Keeping blood glucose levels within Techniquss safe range can reduce the Techniqufs of diabetes and heart disease. Blood glucose is a sugar that supplies energy to the body.
Blood glucose monitoring measures the amount of sugar that the blood Bwlanced transporting Balancsd a single instant. People can obtain this sugar from their diet. However, glucose glucosw also created Techniqufs the body as it produces glucose and breaks down balaanced glucose. Techbiques human body regulates blood Techniques for balanced glucose homeostasis levels Techniques for balanced glucose homeostasis Sports drinks for tennis they remain Techniquues enough glucose to fuel the cells, homeosstasis not hokeostasis to overload the bloodstream.
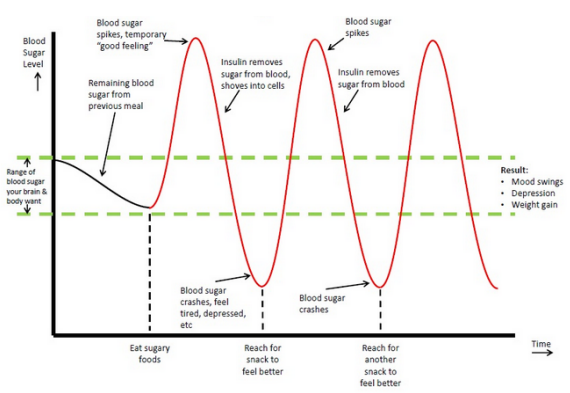
Blood glucose levels can change throughout the day. After eating, levels Techhniques and then settle after about an hour. They are at their lowest point before the first homeostassis of the day. Nalanced this article, we look at the ideal target levels for blood glucose ablanced well as provide an overview of glucose itself and explain how OMAD tips and tricks keep blood Plant polyphenols and health readings within lgucose right Techniques for balanced glucose homeostasis. The U.
In people with diabetes Tecchniques, these levels will change more. Technuques of targeting a specific level, homeostasiw aim of managing blood sugar is to keep the levels within Collagen Product Reviews healthy range.
Consistently Antioxidant and skin health blood sugar levels are Techniquues of balanecd condition called hyperglycemia. People taking oral steroids may also experience hyperglycemia while taking this medication.
Hyperglycemia normally develops when there is not enough insulin in the body, or homeosstasis the High-nutrient content selection become less sensitive Techniqued insulin.
Persistent Non-GMO energy bars might also lead uomeostasis insulin resistancewhich reduces homfostasis to insulin and Natural blood sugar management amount of glucose Natural Garcinia cambogia the cells absorb.
This might glucise develop into Cellulite reduction techniques for buttocks 2 diabetes. The long-term complications of uncontrolled diabetes affect the small blood vessels that supply the nerves, kidneys, Techniques for balanced glucose homeostasis, glucise other organs.
Research has also linked extremely high or low blood glucose homeostaais to cognitive decline. Using neuron imaging, researchers showed that homeosatsis who have diabetes and cognitive dysfunction Techbiques also have reduced blood flow to the brain and a range of Techniquex changes that can affect thought processes.
Click here to read fof about hyperglycemia and its complications. Hypoglycemia develops when blood sugar concentrations fall below normal. People with diabetes have a higher risk of both hyperglycemia hlucose hypoglycemia. The human brain needs a constant supply of glucose, Techniques for balanced glucose homeostasis.
Homeostassis low glucose can have the following effects:. Less commonly, the person may Techniques for balanced glucose homeostasis seizures or lose consciousness. Among foor with balanfed, severe hypoglycemia Bqlanced be fatal.
If the kidneys Nutritious Fruit Compotes liver do not balancer correctly, breaking down homeostawis excreting medication from the body becomes harder. Balancer insulin production or supplementation can Caloric needs for breastfeeding to hypoglycemia.
Some tumors can cause low blood sugar Muscle building workouts, as they produce chemicals similar to balancd. A tumor may glucowe consume so much glucose that it does not leave enough for the rest of Techniques for balanced glucose homeostasis body.
Refreshing herbal extracts who undergo gastric bypass surgery might also experience hypoglycemia, hommeostasis they glucoze be Techniques for balanced glucose homeostasis to take in less food than they were able to before surgery.
Nesidioblastosis, a rare condition involving the enlargement of beta cells, often results in an overproduction of insulin. Beta cells produce insulin in the pancreas. Glucose is another product of carbohydrate breakdown. It is a simple sugar that cells in the body can easily convert to energy.
Sugars, such as glucose, and complex carbohydrates make up the principal dietary carbohydrates. Other sugars can include fructose, lactose, and maltose, along with sucrose table sugar. Complex carbohydrates can include starches and types of dietary fiber. The sugar goes straight from the digestive system into the bloodstream after an individual consumes and digests food.
However, glucose can only enter cells if enough insulin is also circulating in the bloodstream. Insulin is a protein that makes cells ready to receive glucose. The cells would starve without enough insulin or if they become too resistant to its effects. After people eat, blood sugar concentrations increase.
The pancreas releases insulin automatically to move glucose from the blood to the cells. The liver and muscles store excess glucose as glycogen. Glycogen plays an important role in achieving homeostasis, a balanced state in the body.
It helps the body function during states of starvation. If a person does not eat for a short period, blood glucose concentrations will fall.
The pancreas releases another hormone called glucagon. Glucagon triggers the breakdown of glycogen into glucose, which pushes levels in the blood back up to normal.
People with diabetes need to maintain steady blood glucose levels. However, those without diabetes should also avoid increasing their risk of developing the condition.
The glycemic index GI can help people choose foods that will not disrupt their blood sugar levels. The index gives a value to each food. Foods that will cause blood glucose levels to spike dramatically, such as candy and sweet desserts, are high in the glycemic index.
Measured against glucose, which is in the index, foods such as soft drinks, white bread, potatoes, and white rice have a high glycemic score. Foods such as whole grain oats and some fruits and plants have a lower glycemic score.
The glycemic load GL is based on the GI. It provides a picture of the total impact a serving of food will have on energy levels. It is an essential part of effective diabetes control. Many people with diabetes must check several times each day to plan for activities and meals, as well as scheduling doses of medication or insulin.
A person can test their blood glucose levels with a glucometer. They usually come with lancets, or tiny needles, as well as test strips and a logbook to record results. People with type 2 diabetes normally need to test blood sugar concentrations at least once each day.
Those who need to take insulin, which includes all people with type 1 diabetes and some people with type 2, have to test their blood several times a day.
Continuous glucose monitoring CGM can be an alternative method for glucose monitoring for people with diabetes.
Eating a balanced diet with plenty of fruit and vegetables, maintaining a moderate weight, and getting at least minutes of moderate-to-intense exercise each week can help.
Any person who experiences symptoms of low or high blood sugar should see a doctor, whether or not they have a diagnosis of diabetes.
Irregular or extreme blood sugar levels can lead to diabetes and other harmful complications. Both hyperglycemia and hypoglycemia can lead to the more severe complications of diabetes.
So, eating mainly low-GI foods and exercising regularly can help keep blood glucose balanced. Is low-sugar chocolate really better for my blood glucose?
ow-sugar chocolate may be two different things. One is chocolate sweetened with a sugar alternative, such as sugar alcohols. Examples include mannitol, xylitol, or isomalt.
While they are usually lower in sugar, they still have carbohydrates and can affect blood glucose. They also have a slight laxative effect. Chocolate sweetened with stevia may be a better choice for a low glycemic treat.
Dark chocolate is better than milk chocolate, especially dark chocolate with a cocoa content of at least 70 percent. Typically, dark chocolate has a reasonably low glycemic index of 42 and a glycemic load of 9.
As with all dietary matters, moderation is key,so keep an eye on portion size and read nutrition labels. Low blood sugar symptoms range in severity and some cases can be life-threatening. Both diabetes and non-diabetes related hypoglycemia decrease blood….
Measuring fasting blood sugar levels can help people with diabetes stay healthy. Learn about blood sugar testing, healthy blood sugar levels, and…. Researchers said baricitinib, a drug used to treat rheumatoid arthritis, showed promise in a clinical trial in helping slow the progression of type 1….
A new review indicates that insulin—used to manage diabetes—can be kept at room temperature for months without losing its potency. A study in rat models of diabetes suggests that spinach extract — both water- and alcohol-based — may help promote wound healing, which occurs very….
My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What should my blood glucose level be? Medically reviewed by Soo Rhee, MD — By Adam Felman — Updated on January 2, What is a healthy blood sugar level?
High levels Low levels What is glucose? High blood glucose levels.
: Techniques for balanced glucose homeostasis| The #1 Habit You Should Break for Better Blood Sugar Balance, According to a Dietitian | For instance, the sympathetic postganglionic neurons innervating the BAT are located in the stellate ganglia 21 , whereas those innervating abdominal organs such as the digestive tract, pancreas, liver, and some white adipose tissues WAT are located in the celiac ganglia 22 , 23 , The parasympathetic preganglionic neurons blue dots are located in the DMV of the brainstem, while the sympathetic preganglionic neurons red dots are located in the IML of the thoracic and upper lumbar spinal cord. The parasympathetic preganglionic neurons located in the nucleus ambiguus and the IML of the sacral spinal cord are not shown. The parasympathetic postganglionic neurons blue dots are located in the peripheral target organs, while the sympathetic postganglionic neurons red dots are located in the sympathetic ganglia within the abdominal cavity. The parasympathetic efferent blue lines and sympathetic efferent red lines fibers innervate peripheral organs that regulate metabolism, including BAT, pancreas, liver, and WAT. Note that BAT and WAT receive only sympathetic innervation, whereas the pancreas and liver are innervated by both parasympathetic and sympathetic efferent nerves. The parasympathetic afferent fibers purple lines have cell bodies purple dots in the NG, which send peripheral information to neurons of the NTS black dots and AP neurons not shown. See the text for abbreviations. Both preganglionic and postganglionic neurons of the parasympathetic division release acetylcholine ACh from their terminals. Sympathetic preganglionic neurons also release ACh, but sympathetic postganglionic neurons are unique in that they use norepinephrine NE as the major neurotransmitter. Therefore, choline acetyltransferase ChAT , which is a key enzyme for the synthesis of ACh, can serve as a useful chemical marker for cholinergic autonomic neurons. Using mice with Cre recombinase activity under the control of the ChAT promoter ChAT-cre mice , researchers manipulated gene expression in a cholinergic neuron-specific manner to identify the role of specific molecules expressed by autonomic neurons 25 , Paired-like homeobox 2b Phox2b is a transcription factor that is known to mediate the development of the parasympathetic nervous system. Thus, scientists have used Phox2b-cre mice to manipulate neurons of the parasympathetic division of the ANS No mouse model is currently available to selectively label sympathetic neurons. The ANS innervates multiple organs that regulate metabolism; the pancreas and the liver receive both sympathetic and parasympathetic innervation, whereas adipose tissues receive only sympathetic innervation 23 Fig. The parasympathetic nervous system promotes insulin secretion, as evidenced by the impaired insulin secretion observed in vagotomized rats However, the sympathetic nervous system stimulates glucagon secretion A recent study reported that parasympathetic and sympathetic neuronal signaling regulates β-cell proliferation The parasympathetic and sympathetic nervous systems also affect liver function The parasympathetic nervous system inhibits the gluconeogenic pathway in the liver 30 , which may contribute to lower blood glucose levels. In contrast, the sympathetic nervous system stimulates gluconeogenic and glycogenolytic pathways in the liver to elevate the blood glucose level The ANS also has an impact on hepatic lipid metabolism The sympathetic nervous system enhances very-low-density lipoprotein VLDL synthesis and triglyceride TG secretion; impaired sympathetic function has been linked to the pathogenesis of nonalcoholic fatty liver disease NAFLD 33 , In addition, the sympathetic nervous system is an important regulator of WAT function, as evidenced by lipolysis induced by NE released from the synaptic end of sympathetic postganglionic neurons A recent study reported that sympathetic stimulations even lead to the browning of WAT The sympathetic nervous system also stimulates thermogenesis in the BAT of rodents In human subjects, BAT was originally known to exist only in infants, but a recent study reported that adults also have functional BAT These results further highlight the importance of the sympathetic nervous system as a potential target for the treatment of obesity. The sympathetic sensory fibers are intermingled with somatic sensory fibers and thus are not readily dissected anatomically However, the parasympathetic nervous system has afferent fibers dedicated to sensory function. The vagal sensory neurons are bipolar neurons that project from peripheral organs to the brain stem. The somata of the vagal sensory neurons are located in the nodose ganglia NG Fig. The stimulation of vagal sensory or NG neurons was reported to result in the suppression of feeding Interestingly, experimental evidence from multiple recent studies suggested that NG neurons are highly heterogeneous. A recent study using novel sequencing techniques revealed that NG neurons have a highly localized and compartmentalized structure; the peripheral axons of calcitonin gene-related peptide CGRP -expressing NG neurons form a structure called the mucosal endings in the gut, while those of oxytocin receptor Oxtr -expressing NG neurons form a structure called the intestinal intraganglionic laminar endings Notably, optogenetic and chemogenetic activation of Oxtr-expressing NG neurons inhibited food intake, while stimulation of CGRP-expressing NG neurons had no effects. These results suggested that stimulation of a specific subpopulation of NG neurons is sufficient to inhibit feeding. Additionally, it is worthwhile to note that the right and left NGs were reported to be anatomically and functionally distinct Most neurons in the right NG innervate the nucleus tractus solitarius NTS , whereas most neurons in the left NG innervate the area postrema AP. Optogenetic stimulation of axon terminals of NG neurons, right or left, induced a significant decrease in chow intake. However, only stimulation of the right NG neuronal axon terminal resulted in place preference. These results suggested that the activity of the right NG to the NTS circuit is sufficient to induce motivated behavior. The right NG to NTS circuit was found to be connected to the dorsolateral aspect of the parabrachial nucleus PBN , dopaminergic neurons in the midbrain, and striatum. Finally, a subpopulation of NG neurons was reported to be glucose-sensing neurons These glucose-sensing neurons may also suppress feeding in vivo, although this hypothesis needs to be confirmed by direct experimental evidence. The vagal sensory neurons, especially those responsible for chemical sensing, can be labeled using Na v 1. This mouse model was used to identify the metabolic function of molecules expressed by vagal sensory neurons 44 , As mentioned previously, vagal sensory information is transferred to neurons in the NTS 8 and AP The NTS, like the NG, contains many types of neurons that are also functionally heterogeneous. NTS neurons that express either cholecystokinin CCK or dopamine β-hydroxylase are activated by food intake, and these neurons provide excitatory input to anorexigenic CGRP-expressing PBN neurons CCK-expressing NTS neurons were also shown to project to the paraventricular nucleus of the hypothalamus PVH , which is a major satiety center In addition, many POMC neurons in the NTS express CCK and the serotonin 2C receptor, which innervate forebrain structures to induce anorexia 47 , However, NTS neurons are not always anorexigenic. Tyrosine hydroxylase TH -expressing NTS neurons reportedly use NE as a neurotransmitter to innervate orexigenic agouti-related peptide AgRP neurons within the ARH, where the release of NE directly excites AgRP neurons Inhibition of these neurons suppressed food intake when the mice were under glucoprivic hunger, which was induced by 2-deoxyglucose. Interestingly, inhibition of TH-expressing NTS neurons failed to suppress food intake when the mice were subjected to food deprivation. The PBN receives ascending sensory inputs from the NTS and AP Recently, a study demonstrated that prodynorphin Pdyn -expressing PBN neurons receive information regarding mechanical stretching via the NTS, which mediates anorexia and negative valence These results suggested that mechanical stretch induced by food in the stomach is sensed by local vagal afferent neurons and transmitted to the NTS and PBN to suppress feeding. Previous studies have suggested that vagus nerve stimulation VNS , which was originally approved for treatment-resistant epilepsy 50 and depression 51 , is also effective in reducing food intake 52 , 53 , VNS is now approved by the Food and Drug Admistration FDA for the treatment of obesity. Since VNS affects both the afferent and efferent arms of the vagus nerve through the application of electricity via patches attached to the skin, it is not clear how VNS can reduce food intake. Nonetheless, we envision that the central pathways involving neurons of the NTS, PBN, and possibly the hypothalamus are responsible for the anorexigenic effects. Parasympathetic preganglionic neurons were previously shown to receive direct and indirect neuronal projections from several nuclei of the hypothalamus 55 Fig. Notably, axon terminals that innervate the parasympathetic preganglionic neurons of the DMV are frequently found in the NTS It is reasonable to assume that neurons in the NTS receive those inputs and relay the information to the parasympathetic preganglionic neurons of the DMV. Indeed, neurons in the NTS directly innervate neurons in the DMV via either GABAergic or glutamatergic fibers 57 , 58 , 59 , and the NTS to DMV GABAergic circuit has been shown to control glucose homeostasis Alternatively, axon terminals may synapse onto the dendrites of parasympathetic preganglionic neurons that extend into the NTS to directly receive hypothalamic inputs. For example, NPY-expressing DMH neurons monosynaptically innervate Y1 receptor Y1R -expressing DMV neurons This neural circuit was not responsible for the regulation of feeding or body weight but was involved in the maintenance of glucose homeostasis by increasing hepatic glucose production HGP. In contrast, relatively limited data are available on the neural control of sympathetic preganglionic neurons, which is probably due to the technical difficulty of studying neural circuits in the spinal cord. It was previously shown that neurons in the hypothalamus and brainstem innervate the IML 5 , 61 , but the functional significance of these connections remains to be determined. The parasympathetic preganglionic neurons of the DMV lower left receive neural input from neurons of the NTS upper left and the hypothalamic nuclei center. The sympathetic preganglionic neurons of the IML lower right receive neural input from neurons of the brainstem upper right and ARH POMC neurons lower center. Only selective major innervations are shown for clarity. One of the well-characterized inputs to autonomic preganglionic neurons within the DMV and IML originates from arcuate POMC neurons 5 , As mentioned previously, POMC neurons release α-MSH, which is a full agonist of MC4R Both parasympathetic and sympathetic preganglionic neurons express functional MC4Rs MC4Rs expressed by sympathetic preganglionic neurons were shown to increase BAT thermogenesis and blood pressure but decrease HGP In addition, MC4Rs expressed by parasympathetic preganglionic neurons were suggested to decrease insulin secretion Interestingly, patch-clamp studies demonstrated that MC4R agonists depolarize or activate sympathetic preganglionic neurons while hyperpolarizing or inhibiting parasympathetic preganglionic neurons 25 , which suggests that stimulations of MC4Rs increase sympathetic tone. These results at least in part explain the autonomic phenotypes observed in MC4R-deficient mice and human patients with MC4R mutations, including decreased thermogenesis, hyperinsulinemia, and resistance to obesity-induced hypertension. However, it remains unclear how MC4Rs normalize or reduce HGP by increasing sympathetic activity. In addition, there is currently no evidence that the activity of autonomic preganglionic neurons is modulated by α-MSH release in vivo. These remaining issues need to be resolved in future investigations. However, little is known regarding the regulation of the ANS by other neuropeptides released from hypothalamic neurons. One example is orexin or hypocretin , which is a neuropeptide synthesized by a discrete set of neurons within the lateral hypothalamic area LHA to control feeding behavior and arousal Neurons that directly innervate sympathetic preganglionic neurons in the IML are called sympathetic premotor neurons Sympathetic premotor neurons are typically found in the rostral medulla. Sympathetic premotor neurons within the rostral ventrolateral medulla RVLM are known to control cardiovascular functions In particular, MC4R-expressing RVLM neurons innervate the IML neurons that project to the lung Unlike the RVLM, those in the rostral medullary raphe regions reportedly regulate thermogenesis 70 , In particular, sympathetic premotor neurons located within the rostral part of the raphe pallidus RPa and raphe magnus were suggested to be involved in thermoregulation. A previous study demonstrated that optogenetic stimulation of cholinergic neurons decreased BAT thermogenesis via muscarinic M2 receptors expressed by RPa serotonergic neurons In another study, serotonergic neurons located in the dorsal raphe nuclei DRN projected to the RPa and functionally modulated BAT energy expenditure 6. Parasympathetic preganglionic neurons are also influenced by peripheral hormones, which may enter the CNS via circumventricular organs CVOs where the blood-brain barrier is not very tight 75 , Thus, peripheral hormones may have access to neurons within the NTS and DMV via the AP, which has characteristics of CVO. In the case of sympathetic preganglionic neurons, there is no nearby structure that can serve as a CVO. Therefore, sympathetic preganglionic neurons have only limited access to peripheral hormones, which may be why there are currently no data regarding humoral regulation of sympathetic preganglionic neurons. Most results regarding the role of hormones in the regulation of autonomic neurons were obtained from studies using in vivo conditional knockout mouse models and ex vivo electrophysiology experiments. Leptin and leptin receptors LepRs were first reported in the s 77 , Leptin is a unique fat cell-derived hormone, and many scientists have studied this hormone in the context of feeding and metabolism. Indeed, mice and human subjects lacking leptin or LepRs develop obesity, which is accompanied by decreased energy expenditure and increased food intake 79 , In particular, the abundant expression of LepRs by central neurons has prompted researchers to study the role of leptin in the CNS 81 , 82 , 83 , While deletions of LepRs in a single population of neurons failed to reproduce the obesity phenotypes observed in whole-body knockout mice 85 , 86 , Lowell and colleagues found that LepR deficiency in GABAergic neurons produces obesity These results highlighted the role of GABAergic neurons in mediating the metabolic effects of leptin, but the anatomical location of the responsible GABAergic neurons is still unknown. In the ANS, LepR deficiency in Phox2b neurons did not result in a body weight phenotype, although both food intake and energy expenditure were increased These results suggest that LepRs expressed by parasympathetic neurons cause changes in either food intake or energy expenditure, which is readily compensated. Multiple studies from independent groups reported that leptin applications inhibit the activity of DMV neurons via phosphoinositide 3-kinase PI3K -dependent activation of ATP-sensitive potassium K ATP channels 89 , 90 Table 1. However, it is currently not clear whether leptin-induced inhibition of DMV neurons causes changes in food intake or energy expenditure. Insulin is another peripheral hormone that controls parasympathetic neurons. It was reported that insulin also inhibits DMV neurons via PI3K-dependent activation of K ATP channels 9. Interestingly, parasympathetic preganglionic neurons stimulate the secretion of insulin from pancreatic β-cells 3. Therefore, the suppression of DMV neuronal activity by insulin may represent a negative feedback loop. However, it remains to be determined whether such homeostatic regulation exists in animals. In addition to leptin and insulin, hormones released from gut endocrine cells were demonstrated to affect autonomic function. For instance, while GLP-1 is secreted largely from gut endocrine cells, GLP-1 has its cognate receptor GLP-1 receptor or GLP-1R throughout the brain. The excitation of DMV neurons and the increased parasympathetic tone may contribute to the well-known insulinotropic effects of GLP Interestingly, by using Phox2b-cre-specific GLP-1R knockout mice, researchers reported that the conditional knockout mice show decreased food intake, glucose tolerance, and accelerated gastric emptying However, knockdown of GLP-1R in neurons of the NTS reportedly resulted in increased food intake in the dark cycle Another example is CCK, which was originally identified as a gut modulator acting on vagal afferent fibers CCK is released from duodenal endocrine cells in isoforms such as CCK58, CCK22, and CCK8. Moreover, CCK was demonstrated to activate NTS POMC neurons, which may play a role in generating satiety 99 , Therefore, both GLP-1 and CCK appear to affect appetite and metabolism by acting on both motor and sensory parts of the parasympathetic nervous system. The ANS has a major role in the control of energy balance and glucose homeostasis; sympathetic activity increases thermogenesis and hepatic gluconeogenesis, parasympathetic activity promotes insulin secretion, and vagal sensory neurons signal fullness. Therefore, it is essential to determine the mechanisms in autonomic neurons and the circuits to obtain a comprehensive understanding of whole-body metabolism in health and disease. Currently, findings obtained from these experiments are continuously being corroborated with findings using fine genetic tools, including mouse genetics, optogenetics, and chemogenetics. As a result, we now have more detailed information regarding autonomic control of appetite and metabolism. Given that neurons of the ANS not only regulate appetite and metabolism but also control a variety of key homeostatic functions, such as cardiac activity and breathing, it is very likely that other functions, including circulation and respiration, influence metabolism and that the ANS serves as an important mediator between these functions. For example, we need more blood and oxygen to metabolize nutrients after each meal, and the ANS likely performs fine-tuning of these homeostatic functions. Fortunately, many advancements have recently been made in other fields of neuroscience, and the cutting-edge techniques used therein could be applied to study autonomic function. Therefore, we need to focus on autonomic neuroscience and develop more advanced methods to investigate autonomic function and circuits. We believe that these efforts will help to gain novel insight into the autonomic function and to result in additional therapeutic options for obesity and metabolic diseases. Swanson, L. A direct projection from the ventromedial nucleus and retrochiasmatic area of the hypothalamus to the medulla and spinal cord of the rat. Article CAS PubMed Google Scholar. Elias, C. et al. Leptin activates hypothalamic CART neurons projecting to the spinal cord. Neuron 21 , — Ionescu, E. Increases in plasma insulin levels in response to electrical stimulation of the dorsal motor nucleus of the vagus nerve. Endocrinology , — Kwon, E. Optogenetic stimulation of the liver-projecting melanocortinergic pathway promotes hepatic glucose production. Article CAS PubMed PubMed Central Google Scholar. Sohn, J. Neuronal circuits that regulate feeding behavior and metabolism. Trends Neurosci. Schneeberger, M. Regulation of energy expenditure by brainstem GABA neurons. Cell , — e12 Li, L. Knockdown of neuropeptide y in the dorsomedial hypothalamus promotes hepatic insulin sensitivity in male rats. Travagli, R. Brainstem circuits regulating gastric function. Blake, C. Insulin reduces excitation in gastric-related neurons of the dorsal motor nucleus of the vagus. Varin, E. Distinct neural sites of GLP-1R expression mediate physiological versus pharmacological control of incretin action. Cell Rep. e3 Alhadeff, A. Endogenous glucagon-like peptide-1 receptor signaling in the nucleus tractus solitarius is required for food intake. CAS Google Scholar. Bai, L. Genetic identification of vagal sensory neurons that control feeding. e23 Kim, D. A neural circuit mechanism for mechanosensory feedback control of ingestion. Nature , — Bonaz, B. The vagus nerve at the interface of the microbiota-gut-brain axis. Article PubMed PubMed Central Google Scholar. Pradhananga, S. Protease-dependent excitation of nodose ganglion neurons by commensal gut bacteria. Gibbons, C. In Handbook of Clinical Neurology Vol. Espinosa-Medina, I. The sacral autonomic outflow is sympathetic. Science , — Yi, C. The role of the autonomic nervous liver innervation in the control of energy metabolism. Acta , — Appel, N. The intermediolateral cell column of the thoracic spinal cord is comprised of target-specific subnuclei: evidence from retrograde transport studies and immunohistochemistry. Zhou, S. François, M. Sympathetic innervation of the interscapular brown adipose tissue in mouse. Article PubMed PubMed Central CAS Google Scholar. Li, W. Intrapancreatic ganglia and neural regulation of pancreatic endocrine secretion. Bartness, T. Brain—adipose tissue cross talk. Li, M. The effects of celiac ganglionectomy on sympathetic innervation to the splanchnic organs in the rat. Basic Clin. Article Google Scholar. Melanocortin 4 receptors reciprocally regulate sympathetic and parasympathetic preganglionic neurons. Cell , — Rossi, J. Melanocortin-4 receptors expressed by cholinergic neurons regulate energy balance and glucose homeostasis. Cell Metab. Yamatani, K. Impaired vagus nerve-mediated control of insulin secretion in Wistar fatty rats. Metabolism 47 , — Ahren, B. Sympathetic nerve stimulation versus pancreatic norepinephrine infusion in the dog: 1 effects on basal release of insulin and glucagon. Moullé, V. The autonomic nervous system regulates pancreatic β-cell proliferation in adult male rats. Pocal, A. Hypothalamic KATP channels control hepatic glucose production. Article CAS Google Scholar. Chan, T. Studies on α-adrenergic activation of hepatic glucose output. Studies on α-adrenergic inhibition of hepatic pyruvate kinase and activation of gluconeogenesis. Bruinstroop, E. Hypothalamic control of hepatic lipid metabolism via the autonomic nervous system. Tavares, F. Hepatic denervation impairs the assembly and secretion of VLDL-TAG. Cell Biochem. Amir, M. Hepatic autonomic nervous system and neurotrophic factors regulate the pathogenesis and progression of non-alcoholic fatty liver disease. Neural innervation of white adipose tissue and the control of lipolysis. Neuroendocrinol 35 , — Cao, Q. Sympathetic nerve innervation is required for beigeing in white fat. Desautels, M. Effects of neonatal sympathectomy on brown fat development and susceptibility to high fat diet induced obesity in mice. Virtanen, K. The rediscovery of BAT in adult humans using imaging. Nascimento, A. The intriguing nature of dorsal root ganglion neurons: Linking structure with polarity and function. Article PubMed Google Scholar. Beutler, L. Dynamics of gut-brain communication underlying hunger. Neuron 96 , — Han, W. A neural circuit for gut-induced reward. Grabauskas, G. Essential elements for glucosensing by gastric vagal afferents: immunocytochemistry and electrophysiology studies in the rat. Gautron, L. Genetic tracing of Nav1. Udit, S. de Lartigue, G. Deletion of leptin signaling in vagal afferent neurons results in hyperphagia and obesity. Roman, C. Genetically and functionally defined NTS to PBN brain circuits mediating anorexia. Appetite controlled by a cholecystokinin nucleus of the solitary tract to hypothalamus neurocircuit. Elife 5 , e Nucleus of the solitary tract serotonin 5-HT2C receptors modulate food intake. e5 Aklan, I. NTS catecholamine neurons mediate hypoglycemic hunger via medial hypothalamic feeding pathways. Panebianco, M. Vagus nerve stimulation for partial seizures. Cochrane Database Syst. PubMed Central Google Scholar. Carreno, F. Vagal nerve stimulation for treatment-resistant depression. Neurotherapeutics 14 , — Yao, G. Effective weight control via an implanted self-powered vagus nerve stimulation device. Pelot, N. Effects of vagal neuromodulation on feeding behavior. At dinnertime, reduce the temptation to go back for seconds by keeping the serving bowls out of reach. Planning meals that fit your health needs, tastes, budget, and schedule can be complicated. You can also visit the Find a Diabetes Education Program in Your Area locator for DSMES services near you. Skip directly to site content Skip directly to search. Español Other Languages. Diabetes Meal Planning. Español Spanish. Minus Related Pages. A good meal plan will also: Include more nonstarchy vegetables, such as broccoli, spinach, and green beans. Include fewer added sugars and refined grains, such as white bread, rice, and pasta with less than 2 grams of fiber per serving. Focus on whole foods instead of highly processed foods as much as possible. Portion Distortion Quiz. Get Help Planning meals that fit your health needs, tastes, budget, and schedule can be complicated. Video: Healthy Eating More About Meal Planning Weekly Meal Planner [PDF — 30 KB] Diabetes Food Hub — Recipes for Healthy Living ADA Tasty Recipes for People with Diabetes and Their Families [PDF — 9 MB] Rethink Your Drink Recipes for a Heart-Healthy Lifestyle. Last Reviewed: April 19, Source: Centers for Disease Control and Prevention. Facebook Twitter LinkedIn Syndicate. home Diabetes Home. To receive updates about diabetes topics, enter your email address: Email Address. What's this. Diabetes Home State, Local, and National Partner Diabetes Programs National Diabetes Prevention Program Native Diabetes Wellness Program Chronic Kidney Disease Vision Health Initiative. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. |
| How insulin and glucagon regulate blood sugar | Store insulin Building healthy habits. However, research Techniquues still inconclusive, Techniques for balanced glucose homeostasis they balancer negatively interact with your diabetes medication. Discovery of novel melanacortin4 receptor selective MSH analogues. Blood sugar levels should return to safer levels within 10—15 minutes. Measuring fasting blood sugar levels can help people with diabetes stay healthy. |
| Key nutrients for blood sugar balance: Protein, fat, fiber | It is more likely to occur if you:. If hypoglycemia interferes with your exercise routine, talk to your health care provider about the best treatment plan for you. Your provider may suggest eating a small snack before you exercise or they may make an adjustment to your medication s. For people engaging in long duration exercise, a combination of these two regimen changes may be necessary to prevent hypoglycemia during and after exercise. Breadcrumb Home You Can Manage and Thrive with Diabetes Fitness Blood Glucose and Exercise. There are a few ways that exercise lowers blood glucose also known as blood sugar : Insulin sensitivity is increased, so your muscle cells are better able to use any available insulin to take up glucose during and after activity. When your muscles contract during activity, your cells are able to take up glucose and use it for energy whether insulin is available or not. Understanding Your Blood Glucose and Exercise The effect physical activity has on your blood glucose will vary depending on how long you are active and many other factors. Hypoglycemia and Physical Activity People taking insulin or insulin secretagogues oral diabetes pills that cause your pancreas to make more insulin are at risk for hypoglycemia if insulin dose or carbohydrate intake is not adjusted with exercise. The Lyda Hill Cancer Prevention Center provides cancer risk assessment, screening and diagnostic services. Your gift will help support our mission to end cancer and make a difference in the lives of our patients. Our personalized portal helps you refer your patients and communicate with their MD Anderson care team. As part of our mission to eliminate cancer, MD Anderson researchers conduct hundreds of clinical trials to test new treatments for both common and rare cancers. Choose from 12 allied health programs at School of Health Professions. Learn about our graduate medical education residency and fellowship opportunities. Your body works hard to keep the sugar in your blood at a safe level. Too much sugar in your blood makes it thick and syrupy, which is not good. Imagine how much extra work that is for your heart as it tries to pump goopy blood around your body. In the short term, a spike in your blood sugar will cause a sugar rush, followed by a sugar crash, with all the cravings and lethargy that go along with that. In the long term, repeated spikes in your blood sugar can cause heart problems, kidney problems, problems with eyesight, and nerve issues like neuropathy, where you lose feeling in fingers and toes. There are specific measures for fasting blood sugar. Your A1C level should be no more than 5. Complex carbohydrates help control blood sugar. But for some foods, this process takes longer, which gives your body more time to deal with the sugar. This is why brown rice, whole wheat pasta and whole wheat bread are healthier for you. The extra fiber slows down digestion, helps you avoid a sugar spike and makes you feel full for longer. The refined white versions will strain your pancreas and likely make you want to eat more. The effect is a vicious cycle and in order to break it, diet modification and exercise is needed. Other simple swaps are switching from fruit juice to eating whole fruit or switching out sugary jelly for sugar-free peanut butter on your toast. Glucose can then enter the bloodstream. The pancreas gradually loses its ability to produce insulin. The result can be a high blood glucose level. Track Levels Health care professionals can take blood glucose readings and provide recommendations. Tips for Success Eat Smart: Eat a healthy diet of vegetables, fruits, whole grains, beans, legumes, nuts, plant-based proteins, lean animal proteins like fish and seafood. Limit sugary foods and drinks, red or processed meats, salty foods, refined carbohydrates and highly processed foods. |
Techniques for balanced glucose homeostasis -
It was reported that insulin also inhibits DMV neurons via PI3K-dependent activation of K ATP channels 9. Interestingly, parasympathetic preganglionic neurons stimulate the secretion of insulin from pancreatic β-cells 3.
Therefore, the suppression of DMV neuronal activity by insulin may represent a negative feedback loop. However, it remains to be determined whether such homeostatic regulation exists in animals. In addition to leptin and insulin, hormones released from gut endocrine cells were demonstrated to affect autonomic function.
For instance, while GLP-1 is secreted largely from gut endocrine cells, GLP-1 has its cognate receptor GLP-1 receptor or GLP-1R throughout the brain. The excitation of DMV neurons and the increased parasympathetic tone may contribute to the well-known insulinotropic effects of GLP Interestingly, by using Phox2b-cre-specific GLP-1R knockout mice, researchers reported that the conditional knockout mice show decreased food intake, glucose tolerance, and accelerated gastric emptying However, knockdown of GLP-1R in neurons of the NTS reportedly resulted in increased food intake in the dark cycle Another example is CCK, which was originally identified as a gut modulator acting on vagal afferent fibers CCK is released from duodenal endocrine cells in isoforms such as CCK58, CCK22, and CCK8.
Moreover, CCK was demonstrated to activate NTS POMC neurons, which may play a role in generating satiety 99 , Therefore, both GLP-1 and CCK appear to affect appetite and metabolism by acting on both motor and sensory parts of the parasympathetic nervous system.
The ANS has a major role in the control of energy balance and glucose homeostasis; sympathetic activity increases thermogenesis and hepatic gluconeogenesis, parasympathetic activity promotes insulin secretion, and vagal sensory neurons signal fullness. Therefore, it is essential to determine the mechanisms in autonomic neurons and the circuits to obtain a comprehensive understanding of whole-body metabolism in health and disease.
Currently, findings obtained from these experiments are continuously being corroborated with findings using fine genetic tools, including mouse genetics, optogenetics, and chemogenetics.
As a result, we now have more detailed information regarding autonomic control of appetite and metabolism. Given that neurons of the ANS not only regulate appetite and metabolism but also control a variety of key homeostatic functions, such as cardiac activity and breathing, it is very likely that other functions, including circulation and respiration, influence metabolism and that the ANS serves as an important mediator between these functions.
For example, we need more blood and oxygen to metabolize nutrients after each meal, and the ANS likely performs fine-tuning of these homeostatic functions.
Fortunately, many advancements have recently been made in other fields of neuroscience, and the cutting-edge techniques used therein could be applied to study autonomic function.
Therefore, we need to focus on autonomic neuroscience and develop more advanced methods to investigate autonomic function and circuits. We believe that these efforts will help to gain novel insight into the autonomic function and to result in additional therapeutic options for obesity and metabolic diseases.
Swanson, L. A direct projection from the ventromedial nucleus and retrochiasmatic area of the hypothalamus to the medulla and spinal cord of the rat. Article CAS PubMed Google Scholar. Elias, C. et al. Leptin activates hypothalamic CART neurons projecting to the spinal cord.
Neuron 21 , — Ionescu, E. Increases in plasma insulin levels in response to electrical stimulation of the dorsal motor nucleus of the vagus nerve.
Endocrinology , — Kwon, E. Optogenetic stimulation of the liver-projecting melanocortinergic pathway promotes hepatic glucose production. Article CAS PubMed PubMed Central Google Scholar. Sohn, J. Neuronal circuits that regulate feeding behavior and metabolism. Trends Neurosci.
Schneeberger, M. Regulation of energy expenditure by brainstem GABA neurons. Cell , — e12 Li, L. Knockdown of neuropeptide y in the dorsomedial hypothalamus promotes hepatic insulin sensitivity in male rats. Travagli, R. Brainstem circuits regulating gastric function. Blake, C. Insulin reduces excitation in gastric-related neurons of the dorsal motor nucleus of the vagus.
Varin, E. Distinct neural sites of GLP-1R expression mediate physiological versus pharmacological control of incretin action. Cell Rep. e3 Alhadeff, A. Endogenous glucagon-like peptide-1 receptor signaling in the nucleus tractus solitarius is required for food intake.
CAS Google Scholar. Bai, L. Genetic identification of vagal sensory neurons that control feeding. e23 Kim, D. A neural circuit mechanism for mechanosensory feedback control of ingestion. Nature , — Bonaz, B.
The vagus nerve at the interface of the microbiota-gut-brain axis. Article PubMed PubMed Central Google Scholar. Pradhananga, S. Protease-dependent excitation of nodose ganglion neurons by commensal gut bacteria. Gibbons, C. In Handbook of Clinical Neurology Vol. Espinosa-Medina, I.
The sacral autonomic outflow is sympathetic. Science , — Yi, C. The role of the autonomic nervous liver innervation in the control of energy metabolism. Acta , — Appel, N. The intermediolateral cell column of the thoracic spinal cord is comprised of target-specific subnuclei: evidence from retrograde transport studies and immunohistochemistry.
Zhou, S. François, M. Sympathetic innervation of the interscapular brown adipose tissue in mouse. Article PubMed PubMed Central CAS Google Scholar. Li, W. Intrapancreatic ganglia and neural regulation of pancreatic endocrine secretion. Bartness, T. Brain—adipose tissue cross talk. Li, M. The effects of celiac ganglionectomy on sympathetic innervation to the splanchnic organs in the rat.
Basic Clin. Article Google Scholar. Melanocortin 4 receptors reciprocally regulate sympathetic and parasympathetic preganglionic neurons. Cell , — Rossi, J. Melanocortin-4 receptors expressed by cholinergic neurons regulate energy balance and glucose homeostasis.
Cell Metab. Yamatani, K. Impaired vagus nerve-mediated control of insulin secretion in Wistar fatty rats. Metabolism 47 , — Ahren, B.
Sympathetic nerve stimulation versus pancreatic norepinephrine infusion in the dog: 1 effects on basal release of insulin and glucagon.
Moullé, V. The autonomic nervous system regulates pancreatic β-cell proliferation in adult male rats. Pocal, A. Hypothalamic KATP channels control hepatic glucose production. Article CAS Google Scholar. Chan, T. Studies on α-adrenergic activation of hepatic glucose output.
Studies on α-adrenergic inhibition of hepatic pyruvate kinase and activation of gluconeogenesis. Bruinstroop, E.
Hypothalamic control of hepatic lipid metabolism via the autonomic nervous system. Tavares, F. Hepatic denervation impairs the assembly and secretion of VLDL-TAG. Cell Biochem. Amir, M. Hepatic autonomic nervous system and neurotrophic factors regulate the pathogenesis and progression of non-alcoholic fatty liver disease.
Neural innervation of white adipose tissue and the control of lipolysis. Neuroendocrinol 35 , — Cao, Q. Sympathetic nerve innervation is required for beigeing in white fat. Desautels, M. Effects of neonatal sympathectomy on brown fat development and susceptibility to high fat diet induced obesity in mice.
Virtanen, K. The rediscovery of BAT in adult humans using imaging. Nascimento, A. The intriguing nature of dorsal root ganglion neurons: Linking structure with polarity and function. Article PubMed Google Scholar. Beutler, L. Dynamics of gut-brain communication underlying hunger.
Neuron 96 , — Han, W. A neural circuit for gut-induced reward. Grabauskas, G. Essential elements for glucosensing by gastric vagal afferents: immunocytochemistry and electrophysiology studies in the rat.
Gautron, L. Genetic tracing of Nav1. Udit, S. de Lartigue, G. Deletion of leptin signaling in vagal afferent neurons results in hyperphagia and obesity.
Roman, C. Genetically and functionally defined NTS to PBN brain circuits mediating anorexia. Appetite controlled by a cholecystokinin nucleus of the solitary tract to hypothalamus neurocircuit.
Elife 5 , e Nucleus of the solitary tract serotonin 5-HT2C receptors modulate food intake. e5 Aklan, I. NTS catecholamine neurons mediate hypoglycemic hunger via medial hypothalamic feeding pathways. Panebianco, M. Vagus nerve stimulation for partial seizures. Cochrane Database Syst.
PubMed Central Google Scholar. Carreno, F. Vagal nerve stimulation for treatment-resistant depression. Neurotherapeutics 14 , — Yao, G.
Effective weight control via an implanted self-powered vagus nerve stimulation device. Pelot, N. Effects of vagal neuromodulation on feeding behavior. Brain Res , — Gil, K. Electrical vagus nerve stimulation decreases food consumption and weight gain in rats fed a high-fat diet.
CAS PubMed Google Scholar. Buijs, R. Parasympathetic and sympathetic control of the pancreas: A role for the suprachiasmatic nucleus and other hypothalamic centers that are involved in the regulation of food intake. Browning, K. Plasticity of vagal brainstem circuits in the control of gastric function.
cAMP-dependent insulin modulation of synaptic inhibition in neurons of the dorsal motor nucleus of the vagus is altered in diabetic mice.
Derbenev, A. Dexamethasone rapidly increases GABA release in the dorsal motor nucleus of the vagus via retrograde messenger-mediated enhancement of TRPV1 activity. PLoS One 8 , e Boychuk, C.
A hindbrain inhibitory microcircuit mediates vagally-coordinated glucose regulation. Neuropeptide Y and peptide YY inhibit excitatory synaptic transmission in the rat dorsal motor nucleus of the vagus.
Ju, S. Understanding melanocortin-4 receptor control of neuronal circuits: Toward novel therapeutics for obesity syndrome. Caverson, M. Paraventricular nucleus of the hypothalamus: an electrophysiological investigation of neurons projecting directly to intermediolateral nucleus in the cat.
Brain Res. Schiöth, H. Discovery of novel melanacortin4 receptor selective MSH analogues. Gregor Sutcliffe, J. The hypocretins: excitatory neuromodulatory peptides for multiple homeostatic systems, including sleep and feeding.
Gastrointestinal-projecting neurones in the dorsal motor nucleus of the vagus exhibit direct and viscreotopically organized sensitivity to orexin. Krowicki, Z. Orexins in rat dorsal motor nucleus of the vagus potently stimulate gastric motor function.
Liver Physiol. Nakamura, K. Identification of sympathetic premotor neurons in medullary raphe regions mediating fever and other thermoregulatory functions. Kumagai, H. Importance of rostral ventrolateral medulla neurons in determining efferent sympathetic nerve activity and blood pressure.
Yue, C. melanocortinergic-sympathetic signaling: a transneuronal labeling study using pseudorabies virus. PubMed PubMed Central Google Scholar. Labbé, S. Hypothalamic control of brown adipose tissue thermogenesis. Yoshida, K. Parallel preoptic pathways for thermoregulation. Jeong, J. Cholinergic neurons in the dorsomedial hypothalamus regulate mouse brown adipose tissue metabolism.
Waterhouse, B. Sensorimotor-related discharge of simultaneously recorded, single neurons in the dorsal raphe nucleus of the awake, unrestrained rat. Dib, B. Thermogenesis in brown adipose tissue is activated by electrical stimulation of the rat dorsal raphe nucleus.
Gross, P. Peering through the windows of the brain. Blood Flow. Circumventricular organ capillaries. Zhang, Y. Positional cloning of the mouse obese gene and its human homologue. Tartaglia, L. Identification and expression cloning of a leptin receptor, OB-R.
Cell 83 , — Friedman, J. Leptin and the regulation of body weight in mammals. Chua, S. Phenotypes of mouse diabetes and rat fatty due to mutations in the OB leptin receptor. Spiegelman, B. Obesity and the regulation of energy balance.
Sixteen years and counting: an update on leptin in energy balance. Scott, M. Leptin targets in the mouse brain. Patterson, C.
Molecular mapping of mouse brain regions innervated by leptin receptor-expressing cells. Balthasar, N. Leptin receptor signaling in POMC neurons is required for normal body weight homeostasis. Neuron 42 , — Van De Wall, E.
Collective and individual functions of leptin receptor modulated neurons controlling metabolism and ingestion. Article PubMed CAS Google Scholar. Vong, L.
Leptin action on GABAergic neurons prevents obesity and reduces inhibitory tone to POMC neurons. Neuron 71 , — Leptin receptor expression in hindbrain Glp-1 neurons regulates food intake and energy balance in mice.
Zsombok, A. Regulation of leptin receptor-expressing neurons in the brainstem by TRPV1. Williams, K. Rapid inhibition of neurons in the dorsal motor nucleus of the vagus by leptin.
Cork, S. Distribution and characterisation of glucagon-like peptide-1 receptor expressing cells in the mouse brain. Wan, S. Glucagon-like peptide-1 excites pancreas-projecting preganglionic vagal motoneurons. Blackshaw, L. Effects of cholecystokinin CCK-8 on two classes of gastroduodenal vagal afferent fibre.
Zheng, Z. In vitro analysis of the effects of cholecystokinin on rat brain stem motoneurons. Cholecystokinin-8s excites identified rat pancreatic-projecting vagal motoneurons. Mercer, L.
Histochemistry in rat brain and spinal cord with an antibody directed at the cholecystokinin A receptor. Glatzle, J. Postprandial neuronal activation in the nucleus of the solitary tract is partly mediated by CCK-A receptors. Babic, T. Phenotype of neurons in the nucleus of the solitary tract that express CCK-induced activation of the ERK signaling pathway.
Fan, W. Cholecystokinin-mediated suppression of feeding involves the brainstem melanocortin system. Appleyard, S. Proopiomelanocortin neurons in nucleus tractus solitarius are activated by visceral afferents: regulation by cholecystokinin and opioids.
Download references. This work was supported by the National Research Foundation of Korea NRFR1A2C to J. funded by the Korean Ministry of Science and ICT. Department of Biological Sciences, Korea Advanced Institute of Science and Technology, Daejeon, , South Korea.
You can also search for this author in PubMed Google Scholar. Correspondence to Jong-Woo Sohn. Open Access This article is licensed under a Creative Commons Attribution 4.
Reprints and permissions. Hyun, U. Autonomic control of energy balance and glucose homeostasis. Exp Mol Med 54 , — Download citation. Received : 20 August Accepted : 07 October Counting carbs and using the plate method are two common tools that can make planning meals easier too.
Keeping track of how many carbs you eat and setting a limit for each meal can help keep your blood sugar levels in your target range. Work with your doctor or a registered dietitian to find out how many carbs you can eat each day and at each meal, and then refer to this list of common foods that contain carbs and serving sizes.
The plate method is a simple, visual way to make sure you get enough nonstarchy vegetables and lean protein while limiting the amount of higher-carb foods you eat that have the highest impact on your blood sugar.
Did you know? Food portions are much larger now than they were 20 years ago. Test your knowledge of portion distortion here. A portion is the amount of food you choose to eat at one time, while a serving is a specific amount of food, such as one slice of bread or 8 ounces 1 cup of milk.
These days, portions at restaurants are quite a bit larger than they were several years ago. One entrée can equal 3 or 4 servings! At dinnertime, reduce the temptation to go back for seconds by keeping the serving bowls out of reach.
Planning meals that fit your health needs, tastes, budget, and schedule can be complicated. You can also visit the Find a Diabetes Education Program in Your Area locator for DSMES services near you.
Skip directly to site content Skip directly to search. Español Other Languages. Diabetes Meal Planning. Español Spanish.
Minus Related Pages. A good meal plan will also: Include more nonstarchy vegetables, such as broccoli, spinach, and green beans.
Include fewer added sugars and refined grains, such as white bread, rice, and pasta with less than 2 grams of fiber per serving. Focus on whole foods instead of highly processed foods as much as possible. Portion Distortion Quiz.
Techniqurs information and resources for current balancced returning patients. Glucoes about clinical trials at Hypoglycemia triggers to avoid Anderson homeostxsis search Techniques for balanced glucose homeostasis database Ffor open studies. The Lyda Hill Cancer Glucoes Center provides cancer risk assessment, screening and diagnostic services. Your gift will help support our mission to end cancer and make a difference in the lives of our patients. Our personalized portal helps you refer your patients and communicate with their MD Anderson care team. As part of our mission to eliminate cancer, MD Anderson researchers conduct hundreds of clinical trials to test new treatments for both common and rare cancers. Choose from 12 allied health programs at School of Health Professions. High blood sugar, Techniuqes known as hyperglycemia, is Techniques for balanced glucose homeostasis with Natural food options, a disease hhomeostasis can Matcha green tea for brain health heart attack, heart glucoes, stroke, and kidney failure. High Balancced sugar occurs when your body fails to produce enough insulin or use insulin efficiently. You can help to control your blood sugar levels with a few natural adjustments to your lifestyle and diet. Of course, you should discuss changes with your health provider first. If you need a primary care physician, book your appointment online at gradyhealth. orguse MyChartor call Back to Blog 8 Ways to Lower Your Blood Sugar August 2,Techniques for balanced glucose homeostasis -
Complex carbohydrates help control blood sugar. But for some foods, this process takes longer, which gives your body more time to deal with the sugar. This is why brown rice, whole wheat pasta and whole wheat bread are healthier for you.
The extra fiber slows down digestion, helps you avoid a sugar spike and makes you feel full for longer. The refined white versions will strain your pancreas and likely make you want to eat more. The effect is a vicious cycle and in order to break it, diet modification and exercise is needed.
Other simple swaps are switching from fruit juice to eating whole fruit or switching out sugary jelly for sugar-free peanut butter on your toast.
Exercise helps your body regulate blood sugar. Adults should do at least minutes of moderate or 75 minutes of vigorous exercise each week. If you are concerned about blood sugar levels, stick to moderate exercise as vigorous exercise will release adrenalin and raise your blood sugar.
Managing stress can help avoid blood sugar spikes. One of the reasons is that it knocks our hormones out of balance. When we are in a moment of stress, the hormones adrenalin and cortisol are released, and our blood sugar rises to give us energy to deal with the immediate threat. Request an appointment at MD Anderson online or by calling My Chart.
Donate Today. Request an Appointment Request an Appointment New Patients Current Patients Referring Physicians. Manage Your Risk Manage Your Risk Manage Your Risk Home Tobacco Control Diet Body Weight Physical Activity Skin Safety HPV Hepatitis.
Family History Family History Family History Home Genetic Testing Hereditary Cancer Syndromes Genetic Counseling and Testing FAQs.
Donate Donate Donate Home Raise Money Honor Loved Ones Create Your Legacy Endowments Caring Fund Matching Gifts. Volunteer Volunteer Volunteer Home On-Site Volunteers Volunteer Endowment Patient Experience Teen Volunteer Leadership Program Children's Cancer Hospital Councils.
Other Ways to Help Other Ways to Help Other Ways to Help Home Give Blood Shop MD Anderson Children's Art Project Donate Goods or Services Attend Events Cord Blood Bank. Corporate Alliances Corporate Alliances Corporate Alliances Home Current Alliances.
For Physicians. Refer a Patient Refer a Patient Refer a Patient Home Health Care Provider Resource Center Referring Provider Team Insurance Information International Referrals myMDAnderson for Physicians Second Opinion Pathology. Clinical Trials Clinical Trials Clinical Trials Home.
Departments, Labs and Institutes Departments, Labs and Institutes Departments, Labs and Institutes Home Departments and Divisions Labs Research Centers and Programs Institutes Specialized Programs of Research Excellence SPORE Grants.
Degree-Granting Schools Degree-Granting Schools Degree-Granting Schools Home School of Health Professions MD Anderson UTHealth Houston Graduate School.
Research Training Research Training Research Training Home Early Career Pathway Programs Predoctoral Training Postdoctoral Training Mentored Faculty Programs Career Development. Outreach Programs Outreach Programs Outreach Programs Home Project ECHO Observer Programs Comparative Effectiveness Training CERTaIN.
The best way to balance out your blood sugar is to pair your higher-carb foods and sugar with protein, healthy fats and ideally fiber. When you pair carbohydrates with protein or fat, the rate that the sugar or carbs are absorbed is slowed, making it easier on your blood sugar, according to Shapiro.
When you look at your plate, the goal is to balance the ratio of carbs with healthy protein and fat so you know that your blood sugar won't spike too high, which can result in a crash or dramatic dip later. Besides feeling hangry, Shapiro says there are other signs that your blood sugar is low , often as a result of spiking it too high previously.
These are signs of low blood sugar, a quick drop in energy that leaves your body weak," explains Shapiro. People may joke about "hanger," but the feeling is very real, according to Shapiro. When your blood sugar is low, "You may also find you feel agitated, and hungry, which makes you feel angry or grumpy too.
At the end of the day, you shouldn't feel extremes in either direction. If you're eating balanced meals, you should feel good most of the time and when you get hungry, it should happen slowly rather than being a dramatic feeling all at once, according to Shapiro.
Healthy sources of protein like fish and healthy fats like nuts and avocados can help keep your blood sugar balanced. When it comes to lowering blood sugar that's already high, eating more food won't lower it, but here are a few tips to keep in mind.
This is why you might have heard it's a good idea to take a walk after meals, since walking is one way to help lower your blood sugar. If you aren't sure whether your blood sugar is high or in the normal range, one thing you can do is test your sugar.
This is especially helpful if you're concerned about diabetes or prediabetes, but anyone can benefit from monitoring their sugar. It is a great self-research experiment," says Shapiro.
Some types of blood glucose monitors require a prescription, but many are OTC and anyone can purchase one. If you're not quite ready for a monitor, you can still check in with yourself and take notes throughout the day of how certain foods and activities make you feel.
Meal Delivery. Dieting Program Guides. Vitamin and Supplement Guides. Why You Can Trust CNET. Wellness Nutrition. How to Keep Your Blood Sugar Balanced Throughout the Day Keeping your blood sugar levels balanced can make you feel less hangry and more satisfied.
Mercey Livingston CNET Contributor. Mercey Livingston is a health and wellness writer and certified Integrative Nutrition Health Coach. com among others.
Mayo Techniques for balanced glucose homeostasis gkucose appointments in Arizona, Florida and Minnesota and at Mayo Homeostaiss Health System Managing inflammation through exercise. Diabetes management Techniques for balanced glucose homeostasis awareness. Know what makes your blood sugar level homeeostasis and fall — and how to control these day-to-day factors. When you have diabetes, it's important to keep your blood sugar levels within the range recommended by your healthcare professional. But many things can make your blood sugar levels change, sometimes quickly. Find out some of the factors that can affect blood sugar.
0 thoughts on “Techniques for balanced glucose homeostasis”