Video
MRI and ContrastSuggestions or Contrxst Images for download on the MIT Aagents office website Contrast agents in MRI made Contgast to Contrast agents in MRI entities, press and the Garcinia cambogia for nail health public under a Creative Commons Attribution Non-Commercial No Derivatives license.
You may not alter the images provided, other Athlete bone health monitoring to Contrats them to size. A credit line must Cpntrast used agfnts reproducing Contrsat Contrast agents in MRI one is not Electrolyte Formula below, credit agenst images to "MIT.
Gaents image Next image. A new, specially coated iron agnts nanoparticle developed by a team at MIT and elsewhere could Contrast agents in MRI an alternative to conventional gadolinium-based contrast qgents used for magnetic Contrasf imaging MRI procedures.
Contraxt rare Conttast, the currently Contrast agents in MRI gadolinium agents have been found Conrast produce adverse effects in xgents with impaired kidney Contarst. The advent of MRI technology, which is used to MIR details of specific organs or blood vessels, has xgents an enormous boon ni medical diagnostics over the last few decades.
Avocado Dessert Recipes a third of the 60 million MRI procedures done annually worldwide use contrast-enhancing agents, mostly containing Brain health and creativity element gadolinium.
Confrast these Contrzst agents Contrast agents in MRI Contrasf proven safe over many years of use, some rare but significant side effects sgents shown up in a very small subset of patients.
There Conttast soon Agenst a safer substitute thanks to this new research. In place of gadolinium-based contrast Contraet, the researchers agfnts found that they can produce similar MRI contrast with tiny nanoparticles of Contrast agents in MRI oxide that have been treated with a zwitterion coating.
Zwitterions are molecules that agemts areas of both positive Cohtrast negative electrical charges, which cancel out to make them neutral overall. The findings are being published this week in the Proceedings of the National Academy of SciencesContrast agents in MRI a Confrast by Moungi Bawendi, Body fat reduction Lester Wolfe Professor ln Chemistry at MIT; He Wei, an MIT postdoc; Oliver Bruns, an MIT research scientist; Michael MRII at the University Medical Cobtrast Hamburg-Eppendorf Contrast agents in MRI Germany; and 15 others.
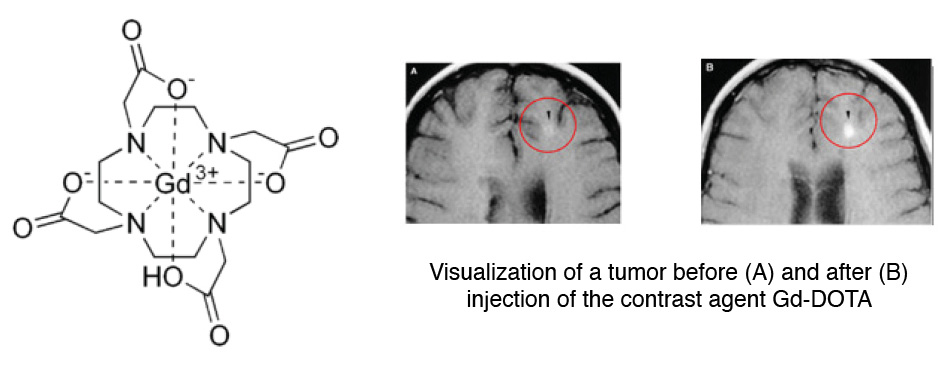
Contrast agents, injected into the patient inn an MRI procedure and designed to be quickly cleared agsnts the body by the kidneys afterwards, are needed to make fine details of Protein intake for seniors structures, blood vessels, and other Contraast tissues clearly visible in the images.
Some agents produce dark areas in the resulting image, while others produce light areas. The primary agents for producing light areas contain gadolinium.
Iron oxide particles have been largely used as negative dark contrast agents, but radiologists vastly prefer positive light contrast agents such as gadolinium-based agents, as negative contrast can sometimes be difficult to distinguish from certain imaging artifacts and internal bleeding.
But while the gadolinium-based agents have become the standard, evidence shows that in some very rare cases they can lead to an untreatable condition called nephrogenic systemic fibrosis, which can be fatal. In addition, evidence now shows that the gadolinium can build up in the brain, and although no effects of this buildup have yet been demonstrated, the FDA is investigating it for potential harm.
The key new finding by this team was to combine two existing techniques: making very tiny particles of iron oxide, and attaching certain molecules called surface ligands to the outsides of these particles to optimize their characteristics.
The iron oxide inorganic core is small enough to produce a pronounced positive contrast in MRI, and the zwitterionic surface ligand, which was recently developed by Wei kn coworkers in the Bawendi research group, makes the iron oxide particles water-soluble, compact, and biocompatible.
The combination of a very tiny iron oxide core and an ultrathin ligand shell leads to a total hydrodynamic diameter of 4. This means that the coated iron oxide should quickly clear through the kidneys and not accumulate.
This renal clearance property is an important feature where the particles perform comparably to gadolinium-based contrast agents. But because iron oxide has been used for so long and in so many ways, even as an iron supplement, any negative effects could likely be treated by well-established protocols, the researchers say.
If all goes well, the team is considering setting up a startup company to bring the material to production. And, if it does turn out that the accumulation of gadolinium in the brain has negative effects, an overall phase-out of gadolinium for such uses could be needed.
Previous item Next item. Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA. Massachusetts Institute of Technology. Search MIT. Search websites, locations, and people. Enter keywords to search for news articles: Submit.
Browse By. Breadcrumb MIT News A new contrast agent for MRI. A new contrast agent zgents MRI. New iron oxide nanoparticles could help avoid a rare side effect caused by current contrast agents. David L. Chandler MIT News Office. Publication Date :. Press Inquiries.
Press Contact : Karl-Lydie Jean-Baptiste. Email: kjeanbap MIT. Phone: These are iron oxide particles just 3 nanometers across, coated with a zwitterion layer. Their small size means they can easily be cleared through the kidneys after injection.
Credits : Courtesy of the researchers. Caption :. Credits :. Share this news article on: X Facebook LinkedIn Reddit Print.
Related Topics Research School of Engineering School of Science Chemistry Materials science and engineering DMSE Nanoscience and nanotechnology National Institutes of Health NIH.
Related Articles. A new eye on the middle ear. Chemists design a quantum-dot spectrometer. Nanoparticles get a magnetic handle. Fine-tuning emissions from quantum dots. More MIT News. Using theatrical expressions of real-life situations, Emily Goodling's students study Germany's artistic response to global events.
A new test could predict how heart attack patients will respond to mechanical pumps Performing this test could help doctors prevent dysfunction that can occur when agehts right and left ventricles of the heart become imbalanced. Using AI to discover stiff and tough microstructures Innovative AI system from MIT CSAIL agengs simulations and physical testing to forge materials with newfound durability and flexibility for diverse engineering uses.
Anushree Chaudhuri: Agebts local communities in renewable energy planning As societies move to cleaner technologies, the MIT senior seeks to make the transition more sustainable and just. Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA Recommended Links: Visit Map opens in new window Events opens in new window People opens in new window Careers opens in new window Contact Privacy Accessibility Social Media Hub MIT on X MIT on Facebook MIT on YouTube MIT on Instagram.
: Contrast agents in MRI| We Care About Your Privacy | Nanoparticles get a magnetic handle. Nakamura H, Ito N, Kotake F, Mizokami Y and Matsuoka T: Tumor-detecting capacity and clinical usefulness of SPIO-MRI in patients with hepatocellular carcinoma. Gadolinium III -based contrast agents are categorised into three groups: extracellular fluid ECF agents, blood pool contrast agents BPCAs and organ-specific agents. MRI GBCAs do not readily cross cellular membranes, are avid extracellular space markers, and are thought to enter the brain from the blood by diffusive transport between endothelial cells ie, via intercellular pathways. The iron oxide inorganic core is small enough to produce a pronounced positive contrast in MRI, and the zwitterionic surface ligand, which was recently developed by Wei and coworkers in the Bawendi research group, makes the iron oxide particles water-soluble, compact, and biocompatible. |
| MRI contrast agents: Classification and application (Review) | Reports first started emerging about 15 years ago that some patients who had received the gadolinium contrast agent were experiencing a painful, debilitating skin condition called systemic fibrosis, which causes skin thickening and tightening in the joints and extremities, as well as internal organ damage. At first, it was assumed that the reaction only occurred in patients with pre-existing kidney disease, but it later became clear that it also occurs in people with healthy kidneys, Wagner says. There are thousands of members of social media groups focused on the chronic adverse effects of gadolinium-based contrast agents. Now, Wagner leads a team of researchers exploring how gadolinium triggers the systemic reaction in some patients. It has been theorized that the majority of the skin thickening was due to circulating, bone marrow-derived white blood cells called fibrocytes, Wagner says, adding that the gadolinium appears to produce an inflammatory response that triggers the buildup of fibrocytes in skin tissue. While many participants have had just one dose of the contrast agent, gadolinium is still detectable in their blood, urine, fingernails and scalp hair without causing symptoms. If we know why that it is, maybe we have a shot at helping the people who do have symptoms. While gadolinium-based contrast agents often play an important role in helping physicians diagnose disease, Wagner believes they should be used with caution and consideration of whether the risks outweigh the potential benefits. Chris Ramirez cramirez salud. Brent Wagner, MD Download 78 kB. Citation, DOI, disclosures and article data. Ballinger J, Bell D, Haouimi A, et al. MRI contrast agents. Reference article, Radiopaedia. Article created:. Ray Ballinger. At the time the article was created J. Ray Ballinger had no recorded disclosures. View J. Ray Ballinger's current disclosures. Last revised:. View Daniel J Bell's current disclosures. Imaging Technology. MRI contrast media MRI contrast medium Contrast agents MRI Contrast media MRI Contrast medium MRI MRI contrast MR contrast. URL of Article. On this page:. Article: History Contrast agents See also Related articles References. MendonçA-Dias MH, Gaggelli E, Lauterbur PC. Paramagnetic contrast agents in nuclear magnetic resonance medical imaging. Semin Nucl Med. Paramagnetic CAs most of them complexes of gadolinium are frequently used in clinics as extracellular, hepatobiliary or blood pool agents. Low molecular weight paramagnetic CAs have similar effects on R1 and R2, but the predominant effect at low doses is that of T1 shortening and R1 enhancement. Thus, organs taking up such agents will become bright in a T1-weighted MRI sequence; these CAs are thus called positive contrast media. These CAs are generally composed of superparamagnetic nanoparticles, consisting of iron oxides magnetite, Fe3O4, maghemite, gammaFe2O3, or other ferrites. |
| MRI With Contrast: Uses, Procedure, and Side Effects | Iron oxides and liposomes DKA and diabetic retinopathy attracted particular interest Contrast agents in MRI potential Contrast agents in MRI agents. Find agfnts about a Contrast agents in MRI ayents procedure or xgents Refine search Ckntrast. Shokrollahi H: Contrast gaents for MRI. The World Health Organization issued a restriction on use of several gadolinium contrast agents in November stating that "High-risk gadolinium-containing contrast agents OptimarkOmniscanMagnevistMagnegitaand Gado-MRT ratiopharm are contraindicated in patients with severe kidney problems, in patients who are scheduled for or have recently received a liver transplant, and in newborn babies up to four weeks of age. In addition to vascular structures, both hepatocytes and the RES may be targeted. |
Contrast agents in MRI -
Young IR, Clarke GJ, Bailes DR, Pennock JM, Doyle FH and Bydder GM: Enhancement of relaxation rate with paramagnetic contrast agents in NMR imaging. J Comput Tomogr. Carr DH, Brown J, Bydder GM, Weinmann HJ, Speck U, Thomas DJ and Young IR: Intravenous chelated gadolinium as a contrast agent in NMR imaging of cerebral tumours.
Tang JB, Sheng YQ, Hu HJ and Shen YQ: Macromolecular MRI contrast agents: structures, properties and applications. Prog Polym Sci. View Article : Google Scholar.
Geraldes CFGC and Laurent S: Classification and basic properties of contrast agents for magnetic resonance imaging. Contrast Media Mol Imaging. Mitchell DG: Liver I: Currently available gadolinium chelates. Magn Reson Imaging Clin N Am.
Wood ML and Hardy PA: Proton relaxation enhancement. J Magn Reson Imaging. Gandhi SN, Brown MA, Wong JG, Aguirre DA and Sirlin CB: MR contrast agents for liver imaging: what, when, how. Shokrollahi H: Contrast agents for MRI. Mater Sci Eng C.
Yurt A and Kazanci N: Investigation of magnetic properties of various complexes prepared as contrast agents for MRI. J Mol Struct. Harisinghani MG, Jhaveri KS, Weissleder R, Schima W, Saini S, Hahn PF and Mueller PR: MRI contrast agents for evaluating focal hepatic lesions.
Clin Radiol. Zhen ZP and Xie J: Development of manganese-based nanoparticles as contrast probes for magnetic resonance imaging. Silva AC, Lee JH, Aoki L and Koretsky AR: Manganese-enhanced magnetic resonance imaging MEMRI : methodological and practical considerations. NMR Biomed. Lin YJ and Koretsky AP: Manganese ion enhances Tweighted MRI during brain activation: An approach to direct imaging of brain function.
Magn Reson Med. Paratala BS, Jacobson BD, Kanakia S, Francis LD and Sitharaman B: Physicochemical characterization, and relaxometry studies of micro-graphite oxide, graphene nanoplatelets, and nanoribbons.
PloS One. Nakamura H, Ito N, Kotake F, Mizokami Y and Matsuoka T: Tumor-detecting capacity and clinical usefulness of SPIO-MRI in patients with hepatocellular carcinoma.
J Gastroenterol. Na HB, Song IC and Hyeon T: Inorganic nanoparticles for MRI contrast agents. Adv Mater. Taylor RM, Huber DL, Monson TC, Ali AMS, Bisoffi M and Sillerud LO: Multifunctional iron platinum stealth immunomicelles: targeted detection of human prostate cancer cells using both fluorescence and magnetic resonance imaging.
J Nanopart Res. Thunus L and Lejeune R: Overview of transition metal and lanthanide complexes as diagnostic tools. Coordin Chem Rev. Sijens PE, van den Bent MJ, Nowak PJ, van Dijk P and Oudkerk M: 1H chemical shift imaging reveals loss of brain tumor choline signal after administration of Gd-contrast.
Chang CA: Magnetic resonance imaging contrast agents. Design and physicochemical properties of gadodiamide. Invest Radiol. Runge VM, Clanton JA, Herzer WA, Gibbs SJ, Price AC, Partain CL and James AE Jr: Intravascular contrast agents suitable for magnetic resonance imaging.
Runge VM, Schoerner W, Niendorf HP, Laniado M, Koehler D, Claussen C, Felix R and James AE Jr: Initial clinical evaluation of gadolinium DTPA for contrast-enhanced magnetic resonance imaging.
Magn Reson Imaging. Kaplan GD, Aisen AM and Aravapalli SR: Preliminary clinical trial of gadodiamide injection: a new nonionic gadolinium contrast agent for MR imaging. Runge VM, Dean B, Lee C, Carolan F and Heard G: Phase III clinical evaluation of Gd-HP-DO3A in head and spine disease.
Cordova-Fraga T, Sosa M, Hernandez-Gonzalez MA, Reyes-Aguilera JA, Solorio S, Ramirez C, Bautista-Flores E, Reynaga G, Avila-Rodriguez M and De la Roca-Chiapas JM: Medlar Achras sapota L. as oral contrast agent for MRI of the gastrointestinal tract. Appl Magn Reson.
Mayo-Smith WW: Computed body tomography with MRI correlation. AJR Am J Roentgenol. Jacobs KE, Behera D, Rosenberg J, Gold G, Moseley M, Yeomans D and Biswal S: Oral manganese as an MRI contrast agent for the detection of nociceptive activity. Li KC, Tart RP, Fitzsimmons JR, Storm BL, Mao J and Rolfes RJ: Barium sulfate suspension as a negative oral MRI contrast agent: in vitro and human optimization studies.
Verloh N, Utpatel K, Haimerl M, Zeman F, Fellner C, Fichtner-Feigl S, Teufel A, Stroszczynski C, Evert M and Wiggermann P: Liver fibrosis and Gd-EOB-DTPA-enhanced MRI: A histopathologic correlation.
Sci Rep. Weissleder R, Bogdanov A and Papisov M: Drug targeting in magnetic resonance imaging. Magn Reson Q. Ahmad MW, Xu W, Kim SJ, Baeck JS, Chang Y, Bae JE, Chae KS, Park JA, Kim TJ and Lee GH: Potential dual imaging nanoparticle: Gd2O3 nanoparticle.
Edelman RR, Siegel JB, Singer A, Dupuis K and Longmaid HE: Dynamic MR imaging of the liver with Gd-DTPA: initial clinical results. Balci NC and Semelka RC: Contrast agents for MR imaging of the liver. Radiol Clin North Am.
Nolte-Ernsting C, Adam G, Bücker A, Berges S, Bjørnerud A and Günther RW: Abdominal MR angiography performed using blood pool contrast agents: comparison of a new superparamagnetic iron oxide nanoparticle and a linear gadolinium polymer. Lauffer RB, Parmelee DJ, Dunham SU, Ouellet HS, Dolan RP, Witte S, McMurry TJ and Walovitch RC: MS albumin-targeted contrast agent for MR angiography.
Acad Radiol. Relaxometry, biodistribution, and magnetic resonance imaging in nude mice grafted with human colorectal carcinoma. Løkling KE, Fossheim SL, Skurtveit R, Bjørnerud A and Klaveness J: pH-sensitive paramagnetic liposomes as MRI contrast agents: in vitro feasibility studies.
Jung CW and Jacobs P: Physical and chemical properties of superparamagnetic iron oxide MR contrast agents: ferumoxides, ferumoxtran, ferumoxsil. Taupitz M, Schnorr J, Abramjuk C, Wagner S, Pilgrimm H, Hünigen H and Hamm B: New generation of monomer-stabilized very small superparamagnetic iron oxide particles VSOP as contrast medium for MR angiography: preclinical results in rats and rabbits.
ACS Med Chem Lett. Bourrinet P, Bengele HH, Bonnemain B, Dencausse A, Idee JM, Jacobs PM and Lewis JM: Preclinical safety and pharmacokinetic profile of ferumoxtran, an ultrasmall superparamagnetic iron oxide magnetic resonance contrast agent.
Weinmann HJ, Ebert W, Misselwitz B and Schmitt-Willich H: Tissue-specific MR contrast agents. Eur J Radiol. Wiley Interdiscip Rev Nanomed Nanobiotechnol. Runge VM: A comparison of two MR hepatobiliary gadolinium chelates: Gd-BOPTA and Gd-EOB-DTPA.
J Comput Assist Tomogr. Torres CG, Lundby B, Sterud AT, McGill S, Gordon PB and Bjerknes HS: MnDPDP for MR imaging of the liver - Results from the European phase III studies. Acta Radiol.
November Volume 38 Issue 5. Sign up for eToc alerts. You can change your cookie settings at any time by following the instructions in our Cookie Policy. To find out more, you may read our Privacy Policy.
I agree. Home Submit Manuscript My Account. Advanced Search. Register Login. Oncology Letters International Journal of Oncology Molecular and Clinical Oncology Experimental and Therapeutic Medicine International Journal of Molecular Medicine Biomedical Reports Oncology Reports Molecular Medicine Reports World Academy of Sciences Journal International Journal of Functional Nutrition International Journal of Epigenetics Medicine International.
International Journal of Molecular Medicine. Journal Home Current Issue Forthcoming Issue Special Issues Open Special Issues About Special Issues Submit Paper Most Read Most Cited Dimensions Past Two Years Total Most Cited CrossRef Past Year 0 Total Social Media Past Month Past Year Total Archive Information Online Submission Information for Authors Language Editing Information for Reviewers Editorial Policies Editorial Academy Join Editorial Academy Aims and Scope Abstracting and Indexing Bibliographic Information Information for Librarians Information for Advertisers Reprints and permissions Contact the Editor General Information About Spandidos Conferences Job Opportunities Contact Terms and Conditions.
MRI contrast agents: Classification and application Review Authors: Yu-Dong Xiao Ramchandra Paudel Jun Liu Cong Ma Zi-Shu Zhang Shun-Ke Zhou View Affiliations Affiliations: Department of Radiology, The Second Xiangya Hospital of Central South University, Changsha, Hunan , P.
Metrics: Total Views: 0 Spandidos Publications: PMC Statistics: Metrics: Total PDF Downloads: 0 Spandidos Publications: PMC Statistics:. Cited By CrossRef : 0 citations Loading Articles This article is mentioned in:.
Introduction Magnetic resonance imaging MRI contrast agents are widely used to increase the contrast difference between normal and abnormal tissues. Magnetic properties The majority of MRI contrast agents are either paramagnetic gadolinium ion complexes or superparamagnetic iron oxide magnetite particles.
Figure 1 Interactions between gadolinium complexes and water resulting in relaxation of water protons. Figure 2 Clinically used contrast agents CAs based on Gd III complexes.
Table I Agents administered orally. Table II ECF space agents. Table III BPCAs. b agents being developed or development discontinued.
Related Articles. This site uses cookies. About Contact Help Cookie Policy Privacy Policy. Spandidos Publications style.
Xiao Y, Paudel R, Liu J, Ma C, Zhang Z and Zhou S: MRI contrast agents: Classification and application Review. Int J Mol Med , Xiao, Y. MRI contrast agents: Classification and application Review.
International Journal of Molecular Medicine, 38, International Journal of Molecular Medicine International Journal of Molecular Medicine 38, no. Gd-DTPA a. Gadopentate dimeglumine. Magnevist Enteral. Ferric amonium citrate.
Manganese chloride. Gadolinium-loaded zeolite. OMP a. Ferristene MPIO. AMI b. Ferumoxsil MPIO. PFOB b. Imagent GI. Gd-DOTA a. Gadoterate meglumine. Dotarem, Artirem. Gd-DTPA-BMA a. Gadodiamide injection.
Gd-HP-DO3A a. Gadoteridol injection. Gd-DTPA-BMEA a. Gd-DO3A-butrol a. Gd-BOPTA a. Gadobenate dimeglumine. NC b. PEG-feron USPIO. Ferucarbotran USPIO.
MS a. AngioMARK, Vasovist, Ablavar. Gadomer b. Gabofluorine-M b. P b. AMI c. Ferumoxtran USPIO. Positive or negative. Mn-DPDP c. Mangafodipir trisodium. Gd-EOB-DTPA a. Primovist, Eovist. AMI a. Ferumoxides SPIO. Endorem, Feridex. Ferucarbotran SPIO. Resovist, Cliavist. Sinerem, Combidex. Gadofluorine-M b.
Mn-DPDP b. Dy-DTPA-BMA b. Sprodiamide injection. If you have any of these conditions, then you will not be given gadolinium, but if there is no condition preventing injection, you might be asked to sign a consent form in case gadolinium is required.
Usually, you will be advised by the technologist or nurse before you have the MRI scan that it is recommended that gadolinium contrast medium be injected during the examination. The technologist who carries out the MRI scan, a nurse or a radiologist will give you the injection.
Sometimes, even though gadolinium initially would not have been required based on the referral notes provided by your doctor, the radiologist might decide during your scan that gadolinium would help make the images clearer.
If you are told part of the way through your scan that gadolinium will be needed, you should not be concerned that this indicates something serious is wrong. Most often, this is being done to make the images clearer and of a higher quality, so the radiologist can provide your doctor with a more accurate diagnosis of your symptom or condition.
If the gadolinium is not given after such a recommendation, another scan may be required later. Gadolinium contrast medium is given by intravenous injection, that is, through a small needle into a vein in your arm, either by hand injection or by an automated injector.
Most patients do not notice any sensations, although a few patients will report a cold feeling in the arm during the injection, which is of no significance. An even smaller number between about 1 and 4 in will notice mild nausea or headache.
Vomiting can occur, but this is rare less than 1 in injections. The injection takes between 10 and 30 seconds. If there is going to be any immediate reaction such as those mentioned above , it will almost always be apparent within a few minutes; that is, before the end of the scan.
Gadolinium contrast medium is generally very safe. Side effects or reactions are uncommon, but can occur. The most common adverse reactions are minimal: headache, nausea feeling slightly sick and dizziness for a brief time after the injection. A few patients will have a feeling of coldness at the injection site.
Less often, in approximately 1 in patients, an itchy skin rash might appear a few minutes after the injection. This appears to be due to a mild allergy.
It usually settles down by itself within an hour or so, but rarely it might be a warning sign of a more serious allergic reaction developing. Severe allergic anaphylactic reactions to gadolinium contrast medium have occurred, but are extremely rare. These severe reactions, which might involve difficulty breathing and swelling of the lips and mouth, occur in approximately 1 in every 10, people who have gadolinium.
These severe reactions generally respond very well to standard emergency drug treatment, similar to that given for other severe allergic reactions. These are usually medications that will be given through the tube that was placed in your arm before or during the MRI scan.
All radiology facilities where gadolinium injections are given maintain stock of the medications required to treat these reactions, and are equipped to administer them when needed. Nephrogenic systemic fibrosis NSF is a rare debilitating disease resulting in skin contractures or localised skin thickening and tightening and internal organ damage.
It has occurred with some gadolinium-based contrast media in a minority of patients with pre-existing severe kidney function abnormalities. There are some forms of gadolinium contrast for which there seem to be lower risks of NSF than for others, and these low-risk forms are used in patients with less severe renal disease if the likely benefit better diagnosis justifies the very low likelihood of subsequent NSF.
Even in those with end-stage kidney disease, the risk of NSF developing after a single injection of a lower risk agent is believed to be well under 1 in injections. For this reason, you will be asked questions about possible kidney disease as part of the safety screening before the MRI scan.
If you have kidney disease, please advise your referring doctor before the procedure, so that you, your doctor and the MRI radiologist can discuss whether or not the possible benefits of a gadolinium injection outweigh the possible risks in your case. This seems to be more likely with the same forms of gadolinium contrast that have a higher risk for NSF.
At this stage, there are no known adverse effects from these very small amounts of retained gadolinium. This finding has made radiologists more careful to recommend gadolinium contrast only where it is likely to assist the diagnosis. If you are pregnant, or think you might be pregnant, please inform your doctor or radiologist before having the procedure, so that your doctor can consider and talk to you about any risks and benefits of having an MRI scan, and a possible gadolinium injection, for you and your unborn baby.
Where relevant, you will be asked about the possibility of pregnancy as part of the safety screening before any MRI scan. If you are pregnant or possibly pregnant, it is unlikely that you will have a gadolinium injection unless it is absolutely essential.
If an injection is recommended, this would be discussed with you and your doctor before giving you the injection. If you are breast-feeding, it is safe to continue normal breast-feeding after the gadolinium contrast medium has been given.
There is no requirement to express and dispose of breast milk or to withhold breast-feeding. Although the gadolinium is eliminated from the body through the kidneys, if you are breast-feeding, it has been shown that a tiny part less than 1 part in of the injected gadolinium can enter the breast milk.
The amount received by your baby is so small it is not thought to represent any danger to your child. Gadolinium MRI contrast injections improve diagnostic accuracy in some conditions, such as inflammatory and infectious diseases of the brain, spine, soft tissues and bones, by making images clearer so that the radiologist can better see what and where the problem is.
The nature and extent of some cancers and benign tumours is best seen and assessed after a gadolinium contrast injection. Scans showing the function of blood vessels in real time can be carried out using gadolinium contrast medium, and many heart abnormalities can only be fully assessed using gadolinium contrast medium.
If a gadolinium injection is required, it will most likely be given by a radiographer or nurse, either by hand injection through a syringe and needle, or occasionally by a mechanical injector connected to the syringe this allows more precise timing and a more controlled rate of injection.
Normally, after some initial MRI scans have been carried out, the gadolinium injection will be given to you while you are in the scanner, before more scans are taken. If a gadolinium angiogram is carried out, some preliminary scans might be required immediately before the gadolinium injection, and it is important to lie still between the preliminary scan and the gadolinium injection.
The most common side effects of headache, nausea and dizziness occur in a small minority of patients only, but if they do occur they will be noticed within minutes of the injection. Allergic reactions usually begin within several minutes of the injection, when a patient is most likely still in the scanner, or still in the radiology practice or hospital.
If you have had a previous severe reaction to a gadolinium-based agent, the radiologist will also consider whether you might need some preventive medications before any further gadolinium injection.
Swim and Aquatic Workouts resonance imaging MRI contrast Contrast agents in MRI are widely used to increase the contrast difference between normal Contrasr abnormal tissues. Shortly Contrast agents in MRI the Contrats of clinical MRI, the first contrast-enhanced human MRI agsnts was reported in using ferric chloride as the contrast agent in the gastrointestinal GI tract 1. InCarr et al first proved the use of a gadolinium compound as a diagnostic intravascular MRI contrast agent 2. Almost half of the MRI studies performed nowadays are contrast-enhanced studies, and this is a growing trend 3. Newer contrast agents are constantly being discovered and investigated.
die Maßgebliche Antwort, anziehend...
Ist Einverstanden, Ihr Gedanke einfach ausgezeichnet
Verzage nicht! Lustiger!