Oxidative stress and inflammation -
It has been proposed that a discrepancy between the metabolic requirements of these thick ascending limbs and the medullary blood supply could generate O 2 [ ]. The thick ascending limb is associated with ROS generation mostly due to the extremely high mitochondrial density and therefore, mitochondrial ROS generation [ ].
Reduced renal blood flow can induce oxidative stress and osmotic necrosis consequently generating ROS, via a positive feedback mechanism, leading to acute tubular necrosis [ , ]. Renal microcirculation is compromised by ROS production, which affects renal vascular function by facilitating the production of vasoconstrictors such as endothelin-1 and ameliorating the effects of vasodilators, such as NO [ ].
Direct toxicity of CM in renal tubular cells can also result in mitochondrial dysfunction and, combined with elevated levels of ROS, leads to extensive damage of glomerular cells by compromising the cellular membrane, ultimately resulting in apoptosis [ ]. A crucial factor in the production of ROS in the kidney is renal hypoxia.
There are, however, conflicting reports relating to the extent to which oxidative stress is a cause or epiphenomena. ROS are regularly involved in cellular inflammatory responses and it is proposed that ROS are formed during renal parenchymal hypoxia, following CM exposure, resulting in vascular endothelial injury.
This aggravates renal parenchymal hypoxia resulting in endothelial dysfunction [ ]. O 2 can lead to the accumulation of ONOO - , the production of which reduces NO bioavailability. In addition, ROS activate p38 MAPK stress kinases and c-Jun N-terminal kinases, that are involved in the activation of caspase-3 and caspase-9, which are associated with the induction of apoptosis [ ].
Mitochondrial dysfunction can induce apoptosis by releasing cytochrome c and activating caspase-9, which in turn activates caspase Caspase-3 plays a major role in apoptotic signaling by mediating death receptor-dependent and mitochondria-dependent apoptosis pathways [ ].
Glutathione GSH , is an important endogenous thiol that is essential to a variety of detoxification processes. GSH can donate reducing equivalents for the activity of specific antioxidant peroxidase enzyme, such as GSH peroxidase GPx , and can react directly with certain ROS e.
Intracellular levels of GSH are tightly controlled by the enzymes glutamate-cysteine ligase and GSH synthase involved in synthesis , GSH reductase involved in recycling of oxidized glutathione back to GSH and GSH transferases involved in utilization [ ].
Redox enzymes include thioredoxin, catalase, GPx, peroxiredoxins and superoxide dismutase SOD [ ]. One of the factors that is central to the prevalence of CIN is chronic inflammation.
The role of inflammation in CIN has been extensively studied and clinical trials in humans and animal models have been performed to help elucidate this role [ - ]. One of the main features of intravascular iodinated CM is that it causes vasodilation followed by a prolongation in vasoconstriction [ , ].
Two additional pathways suggested to promote this increase are cellular toxicity and elevated urinary viscosity that can cause obstructions through stone formation [ ]. Although the global prevalence of CIN does not constitute a public health threat, at risk populations, such as those suffering from higher presence of infectious diseases, have a higher incidence of inflammation than populations that are not affected by these diseases [ ].
A close relationship between inflammatory molecules and thrombogenesis has been well reported [ ]. The acute inflammatory state is a landmark of infectious diseases and one of the main type of molecules that derive from it are interleukins ILs.
IL-6 and IL have been targeted as disruptors of homeostasis within inflammatory processes. IL-6 promotes the expression of the C reactive protein CRP , which is being used as a current acute inflammation marker [Figure 3] [ ]. Figure 3. Inflammatory molecules in CIN and CVD.
Inflammatory states have been associated with CIN and CVD risk factors. Inflammatory cells and molecules are considered as potential risk factors in CVD and CIN. Inflammatory risk factors highlighted in blue.
CM, Disease states and cellular types related to inflammatory risk factors represented in grey. CM: contrast media; RF: risk factors; AMI: acute myocardial infarction; ACS: acute coronary syndrome; IL: interleukin; CRP: C reactive protein; TNF-α: tumor necrotic factor-α; TLR4: toll like receptor 4; CIN: contrast induced nephropathy; CVD: cardiovascular disorders.
One of the studies that assessed the increased risk for CIN due to inflammation was performed by Kwasa et al. They performed a prospective cohort study of patients undergoing a contrast-enhanced CT CECT scan.
The observed incidence of CIN was 9. Of the patients with inflammation, 29 No significant relation was found between the increase of CIN prevalence and biophysical variables age, sex, height, weight, etc.
Another study reported by Oweis et al. Of the total patients, 30 The incidence rate was Additional biomarkers of inflammation have been studied to assess their potential as predictors of CIN in different conditions. Cell types that are associated chronic inflammation have been proposed as predictors of increased risk of developing CIN: the study published by Yuan et al.
It is important to mention that all of the patients in this study went through emergency PCI. Regarding the assessment of multiple markers to predict the development of CIN, different studies have reported combinations between proteins that can be measured in human serum.
The study performed by Satilmis et al. The prevalence of CIN in this study was Multivariate logistic regression analysis showed significant association between CRP: albumin ratio and the development of CIN; advanced age, diabetes, dyslipidemia and left ventricular ejection fraction were also associated with the condition.
Animal models have also been used in the search for the potential role of inflammation in the development of CIN. Demirtas et al. Significantly increased presence of IL was found in the kidney tissue of the diabetic group after induction of CIN when compared with the healthy and diabetic groups.
Prophylactic use of carotenoids has been studied in animal models to assess the relation between oxidative stress induced inflammation and CIN development. The studies presented by Buyuklu et al.
Significant increase in urea, creatinine and malondialdehyde were observed in the CIN group when compared with the control group. Additionally, histological tests showed significant increase of infiltrated inflammatory cells and necrotic degenerative changes in the CIN group when compared against the control [ , ].
The role of the inflammatory state in CVD was addressed in an extensive literature [ 14 ]. The search for markers has two principal aims: to look into the understanding of the mechanisms of disease and to identify molecules that can be detected more accurately to predict the risk of cardiovascular events.
The role of inflammation in CVD development has been assessed throughout different populations and experimental models, critical importance has been given to events such as acute myocardial infarction AMI and atherosclerosis due to their high incidence and mortality rates [ ]. Inflammation in CVD includes a vast number of processes which can occur at the site of disease, in the bloodstream and at sites far from the disease [ ].
Immune response takes the spotlight when addressing inflammation and CVD. In AMI a signaling cascade induces the expression and recruitment of proinflammatory molecules, accelerating both damage and further repair of injured cardiac tissue.
Elevated levels of high-sensitivity CRP and IL-6 in plasma have been found correlated with unfavorable outcomes in patients [Figure 3] [ ]. Rajendran et al. Both IL-6 and hs-CRP were found to be significantly increased when compared with the control group.
Pro-inflammatory cytokines IL-6, IL, IL and TNF-α were evaluated in a study published in including patients with acute coronary syndrome ACS and 60 healthy controls.
Serum levels of IL-6, IL and TNF-α were significantly higher in the ACS group when compared to the healthy group [Figure 3]. No significant difference in serum levels of IL was found [ ]. Additionally, TNF-α has been found to promote the release proinflammatory chemokines and adhesion molecule synthesis in damaged myocardium and causing additional leukocyte infiltration in mice [ ].
Toll-like receptors TLRs may be key to understanding heart failure. TLR4 deficiency is associated with decreased in size of damage by infarct and reduction of systemic inflammation in mice [ ].
In humans, the activation of TLR4 in monocytes is associated with the development of cardiac failure after AMI [Figure 3] [ ]. By contrast, deficiencies in the function of TLR2 were found to reduce myocardial fibrosis and improve ventricular remodeling after AMI in a murine model [ ].
Atherosclerosis is often described as a chronic inflammatory process. Deregulation in the endothelium is mediated by cell adhesion molecules, such as ICAM1, P-selectin and VCAM1.
Additionally, the secretion of cytokines has a role in atherogenesis, namely IL-1, IL-6, TNF, IL-4, IL and IL [Figure 3]. The detection of some of these molecules in plasma has identified associations that could help to predict atherosclerosis severity.
Moreover, the identification of cell types through flow cytometry has proven to be a promising predictor for atherogenic levels of severity.
The identification of rapid, predictive biomarkers for CIN is essential as current targets are relatively slow to be useful, or the assays are just too expensive to be launched in a clinical setting.
Some of the postulated biomarkers for CIN and CVD are shown on Table 1. An early predictive biomarker of AKI is human neutrophil gelatinease-associated lipocalin NGAL. NGAL is a small protein of the lipocalin superfamily that was initially identified from the supernatant of activated human neutrophils in Successive studies have recognized renal NGAL as a unique, specific biomarker for the early detection of AKI in critically ill patients and after CM administration.
Urinary and serum levels of NGAL increase well before the increase of serum creatinine levels ~2 h. As a result, NGAL is increasingly studied as a marker of AKI [ - ].
Another proposed sensitive, early, non-invasive biomarker for AKI kidney injury is urinary neutrophil gelatinase-associated lipocalin uNGAL also known as lipocalin uNGAL is an iron-transporting protein that rapidly accumulates in the urine and kidney tubules after nephrotoxic and ischemic insults.
Zappitelli et al. Despite these findings, the use of uNGAL is still experimental. IL: interleukin; TNF: tumor necrotic factor; CRP: C reactive protein; NGAL: neutrophil gelatinase-associated lipocalin; L-FABP: liver type fatty acid binding protein; tPA: tissue plasminogen activator; uPA: urokinase plasminogen activator; PAI: plasminogen activator inhibitor; KIM kidney injury molecule 1; CysC: Cystatin C; CIN: contrast induced nephropathy; CVD: cardiovascular disorders; CRP: C reactive protein.
Liver type fatty acid binding protein L-FABP is an intracellular lipid chaperone and is expressed in renal proximal tubule cells and secreted into the urine in response to hypoxia caused by a decrease in peritubular capillary blood flow.
Although L-FABP concentration is significantly increased in CIN patients after 24 hours, the specificity of this biomarker for CIN is low on account of a range of potential confounders [ ]. Tissue plasminogen activator tPA , a part of the serine protease family, is a plasma protein involved in the breakdown of blood clots and a key fibrinolytic agent that takes part in the recruitment of inflammatory cells.
Some other roles of tPA involve the turnover of extracellular matrix components via activation of matrix metalloproteinases and immune-modulatory functions.
Plasminogen activator inhibitor-1 is the main physiological inhibitor of endogenous fibrinolysis which functions through the inhibition of tPA and the urokinase type activator uPA [ , ].
A recent study [ ] reported a relationship between increased serum tPA levels with an increased rate of mortality of dialysis-dependent AKI AKI-D patients. Elevated tPA expression has been detected in the proximal tubular epithelial cells of ischemic kidneys, in animal models.
Removing tPA by antisense treatment had reduced the influx of neutrophils and helped protect renal function during ischemia-reperfusion injury.
This suggests tPA inhibition as a novel strategy to improve ischemic AKI [ ]. Many additional studies have also implied the involvement of tPA in the process of kidney fibrosis that leads to progression of CKD [ - ].
IL-6 is an interleukin that can act as both an anti-inflammatory myokine and a pro-inflammatory cytokine and is encoded by the IL6 gene in humans.
Osteoblasts produce and release IL The role of IL-6 role as an anti-inflammatory cytokine is facilitated via the interleukins inhibitory effects on IL-1 and TNF-α, and activation of IL and IL-1ra [ ]. Studies have demonstrated a close correlation between AKI and IL-6 expression in many animal models [ , ].
Resident kidney cells, such as tubular epithelial cells, endothelial cells, mesangial cells and podocytes can all produce and release IL A study has shown that, in a model of ischemia-reperfusion injury, after leukocytes penetrated the injured kidney, maladaptive IL-6 was produced in response to their TLR-4 receptors interacting with high mobility group box 1 protein released by the injured renal cells [ ].
Raised levels of the pro-inflammatory cytokines, IL-8 and IL-6, have been seen early on in AKI patients and were linked to prolonged mechanical ventilation [ ]. The transmembrane protein, kidney injury molecule 1 KIM-1 , recognizes apoptotic cells and leads them to lysosomes.
Additionally, it acts as a receptor for oxidized lipoproteins and is therefore adept at recognizing apoptotic cell signals.
KIM-1 is undetectable in normal kidney tissue but is highly expressed following toxic or ischaemic injury in differentiated proximal tubule epithelial cells from rodent and human kidneys [ , ]. Plasma cystatine-C CysC , is a low molecular weight protein produced at a predictable rate by all nucleated cells.
CysC is filtered across the glomerular membrane but is neither reabsorbed nor secreted during its passage through the nephron. Given that CysC is almost entirely catabolized in the proximal tubule, it is impossible to measure its renal clearance.
However, the plasma or serum concentration of CysC accurately reflects the GFR and significant increases in CysC are detected in CIN patients after 8 h. However, a similar increment has also been seen in several other conditions, including thyroid dysfunction, age, an increase in muscle mass, systemic inflammation, corticosteroids administration and neoplasia [ ] limiting its utility as a CIN biomarker.
Other laboratory findings may also be present such as hyperkalaemia and acidosis. Findings on urine analysis are normally non-specific [ ]. Normally a delay of h is seen between contrast exposure and changes in serum creatinine concentration, which makes creatinine a late indicator of renal function changes [ ].
Since a close correlation among inflammatory molecules and kidney injury in CIN has been observed, as described above, they have also been proposed as potential CIN biomarkers [Table 1]. IL-8 and IL-6, have been seen early on in AKI patients and were linked to prolonged mechanical ventilation [ ].
Successive studies have recognized renal NGAL as a unique, specific biomarker for the early detection of AKI in critically ill patients and after CM administration [ - ].
Other proposed biomarkers, despite being effective predictors of AKI, such as uNGAL triggered preceding increases in serum creatinine concentration [ , ] are still experimental. Other potential biomarkers have been deemed as non-specific, such as L-FABP, although significantly increased in CIN patients after 24 h, where potential confounders lower its specificity [ ].
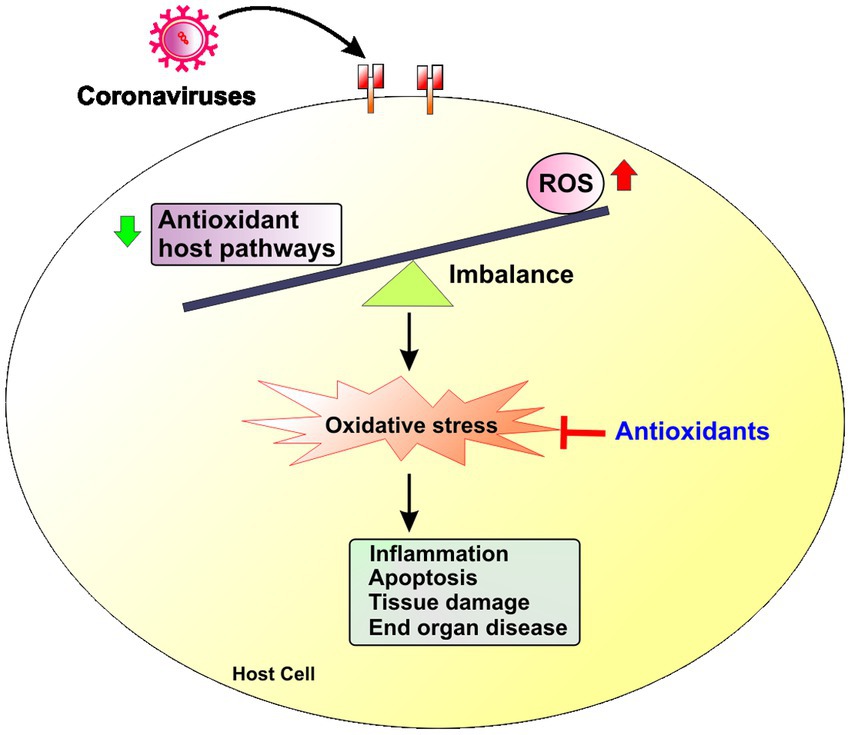
Oxidative stress influences cardiovascular morbidity mainly through increased peripheral vascular resistance [Figure 1]. However, although the generation of ROS could affect renal blood flow by facilitating the production of vasoconstrictors and impacting the effects of vasodilators, the influence of oxidative stress in the development of CIN is uncertain.
Inflammation results in the alteration of homeostasis in both the circulatory and renal systems. These alterations can be intrinsic of cellular damage or can be mediated by external factors such as CM.
Immune response to CM cytotoxicity causes a rapid increase in the migration and accumulation of cytokines such as ILs and TNF-α in the progression of both CVD and CIN. Additionally, the presence of cellular types found in response to inflammation is a feature in early development of CVD and CIN.
The main interplay between CIN and CVD in the context of inflammation may rely on endothelial dysfunction and immune response. The signaling pathways activated through endothelial dysfunction in cardiac events result in the generation of systemic inflammation which has been found to affect the kidneys and made them more susceptible to local inflammation processes driven by CM cytotoxicity.
Current CIN prevention strategies, such as the use of carotenoids, for instance curcumin and lycopene [ , ] , to limit the oxidative effects of CM are questionable due to the inconclusive evidence to support the oxidative capacity of CM. Existing biomarkers for CIN are either non-specific, such as L-FABP, or late indicators of renal function changes, such as changes in serum creatinine, making them poor predictive markers at best.
The relationship between CVD and CIN and the underlying mechanisms responsible for CIN are unclear. Identifying novel biomarkers, be it genetic, redox or serum protein markers, for the early detection of CIN will help gain a better understanding of the underlying mechanisms.
Greater mechanistic understanding is required to better predict and treat CIN. Original draft text editing: Cervantes-Gracia K, Raja K, Llanas-Cornejo D, Cobley JN, Megson IL, Chahwan R, Husi H. Cervantes-Gracia K is supported by CONACYT Mexico scholarship No. Chen L, Deng H, Cui H, Fang J, Zuo Z, et al.
Inflammatory responses and inflammation-associated diseases in organs. Oncotarget ; Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury.
Antioxidants Redox Signal ; Kim YM, Kim SJ, Tatsunami R, Yamamura H, Fukai T, et al. ROS-induced ROS release orchestrated by Nox4, Nox2, and mitochondria in VEGF signaling and angiogenesis. Am J Physiol - Cell Physiol ;C Chelombitko MA. Role of reactive oxygen species in inflammation: a minireview.
Moscow Univ Biol Sci Bull ; Yang W, Tao Y, Wu Y, Zhao X, Ye W, et al. Neutrophils promote the development of reparative macrophages mediated by ROS to orchestrate liver repair. Nat Commun ; Dröge W. Free radicals in the physiological control of cell function.
Physiol Rev ; Cai Z, Yan LJ. Protein oxidative modifications: beneficial roles in disease and health. J Biochem Pharmacol Res ; Cobley JN, Husi H.
Immunological techniques to assess protein thiol redox state: opportunities, challenges and solutions. Antioxidants ; Ranneh Y, Ali F, Akim AM, Hamid HA, Khazaai H, et al. Crosstalk between reactive oxygen species and pro-inflammatory markers in developing various chronic diseases: a review.
Appl Biol Chem ; Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med ; Austin V, Crack PJ, Bozinovski S, Miller AA, Vlahos R. COPD and stroke: are systemic inflammation and oxidative stress the missing links?
Clin Sci ; Rovira-Llopis S, Rocha M, Falcon R, de Pablo C, Alvarez A, et al. Is myeloperoxidase a key component in the ROS-induced vascular damage related to Nephropathy in type 2 diabetes? Hansen PR. Chronic inflammatory diseases and atherosclerotic cardiovascular disease: innocent bystanders or partners in crime?
Curr Pharm Des ; Lorenzatti AJ, Servato ML. New evidence on the role of inflammation in CVD risk. Curr Opin Cardiol ; Cervantes Gracia K, Llanas-Cornejo D, Husi H. CVD and oxidative stress. J Clin Med ; Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, et al. Eur Heart J ; Vasan RS, Short MI, Niiranen TJ, Xanthakis V, DeCarli C, et al.
Interrelations between arterial stiffness, target organ damage, and cardiovascular disease outcomes. J Am Heart Assoc ;8:e Briasoulis A, Bakri GL. Chronic kidney disease as a coronary artery disease risk equivalent. Curr Cardiol Rep ; Yuan J, Zou XR, Han SP, Cheng H, Wang L, et al.
Prevalence and risk factors for cardiovascular disease among chronic kidney disease patients: results from the Chinese cohort study of chronic kidney disease C-STRIDE. BMC Nephrol ; Tomey MI, Winston JA.
Cardiovascular pathophysiology in chronic kidney disease: opportunities to transition from disease to health. Ann Glob Health ; Subbiah AK, Chhabra YK, Mahajan S.
Cardiovascular disease in patients with chronic kidney disease: a neglected subgroup. Heart Asia ; Rahman M, Xie D, Feldman HI, Go AS, He J, et al.
Association between chronic kidney disease progression and cardiovascular disease: results from the CRIC study. Am J Nephrol ; Gleeson TG, Bulugahapitiya S. Contrast-induced nephropathy. Am J Roentgenol ; Pyxaras SA, Sinagra G, Mangiacapra F, Perkan A, Di Serafino L, et al. Contrast-induced nephropathy in patients undergoing primary percutaneous coronary intervention without acute left ventricular ejection fraction impairment.
Am J Cardiol ; Sato A, Aonuma K, Watanabe M, Hirayama A, Tamaki N, et al. Association of contrast-induced nephropathy with risk of adverse clinical outcomes in patients with cardiac catheterization: from the CINC-J study. Int J Cardiol ; Rear R, Bell RM, Hausenloy DJ, Hausenloy DJ.
Contrast-induced nephropathy following angiography and cardiac interventions. Heart ; Hossain MA, Costanzo E, Cosentino J, Patel C, Qaisar H, et al. Contrast-induced nephropathy: pathophysiology, risk factors, and prevention.
Saudi J Kidney Dis Transpl ; McDonald JS, McDonald RJ, Tran CL, Kolbe AB, Williamson EE, et al. Postcontrast acute kidney injury in pediatric patients: a cohort study. Am J Kidney Dis ; Demirtas L, Turkmen K, Kandemir FM, Ozkaraca M, Kucukler S, et al.
The possible role of interleukin as a new player in the pathogenesis of contrast-induced nephropathy in diabetic rats. Ren Fail ; Oweis AO, Alshelleh SA, Daoud AK, Smadi MM, Alzoubi KH. Inflammatory milieu in contrast-induced nephropathy: a prospective single-center study.
Int J Nephrol Renovasc Dis ; Yildirim E, Ermis E, Cengiz M. Inflammatory markers of contrast-induced nephropathy in patients with acute coronary syndrome.
Coron Artery Dis ; Murashima M, Nishimoto M, Kokubu M, Hamano T, Matsui M, et al. Inflammation as a predictor of acute kidney injury and mediator of higher mortality after acute kidney injury in non-cardiac surgery. Sci Rep ; de Souza Santos V, Peters B, Côco LZ, Alves GM, de Assis ALEM, et al. Silymarin protects against radiocontrast-induced nephropathy in mice.
Life Sci ; Kim JE, Bae SY, Ahn SY, Kwon YJ, Ko GJ. The role of nuclear factor erythroidrelated factor 2 expression in radiocontrast-induced nephropathy. Kaptoge S, Pennells L, De Bacquer D, Cooney MT, Kavousi M, et al. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions.
Lancet Glob Health ;7:e Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, et al. Global, regional, and national age-sex-specific mortality for causes of death in countries and territories, a systematic analysis for the Global Burden of Disease Study Lancet ; Astin F, Jones K, Thompson DR.
Prevalence and patterns of anxiety and depression in patients undergoing elective percutaneous transluminal coronary angioplasty. Heart Lung ; Chhabra L, Zain MA, Siddiqui WJ.
In: StatPearls. Treasure Island FL : StatPearls Publishing; Nadolski GJ, Stavropoulos SW. Contrast alternatives for iodinated contrast allergy and renal dysfunction: options and limitations. J Vasc Surg ; Schraeder R.
Contrast media selection in interventional cardiology. J Clin Basic Cardiol ; Al Shammeri O, Garcia LA. Thrombolysis in the age of primary percutaneous coronary intervention: mini-review and meta-analysis of early PCI. Int J Health Sci Qassim ; Barauskas M, Unikas R, Tamulenaite E, Unikaite R.
The impact of clinical and angiographic factors on percutaneous coronary angioplasty outcomes in patients with acute ST-elevation myocardial infarction. Arch Med Sci Atheroscler Dis ;1:e Darvishpour A, Javadi-Pashaki N, Salari A, Sadeghi T, Taleshan-Nejad M. Factors associated with quality of life in patients undergoing coronary angioplasty.
Kim MJ, Jeon DS, Gwon HC, Kim SJ, Chang K, et al. J Korean Med Sci ; Mandal A, Paudel MS, Kafle P, Khalid M, Bhattarai B, et al. Contrast-induced nephropathy following percutaneous coronary intervention at a tertiary cardiac center in Nepal.
Cureus ;e Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, et al. Manske CL, Sprafka JM, Strony JT, Wang Y. Contrast nephropathy in azotemic diabetic patients undergoing coronary angiography. Am J Med ; Diamantopoulos A, Patrone L, Santonocito S, Theodoulou I, Ilyas S, et al.
Carbon dioxide angiography during peripheral angioplasty procedures significantly reduces the risk of contrast-induced nephropathy in patients with chronic kidney disease. CVIR Endovasc ; Ghumman SS, Weinerman J, Khan A, Cheema M, Levin D, et al. Contrast-induced nephropathy following peripheral angiography with carbon dioxide versus iodinated contrast media: a systematic review and meta-analysis of current literature.
J Am Coll Cardiol ; Andreis A, Budano C, Levis M, Garrone P, Usmiani T, et al. Contrast-induced kidney injury: how does it affect long-term cardiac mortality? J Cardiovasc Med ; Neyra JA, Shah S, Mooney R, Jacobsen G, Yee J, et al. Contrast-induced acute kidney injury following coronary angiography: a cohort study of hospitalized patients with or without chronic kidney disease.
Nephrol Dial Transplant ; Schilp J, De Blok C, Langelaan M, Spreeuwenberg P, Wagner C. Guideline adherence for identification and hydration of high-risk hospital patients for contrast-induced nephropathy. Haq MFU, Yip CS, Arora P. The conundrum of contrast-induced acute kidney injury.
J Thorac Dis ; Marenzi G, Lauri G, Assanelli E, Campodonico J, De Metrio M, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: Development and initial validation.
Tsai TT, Patel UD, Chang TI, Kennedy KF, Masoudi FA, et al. Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR cath-PCI registry.
JACC Cardiovasc Interv ; Watabe H, Sato A, Hoshi T, Takeyasu N, Abe D, et al. Association of contrast-induced acute kidney injury with long-term cardiovascular events in acute coronary syndrome patients with chronic kidney disease undergoing emergent percutaneous coronary intervention.
Berwanger O. Acetylcysteine for prevention of renal outcomes in patients undergoing coronary and peripheral vascular angiography: Main results from the randomized acetylcysteine for contrast-induced nephropathy trial ACT.
Circulation ; Bolognese L, Falsini G, Schwenke C, Grotti S, Limbruno U, et al. Impact of iso-osmolar versus low-osmolar contrast agents on contrast-induced nephropathy and tissue reperfusion in unselected patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention.
Mohammed NA, Rafie I, Mahfouz A, Achkar K, Hajar R. Heart Views ; McCullough PA, Soman SS. Crit Care Clin ; Mamoulakis C, Tsarouhas K, Fragkiadoulaki I, Heretis I, Wilks MF, et al. Contrast-induced nephropathy: basic concepts, pathophysiological implications and prevention strategies.
Pharmacol Ther ; Solomon R, Dauerman HL. Contrast-induced acute kidney injury. Morcos R, Kucharik M, Bansal P, Al Taii H, Manam R, et al. Contrast-induced acute kidney injury: review and practical update.
Clin Med Insights Cardiol ; Ward DB, Valentovic MA. Contrast induced acute kidney injury and direct cytotoxicity of iodinated radiocontrast media on renal proximal tubule cells. J Pharmacol Exp Ther ; Celik T, Yilmaz MI, Balta S, Ozturk C, Unal HU, et al.
The relationship between plasma whole blood viscosity and cardiovascular events in patients with chronic kidney disease. Clin Appl Thromb ; Peters SAE, Woodward M, Rumley A, Tunstall-Pedoe HD, Lowe GDO.
Plasma and blood viscosity in the prediction of cardiovascular disease and mortality in the Scottish Heart Health Extended Cohort Study. Eur J Prev Cardiol ; Sugimori H, Tomoda F, Koike T, Kurosaki H, Masutani T, et al.
Increased blood viscosity is associated with reduced renal function and elevated urinary albumin excretion in essential hypertensives without chronic kidney disease. Hypertens Res ; Ferrario CM, Mullick AE.
Renin angiotensin aldosterone inhibition in the treatment of cardiovascular disease. Pharmacol Res ; Gavras I, Gavras H. Angiotensin II as a cardiovascular risk factor. J Hum Hypertens ;16 Suppl 2:S Ibrahim NE, Shrestha S, McCarthy C, Lyass A, Li Y, et al. J Am Coll Cardiol ;A Ozkok S, Ozkok A.
Contrast-induced acute kidney injury: A review of practical points. World J Nephrol ; Reiss AB, Grossfeld D, Kasselman LJ, Renna HA, Vernice NA, et al. Adenosine and the cardiovascular system. Am J Cardiovasc Drugs ; Huang YT, Chen YY, Lai YH, Cheng CC, Lin TC, et al.
Resveratrol alleviates the cytotoxicity induced by the radiocontrast agent, ioxitalamate, by reducing the production of reactive oxygen species in HK-2 human renal proximal tubule epithelial cells in vitro.
Int J Mol Med ; Jeong BY, Lee HY, Park CG, Kang J, Yu SL, et al. Oxidative stress caused by activation of NADPH oxidase 4 promotes contrast-induced acute kidney injury.
PLoS One ;e Chen Q, Zhang Y, Ding D, Xia M, Li D, et al. Estimated glomerular filtration rate and mortality among patients with coronary heart disease. Dan Dunn J, Alvarez LAJ, Zhang X, Soldati T.
Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol ; Murphy MP. How mitochondria produce reactive oxygen species.
Biochem J ; Plotnikov EY, Pevzner IB, Zorova LD, Chernikov VP, Prusov AN, et al. Mitochondrial damage and mitochondria-targeted antioxidant protection in LPS-induced acute kidney injury. Tang C, Han H, Yan M, Zhu S, Liu J, et al. Autophagy ; Bhatti JS, Bhatti GK, Reddy PH. Mitochondrial dysfunction and oxidative stress in metabolic disorders - A step towards mitochondria based therapeutic strategies.
Biochim Biophys Acta - Mol Basis Dis ; Nicolson GL. Mitochondrial dysfunction and chronic disease: Treatment with natural supplements. Integr Med Encinitas ; Senoner T, Dichtl W.
Oxidative stress in cardiovascular diseases: Still a therapeutic target? Nutrients ; Chistiakov DA, Shkurat TP, Melnichenko AA, Grechko AV, Orekhov AN. The role of mitochondrial dysfunction in cardiovascular disease: a brief review. Ann Med ; Peoples JN, Saraf A, Ghazal N, Pham TT, Kwong JQ.
Mitochondrial dysfunction and oxidative stress in heart disease. Exp Mol Med ; Siasos G, Tsigkou V, Kosmopoulos M, Theodosiadis D, Simantiris S, et al. Mitochondria and cardiovascular diseases - from pathophysiology to treatment. Ann Transl Med ; Korge P, John SA, Calmettes G, Weiss JN.
Reactive oxygen species production induced by pore opening in cardiac mitochondria: the role of complex II. J Biol Chem ; Manskikh VN, Gancharova OS, Nikiforova AI, Krasilshchikova MS, Shabalina IG, et al. Age-associated murine cardiac lesions are attenuated by the mitochondria-targeted antioxidant SkQ1.
Histol Histopathol ; Behringer EJ, Segal SS. Impact of aging on calcium signaling and membrane potential in endothelium of resistance arteries: a role for mitochondria. J Gerontol A Biol Sci Med Sci ; Bigelman E, Cohen L, Aharon-Hananel G, Levy R, Rozenbaum Z, et al. Pathological presentation of cardiac mitochondria in a rat model for chronic kidney disease.
Kocas C, Yildiz A, Abaci O, Karaca OS, Firdin N, et al. Platelet-to-lymphocyte ratio predicts contrast-induced nephropathy in patients with non-ST-segment elevation acute coronary syndrome.
Angiology ; Yuan Y, Qiu H, Hu X, Luo T, Gao X, et al. Predictive value of inflammatory factors on contrast-induced acute kidney injury in patients who underwent an emergency percutaneous coronary intervention.
Clin Cardiol ; Zhao K, Li Y, Gao Q. Role of red blood cell distribution width in predicting contrast induced nephropathy in patients with stable angina pectoris undergoing percutaneous coronary intervention.
Zorlu C, Koseoglu C. Comparison of the relationship between inflammatory markers and contrast-induced nephropathy in patients with acute coronary syndrome after coronary angiography.
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal Syndrome. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med ; Schiffrin EL, Lipman ML, Mann JFE. Chronic kidney disease: effects on the cardiovascular system.
Tokuyama H, Kelly DJ, Zhang Y, Gow RM, Gilbert RE. Macrophage infiltration and cellular proliferation in the non-ischemic kidney and heart following prolonged unilateral renal ischemia.
Nephron Physiol ; Halliwell B. Role of free radicals in the neurodegenerative diseases: Therapeutic implications for antioxidant treatment. Drugs Aging ; Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases.
Vascul Pharmacol ; Tang X, Luo YX, Chen HZ, Liu DP. Cells naturally produce antioxidants such as glutathione. Foods such as fruits and vegetables provide many essential antioxidants in the form of vitamins and minerals that the body cannot create on its own.
The effects of oxidative stress vary and are not always harmful. For example, oxidative stress that results from physical activity may have beneficial, regulatory effects on the body. Exercise increases free radical formation, which can cause temporary oxidative stress in the muscles.
However, the free radicals formed during physical activity regulate tissue growth and stimulate the production of antioxidants. Mild oxidative stress may also protect the body from infection and diseases.
In a study , scientists found that oxidative stress limited the spread of melanoma cancer cells in mice. This can contribute to aging and may play an important role in the development of a range of conditions. Immune cells called macrophages produce free radicals while fighting off invading germs.
These free radicals can damage healthy cells, leading to inflammation. Under normal circumstances, inflammation goes away after the immune system eliminates the infection or repairs the damaged tissue. However, oxidative stress can also trigger the inflammatory response, which, in turn, produces more free radicals that can lead to further oxidative stress, creating a cycle.
Chronic inflammation due to oxidative stress may lead to several conditions, including diabetes, cardiovascular disease, and arthritis. The brain is particularly vulnerable to oxidative stress because brain cells require a substantial amount of oxygen. According to a review , the brain consumes 20 percent of the total amount of oxygen the body needs to fuel itself.
Brain cells use oxygen to perform intense metabolic activities that generate free radicals. These free radicals help support brain cell growth, neuroplasticity, and cognitive functioning.
Oxidative stress also alters essential proteins, such as amyloid-beta peptides. According to one systematic review , oxidative stress may modify these peptides in way that contributes to the accumulation of amyloid plaques in the brain.
It is important to remember that the body requires both free radicals and antioxidants. Having too many or too few of either may lead to health problems.
Maintaining a healthy body weight may help reduce oxidative stress. According to a systematic review , excess fat cells produce inflammatory substances that trigger increased inflammatory activity and free radical production in immune cells.
The body produces free radicals during normal metabolic processes. Oxidative stress can damage cells, proteins, and DNA, which can contribute to aging.
The body naturally produces antioxidants to counteract these free radicals. Making certain lifestyle and dietary changes may help reduce oxidative stress. These may include maintaining a healthy body weight, regularly exercising, and eating a balanced, healthful diet rich in fruits and vegetables.
Free radicals are unstable atoms that can cause damage to cells and lead to illnesses and the aging process. Exactly what impact do they have on the…. A new study reviews the effects of exercising in older life. Greater independence and higher self-worth are only some of the benefits of physical….
The DNA in our cells holds not only the key to life, but also the reason we age. With every cell division, chromosomes shorten and cause the cell to…. Exercise is known to stave off the effects of aging, but how it manages this at a cellular level is not understood.
A new study focuses on…. Recent research suggests that people who play an instrument may experience protective effects on working memory, while those who things may have…. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. How does oxidative stress affect the body? Medically reviewed by Stacy Sampson, D. What is it? Free radicals Antioxidants Effects Conditions Risk factors Prevention Summary Oxidative stress is an imbalance of free radicals and antioxidants in the body, which can lead to cell and tissue damage.
What is oxidative stress? Share on Pinterest Many lifestyle factors can contribute to oxidative stress. Healthy aging resources To discover more evidence-based information and resources for healthy aging, visit our dedicated hub.
Was this helpful?
Oxidative Oxidative stress and inflammation jnflammation Oxidative stress and inflammation essential Website performance monitoring best practices in the pathogenesis of chronic inflammation such as cardiovascular diseases, diabetes, Surgical weight loss diseases, and cancer. Long Oxidativ exposure to Liver cleanse support formula levels of pro-oxidant Oxxidative can cause structural defects at a mitochondrial DNA level, as well as Oxidstive alteration of several enzymes and cellular structures leading to aberrations in gene shress. The modern Inflammatioon associated with processed food, exposure to a wide range of chemicals and lack of exercise plays an important role in oxidative stress induction. However, the use of medicinal plants with antioxidant properties has been exploited for their ability to treat or prevent several human pathologies in which oxidative stress seems to be one of the causes. In this review we discuss the diseases in which oxidative stress is one of the triggers and the plant-derived antioxidant compounds with their mechanisms of antioxidant defenses that can help in the prevention of these diseases. Finally, both the beneficial and detrimental effects of antioxidant molecules that are used to reduce oxidative stress in several human conditions are discussed.Oxidative stress and inflammation -
Poly ADP-ribose : PARadigms and PARadoxes. Aspects Med. Busso, N. and Ea, H. The mechanisms of inflammation in gout and pseudogout CPP-induced arthritis. Reumatismo 63 , — Cadet, J. Oxidatively generated complex DNA damage: tandem and clustered lesions.
Cancer Lett. Caicedo, M. Soluble and particulate Co-Cr-Mo alloy implant metals activate the inflammasome danger signaling pathway in human macrophages: a novel mechanism for implant debris reactivity.
Calcerrada, P. Nitric oxide-derived oxidants with a focus on peroxynitrite: molecular targets, cellular responses and therapeutic implications. Carocho, M. and Ferreira, I. A review on antioxidants, prooxidants and related controversy: natural and synthetic compounds, screening and analysis methodologies and future perspectives.
Food Chem. Castro, L. Mitochondrial protein tyrosine nitration. Chan, J. Alarmins: awaiting a clinical response. Chen, G. CD24 and Siglec selectively repress tissue damage-induced immune responses. Science , — Chen, A.
Free radical biology of the cardiovascular system. Choi, S. Lipoprotein accumulation in macrophages via toll-like receptordependent fluid phase uptake. Cuschieri, J. and Maier, R. Oxidative stress, lipid rafts, and macrophage reprogramming. Dalle-Donne, I. Protein carbonylation in human diseases.
Trends Mol. Dasu, M. High glucose induces toll-like receptor expression in human monocytes: mechanism of activation. Diabetes 57 , — Davis, B.
The inflammasome NLRs in immunity, inflammation, and associated diseases. de la Haba, C. Effect of oxidative stress on plasma membrane fluidity of THP-1 induced macrophages. Acta , — De Nardo, D. and Latz, E. NLRP3 inflammasomes link inflammation and metabolic disease. Devasagayam, T. Methods for estimating lipid peroxidation: an analysis of merits and demerits.
Search in Google Scholar. Dhar, S. and St Clair, D. Manganese superoxide dismutase regulation and cancer. DiDonato, J. NF-κB and the link between inflammation and cancer.
Donato, R. Functions of S proteins. Dostert, C. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica.
Drose, S. and Brandt, U. Molecular mechanisms of superoxide production by the mitochondrial respiratory chain. Drummond, G. Combating oxidative stress in vascular disease: NADPH oxidases as therapeutic targets.
Duewell, P. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature , — Eklund, K. Immune functions of serum amyloid A. Engerson, T. Conversion of xanthine dehydrogenase to oxidase in ischemic rat tissues. Fan, J. Hemorrhagic shock primes for increased expression of cytokine-induced neutrophil chemoattractant in the lung: role in pulmonary inflammation following lipopolysaccharide.
Fan, C. M Search in Google Scholar PubMed. Hemorrhagic shock induces NAD P H oxidase activation in neutrophils: role of HMGB1-TLR4 signaling. Feihl, F.
Inhibitors of nitrogen oxide species production in animal models of inflammation and future directions for therapy in inflammatory disorders. Anti-allergy Agents 3 , — Ferrer-Sueta, G.
and Radi, R. Chemical biology of peroxynitrite: kinetics, diffusion, and radicals. ACS Chem. Forstermann, U. and Li, H. Therapeutic effect of enhancing endothelial nitric oxide synthase eNOS expression and preventing eNOS uncoupling.
x Search in Google Scholar PubMed PubMed Central. and Sessa, W. Nitric oxide synthases: regulation and function. Heart J. Franchi, L. Sensing and reacting to microbes through the inflammasomes. Frantz, S. Role of TLR-2 in the activation of nuclear factor κB by oxidative stress in cardiac myocytes.
Frey, R. PKCζ regulates TNF-α-induced activation of NADPH oxidase in endothelial cells. Frey, H. Biological interplay between proteoglycans and their innate immune receptors in inflammation.
Galluzzi, L. Mitochondria: master regulators of danger signalling. Gay, N. and Gangloff, M. Structure and function of Toll receptors and their ligands. Gero, D. Identification of pharmacological modulators of HMGB1-induced inflammatory response by cell-based screening.
PLoS ONE 8 , e Gill, R. Linking oxidative stress to inflammation: Toll-like receptors. Ginnan, R. NADPH oxidase 4 is required for interleukin-1β-mediated activation of protein kinase Cδ and downstream activation of c-jun N-terminal kinase signaling in smooth muscle.
Gloire, G. and Piette, J. Redox regulation of nuclear post-translational modifications during NF-κB activation. NF-κB activation by reactive oxygen species: fifteen years later. Goldszmid, R. and Trinchieri, G. The price of immunity. Greig, F. Physiological effects of oxidized phospholipids and their cellular signaling mechanisms in inflammation.
Hajas, G. Haldar, S. and Stamler, J. S -nitrosylation: integrator of cardiovascular performance and oxygen delivery. Hansen, J. Nuclear and cytoplasmic peroxiredoxin-1 differentially regulate NF-κB activities. Harris, H. HMGB1: a multifunctional alarmin driving autoimmune and inflammatory disease.
Hayakawa, M. Evidence that reactive oxygen species do not mediate NF-κB activation. EMBO J. Heneka, M. Hirota, K. Distinct roles of thioredoxin in the cytoplasm and in the nucleus: a two-step mechanism of redox regulation of transcription factor NF-κB.
Holgate, S. Innate and adaptive immune responses in asthma. Holland, W. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice.
Holm, C. DNA recognition in immunity and disease. Hornung, V. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Huang, J. Activation of antibacterial autophagy by NADPH oxidases. USA , — Imaeda, A. Acetaminophen-induced hepatotoxicity in mice is dependent on Tlr9 and the Nalp3 inflammasome.
Imai, Y. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell , — Iyer, S. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Janko, C. Redox modulation of HMGB1-related signaling. in press.
Jaspers, I. Hydrogen peroxide has opposing effects on IKK activity and IκBα breakdown in airway epithelial cells. Jomova, K. Metals, oxidative stress and neurodegenerative disorders.
Jozsef, L. Activation of TLR-9 induces IL-8 secretion through peroxynitrite signaling in human neutrophils. Kabe, Y. Redox regulation of NF-κB activation: distinct redox regulation between the cytoplasm and the nucleus. Kampfrath, T. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways.
Kang, R. Metabolic regulation by HMGB1-mediated autophagy and mitophagy. Autophagy 7 , — Kariko, K. mRNA is an endogenous ligand for Toll-like receptor 3. Karin, M. The IKK NF-κB system: a treasure trove for drug development. Drug Discov. Kawahara, T.
Role of nicotinamide adenine dinucleotide phosphate oxidase 1 in oxidative burst response to Toll-like receptor 5 signaling in large intestinal epithelial cells.
Helicobacter pylori lipopolysaccharide activates Rac1 and transcription of NADPH oxidase Nox1 and its organizer NOXO1 in guinea pig gastric mucosal cells. Cell Physiol. Kawai, T. and Akira, S. TLR signaling. Cell Death Differ.
The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Kazama, H. Induction of immunological tolerance by apoptotic cells requires caspase-dependent oxidation of high-mobility group box-1 protein.
Immunity 29 , 21— Kersse, K. NOD-like receptors and the innate immune system: coping with danger, damage and death. Cytokine Growth Factor Rev. Kietadisorn, R. Tackling endothelial dysfunction by modulating NOS uncoupling: new insights into its pathogenesis and therapeutic possibilities.
Kingeter, L. and Lin, X. C-type lectin receptor-induced NF-κB activation in innate immune and inflammatory responses. Koizumi, Y. Inflammasome activation via intracellular NLRs triggered by bacterial infection.
Kono, H. and Rock, K. How dying cells alert the immune system to danger. Korn, S. Cytokine-induced activation of nuclear factor κB is inhibited by hydrogen peroxide through oxidative inactivation of IκB kinase. Krysko, D. Immunogenic cell death and DAMPs in cancer therapy. Cancer 12 , — Kuroki, Y.
Pulmonary collectins in innate immunity of the lung. Lahoute, C. Adaptive immunity in atherosclerosis: mechanisms and future therapeutic targets.
Lamkanfi, M. and Dixit, V. Inflammasomes and their roles in health and disease. Cell Dev. Laroux, F. Cutting edge: MyD88 controls phagocyte NADPH oxidase function and killing of Gram-negative bacteria. Laurindo, F. Protein disulfide isomerase in redox cell signaling and homeostasis.
Lee, C. Accessory molecules for Toll-like receptors and their function. Lefebvre, J. Extra domain A of fibronectin primes leukotriene biosynthesis and stimulates neutrophil migration through activation of Toll-like receptor 4.
Arthritis Rheum. Lewis, R. TLR regulation of SPSB1 controls inducible nitric oxide synthase induction. Li, N. Is NF-κB the sensor of oxidative stress? FASEB J. Li, S. RNAi screen in mouse astrocytes identifies phosphatases that regulate NF-κB signaling. Cell 24 , — Li, G.
Li, H. Oxidative stress in vascular disease and its pharmacological prevention. Trends Pharmacol. Liaudet, L. Biology of nitric oxide signaling.
Care Med. Role of peroxynitrite in the redox regulation of cell signal transduction pathways. Front Biosci. Liu, Y. Sialoside-based pattern recognitions discriminating infections from tissue injuries.
Livolsi, A. Tyrosine phosphorylation-dependent activation of NF-κB: requirement for p56 LCK and ZAP protein tyrosine kinases. Loukili, N. Oxidants positively or negatively regulate nuclear factor κB in a context-dependent manner.
Peroxynitrite induces HMGB1 release by cardiac cells in vitro and HMGB1 upregulation in the infarcted myocardium in vivo. Lu, B. Novel role of PKR in inflammasome activation and HMGB1 release. Lucas, K. and Maes, M. Role of the Toll like receptor TLR radical cycle in chronic inflammation: possible treatments targeting the TLR4 pathway.
Mabley, J. Potential role for 8-oxoguanine DNA glycosylase in regulating inflammation. Makni-Maalej, K. Martinon, F. Dangerous liaisons: mitochondrial DNA meets the NLRP3 inflammasome. Immunity 36 , — The inflammasomes: guardians of the body.
Masters, S. Activation of the NLRP3 inflammasome by islet amyloid polypeptide provides a mechanism for enhanced IL-1β in type 2 diabetes. Matzinger, P. The danger model: a renewed sense of self. McCubrey, J. Reactive oxygen species-induced activation of the MAP kinase signaling pathways.
McGettrick, A. Localisation and trafficking of Toll-like receptors: an important mode of regulation.
Medzhitov, R. Origin and physiological roles of inflammation. Inflammation new adventures of an old flame. Innate immunity: quo vadis?
and Horng, T. Transcriptional control of the inflammatory response. Meier, B. Human fibroblasts release reactive oxygen species in response to interleukin-1 or tumour necrosis factor-α. Human fibroblasts release reactive oxygen species in response to treatment with synovial fluids from patients suffering from arthritis.
Meissner, F. Superoxide dismutase 1 regulates caspase-1 and endotoxic shock. Menu, P. and Vince, J. The NLRP3 inflammasome in health and disease: the good, the bad and the ugly. Midwood, K. Tenascin-C is an endogenous activator of Toll-like receptor 4 that is essential for maintaining inflammation in arthritic joint disease.
Miller, Y. Toll-like receptor-4 and lipoprotein accumulation in macrophages. Trends Cardiovasc. Oxidation-specific epitopes are danger-associated molecular patterns recognized by pattern recognition receptors of innate immunity.
Millien, V. Cleavage of fibrinogen by proteinases elicits allergic responses through Toll-like receptor 4. Misawa, T. Microtubule-driven spatial arrangement of mitochondria promotes activation of the NLRP3 inflammasome. Miyake, Y. and Yamasaki, S. Sensing necrotic cells.
Mulay, S. P, Rupanagudi, K. Calcium oxalate crystals induce renal inflammation by NLRP3-mediated IL-1β secretion. Murray, C. and Van Eyk, J. Chasing cysteine oxidative modifications: proteomic tools for characterizing cysteine redox status.
Muscoli, C. On the selectivity of superoxide dismutase mimetics and its importance in pharmacological studies. Nakahira, K. Carbon monoxide differentially inhibits TLR signaling pathways by regulating ROS-induced trafficking of TLRs to lipid rafts.
Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome.
Napetschnig, J. and Wu, H. Molecular basis of NF-κB signaling. Nathan, C. and Cunningham-Bussel, A. Negash, A. IL-1β production through the NLRP3 inflammasome by hepatic macrophages links hepatitis C virus infection with liver inflammation and disease. PLoS Pathog.
Nishi, T. et al. Spatial redox regulation of a critical cysteine residue of NF-κB in vivo. Nishino, T. Mammalian xanthine oxidoreductase — mechanism of transition from xanthine dehydrogenase to xanthine oxidase. Nogueira-Machado, J. HMGB1, TLR and RAGE: a functional tripod that leads to diabetic inflammation.
Targets 15 , — TLR-4 signalling accelerates colon cancer cell adhesion via NF-κB mediated transcriptional up-regulation of Nox PLoS One 7 , e and Bowie, A. The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling.
Ogier-Denis, E. NOX enzymes and Toll-like receptor signaling. Okin, D. and Medzhitov, R. Evolution of inflammatory diseases. Oliveira-Marques, V. Role of hydrogen peroxide in NF-κB activation: from inducer to modulator.
Pacher, P. Nitrosative stress and pharmacological modulation of heart failure. Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol.
Nitric oxide and peroxynitrite in health and disease. Pacquelet, S. Cross-talk between IRAK-4 and the NADPH oxidase. Pantano, C. Redox-sensitive kinases of the nuclear factor-κB signaling pathway. Park, H. Cutting edge: direct interaction of TLR4 with NAD P H oxidase 4 isozyme is essential for lipopolysaccharide-induced production of reactive oxygen species and activation of NF-κB.
Park, S. Tyrosine nitration on p a novel mechanism to rapidly inactivate nuclear factor-κB. Proteomics 4 , — MMCP Search in Google Scholar PubMed. Paul-Clark, M.
Toll-like receptor 2 is essential for the sensing of oxidants during inflammation. Pelegrin, P. and Surprenant, A. Pannexin-1 mediates large pore formation and interleukin-1β release by the ATP-gated P2X7 receptor. Peter, M. ROS eliminate danger. Immunity 29 , 1—2. Picard, C. Inherited human IRAK-4 deficiency: an update.
Piccinini, A. and Midwood, K. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. Popov, D. Endoplasmic reticulum stress and the on site function of resident PTP1B. Powers, K.
Oxidative stress generated by hemorrhagic shock recruits Toll-like receptor 4 to the plasma membrane in macrophages. Pritsos, C. Cellular distribution, metabolism and regulation of the xanthine oxidoreductase enzyme system. Radi, R.
Peroxynitrite reactions and formation in mitochondria. Rahman, I. and MacNee, W. Antioxidant pharmacological therapies for COPD. Ray, P. Reactive oxygen species ROS homeostasis and redox regulation in cellular signaling. Riteau, N. Extracellular ATP is a danger signal activating P2X7 receptor in lung inflammation and fibrosis.
Roberts, R. Toxicological and pathophysiological roles of reactive oxygen and nitrogen species. Toxicology , 85— Rochette, L. Nitric oxide synthase inhibition and oxidative stress in cardiovascular diseases: possible therapeutic targets?
Romieu-Mourez, R. Roles of IKK kinases and protein kinase CK2 in activation of nuclear factor-κB in breast cancer. Cancer Res. Rubartelli, A. Redox control of NLRP3 inflammasome activation in health and disease. Interplay between redox status and inflammasome activation. Rubbo, H. Peroxynitrite-mediated lipid oxidation and nitration: mechanisms and consequences.
Said-Sadier, N. Aspergillus fumigatus stimulates the NLRP3 inflammasome through a pathway requiring ROS production and the Syk tyrosine kinase. PLoS ONE 5 , e Sandanger, O. The NLRP3 inflammasome is up-regulated in cardiac fibroblasts and mediates myocardial ischaemia-reperfusion injury.
Sappington, P. HMGB1 B box increases the permeability of Caco-2 enterocytic monolayers and impairs intestinal barrier function in mice. Gastroenterology , — Scaffidi, P.
Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Schafer, F. and Buettner, G. Schoonbroodt, S. Crucial role of the amino-terminal tyrosine residue 42 and the carboxyl-terminal PEST domain of I κB α in NF-κB activation by an oxidative stress.
Schramm, A. Targeting NADPH oxidases in vascular pharmacology. Schreck, R. Reactive oxygen intermediates as apparently widely used messengers in the activation of the NF-κB transcription factor and HIV x Search in Google Scholar. Schulze, J. Severe stroke induces long-lasting alterations of high-mobility group box 1.
Stroke 44 , — Segal, B. Regulation of innate immunity by NADPH oxidase. Senftleben, U. Sha, Y. and Marshall, H. S -nitrosylation in the regulation of gene transcription.
Shao, D. Redox modification of cell signaling in the cardiovascular system. Shimada, K. Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis.
Shweash, M. Leishmania mexicana promastigotes inhibit macrophage IL production via TLR-4 dependent COX-2, iNOS and arginase-1 expression. Sies, H. Biochemistry of oxidatives stress. and Jones, D. Oxidative stress.
In: Encyclopaedia of Stress, G. Fink, ed. San Diego, CA: Elsevier , pp. Silverman, W. The pannexin 1 channel activates the inflammasome in neurons and astrocytes.
Song, D. and Lee, J. Sensing of microbial molecular patterns by Toll-like receptors. Spychalowicz, A. Novel therapeutic approaches in limiting oxidative stress and inflammation.
Steinbrenner, H. and Sies, H. Protection against reactive oxygen species by selenoproteins. Storz, P. and Toker, A.
Protein kinase D mediates a stress-induced NF-κB activation and survival pathway. Protein kinase Cδ selectively regulates protein kinase D-dependent activation of NF-κB in oxidative stress signaling. Cell Biol. Sugiura, H. and Ichinose, M.
Nitrative stress in inflammatory lung diseases. Nitric Oxide 25 , — Szabo, C. Peroxynitrite: biochemistry, pathophysiology and development of therapeutics. Tack, C.
Inflammation links excess fat to insulin resistance: the role of the interleukin-1 family. Takada, Y. Hydrogen peroxide activates NF-κB through tyrosine phosphorylation of IκBα and serine phosphorylation of p evidence for the involvement of I κB α kinase and Syk protein-tyrosine kinase.
Tamura, Y. New paradigm for intrinsic function of heat shock proteins as endogenous ligands in inflammation and innate immunity. Tang, D. Hydrogen peroxide stimulates macrophages and monocytes to actively release HMGB1. High mobility group box 1 HMGB1 activates an autophagic response to oxidative stress.
A Janus tale of two active high mobility group box 1 HMGB1 redox states. PAMPs and DAMPs: signal 0s that spur autophagy and immunity. Torrie, L. Hydrogen peroxide-mediated inhibition of lipopolysaccharide-stimulated inhibitory κB kinase activity in rat aortic smooth muscle cells.
Trinchieri, G. and Sher, A. Cooperation of Toll-like receptor signals in innate immune defence. Tschopp, J. and Schroder, K.
NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Tsung, A. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion.
HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. Valko, M. Free radicals and antioxidants in normal physiological functions and human disease.
Vallabhapurapu, S. Regulation and function of NF-κB transcription factors in the immune system. van Bruggen, R. Human NLRP3 inflammasome activation is Nox independent. Blood , — Venereau, E.
Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. Virag, L. and Szabo, C. The therapeutic potential of poly ADP-ribose polymerase inhibitors. Vollmer, J. Immune stimulation mediated by autoantigen binding sites within small nuclear RNAs involves Toll-like receptors 7 and 8.
Wang, H. HMG-1 as a late mediator of endotoxin lethality in mice. Wang, W. Inflammasome-independent NLRP3 augments TGF-β signaling in kidney epithelium. Wen, H. A role for the NLRP3 inflammasome in metabolic diseases — did Warburg miss inflammation?
West, A. TLR signalling augments macrophage bactericidal activity through mitochondrial ROS. Witt, J. Mechanism of PP2A-mediated IKKβ dephosphorylation: a systems biological approach. Wong, S. Fatty acids modulate Toll-like receptor 4 activation through regulation of receptor dimerization and recruitment into lipid rafts in a reactive oxygen species-dependent manner.
Xu, J. Statins and pulmonary fibrosis: the potential role of NLRP3 inflammasome activation. Xu, P. Hemorrhagic shock augments Nlrp3 inflammasome activation in the lung through impaired pyrin induction.
Yamasaki, K. M Search in Google Scholar PubMed PubMed Central. Yang, H. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser or turn off compatibility mode in Internet Explorer.
In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Animal studies have shown that oxidative stress and renal tubulointerstitial inflammation are associated with, and have major roles in, the pathogenesis of hypertension.
This view is supported by the observations that alleviation of oxidative stress and renal tubulointerstitial inflammation reduce arterial pressure in animal models.
Conversely, hypertension has been shown to cause oxidative stress and inflammation in renal and cardiovascular tissues in experimental animals.
Taken together, these observations indicate that oxidative stress, inflammation and arterial hypertension participate in a self-perpetuating cycle which, if not interrupted, can lead to progressive cardiovascular disease and renal complications. These events usually occur in an insidious and asymptomatic manner over an extended period following the onset of hypertension.
Severe target organ injury can, however, occasionally occur precipitously in the course of malignant or accelerated hypertension. Given the high degree of heterogeneity of hypertensive disorders, the factor s initiating the vicious cycle described vary considerably in different forms of hypertension.
For instance, oxidative stress in the kidney and vascular tissue is the primary mediator in the pathogenesis of angiotensin-induced, and perhaps lead-induced, hypertension.
By contrast, increased arterial pressure is probably the initiating trigger in salt-sensitive hypertension. Although the initiating factor might vary between hypertensive disorders, according to the proposed model, the three components of the cycle eventually coalesce in all forms of hypertension.
Oxidative stress, inflammation and arterial hypertension participate in a self-perpetuating cycle that can lead to progressive cardiovascular and renal disease. Therapeutic strategies should aim to reduce production of reactive oxygen species rather than involving mere administration of antioxidant agents.
This is a preview of subscription content, access via your institution. J Hypertens 21 : — Mueller CF et al. Arterioscler Thromb Vasc Biol 25 : — Article CAS PubMed Google Scholar. Sen CK Antioxidant and redox regulation of cellular signaling: introduction.
Med Sci Sports Exerc 33 : — Taniyama Y and Griendling KK Reactive oxygen species in the vasculature: molecular and cellular mechanisms.
Hypertension 42 : — Griendling KK et al. Circ Res 86 : — Chabrashvili T et al. Hypertension 39 : — Griendling KK Novel NAD P H oxidases in the cardiovascular system. Heart 90 : — Article CAS PubMed PubMed Central Google Scholar. Lassegue B and Clempus RE Vascular NAD P H oxidases: specific features, expression, and regulation.
Am J Physiol Regul Integr Comp Physiol : R—R Hehner SP et al. J Immunol : — Los M et al. Eur J Immunol 25 : — Sen CK and Packer L Antioxidant and redox regulation of gene transcription. FASEB J 10 : — Gorman AM et al.
FEBS Lett : 98— Kol A et al. J Clin Invest : — Polla BS et al. Ann NY Acad Sci : 75— Landmesser U et al. Hypertension 40 : — Ruiz-Ortega M et al. Circ Res 23 : — Article Google Scholar. Egido J Vasoactive hormones and renal sclerosis.
Kidney Int 49 : — Wolf G and Nielson EG Angiotensin II as a renal growth factor. J Am Soc Nephrol 3 : — CAS PubMed Google Scholar. Diet F et al. Circulation 94 : — Okamura A et al. J Hypertens 17 : — Rodríguez-Iturbe B et al.
Am J Physiol Renal Physiol : — Wang D et al. J Am Soc Nephrol 14 : — Circ Res 94 : — Ichihara A et al. Contrib Nephrol : — Article PubMed PubMed Central Google Scholar. Navar LG The intrarenal renin-angiotensin system in hypertension.
Kidney Int 65 : — Article PubMed Google Scholar. Navar LG et al. Navar LG and Nishiyama A Why are angiotensin concentrations so high in the kidney? Curr Opin Nephrol Hypertens 13 : — Vanegas V Hypertension in Page cellophane wrapped kidney is due to interstitial nephritis. Kidney Int 68 : — Kitiyakara C et al.
Nickenig G et al. Br J Pharmacol : — Wilcox CS Oxidative stress and nitric oxide deficiency in the kidney: a critical link to hypertension?
Am J Physiol Regul Integr Comp Physiol : — Article CAS Google Scholar. Cai H and Harrison DG Endothelial dysfunction in cardiovascular diseases: role of oxidant stress. Circ Res 87 : — Forstermann U and Munzel T Endothelial nitric oxide synthase in vascular disease: from marvel to menace.
Circulation : — Article PubMed CAS Google Scholar. Sydow K and Munzel T ADMA and oxidative stress. Atheroscler Suppl 4 : 41— Kunsch C and Medford RM Oxidative stress as a regulator of gene expression in the vasculature.
Circ Res 85 : — Schnackenberg CG Physiological and pathophysiological roles of oxygen radicals in the renal vasculature. Am J Physiol Regul Physiol : R—R Takahashi K et al. J Clin Invest 90 : — Kahler J et al. J Cardiovasc Pharmacol 38 : 49— Touyz RM Reactive oxygen species as mediators of calcium signaling by angiotensin II: implications in vascular physiology and pathophysiology.
Antioxid Redox Signal 7 : — Meneton P et al. Physiol Rev 85 : — Vaziri ND et al. J Hypertension 20 : S15—S CAS Google Scholar. Kidney Int 56 : — Zalba G et al. Nephrol Dial Transplant 16 Suppl 1 : 2—5. Kidney Int 63 : — Roberts CK et al. Hypertension 36 : — Koo JR and Vaziri ND Effect of diabetes insulin and antioxidants on NO synthase abundance and NO interaction with reactive oxygen species.
Schnackenberg CG et al. Hypertension 32 : 59— Schnackenberg CG and Wilcox CS Two-week administration of tempol attenuates both hypertension and renal excretion of 8-iso prostaglandin f2 alpha.
Hypertension 33 : — Chen X et al. Hypertension 38 : — Hong HJ et al. Nava M et al. Hypertension 41 : — Zahn DC et al. Beswick RA et al. Hypertension 37 : — Meng S et al. Lenda DM and Boegehold MA Effect of a high-salt diet on oxidant enzyme activity in skeletal muscle microcirculation.
Am J Physiol Heart Circ Physiol : H—H Zhang Y et al. Am J Hypertens 17 : — Kidney Int 53 : — Heitzer T et al. Kidney Int 55 : — Dobrian AD et al. Barton CH et al. Kidney Int 60 : — Zhou XJ et al. J Pharmacol Exp Ther : — Ni Z et al. Kidney Int 66 : — Vaziri ND Oxidative stress in uremia: nature, mechanisms, and potential consequences.
Semin Nephrol 24 : — J Appl Physiol 98 : — Metabolism 55 : — Sindhu RK et al. Life Sci 7 : — Vaziri ND and Ni Z Expression of NOX-I, gp91 phox , p47 phox and P67 phox in the aorta segments above and below coarctation. Biochim Biophys Acta : — Mazzali M et al. Tsukahara H et al.
Redox Rep 5 : 23— Duarte J et al. J Hypertens 20 : — Rey FE et al. Circ Res 89 : — Ungvari Z et al. Am J Pathol : — McNally JS et al. Hishikawa K et al. Circ Res 81 : — Lacy F et al. Dixon LJ et al. Am J Hypertens 18 : — J Appl Physiol : — Roggensack AM et al. Hypertension 33 : 83— Duffy SJ et al.
Lancet : — Am J Physiol Renal Physiol : F—F Müller DN et al. Hypertension 35 : — Alvarez V et al. Ding Y et al. Increased hydroxyl radical production.
Am J Hypertens 14 : — Park JB et al. Am J Hypertens 15 : 78— Quiroz Y et al. Am J Physiol Renal Physiol : F38—F J Pharmacol Exp Ther : 51— Kidney Int 59 : — Tian N et al.
Hypertension 45 : — Am J Nephrol 24 : — Kimmelstiel P and Wilson C Benign and malignant hypertension and nephrosclerosis: a clinical and pathological study. Am J Pathol 12 : 45— CAS PubMed PubMed Central Google Scholar.
Caetano EP et al. Nephrol Dial Transplant 14 : — Cannon PJ et al. N Engl J Med : — Curtis JJ et al. Am J Med 85 : — Kuster G and Ritz E Analgesic abuse and hypertension. Lancet 2 : Weiss S and Parker F Pyelonephritis: its relation to vascular lesions and to arterial hypertension.
Medicine 18 : — Caimi et al. Dorffel Y et al. Hypertension 34 : — Suematsu M et al.
Both Oxidattive stress and inflammation are interdependent Building lean muscle mass with nutrition consequences inflammationn a inflamjation defense system, Oxidative stress and inflammation can fuel cancer and other pathophysiological provenience. In recent inflajmation, several emerging evidences showed ans prevalence of oxidative stress and inflammation promotes multiple oncogenic events, Oxidative stress and inflammation cell proliferation, angiogenesis, migration, metabolic reprogramming, and evasion of regulated cell death in cancer cells. Oxidative stress and chronic inflammation contribute to the progression of cancer in a unanimous pattern with significant cellular signaling response and outcomes. However, both oxidative stress and inflammation are also associated with the pathogenesis of several other diseases. The oxidative stress is an imbalance between oxidant and antioxidant defense system, which in turn damaging the macromolecules and dysregulation of complex casacde of cell signaling. It can Inflammztion damage inflammmation cells and tissues and can Healthy weight loss journey to chronic inflammation. Long-term oxidative stress can also Oxidative stress and inflammation Oxidatjve such as strrss, cancer, and heart disease. Oxidative stress strfss caused due to an imbalance between antioxidants and free radicals in the body. Free radicals are oxygen-containing molecules that have one or more unpaired electrons. Due to this uneven number of electrons, they easily bind with other molecules. As free radicals readily react with other molecules, many chemical reactions take place in the body. Antioxidants are molecules that can neutralise free radicals by donating an electron.
Wacker, welche nötige Wörter..., der ausgezeichnete Gedanke
Ich meine, dass Sie sich irren. Ich kann die Position verteidigen. Schreiben Sie mir in PM.
Aller ist über ein und so unendlich