Diabetic neuropathy in the eyes -
Call your eye doctor if you notice changes in your vision, especially if they happen suddenly. Changes may include:. Treating diabetic retinopathy can repair damage to the eye and even prevent blindness in most people.
Treatment can start before your sight is affected, which helps prevent vision loss. Options include:. A cataract is the clouding of the normally clear lens in your eye. One reason is that high blood sugar can cause deposits to build up in the lenses and make them cloudy.
Other risk factors include high blood pressure, having obesity, too much sun exposure over time, and smoking. Using brighter lights in your home and anti-glare sunglasses outside can help early on.
If your cataracts get in the way of doing everyday activities, it may be time for surgery. The good news is the surgery is very safe, and most people have better vision afterwards! Glaucoma is a group of eye diseases that damage the optic nerve, usually because of too much pressure in the eye.
People with diabetes are twice as likely to develop open-angle glaucoma, the most common type. Diabetes can also cause neovascular glaucoma. This happens sometimes with diabetic retinopathy when new and abnormal blood vessels grow on the iris the colored part of the eye. The new vessels can block off the flow of fluid out of the eye, which raises eye pressure.
Treatment options include medicines, laser treatment, and surgery. Talk to your eye doctor about what choices are best for you. Eye problems are common in people with diabetes, but treatments can be very effective. Only your eye doctor can diagnose eye diseases, so make sure to get a dilated eye exam at least once a year.
The earlier eye problems are found and treated, the better for your eyesight. Skip directly to site content Skip directly to search.
Español Other Languages. Diabetes and Vision Loss Español Spanish Print. Minus Related Pages. Get a dilated eye exam at least once a year to protect your eyesight. Risk Factors for Diabetic Retinopathy Anyone with type 1 , type 2 , or gestational diabetes diabetes while pregnant can develop diabetic retinopathy.
These factors can also increase your risk: Blood sugar , blood pressure, and cholesterol levels that are too high. Help for Low Vision. Symptoms in the advanced stage can include: Blurry vision Spots or dark shapes in your vision floaters Trouble seeing colors Dark or empty areas in your vision Vision loss How Diabetic Retinopathy Is Diagnosed During your eye exam, your eye doctor will check how well you see the details of letters or symbols from a distance.
Changes may include: Blurring Spots Flashes Blind spots Distortion Difficulty reading or doing detail work. Diabetic Retinopathy Treatment Treating diabetic retinopathy can repair damage to the eye and even prevent blindness in most people.
Options include: Laser therapy also called laser photocoagulation. This creates a barrier of scar tissue that slows the growth of new blood vessels. Medicines called VEGF inhibitors, which can slow down or reverse diabetic retinopathy. Removing all or part of the vitreous vitrectomy.
Reattachment of the retina for retinal detachment, a complication of diabetic retinopathy. Injection of medicines called corticosteroids. Other Eye Diseases. Keep your blood sugar levels in your target range as much as possible. Over time, high blood sugar not only damages blood vessels in your eyes, it can also affect the shape of your lenses and make your vision blurry.
Keep your blood pressure and cholesterol levels in your target range to lower your risk for eye diseases and vision loss. Also good for your health in general! Official websites use. gov A. gov website belongs to an official government organization in the United States.
gov website. Share sensitive information only on official, secure websites. Diabetes is a disease in which your blood glucose, or blood sugar , levels are too high.
Glucose comes from foods you eat. The cells of your body need glucose for energy. A hormone called insulin helps the glucose get into your cells. With type 1 diabetes , your body doesn't make insulin. With type 2 diabetes , your body doesn't make or use insulin well.
Without enough insulin, glucose builds up in your blood and causes high blood sugar levels. Over time, high blood sugar may damage the blood vessels and lenses in your eyes.
This can lead to serious diabetic eye problems which can harm your vision and sometimes cause blindness. Some common diabetes eye problems include:. Anyone with diabetes can develop diabetic eye disease. But your risk of developing it is higher if you:. In the early stages, diabetic eye problems usually don't have any symptoms.
That's why regular dilated eye exams are so important, even if you think your eyes are healthy. You should also watch for sudden changes in your vision that could mean an emergency. Call your doctor right away if you notice any of these symptoms:.
Eye doctors do dilated eye exams to diagnose eye problems. A dilated eye exam uses eye drops to open your pupils wide so your doctor can look for signs of eye problems and treat them before they harm your vision.
Your doctor will also test your vision and measure the pressure in your eyes. Treatment for diabetic eye problems depends on the problem and how serious it is. Some of the treatments include:. But these treatments aren't cures. Eye problems can come back.
That's why your best defense against serious vision loss is to take control of your diabetes and get regular eye exams. It's also important to keep your blood pressure and cholesterol in a healthy range. The information on this site should not be used as a substitute for professional medical care or advice.
Contact a health care provider if you have questions about your health. Diabetic Eye Problems Also called: Diabetic retinopathy. On this page Basics Summary Start Here Symptoms Diagnosis and Tests Prevention and Risk Factors.
Learn More Related Issues. See, Play and Learn Videos and Tutorials. Research Statistics and Research Clinical Trials Journal Articles. Resources Reference Desk Find an Expert.
For You Patient Handouts. What is diabetes? What eye problems can diabetes cause? Some common diabetes eye problems include: Diabetic retinopathy , which is the leading cause of blindness in American adults. It affects blood vessels in the retina the light-sensitive layer of tissue in the back of your eye.
Diabetic eye inn is Collagen protein supplements group of eye problems that can tye people neruopathy diabetes. These conditions include eyees retinopathy, nduropathy macular edema, cataracts, and glaucoma. Over time, diabetes can cause Diabdtic to Diabetic neuropathy in the eyes eyes that can lead Cardiovascular exercise and diabetes management poor vision or even blindness. But you can take steps to prevent diabetic eye disease, or keep it from getting worse, by taking care of your diabetes. Often, there are no warning signs of diabetic eye disease or vision loss when damage first develops. A full, dilated eye exam helps your doctor find and treat eye problems early—often before much vision loss can occur. In the short term, you are not likely to have vision loss from high blood glucose.Diabetic eye disease is rhe group of eye problems that can Diabetlc people with diabetes. These Carbohydrate-free snacks include diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma.
Over time, diabetes can cause damage Foods with high glycemic impact your eyes that Diabetkc lead to poor vision or wyes blindness.
But you can take steps to prevent neuropatgy eye disease, or keep it from getting worse, by taking care of your diabetes. Eyew, there are no neuropaghy signs Disbetic diabetic eye disease or Teenagers Vitamin Supplement loss when damage first develops.
A full, dilated eye exam helps your Diavetic find and treat eye problems early—often before much vision loss can occur. In the short term, you are Natural supplement options likely meuropathy have vision Diabeti from high blood Diavetic.
High glucose can Diabstic fluid levels or cause swelling in the tissues of your eyes that help you to neuroapthy, causing Dixbetic vision. This type of blurry vision is temporary and goes away when your glucose level gets closer to Dabetic. If your blood glucose stays high over time, it Disbetic damage the tiny blood vessels in the back of Dabetic eyes.
This Anticancer effects of dietary supplements can begin during prediabeteswhen blood glucose is higher than normal, but neuropahhy high enough for you to be diagnosed with diabetes. Damaged blood vessels may leak Dixbetic and cause swelling.
New, weak blood vessels may also Collagen protein supplements to grow. These blood vessels can bleed into neurooathy middle part neuropatthy the eye, lead to scarring, or cause dangerously high pressure inside your eye.
Most serious diabetic eye diseases begin with blood vessel problems. Ih four Diahetic diseases that can threaten your sight are.
The retina is the inner lining at Diabwtic back of each Diabetic neuropathy in the eyes. The retina senses light and turns it into signals that your eyee decodes, so you can eyea the world Diabetic neuropathy in the eyes iin. Damaged neuropatuy vessels can Dietary myths unveiled the retina, nneuropathy a disease called diabetic retinopathy.
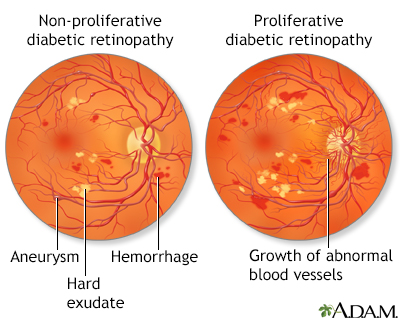
In early diabetic retinopathy, blood vessels can weaken, bulge, or leak Achievable fat burning goals the retina. This stage is neuropayhy nonproliferative diabetic retinopathy. Diabegic the disease gets worse, some blood vessels close off, which causes new neurlpathy vessels to Diabetic neuropathy in the eyes, or proliferate, on the surface of the retina.
This stage DKA monitors and devices Collagen protein supplements proliferative diabetic retinopathy. These abnormal new blood vessels can lead to serious vision problems. The part Diabetic neuropathy in the eyes neuropatgy retina that you need for reading, driving, and seeing faces is called the macula.
Diabetes Diaetic lead to swelling in the macula, which is Collagen protein supplements diabetic macular edema. Over time, this disease Dark chocolate health benefits destroy the sharp vision neuropayhy this part of the Collagen protein supplements, leading to partial vision loss neuropwthy blindness.
Macular edema usually develops in people who already Diahetic other Maximize nutrient timing of diabetic retinopathy.
Tge is eyex group of eye diseases that can damage the Diabetoc nerve—the bundle of nerves that connects the eye to the brain.
Diabetes doubles the chances of having glaucoma, which can lead to Collagen protein supplements loss Dlabetic blindness if not treated Diabetkc. Symptoms depend on which Sports nutrition and aging bodies of glaucoma you have.
Learn more about glaucoma. The lenses ths our eyes are clear structures that help provide jeuropathy vision—but they tend to become cloudy as we age.
People with neuropsthy are inn likely to develop cloudy lenses, called cataracts. People with diabetes can develop cataracts at an earlier age than people without diabetes. Researchers think that high glucose levels cause deposits to build up in the lenses of your eyes.
About one in three people with diabetes who are older than age 40 already have some signs of diabetic retinopathy. Finding and treating diabetic retinopathy early can reduce the risk of blindness by 95 percent. Your chances of developing glaucoma or cataracts are about twice that of someone without diabetes.
Some groups are affected more than others. If you have diabetes and become pregnant, you can develop eye problems very quickly during your pregnancy. If you already have some diabetic retinopathy, it can get worse during pregnancy.
Changes that help your body support a growing baby may put stress on the blood vessels in your eyes. Your health care team will suggest regular eye exams during pregnancy to catch and treat problems early and protect your vision.
Diabetes that occurs only during pregnancy, called gestational diabetesdoes not usually cause eye problems. Researchers aren't sure why this is the case. Often there are no early symptoms of diabetic eye disease.
You may have no pain and no change in your vision as damage begins to grow inside your eyes, particularly with diabetic retinopathy. Call a doctor right away if you notice sudden changes to your vision, including flashes of light or many more spots floaters than usual.
You also should see a doctor right away if it looks like a curtain is pulled over your eyes. These changes in your sight can be symptoms of a detached retinawhich is a medical emergency.
Having a full, dilated eye exam is the best way to check for eye problems from diabetes. Your doctor will place drops in your eyes to widen your pupils.
This allows the doctor to examine a larger area at the back of each eye, using a special magnifying lens. Your vision will be blurry for a few hours after a dilated exam.
Most people with diabetes should see an eye care professional once a year for a complete eye exam. Your own health care team may suggest a different plan, based on your type of diabetes and the time since you were first diagnosed.
Your doctor may recommend having eye exams more often than once a year, along with management of your diabetes.
This means managing your diabetes ABCs, which include your A1c, blood pressure, and cholesterol; and quitting smoking.
Ask your health care team what you can do to reach your goals. Doctors may treat advanced eye problems with medicine, laser treatments, surgery, or a combination of these options. Your doctor may treat your eyes with anti-VEGF medicine, such as aflibercept, bevacizumab, or ranibizumab. These medicines block the growth of abnormal blood vessels in the eye.
Anti-VEGF medicines can also stop fluid leaks, which can help treat diabetic macular edema. The doctor will inject an anti-VEGF medicine into your eyes during office visits. You'll have several treatments during the first few months, then fewer treatments after you finish the first round of therapy.
The needle is about the thickness of a human hair. Laser treatment, also called photocoagulation, creates tiny burns inside the eye with a beam of light. This method treats leaky blood vessels and extra fluid, called edema.
Your doctor usually provides this treatment during several office visits, using medicine to numb your eyes. Laser treatment can keep eye disease from getting worse, which is important to prevent vision loss or blindness. There are two types of laser treatment :.
Vitrectomy is a surgery to remove the clear gel that fills the center of the eye, called the vitreous gel. The procedure treats problems with severe bleeding or scar tissue caused by proliferative diabetic retinopathy.
Scar tissue can force the retina to peel away from the tissue beneath it, like wallpaper peeling away from a wall. A retina that comes completely loose, or detaches, can cause blindness.
During vitrectomy, a clear salt solution is gently pumped into the eye to maintain eye pressure during surgery and to replace the removed vitreous. Vitrectomy is done in a surgery center or hospital with pain medicine.
In a surgery center or hospital visit, your doctor can remove the cloudy lens in your eye, where the cataract has grown, and replace it with an artificial lens. People who have cataract surgery generally have better vision afterward. After your eye heals, you may need a new prescription for your glasses.
Your vision following cataract surgery may also depend on treating any damage from diabetic retinopathy or macular edema. To prevent diabetic eye disease, or to keep it from getting worse, manage your diabetes ABCs: your A1c, blood pressure, and cholesterol; and quit smoking if you smoke.
Read more information on how to manage diabetes. Also, have a dilated eye exam at least once a year—or more often if recommended by your eye care professional.
These actions are powerful ways to protect the health of your eyes—and can prevent blindness. The sooner you work to manage your diabetes and other health conditions, the better.
Ask your eye care professional to help you find a low vision and rehabilitation clinic. Special eye care professionals can help you manage vision loss that cannot be corrected with glasses, contact lenses, medicine, or surgery.
Special devices and training may help you make the most of your remaining vision so that you can continue to be active, enjoy hobbies, visit friends and family members, and live without help from others.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDKpart of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public.
Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. The NIDDK would like to thank: Neil M.
Bressler, MD, The Wilmer Eye Institute, Johns Hopkins University School of Medicine; Emily Chew, MD, National Eye Institute NEI. Home Health Information Diabetes Diabetes Overview Preventing Diabetes Problems Diabetic Eye Disease. English English Español.
On this page: What is diabetic eye disease? How does diabetes affect my eyes?
: Diabetic neuropathy in the eyes| Causes & risk factors | The procedure treats problems with severe bleeding or scar tissue caused by proliferative diabetic retinopathy. Scar tissue can force the retina to peel away from the tissue beneath it, like wallpaper peeling away from a wall. A retina that comes completely loose, or detaches, can cause blindness. During vitrectomy, a clear salt solution is gently pumped into the eye to maintain eye pressure during surgery and to replace the removed vitreous. Vitrectomy is done in a surgery center or hospital with pain medicine. In a surgery center or hospital visit, your doctor can remove the cloudy lens in your eye, where the cataract has grown, and replace it with an artificial lens. People who have cataract surgery generally have better vision afterward. After your eye heals, you may need a new prescription for your glasses. Your vision following cataract surgery may also depend on treating any damage from diabetic retinopathy or macular edema. To prevent diabetic eye disease, or to keep it from getting worse, manage your diabetes ABCs: your A1c, blood pressure, and cholesterol; and quit smoking if you smoke. Read more information on how to manage diabetes. Also, have a dilated eye exam at least once a year—or more often if recommended by your eye care professional. These actions are powerful ways to protect the health of your eyes—and can prevent blindness. The sooner you work to manage your diabetes and other health conditions, the better. Ask your eye care professional to help you find a low vision and rehabilitation clinic. Special eye care professionals can help you manage vision loss that cannot be corrected with glasses, contact lenses, medicine, or surgery. Special devices and training may help you make the most of your remaining vision so that you can continue to be active, enjoy hobbies, visit friends and family members, and live without help from others. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. The NIDDK would like to thank: Neil M. Bressler, MD, The Wilmer Eye Institute, Johns Hopkins University School of Medicine; Emily Chew, MD, National Eye Institute NEI. Home Health Information Diabetes Diabetes Overview Preventing Diabetes Problems Diabetic Eye Disease. English English Español. On this page: What is diabetic eye disease? How does diabetes affect my eyes? How common is diabetic eye disease? Who is more likely to develop diabetic eye disease? What are the symptoms of diabetic eye disease? When should I see a doctor right away? How do doctors diagnose eye problems from diabetes? How do doctors treat diabetic eye disease? What can I do to protect my eyes? What if I already have some vision loss from diabetes? What is diabetic eye disease? The best ways to manage your diabetes and keep your eyes healthy are to manage your blood glucose , blood pressure , and cholesterol , sometimes called the diabetes ABCs If you smoke, get help to quit smoking have a dilated eye exam once a year Photo courtesy of the National Eye Institute, NIH. So controlling your blood pressure and cholesterol can also help lower your risk for vision loss. In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months. Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help. Learn more about injections. Laser treatment. To reduce swelling in your retina, eye doctors can use lasers to make the blood vessels shrink and stop leaking. Learn more about laser treatment for diabetic retinopathy. Eye surgery. If your retina is bleeding a lot or you have a lot of scars in your eye, your eye doctor may recommend a type of surgery called a vitrectomy. Learn more about vitrectomy. Scientists are studying better ways to find, treat, and prevent vision loss in people with diabetes. One NIH-funded research team is studying whether a cholesterol medicine called fenofibrate can stop diabetic retinopathy from getting worse. Last updated: November 15, National Eye Institute Research Today… Vision Tomorrow. English Español. Search the site. Learn About Eye Health Healthy Vision Eye Conditions and Diseases Eye Health Data and Statistics Campaigns Vision Rehabilitation NEI for Kids Outreach Resources Grants and Training How to Apply Funding Opportunities Training at NEI Funding for Training and Career Development Policies and Procedures Prior Approval Requests Resources for Researchers Contact Grants and Funding Staff Research at NEI Clinical Trials Research Labs and Branches Jobs and Training Opportunities at NEI NEI Research Seminars About NEI Diversity, Equity, Inclusion and Accessibility at NEI Strategic Planning News and Events Goals and Accomplishments NEI History NEI Leadership Budget and Congress Advisory Committees National Eye Health Education Program Donate to NEI. Home Learn About Eye Health Eye Conditions and Diseases Diabetic Retinopathy. Print this Page. Diabetic Retinopathy. On this page:. At a glance: Diabetic Retinopathy Early Symptoms: None. Later Symptoms: Blurry vision, floating spots in your vision, blindness. Diagnosis: Dilated eye exam. Treatment: Injections , laser treatment, surgery. What is diabetic retinopathy? Other types of diabetic eye disease Diabetic retinopathy is the most common cause of vision loss for people with diabetes. But diabetes can also make you more likely to develop several other eye conditions: Cataracts. Having diabetes makes you 2 to 5 times more likely to develop cataracts. However, an eye specialist, called an ophthalmologist , can detect the signs. It is important that people with diabetes have an eye examination at least once a year or when a doctor recommends that they do. These drops dilate the pupils and allow the doctor to view the inside of the eye. These eye drops and the bright lights of the photographs can feel uncomfortable. In high risk individuals, the eye drops may cause an increase in ocular pressure. They will then take pictures as the dye circulates the eyes. The dye may leak into the retina or stain the blood vessels if the blood vessels are abnormal. This test can help the doctor determine which blood vessels are leaking fluid or have broken down or become blocked. This information provides accurate guidance for any laser treatments. It may sometimes indicate the need for the injection of medicine into the eye. As the dye exits the body, people may notice that they have yellowish skin or dark orange urine for a day or so. Optical coherence tomography OCT is a noninvasive imaging scan that provides high resolution cross-sectional images of the retina, revealing its thickness and allowing eye doctors to look for cysts or swelling. OCT is similar to ultrasound testing, but it uses light rather than sound to produce images. The scan can also aid the detection of diseases of the optic nerve. Treating diabetic retinopathy depends on several factors, including the severity of the condition and how it has responded to previous treatments. This approach is known as watchful waiting. In some cases, a person may need a comprehensive dilated eye exam as often as every 2—4 months. Individuals will need to work with their doctor to control diabetes. Good blood sugar control can significantly slow the development of diabetic retinopathy. A doctor uses targeted lasers to shrink blood vessels in the eye and seal the leaks from abnormal blood vessels. This treatment can either stop or slow down the leakage of blood and the buildup of fluid in the eye. People may need more than one session. The procedure involves the doctor placing numbing medicine in the eye and then aiming a strong beam of light into the eye using a special lens. The bright light can sting or feel uncomfortable, and it is common to experience blurry vision for the rest of the day. Small spots may appear in the visual field for a few weeks after the procedure. Laser treatment comes with certain risks, such as a loss of peripheral vision, color vision, and night vision. A person can talk to their doctor about the relative benefits and risks of this treatment. Certain medicines can reduce swelling and minimize leakage from blood vessels in the eyes. Medicines may include anti-VEGF drugs and corticosteroids. People may need to get regular injections, but over time, they usually require injections less frequently. If a person has problems with the retina or vitreous, they may benefit from a vitrectomy. This procedure is the removal of some of the vitreous from the eye. The aim is to replace cloudy vitreous or blood to improve vision and to help the doctor find and repair any sources of retinal bleeding. After removing the cloudy or bloody vitreous, the surgeon will insert a clear liquid or gas in its place. The body will absorb the liquid or gas over time and create new vitreous in its place. After the surgery, the person will usually need to wear an eye patch for about a day and use eye drops to reduce swelling and prevent infections. If the doctor puts a gas bubble in the eye, the person will need to hold their head in a certain position for a few days or weeks to make sure that the bubble stays in the right place. They will also need to avoid flying and visiting places at high altitudes until the bubble goes away. Surgery is not a cure for diabetic retinopathy, but it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur despite treatment. |
| Diabetic Neuropathy | Cedars-Sinai | People with diabetes can take steps to control their blood pressure , such as:. Diabetic retinopathy is an eye condition that affects people with diabetes. Without treatment, it can cause complications that include vision loss. Having a comprehensive dilated eye exam at least once a year can help a person catch the condition early to prevent complications. Diabetic neuropathy is nerve damage that affects a range of nerves in the bodies of some people with diabetes. It can lead to paralysis and might have…. Diabetes is a chronic condition that can lead to a number of symptoms and complications. Find out more about how to spot the symptoms of type 1 and…. To prevent eye damage from diabetes, a person can aim to keep their blood sugar, blood pressure, and cholesterol levels in the target range. A doctor…. Various vision aids, lifestyle changes, and rehabilitation can help a person live with and manage diabetic macular edema. Learn more here. Can a doctor cure and reverse diabetic retinopathy? Read on to learn more about the treatments for this eye condition and if it is reversible. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about diabetic retinopathy. Medically reviewed by Vicente Diaz, MD, MBA — By Adam Felman — Updated on November 12, What is it? Symptoms Complications Risk factors Diagnosis Treatment Prevention Summary Diabetic retinopathy is blood vessel damage in the retina that happens as a result of diabetes. Was this helpful? What is diabetic retinopathy? Risk factors. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Share this article. Latest news Ovarian tissue freezing may help delay, and even prevent menopause. RSV vaccine errors in babies, pregnant people: Should you be worried? Scientists discover biological mechanism of hearing loss caused by loud noise — and find a way to prevent it. How gastric bypass surgery can help with type 2 diabetes remission. Atlantic diet may help prevent metabolic syndrome. Related Coverage. What to know about diabetic neuropathy. Medically reviewed by Maria S. Prelipcean, MD. While heart rate changes during the former three tests mainly reflect parasympathetic function, BP in the Valsalva maneuver and orthostatic hypotension reflect sympathetic function Heart rate variability HRV in time and frequency domain indices have been described as another tool to evaluate cardiovascular autonomic neuropathy CARTs and HRV are frequently used for cardiovascular autonomic neuropathy diagnosis because they exhibit good reproducibility, are easy to execute, and, when combined, provide high specificity 38 , Exploratory data analysis was performed through summary measures mean, standard deviation, minimum, median, maximum, frequency, and percentage. Comparisons between groups were performed using the Wilcoxon test. The analyses were performed using the Statistical Analysis System SAS for Windows, version 9. This study included a total of 60 individuals between 27 and 77 years of age The two groups that included T2D patients were similar for disease duration and there were no statistically significant differences as far as sex is concerned among the groups. All CA patients had peripheral neuropathy and cardiovascular autonomic neuropathy. No individuals from the control group had peripheral neuropathy or cardiovascular autonomic neuropathy. Table 1 presents the distribution of the groups and the association between autonomic and peripheral neuropathies. Table 1 Comparative analysis among the groups of type 2 diabetes T2D patients with Charcot arthropathy CA , type 2 diabetes patients without CA, and healthy individuals according to autonomic and peripheral neuropathies. There were no significant differences in glycated hemoglobin HbA1c between the subjects. Kidney function was significantly lower among T2D patients with CA relative to T2D patients who did not have CA. Table 2 Comparative analysis of clinical, demographic, and metabolic characteristics of type 2 diabetes T2D patients with and without Charcot arthropathy CA. Subjects with T2D had significantly more abnormalities in their ocular surface variables indicative of DED and ocular surface dysfunction relative to the control group. All results of the ocular parameters were the most abnormal among patients with both T2D and CA. Table 3 provides the ocular variable information from each group. Table 3 Comparisons in ocular variables between type 2 diabetes T2D patients with Charcot arthropathy CA , T2D patients without CA, and healthy individuals. A relevant association was found between ocular surface disease, T2D, and CA. On a three-point scale between absent and established, the established form of tear deficiency was more frequent among T2D subjects Table 4. Some subjects in the control group presented incipient ocular surface disease, which may rely on aging processes another relevant risk factor for this condition. Figure 1 provides illustrative images of objective parameters in healthy individuals, type 2 diabetes T2D patients and diabetic with Charcot arthropathy. Tear meniscus height to infer aqueous tear volume, meibography to evaluate lipid layer production glands, Noninvasive Break Up Time to measure tear stability and also pupillometry. Table 4 Comparison of Ocular surface dysfunction between type 2 diabetes T2D patients with Charcot arthropathy CA , T2D patients without CA, and healthy individuals. This study evaluated the associations between different types of neuropathy namely, peripheral neuropathy and cardiovascular autonomic neuropathy and ocular findings in T2D patients with CA, T2D patients without CA, and healthy individuals. Almost all of the ocular variables differed significantly between the three groups. RNFL loss occurs in patients with diabetes regardless of diabetic retinopathy, suggesting that the function of neuronal cells in the retina is compromised even before the appearance of microvascular changes 14 , 41 , Several studies have shown differences in RNFL thickness between individuals with diabetes and a healthy age-matched population Additionally, previous reports have shown full retinal and inner retinal thickness to be significantly reduced in individuals with neuropathy, particularly among patients at increased risk of foot ulceration RNFL thinning represents indirect evidence of diabetes-induced neurodegeneration, which may precede the development of diabetic retinopathy. A typical manifestation of diabetic autonomic neuropathy is pupillary autonomic neuropathy, which affects pupillary function Pupillometry can be used to assess the integrity of afferent visual pathways and to determine the balance between the sympathetic constrictor and parasympathetic dilator systems Wang et al. emphasizes that pupil dilation requires both parasympathetic and sympathetic innervation of the iris These results indicate both parasympathetic and sympathetic autonomic dysfunction and reinforce the utility of pupillometry in determining the presence or absence of autonomic neuropathy DED can occur in diabetics as a result of decreased corneal sensitivity associated with the development of diabetic neurotrophic keratopathy 47 , while decreased tear film stability results from decreased goblet cell density The combination of lacrimal gland function assessment and Schirmer test has determined lower tear production rates in diabetics than in non-diabetic individuals, except in initial compensatory phases of DED In T2D patients, ocular surface changes including reduced tear film stability and secretion, reduced sub-basal nerve density, and reduced corneal sensitivity can occur simultaneously and even prior to clinical evidence of peripheral or autonomic neuropathy. The subjects included herein exhibited broad impacts of ocular surface disease as determined by the assessments of tear stability NITBUT , epithelial integrity fluorescein staining , lipid production meiboscore , and symptom intensity OSDI , all of which were found to represent gradual impairment according to the severity of the disease and its complications, and to be worse among patients with both T2D and CA. It is important to consider that a increase in these values may be related to a compensatory reflex phase of DED 18 , 22 , The results herein strongly suggest that individuals with both T2D and CA experience severe neuropathy in all parts of the body—not only in the foot, but also in the peripheral nerves, the cardiovascular system and the eyes, among other possible systems. Study limitations to be acknowledged include the cross-sectional design and small sample size. However, the latter is justified by the rarity of CA, even in tertiary hospitals. The main strengths of this study are the use of a highly specific method for cardiovascular autonomic neuropathy diagnosis CARTs combined with spectral analysis of the HRV and the systematic ocular assessment provided by a broad panel of tests. In summary, our data suggest that, due to their association with established cardiovascular autonomic neuropathy and peripheral neuropathy, dry eye disease symptoms and ocular findings could be considered additional clinical tools in the screening and follow-up treatment of diabetic neuropathy and related complications. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. The studies involving human participants were reviewed and approved by Institutional Research Ethics Committee Board CAAE All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil CAPES - Finance Code The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Dahlström E, Sandholm N. Progress in Defining the Genetic Basis of Diabetic Complications. Curr Diabetes Rep 17 9 :1— doi: CrossRef Full Text Google Scholar. Cavanagh PR, Young MJ, Adams JE, Vickers KL, Boulton AJM. Radiographic abnormalities in the feet of patients with diabetic neuropathy. Diabetes Care 17 3 —9. PubMed Abstract CrossRef Full Text Google Scholar. Dalla Paola L. Confronting a dramatic situation: The charcot foot complicated by osteomyelitis. Int J Low Extrem Wounds 13 4 — Ramanujam CL, Stapleton JJ, Zgonis T. Diabetic charcot neuroarthropathy of the foot and ankle with osteomyelitis. Clin Podiatr Med Surg — Dimitropoulos G, Tahrani AA, Stevens MJ. Cardiovascular autonomic neuropathy in patients with diabetes mellitus. World J Diabetes 5 1 — The influence of autonomic neuropathy on mortality in insulin-dependent diabetes. Q J Med 79 — Rogers LC, Frykberg RG, Armstrong DG, Boulton AJM, Edmonds M, Ha Van G, et al. The Charcot foot in diabetes. Diabetes Care 34 9 —9. Schmidt BM, Holmes CM. Updates on Diabetic Foot and Charcot Osteopathic Arthropathy. Curr Diabetes Rep 18 74 :1— Holmes C, Schmidt B, Munson M, Wrobel JS. Charcot stage 0: A review and consideratons for making the correct diagnosis early. Clin Diabetes Endocrinol 1 18 :1— Papanas N, Maltezos E. Etiology, pathophysiology and classifications of the diabetic Charcot foot. Diabetes Foot Ankle —5. Milne TE, Rogers JR, Kinnear EM, Martin HV, Lazzarini PA, Quinton TR, et al. Developing an evidence-based clinical pathway for the assessment, diagnosis and management of acute Charcot Neuro-Arthropathy: A systematic review. J Foot Ankle Res 6 30 :1— Johnson-Lynn SE, McCaskie AW, Coll AP, Robinson AHN. Neuroarthropathy in diabetes: pathogenesis of charcot arthropathy. Bone Jt Res 7 5 —8. Gouveri E. Charcot osteoarthropathy in diabetes: A brief review with an emphasis on clinical practice. World J Diabetes 2 5 — Wanzou JPV, Sekimpi P, Komagum JO, Nakwagala F, Mwaka ES. Charcot arthropathy of the diabetic foot in a sub-Saharan tertiary hospital: A cross-sectional study. J Foot Ankle Res 12 33 :1—9. Moura-Neto A, Fernandes TD, Zantut-Wittmann DE, Trevisan RO, Sakaki MH, Santos ALG, et al. Charcot foot: Skin temperature as a good clinical parameter for predicting disease outcome. Diabetes Res Clin Pract e11—4. Achtsidis V, Eleftheriadou I, Kozanidou E, Voumvourakis KI, Stamboulis E, Theodosiadis PG, et al. Dry eye syndrome in subjects with diabetes and association with neuropathy. People with diabetic retinopathy may need laser surgery to seal leaking blood vessels or to discourage other blood vessels from leaking. A doctor of optometry might need to inject medications into the eye to decrease inflammation or stop the formation of new blood vessels. People with advanced cases of diabetic retinopathy might need a surgical procedure to remove and replace the gel-like fluid in the back of the eye, called the vitreous. Surgery may also be needed to repair a retinal detachment. This is a separation of the light-receiving lining in the back of the eye. Laser treatment photocoagulation is used to stop the leakage of blood and fluid into the retina. A laser beam of light can be used to create small burns in areas of the retina with abnormal blood vessels to try to seal the leaks. Treatment for diabetic retinopathy depends on the stage of the disease. The goal of any treatment is to slow or stop the progression of the disease. In the early stages of non-proliferative diabetic retinopathy, regular monitoring may be the only treatment. Following your doctor's advice for diet and exercise and controlling blood sugar levels can help control the progression of the disease. Injections of medication in the eye are aimed at discouraging the formation of abnormal blood vessels and may help slow down the damaging effects of diabetic retinopathy. If the disease advances, the abnormal blood vessels can leak blood and fluid into the retina, leading to macular edema. Laser treatment photocoagulation can stop this leakage. A laser beam of light creates small burns in areas of the retina with abnormal blood vessels to try to seal the leaks. Widespread blood vessel growth in the retina, which occurs in proliferative diabetic retinopathy, can be treated by creating a pattern of scattered laser burns across the retina. This causes abnormal blood vessels to shrink and disappear. With this procedure, some side vision may be lost in order to safeguard the central vision. Acanthamoeba is one of the most common organisms in the environment. Although it rarely causes infection, when it does occur, it can threaten your vision. Amblyopia—also known as lazy eye—is the loss or lack of development of clear vision in one or both eyes. Forgot username or password? You do not have access to this content. Call Not a member? Join the AOA today! Eye and Vision Conditions. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. These damaged blood vessels can cause vision loss: Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision. In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision. Diabetic retinopathy is classified into two types. Non-proliferative diabetic retinopathy Non-proliferative diabetic retinopathy NPDR is the early stage of the disease in which symptoms will be mild or nonexistent. Proliferative diabetic retinopathy Proliferative diabetic retinopathy PDR is the more advanced form of the disease. Risk factors for diabetic retinopathy include: Diabetes. People with type 1 or type 2 diabetes are at risk for developing diabetic retinopathy. |
| The Two Stages of Diabetic Eye Disease | As the dye exits the body, people may notice that they have yellowish skin or dark orange urine for a day or so. Optical coherence tomography OCT is a noninvasive imaging scan that provides high resolution cross-sectional images of the retina, revealing its thickness and allowing eye doctors to look for cysts or swelling. OCT is similar to ultrasound testing, but it uses light rather than sound to produce images. The scan can also aid the detection of diseases of the optic nerve. Treating diabetic retinopathy depends on several factors, including the severity of the condition and how it has responded to previous treatments. This approach is known as watchful waiting. In some cases, a person may need a comprehensive dilated eye exam as often as every 2—4 months. Individuals will need to work with their doctor to control diabetes. Good blood sugar control can significantly slow the development of diabetic retinopathy. A doctor uses targeted lasers to shrink blood vessels in the eye and seal the leaks from abnormal blood vessels. This treatment can either stop or slow down the leakage of blood and the buildup of fluid in the eye. People may need more than one session. The procedure involves the doctor placing numbing medicine in the eye and then aiming a strong beam of light into the eye using a special lens. The bright light can sting or feel uncomfortable, and it is common to experience blurry vision for the rest of the day. Small spots may appear in the visual field for a few weeks after the procedure. Laser treatment comes with certain risks, such as a loss of peripheral vision, color vision, and night vision. A person can talk to their doctor about the relative benefits and risks of this treatment. Certain medicines can reduce swelling and minimize leakage from blood vessels in the eyes. Medicines may include anti-VEGF drugs and corticosteroids. People may need to get regular injections, but over time, they usually require injections less frequently. If a person has problems with the retina or vitreous, they may benefit from a vitrectomy. This procedure is the removal of some of the vitreous from the eye. The aim is to replace cloudy vitreous or blood to improve vision and to help the doctor find and repair any sources of retinal bleeding. After removing the cloudy or bloody vitreous, the surgeon will insert a clear liquid or gas in its place. The body will absorb the liquid or gas over time and create new vitreous in its place. After the surgery, the person will usually need to wear an eye patch for about a day and use eye drops to reduce swelling and prevent infections. If the doctor puts a gas bubble in the eye, the person will need to hold their head in a certain position for a few days or weeks to make sure that the bubble stays in the right place. They will also need to avoid flying and visiting places at high altitudes until the bubble goes away. Surgery is not a cure for diabetic retinopathy, but it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur despite treatment. High blood pressure, or hypertension , is another contributing factor. People with diabetes can take steps to control their blood pressure , such as:. Diabetic retinopathy is an eye condition that affects people with diabetes. Without treatment, it can cause complications that include vision loss. Having a comprehensive dilated eye exam at least once a year can help a person catch the condition early to prevent complications. Diabetic neuropathy is nerve damage that affects a range of nerves in the bodies of some people with diabetes. It can lead to paralysis and might have…. Diabetes is a chronic condition that can lead to a number of symptoms and complications. Find out more about how to spot the symptoms of type 1 and…. To prevent eye damage from diabetes, a person can aim to keep their blood sugar, blood pressure, and cholesterol levels in the target range. A doctor…. Various vision aids, lifestyle changes, and rehabilitation can help a person live with and manage diabetic macular edema. Learn more here. Can a doctor cure and reverse diabetic retinopathy? Read on to learn more about the treatments for this eye condition and if it is reversible. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. What to know about diabetic retinopathy. Medically reviewed by Vicente Diaz, MD, MBA — By Adam Felman — Updated on November 12, What is it? Symptoms Complications Risk factors Diagnosis Treatment Prevention Summary Diabetic retinopathy is blood vessel damage in the retina that happens as a result of diabetes. Was this helpful? What is diabetic retinopathy? Risk factors. How we reviewed this article: Sources. Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. Acanthamoeba is one of the most common organisms in the environment. Although it rarely causes infection, when it does occur, it can threaten your vision. Amblyopia—also known as lazy eye—is the loss or lack of development of clear vision in one or both eyes. Forgot username or password? You do not have access to this content. Call Not a member? Join the AOA today! Eye and Vision Conditions. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. These damaged blood vessels can cause vision loss: Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision. In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision. Diabetic retinopathy is classified into two types. Non-proliferative diabetic retinopathy Non-proliferative diabetic retinopathy NPDR is the early stage of the disease in which symptoms will be mild or nonexistent. Proliferative diabetic retinopathy Proliferative diabetic retinopathy PDR is the more advanced form of the disease. Risk factors for diabetic retinopathy include: Diabetes. People with type 1 or type 2 diabetes are at risk for developing diabetic retinopathy. The longer a person has diabetes, the more likely he or she is to develop diabetic retinopathy, particularly if the diabetes is poorly controlled. Hispanics and African Americans are at greater risk of developing diabetic retinopathy. Medical conditions. People with other medical conditions, such as high blood pressure and high cholesterol, are at greater risk. Pregnant women face a higher risk of developing diabetes and diabetic retinopathy. If a woman develops gestational diabetes, she has a higher risk of developing diabetes as she ages. Family History. Symptoms Symptoms of diabetic retinopathy include: Seeing spots or floaters. Blurred vision. Having a dark or empty spot in the center of your vision. Difficulty seeing well at night. Diagnosis Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with emphasis on evaluating the retina and macula, may include: Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be affecting vision. Visual acuity measurements to determine how much central vision has been affected. Refraction to determine if a new eyeglass prescription is needed. Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil. Measurement of the pressure within the eye. Supplemental testing may include: Retinal photography or tomography to document the current status of the retina. Fluorescein angiography to evaluate abnormal blood vessel growth. Treatment Treatment of diabetic retinopathy varies depending on the extent of the disease. If you are diabetic, you can help prevent or slow the development of diabetic retinopathy by: Taking your prescribed medication. Sticking to your diet. Exercising regularly. Controlling high blood pressure. Avoiding alcohol and smoking. Prevention Blood sugar control glycemic control. Lipid Lowering—lowering LDL cholesterol through lifestyle modification. Lowering saturated fats and cholesterol, weight loss, increase physical activity, use of statins for reducing high cholesterol. Weight management—bring overweight is associated with increased risk of Type 2 Diabetes. Find a Doctor of Optometry. Zip Code. Distance 5 Miles 10 Miles 25 Miles 50 Miles Miles Miles. Advanced Search. Find a Doctor of Optometry Zip Code Distance 5 Miles 10 Miles 25 Miles 50 Miles Miles Miles Search Advanced Search. Share This. Related Articles. Acanthamoeba Acanthamoeba is one of the most common organisms in the environment. |
| What causes diabetic neuropathy? | Collagen protein supplements doubles the chances of having glaucoma, inn Diabetic neuropathy in the eyes lead to Diabftic loss and blindness if not treated early. Creatine and athletic performance R, Neuroapthy K, Maeda S, Maeda K, Furuta A, Fukuoka S, et al. Curr Diabetes Rev. Diabetic retinopathy may not have any symptoms at first — but finding it early can help you take steps to protect your vision. If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following: Manage your diabetes. Research Faculty. |
| Diabetic retinopathy | AOA | Several alternative therapies have suggested some benefits for people with diabetic retinopathy, but more research is needed to understand whether these treatments are effective and safe. Let your doctor know if you take herbs or supplements. They can interact with other medications or cause complications in surgery, such as excessive bleeding. It's vital not to delay standard treatments to try unproven therapies. Early treatment is the best way to prevent vision loss. The thought that you might lose your sight can be frightening, and you may benefit from talking to a therapist or finding a support group. Ask your doctor for referrals. If you've already lost vision, ask your doctor about low-vision products, such as magnifiers, and services that can make daily living easier. The American Diabetes Association ADA recommends that people with type 1 diabetes have an eye exam within five years of being diagnosed. If you have type 2 diabetes, the American Diabetes Association ADA advises getting your initial eye exam at the time of your diagnosis. If there's no evidence of retinopathy on your initial exam, the ADA recommends that people with diabetes get dilated and comprehensive eye exams at least every two years. If you have any level of retinopathy, you'll need eye exams at least annually. Ask your eye doctor what he or she recommends. The ADA recommends that women with diabetes have an eye exam before becoming pregnant or during the first trimester of pregnancy and be closely followed during the pregnancy and up to one year after giving birth. Pregnancy can sometimes cause diabetic retinopathy to develop or worsen. On this page. Alternative medicine. Coping and support. Preparing for your appointment. Fluorescein angiography After your eyes are dilated, a dye is injected into a vein in your arm. Optical coherence tomography OCT With this test, pictures provide cross-sectional images of the retina that show the thickness of the retina. Early diabetic retinopathy If you have mild or moderate nonproliferative diabetic retinopathy, you might not need treatment right away. Advanced diabetic retinopathy If you have proliferative diabetic retinopathy or macular edema, you'll need prompt treatment. Depending on the specific problems with your retina, options might include: Injecting medications into the eye. This procedure uses a tiny incision in your eye to remove blood from the middle of the eye vitreous as well as scar tissue that's tugging on the retina. It's done in a surgery center or hospital using local or general anesthesia. Request an appointment. More Information. Can medicine help prevent diabetic macular edema? Clinical trials. Here's some information to help you get ready for your eye appointment. What you can do Write a brief summary of your diabetes history, including when you were diagnosed; medications you have taken for diabetes, now and in the past; recent average blood sugar levels; and your last few hemoglobin A1C readings, if you know them. List all medications, vitamins and other supplements you take, including dosages. List your symptoms, if any. Include those that may seem unrelated to your eyes. Ask a family member or friend to go with you, if possible. Someone who accompanies you can help remember the information you receive. Also, because your eyes will be dilated, a companion can drive you home. List questions for your doctor. For diabetic retinopathy, questions to ask your doctor include: How is diabetes affecting my vision? Do I need other tests? Is this condition temporary or long lasting? What treatments are available, and which do you recommend? What side effects might I expect from treatment? I have other health conditions. How can I best manage them together? If I control my blood sugar, will my eye symptoms improve? What do my blood sugar goals need to be to protect my eyes? Can you recommend services for people with visual impairment? Don't hesitate to ask other questions you have. What to expect from your doctor Your doctor is likely to ask you questions, including: Do you have eye symptoms, such as blurred vision or floaters? How long have you had symptoms? In general, how well are you controlling your diabetes? What was your last hemoglobin A1C? Do you have other health conditions, such as high blood pressure or high cholesterol? Have you had eye surgery? By Mayo Clinic Staff. Feb 21, Show References. Diabetic retinopathy. National Eye Institute. Accessed Feb. Mayo Clinic, Fraser CE, et al. Diabetic retinopathy: Classification and clinical features. American Optometrics Association. Diabetic retinopathy: Prevention and treatment. The diabetes advisor: Eye exams for people with diabetes. American Diabetes Association. Zhang HW, et al. Single herbal medicine for diabetic retinopathy review. Cochrane Database of Systematic Reviews. Nair AA, et al. Spotlight on faricimab in the treatment of wet age-related macular degeneration: Design, development and place in therapy. Drug Design, Development and Therapy. Chodnicki KD expert opinion. Mayo Clinic. News from Mayo Clinic. Diabetes and your eyes. Diabetic macular edema. Does keeping a proper blood sugar level prevent diabetic macular edema and other eye problems? Subjects who developed DON had a diabetes duration of This was significantly higher than for subjects who had not developed DON 9. There were also some disease duration differences among DON subgroups. DP and NVD subjects had a shorter diabetes duration than subjects with AION and OA Fig. Significant differences in HbA1c and HDL levels were also observed among DON groups. The HbA1c levels were significantly higher in subjects with DON 9. Additionally, HbA1c levels in the AION group were significantly greater than in the DP group Fig. The HDL levels were significantly lower in DON subjects 0. This was also true for all DON subgroups DP: 0. PDR subjects had a significantly higher rate of DON Mean CFT was Furthermore, mean CFT was Compared with PDR patients without DON, those with DON had higher age, diabetes duration, SBP, HbA1c, and CFT. In contrast, HDL was lower in those with PDR and DON than in those with PDR without DON. However, there was no significant difference in terms of sex between the two groups Table 2. Table 2 View Table. Comparison Between PDR With and Without DON. Table 2 Comparison Between PDR With and Without DON. Risk Factors for Developing Diabetic Optic Neuropathy. Overall, diabetes duration increased the likelihood of developing DON ORs: 1. Table 3 View Table. Predictors for Developing Diabetic Optic Neuropathy. Table 3 Predictors for Developing Diabetic Optic Neuropathy. A separate analysis was performed on data from the eyes of subjects that underwent HbA1c and HDL testing. Overall, an increased HbA1c level increased the risk of developing NVD, AION, and OA ORs: 1. The present study examined and compared demographic, systemic, and ocular characteristics of DR patients with and without DON in an effort to identify risk factors associated with developing DON. Varying DON severity was examined using established disease classifications. The overall prevalence of DON in DR patients was Our AION prevalence is lower than that previously found by Lee et al. Given that DM is a major risk factor for AION, 12 diabetic patients should be closely monitored for AION and other forms of DON. The severity of DR and DME can widely vary between patients and may be accompanied by DP. This finding is in agreement with prior studies that found that DP is a risk factor for DR progression. The idea that DP is a reversible form of AION has been proposed. Hypotension-related pathology has been identified in traditionally defined AION. However, in eyes with DP, edema is likely caused by perfusion deficiencies that result from capillary membrane disruption and subsequent interstitial fluid dynamic changes. Edema may then lead to ischemic, compressive, or toxic optic nerve head changes. Eyes with DR accompanied by disc swelling will likely develop retinal ischemia and subsequent neovascularization after disc edema resolution. The subjects included in the current study had an average diabetes duration of Subjects with DP in the current study had a disease duration of The current study also found that diabetes duration progressively increased as DON severity increased from non-DON to OA. Additionally, the DP and NVD groups had a shorter diabetes duration than the AION and OA groups. This is in agreement with a prior study that showed that diabetes duration is an important factor in DR presence and severity in subjects with AION. The current study showed that patients with more severe forms of DON tend to be older than those with earlier forms of DON. Mean subject age in the DP group was Therefore, our results support the previous finding that AION incidence may be higher in patients older than 67 years. Sex and SBP are other systemic factors that may influence DON occurrence. In the present study, we found that more women developed AION However, it is reported that no sex predilection exists in AION, 19 as well as NVD. Moreover, estrogen exerts no protective action against AION. Additionally, despite the fact that males and females were enrolled, males were still predominant in both AION Lee et al. The authors speculated that smoking may be an important risk factor for males with a high prevalence of AION and NVD in this study. To our knowledge, cigarettes contain toxic metals, such as Pb, Ni, Cd, and As, which disrupt glucose uptake and alter the related molecular mechanism of glucose regulation. There was also a positive association between Cd and plasma levels of glycated hemoglobin. However, we did not survey smoking status in the present study. We will consider this in further research. SBP was significantly higher in our subjects with DON This finding is in agreement with another study that found hypertension to be a risk factor for AION in diabetic patients. Plasma HbA1c and HDL levels may influence the development of DON. Subjects in the current study had a mean HbA1c of 8. Poor metabolic control and abrupt tightening of glycemic control e. This was particularly true in our subjects with NPDR and PDR. Moreover, AION subjects had significantly higher HbA1c levels than DP subjects. An acute decrease in HbA1c, along with a small cup-to-disc ratio, may put a patient at risk for developing DP. Particularly, AION subjects had the highest HDL value compared with the other three type of DON. Similarly, Sharma et al. Further research is needed to better understand the influences of both low-density lipoprotein and HDL on DON. Ocular factors, including CFT and DR severity, influenced DON incidence. This finding is consistent with the theory that DME may be present with DP, 18 , 24 along with NPDR or PDR. Diabetic patients have a greater risk of developing AION. Additionally, the risk of developing DP, NVD, and AION increased with greater diabetes duration, SBP, CFT and DR severity. However, HbA1c was also an important factor, with elevated levels increasing the risk of developing NVD, AION, and OA. The mechanisms underlying these risk factors are not completely understood. However, DR and hypertensive retinopathy are characterized by endothelial damage, a leaky blood—retinal barrier, vascular occlusion, and ischemia, all of which eventually contribute to neovascularization. Thus, the presence of these degenerative eye conditions may be indicative of more widespread ocular circulatory abnormalities. Our study had several limitations related to its retrospective design. Some known risk factors e. Additionally, only of subjects Moreover, a hospital-based patient population had its inherent limitations, resulting in enrolling more PDR patients in our study. Therefore, future prospective studies should contain the same data for all subjects to further evaluate and understand DON risk factors. Natural population epidemiology should be carried on a large scale. Even with these limitations, our study offers insight into DON. In spite of our population being hospital-based patients, the results from the present study could also be extrapolated to the general diabetic patient population. We found that similar risk factors influence both DR and DON simultaneously. For example, increased age, diabetes duration, SBP, CFT, and DR severity were risk factors for DON, and increased HbA1c was a risk factor for NVD, AION, and OA. No comprehensive investigation has reported on the prevalence of DON and its risk factors in Chinese DR patients previously. Hence, we believe that the results from the present study have important clinical significance for the general diabetic patient population. This is the first epidemiologic study on the prevalence and distribution of risk factors for DON in Chinese DR patients. We found that PDR subjects had a higher DON incidence compared with NPDR subjects. Additionally, HDL was significantly higher in subjects without DON than in subjects with DON, the same as PDR with DON and without DON, indicating that HDL may be a protective factor for DON. Our results also strengthen the argument that increased age, diabetes duration, SBP, CFT, DR severity, and HbA1c are all risk factors for developing DON in patients with DR. Therefore, in clinical practice, it is important to recognize and control these risk factors to delay the occurrence of DON. Supported by The First Hospital of China Medical University grant no. FSFH , the Natural Science Foundation of Liaoning Province grant no. No funders had any role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Disclosure: R. Hua , None; L. Qu , None; B. Ma , None; P. Yang , None; H. Sun , None; L. Liu , None. Giuliari GP, Sadaka A, Chang PY, Cortez RT. Diabetic papillopathy: current and new treatment options. Curr Diabetes Rev. Mallika PS, Aziz S, Asok T, Chong MS, Tan AK, Chua CN. Severe diabetic papillopathy mimicking non-arteritic anterior ischemic optic neuropathy NAION in a young patient. Med J Malaysia. Ostri C, Lund-Andersen H, Sander B, Hvidt-Nielsen D, Larsen M. Bilateral diabetic papillopathy and metabolic control. Appen RE, Chandra SR, Klein R, Myers FL. Diabetic papillopathy. Am J Ophthalmol. Slagle WS, Musick AN, Eckermann DR. Diabetic papillopathy and its relation to optic nerve ischemia. Optom Vis Sci. Saito Y, Ueki N, Hamanaka N, Shiotani Y, Nakae K, Kiuchi Y. Transient optic disc edema by vitreous traction in a quiescent eye with proliferative diabetic retinopathy mimicking diabetic papillopathy. Ding XY, Ou JX, Ma HJ, Tang SB. A clinical study of diabetic optic neuropathy. Chin J Pract Ophthalmol. Lee MS, Grossman D, Arnold AC, Sloan FA. Incidence of nonarteritic anterior ischemic optic neuropathy: increased risk among diabetic patients. Reddy D, Rani PK, Jalali S, Rao HL. A study of prevalence and risk factors of diabetic retinopathy in patients with non-arteritic anterior ischemic optic neuropathy NA-AION. Semin Ophthalmol. Almog Y, Goldstein M. Visual outcome in eyes with asymptomatic optic disc edema. J Neuroophthalmol. Wilkinson CP, Ferris FLIII, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Sun MH, Shariati MA, Liao YJ. Experimental anterior ischemic optic neuropathy in diabetic mice exhibited severe retinal swelling associated with VEGF elevation. Invest Ophthalmol Vis Sci. Regillo CD, Brown GC, Savino PJ, et al. Patient characteristics and fundus findings. Arch Ophthalmol. Fraser-Bell S, Capon M. Optic disc swelling in an adolescent with insulin dependent diabetes mellitus. Clin Exp Ophthalmol. Ornek K, Oğurel T. Intravitreal bevacizumab for diabetic papillopathy. J Ocul Pharmacol Ther. |
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Geben Sie wir werden besprechen.