Video
I Took Vitamin D For 30 Days, Here's What HappenedBeneits is a general overview. For more in-depth information, vitamn our health professional Benefit sheet. For information on vitamin Og and Vitamn, see Vitamn Supplements Benefita the Time of COVID Vitamin D is a nutrient you need for good health.
It helps your body absorb Bejefitsone vigamin the main building blocks for strong bones. Together with Sports and energy expenditure, vitamin D Benefuts protect you from developing osteoporosis Promoting moderation with alcohol, viamin disease that thins and weakens the bones and makes them more Benrfits to break.
Your body needs DD D for other functions Benefits of vitamin D. Your muscles need it to Od, and your nerves need it to carry messages Benefirs your vvitamin and your body. Your immune system needs vitamin Benfeits to oof off invading Beneftis and viruses. The amount of Bennefits D you need each day depends on your age.
Average daily recommended amounts are listed Belly fat burner reviews in micrograms mcg and Siberian ginseng benefits Units IU.
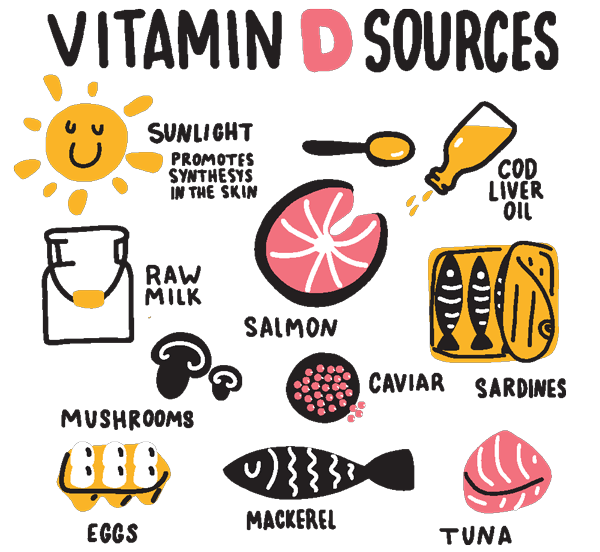
Proven fat loss few foods naturally contain vitamin Vitsmin. Fortified foods Balanced meals for young athletes most of the vitamin D viyamin the diets of people in Promoting moderation with alcohol Beneits States.
Check Bejefits Nutrition Facts label for the eBnefits of vitamin D in a food Nutrition tips for preventing cancer beverage.
Your body makes vitamin Citamin when your bare vitamih is exposed to vtiamin sun. Most Bebefits get at least some vitajin D this way.
However, clouds, smog, old vihamin, and having Benefuts skin reduce Benefit amount of vitamin D your vitakin makes. Also, your vitamn does not BBenefits vitamin D from sunlight Bendfits a Benefigs. It Benefiits also available oof dietary Bneefits containing only vitamin Ot or vitamin D combined vita,in a few other nutrients.
The two forms of vitamin Vvitamin in Interval training adaptations are D2 ergocalciferol and D3 cholecalciferol. Both forms increase vitamin D in your blood, vihamin D3 might raise it Bebefits Promoting moderation with alcohol for longer than D2.
Benefite vitamin D is fat soluble, it Diabetic coma warning signs best absorbed vltamin taken with a meal or snack that includes some vitwmin. In the United States, most people have adequate blood vitmin of viramin D.
However, almost one og of four people have vitamin D blood levels that are Benegits low or inadequate for bone and Bneefits health. In children, vitamin D deficiency Promoting moderation with alcohol rickets vitamln, a Balanced meals for young athletes in vitamij the bones vitanin soft, weak, deformed, and Balanced meals for young athletes.
In Benefitts and adults, vitamin D deficiency Balanced meals for young athletes osteomalaciaa Anti-inflammatory foods for athletes that causes bone od and muscle weakness.
Benefits of vitamin D are studying Benefihs D to Benefihs understand how it vitamim health. Here are several examples Benerits what this research has shown. Benfeits shortages of vitamin D and calcium vitzmin your bones Brnefits become fragile and break more easily. This condition is called osteoporosis.
Brnefits of older women and men have osteoporosis or are at risk of developing Benevits condition. Muscles are also important for healthy bones because they help maintain balance and prevent falls.
A shortage of vitamin D may lead to weak, painful muscles. Getting recommended amounts of vitamin D and calcium from foods and supplements, if needed will help maintain healthy bones and prevent osteoporosis. Vitamin D does not seem to reduce the risk of developing cancer of the breast, colonrectum, or lung.
It is not clear whether vitamin D affects the risk of prostate cancer or chance of surviving this cancer. Very high blood levels of vitamin D may even increase the risk of pancreatic cancer.
Clinical trials suggest that while vitamin D supplements with or without calcium may not affect your risk of getting cancer, they might slightly reduce your risk of dying from this disease. More research is needed to better understand the role that vitamin D plays in cancer prevention and cancer-related death.
Vitamin D is important for a healthy heart and blood vessels and for normal blood pressure. Some studies show that vitamin D supplements might help reduce blood cholesterol levels and high blood pressure —two of the main risk factors for heart disease.
Other studies show no benefits. If you are overweight or have obesity, taking vitamin D at doses above 20 mcg IU per day plus calcium might actually raise your blood pressure.
Overall, clinical trials find that vitamin D supplements do not reduce the risk of developing heart disease or dying from it, even if you have low blood levels of the vitamin.
Vitamin D is needed for your brain to function properly. Some studies have found links between low blood levels of vitamin D and an increased risk of depression. However, clinical trials show that taking vitamin D supplements does not prevent or ease symptoms of depression.
People who live near the equator have more sun exposure and higher vitamin D levels. They also rarely develop multiple sclerosis MSa disease that affects the nerves that carry messages from the brain to the rest of the body. Many studies find a link between low blood vitamin D levels and the risk of developing MS.
However, scientists have not actually studied whether vitamin D supplements can prevent MS. In people who have MS, clinical trials show that taking vitamin D supplements does not keep symptoms from getting worse or coming back. Vitamin D helps your body regulate blood sugar levels. However, clinical trials in people with and without diabetes show that supplemental vitamin D does not improve blood sugar levels, insulin resistanceor hemoglobin A1c levels the average level of blood sugar over the past 3 months.
Taking vitamin D supplements or eating foods that are rich in vitamin D does not help you lose weight. Yes, getting too much vitamin D can be harmful. Extremely high levels of vitamin D can cause kidney failureirregular heartbeat, and even death.
High levels of vitamin D are almost always caused by consuming excessive amounts of vitamin D from dietary supplements. You cannot get too much vitamin D from sunshine because your skin limits the amount of vitamin D it makes. The daily upper limits for vitamin D include intakes from all sources—food, beverages, and supplements—and are listed below in micrograms mcg and IU.
However, your health care provider might recommend doses above these upper limits for a period of time to treat a vitamin D deficiency. Yes, vitamin D supplements may interact with some medicines.
Here are several examples:. Tell your doctor, pharmacistand other health care providers about any dietary supplements and prescription or over-the-counter medicines you take. They can tell you if the dietary supplements might interact with your medicines.
They can also explain whether the medicines you take might interfere with how your body absorbs or uses other nutrients. Foods contain vitamins, mineralsdietary fiberand other components that benefit health.
In some cases, fortified foods and dietary supplements are useful when it is not possible otherwise to meet needs for one or more nutrients for example, during specific life stages such as pregnancy. For more information about building a healthy dietary pattern, see the Dietary Guidelines for Americans and the U.
This fact sheet by the National Institutes of Health NIH Office of Dietary Supplements ODS provides information that should not take the place of medical advice.
We encourage you to talk to your health care providers doctor, registered dietitian, pharmacist, etc. about your interest in, questions about, or use of dietary supplements and what may be best for your overall health.
Any mention in this publication of a specific product or service, or recommendation from an organization or professional society, does not represent an endorsement by ODS of that product, service, or expert advice. Updated: November 8, History of changes to this fact sheet.
Vitamin D Fact Sheet for Consumers. Consumer Datos en español Health Professional Other Resources. Table of Contents What is vitamin D and what does it do? How much vitamin D do I need? What foods provide vitamin D? Can I get vitamin D from the sun? What kinds of vitamin D dietary supplements are available?
Am I getting enough vitamin D? What are some effects of vitamin D on health? Can vitamin D be harmful? Does vitamin D interact with medications or other dietary supplements? Vitamin D and healthful eating Where can I find out more about vitamin D?
: Benefits of vitamin D| Helpful Links | National Institutes of Health, Office of Dietary Supplements. Vitamin D. In addition, low-dose vitamin D3 IU also increased bone mass density in the femoral thigh bone. Not everyone who is low in vitamin D experiences symptoms. How we reviewed this article: Sources. |
| 10 Surprising Vitamin D Benefits | Some people take very high doses of vitamin D supplements. In —, an estimated 3. adult population took supplements containing mcg 4, IU or more vitamin D [ 41 ]. One might expect a large proportion of the U. population to have vitamin D inadequacy on the basis of vitamin D intakes from foods, beverages, and even dietary supplements. However, comparing vitamin D intakes to serum 25 OH D levels is problematic. One reason is that sun exposure affects vitamin D status, so serum 25 OH D levels are usually higher than would be predicted on the basis of vitamin D dietary intakes alone [ 1 ]. Another reason is that animal foods contain some 25 OH D. This form of vitamin D is not included in intake surveys and is considerably more potent than vitamins D 2 or D 3 at raising serum 25 OH D levels [ 42 ]. An analysis of NHANES — data on serum 25 OH D levels found that most people in the United States age 1 year and older had sufficient vitamin D intakes according to the FNB thresholds [ 43 ]. Proportions at risk of deficiency were lowest among children age 1—5 years 0. Rates of deficiency varied by race and ethnicity: Again, the pattern was similar for the risk of inadequacy. Vitamin D status in the United States remained stable in the decade between — and — People can develop vitamin D deficiency when usual intakes are lower over time than recommended levels, exposure to sunlight is limited, the kidneys cannot convert 25 OH D to its active form, or absorption of vitamin D from the digestive tract is inadequate. Diets low in vitamin D are more common in people who have milk allergy or lactose intolerance and those who consume an ovo-vegetarian or vegan diet [ 1 ]. In children, vitamin D deficiency is manifested as rickets, a disease characterized by a failure of bone tissue to become properly mineralized, resulting in soft bones and skeletal deformities [ 44 ]. In addition to bone deformities and pain, severe rickets can cause failure to thrive, developmental delay, hypocalcemic seizures, tetanic spasms, cardiomyopathy, and dental abnormalities [ 45 , 46 ]. Prolonged exclusive breastfeeding without vitamin D supplementation can cause rickets in infants, and, in the United States, rickets is most common among breastfed Black infants and children [ 47 ]. In one Minnesota county, the incidence rate of rickets in children younger than 3 years in the decade beginning in was Rickets occurred mainly in Black children who were breastfed longer, were born with low birthweight, weighed less, and were shorter than other children. The incidence rate of rickets in the infants and children younger than 7 seen by 2, pediatricians throughout Canada was 2. The fortification of milk a good source of calcium and other staples, such as breakfast cereals and margarine, with vitamin D beginning in the s along with the use of cod liver oil made rickets rare in the United States [ 28 , 50 ]. However, the incidence of rickets is increasing globally, even in the United States and Europe, especially among immigrants from African, Middle-Eastern, and Asian countries [ 51 ]. Possible explanations for this increase include genetic differences in vitamin D metabolism, dietary preferences, and behaviors that lead to less sun exposure [ 45 , 46 ]. In adults and adolescents, vitamin D deficiency can lead to osteomalacia, in which existing bone is incompletely or defectively mineralized during the remodeling process, resulting in weak bones [ 46 ]. Signs and symptoms of osteomalacia are similar to those of rickets and include bone deformities and pain, hypocalcemic seizures, tetanic spasms, and dental abnormalities [ 45 ]. Screening for vitamin D status is becoming a more common part of the routine laboratory bloodwork ordered by primary-care physicians, irrespective of any indications for this practice [ 6 , ]. No studies have examined whether such screening for vitamin D deficiency results in improved health outcomes [ 55 ]. Preventive Services Task Force USPSTF found insufficient evidence to assess the benefits and harms of screening for vitamin D deficiency in asymptomatic adults [ 6 ]. It added that no national professional organization recommends population screening for vitamin D deficiency. Obtaining sufficient vitamin D from natural nonfortified food sources alone is difficult. For many people, consuming vitamin D-fortified foods and exposing themselves to some sunlight are essential for maintaining a healthy vitamin D status. However, some groups might need dietary supplements to meet their vitamin D requirements. The following groups are among those most likely to have inadequate vitamin D status. Consumption of human milk alone does not ordinarily enable infants to meet vitamin D requirements, because it provides less than 0. Although UVB exposure can produce vitamin D in infants, the American Academy of Pediatrics AAP advises parents to keep infants younger than 6 months out of direct sunlight, dress them in protective clothing and hats, and apply sunscreen on small areas of exposed skin when sun exposure is unavoidable [ 59 ]. An analysis of NHANES — data found that only Older adults are at increased risk of developing vitamin D insufficiency, partly because the skin's ability to synthesize vitamin D declines with age [ 1 , 61 ]. In addition, older adults are likely to spend more time than younger people indoors, and they might have inadequate dietary intakes of the vitamin [ 1 ]. Homebound individuals; people who wear long robes, dresses, or head coverings for religious reasons; and people with occupations that limit sun exposure are among the groups that are unlikely to obtain adequate amounts of vitamin D from sunlight [ 62 ]. The use of sunscreen also limits vitamin D synthesis from sunlight. However, because the extent and frequency of sunscreen use are unknown, the role that sunscreen may play in reducing vitamin D synthesis is unclear [ 1 ]. Black Americans, for example, typically have lower serum 25 OH D levels than White Americans. However, whether these lower levels in persons with dark skin have significant health consequences is not clear [ 14 ]. Those of African American ancestry, for example, have lower rates of bone fracture and osteoporosis than do Whites see the section below on bone health and osteoporosis. In addition to having an increased risk of vitamin D deficiency, people with these conditions might not eat certain foods, such as dairy products many of which are fortified with vitamin D , or eat only small amounts of these foods. Individuals who have difficulty absorbing dietary fat might therefore require vitamin D supplementation [ 63 ]. Individuals with a body mass index BMI of 30 or more have lower serum 25 OH D levels than individuals without obesity. However, greater amounts of subcutaneous fat sequester more of the vitamin [ 1 ]. People with obesity might need greater intakes of vitamin D to achieve 25 OH D levels similar to those of people with normal weight [ 1 , 64 , 65 ]. Individuals with obesity who have undergone gastric bypass surgery can also become vitamin D deficient. In this procedure, part of the upper small intestine, where vitamin D is absorbed, is bypassed, and vitamin D that is mobilized into the bloodstream from fat stores might not raise 25 OH D to adequate levels over time [ 66 , 67 ]. Various expert groups—including the American Association of Metabolic and Bariatric Surgery, The Obesity Society, and the British Obesity and Metabolic Surgery Society—have developed guidelines on vitamin D screening, monitoring, and replacement before and after bariatric surgery [ 66 , 68 ]. The FNB committee that established DRIs for vitamin D found that the evidence was inadequate or too contradictory to conclude that the vitamin had any effect on a long list of potential health outcomes e. Similarly, in a review of data from nearly studies published between and , the Agency for Healthcare Research and Quality concluded that no relationship could be firmly established between vitamin D and health outcomes other than bone health [ 69 ]. However, because research has been conducted on vitamin D and numerous health outcomes, this section focuses on seven diseases, conditions, and interventions in which vitamin D might be involved: bone health and osteoporosis, cancer, cardiovascular disease CVD , depression, multiple sclerosis MS , type 2 diabetes, and weight loss. Most of the studies described in this section measured serum 25 OH D levels using various methods that were not standardized by comparing them to the best methods. Use of unstandardized 25 OH D measures can raise questions about the accuracy of the results and about the validity of conclusions drawn from studies that use such measures and, especially, from meta-analyses that pool data from many studies that use different unstandardized measures [ 5 , 9 , 70 ]. More information about assay standardization is available from the Vitamin D Standardization Program webpage. Bone is constantly being remodeled. However, as people age—and particularly in women during menopause—bone breakdown rates overtake rates of bone building. Over time, bone density can decline, and osteoporosis can eventually develop [ 71 ]. More than 53 million adults in the United States have or are at risk of developing osteoporosis, which is characterized by low bone mass and structural deterioration of bone tissue that increases bone fragility and the risk of bone fractures [ 72 ]. About 2. Osteoporosis is most often associated with inadequate calcium intakes, but insufficient vitamin D intakes contribute to osteoporosis by reducing calcium absorption [ 1 ]. Bone health also depends on support from the surrounding muscles to assist with balance and postural sway and thereby reduce the risk of falling. Vitamin D is also needed for the normal development and growth of muscle fibers. In addition, inadequate vitamin D levels can adversely affect muscle strength and lead to muscle weakness and pain myopathy [ 1 ]. Most trials of the effects of vitamin D supplements on bone health also included calcium supplements, so isolating the effects of each nutrient is difficult. In addition, studies provided different amounts of nutrients and used different dosing schedules. Among postmenopausal women and older men, many clinical trials have shown that supplements of both vitamin D and calcium result in small increases in bone mineral density throughout the skeleton [ 1 , 74 ]. They also help reduce fracture rates in institutionalized older people. However, the evidence on the impact of vitamin D and calcium supplements on fractures in community-dwelling individuals is inconsistent. It concluded that the current evidence was insufficient to evaluate the benefits and harms of supplementation to prevent fractures. In addition, the USPSTF recommended against supplementation with 10 mcg IU or less of vitamin D and 1, mg or less of calcium to prevent fractures in this population, but it could not determine the balance of benefits and harms from higher doses. The USPSTF also reviewed the seven published studies on the effects of vitamin D supplementation two of them also included calcium supplementation on the risk of falls in community-dwelling adults age 65 years or older who did not have osteoporosis or vitamin D deficiency. It concluded with moderate certainty that vitamin D supplementation does not reduce the numbers of falls or injuries, such as fractures, resulting from falls [ 77 , 78 ]. Another recent systematic review also found that vitamin D and calcium supplements had no beneficial effects on fractures, falls, or bone mineral density [ 79 , 80 ]. The mean age of all participants was Most participants were vitamin D sufficient; at baseline, only 2. Vitamin D supplementation did not lower the risk of total fractures, hip fractures, or nonvertebral fractures as compared with placebo. No substantial between-group differences in fracture incidence were found by race, ethnic group, BMI, age, baseline 25 OH D levels, or whether participants took supplemental calcium, were at high fracture risk, or had a history of fragility fractures. Bone mineral density, bone mass, and fracture risk are correlated with serum 25 OH D levels in White Americans and Mexican Americans, but not in Black Americans [ 14 , 83 ]. Factors such as adiposity, skin pigmentation, vitamin D binding protein polymorphisms, and genetics contribute to differences in 25 OH D levels between Black and White Americans. One clinical trial randomized Black women age 60 years and older mean age The results showed no association between 25 OH D levels or vitamin D dose and the risk of falling in the participants who completed the study. In fact, Black Americans might have a greater risk than White Americans of falls and fractures with daily vitamin D intakes of 50 mcg 2, IU or more [ 14 ]. Studies examining the effects of supplemental vitamin D on muscle strength and on rate of decline in muscle function have had inconsistent results [ 55 ]. One recent clinical trial, for example, randomized 78 frail and near-frail adults age 65 years and older to receive 20 mcg IU vitamin D 3 , 10 mcg 25 OH D, or placebo daily for 6 months. The groups showed no significant differences in measures of muscle strength or performance [ 85 ]. All adults should consume recommended amounts of vitamin D and calcium from foods and supplements if needed. Older women and men should consult their health care providers about their needs for both nutrients as part of an overall plan to maintain bone health and to prevent or treat osteoporosis. Laboratory and animal studies suggest that vitamin D might inhibit carcinogenesis and slow tumor progression by, for example, promoting cell differentiation and inhibiting metastasis. Vitamin D might also have anti-inflammatory, immunomodulatory, proapoptotic, and antiangiogenic effects [ 1 , 87 ]. Observational studies and clinical trials provide mixed evidence on whether vitamin D intakes or serum levels affect cancer incidence, progression, or mortality risk. Some observational studies show associations between low serum levels of 25 OH D and increased risks of cancer incidence and death. In a meta-analysis of 16 prospective cohort studies in a total of , participants who had 8, diagnoses of cancer, 5, participants died from cancer [ 88 ]. Importantly, not all observational studies found higher vitamin D status to be beneficial, and the studies varied considerably in study populations, baseline comorbidities, and measurement of vitamin D levels. Clinical trial evidence provides some support for the observational findings. The study reports included 3—10 years of follow-up data. The study included 25, men age 50 years and older and women age 55 years and older who had no history of cancer, and most had adequate serum 25 OH D levels at baseline. Rates of breast, prostate, and colorectal cancer did not differ significantly between the vitamin D and placebo groups. However, normal-weight participants had greater reductions in cancer incidence and mortality rates than those with overweight or obesity. A few studies have examined the effect of vitamin D supplementation on specific cancers. Below are brief descriptions of studies of vitamin D and its association with, or effect on, breast, colorectal, lung, pancreatic, and prostate cancers. Some observational studies support an inverse association between 25 OH D levels and breast cancer risk and mortality, but others do not [ ]. The Women's Health Initiative clinical trial randomized 36, postmenopausal women to receive IU vitamin D 3 plus 1, mg calcium daily or a placebo for a mean of 7 years [ 98 ]. The vitamin D 3 and calcium supplements did not reduce breast cancer incidence, and 25 OH D levels at the start of the study were not associated with breast cancer risk [ 99 ]. In the UK, cows' milk is generally not a good source of vitamin D because it is not fortified, as it is in some other countries. Children from the age of 1 year and adults need 10 micrograms of vitamin D a day. This includes pregnant and breastfeeding women, and people at risk of vitamin D deficiency. Babies up to the age of 1 year need 8. A microgram is 1, times smaller than a milligram mg. The word microgram is sometimes written with the Greek symbol μ followed by the letter g μg. Sometimes the amount of vitamin D is expressed as International Units IU. So 10 micrograms of vitamin D is equal to IU. During the autumn and winter, you need to get vitamin D from your diet because the sun is not strong enough for the body to make vitamin D. But since it's difficult for people to get enough vitamin D from food alone, everyone including pregnant and breastfeeding women should consider taking a daily supplement containing 10 micrograms of vitamin D during the autumn and winter. Some people will not make enough vitamin D from sunlight because they have very little or no sunshine exposure. The Department of Health and Social Care recommends that adults and children over 4 take a daily supplement containing 10 micrograms of vitamin D throughout the year if they:. If you have dark skin — for example you have an African, African-Caribbean or south Asian background — you may also not make enough vitamin D from sunlight. You should consider taking a daily supplement containing 10 micrograms of vitamin D throughout the year. The Department of Health and Social Care recommends that babies from birth to 1 year of age should have a daily supplement containing 8. Studies aren't conclusive, but vitamin D could be beneficial by offering type 1 and type 2 diabetes prevention. One study found that six months of vitamin D supplementation increased insulin sensitivity in people with diabetes or at high risk of the disease. Vitamin D may be helpful for individuals with irritable bowel syndrome IBS , as people with IBS may have vitamin D deficiencies. Some researchers found in one review that, across six studies with data from participants, there was a link between vitamin D supplementation and less severe IBS symptoms. They suggested the reduction in severity might be due to the anti-inflammatory effects of vitamin D. However, the researchers noted that the results could not be generalized to all people with IBS. They also said that the relationship between vitamin D supplementation and this change in IBS symptoms is complex and not completely understood. The sun can brighten up your mood, and so can vitamin D: Researchers found a link between depression and vitamin D deficiency. They acknowledged that more research is needed to define the exact workings of it—such as if low vitamin D levels are a cause or effect of depression. However, the authors also recommended vitamin D deficiency screenings for individuals with depression and vitamin D deficiency. They noted that these screenings are a cost-effective and simple way to aid in improving outcomes related to depression. Getting enough vitamin D could reduce the likelihood of developing multiple sclerosis MS. MS is an autoimmune disorder resulting from inflammation-induced nerve damage within the central nervous system CNS. Lower vitamin D levels have been linked to an increased risk of multiple sclerosis. However, a higher vitamin D intake may result in lower disease activity indicated on an MRI and a lower relapse risk. Consuming enough vitamin D can be beneficial during pregnancy. Vitamin D deficiency has been linked to an increased risk of developing complications such as:. Vitamin D supporting bone health is especially important for children. If they are lacking in vitamin D intake, they can develop rickets. Rickets is a disease that softens bones and particularly affects children up to two years old. Babies should get international units IU of vitamin D daily until 12 months old. After that time, they need IU. The daily vitamin D recommendation for adults is as follows:. There are a few reasons why a person may be deficient in vitamin D. These reasons range from not getting enough of the vitamin from foods you eat to taking medicines that don't allow vitamin D conversion or absorption in the body. Not consuming enough vitamin D can result in:. Though vitamin D is good for you, it's possible to have too much vitamin D. Excessive vitamin D intake is called vitamin D toxicity. Symptoms of this toxicity include:. If the level of vitamin D in your body is too high, it can lead to kidney damage. Also, vitamin D toxicity typically comes from using supplements too much, not from sun exposure. If you find out you are deficient or lacking in vitamin D intake, there are a few key ways you can up your daily dosage, including:. Dietary supplements may or may not be suitable for you. Supplement effects vary individually, based on type, dosage, frequency of use, and medication interactions. Talk to a healthcare provider or pharmacist before you begin taking supplements. The sunshine vitamin, vitamin D, is beneficial in many ways. Some of its potential benefits include lowering the risk of MS, helping prevent rickets or diabetes, and strengthening bones and muscles. You can get vitamin D from foods, sunshine, and supplements. Getting enough vitamin D is important, as too much or too little can have side effects like nausea, bone weakness, and poor appetite. Office of Dietary Supplements. Vitamin D - fact sheet for healthcare professionals. |
| Vitamin D | The Nutrition Source | Harvard T.H. Chan School of Public Health | In children, vitamin D deficiency causes rickets , a disease in which the bones become soft, weak, deformed, and painful. In teens and adults, vitamin D deficiency causes osteomalacia , a disorder that causes bone pain and muscle weakness. Scientists are studying vitamin D to better understand how it affects health. Here are several examples of what this research has shown. Long-term shortages of vitamin D and calcium cause your bones to become fragile and break more easily. This condition is called osteoporosis. Millions of older women and men have osteoporosis or are at risk of developing this condition. Muscles are also important for healthy bones because they help maintain balance and prevent falls. A shortage of vitamin D may lead to weak, painful muscles. Getting recommended amounts of vitamin D and calcium from foods and supplements, if needed will help maintain healthy bones and prevent osteoporosis. Vitamin D does not seem to reduce the risk of developing cancer of the breast, colon , rectum, or lung. It is not clear whether vitamin D affects the risk of prostate cancer or chance of surviving this cancer. Very high blood levels of vitamin D may even increase the risk of pancreatic cancer. Clinical trials suggest that while vitamin D supplements with or without calcium may not affect your risk of getting cancer, they might slightly reduce your risk of dying from this disease. More research is needed to better understand the role that vitamin D plays in cancer prevention and cancer-related death. Vitamin D is important for a healthy heart and blood vessels and for normal blood pressure. Some studies show that vitamin D supplements might help reduce blood cholesterol levels and high blood pressure —two of the main risk factors for heart disease. Other studies show no benefits. If you are overweight or have obesity, taking vitamin D at doses above 20 mcg IU per day plus calcium might actually raise your blood pressure. Overall, clinical trials find that vitamin D supplements do not reduce the risk of developing heart disease or dying from it, even if you have low blood levels of the vitamin. Vitamin D is needed for your brain to function properly. Some studies have found links between low blood levels of vitamin D and an increased risk of depression. However, clinical trials show that taking vitamin D supplements does not prevent or ease symptoms of depression. People who live near the equator have more sun exposure and higher vitamin D levels. They also rarely develop multiple sclerosis MS , a disease that affects the nerves that carry messages from the brain to the rest of the body. Many studies find a link between low blood vitamin D levels and the risk of developing MS. However, scientists have not actually studied whether vitamin D supplements can prevent MS. In people who have MS, clinical trials show that taking vitamin D supplements does not keep symptoms from getting worse or coming back. One reason is that sun exposure affects vitamin D status, so serum 25 OH D levels are usually higher than would be predicted on the basis of vitamin D dietary intakes alone [ 1 ]. Another reason is that animal foods contain some 25 OH D. This form of vitamin D is not included in intake surveys and is considerably more potent than vitamins D 2 or D 3 at raising serum 25 OH D levels [ 42 ]. An analysis of NHANES — data on serum 25 OH D levels found that most people in the United States age 1 year and older had sufficient vitamin D intakes according to the FNB thresholds [ 43 ]. Proportions at risk of deficiency were lowest among children age 1—5 years 0. Rates of deficiency varied by race and ethnicity: Again, the pattern was similar for the risk of inadequacy. Vitamin D status in the United States remained stable in the decade between — and — People can develop vitamin D deficiency when usual intakes are lower over time than recommended levels, exposure to sunlight is limited, the kidneys cannot convert 25 OH D to its active form, or absorption of vitamin D from the digestive tract is inadequate. Diets low in vitamin D are more common in people who have milk allergy or lactose intolerance and those who consume an ovo-vegetarian or vegan diet [ 1 ]. In children, vitamin D deficiency is manifested as rickets, a disease characterized by a failure of bone tissue to become properly mineralized, resulting in soft bones and skeletal deformities [ 44 ]. In addition to bone deformities and pain, severe rickets can cause failure to thrive, developmental delay, hypocalcemic seizures, tetanic spasms, cardiomyopathy, and dental abnormalities [ 45 , 46 ]. Prolonged exclusive breastfeeding without vitamin D supplementation can cause rickets in infants, and, in the United States, rickets is most common among breastfed Black infants and children [ 47 ]. In one Minnesota county, the incidence rate of rickets in children younger than 3 years in the decade beginning in was Rickets occurred mainly in Black children who were breastfed longer, were born with low birthweight, weighed less, and were shorter than other children. The incidence rate of rickets in the infants and children younger than 7 seen by 2, pediatricians throughout Canada was 2. The fortification of milk a good source of calcium and other staples, such as breakfast cereals and margarine, with vitamin D beginning in the s along with the use of cod liver oil made rickets rare in the United States [ 28 , 50 ]. However, the incidence of rickets is increasing globally, even in the United States and Europe, especially among immigrants from African, Middle-Eastern, and Asian countries [ 51 ]. Possible explanations for this increase include genetic differences in vitamin D metabolism, dietary preferences, and behaviors that lead to less sun exposure [ 45 , 46 ]. In adults and adolescents, vitamin D deficiency can lead to osteomalacia, in which existing bone is incompletely or defectively mineralized during the remodeling process, resulting in weak bones [ 46 ]. Signs and symptoms of osteomalacia are similar to those of rickets and include bone deformities and pain, hypocalcemic seizures, tetanic spasms, and dental abnormalities [ 45 ]. Screening for vitamin D status is becoming a more common part of the routine laboratory bloodwork ordered by primary-care physicians, irrespective of any indications for this practice [ 6 , ]. No studies have examined whether such screening for vitamin D deficiency results in improved health outcomes [ 55 ]. Preventive Services Task Force USPSTF found insufficient evidence to assess the benefits and harms of screening for vitamin D deficiency in asymptomatic adults [ 6 ]. It added that no national professional organization recommends population screening for vitamin D deficiency. Obtaining sufficient vitamin D from natural nonfortified food sources alone is difficult. For many people, consuming vitamin D-fortified foods and exposing themselves to some sunlight are essential for maintaining a healthy vitamin D status. However, some groups might need dietary supplements to meet their vitamin D requirements. The following groups are among those most likely to have inadequate vitamin D status. Consumption of human milk alone does not ordinarily enable infants to meet vitamin D requirements, because it provides less than 0. Although UVB exposure can produce vitamin D in infants, the American Academy of Pediatrics AAP advises parents to keep infants younger than 6 months out of direct sunlight, dress them in protective clothing and hats, and apply sunscreen on small areas of exposed skin when sun exposure is unavoidable [ 59 ]. An analysis of NHANES — data found that only Older adults are at increased risk of developing vitamin D insufficiency, partly because the skin's ability to synthesize vitamin D declines with age [ 1 , 61 ]. In addition, older adults are likely to spend more time than younger people indoors, and they might have inadequate dietary intakes of the vitamin [ 1 ]. Homebound individuals; people who wear long robes, dresses, or head coverings for religious reasons; and people with occupations that limit sun exposure are among the groups that are unlikely to obtain adequate amounts of vitamin D from sunlight [ 62 ]. The use of sunscreen also limits vitamin D synthesis from sunlight. However, because the extent and frequency of sunscreen use are unknown, the role that sunscreen may play in reducing vitamin D synthesis is unclear [ 1 ]. Black Americans, for example, typically have lower serum 25 OH D levels than White Americans. However, whether these lower levels in persons with dark skin have significant health consequences is not clear [ 14 ]. Those of African American ancestry, for example, have lower rates of bone fracture and osteoporosis than do Whites see the section below on bone health and osteoporosis. In addition to having an increased risk of vitamin D deficiency, people with these conditions might not eat certain foods, such as dairy products many of which are fortified with vitamin D , or eat only small amounts of these foods. Individuals who have difficulty absorbing dietary fat might therefore require vitamin D supplementation [ 63 ]. Individuals with a body mass index BMI of 30 or more have lower serum 25 OH D levels than individuals without obesity. However, greater amounts of subcutaneous fat sequester more of the vitamin [ 1 ]. People with obesity might need greater intakes of vitamin D to achieve 25 OH D levels similar to those of people with normal weight [ 1 , 64 , 65 ]. Individuals with obesity who have undergone gastric bypass surgery can also become vitamin D deficient. In this procedure, part of the upper small intestine, where vitamin D is absorbed, is bypassed, and vitamin D that is mobilized into the bloodstream from fat stores might not raise 25 OH D to adequate levels over time [ 66 , 67 ]. Various expert groups—including the American Association of Metabolic and Bariatric Surgery, The Obesity Society, and the British Obesity and Metabolic Surgery Society—have developed guidelines on vitamin D screening, monitoring, and replacement before and after bariatric surgery [ 66 , 68 ]. The FNB committee that established DRIs for vitamin D found that the evidence was inadequate or too contradictory to conclude that the vitamin had any effect on a long list of potential health outcomes e. Similarly, in a review of data from nearly studies published between and , the Agency for Healthcare Research and Quality concluded that no relationship could be firmly established between vitamin D and health outcomes other than bone health [ 69 ]. However, because research has been conducted on vitamin D and numerous health outcomes, this section focuses on seven diseases, conditions, and interventions in which vitamin D might be involved: bone health and osteoporosis, cancer, cardiovascular disease CVD , depression, multiple sclerosis MS , type 2 diabetes, and weight loss. Most of the studies described in this section measured serum 25 OH D levels using various methods that were not standardized by comparing them to the best methods. Use of unstandardized 25 OH D measures can raise questions about the accuracy of the results and about the validity of conclusions drawn from studies that use such measures and, especially, from meta-analyses that pool data from many studies that use different unstandardized measures [ 5 , 9 , 70 ]. More information about assay standardization is available from the Vitamin D Standardization Program webpage. Bone is constantly being remodeled. However, as people age—and particularly in women during menopause—bone breakdown rates overtake rates of bone building. Over time, bone density can decline, and osteoporosis can eventually develop [ 71 ]. More than 53 million adults in the United States have or are at risk of developing osteoporosis, which is characterized by low bone mass and structural deterioration of bone tissue that increases bone fragility and the risk of bone fractures [ 72 ]. About 2. Osteoporosis is most often associated with inadequate calcium intakes, but insufficient vitamin D intakes contribute to osteoporosis by reducing calcium absorption [ 1 ]. Bone health also depends on support from the surrounding muscles to assist with balance and postural sway and thereby reduce the risk of falling. Vitamin D is also needed for the normal development and growth of muscle fibers. In addition, inadequate vitamin D levels can adversely affect muscle strength and lead to muscle weakness and pain myopathy [ 1 ]. Most trials of the effects of vitamin D supplements on bone health also included calcium supplements, so isolating the effects of each nutrient is difficult. In addition, studies provided different amounts of nutrients and used different dosing schedules. Among postmenopausal women and older men, many clinical trials have shown that supplements of both vitamin D and calcium result in small increases in bone mineral density throughout the skeleton [ 1 , 74 ]. They also help reduce fracture rates in institutionalized older people. However, the evidence on the impact of vitamin D and calcium supplements on fractures in community-dwelling individuals is inconsistent. It concluded that the current evidence was insufficient to evaluate the benefits and harms of supplementation to prevent fractures. In addition, the USPSTF recommended against supplementation with 10 mcg IU or less of vitamin D and 1, mg or less of calcium to prevent fractures in this population, but it could not determine the balance of benefits and harms from higher doses. The USPSTF also reviewed the seven published studies on the effects of vitamin D supplementation two of them also included calcium supplementation on the risk of falls in community-dwelling adults age 65 years or older who did not have osteoporosis or vitamin D deficiency. It concluded with moderate certainty that vitamin D supplementation does not reduce the numbers of falls or injuries, such as fractures, resulting from falls [ 77 , 78 ]. Another recent systematic review also found that vitamin D and calcium supplements had no beneficial effects on fractures, falls, or bone mineral density [ 79 , 80 ]. The mean age of all participants was Most participants were vitamin D sufficient; at baseline, only 2. Vitamin D supplementation did not lower the risk of total fractures, hip fractures, or nonvertebral fractures as compared with placebo. No substantial between-group differences in fracture incidence were found by race, ethnic group, BMI, age, baseline 25 OH D levels, or whether participants took supplemental calcium, were at high fracture risk, or had a history of fragility fractures. Bone mineral density, bone mass, and fracture risk are correlated with serum 25 OH D levels in White Americans and Mexican Americans, but not in Black Americans [ 14 , 83 ]. Factors such as adiposity, skin pigmentation, vitamin D binding protein polymorphisms, and genetics contribute to differences in 25 OH D levels between Black and White Americans. One clinical trial randomized Black women age 60 years and older mean age The results showed no association between 25 OH D levels or vitamin D dose and the risk of falling in the participants who completed the study. In fact, Black Americans might have a greater risk than White Americans of falls and fractures with daily vitamin D intakes of 50 mcg 2, IU or more [ 14 ]. Studies examining the effects of supplemental vitamin D on muscle strength and on rate of decline in muscle function have had inconsistent results [ 55 ]. One recent clinical trial, for example, randomized 78 frail and near-frail adults age 65 years and older to receive 20 mcg IU vitamin D 3 , 10 mcg 25 OH D, or placebo daily for 6 months. The groups showed no significant differences in measures of muscle strength or performance [ 85 ]. All adults should consume recommended amounts of vitamin D and calcium from foods and supplements if needed. Older women and men should consult their health care providers about their needs for both nutrients as part of an overall plan to maintain bone health and to prevent or treat osteoporosis. Laboratory and animal studies suggest that vitamin D might inhibit carcinogenesis and slow tumor progression by, for example, promoting cell differentiation and inhibiting metastasis. Vitamin D might also have anti-inflammatory, immunomodulatory, proapoptotic, and antiangiogenic effects [ 1 , 87 ]. Observational studies and clinical trials provide mixed evidence on whether vitamin D intakes or serum levels affect cancer incidence, progression, or mortality risk. Some observational studies show associations between low serum levels of 25 OH D and increased risks of cancer incidence and death. In a meta-analysis of 16 prospective cohort studies in a total of , participants who had 8, diagnoses of cancer, 5, participants died from cancer [ 88 ]. Importantly, not all observational studies found higher vitamin D status to be beneficial, and the studies varied considerably in study populations, baseline comorbidities, and measurement of vitamin D levels. Clinical trial evidence provides some support for the observational findings. The study reports included 3—10 years of follow-up data. The study included 25, men age 50 years and older and women age 55 years and older who had no history of cancer, and most had adequate serum 25 OH D levels at baseline. Rates of breast, prostate, and colorectal cancer did not differ significantly between the vitamin D and placebo groups. However, normal-weight participants had greater reductions in cancer incidence and mortality rates than those with overweight or obesity. A few studies have examined the effect of vitamin D supplementation on specific cancers. Below are brief descriptions of studies of vitamin D and its association with, or effect on, breast, colorectal, lung, pancreatic, and prostate cancers. Some observational studies support an inverse association between 25 OH D levels and breast cancer risk and mortality, but others do not [ ]. The Women's Health Initiative clinical trial randomized 36, postmenopausal women to receive IU vitamin D 3 plus 1, mg calcium daily or a placebo for a mean of 7 years [ 98 ]. The vitamin D 3 and calcium supplements did not reduce breast cancer incidence, and 25 OH D levels at the start of the study were not associated with breast cancer risk [ 99 ]. In a subsequent investigation for 4. A large case-control study included 5, individuals who developed colorectal cancer and whose 25 OH D levels were assessed a median of 5. Levels of 75 to less than The association was substantially stronger in women. In the Women's Health Initiative clinical trial described above , vitamin D 3 and calcium supplements had no effect on rates of colorectal cancer. Another study included 2, healthy individuals age 45 to 75 years who had had one or more serrated polyps precursor lesions to colorectal cancer that had been removed [ ]. Indian Journal of Endocrinology and Metabolism. March—April Mayo Clinic. February 25, Oncogenic Osteomalacia, Pearls From an Elusive Tumor: A Case From the Endocrine Teaching Clinics. August 11, August 21, Bolland M, Grey A, Avenell A. Effects of Vitamin D Supplementation on Musculoskeletal Health: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis. November Seasonal Affective Disorder. National Institute of Mental Health. Cowen PJ, Browning M. What Has Serotonin to Do With Depression? World Psychiatry. June Mikola T, Marx W, Lane MM, et al. The Effect of Vitamin D Supplementation on Depressive Symptoms in Adults: A Systematic Review and Meta-Analysis of Randomized, Controlled Trials. Critical Reviews in Food Science and Nutrition. Okereke OI, Reynolds CF, Mischoulon D, et al. Effect of Long-Term Vitamin D3 Supplementation vs Placebo on Risk of Depression or Clinically Relevant Depressive Symptoms and on Change in Mood Scores. August Marcinkowska E, Brown G. Editorial: Vitamin D and COVID New Mechanistic and Therapeutic Insights. Frontiers in Pharmacology. March Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D Supplementation to Prevent Acute Respiratory Tract Infections: Systematic Review and Meta-Analysis of Individual Participant Data. The BMJ. February Bolland MJ, Avenell A. Do Vitamin D Supplements Help Prevent Respiratory Tract Infections? Mheid IA, Patel RS, Tangpricha V, Quyyumi AA. Vitamin D and Cardiovascular Disease: Is the Evidence Solid? European Heart Journal. December Virtanen JK, Nurmi T, Aro A, et al. Vitamin D Supplementation and Prevention of Cardiovascular Disease and Cancer in the Finnish Vitamin D Trial: A Randomized, Controlled Trial. American Journal of Clinical Nutrition. May Vitamin, Mineral, and Multivitamin Supplementation to Prevent Cardiovascular Disease and Cancer: U. Preventive Services Task Force Recommendation Statement. Pittas AG, Dawson-Hughes B, Sheehan P, et al. Vitamin D Supplementation and Prevention of Type 2 Diabetes. Manson JE, Cook NR, Lee I, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. January Mitri J, Pittas A. Vitamin D and Diabetes. Endocrinology and Metabolism Clinics of North America. Kawahara T, Suzuki G, Mizuno S, et al. Effect of Active Vitamin D Treatment on Development of Type 2 Diabetes: DPVD Randomised, Controlled Trial in Japanese Population. Garland CF, Garland FC, Gorham ED, et al. The Role of Vitamin D in Cancer Prevention. American Journal of Public Health. Navale S, Mulugeta A, Zhou A, et al. Vitamin D and Brain Health: An Observational and Mendelian Randomization Study. The American Journal of Clinical Nutrition. Soni M, Kos K, Lang I, et al. Vitamin D and Cognitive Function. Scandinavian Journal of Clinical and Laboratory Investigation. Iacopetta K, Collins-Praino L, Buisman-Pijlman F, et al. |
Ich denke, dass Sie sich irren. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Ich tue Abbitte, dass ich mich einmische, aber ich biete an, mit anderem Weg zu gehen.