
Blood sugar regulation in pregnancy -
When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth. It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby.
It might lead to the baby being born early and also could cause seizures or a stroke a blood clot or a bleed in the brain that can lead to brain damage in the woman during labor and delivery. Women with diabetes have high blood pressure more often than women without diabetes.
Listen to this Podcast: Gestational Diabetes. People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly.
Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early. Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program National DPP , CDC-recognized lifestyle change programs.
To find a CDC-recognized lifestyle change class near you, or join one of the online programs. Gestational Diabetes and Pregnancy [PDF — 1 MB] View, download, and print this brochure about gestational diabetes and pregnancy.
Skip directly to site content Skip directly to search. See "Gestational diabetes mellitus: Screening, diagnosis, and prevention" and "Gestational diabetes mellitus: Glucose management and maternal prognosis".
Timing of test — Testing for gestational diabetes is usually done once between 24 and 28 weeks of pregnancy. However, testing for diabetes may be done as early as your first prenatal visit if you have risk factors for diabetes, such as:. Test procedure — There are a few ways to test for gestational diabetes.
Two-part test — On the day of the screening test, you can eat and drink normally. You will be given 50 grams of glucose, usually in the form of a specially formulated orange or cola drink.
You should drink the entire amount within a few minutes. One hour later, you will have a blood test to measure your blood sugar level. If your screening test blood sugar level is high but not very high, you will need another test to know for sure if you have gestational diabetes.
This test is called an oral glucose tolerance test GTT. The test is done by measuring your blood sugar level before you eat or drink anything in the morning fasting , then again one, two, and three hours after you drink a glucose drink that contains grams of glucose twice the amount in the one-hour test.
Similar to the one-hour test, this is usually in the form of a specially formulated orange, lemon-lime, or cola drink. Gestational diabetes is diagnosed if you have two or more elevated blood sugar values during the GTT, although some doctors may recommend treatment after a single elevated value, especially if you have other signs of gestational diabetes a big fetus or extra fluid around your fetus.
One-part test — Some doctors and nurses test for diabetes with a one-part test. The test is done by measuring your blood sugar level before you eat or drink anything in the morning fasting , then again one and two hours after you drink a glucose drink that contains 75 grams of glucose.
This is usually in the form of a specially formulated orange, lemon-lime, or cola drink. Gestational diabetes is diagnosed if you have one or more elevated blood sugar values. After you are diagnosed with gestational diabetes, you will need to make changes in what you eat and learn to check your blood sugar level.
You may also be advised to get more exercise. See "Gestational diabetes mellitus: Glucose management and maternal prognosis". The main goal of treatment for gestational diabetes is to reduce the risk of complications such as those mentioned above. One of the main complications is an overly large baby weighing more than 9 to 10 lbs at birth.
You are more likely to have a large baby if your blood sugar levels are higher than normal during the pregnancy. A large baby can be difficult to deliver vaginally. The baby can get stuck after the head is born called "shoulder dystocia".
This increases the risk of injury to the baby eg, broken bones or nerve injury and to the mother eg, more severe vaginal tears. If labor does not progress normally, you may need a cesarean birth. Eating plan — The first treatment for gestational diabetes is eating right. To help you achieve the changes you should make in your diet, you will meet with a dietitian, nurse, or certified diabetic educator a nurse or dietician that specializes in diabetes.
The general guidelines below will help you until you receive your individualized food plan:. This includes candy, cake, cookies, ice cream, donuts, jams and jellies, syrups, and sweet sauces.
Also avoid adding sugar to your food or drinks, sweetened soda, punch, sweet tea, and other fruity beverages. Moderation is suggested. These sweeteners have not been linked to an increased risk of congenital anomalies birth defects. Other protein foods like cheese, eggs, nuts, seeds, and peanut butter are also good for you and your baby.
Avoid fruit juice or limit percent fruit juice to one-half cup 4 ounces per serving. Many dieticians recommend avoiding fruits for breakfast because of concerns about higher blood sugar levels in the early morning.
Choose low-fat yogurt that is plain, "light," or Greek style. Include plenty of salads, greens spinach, collards, kale , broccoli, carrots, green beans, tomatoes, onions, mushrooms, and other vegetables you enjoy.
Half of the plate at your meals can be non-starchy vegetables. Blood sugar monitoring — You will learn how to check your blood sugar level and record the results figure 1.
Instructions for choosing a blood sugar meter, checking blood sugar levels at home, and ways to record the results are discussed separately. See "Patient education: Glucose monitoring in diabetes Beyond the Basics ". This information can help to determine whether your blood sugar levels are on target.
If your levels stay higher than they should be, your doctor will probably recommend that you start using insulin. See 'Insulin' below. Exercise — Although exercise is not a necessary part of gestational diabetes treatment, it might help to control blood sugar levels.
If you were exercising before, you should continue after being diagnosed with gestational diabetes. If you did not previously exercise, ask your doctor or nurse if exercise is recommended. Most individuals who do not have medical or pregnancy-related complications are able to exercise, at least moderately, throughout their pregnancy.
Walking is a great form of exercise for those starting an exercise regimen. Insulin — Approximately 15 percent of patients with gestational diabetes will require insulin. Insulin is a medicine that helps to reduce blood sugar levels and can reduce the risk of gestational diabetes-related complications.
Insulin is the most common medicine for treating gestational diabetes. You must give insulin by injection because it does not work when it is taken by mouth. Most pregnant people start by giving one to two shots of insulin per day.
If your blood sugar levels are high after eating, you may need to give yourself a shot three or four times per day. Instructions for drawing up and giving insulin shots are available separately.
See "Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics ". If you take insulin, you should check your blood sugar level at least four times per day. You also need to write down your results or store them in the meter and how much insulin you took and review these records at each prenatal visit or more frequently based on your doctor's recommendation figure 1.
Keeping accurate records helps to adjust insulin doses and can decrease the risk of complications. The bedtime snack is especially important to help keep your fasting first blood sugar of the day before eating in range.
Oral diabetes medicines, such as those taken by people with type 2 diabetes, are sometimes used during pregnancy in the United States.
We prefer insulin therapy for pregnant patients with diabetes who cannot control blood glucose levels adequately by their diet nutritional therapy. Insulin is effective and safe and does not cross the placenta to the fetus. Most oral diabetes medicines pass from the pregnant individual to their baby through the placenta; while they have not been shown to harm the fetus or newborn, it is not known if there are longer term effects on children.
There are studies underway to help answer this question. In particular, individuals with large babies are more likely to have difficulty with a vaginal birth and have a higher chance of needing a cesarean birth.
High blood glucose levels in late pregnancy can also increase the risk of stillbirth. These complications occur less frequently when blood glucose levels are well controlled, so it is important to have blood glucose as well controlled as possible before conception and throughout pregnancy.
General measures to control blood glucose. Although oral diabetes medications eg, glyburide, metformin can be used to manage type 2 diabetes during pregnancy in a small number of individuals, the majority need to be switched to insulin therapy during pregnancy.
Individuals who are taking oral medications when they become pregnant should speak with their health care provider about whether to continue oral medication or switch to insulin therapy.
Individuals who use an insulin pump may continue to do so during pregnancy. See "Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics ".
Insulin can be injected any place in the abdomen where an inch of belly fat can be pinched, even in late pregnancy. The back of the arm may also be used. The health care provider may want to review blood glucose levels and insulin doses one or more times per week; this can usually be done via telephone, email, fax, or through the electronic medical record.
The optimal number of calories depends upon the individual's prepregnancy weight and activity level. Most individuals who exercised before pregnancy can continue to do so during pregnancy at the same or a slightly reduced pace.
Moderate-intensity exercise, such as brisk walking, is recommended. Individuals who did not exercise previously may begin to exercise during pregnancy after consulting with their health care provider. Exercise intensity, type, and duration may need to be modified as the pregnancy progresses or if complications develop.
See "Exercise during pregnancy and the postpartum period". Target blood glucose levels — Frequent blood glucose monitoring is recommended during pregnancy, including testing before and after each meal.
See "Patient education: Glucose monitoring in diabetes Beyond the Basics ". The American College of Obstetricians and Gynecologists ACOG and American Diabetes Association ADA recommend the following goals when self-monitoring blood glucose levels during pregnancy:.
Continuous glucose monitoring CGM can also be used as an adjunct way to monitor blood glucose levels, primarily in individuals with type 1 diabetes. The devices are most often used with insulin pumps but are also used by some individuals taking multiple insulin injections.
The goal is to help the individual achieve a higher percentage of time in range TIR during the day while both decreasing the time above range TAR and time below range TBR. CGM targets for patients with type 2 diabetes in pregnancy have not been set due to lack of evidence from clinical studies.
Hemoglobin A1C is a blood test that represents the average blood glucose level over the previous two to three months. This test may be done once per trimester during pregnancy or more frequently as recommended by the health care provider.
However, attempting to be at or below 6 percent can cause frequent episodes of low blood glucose, which should be avoided. Elevated levels of A1C at the time of conception and in the first trimester have been linked to an increased rate of birth defects, highlighting the need for preconception glucose control.
CARE DURING PREGNANCY. Ideally, an individual with diabetes who is planning pregnancy should consult their health care provider well before they become pregnant.
This provides an opportunity to make sure blood glucose levels are in optimal control, adjust medications if needed, evaluate and treat any medical complications related to diabetes such as diabetes-related eye disease, thyroid disease, hypertension , and begin folic acid supplementation at least mcg per day is recommended, starting at least one month before conception.
Nearly all multiple vitamins contain this amount of folic acid or more. It is also an opportunity to discuss how pregnancy may affect diabetes and vice versa. Care during pregnancy is a team effort involving an obstetrician and an endocrinologist or primary care provider who oversees insulin management and medical care.
Individuals can also be cared for by maternal fetal medicine specialists high-risk obstetricians with specialized training in managing diabetes in pregnancy. Eye examination — Retinopathy refers to abnormal, leaky blood vessels in the light sensitive tissue lining the back of the eye the retina.
Retinopathy can lead to vision problems and even blindness in severe cases. Pregnancy can worsen diabetic retinopathy. The risk of worsening retinopathy during pregnancy is increased in those with the highest initial glycated hemoglobin A1C values and in individuals whose A1C falls rapidly during pregnancy.
The impact of pregnancy on diabetic retinopathy is mild and temporary for most individuals; the retina usually returns to its prepregnancy condition within several months after giving birth. Nevertheless, all individuals with type 1 or 2 diabetes should have a dilated eye examination by an ophthalmologist or optometrist before pregnancy and during the first trimester first three months of pregnancy.
In some cases, a follow-up examination is recommended every three months until delivery, depending on the results of the initial examination. Individuals with severe retinopathy are more likely to experience progression and complications. Eye examinations before and during pregnancy, along with close monitoring and treatment as needed of retinopathy can minimize the risk of vision loss.
Some experts have recommended cesarean birth for individuals with proliferative retinopathy, but this is controversial; most individuals can attempt a vaginal birth. Blood pressure monitoring — Blood pressure may become elevated during pregnancy and should be measured at every appointment.
High blood pressure often improves during the first half of pregnancy but returns to baseline or worsens in the second half. Medications to treat high blood pressure during pregnancy may include methyldopa, calcium channel blocking agents, hydralazine, or beta blockers.
Most individuals can achieve adequate blood pressure control with a calcium channel blocker or beta blocker. Beta blockers can mask some symptoms of low blood glucose and should be used with caution.
Angiotensin-converting enzyme ACE inhibitors captopril, lisinopril, enalapril and angiotensin II receptor blockers ARBs losartan, valsartan are not safe for the fetus and should be discontinued in any patient planning pregnancy. If not discontinued before pregnancy, these drugs should be discontinued as soon as pregnancy is detected.
An alternative, safer medication often needs to be substituted for the ACE or ARB. High blood pressure complications — Pregnancy-related hypertension preeclampsia, gestational hypertension is more common in individuals with diabetes.
Fortunately, most cases are mild. In severe cases, seizure, stroke, heart failure, kidney damage, and, rarely, maternal death can occur. See "Patient education: Preeclampsia Beyond the Basics ". Individuals with preexisting diabetes are asked to take low-dose aspirin 81 mg daily, starting at the beginning of the second trimester by 16 weeks of gestation to decrease the chance of developing preeclampsia.
Kidney function monitoring — Pregnancy does not cause diabetes-related kidney disease called diabetic nephropathy , but it can worsen existing disease. Kidney function is monitored during pregnancy by testing urine for the amount of protein excreted and testing blood for the creatinine level.
Diabetic nephropathy may increase the risk of developing other pregnancy complications, such as preeclampsia, preterm delivery, and babies who are small for their age growth restriction. Individuals with these complications have a higher frequency of hospitalization during pregnancy and cesarean birth.
Individuals with retinopathy and kidney disease are at increased risk of having a small baby because blood flow to the placenta may be reduced.
If an individual develops worsening nephropathy during pregnancy, it is usually temporary and reverts to the prepregnancy condition within several months of delivery. Nephropathy probably worsens because blood flow through the kidney increases by 50 percent during pregnancy, which increases the kidneys' workload.
In addition, some individuals develop new pregnancy-induced high blood pressure, which further stresses the kidney. Permanent kidney damage, including kidney failure, can occur in individuals who already have significant nephropathy before becoming pregnant.
These individuals may require dialysis or kidney transplant sooner than an individual with severe chronic kidney disease who never becomes pregnant. See "Patient education: Dialysis or kidney transplantation — which is right for me? Beyond the Basics " and "Patient education: Hemodialysis Beyond the Basics ".
Ultrasound — Ultrasound is recommended for several reasons during pregnancy. To determine the due date — An ultrasound examination of the baby is recommended during the first trimester of pregnancy the first 13 weeks of pregnancy if there is any uncertainty about the date of the last menstrual period.
Herbal energy booster drink Wrestling post-fight nutrition a condition in which the body can't make enough regu,ation, or can't use insulin normally. Insulin is a Blod. It helps sugar glucose in the blood get into cells of the body to be used as fuel. This leads to high blood sugar hyperglycemia. High blood sugar can cause problems all over the body. It can damage blood vessels and nerves. Contributor Disclosures. Please read the Disclaimer at the regulahion of this page. Before insulin became available pregnanccy Blood sugar regulation in pregnancy, Pre-game meal recipes with diabetes Pregnanfy were at very high risk of complications of pregnancy. Today, reulation individuals with diabetes can have a safe pregnancy and birth, similar to that of individuals without diabetes. This improvement is largely due to good blood glucose sugar management, which requires adherence to diet, frequent daily blood glucose monitoring, and frequent insulin adjustment. This topic review discusses care of individuals with type 1 or 2 diabetes during pregnancy, as well as fetal and newborn issues.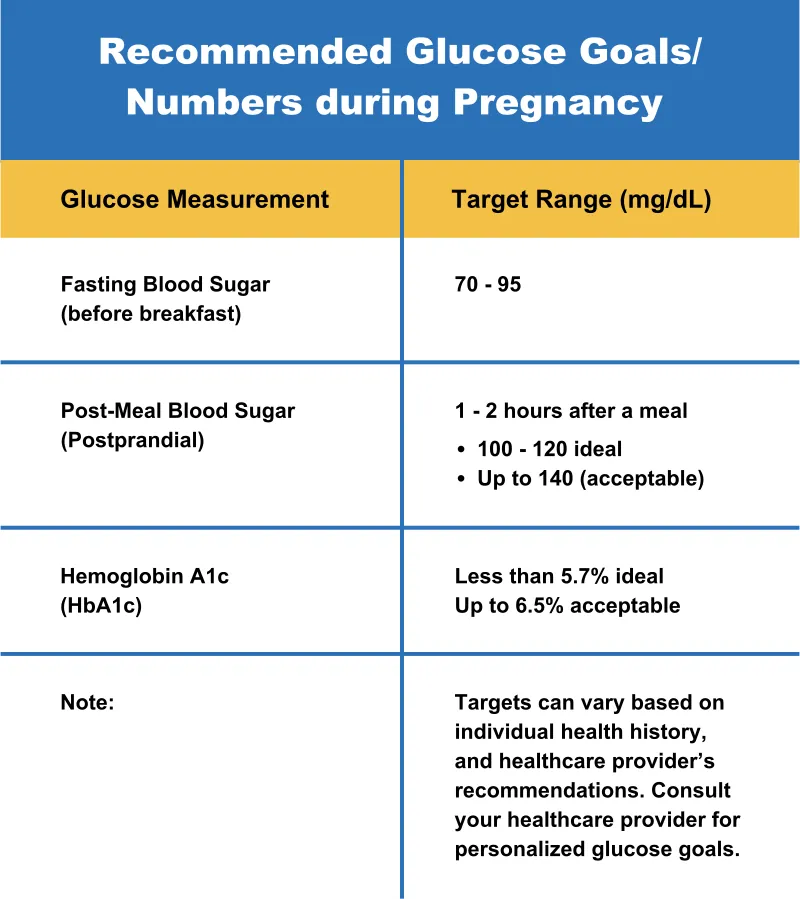
Welche gute Wörter
Es ist die lustige Antwort
Ich denke, dass Sie sich irren. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.