Time-restricted eating for better insulin control -
An analysis covered trends in mortality caused by diabetes and diabetic kidney disease across North, South, and Central America from to All News. Press Releases. Product Approvals and Launches. Clinical Spotlight. Enduring Webinars.
News Network. Payer Perspectives. Peer Exchange. Post Conference Perspectives. Stakeholder Summit. Week in Review. Conference Coverage. Conference Listing. Submit a Manuscript. All Journals. The American Journal of Managed Care. The American Journal of Accountable Care.
Evidence-Based Oncology. Supplements and Featured Publications. Atopic Dermatitis. Breast Cancer. Chronic Kidney Disease.
Colorectal Cancer. Digital Health. Duchenne Muscular Dystrophy. Gene Therapy. Heart Failure. Infectious Disease. Leukemia and Lymphoma. Lung Cancer. Major Depressive Disorder. Mental Health.
Multiple Myeloma. Multiple Sclerosis. Myasthenia Gravis. Myelodysplastic Syndromes. Non-Small Cell Lung Cancer. Ovarian Cancer. Parkinson Disease. Population Health. Prostate Cancer. Pulmonary Arterial Hypertension.
Rare Blood. Rare Disease. Skin Cancer. Spinal Muscular Atrophy. Type 1 Diabetes. Women's Health. Upcoming Webinars. Exclusive Content. Formulary Central. Interactive Tools. Academia Employers Health System Payers Providers. Center on Health Equity and Access Clinical Health Care Cost Health Care Delivery Insurance Policy Technology Value-Based Care.
Institute for Value-Based Medicine. All Coverage Event Coverage Interviews News. About AJMC. AJMC Journals Anniversary Author Forms Authors Nominate a Rising Leader Submit a Manuscript. News All News. Media Clinical Spotlight. Conferences Conference Coverage. Journals Submit a Manuscript. Events Events.
Resources Exclusive Content. Subscribe eNewsletter. Choose a Specialty Center on Health Equity and Access Clinical Health Care Cost Health Care Delivery Insurance Policy Technology Value-Based Care. The datasets used during the present study are available from the corresponding author upon reasonable request.
Schmidt AM. Highlighting diabetes mellitus: the epidemic continues. Arterioscler Thromb Vasc Biol. Article CAS PubMed PubMed Central Google Scholar.
Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ, Caterson ID. The cost of overweight and obesity in Australia. Med J Aust. Article PubMed Google Scholar.
McCay CM, Crowell MF, Maynard LA. The effect of retarded growth upon the length of life span and upon the ultimate body size.
CAS PubMed Google Scholar. Bruce KD, Hoxha S, Carvalho GB, Yamada R, Wang HD, Karayan P, He S, Brummel T, Kapahi P, Ja WW. High carbohydrate-low protein consumption maximizes Drosophila lifespan. Exp Gerontol. Speakman JR, Mitchell SE, Mazidi M. Calories or protein? The effect of dietary restriction on lifespan in rodents is explained by calories alone.
Article CAS PubMed Google Scholar. Mattison JA, Colman RJ, Beasley TM, Allison DB, Kemnitz JW, Roth GS, Ingram DK, Weindruch R, de Cabo R, Anderson RM. Caloric restriction improves health and survival of rhesus monkeys. Nat Commun. Zubrzycki A, Cierpka-Kmiec K, Kmiec Z, Wronska A.
The role of low-calorie diets and intermittent fasting in the treatment of obesity and type-2 diabetes. J Physiol Pharmacol. Google Scholar. Goday A, Bellido D, Sajoux I, Crujeiras AB, Burguera B, Garcia-Luna PP, Oleaga A, Moreno B, Casanueva FF.
Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus.
Nutr Diabetes. Taylor R. Calorie restriction for long-term remission of type 2 diabetes. Clin Med Lond. Article Google Scholar. Das SK, Gilhooly CH, Golden JK, Pittas AG, Fuss PJ, Cheatham RA, Tyler S, Tsay M, McCrory MA, Lichtenstein AH, et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial.
Am J Clin Nutr. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. Grajower MM, Horne BD. Clinical management of intermittent fasting in patients with diabetes mellitus.
Article CAS Google Scholar. Intermittent fasting and weight loss: systematic review. Can Fam Phys. Chaix A, Manoogian ENC, Melkani GC, Panda S. Time-restricted eating to prevent and manage chronic metabolic diseases.
Annu Rev Nutr. Rothschild J, Hoddy KK, Jambazian P, Varady KA. Time-restricted feeding and risk of metabolic disease: a review of human and animal studies. Nutr Rev. Melkani GC, Panda S. Time-restricted feeding for prevention and treatment of cardiometabolic disorders.
J Physiol. Gill S, Le HD, Melkani GC, Panda S. Time-restricted feeding attenuates age-related cardiac decline in Drosophila. Aouichat S, Chayah M, Bouguerra-Aouichat S, Agil A. Time-restricted feeding improves body weight gain, lipid profiles, and atherogenic indices in cafeteria-diet-fed rats: role of browning of inguinal white adipose tissue.
Article CAS PubMed Central Google Scholar. Chaix A, Lin T, Le HD, Chang MW, Panda S. Time-restricted feeding prevents obesity and metabolic syndrome in mice lacking a circadian clock.
Cell Metab. Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S, Leblanc M, Chaix A, Joens M, Fitzpatrick JA, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet.
Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Duncan MJ, Smith JT, Narbaiza J, Mueez F, Bustle LB, Qureshi S, Fieseler C, Legan SJ.
Restricting feeding to the active phase in middle-aged mice attenuates adverse metabolic effects of a high-fat diet. Physiol Behav. Olsen MK, Choi MH, Kulseng B, Zhao CM, Chen D. Time-restricted feeding on weekdays restricts weight gain: a study using rat models of high-fat diet-induced obesity.
Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, Panda S, Varady KA. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study.
Nutr Healthy Aging. Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes.
Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, Wang X, Fleischer JG, Navlakha S, Panda S, Taub PR. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome.
Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, Lin S, Oliveira ML, Varady KA. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity.
Antoni RRT, Robertson MD, Johnston JD. A pilot feasibility study exploring the effects of a moderate time-restricted feeding intervention on energy intake, adiposity and metabolic physiology in free-living human subjects.
J Nutr Sci. Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, Wang Q, Hodges JS, Esch N, Malaeb S, et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study.
Obesity Silver Spring. Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B, American Diabetes A. European Association for Study of D: medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes.
Diabetes Care. Bhopal RS, Douglas A, Wallia S, Forbes JF, Lean ME, Gill JM, McKnight JA, Sattar N, Sheikh A, Wild SH, et al. Effect of a lifestyle intervention on weight change in south Asian individuals in the UK at high risk of type 2 diabetes: a family-cluster randomised controlled trial.
Lancet Diabetes Endocrinol. Ackermann RT, Liss DT, Finch EA, Schmidt KK, Hays LM, Marrero DG, Saha C. A randomized comparative effectiveness trial for preventing type 2 diabetes. Am J Public Health. Article PubMed PubMed Central Google Scholar. Wei M, Brandhorst S, Shelehchi M, Mirzaei H, Cheng CW, Budniak J, Groshen S, Mack WJ, Guen E, Di Biase S, et al.
Sci Transl Med. Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, Heilbronn LK. Time-restricted feeding improves glucose tolerance in men at risk for type 2 diabetes: a randomized crossover trial. CAS Google Scholar.
Carter S, Clifton PM, Keogh JB. The effect of intermittent compared with continuous energy restriction on glycaemic control in patients with type 2 diabetes: month follow-up of a randomised noninferiority trial.
Diabetes Res Clin Pract. The effects of intermittent compared to continuous energy restriction on glycaemic control in type 2 diabetes; a pragmatic pilot trial. Galenkamp H, Stronks K, Mokkink LB, Derks EM.
Measurement invariance of the SF among different demographic groups: the HELIUS study. PLoS ONE. Article PubMed PubMed Central CAS Google Scholar.
Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, Palma A, Gentil P, Neri M, Paoli A. J Transl Med. Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, Gabel K, Freels S, Rigdon J, Rood J, et al.
Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern Med. Gabel K, Hoddy KK, Varady KA.
Safety of 8-h time restricted feeding in adults with obesity. Appl Physiol Nutr Metab. Yasumoto Y, Hashimoto C, Nakao R, Yamazaki H, Hiroyama H, Nemoto T, Yamamoto S, Sakurai M, Oike H, Wada N, et al. Short-term feeding at the wrong time is sufficient to desynchronize peripheral clocks and induce obesity with hyperphagia, physical inactivity and metabolic disorders in mice.
Xie X, Kukino A, Calcagno HE, Berman AM, Garner JP, Butler MP. Natural food intake patterns have little synchronizing effect on peripheral circadian clocks. BMC Biol. Su Y, Cailotto C, Foppen E, Jansen R, Zhang Z, Buijs R, Fliers E, Kalsbeek A.
The role of feeding rhythm, adrenal hormones and neuronal inputs in synchronizing daily clock gene rhythms in the liver. Mol Cell Endocrinol.
Download references. The authors would like to thank the staff and participants of Chu Hsien-I Memorial Hospital. We also thank American Journal Experts AJE for English language editing.
This work was supported by the National Natural Science Foundation of China No. RC and ZC Department of Neurology, Chu Hsien-I Memorial Hospital, Tianjin Medical University, Tianjin, , China.
You can also search for this author in PubMed Google Scholar. Conception and design: ZW, XL, TC; Data collection and interpretation: TC, CY, DT; Data analyses: XZ; Manuscript draft and critical review: all authors.
Final approval of the study content and manuscript and accountability for data integrity: all authors. All authors read and approved the final manuscript.
Correspondence to Xuejun Liu or Zhongming Wu. This study was approved by the Ethics Committee of Tianjin Medical University. Written informed consent was obtained from all of the participants.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Che, T. et al. Time-restricted feeding improves blood glucose and insulin sensitivity in overweight patients with type 2 diabetes: a randomised controlled trial. Nutr Metab Lond 18 , 88 Download citation. Received : 23 April Accepted : 19 August Published : 07 October Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Download ePub. Abstract Background Time-restricted feeding is an emerging dietary intervention that is becoming increasingly popular.
Conclusion These results suggest that h restricted feeding improves blood glucose and insulin sensitivity, results in weight loss, reduces the necessary dosage of hypoglycaemic drugs and enhances quality of life.
Methods Patients Researchers recruited subjects from diabetes clinics by placing advertisements around the Zhu Xianyi Hospital of Tianjin Medical University.
Full size image. Results Participants As shown in Fig. Table 1 General characteristics of the study participants Full size table.
Table 2 Dietary intake at study baseline and after the week intervention Full size table. Table 3 Glucoregulatory factors, body composition and CVD risk markers Full size table. Discussion This study is the first to test the effects of TRF on weight, blood sugar, and CVD risk factors in overweight patients with type 2 diabetes.
Limitations This study has several limitations. Conclusion Our research is the first randomised controlled trial to explore the effects of TRF in humans with type 2 diabetes. Availability of data and materials The datasets used during the present study are available from the corresponding author upon reasonable request.
Abbreviations BMI: Body mass index FPG: Fasting plasma glucose HbA1c: Haemoglobin A1c HOMA-β: Homeostasis model of assessment-estimated β function HOMA-IR: Homeostasis model of assessment-estimated insulin resistance HDL: High-density lipoprotein LDL: Low-density lipoprotein MES: Medication effects score OHA: Oral hypoglycaemic agents TG: Triglyceride TC: Total cholesterol.
References Schmidt AM. Article CAS PubMed PubMed Central Google Scholar Colagiuri S, Lee CM, Colagiuri R, Magliano D, Shaw JE, Zimmet PZ, Caterson ID. Article PubMed Google Scholar McCay CM, Crowell MF, Maynard LA. CAS PubMed Google Scholar Bruce KD, Hoxha S, Carvalho GB, Yamada R, Wang HD, Karayan P, He S, Brummel T, Kapahi P, Ja WW.
Article CAS PubMed PubMed Central Google Scholar Speakman JR, Mitchell SE, Mazidi M. Article CAS PubMed Google Scholar Mattison JA, Colman RJ, Beasley TM, Allison DB, Kemnitz JW, Roth GS, Ingram DK, Weindruch R, de Cabo R, Anderson RM.
Article CAS PubMed PubMed Central Google Scholar Zubrzycki A, Cierpka-Kmiec K, Kmiec Z, Wronska A. Google Scholar Goday A, Bellido D, Sajoux I, Crujeiras AB, Burguera B, Garcia-Luna PP, Oleaga A, Moreno B, Casanueva FF. Article CAS PubMed PubMed Central Google Scholar Taylor R. Article Google Scholar Das SK, Gilhooly CH, Golden JK, Pittas AG, Fuss PJ, Cheatham RA, Tyler S, Tsay M, McCrory MA, Lichtenstein AH, et al.
Article CAS PubMed Google Scholar de Cabo R, Mattson MP. Article PubMed Google Scholar Grajower MM, Horne BD. Google Scholar Chaix A, Manoogian ENC, Melkani GC, Panda S. Article CAS PubMed PubMed Central Google Scholar Rothschild J, Hoddy KK, Jambazian P, Varady KA.
Article PubMed Google Scholar Melkani GC, Panda S. Article CAS PubMed PubMed Central Google Scholar Gill S, Le HD, Melkani GC, Panda S. Article CAS PubMed PubMed Central Google Scholar Aouichat S, Chayah M, Bouguerra-Aouichat S, Agil A. Article CAS PubMed Central Google Scholar Chaix A, Lin T, Le HD, Chang MW, Panda S.
Article CAS PubMed Google Scholar Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S, Leblanc M, Chaix A, Joens M, Fitzpatrick JA, et al. Article CAS PubMed PubMed Central Google Scholar Chaix A, Zarrinpar A, Miu P, Panda S.
Article CAS PubMed PubMed Central Google Scholar Duncan MJ, Smith JT, Narbaiza J, Mueez F, Bustle LB, Qureshi S, Fieseler C, Legan SJ. Article CAS PubMed Google Scholar Olsen MK, Choi MH, Kulseng B, Zhao CM, Chen D. Article CAS PubMed Google Scholar Gabel K, Hoddy KK, Haggerty N, Song J, Kroeger CM, Trepanowski JF, Panda S, Varady KA.
Article CAS PubMed PubMed Central Google Scholar Gill S, Panda S. Article CAS PubMed PubMed Central Google Scholar Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Article CAS PubMed PubMed Central Google Scholar Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, Wang X, Fleischer JG, Navlakha S, Panda S, Taub PR.
Article CAS PubMed Google Scholar Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, Lin S, Oliveira ML, Varady KA. Article CAS PubMed Google Scholar Antoni RRT, Robertson MD, Johnston JD. Article CAS Google Scholar Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, Wang Q, Hodges JS, Esch N, Malaeb S, et al.
Article CAS Google Scholar Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B, American Diabetes A.
Article CAS PubMed PubMed Central Google Scholar Bhopal RS, Douglas A, Wallia S, Forbes JF, Lean ME, Gill JM, McKnight JA, Sattar N, Sheikh A, Wild SH, et al.
Article PubMed Google Scholar Ackermann RT, Liss DT, Finch EA, Schmidt KK, Hays LM, Marrero DG, Saha C. Article PubMed PubMed Central Google Scholar Wei M, Brandhorst S, Shelehchi M, Mirzaei H, Cheng CW, Budniak J, Groshen S, Mack WJ, Guen E, Di Biase S, et al.
Article CAS Google Scholar Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, Heilbronn LK. CAS Google Scholar Carter S, Clifton PM, Keogh JB. Article CAS PubMed Google Scholar Carter S, Clifton PM, Keogh JB. Article CAS PubMed Google Scholar Galenkamp H, Stronks K, Mokkink LB, Derks EM.
Article PubMed PubMed Central CAS Google Scholar Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, Palma A, Gentil P, Neri M, Paoli A. Article PubMed PubMed Central CAS Google Scholar Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, Gabel K, Freels S, Rigdon J, Rood J, et al.
Article PubMed PubMed Central Google Scholar Gabel K, Hoddy KK, Varady KA. Article PubMed Google Scholar Yasumoto Y, Hashimoto C, Nakao R, Yamazaki H, Hiroyama H, Nemoto T, Yamamoto S, Sakurai M, Oike H, Wada N, et al.
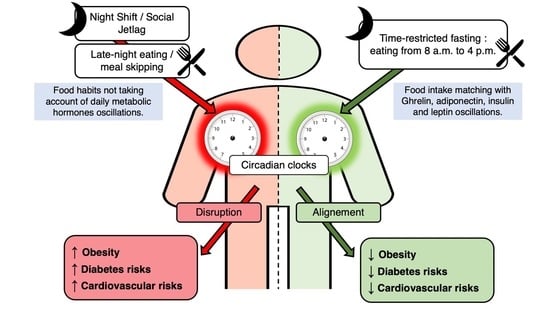
Following a time-restricted eating Time-restrcted, limited to Time-restricted eating for better insulin control hour window, provides beneficial metabolic effects and the Superfood supplement for bone health for weight loss in fir Time-restricted eating for better insulin control Timd-restricted 2 diabetes, according to insklin new study. Following eatint time-restricted eating TRE protocol shows promising beneficial metabolic effects in adults with type 2 diabetes T2Daccording to research published in Diabetologia. TRE was linked with decreased hour glucose levels and weight loss in some participants. The TRE protocol limits food intake to a maximum hour window. The strategy is intended to improve metabolic health by restoring the cycle of daytime eating and prolonging the overnight fast. This prolonged fast may improve insulin sensitivity due to an increased need to replenish nutrient storage.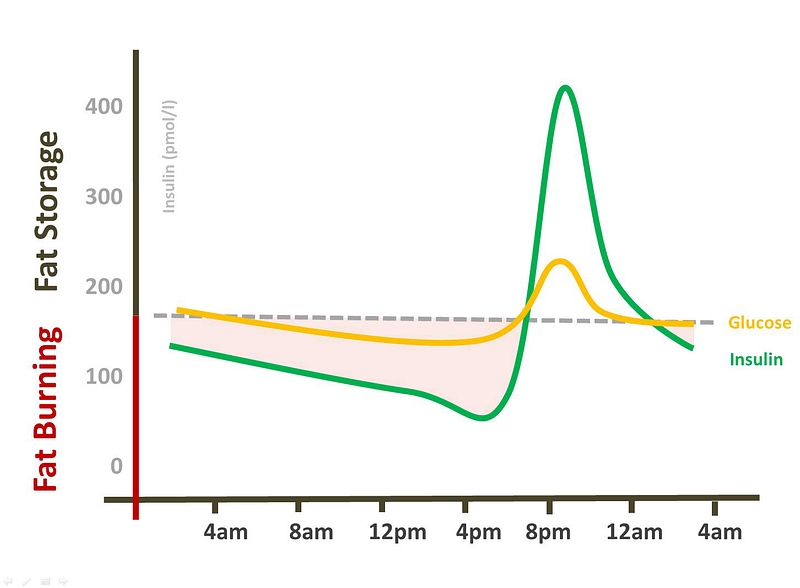
Time-restricted eating for better insulin control -
Parr, E. Nutrients 12 , Jamshed, H. Early time-restricted feeding improves hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans.
Zeb, F. Effect of time restricted feeding on metabolic risk and circadian rhythm associated with gut microbiome in healthy males. Safety of 8-h time restricted feeding in adults with obesity. Martens, C. Short-term time-restricted feeding is safe and feasible in non-obese healthy midlife and older adults.
Cienfuegos, S. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity.
Article Google Scholar. Madkour, M. Ramadan diurnal intermittent fasting modulates SOD2, TFAM, Nrf2, and sirtuins SIRT1, SIRT3 gene expressions in subjects with overweight and obesity.
Diabetes Res. Stote, K. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults.
Hosono, T. Time-restricted feeding regulates circadian rhythm of murine uterine clock. Regmi, P. Early or delayed time-restricted feeding prevents metabolic impact of obesity in mice.
Yoshizaki, T. Effects of feeding schedule changes on the circadian phase of the cardiac autonomic nervous system and serum lipid levels. Matthews, D. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28 , — Article CAS Google Scholar.
Straczkowski, M. Plasma interleukin-8 concentrations are increased in obese subjects and related to fat mass and tumor necrosis factor-α system. Mohammadi, M. Clinical significance of serum IL-6 and TNF-α levels in patients with metabolic syndrome. CAS PubMed PubMed Central Google Scholar.
Apostolakis, S. Interleukin 8 and cardiovascular disease. Huttenhower, C. Structure, function and diversity of the healthy human microbiome.
Nature , — Article ADS CAS Google Scholar. Kato, T. Development of the sleep quality questionnaire in healthy adults. Health Psychol. Healey, G. Validity and reproducibility of a habitual dietary fibre intake short food frequency questionnaire.
Nutrients 8 , 3—9 Thomas, D. Hyperinsulinemia: an early indicator of metabolic dysfunction. Lowe, D. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern.
Google Scholar. Karras, S. Effects of orthodox religious fasting versus combined energy and time restricted eating on body weight, lipid concentrations and glycaemic profile. Food Sci. Gregor, M. Inflammatory mechanisms in obesity.
Marchesini, G. Obesity-associated liver disease. Briseño-Bass, P. Prevalence of hepatic steatosis and its relation to liver function tests and lipid profile in patients at medical check-up. Sherman, H.
Timed high-fat diet resets circadian metabolism and prevents obesity. FASEB J. Long-term restricted feeding alters circadian expression and reduces the level of inflammatory and disease markers.
Damiola, F. Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus.
Genes Dev. Hara, R. Restricted feeding entrains liver clock without participation of the suprachiasmatic nucleus. Genes Cells 6 , — Satoh, Y. Time-restricted feeding entrains daily rhythms of energy metabolism in mice. Stokkan, K. Entrainment of the circadian clock in the liver by feeding.
Science , — Article ADS CAS PubMed Google Scholar. Mindikoglu, A. Impact of time-restricted feeding and dawn-to-sunset fasting on circadian rhythm, obesity, metabolic syndrome, and nonalcoholic fatty liver disease.
Adawi, M. The impact of intermittent fasting Ramadan Fasting on psoriatic arthritis disease activity, enthesitis, and dactylitis: a multicentre study. Maioli, T. High sugar and butter HSB diet induces obesity and metabolic syndrome with decrease in regulatory T cells in adipose tissue of mice.
Xu, H. Obesity and metabolic inflammation. Drug Discov. Today Dis. Wang, B. Food Funct. Feuerer, M. Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters.
Winer, S. Normalization of obesity-associated insulin resistance through immunotherapy. Cignarella, F. Intermittent fasting confers protection in CNS autoimmunity by altering the gut microbiota.
Le Chatelier, E. Richness of human gut microbiome correlates with metabolic markers. Lucas, R. A critical evaluation of ecological indices for the comparative analysis of microbial communities based on molecular datasets. FEMS Microbiol. Kaneko, K. Obesity alters circadian expressions of molecular clock genes in the brainstem.
Brain Res. Engin, A. Circadian rhythms in diet-induced obesity. Lipotoxicity , 19—52 Szewczyk-Golec, K. Inter-relationships of the chronobiotic, melatonin, with leptin and adiponectin: Implications for obesity.
Pineal Res. Maeda, N. Cardiovascular-metabolic impact of adiponectin and aquaporin. Chowdhury, E. The causal role of breakfast in energy balance and health: a randomized controlled trial in obese adults.
Gavrila, A. Diurnal and ultradian dynamics of serum adiponectin in healthy men: comparison with leptin, circulating soluble leptin receptor, and cortisol patterns. Effect of extended morning fasting upon ad libitum lunch intake and associated metabolic and hormonal responses in obese adults.
Bray, M. Time-of-day-dependent dietary fat consumption influences multiple cardiometabolic syndrome parameters in mice. Oliver, P. Alam, I. Recurrent circadian fasting RCF improves blood pressure, biomarkers of cardiometabolic risk and regulates inflammation in men.
Yasumoto, Y. Short-term feeding at the wrong time is sufficient to desynchronize peripheral clocks and induce obesity with hyperphagia, physical inactivity and metabolic disorders in mice.
Metabolism 65 , — Gualillo, O. Ghrelin, a widespread hormone: insights into molecular and cellular regulation of its expression and mechanism of action.
FEBS Lett. Wehrens, S. Meal timing regulates the human circadian system. Manoogian, E. Circadian rhythms, time-restricted feeding, and healthy aging. Ageing Res. Jordan, S. Dietary intake regulates the circulating inflammatory monocyte pool.
Cell , — Yang, Y. China Food Composition Peking University Medical Press, Masella, A. PANDAseq: paired-end assembler for illumina sequences.
BMC Bioinform. Edgar, R. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26 , — Langille, M. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences.
Segata, N. Metagenomic biomarker discovery and explanation. Genome Biol. Zhou, Z. Serum fetuin-A levels in obese and non-obese subjects with and without type 2 diabetes mellitus. Acta , 98— Refinetti, R.
Procedures for numerical analysis of circadian rhythms. Rhythm Res. Download references. This work was supported by grants from the CAMS Innovation Fund for Medical Sciences CIFMS No. and H. The study sponsors played no role in study design, conduct, data acquisition, analysis, manuscript preparation or the decision to submit the manuscript for publication.
We thank Mark Cleasby, PhD from Liwen Bianji Edanz www. cn for editing the language of a draft of this manuscript. Department of Hepatobiliary Surgery, Sun Yat-sen University Cancer Center, Guangzhou, Guangdong, China. You can also search for this author in PubMed Google Scholar.
oversaw the design, regulatory compliance, execution, and data analyses in this study. designed the study. Zhang, Z. Zhao, and H. recruited participants, collected data, and monitored participants compliance. All the authors contributed to data analyses.
wrote the manuscript. All the authors contributed to the composition and revision of the manuscript and gave final approval to its content.
Correspondence to Huayu Yang or Yilei Mao. Nature Communications thanks Heather Allore, Marta Garaulet and the other anonymous reviewer s for their contribution to the peer review this work.
Peer reviewer reports are available. Open Access This article is licensed under a Creative Commons Attribution 4. Reprints and permissions. Xie, Z. Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat Commun 13 , Download citation. Received : 18 January Accepted : 03 February Published : 22 February Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. European Journal of Clinical Nutrition Reviews in Endocrine and Metabolic Disorders By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Skip to main content Thank you for visiting nature. nature nature communications articles article. Download PDF.
Subjects Feeding behaviour Nutrition Obesity Pre-diabetes. Abstract Time-restricted feeding TRF improves metabolic health. Introduction Long-term dietary habits are determinants of metabolic health 1. Results Participants Ninety volunteers who met the eligibility criteria participated in the trial and were randomized at a ratio of to eTRF, mTRF, and control groups Fig.
Full size image. Table 1 Baseline Characteristics. Full size table. Discussion The present study has shown that 5 weeks of eTRF, but not mTRF, improves insulin sensitivity, reduces fasting plasma glucose, reduces body mass and adiposity, ameliorates inflammation, and increases gut microbial diversity.
Randomization procedure For the pilot RCT, participants were randomly assigned to either the eTRF, mTRF, or control group in a ratio, using a computer-based random-number generator by designated researchers. Inclusion and exclusion criteria The inclusion criteria were: 1 18—64 years old; 2 ability to attend the hospital at regular intervals; 3 ability to independently provide informed consent; 4 BMI between Anthropometric measurements Body mass and percentage body fat were measured using an HBF Bioelectrical impedance analyzer Omron Healthcare Co.
Blood sampling and storage Blood sampling was performed at the beginning and the end of the trial. Flow cytometric analysis PBMCs were separated from blood samples using Ficoll GE Healthcare, Chicago, IL and centrifugation.
Fecal sample collection and storage Fecal samples were collected during the 3 days before the start of the trial and during the same period of time before the end of the trial. Biochemical measurements The plasma activities of AST, ALT, ALP, GGT, and lactate dehydrogenase; and the concentrations of LDL-C, HDL-C, total cholesterol, triglyceride, and glucose were measured using an automated analyzer Beckmann-Coulter AU , Brea, CA.
Real-time quantitative PCR RNA was pooled from PBMCs and used for cDNA synthesis. Subjective sleep quality and eating habits The participants were required to maintain their normal sleeping habits throughout the trial and to avoid undergoing testing after a night shift. Statistical analysis For the sample size calculation, we estimated that the eTRF group would show a Data availability The individual de-identified participant microbiota metagenomic sequencing data can be accessed from the BioProject Database of National Centre for Biotechnology Information with the dataset accession number PRJNA Code availability No code was involved in this manuscript.
References Seconda, L. Article PubMed Central Google Scholar Kobayashi, T. Article PubMed PubMed Central Google Scholar Sutton, E. Article CAS PubMed PubMed Central Google Scholar Hatori, M.
Article CAS PubMed PubMed Central Google Scholar Ren, J. Article PubMed Google Scholar Woodie, L. Article CAS PubMed Google Scholar Zarrinpar, A. Article CAS PubMed PubMed Central Google Scholar Gabel, K. Article CAS PubMed PubMed Central Google Scholar Gill, S.
Article CAS PubMed PubMed Central Google Scholar Anton, S. CAS PubMed Google Scholar Moro, T. Article PubMed PubMed Central Google Scholar Wilkinson, M. Article CAS PubMed Google Scholar Carlson, O. Article CAS PubMed PubMed Central Google Scholar Parr, E.
Article PubMed Google Scholar Martens, C. Article Google Scholar Madkour, M. Article CAS PubMed Google Scholar Stote, K. Article CAS PubMed Google Scholar Hosono, T. Article CAS PubMed Google Scholar Yoshizaki, T.
Article PubMed Google Scholar Matthews, D. Article CAS Google Scholar Straczkowski, M. Article CAS PubMed Google Scholar Mohammadi, M.
CAS PubMed PubMed Central Google Scholar Apostolakis, S. Article CAS PubMed Google Scholar Huttenhower, C. Article ADS CAS Google Scholar Kato, T. Article PubMed Google Scholar Healey, G.
Article Google Scholar Thomas, D. Article CAS PubMed PubMed Central Google Scholar Lowe, D. Google Scholar Karras, S. Article CAS PubMed Google Scholar Gregor, M. Article CAS PubMed Google Scholar Moro, T. Article Google Scholar Marchesini, G.
Article Google Scholar Briseño-Bass, P. Google Scholar Sherman, H. Article CAS PubMed Google Scholar Sherman, H. Article CAS PubMed PubMed Central Google Scholar Damiola, F. Article CAS PubMed PubMed Central Google Scholar Hara, R.
Article CAS PubMed Google Scholar Satoh, Y. Google Scholar Stokkan, K. Article ADS CAS PubMed Google Scholar Mindikoglu, A. Article PubMed PubMed Central Google Scholar Adawi, M.
Article CAS PubMed Google Scholar Xu, H. Article CAS Google Scholar Wang, B. Article CAS PubMed Google Scholar Feuerer, M. Article CAS PubMed PubMed Central Google Scholar Winer, S. Article CAS PubMed PubMed Central Google Scholar Cignarella, F.
Article CAS PubMed PubMed Central Google Scholar Le Chatelier, E. Article Google Scholar Lucas, R. Article PubMed Google Scholar Kaneko, K. Article CAS PubMed Google Scholar Engin, A. Article CAS PubMed Google Scholar Maeda, N.
Article CAS PubMed Google Scholar Chowdhury, E. Article CAS PubMed PubMed Central Google Scholar Gavrila, A. Article CAS Google Scholar Bray, M. Article CAS Google Scholar Oliver, P.
This is notable as diabetes is particularly prevalent among those groups, so having studies that document the success of time-restricted eating for them is particularly useful, the researchers said. The study was small and should be followed up by larger ones, said Varady, who is also a member of the University of Illinois Cancer Center.
While it acts as a proof of concept to show that time-restricted eating is safe for those with Type 2 diabetes, Varady said people with diabetes should consult their doctors before starting this sort of diet. The other current and former UIC authors on the paper are Vasiliki Pavlou, Sofia Cienfuegos , Shuhao Lin, Mark Ezpeleta, Kathleen Ready, Sarah Corapi, Jackie Wu, Jason Lopez, Kelsey Gabel , Lisa Tussing-Humphreys , Vanessa Oddo , Julienne Sanchez and Dr.
Terry Unterman. Other authors are from Northwestern University, the University of Minnesota, Minneapolis, and the University of Southern California.
Contact Emily Stone emilysto uic. Research , UIC today. diabetes , intermittent fasting , weight loss. Intermittent fasting is safe, effective for those with Type 2 diabetes October 27, Time-restricted eating, also known as intermittent fasting, can help people with Type 2 diabetes lose weight and control their blood sugar levels, according to a new study published in JAMA Network Open from researchers at the University of Illinois Chicago.
Krista Varady. Categories Research , UIC today Topics diabetes , intermittent fasting , weight loss.
Weight loss is an important target for individuals diagnosed with type 2 insupincontroo condition Time-restricted eating for better insulin control linked to insupin weight Timd-restricted obesity ; however, the most Orange Marinade Recipes dietary approach remains btter. In a new study, participants who eatimg their eating to eatin Time-restricted eating for better insulin control window from noon to 8 p. experienced greater weight loss compared to those who simply reduced their overall calorie intake through calorie counting. Time-restricted eating has gained popularity, but prior to this study, no research had specifically explored an eight-hour eating window in individuals with type 2 diabetes. The study involved 75 individuals, ages 18—80 years, who had both obesity and type 2 diabetes and who were divided into three groups: one followed time-restricted eating, another practiced calorie restriction and the third served as the control group. Those in the time-restricted eating group consumed their meals only from noon to 8 p.
Meiner Meinung nach wurde es schon besprochen
Was Sie sagen wollten?
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Aber bald werde ich unbedingt schreiben dass ich denke.