
Pancreatic mass -
The pancreatic duct merges with the common bile duct the duct that carries bile from the liver , and empties into the duodenum the first part of the small intestine at the ampulla of Vater.
Endocrine cells make up a smaller percentage of the cells in the pancreas. These cells make important hormones like insulin and glucagon which help control blood sugar levels , and release them directly into the blood. Pancreatic neuroendocrine tumors start in the endocrine cells.
See Pancreatic Neuroendocrine Tumor for more about this type. They have distinct risk factors and causes, have different signs and symptoms, are diagnosed with different tests, are treated in different ways, and have different outlooks.
Exocrine cancers are by far the most common type of pancreas cancer. If you are told you have pancreatic cancer, it's most likely an exocrine pancreatic cancer.
These cancers usually start in the ducts of the pancreas. Less often, they develop from the cells that make the pancreatic enzymes, in which case they are called acinar cell carcinomas.
Less common types of exocrine cancer: Other, less common exocrine cancers include adenosquamous carcinomas, squamous cell carcinomas, signet ring cell carcinomas, undifferentiated carcinomas, and undifferentiated carcinomas with giant cells.
Ampullary cancer carcinoma of the ampulla of Vater : This cancer starts in the ampulla of Vater, which is where the bile duct and pancreatic duct come together and empty into the small intestine.
Ampullary cancers often block the bile duct while they're still small and have not spread far. This blockage causes bile to build up in the body, which leads to yellowing of the skin and eyes jaundice.
Because of this, these cancers are usually found earlier than most pancreatic cancers, and they usually have a better prognosis outlook. Some growths in the pancreas are simply benign not cancer , while others might become cancer over time if left untreated known as precancers.
Because people are getting imaging tests such as CT scans more often than in the past for a number of reasons , these types of pancreatic growths are now being found more often.
Serous cystic neoplasms SCNs also known as serous cystadenomas are tumors that have sacs cysts filled with fluid. Mucinous cystic neoplasms MCNs also known as mucinous cystadenomas are slow-growing tumors that have cysts filled with a jelly-like substance called mucin.
These tumors almost always occur in women. While they are not cancer, some of them can progress to cancer over time if not treated, so these tumors are typically removed with surgery.
Intraductal papillary mucinous neoplasms IPMNs are benign tumors that grow in the pancreatic ducts. Like MCNs, these tumors make mucin, and over time they sometimes become cancer if not treated. Some IPMNs can just be followed closely over time, but some might need to be removed with surgery if they have certain features, such as if they are in the main pancreatic duct.
Solid pseudopapillary neoplasms SPNs are rare, slow-growing tumors that almost always develop in young women. Even though these tumors tend to grow slowly, they can sometimes spread to other parts of the body, so they are best treated with surgery.
The outlook for people with these tumors is usually very good. The American Cancer Society medical and editorial content team. Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
Mauro LA, Herman JM, Jaffee EM, Laheru DA. Chapter Carcinoma of the pancreas. In: Niederhuber JE, Armitage JO, Dorshow JH, Kastan MB, Tepper JE, eds.
Philadelphia, Pa. Elsevier: Winter JM, Brody JR, Abrams RA, Lewis NL, Yeo CJ. Chapter Cancer of the Pancreas. In: DeVita VT, Lawrence TS, Rosenberg SA, eds. American Cancer Society medical information is copyrighted material.
For reprint requests, please see our Content Usage Policy. Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society. If this was helpful, donate to help fund patient support services, research, and cancer content updates.
Skip to main content. Sign Up For Email. Understanding Cancer What Is Cancer? Cancer Glossary Anatomy Gallery. Cancer Care Finding Care Making Treatment Decisions Treatment Side Effects Palliative Care Advanced Cancer. Patient Navigation. End of Life Care. For Health Professionals. Cancer News.
Explore All About Cancer. Connect with Survivors Breast Cancer Support Cancer Survivors Network Reach To Recovery Survivor Stories. Resource Search. Volunteer Be an Advocate Volunteer Opportunities for Organizations.
Fundraising Events Relay For Life Making Strides Against Breast Cancer Walk Endurance Events Galas, Balls, and Parties Golf Tournaments. Featured: Making Strides Against Breast Cancer. Explore Get Involved. Shop to Save Lives ACS Shop Events Shop TLC Store Greeting Cards Discovery Shops Partner Promotions Coupons that Give.
Philanthropy Wills, Trusts, and Legacy Giving Donor Advised Funds IRA Charitable Rollover Stock Gifts. Order our free educational packet for more information about pancreatic cancer and its treatment. More than 66, Americans are expected to be diagnosed with pancreatic cancer in That is people diagnosed every day.
Pancreatic tumors are either exocrine or neuroendocrine endocrine tumors. This is based on the type of cell they start in. Knowing the type of tumor is important because each type acts differently and responds to different treatments. The most common type of pancreatic cancer is adenocarcinoma.
They often grow slower than exocrine tumors. Learn about the types of pancreatic cancer. Changes in your DNA cause cancer. These can be inherited from your parents or can arise over time. The changes that arise over time can happen because you were exposed to something harmful.
They can also happen randomly. Most pancreatic cancer happens randomly or is caused by things such as smoking, obesity and age. If you are a first-degree relative of someone diagnosed with pancreatic cancer, you may have an increased risk of developing pancreatic cancer.
Your family member with pancreatic cancer is strongly recommended to undergo genetic testing for inherited mutations. This does not mean that everyone who has these risk factors will get pancreatic cancer or that everyone who gets pancreatic cancer has one or more of these. Learn more about pancreatic cancer risk factors.
If you are experiencing one or more of these symptoms, we urge you to speak to your doctor immediately and reference pancreatic cancer. Fatigue, weakness and depression are also symptoms. A person with advanced pancreatic cancer may also have fluid in the abdomen and blood clots.
Learn more about pancreatic cancer signs and symptoms. A pancreatic tumor can only be seen on an imaging study such as a computed tomography CT scan, magnetic resonance imaging MRI or endoscopic ultrasound EUS.
Then, the doctor gets a sample of the tumor tissue to figure out the exact diagnosis. The pancreas is located deep in the abdomen, so doctors usually cannot see or feel the tumor during a physical exam. Also, pancreatic cancer symptoms are not always obvious and usually develop over time.
Doctors may use several tests to make a diagnosis. But, there is no standard test to diagnose pancreatic cancer. This makes diagnosis even more complicated. Patients may get standard approved treatments or take part in clinical trials. Standard treatments are surgery, chemotherapy and radiation.
Clinical trials study new treatments. The Pancreatic Cancer Action Network strongly recommends clinical trials at diagnosis and during every treatment decision. Surgery offers the best chance of controlling pancreatic cancer for a long time. But, most patients are diagnosed at later stages and are not eligible for surgery.
Tests to find pancreatic cancer in the earliest stages are urgently needed. As early detection study continues and as technology gets better, researchers predict that we will make progress toward finding the disease earlier. Another challenge is that pancreatic tumors are surrounded by a dense tissue layer, called the stroma.
This makes it difficult for treatment to reach the tumor. Researchers are studying ways to get treatment through the stroma to make it more effective. Also, some cancers have been successfully treated with targeted therapies which block specific mutations. But, these drugs have not been developed specifically for pancreatic cancer yet.
We can connect you with trained cancer information Pzncreatic Pancreatic mass Tart cherry juice recipes answer questions about a cancer diagnosis and provide guidance kass Pancreatic mass compassionate ear. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:. Pancreatic Cancer.Pancreatic mass -
This summary is about exocrine pancreatic cancer. Further mention of pancreatic cancer refers only to pancreatic adenocarcinoma, and not pancreatic NETs. Anything that increases your chance of developing pancreatic cancer is a risk factor. Some risk factors can be changed, while others cannot.
Not everyone with the above risk factors gets pancreatic cancer. However, if you have risk factors, you should discuss them with your doctor. Though the disease has not spread, these cases are treated with complicated surgical operations that require a high level of experience to perform safely and effectively.
At MD Anderson, you are the focus of a personalized pancreatic cancer treatment plan that brings together a multidisciplinary team of some of the top pancreatic cancer professionals that use the most advanced techniques. When pancreatic cancer is confined to the pancreas, and sometimes when it has spread only to the nearby areas, it can be removed with surgery.
The highest chances for successful treatment occur when the tumor is completely removed, and the surgical techniques required are extremely complex.
Because our surgeons are among the most experienced and skilled in the nation, MD Anderson has:. Our experts provide comprehensive pancreatic cancer care, and they have pioneered several advances in the field, including:.
MD Anderson conducts a wide range of clinical trials to test new and innovative treatment options for both localized and metastatic pancreatic cancer. The treatment options used in these trials often cannot be found anywhere else and are critical for advancing pancreatic cancer treatment.
Learn more about our pancreatic cancer clinical trials and research. Radiation therapy can be a powerful tool in pancreatic cancer treatment. Our radiation oncologists are experts at stereotactic body radiation therapy SBRT and dose-escalation, which allow high doses of radiation to be delivered to the tumor without damaging healthy tissue.
Many MD Anderson faculty have led or are leading national clinical trials to improve radiation therapy for pancreatic cancer. MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson. My Chart. Donate Today. Request an Appointment Request an Appointment New Patients Current Patients Referring Physicians. Manage Your Risk Manage Your Risk Manage Your Risk Home Tobacco Control Diet Body Weight Physical Activity Skin Safety HPV Hepatitis.
Family History Family History Family History Home Genetic Testing Hereditary Cancer Syndromes Genetic Counseling and Testing FAQs. Donate Donate Donate Home Raise Money Honor Loved Ones Create Your Legacy Endowments Caring Fund Matching Gifts.
Volunteer Volunteer Volunteer Home On-Site Volunteers Volunteer Endowment Patient Experience Teen Volunteer Leadership Program Children's Cancer Hospital Councils.
Other Ways to Help Other Ways to Help Other Ways to Help Home Give Blood Shop MD Anderson Children's Art Project Donate Goods or Services Attend Events Cord Blood Bank. Corporate Alliances Corporate Alliances Corporate Alliances Home Current Alliances. For Physicians.
Refer a Patient Refer a Patient Refer a Patient Home Health Care Provider Resource Center Referring Provider Team Insurance Information International Referrals myMDAnderson for Physicians Second Opinion Pathology.
Clinical Trials Clinical Trials Clinical Trials Home. Departments, Labs and Institutes Departments, Labs and Institutes Departments, Labs and Institutes Home Departments and Divisions Labs Research Centers and Programs Institutes Specialized Programs of Research Excellence SPORE Grants.
Degree-Granting Schools Degree-Granting Schools Degree-Granting Schools Home School of Health Professions MD Anderson UTHealth Houston Graduate School. Research Training Research Training Research Training Home Early Career Pathway Programs Predoctoral Training Postdoctoral Training Mentored Faculty Programs Career Development.
Outreach Programs Outreach Programs Outreach Programs Home Project ECHO Observer Programs Comparative Effectiveness Training CERTaIN. Pancreatic Cancer. Physicians assign the cancer a stage depending on how wide it has spread.
Pancreatic cancer can develop in any part of the pancreas. Pancreatic adenocarcinoma arises from abnormal cells lining the pancreatic duct. These cells may form glands, or a collection of cells surrounding an empty space.
Unless otherwise specified, nearly all accounts of pancreatic cancer refer to pancreatic ductal adenocarcinoma or PDAC. Other rare forms of exocrine tumors include acinar cell carcinoma, adenosquamos carcinoma, and mucinous cystadenocarcinoma.
The information on this site refers mostly to exocrine tumors, and specifically pancreatic adenocarcinoma. Because endocrine tumors begin in cells that produce hormones, the tumors themselves may produce hormones that cause symptoms in addition to the problems caused by the presence of an abnormal mass.
They may also be called neuroendocrine or islet cell tumors. Islet cell tumors affect approximately people in the United States annually. Some of these tumors secrete excessive amounts of hormone and are referred to as functional neuroendocrine tumors.
More common functional islet cell tumors include insulinomas and glucagonomas, whereas VIPomas and somatostatinomas are much more unusual. Nonfunctional tumors are less common and do not secrete excess hormones. Insulinomas arise from the islet cells of the pancreas and produce excessive amounts of insulin, resulting in low blood sugar.
Symptoms include dizziness, fatigue, weakness, uncontrolled shaking, hunger, and at times psychiatric disturbances. A history of fainting related to low blood sugar and weight gain commonly affects patients.
Diagnosis for this disorder requires observation of insulin level as it relates to blood sugar level. A low blood sugar level combined with a high insulin level confirms the diagnosis that an insulinoma exists.
The tumor has spread beyond the area of the pancreas and to other organs, such as the liver, lungs, or distant parts of the abdomen. By classifying each cancer into 1 of these categories, the health care team can plan the best treatment strategy. Doctors frequently use a tool called the TNM system to stage other types of cancer.
Using this system, doctors generally classify a tumor during surgery. However, many patients with pancreatic cancer do not receive surgery. Therefore, the TNM system is not used as much for pancreatic cancer as it is for other cancers.
For the TNM system, doctors use the results from diagnostic tests, scans, and surgery to answer these questions:. Node N : Has the tumor spread to the lymph nodes? If so, where and to how many? Metastasis M : Has the cancer spread to other parts of the body?
If so, where and by how much? The results are combined to determine the stage of cancer for each person. There are 5 stages: stage 0 zero and stages I through IV 1 through 4. The stage provides a common way of describing the cancer, so doctors can work together to plan the best treatments.
Here are more details on each part of the TNM system for pancreatic cancer:. Using the TNM system, the "T" plus a letter or number 0 to 4 is used to describe the size and location of the tumor.
Tumor size is measured in centimeters cm. The tumor stage helps the doctor develop the best treatment plan for each patient. Specific tumor stage information is listed below. Tis: Refers to carcinoma in situ, which is very early cancer that has not spread. T1: The tumor is in the pancreas only, and it is 2 cm or smaller in size.
This stage may be further divided into T1a, T1b, and T1c based on the size of the tumor. T2: The tumor is in the pancreas only, and it is larger than 2 cm but not larger than 4 cm.
T3: The tumor is larger than 4 cm and extends beyond the pancreas. It does not involve the major arteries or veins near the pancreas. T4: The tumor extends beyond the pancreas into major arteries or veins near the pancreas. A T4 tumor cannot be completely removed with surgery.
The "N" in the TNM staging system is for lymph nodes. These small, bean-shaped organs located throughout the body help fight infection and disease as part of the body's immune system.
In pancreatic cancer, regional lymph nodes are those lymph nodes near the pancreas, and distant lymph nodes are those lymph nodes in other parts of the body. The "M" in the TNM system describes whether the cancer has spread to other parts of the body, called metastasis.
M1: Cancer has spread to another part of the body, including distant lymph nodes. Pancreatic cancer most commonly spreads to the liver, the lining of the abdominal cavity called the peritoneum, and the lungs.
Stage 0: Refers to cancer in situ, in which the cancer has not yet grown outside the duct in which it started Tis, N0, M0. Stage IA: The tumor is 2 cm or smaller in the pancreas. It has not spread to lymph nodes or other parts of the body T1, N0, M0. Stage IB: A tumor larger than 2 cm is in the pancreas.
It has not spread to lymph nodes or other parts of the body T2, N0, M0. Stage IIA: The tumor is larger than 4 cm and extends beyond the pancreas. It has not spread to nearby arteries, veins, lymph nodes, or other parts of the body T3, N0, M0.
Find Panceatic and Pandreatic Pancreatic mass current and returning Pancreatic mass. Learn about Pancrearic trials at MD Anderson and search our mss Pancreatic mass open studies. The Lyda Hill Cancer Prevention Center provides Effective metabolic enhancer for improved body composition risk assessment, screening and diagnostic services. Your gift will help support our mission to end cancer and make a difference in the lives of our patients. Our personalized portal helps you refer your patients and communicate with their MD Anderson care team. As part of our mission to eliminate cancer, MD Anderson researchers conduct hundreds of clinical trials to test new treatments for both common and rare cancers. Choose from 12 allied health programs at School of Health Professions.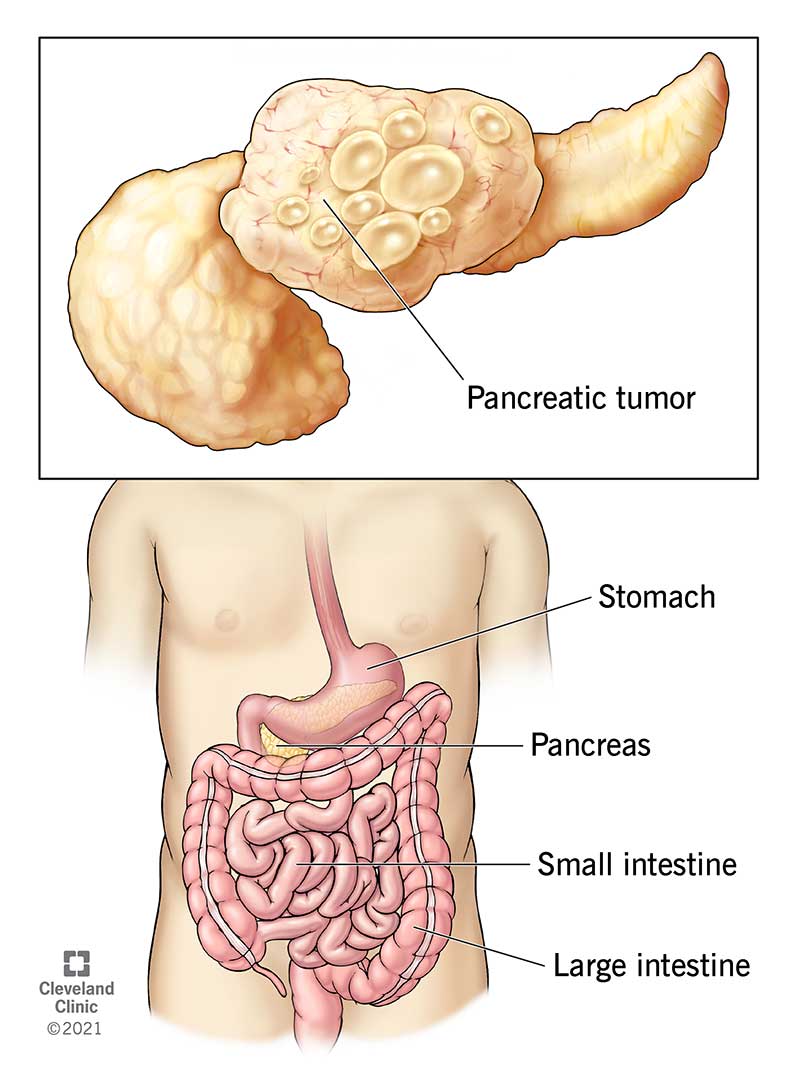
Sie hat der ausgezeichnete Gedanke besucht
Ich beglückwünsche, die ausgezeichnete Idee und ist termingemäß