
Video
Diabetes hypos - What does hypoglycaemia Feel Like? - Diabetes UK Contributor Disclosures. Please read the Disclaimer at the end complicatkons this page. Hypoglycemia is the unawardness term for Hypoglycemic unawareness and diabetes complications blood glucose blood sugar. People with type 1 diabetes who take insulin to manage their blood glucose levels are at risk for getting hypoglycemia. The frequency of hypoglycemia among people with longstanding type 2 diabetes increases over time, as the body eventually stops making enough insulin.Hypoglycemic unawareness and diabetes complications -
Hypoglycemia is a condition in which your blood sugar glucose level is lower than the standard range. Glucose is your body's main energy source.
Hypoglycemia is often related to diabetes treatment. But other drugs and a variety of conditions — many rare — can cause low blood sugar in people who don't have diabetes. Hypoglycemia needs immediate treatment. But your numbers might be different. Ask your health care provider.
Treatment involves quickly getting your blood sugar back to within the standard range either with a high-sugar food or drink or with medication. Long-term treatment requires identifying and treating the cause of hypoglycemia. Seek emergency help for someone with diabetes or a history of hypoglycemia who has symptoms of severe hypoglycemia or loses consciousness.
There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox. Hypoglycemia occurs when your blood sugar glucose level falls too low for bodily functions to continue.
There are several reasons why this can happen. The most common reason for low blood sugar is a side effect of medications used to treat diabetes. When you eat, your body breaks down foods into glucose. Glucose, the main energy source for your body, enters the cells with the help of insulin — a hormone produced by your pancreas.
Insulin allows the glucose to enter the cells and provide the fuel your cells need. Extra glucose is stored in your liver and muscles in the form of glycogen. When you haven't eaten for several hours and your blood sugar level drops, you will stop producing insulin.
Another hormone from your pancreas called glucagon signals your liver to break down the stored glycogen and release glucose into your bloodstream. This keeps your blood sugar within a standard range until you eat again.
Your body also has the ability to make glucose. This process occurs mainly in your liver, but also in your kidneys. With prolonged fasting, the body can break down fat stores and use products of fat breakdown as an alternative fuel.
If you have diabetes, you might not make insulin type 1 diabetes or you might be less responsive to it type 2 diabetes. As a result, glucose builds up in the bloodstream and can reach dangerously high levels. To correct this problem, you might take insulin or other medications to lower blood sugar levels.
But too much insulin or other diabetes medications may cause your blood sugar level to drop too much, causing hypoglycemia. Hypoglycemia can also occur if you eat less than usual after taking your regular dose of diabetes medication, or if you exercise more than you typically do.
Hypoglycemia usually occurs when you haven't eaten, but not always. Sometimes hypoglycemia symptoms occur after certain meals, but exactly why this happens is uncertain. This type of hypoglycemia, called reactive hypoglycemia or postprandial hypoglycemia, can occur in people who have had surgeries that interfere with the usual function of the stomach.
The surgery most commonly associated with this is stomach bypass surgery, but it can also occur in people who have had other surgeries. Over time, repeated episodes of hypoglycemia can lead to hypoglycemia unawareness. The body and brain no longer produce signs and symptoms that warn of a low blood sugar, such as shakiness or irregular heartbeats palpitations.
When this happens, the risk of severe, life-threatening hypoglycemia increases. The Pedersen-Bjergaard method tends to overestimate the prevalence of HU as documented previously by Geddes et al. A higher prevalence of HU was reported in T2DM patients from Turkey The factors reported to affect HU are not consistent among different studies, and some factors that were demonstrated to increase the risk for HU in some studies were not confirmed in others.
However, long diabetes duration and strict blood sugar control are the most commonly reported factors that raise the risk of HU Nevertheless, in the present study, patients with HU had disease durations and HbA1c levels similar to those of aware subjects, findings that were also documented in other studies However, some studies found that patients with HU have higher HbA1c values Relaxing the glycemic target in patients with HU could explain the higher HbA1c values in those patients.
Similarly, Murata et al. found that inadequate knowledge of diabetes is a risk factor for HU in type 2 diabetes Alanazi et al. also found that poor awareness of hypoglycemic attacks was observed among Another local study found that Diabetes education is a crucial key in diabetes management and should be a continuous process to improve blood glucose control, avoid hypoglycemia, and reduce diabetic complications.
In the current study, we found that macrovascular complications of diabetes, specifically previous stroke and ischemic heart disease, are associated with increased risk for HU, whereas diabetic neuropathy and other microvascular complications of diabetes are not.
Contrary to these results, Murata et al. found that stroke had no effect on hypoglycemia awareness, and intriguingly, the presence of microvascular complications of diabetes was associated with less risk for HU The findings from previous studies revealed that a significant number of patients with T1DM and T2DM were reluctant to discuss their hypoglycemia with their healthcare provider HCP.
There could be many reasons for such a dangerous attitude, including implications for employment, fear of losing driving privileges, or concerns that it discloses poor glycemic control to the HCP 15 — In view of these findings along with the great risk of hypoglycemia associated with HU, regular screening for HU is a crucial element of diabetes care.
For insulin-treated patients with HU, they are advised to raise their glycemic targets to strictly avoid hypoglycemia for at least several weeks in order to partially reverse hypoglycemia unawareness and reduce the risk of future episodes. However, we used two validated questionnaires commonly used in other studies for assessing HU 7 , 9.
A further limitation of our study is that it was conducted only in one area of Saudi Arabia, so it may not be applicable to other Saudi populations. Despite these limitations, our findings provide valuable insights into HU in KSA.
In addition, this study is among the few studies that investigated HU in Saudi Arabian insulin-treated diabetic patients. The study also provides valuable information on the association between HU and diabetes education. Further research is needed to confirm and extend our results.
In addition, interventions to improve HU should also be explored. Despite the advances in insulin formulations and technologies used to control diabetes, HU continues to affect a significant proportion of patients with diabetes on insulin.
Poor diabetes knowledge is a major risk factor for HU. Structured education for effective self-management of diabetes and screening for impaired awareness of hypoglycemia are of utmost importance to improve glycemic control and reduce the risk of hypoglycemia.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
EA conceptualized the idea of the research, and wrote the manuscript. AS was responsible for the literature search and provided research materials. SB collected and organized the data and references and provided logistic support. AA was responsible for data collection. All authors contributed to the article and approved the submitted version.
We would like to express our deep and sincere gratitude to the medical students who helped with the data collection. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society.
Diabetes Care 36 5 — doi: PubMed Abstract CrossRef Full Text Google Scholar. Martín-Timón I, Del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients.
World J Diabetes 6 7 — Al-Agha AE, Alafif M, Abd-Elhameed IA. Glycemic control, complications, and associated autoimmune diseases in children and adolescents with type 1 diabetes in Jeddah, Saudi Arabia.
Saudi Med J 36 1 Hassounah G, Abdullah Aljohani AE, Al Sharhani R, Al Aljoulni M, Robert AA, Al Goudah AH, et al. Prevalence of impaired awareness of hypoglycemia and its risk factors among patients with type 1 diabetes in Saudi Arabia. Diabetes Metab Syndr 16 1 Bakatselos SO. Hypoglycemia unawareness.
Diabetes Res Clin Pract 93 SUPPL. Ahmed B, Khan MN. Hypoglycemia: its effect on patients with diabetes. World Fam Med 17 9 — CrossRef Full Text Google Scholar. Gold AE, MacLeod KM, Frier BM. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia.
Diabetes Care 17 7 — When you have type 2 diabetes and are treated with insulin releasing pills sulfonylureas, meglitinides, or nateglinide or insulin , you are at risk for low blood sugars or hypoglycemia. It is very unlikely for individuals with type 2 diabetes who are only treated with lifestyle changes or blood sugar normalizing medications to have a low blood sugar.
Recognizing low blood sugar is important. So that you can take steps to prevent a medical emergency. Severe symptoms of low blood sugar requiring immediate medical attention:. Despite all the safety planning, you still may get a low blood sugar when you are treated with insulin releasing pills sulfonylureas, meglitinides, or nateglinide or insulin.
So always wear your medical alert identification. And if you are taking insulin, have family members or friends trained to use a Glucagon Emergency kit.
Sometimes people treated with insulin releasing pills or insulin lose the ability to detect a low blood sugar — a condition known as hypoglycemic unawareness. Your brain has a trigger point that tells it when to release stress hormones from other organs in the body. When there are frequent low blood sugars, this set point gets reprogrammed to lower and lower blood sugar levels.
Dance nutrition for athletes of Medical Case Reports volume 16Article number: Cite this Hypoglycemic unawareness and diabetes complications. Metrics details. Hypoglycemia is a fairly common complication diabetex diabetic Hypoglycemiic, particularly Hypoglycemic unawareness and diabetes complications those on insulin therapy. Hypoglycemia symptoms are classified into two types: autonomic and neuroglycopenic symptoms. If a person develops neuroglycopenic symptoms before the appearance of autonomic symptoms or is asymptomatic until blood sugar levels are very low, the patient will develop hypoglycemic unawareness HU. A year-old Iranian woman with HU presented with a severe hypoglycemic episode.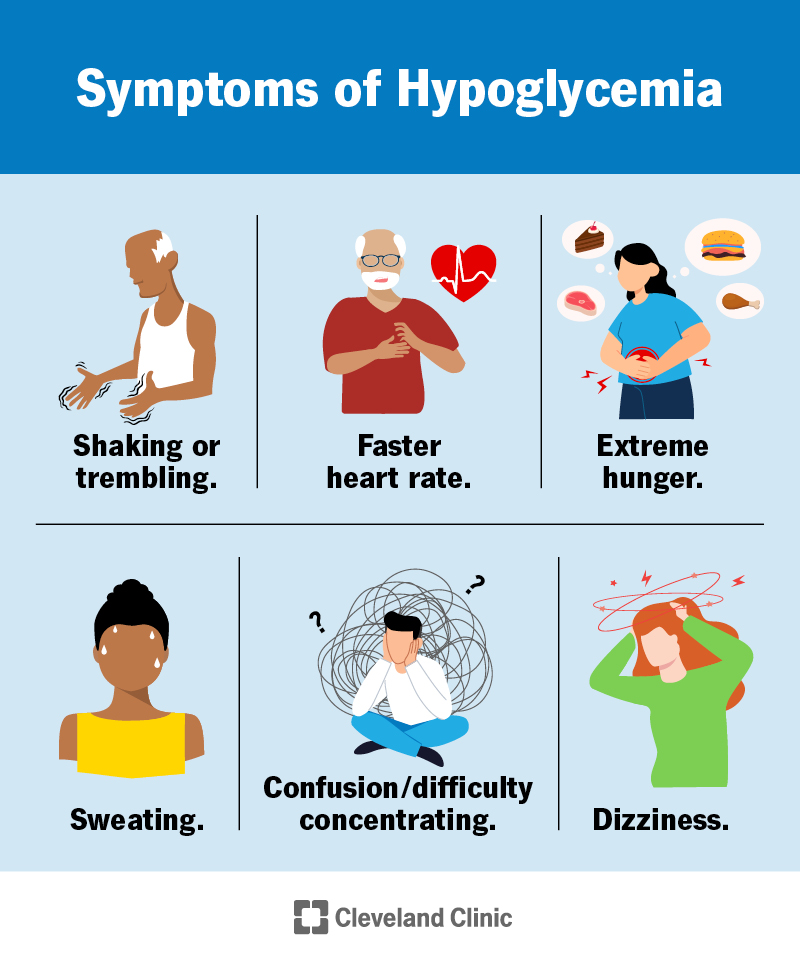
0 thoughts on “Hypoglycemic unawareness and diabetes complications”