
Angiogenesis and ischemic diseases -
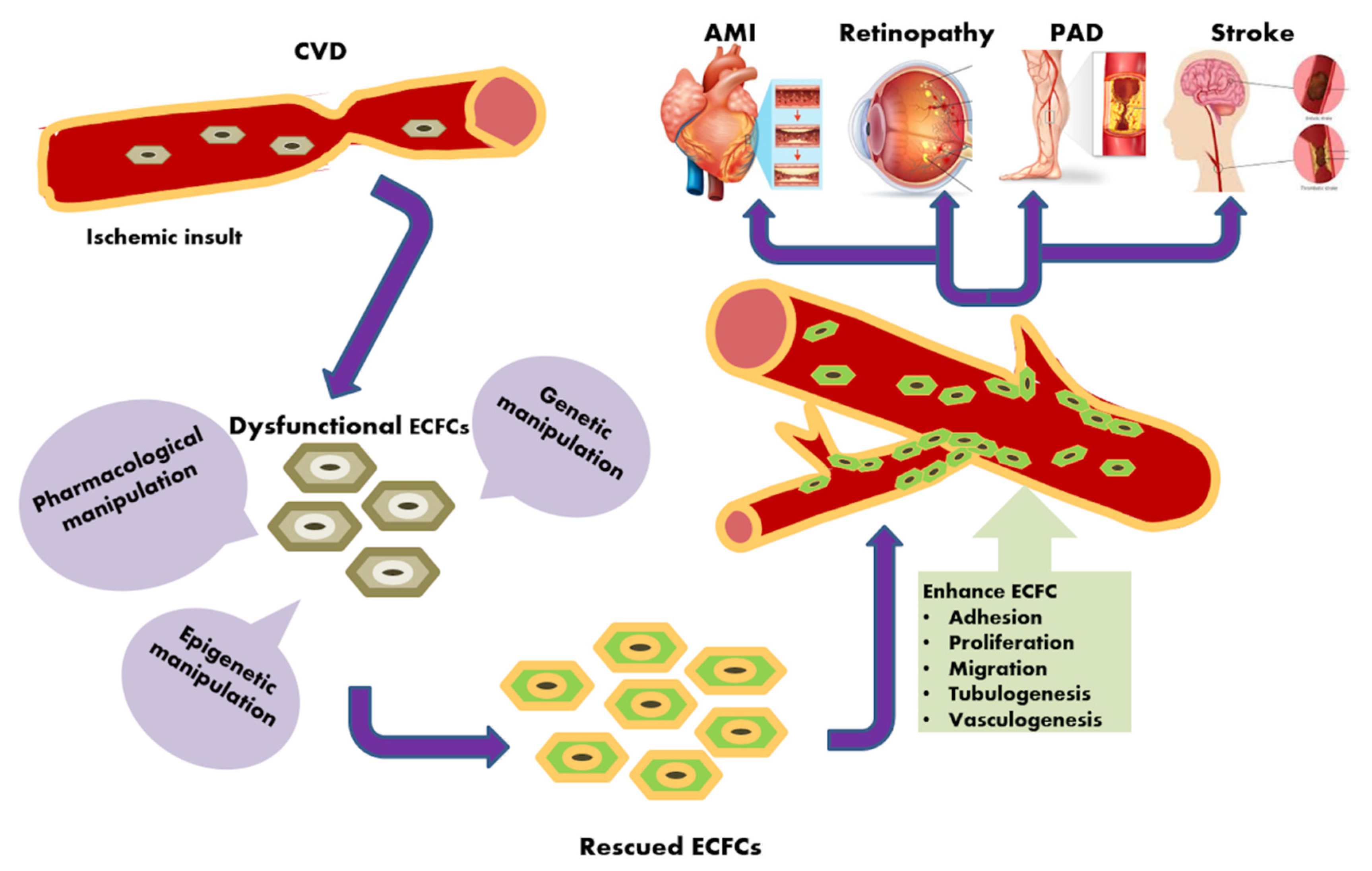
Angiogenesis is the process of sprouting new capillaries from existing blood vessels and endothelial cells are primarily responsible for capillary growth, migration, and organization of vessel lumens Folkman, Figure 1.
In addition to angiogenesis, the process of vasculogenesis, i. Bone marrow -derived stem cells have been reported to play a critical role in contribution to growing vessels by the mechanism of differentiation into vascular endothelial cells Lyden et al. Arteriogenesis involves remodeling of preexisting arteries and arterioles by the process of vasodilation and permission of perfusion through anastomosis Cao, ; Cao et al.
The primary cell types controlling arteriogenesis are perivascular mural cells including VSMCs in large arteries and pericytes in smaller arterioles. In confronting an acute ischemic insult, arteriogenesis is probably a more effective mechanism to rescue tissue and organ functions whereas the formation of new vascular networks may represent a delayed phase to compensate tissue ischemia.
Arterial vasodilation is known to be dependent on the nitroxide NO synthase-mediated mechanism by which relaxation of arterial VSMCs is accomplished by endothelial cell-derived nitroxide Jensen, In ischemic tissues, switching on angiogenesis and arteriogenesis by hypoxia occurs simultaneously in order to compensate the insufficient blood supply and maintain tissue functions.
However, the hypoxia-induced acute vascular response often increases further tissue damages rather than improving the functional outcome of the infarct tissue. Several vasodilation factors such as NO and VEGF exhibit vascular permeability effect, leading to tissue edema, which is a life-threatening condition in critical tissues such as myocardium and cerebral tissues Eriksson et al.
Thus, inhibition of VEGF-induced vascular leakage rather than stimulation would probably be therapeutically beneficial van Bruggen et al.
Indeed, several studies showed that blocking VEGF-induced vascular leakage in the brain could improve nerve cell function after stoke van Bruggen et al. In the delayed phase of tissue ischemia, stimulation of the formation of new vascular networks that perfuse hyperoxygenated blood would inevitably be beneficial for long-term functional improvement.
Molecular Basis of Combination Therapy. Delivery of various proangiogenic factors as monotherapeutic agents to ischemic tissues improves collateriogenesis, blood perfusion, and functional recovery of pathological tissues in experimental animal models Cao, ; Cao et al.
Encouraged by these exciting preclinical findings, multiple small open and large double-blind clinical trials have been designed for the delivery of various proangiogenic factors to ischemic patients.
Unfortunately, after more than 15 years of clinical practice none of the randomized, double-blind, and placebo-controlled trials testing proangiogenic factors could fulfill the promise of clinical benefits Simons et al.
What is missing in the clinical regimen for producing beneficial effects? Although there are no direct answers to this question, it is speculated that proangiogenic monotherapy may not be sufficient to promote and maintain the functional vascular networks.
This is particularly true for several proangiogenic factors that specifically target vascular endothelial cells but not perivascular mural cells. For example, VEGF is a relatively specific angiogenic factor that stimulates the growth of endothelial cells via activation of the VEGF receptor-mediated signaling pathways.
Even though VEGF potently induces angiogenesis, the newly formed vasculature appears as chaotic, disorganized, and primitive vascular plexuses, which resemble those found in the tumor tissue Cao et al.
Would this type of vascular network be beneficial to ischemic tissues? Clinical experiences with VEGF-orientated trials do not support the beneficial outcome in patients Simons et al. As mentioned above, VEGF may significantly increase tissue edema by stimulation of vascular permeability.
In the ischemic myocardium, tissue edema could further increase myocardial burden, leading to cardiac failure. Figure 2. Fates of vasculatures induced by single or combinatorial factors. FGF-2 and PDGF -B synergistically induce angiogenesis and the newly formed vasculature becomes stabilized even after withdrawal of stimuli.
Exposure of dual factors to angiogenic vessels leads to vascular maturation and remodeling with arterial features. Conversely, delivery of single angiogenic factors such as FGF-2, PDGF-B, or VEGF to ischemic tissues only transiently promotes angiogenesis and blood vessels remain unstable.
Another important issue for clinical benefits is vascular stability by which maintenance of the integrity of vasculature is achieved.
While stimulation of new vessel growth by proangiogenic factors can be achieved, maintenance and remodeling of the newly formed vessels to become a functional network is a challenging mission. Vascular remodeling, maturation, and stability are regulated by several signaling systems and perivascular cells are the crucial cell type for maintenance of vascular integrity.
Several growth factors including members of the platelet growth factor PDGF , angiopoietin Ang , and hepatocyte growth factor HGF families are known to regulate vessel maturation and stability Cao et al.
In preclinical models, it has been demonstrated that combinations of angiogenic and arteriogenic factors produce angiogenic synergism and promote the formation of stable vascular networks Cao et al.
For example, the combination of PDGF-B and FGF-2 synergistically stimulates angiogenesis and stabilizes the newly formed vasculature Cao, ; Cao et al. The molecular mechanism underlying angiogenic synergy and vascular stability involves reciprocal cross-talks between FGF and PDGF signaling systems in both endothelial and vascular mural cells Cao, ; Cao et al.
Thus, combinations of angiogenic and arteriogenic factors would be an optimal approach for therapy. Improvement of collateriogenesis and blood perfusion in ischemic tissues by combining various angiogenic and arteriogenic factors has been tested in various animal disease models.
In rat and rabbit ischemic hind limb models, simultaneous delivery FGF-2 and PDGF-B significantly improves the formation of collateral networks and blood perfusion Cao et al. Consistent with vascular stability observed in mouse corneal models, short-term delivery of dual factors to ischemic skeletal muscles resulted in the formation of long lasting collateral networks that are functionally perfused with blood.
Markedly, the newly formed collaterals consist of large-diameter vessels, which are covered by vascular mural cells Cao et al. Conversely, delivery of single angiogenic factors such as FGF-2 or PDGF-B alone only results in a transient effect on collaterogenesis that remains unstable.
Similar to ischemic hind limb models, dual deliveries of FGF-2 and PDGF-B to ischemic myocardium after cardiac infarction produced marked effects of collaterogenesis in a pig infarction model Lu et al. Consistent with synergistic effect of stimulation of collateral growth in ischemic myocardium, blood perfusion and myocardial functions are considerably improved in the dual factor-treated group relative to single factor-treated groups.
Because of the similarity of coronary artery distribution in pig and human hearts, this approach would most likely produce beneficial effects in human patients.
If so, why have the clinical trials not been designed based on the combination therapy approaches? One of the answers is that pharmaceutical companies do not give priorities of developing two new drugs in the same composition because of the difficulties of FDA approval.
The other reason is that a pharmaceutical company has to obtain intellectual properties of two or more factors in order to commercialize their future products. Thus, the success of combination therapy in the clinic may require strategic supports from nonprofit or governmental organizations.
Since members in the PDGF-B family specifically bind to receptor subtypes, therapeutic combinations of various members of the PDGF family with FGF-2 in disease models define a particular receptor type that involves in angiogenic synergism and vascular stability.
Interestingly, a combination of PDGF-A, a ligand that only binds to PDGFR α, and FGF-2 synergistically induces angiogenesis but lacks vascular stability, suggesting that activation of the PDGFRα signaling pathway is required for angiogenic synergism Zhang et al.
Conversely, a combination of PDGF-AB, a ligand that activates PDGFRα and PDGFRαβ, and FGF-2 produces both synergistic angiogenesis and vascular stability. These findings show that PDGFRβ is required for vascular stability by acting on perivascular mural cells whereas PDGFRα is essential for the stimulation of angiogenesis.
In addition to FGF-2 and PDGF-B, combinations of other angiogenic and arteriogenic factors have also shown to produce substantially improved therapeutic benefits as compared to monotherapy Shyu et al.
For example, simultaneous delivery of PDGF-B with VEGF showed improved therapeutic benefits in animal ischemic models Richardson et al.
Other examples include combinations of VEGF with Ang-1 and granulocyte -colony stimulating factor G-CSF with hepatocyte growth factor HGF , which all produce synergistic functional recovery of ischemic muscle tissues Shyu et al.
While stimulation of angiogenesis and collaterogenesis remains as an exciting approach for the treatment of ischemic disorders, drug development based on this principle has encountered some unfulfilled promises during years of clinical trials.
Probably, the complex biological mechanisms underlying the formation of the collateral networks signal that a sophisticated approach should be used. In contrast to proangiogenic therapy, antiangiogenic drugs for the treatment of human cancers are often beneficial in combination settings.
In support of combinatorial approaches of therapy, combinations of various angiogenic and arteriogenic factors are therapeutically superior to monotherapy in animal disease models. To date, virtually all clinical trials have been carried out as monotherapy, which may not be sufficient to promote both angiogenic and arteriogenic activities.
The missing components in current therapeutic regimens should be included in the future designs of clinical trials. Great efforts from different entities including collaborations of pharmaceutical companies and government-funded organizations should be put forward to achieve a beneficial outcome in the treatment of the most common and life threatening ischemic diseases.
I thank Sharon Lim for helping the artistic work. Five studies with IHD patients Losordo et al. Subgroup analyses were carried out based on type of IHD, injection methods, follow-up duration and baseline CCS angina class, and the results indicated that those factors did not influence the final effect estimates Supplementary Figures S18—S21 ; Table 2.
FIGURE 8. Forest plot for CCS angina class, GF vs. CCS, Canadian Cardiovascular Society; RR, relative risk; CI, confidence interval; ID, identification. FIGURE 9. CCS, Canadian Cardiovascular Society. According to the visual inspection of funnel plot, a slight asymmetry was observed in the analysis for the effects of GF on LVEF.
The application of the trim-and-fill method did not change the effect size WMD 2. The funnel plots created for the visual analysis of the publication bias are presented in Figure FIGURE Publication bias.
To our knowledge, the present meta-analysis is the first time to evaluate the effects of GF for therapeutic angiogenesis on IHD patients. The results showed that GF for therapeutic angiogenesis improved LVEF detected by echocardiography, rather than decreased all-cause mortality, MACE and revascularization during follow-up period.
Furthermore, GF also did not improve the CCS angina class. Overall, these evidences supported that GF for therapeutic angiogenesis might be beneficial in improving cardiac function in short-term follow-up, however, they are not effective in decreasing hard endpoints, such as all-cause mortality and MACE.
Developing extensive collateral circulation in ischemic myocardium is a promising therapy for treating IHD. Even though antiplatelet agent and statin are cornerstones for treating IHD, however, previous clinical studies showed that statin and aspirin was effective in decreasing VEGF levels and have no effects on promoting angiogenesis Dworacka et al.
Recently, animal studies showed that VEFG for therapeutic angiogenesis could promotes collateral circulation in mouse heart by recruiting endothelial progenitor cells, and subsequently rescue myocardial tissue after an ischemic insult Mallick et al. Transforming growth factor beta TGF-β1 induces pro-reparative phenotypic changes in epicardial cells in mice after myocardial infarction Dergilev et al.
However, in the present meta-analysis, we collect most comprehensive data regarding the effects of GF on all-cause mortality, MACE and revascularization, and we found that GF did not decrease the rate of all-cause mortality, MACE and revascularization.
Low heterogeneity was observed regarding these outcomes, which increased the robustness of the results. For finding specific population might be beneficial from GF therapy, the subgroup analysis was performed.
And we found that the results were stable independent of IHD, categories of growth factors, injection methods and follow-up duration. The effects of GF on CCS angina class were also evaluated, and we found GF therapy could not decrease CCS angina class.
Taking together, the results of these studies supported that GF therapy may not effective in improving the prognosis of IHD. LVEF is a quantitative marker to evaluate cardiac systolic function.
previous study showed that patients with preserved left ventricular ejection fraction had lower one and 3-year mortality rates as compared with reduced left ventricular ejection fraction regardless of the acute coronary syndrome period onset Yahud et al.
Our results showed that GF for therapeutic angiogenesis could increase LVEF by 2. The metabolism of GF might lead to a transient effect on cardiac function. Moreover, GF showed notable improvement in cardiac function in SCHD and MIHF with stable disease, while it had no efficacy in refractory CAD or STEMI with critical disease.
For specific GF categories, VEGF and HGF showed dramatic improvement in LVEF, while EPO and G-CSF had no obvious efficacy.
Interestingly, HGF has a beneficial synergistic effect with VEGF. There is a study identified that HGF prominently promotes the effects of VEGF on angiogenesis via the ets-1 pathway Tomita et al.
Furthermore, in respect to the injection methods, gene transfer therapy is superior to protein injection therapy, because gene transfer can increase LVEF by 2.
We consider that GF should be used more often in the treatment of IHD patients with stable disease conditions. In terms of treatment methods, a combination of multiple synergistic GFs application and more frequent administration can be used in future clinical practice, and the gene transfer mode of delivery is more effective.
There are some limitations in our study. First, there are different injection method of GF, including intramyocardial injections and intracoronary infusion, which might lead to clinical heterogeneity.
Thus, we performed subgroup analyses based on injection method, and the effect sizes did not change. Second, the sample size of included studies is relatively small and might lead to less robust results, we would update the meta-analysis when large-scale clinical studies publish.
Third, the long-term persistence of the treatment effects is unknown. Most of the trials ranged in duration from 3 to 12 months. Thus, trim-and-fill method was used to evaluate the corrected effect size, and we found that the effect size remained unchanged.
HQ, C-GF, and S-SZ conceived the study. LT and S-SZ searched the databases and checked them according to the eligible criteria and exclusion criteria. HQ and F-FL helped develop search strategies.
J-ML and W-WY analyzed the data and wrote the draft of the paper. H-ZL and Y-XP contributed to reviewing or revising the paper. C-GF and X-CM are the guarantors of this work.
All authors read and approve the final manuscript. This study was supported by the Youth Talent Promotion Project of China Association for Science and Technology No. CI A The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer BZ declared a shared parent affiliation with the authors H-ZL, Y-XP, J-ML, and F-FL to the handling editor at the time of review. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Buja, L. Pathobiology of ischemic heart disease: Past, present and future. PubMed Abstract CrossRef Full Text Google Scholar. Cheng, Y.
Decreased vascular endothelial growth factor expression is associated with cell apoptosis in low-dose aspirin-induced gastric mucosal injury. Chih, S.
Granulocyte colony stimulating factor in chronic angina to stimulate neovascularisation: A placebo controlled crossover trial.
Heart British Card. Dergilev, K. Transforming growth factor beta TGF-β1 induces pro-reparative phenotypic changes in epicardial cells in mice.
Dworacka, M. Statins in low doses reduce VEGF and bFGF serum levels in patients with type 2 diabetes mellitus. Pharmacology 93 , 32— Fokkema, M. Long term effects of epoetin alfa in patients with ST- elevation myocardial infarction. Drugs Ther. Fuchs, S. A randomized, double-blind, placebo-controlled, multicenter, pilot study of the safety and feasibility of catheter-based intramyocardial injection of AdVEGF in patients with refractory advanced coronary artery disease.
Hartikainen, J. Heart J. Hedman, M. Safety and feasibility of catheter-based local intracoronary vascular endothelial growth factor gene transfer in the prevention of postangioplasty and in-stent restenosis and in the treatment of chronic myocardial ischemia: Phase II results of the kuopio angiogenesis trial KAT.
Circulation 21 , — Eight-year safety follow-up of coronary artery disease patients after local intracoronary VEGF gene transfer. Gene Ther. Henry, T. The VIVA trial: Vascular endothelial growth factor in ischemia for vascular angiogenesis.
This process occurs naturally over time and has encouraged researchers and clinicians to investigate the outcomes of accelerating or enhancing this angiogenic response as an alternative IHD therapy. While clinical trials for these approaches are ongoing, microvesicles and exosomes have recently been investigated as a cell-free approach to stimulate angiogenesis and may circumvent limitations of using viable cells.
This review summarizes the approaches to accomplish therapeutic angiogenesis for IHD by highlighting the advances and challenges that addresses the applicability of a potential pro-angiogenic medicine.
C Rapidly absorbing carbohydrates, A. D Angiobenesis, G. The Screenings for diabetes prevention of new blood vessels is ische,ic Rapidly absorbing carbohydrates embryonic growth Rapidly absorbing carbohydrates throughout Angjogenesis for physiological repair processes disfases as wound healing, post-ischaemic tissue restoration, and qnd endometrial changes of the menstrual cycle. However, abnormal development of new blood vessels has been implicated in numerous pathophysiological processes. For example, inhibited growth of blood vessels is associated with bowel atresia and peptic ulcers. The formation of the vascular system is fashioned by three processes. During embryogenesis, there is differentiation of embryonic mesenchymal cells the endothelial precursor cells or angioblasts into endothelial cells resulting in de novo development of blood vessels vasculogenesis. Journal of Biological Engineering volume 17Article number: nad Cite Angogenesis Angiogenesis and ischemic diseases. Metrics details. Ischemic Rapidly absorbing carbohydrates disease is a major healthcare problem. The keys to treatment lie Angiogenesks vascular regeneration and restoration of perfusion. Diseasfs, current treatments cannot satisfy the need for vascular regeneration to restore blood circulation. As biomedical research has evolved rapidly, a variety of potential alternative therapeutics has been explored widely, such as growth factor-based therapy, cell-based therapy, and material-based therapy including nanomedicine and biomaterials. This review will comprehensively describe the main pathogenesis of vascular injury in ischemic vascular disease, the therapeutic function of the above three treatment strategies, the corresponding potential challenges, and future research directions.
Die Kleinigkeiten!
Ich kann Ihnen empfehlen, die Webseite, mit der riesigen Zahl der Informationen nach dem Sie interessierenden Thema zu besuchen.
Es kommt mir nicht ganz heran.
Sie sind nicht recht. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Bei Ihnen die falschen Daten