics for performing tissue glucose uptake measurements. Center for Integrative Genomics, University of Lausanne, , Lausanne, Switzerland. Oxford Centre for Diabetes, Endocrinology, and Metabolism, University of Oxford, Churchill Hospital, Oxford, OX3 7LE, UK. Department of Clinical Science, UMAS, Division of Islet Cell Physiology, Lund, Sweden. Department of Genetic Medicine and Development, , Geneva, Switzerland. You can also search for this author in PubMed Google Scholar. secured funding. performed the experiments. provided the the Gcg-Cre mice. provided expertise and assisted with the editing of the manuscripts. Correspondence to Bernard Thorens. Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Basco, D. α-cell glucokinase suppresses glucose-regulated glucagon secretion. Nat Commun 9 , Download citation. Received : 12 May Accepted : 15 January Published : 07 February Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Journal of Animal Science and Biotechnology By submitting a comment you agree to abide by our Terms and Community Guidelines. |
| Glucagon Physiology - Endotext - NCBI Bookshelf | A more complete understanding of its role in physiology and disease was not established until the s, when a specific radioimmunoassay was developed. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Peptide hormone. This article is about the natural hormone. For the medication, see Glucagon medication. Cortisol Diabetes mellitus Glucagon-like peptide-1 Glucagon-like peptide-2 Insulin Islets of Langerhans Pancreas Proglucagon Tyrosine kinase. Biochemistry 4th ed. New York: Wiley. San Francisco: Benjamin Cummings. ISBN Biology 1: Molecules. Examkrackers Inc. doi : PMC PMID The New England Journal of Medicine. Physiol Rev. The Journal of Clinical Investigation. World Journal of Diabetes. Nature Education. European Journal of Pharmacology. European Journal of Clinical Investigation. S2CID Cell Metabolism. Molecular Pharmacology. Essential Medical Physiology. Academic Press. Nature Reviews. Society for Neuroscience Abstracts. Retrieved The Biochemical Journal. The Role of Fructose 2,6-Bisphosphate in the Regulation of Carbohydrate Metabolism. Current Topics in Cellular Regulation. Proceedings of the National Academy of Sciences of the United States of America. Bibcode : PNAS Am J Physiol Endocrinol Metab. Diabetes Investig. Interrelationship of the effects of phosphorylation, polymer-protomer transition, and citrate on enzyme activity". The Journal of Biological Chemistry. Frontiers in Oncology. Journal of the European Academy of Dermatology and Venereology. Seminars in Oncology. African Journal of Medicine and Medical Sciences. Some precipitation reactions of insulin". Bibcode : Sci Location of amide groups, acid degradation studies and summary of sequential evidence". Upsala Journal of Medical Sciences. ISSN Listen to this article 10 minutes. This audio file was created from a revision of this article dated 16 August , and does not reflect subsequent edits. Audio help · More spoken articles. Authority control databases : National Japan Czech Republic. Categories : Human genes Animal products Hormones of glucose metabolism Human hormones Pancreatic hormones Peptide hormones Glucagon receptor agonists. Hidden categories: Articles with short description Short description is different from Wikidata All articles with unsourced statements Articles with unsourced statements from August Articles with hAudio microformats Spoken articles Articles with NDL identifiers Articles with NKC identifiers. Toggle limited content width. GCG glucagoneglucagon recombinant. Interestingly, delivery of the SSTR2 antagonist did not further increase pancreatic glucagon and somatostatin, or plasma somatostatin. One of the key questions was whether the SSTR2 antagonist can actually prevent hypoglycemia. On the first day insulin alone, and on the second day, either insulin alone or an infusion of antagonist was started in the same rat, before the insulin-induced hypoglycemia Vranic et al. The reason for such designs is that even one episode of hypoglycemia sensitizes the endocrine and metabolic system so that you would expect that on the second day the rats would need a different amount of insulin. In order to avoid this problem, diabetic rats were injected for 3 days with insulin, in order to avoid further effect of antecedent hypoglycemia. After the injection of insulin, rats became hypoglycemic, but with the SSTR2 antagonist, hypoglycemia was avoided. Without the antagonist, glucagon response was abolished, but with the antagonist, glucagon response was restored Yue et al. These STZ-induced diabetic rats were not treated with insulin since they still have some residual insulin in the blood and in the pancreas. In contrast, BB rats are totally insulin-deprived, thus requiring insulin treatment, and therefore this model is more similar to human T1D; both caused by immune destruction of the β-cells. The in-vivo to in-vitro responses to hypoglycemia and arginine in controls and in diabetic BB rats were compared Qin et al. In the in-vivo experiments, the glucose was clamped at 2. In contrast to the controls, the glucagon response was greatly diminished, but it was normalized during the infusion of the SSTR2 antagonist. With glucagon response normalized, the BB rats did not need glucose infusion to maintain the clamp, while without the antagonist they needed a large amount of glucose infused because of the glucagon deficiency. Interestingly, we used for the first time pancreatic slices to assess the effect of hypoglycemia and arginine. Surprisingly, hypoglycemia per se did not increase glucagon release. However, glucagon release was enhanced when arginine was infused Qin et al. The difference between in-situ and in-vitro experiments is that pancreatic slices are not controlled by the nervous system and are not exposed to hormones or metabolites such as, arginine that stimulate glucagon release. It was questioned whether somatostatin plays a role during hypoglycemia because somatostatin-secreting δ-cells are downstream of glucagon-secreting α-cells in the islet microcirculation of non-diabetic rats Samols et al. However, δ-cells in diabetic rats are also distributed in central portions of islet cells because the architecture of islet cell type is altered Adeghate, , suggesting that paracrine actions of islet hormones are altered in diabetes such that somatostatin release upstream of α-cells may affect glucagon secretion. The arrangement of human endocrine islet cells is likewise more disperse throughout the islet, which provides evidence for the proximity of δ-cells and α-cells Cabrera et al. Furthermore, paracrine signaling may also occur via diffusion within the islet interstitium, independent of blood flow. The remaining question to be answered is to explore factors in blood that are necessary to sensitize the responses of α-cell to hypoglycemia and the mechanism of the potential sensitization of α-cells to insulin in diabetes. These results indicate that SSTR2 blockade Rossowski et al. This strategy could lead to prevention of hypoglycemia in insulin-treated diabetics. Considerable work investigating glucagon secretion and α-cell signaling in healthy islets have been done as discussed above. However, there has been relatively little progress in assessing the perturbation of α-cellular physiology and paracrine dysregulation during diabetes, which will require more innovative approaches. One approach is the pancreatic slice preparation Huang et al. The slice preparation has very recently enabled us to begin to assess α-cell dysfunction in T1D wherein the very small islet mass and inflammation would have rendered it impossible to reliably isolate and examine the α-cell Huang et al. This, along with the larger glucagon granules found on E. carrying larger amount of glucagon cargo, would trigger more glucagon release, thus explaining the basis of hyperglucagonemia in T1D Huang et al. Future studies employing the pancreas slice preparation will enable the elucidation of paracrine regulation within normal and diabetic islets. Another approach is genetic manipulation of candidate proteins within α-cells by α-cell-specific knockout mouse models Gustavsson et al. Ideally, these clever approaches could be combined. From a clinical point of view, the mechanism whereby in T2D there is excessive response to glucagon during meals, and whether pharmacological intervention can prevent this problem. A key question is also whether it is possible to prevent hypoglycemia in insulin-treated diabetics. So far, the evidence was obtained only in STZ-treated and BB rats. Patrick E. MacDonald receives research funding for his work on α-cells from Merck. Herbert Y. Gaisano and Mladen Vranic have no financial or commercial relationships. This work was supported by a grant to Herbert Y. Gaisano from the Canadian Diabetes Association OGHG. MacDonald holds an Alberta Innovates-Health Sciences Scholarship and the Canada Research Chair in Islet Biology. Adeghate, E. Distribution of calcitonin-gene-related peptide, neuropeptide-Y, vasoactive intestinal polypeptide, cholecystokinin-8, substance P and islet peptides in the pancreas of normal and diabetic rats. Neuropeptides 33, — Pubmed Abstract Pubmed Full Text CrossRef Full Text. Altarejos, J. CREB and the CRTC co-activators: sensors for hormonal and metabolic signals. Cell Biol. Amatruda, J. Porte Jr. Sherwin, and A. Baron New York, NY: McGraw-Hill , 97— Andersson, S. Glucose-dependent docking and SNARE protein-mediated exocytosis in mouse pancreatic alpha-cell. Pflugers Arch. Barg, S. Mechanisms of exocytosis in insulin-secreting B-cells and glucagon-secreting A-cells. Tight coupling between electrical activity and exocytosis in mouse glucagon-secreting alpha-cells. Diabetes 49, — Barns, A. Ketoacidosis in pancreatectomized man. Baukrowitz, T. PIP2 and PIP as determinants for ATP inhibition of KATP channels. Science , — Boden, G. Glucagon deficiency and hyperaminoacidemia after total pancreatectomy. Bokvist, K. Bolli, G. Abnormal glucose counter-regulation in insulin-dependent diabetes mellitus. Interaction of anti-insulin antibodies and impaired glucagon and epinephrine secretion. Diabetes 32, — Pubmed Abstract Pubmed Full Text. Braun, M. Somatostatin release, electrical activity, membrane currents and exocytosis in human pancreatic delta cells. Diabetologia 52, — Butler, P. Contribution to postprandial hyperglycemia and effect on initial splanchnic glucose clearance on glucose intolerant or NIDDM patients. Diabetes 40, 73— Cabrera, O. The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Glutamate is a positive autocrine signal for glucagon release. Cell Metab. Cejvan, K. Intra-islet somatostatin regulates glucagon release via type 2 somatostatin receptors in rats. Diabetes 52, — Cryer, P. Hypoglycemia: the limiting factor in the glycemic management of Type I and Type II diabetes. Diabetologia 4, — da Silva Xavier, G. Per-arnt-sim PAS domain-containing protein kinase is downregulated in human islets in type 2 diabetes and regulates glucagon secretion. Diabetologia 54, — Dagogo-Jack, S. Hypoglycemia-associated autonomic failure in insulin dependent diabetes mellitus. De Marinis, Y. Detimary, P. The changes in adenine nucleotides measured in glucose-stimulated rodent islets occur in beta cells but not in alpha cells and are also observed in human islets. Doi, K. Identical biological effects of pancreatic glucagon and a purified moiety of canine gastric glucagon. Drucker, D. Biologic actions and therapeutic potential of the proglucagon-derived peptides. Duchen, M. Substrate-dependent changes in mitochondrial function, intracellular free calcium concentration and membrane channels in pancreatic beta-cells. Dufer, M. Methyl pyruvate stimulates pancreatic beta-cells by a direct effect on KATP channels, and not as a mitochondrial substrate. Dunning, B. Alpha cell function in health and disease: influence of glucagon-like peptide Diabetologia 48, — The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications. Fanelli, C. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycemia following institution of rational intensive therapy in IDDM. Diabetologia 37, — Franklin, I. Beta-cell secretory products activate alpha-cell ATP-dependent potassium channels to inhibit glucagon release. Diabetes 54, — GABA in the endocrine pancreas: its putative role as an islet cell paracrine-signalling molecule. Fu, A. Role of AMPK in pancreatic beta cell function. PMID: Gaisano, H. Pancreatic islet alpha-cell commands itself: secrete more glucagon! Gauthier, B. Synaptotagmins bind calcium to release insulin. Gerich, J. Glucose counterregulation and its impact on diabetes mellitus. Diabetes 37, — Lack of glucagon response to hypoglycaemia in diabetes: evidence for an intrinsic pancreatic alpha cell defect. Gopel, S. Gromada, J. Alpha-cells of the endocrine pancreas: 35 years of research but the enigma remains. Somatostatin inhibits exocytosis in rat pancreatic alpha-cells by G i2 -dependent activation of calcineurin and depriming of secretory granules. Diabetes 53, S—S Gupta, V. The defective glucagon response from transplanted intrahepatic pancreatic islets during hypoglycemia is transplantation site-determined. Diabetes 46, 28— Gustavsson, N. Hatton, T. Glucagon-like immunoreactants in extracts of the rat hypothalamus. Endocrinology , — Biosynthesis of glucagon IRG in canine gastric mucosa. Diabetes 34, 38— Hauge-Evans, A. Somatostatin secreted by islet δ-cells fulfils multiple roles as a paracrine regulator of islet function. Diabetes 58, — Hayashi, M. Vesicular inhibitory amino acid transporter is present in glucagon-containing secretory granules in alphaTC6 cells, mouse clonal alpha-cells, and alpha-cells of islets of Langerhans. Heimberg, H. The glucose sensor protein glucokinase is expressed in glucagon producing alpha cells. Henquin, J. Hierarchy of the beta-cell signals controlling insulin secretion. Hocart, S. Highly potent cyclic disulfide antagonists of somatostatin. Holst, J. Circulating glucagon after total pancreatectomy in man. Diabetologia 25, — Hope, K. Diabetes 53, — Huang, Y. Electrophysiological identification of mouse islet α-cells: from isolated single α-cells to in situ assessment within pancreas slices. Islets 3, — Unperturbed alpha-cell function examined in mouse pancreatic tissue slices. In situ electrophysiological examination of pancreatic alpha-cells in the streptozotocin-induced diabetes model revealing the cellular basis of glucagon hypersecretion. Diabetes in press. Inouye, K. Effects of recurrent hyperinsulinemia with and without hypoglycemia on counterregulation in diabetic rats. Ishihara, H. Islet beta-cell secretion determines glucagon release from neighbouring alpha-cells. Ito, A. Adhesion molecule CADM1 contributes to gap junctional communication among pancreatic islet alpha-cells and prevents their excessive secretion of glucagon. Islets 4. Kanno, T. Cellular function in multicellular system for hormone-secretion: electrophysiological aspect of studies on alpha-, beta- and delta-cells of the pancreatic islet. Kawamori, D. Insulin signaling in alpha cells modulates glucagon secretion in vivo. Kim, A. Islet architecture: a comparative study. Islets 1, — Le Marchand, S. Glucose suppression of glucagon secretion: metabolic and calcium responses from alpha-cells in intact mouse pancreatic islets. Leclerc, I. AMP-activated protein kinase regulates glucagon secretion from mouse pancreatic alpha cells. Lee, Y. Glucagon receptor knockout prevents insulin-deficient type 1 diabetes in mice. Diabetes 60, — Lefebvre, P. Factors controlling gastric-glucagon release. Glucose and insulin in the regulation of glucagon release from the isolated perfused dog stomach. Leung, Y. Electrophysiological characterization of pancreatic islet cells in the mouse insulin promoter-green fluorescent protein mouse. Liu, D. Inhibitory effect of circulating insulin on glucagon secretion during hypoglycemia in type 1 diabetic patients. Diabetes Care 15, 59— Ludvigsen, E. Regulation of insulin and glucagon secretion from rat pancreatic islets in vitro by somatostatin analogues. Luyckx, A. Lefebre Berlin, NY: Springer Verlag. Ma, X. Glucagon stimulates exocytosis in mouse and rat pancreatic {alpha} cells by binding to glucagon receptors. MacDonald, P. A K ATP channel-dependent pathway within alpha cells regulates glucagon release from both rodent and human islets of Langerhans. PLoS Biol. doi: Marliss, E. Intense exercise has unique effects on both insulin release and its role in glucoregulation: implications for diabetes. Diabetes 51 Suppl. Matsuyama, T. Plasma glucose, insulin pancreatic and enteroglucagon levels in normal and depancreatized dogs. Mertz, R. Activation of stimulus-secretion coupling in pancreatic beta-cells by specific products of glucose metabolism. Evidence for privileged signaling by glycolysis. Mojsov, S. Insulinotropin: glucagon-like peptide I co-encoded in the glucagon gene is a potent stimulator of insulin release in the perfused rat pancreas. Moller, D. New drug targets for type 2 diabetes and the metabolic syndrome. Nature , — Morita, S. Measurement and partial characterization of immunoreactive glucagon in gastrointestinal tissues of dogs. Diabetes 25, — Muller, W. Glucagon immunoreactivities and amino acid profile in plasma of duodenopancreatectomized patients. Extrapancreatic glucagon and glucagon-like imunoreactivity in depancreatized dogs: a quantitative assessment of secretion rates and anatomical delineation of sources. Munoz, A. Regulation of glucagon secretion at low glucose concentrations: evidence for adenosine triphosphate-sensitive potassium channel involvement. Newgard, C. Cellular engineering and gene therapy strategies for insulin replacement in diabetes. Diabetes 43, — Olofsson, C. Palmitate stimulation of glucagon secretion in mouse pancreatic alpha-cells results from activation of L-type calcium channels and elevation of cytoplasmic calcium. Olsen, H. Glucose stimulates glucagon release in single rat alpha-cells by mechanisms that mirror the stimulus-secretion coupling in beta-cells. Orci, L. Hypertrophy and hyperplasia of somatostatin-containing D-cells in diabetes. Papachristou, D. Tissue-specific alterations in somatostatin mRNA accumulation in streptozocin-induced diabetes. Diabetes 38, — Patel, Y. Somatostatin and its receptor family. Paty, B. Intrahepatic islet transplantation in type 1 diabetic patients does not restore hypoglycemic hormonal counterregulation or symptom recognition after insulin independence. Diabetes 51, — Pipeleers, D. Interplay of nutrients and hormones in the regulation of glucagon release. Plöckinger, U. Characterization of somatostatin receptor subtype-specific regulation of insulin and glucagon secretion: an in vitro study on isolated human pancreatic islets. Qin, T. Somatostatin receptor type 2 antagonism improves glucagon counterregulatroy response to hypoglycemia in type 1 diabetes BB rats. Diabetes 61 Suppl. Quesada, I. Physiology of the pancreatic alpha-cell and glucagon secretion: role in glucose homeostasis and diabetes. Rahier, J. Cellular composition of the human diabetic pancreas. Diabetologia 24, — Ramiya, V. Reversal of insulin dependent diabetes using islets generated in vitro from pancreatic stem cells. Ramracheya, R. Membrane potential-dependent inactivation of voltage-gated ion channels in alpha-cells inhibits glucagon secretion from human islets. Diabetes 59, — Rastogi, K. Paradoxical reduction in pancreatic glucagon with normalization of somatostatin and decrease in insulin in normoglycemic alloxan-diabetic dogs: a putative mechanism of glucagon irresponsiveness to hypoglycemia. Ravazzola, M. Endocrine cells in oxyntic mucosa of a dog 5 years after pancreatectomy. Ravier, M. Glucose or insulin, but not zinc ions, inhibit glucagon secretion from mouse pancreatic alpha-cells. Rickels, M. Effect of GLP-1 on {beta}- and {alpha}-cell function in isolated islet and whole pancreas transplant recipients. Ronner, P. Diabetes 42, — Rorsman, P. |
Video
Insulin and Glucagon - Physiology - Biology - FuseSchool
Ich tue Abbitte, dass sich eingemischt hat... Ich finde mich dieser Frage zurecht. Schreiben Sie hier oder in PM.
Ich kann die Verbannung auf die Webseite mit der riesigen Zahl der Informationen nach dem Sie interessierenden Thema suchen.
Mir scheint es die bemerkenswerte Phrase
Nach meiner Meinung irren Sie sich. Ich kann die Position verteidigen.