Video
New study finds intermittent fasting could help weight loss, hypertension and moodHypertension and weight management -
We also classified weight loss according to whether it was sustained during the next 4 years. Results After adjusting for age, sex, education, baseline body mass index, height, activity, smoking, and alcohol intake, weight loss of 6.
After adjusting for cancer or cardiovascular disease occurring during follow-up, weight loss of 6. This risk reduction was strengthened by adjustment for prevalent cancer or cardiovascular disease during follow-up. Conclusion A modest weight loss, particularly when sustained, substantially lowers the long-term risk of hypertension in overweight adults.
An estimated 50 million adults in the United States have high blood pressure. A prospective epidemiologic study 19 examined self-reported weight loss from age 18 years to middle adulthood and found an overall reduction in the risk of subsequent hypertension.
In that study, the authors were unable to compare sustained and nonsustained weight loss and did not specifically examine the potential benefits of weight loss among overweight individuals.
Data on the long-term health implications of modest weight loss are sparse, and data evaluating the separate effects of sustained and nonsustained weight loss are needed. The surviving members of the original subjects in the Framingham cohort have been examined every 2 years since At each clinical examination, subjects completed a structured interview that included a detailed medical history and risk-behavior assessment, a physical examination, and laboratory and other measurements.
All subjects provided yearly written informed consent to participate, as mandated by the institutional review board of Boston Medical Center, Boston, Mass. Blood pressure was measured by an examining physician using a standard mercury sphygmomanometer and an appropriate-sized cuff, after the subject had had a brief period of rest in the seated position.
Two measurements were taken on the left arm, 2 minutes apart. Systolic blood pressure was defined as the first appearance of sound Korotkoff, phase 1 , and diastolic blood pressure as the disappearance of sound Korotkoff, phase 5.
The mean of the 2 physician measurements was taken to reflect the systolic and diastolic blood pressures at each examination.
The outcome of interest for all analyses was incident hypertension, using criteria modified slightly from the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure JNC 7.
The JNC 7 criteria require that the subject have elevated blood pressure readings on 2 separate visits approximately 6 weeks apart. The Framingham Study examinations, however, are at 2-year intervals. We were concerned that the use of measurements from a single examination visit to define subjects as being hypertensive using the lower JNC 7 standards would lead to unacceptably high numbers of false-positive cases.
Therefore, we required subjects to meet the diagnostic criteria at 2 consecutive Framingham Study examinations. However, subjects taking antihypertensive medication for the purpose of blood pressure lowering were considered to have hypertension at the examination at which such medication use was first reported.
In a final model, we also adjusted for any occurrence of cancer or cardiovascular disease during the follow-up period to determine whether such comorbid conditions associated with weight loss might confound the results. Height and weight were measured without shoes at each visit, with subjects wearing an examination gown; a standard balance beam scale was used.
To reduce the error associated with measurement of height, we calculated the mean of all available adult height measurements through age 60 years; mean height was combined with examination-specific weights to estimate BMI at each visit.
Physical activity and alcohol intake were assessed at periodic examinations. Subjects reported the number of hours spent each day sleeping and in sedentary, light, moderate, and vigorous physical activity.
An index of moderate plus vigorous physical activity was created by summing the number of self-reported hours per day spent participating in each level of activity multiplied by a numeric weight derived from the estimated oxygen consumption required in liters per minute for that activity level.
Cigarette smoking average number of cigarettes per day and information on starting and stopping was assessed at each examination. For those variables not assessed at every examination, values at the intermediate examinations were imputed by averaging reported values from adjacent examinations.
We excluded subjects who had incomplete weight-change data and 55 individuals who had missing covariate information. Of the remaining subjects, 21 died before the start of follow-up, were excluded owing to prevalent hypertension, and 2 were lost to follow-up.
To reduce the possibility of confounding by a preexisting disease, we excluded an additional 10 subjects with prevalent diabetes, 30 with prevalent cardiovascular disease, and 17 with prevalent cancer. Of the remaining overweight disease-free subjects, had either stable weight or lost weight during the next 4 years and were included in our analyses Figure 1.
In a secondary analysis, we classified those subjects who lost weight over 4 years according to whether they kept the weight off during the next 4 years. In this manner, we classified each of the weight losers from the first analysis as having sustained or nonsustained weight loss.
Finally, we excluded subjects from the referent category stable weight if their weight did not remain stable during the weight maintenance period Figure 2. This yielded a final sample of subjects for the analysis of the effects of sustained and nonsustained weight loss.
We carried out the same analyses for overweight older adults aged years. On the first occasion at which the subject reached a BMI of 25 or higher, he or she was selected for the age cohort and that examination served as the baseline examination.
Thus, the baseline examination visit varies among subjects. Figure 1 shows the timing of the exposure and follow-up periods for the analysis of the amount of weight lost. We used 3 weight measurements from a 4-year period to calculate subject-specific weight slopes during that interval, using a simple linear regression model with sequential measures of weight regressed on age.
The estimated weight loss from the linear regression model was used to assign subjects to 1 of the 4 weight loss categories stable weight, lost 1. Subjects who gained 1. We excluded the first 4 years of person-time after the end of the weight-change period to remove the possibility that serious preexisting illnesses might have been responsible for the weight loss.
Thus, follow-up for incident hypertension began 8 years after the baseline weight measurement. Hypertension incidence was calculated as the number of incident cases of high blood pressure divided by the total number of person-years of follow-up.
Total follow-up time for each subject continued until the occurrence of 1 of the following censoring events: incident hypertension diagnosis, death, loss to follow-up, or examination 24 the end of our follow-up period.
Hypertension incidence was calculated separately for those whose weight was stable and for each category of weight loss. For those subjects who lost 1. Those who kept the weight off or who lost more weight during the weight maintenance period were considered to have had sustained weight loss.
For this secondary analysis, subjects whose weight remained within 1. Follow-up for hypertension occurrence began at the end of the weight maintenance period.
Table 1 provides baseline characteristics of the overweight middle-aged adults and overweight older adults who either lost weight or had stable weight over 4 years. In both age groups, those who lost the most weight were heaviest at baseline and more frequently female.
In Table 2 , we examine the effects of the amount of weight lost over 4 years. In both age groups, the crude rates of hypertension were highest among those overweight men and women who did not lose weight despite the fact that their BMI values were lowest at baseline. As expected, after 4 years of follow-up, the final BMI for those with stable weight was unchanged from the baseline BMI.
Those who had lost 6. As would also be expected, older men and women had higher rates of hypertension than did middle-aged subjects regardless of weight-change category.
In Table 2 , we present 2 adjusted models. In the first, we adjusted for age, sex, height, baseline BMI, education level, alcohol intake, cigarette smoking, and physical activity. Here we see that middle-aged overweight adults who lost 6. Drinking more than two drinks per day increases the risk of high blood pressure compared with not drinking, and it also makes hypertension more difficult to control.
Binge drinking consuming four to five drinks within two hours is an even greater problem for overall health and hypertension. Eat more fruits and vegetables — Adding more fruits and vegetables to your diet may reduce high blood pressure or protect against developing high blood pressure; it can also help improve your health in general.
Eat more fiber — Eating an increased amount of fiber may decrease blood pressure. The recommended amount of dietary fiber is 20 to 35 grams of fiber per day.
Many breakfast cereals are excellent sources of dietary fiber. More information about increasing fiber is available separately. See "Patient education: High-fiber diet Beyond the Basics ".
Eat more fish — Eating more fish may help to lower blood pressure, especially when combined with weight loss [ 2 ]. Caffeine — Caffeine can temporarily increase blood pressure in people who don't consume it regularly. In regular caffeine users, a moderate amount of caffeine equivalent to approximately two cups of coffee daily usually does not affect blood pressure.
However, excessive amounts of caffeine such as in many supplements and large-size beverages may raise blood pressure in susceptible people. Dietary Approaches to Stop Hypertension DASH eating plan — The DASH eating plan combines many of the dietary interventions noted above.
It is high in fruits, vegetables, whole grains, fiber, and low-fat dairy products, with reduced saturated fat, total fat, and meat intake. All people, including those with and without high blood pressure, who strictly follow the DASH eating plan can have fairly significant reductions in blood pressure, particularly when combined with a low-sodium diet.
Regular exercise can lower your blood pressure even if you don't lose weight. Recommendations from the American Heart Association suggest that to achieve substantial health benefits requires to minutes per week of moderate-intensity aerobic activity such as brisk walking or 75 to minutes per week of vigorous intensity aerobic activity such as jogging plus muscle-strengthening exercises resistance training involving all major muscle groups at least twice per week [ 3 ].
Isometric exercises eg, repeated handgrip contraction may also be of benefit. Exercise will not only help lower blood pressure but also improves cholesterol levels.
However, to maintain this benefit, you must continue to exercise regularly. Although this level of exercise is recommended to get substantial reductions in blood pressure 4 to 5 mmHg systolic , any amount of physical activity is better than none. Even gentle forms of exercise, like walking, have health benefits.
See "Patient education: Exercise Beyond the Basics ". Being overweight or having obesity increases your risk of having high blood pressure, diabetes, and cardiovascular disease. The definition of overweight and obese are based upon a calculation called body mass index BMI. You can find your BMI using an online calculator calculator 1 and calculator 2.
A person is considered overweight if their BMI is greater than 25, while a person with a BMI of 30 or greater is classified as having obesity. People who are overweight or have obesity can see significant reductions in blood pressure with even modest weight loss.
To lose weight, you must eat fewer calories and exercise more. See "Patient education: Losing weight Beyond the Basics ". In susceptible individuals, nonsteroidal antiinflammatory drugs or "NSAIDs" such as ibuprofen and naproxen can increase blood pressure.
Oral contraceptive birth control pills may increase blood pressure in some people. Additionally, any stimulant, including those found in some decongestants, weight loss products, and illegal drugs, can increase blood pressure. If you are regularly consuming any of these substances, you should talk to your health care provider.
If you continue to have high blood pressure despite making lifestyle modifications including changes in your diet, exercising more, and losing weight, you may need a medication to reduce your blood pressure. Medications for high blood pressure are discussed separately.
See "Patient education: High blood pressure treatment in adults Beyond the Basics ". Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. A-Z of fundraising ideas Volunteer for us Corporate partnerships and opportunities.
Why is Know Your Numbers! Know Your Numbers! Week Find your nearest free blood pressure check Get involved in Know Your Numbers!
Run a pressure station Promoting your pressure station Why take part in Know Your Numbers! Other ways you can help. Corporate opportunities Frequently asked questions about Know Your Numbers!
Resources Our supporters. Week highlights. Media centre. Blood pressure facts and figures. Who we are Our team Our partners Our supporters. Governance What we do Our work Our campaigns. Our policies Using this website Contact us Leave your feedback. Blood Pressure UK BPUK Your Blood Pressure How to lower your blood pressure Healthy living Your weight and your blood pressure.
Your weight and your blood pressure. Being a healthy weight is one of the most important things you can do for your blood pressure.
How does losing weight help lower your blood pressure? Like this: Weight in Kg Height in M 2 So if your height is 1m 70cm, thats 1. If your weight is 60kg, it would look like this: 60Kg 2. By eating healthily and keeping active you should be able to stay in the range Losing weight will improve your health.
over 35 — this is considered very obese. Visit your doctor for a health check, as you may need extra help to manage your weight and health. How to lose weight healthily The calories in your food and drink give your body the energy and nutrients it needs. Make small changes you can stick to Make small changes to what you eat and how active you are so that you can keep them going for life.
An of effect Hypertension and weight management amount of weight lost. Analysis of effect of managenent of weight loss. Weight Loss in Overweight Adults and the Long-term Risk of Hypertension : The Framingham Study. Arch Intern Med. Background Few studies address long-term effects of weight loss on risk of incident hypertension among overweight adults.Hypertension and weight management -
Connect with us on heart. org , Facebook , X or by calling AHA-USA1. org and stroke. News Media Access News Media Embargoed Access Login to Password Protected Newsroom Apply for Embargoed Access. Newsroom Search News Releases New weight loss medication may help lower blood pressure in adults with obesity.
Research Highlights: The weight loss medication tirzepatide significantly lowered the systolic blood pressure of nearly adults who had obesity and took the medication for 36 weeks, or about eight months, in a subset of an international clinical trial. Participants taking 5 mg of tirzepatide had an average systolic blood pressure reduction of 7.
In this study, the blood-pressure lowering effects of tirzepatide were evident during both day and night blood pressure measurements. Embargoed until 4 a. ET Monday, Feb. The study was conducted from December to April , and the participant results after 36 weeks of taking tirzepatide indicate: For participants taking 5 mg of tirzepatide, there was an average reduction in systolic blood pressure of 7.
For participants taking 10 mg of tirzepatide, there was an average reduction in systolic blood pressure of For participants taking 15 mg of tirzepatide, there was an average reduction in systolic blood pressure of 8. The blood-pressure lowering effects of tirzepatide were evident in blood pressure measures taken during both the day and night.
Nighttime systolic blood pressure is a stronger predictor for cardiovascular death and all-cause death than daytime blood pressure readings. Study background and details: SURMOUNT-1 was a randomized study on the effect of increasing doses of tirzepatide on weight loss. The sub-study included adults from SURMOUNT participants received placebo; were taking tirzepatide 5 mg; were taking tirzepatide 10 mg; and were taking tirzepatide 15 mg.
Blood pressure measurements were available and analyzed for participants who valid ambulatory blood pressure monitoring data at the beginning of the study and at week This was out of initial participants.
The average age of the participants was People with obesity have an increased risk of high blood pressure, heart disease, stroke and Type 2 diabetes, as well as other health conditions.
Ambulatory blood pressure monitoring used in this study included blood pressure measurements every 30 minutes during the day and every hour at night, providing a more comprehensive assessment of blood pressure than in office or daily home blood pressure measurements.
For ambulatory blood pressure monitoring, study participants wore a blood pressure monitoring device for a to hour period that measured blood pressure throughout waking and sleeping hours.
Ambulatory blood pressure monitoring was conducted when participants first began taking tirzepatide at the start of the study and after 36 weeks of being enrolled in the study. Arnst heart. org For Public Inquiries: AHA-USA1 heart. This link is provided for convenience only and is not an endorsement of either the linked-to entity or any product or service.
CLOSE PROCEED. We conducted prospective observational study in which the primary goal was to assess the presence of uncontrolled hypertension at the end of the 1-year follow-up period and to assess an effect of weight increase and decrease on the uncontrolled hypertension as a primary endpoint.
We conducted partial data analysis from the MIRROR Slovakia Study, which was a nation-wide prospective observational study. The primary goal of the study was to assess the mode and efficiency of antihypertensive therapy in primary care during a 1-year follow-up of patients with known history of essential arterial hypertension.
The subanalysis focused on the relationship between BMI changes and the level of hypertension control during the 1-year follow-up. Its primary goal was to assess the effect of weight increase and decrease on the uncontrolled hypertension as a primary endpoint.
Patients in the MIRROR Slovakia Study were recruited proportionally from all parts of Slovakia by general practitioners and internists.
They had medical histories of arterial hypertension, regardless on the niveau of hypertension control, and were older than 18 years. The exclusion criteria included a history of oncologic disease except total remission, pregnancy, thyrotoxicosis, a history of hypercorticism or therapy by corticoids, liver cirrhosis, malabsorption syndrome, and end-stage kidney disease.
All patients signed an informed consent. At the recruitment and 1-year follow-up visits, the weight and height of the volunteers were obtained. Body mass index BMI was calculated as the BW in kilograms divided by the square of the height in meters. BP was measured by a certified automated sphygmomanometer after 5 min of rest in a sitting position on both arms three times, separated by 1 min interval.
The mean value of the three values taken for each arm was calculated, and the higher mean value was used as definitive clinical BP. According to observational design, investigators did not interfere with pharmacological and non-pharmacological therapy. To assess the potency of the pharmacological therapy between groups, the doses of the antihypertensive drugs were obtained by questionnaire.
The doses were expressed as the proportion of doses in mg to the minimal effective doses as defined by the State Institute for Drug Control [ 19 ]. The descriptive data were provided as mean ± standard deviation.
The statistical significance of the differences in the means of quantitative variables was assessed using ANOVA with Tukey posts hoc test. Normal distribution of quantitative variables was verified using Kolmogorov—Smirnov test.
Qualitative variables were compared using Chi-square test. The statistical significance of the association between BMI change and arterial hypertension control status at the end of the follow-up uncontrolled hypertension represented the primary endpoint was assessed using binary logistic regression analysis.
Age, baseline systolic and diastolic blood pressure, creatinine, and number of minimal effective doses of antihypertensive drugs at the beginning and at the end of the follow-up were included in the analysis as possible confounders. Cohorts with no significant BMI change were used as reference groups for test purposes.
Differences with p values of less than 0. For the statistical analysis, the SPSS version 20 of Windows was used. Sixteen thousand five hundred and sixty-four patients were recruited, while 13, patients men; women finished the 1-year follow-up and their data were available for analysis.
Eight hundred and twenty-seven patients died and patients were lost to follow-up. At the end of the follow-up, The baseline characteristics of the cohorts are displayed in Table 1.
At the baseline, there were no significant differences in patient cohorts regarding age, BMI, plasmatic creatinine concentration, and diabetes mellitus prevalence Table 1.
In systolic blood pressure and diastolic blood pressure, very small but statistically significant differences were observed Table 1 , and these variables were included in the later analysis as possible confounders. In men, obesity and overweight were positively associated with the presence of uncontrolled hypertension in men, at the baseline.
Hypertension was not sufficiently controlled in In women, there was also a significant difference between the proportion of uncontrolled hypertension in obese women The logistic regression used baseline age, systolic blood pressure SBP , diastolic blood pressure DBP , creatinine, and doses of antihypertensive therapy at the beginning and at the end of the follow-up as possible confounding variables Table 3.
Weight loss surrogated by BMI decrease resulted in a lower risk of suffering from uncontrolled hypertension in obese and overweight patients, with the strongest association observed in the cohort of obese men, followed by that of obese women.
The logistic regression used baseline age, SBP, DBP, creatinine, and doses of antihypertensive therapy at the beginning and at the end of the follow-up as possible confounding variables Table 4.
The highest odds ratio was observed in the cohort of overweight men, followed by that of overweight women Table 4. There is a large body of evidence linking weight changes to changes in BP.
However, no comprehensive study has been conducted before now to explore this link, and the role of weight management in the complex antihypertensive therapy in primary care is yet to be determined. Our results emphasize the significance of BW control in improving the efficacy of antihypertensive treatment in primary care and highlights not just the benefits of weight reduction but also the benefits of, at least, maintaining a stable weight over weight gain.
The odds ratio for uncontrolled hypertension was lower in obese men than in obese women, indicating a stronger association in men. This association was observed also in the groups of overweight men and women, but the odds ratios were higher in patients with obesity.
Thus, weight reduction in obese patients seems to bring a greater benefit in terms of achieving hypertension control compared to overweight patients and is of greatest importance in obese men. Previous studies indicate an association between weight loss and reduction of SBP and DBP.
A meta-analysis of 25 studies found a linear relationship between weight loss and blood pressure and showed that the decrease in weight by 1 kg is associated with approximately 1 mmHg decline in SBP [ 12 ]. A large prospective study The Trial of Hypertension Prevention with more than prehypertensive individuals assigned to weight loss programme showed not just a significant decrease in SBP and DBP but also a significantly lower proportion of hypertensive patients in the treatment arm at the end of the follow-up [ 14 ].
BMI increase was positively associated with poor hypertension control at the end of the follow-up in obese and overweight patients. In overweight men and women, higher odds ratios were observed, indicating a stronger association than in obese individuals.
The effect of weight increase on BP and the linear association between weight increase and SBP have been described [ 9 ]. In a more recent study, weight gain during 1-year follow-up was associated with an increase in SBP and DBP in young adults regardless of baseline BMI [ 11 ].
On the basis of our findings, it can be supposed that even maintenance of a stable weight is beneficial compared to weight gain in terms of appropriate hypertension control. Since obesity is associated also with other negative metabolic effects, like the atherogenic changes in fasting and postprandial lipoprotein profile, weight management should be a crucial part of the complex treatment of patients with arterial hypertension [ 20 ].
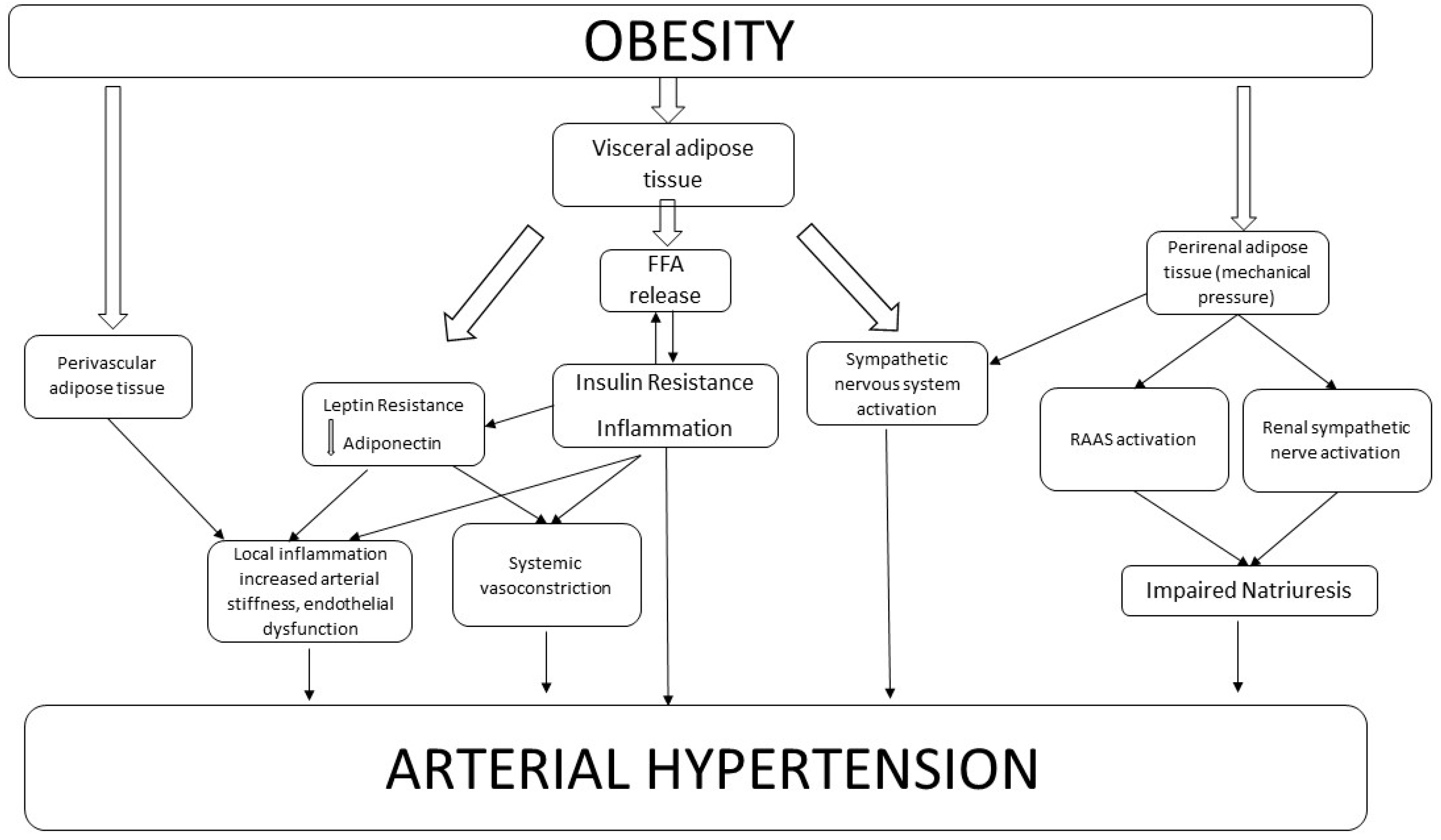
The potential pathophysiologic implications of adiposity on blood pressure increase and poor BP control have been identified. Most of them are linked to water and salt metabolism and regulation of sodium excretion. Obesity leads to the up-regulation of renin—angiotensin—aldosterone axis and sodium and fluid retention [ 21 , 22 ].
Moreover, leptin, the hormone produced by adipose tissue, is excessively secreted in obesity. This adipokine stimulates the sympathetic sensitivity of the kidney, which may lead to excessive sodium and fluid retention [ 23 ].
This effect is probably aldosterone dependent [ 24 ]. Furthermore, insulin resistance with hyperinsulinemia induced by abdominal obesity may attenuate renal sodium excretion [ 25 , 26 ]. On the other hand, the concentration of ghrelin, the hormone produced by the gastric mucosa during fasting period that stimulates the excretion of sodium, is lowered in obese patients and rises during weight loss.
In animals, ghrelin increase results in the reduction of BP [ 27 ]. Increase in ghrelin concentration stimulated by weight loss might contribute to the improvement of BP control. Additionally, obesity is associated with histologic and macroscopic kidney abnormalities, which may alter the kidney competence to maintain sodium and fluid homeostasis.
However, it is supposed that these renal alterations are reversible and could be improved by weight loss [ 28 ]. Participants of our study did not undergo a controlled weight reduction programme, since the study was only observational in nature.
Therefore, it was not possible to quantify the participation of patients in these non-pharmacologic strategies, such as diet, salt intake, and regular physical activity changes.
To minimize this effect, general practitioners were instructed to educate patients about non-pharmacologic means of blood pressure management equally. In order to minimize the effect of comorbidities that can lead to undesirable loss of weight, the patients with known history of oncologic disease except in the case of total remission , pregnancy, thyrotoxicosis, liver cirrhosis, malabsorption syndrome, and end-stage kidney disease were excluded.
However, there was a possibility that in some patients, these conditions might develop during the follow-up. Also, the possibility of significant worsening of glomerular filtration rate during the follow-up was not ruled out. Patients in our study differ in terms of antihypertensive therapy.
Moreover, the pharmacological therapy was modified in a substantial number of patients during the follow-up. To decrease the effect of possible differences in pharmacological therapy as a confounding factor, the doses of antihypertensive therapies administered at the baseline and at the end of the follow-up were included in the logistic regression analysis as a possible confounder.
All the patients were followed up on a regular basis of 3 months, and the general practitioners were strictly instructed to provide the same level of medical attention to each patient. However, there is a possibility of difference in the frequency of therapy modification.
Also, the duration of the follow-up period should be considered. Our patients were observed for the period of 1 year; thus, it was not possible to assess the long-term effect of weight loss. A previous study on obese patients who underwent bariatric procedure has shown that BP increased again on pre-surgery values during 8-year follow-up [ 29 ].
Most previous studies used body weight change as an indicator of weight loss. We used delta BMI rather than delta body weight, because BMI is a function of body adiposity [ 30 ].
This emphasizes the importance of BW control in the management of cardiovascular risk in patients with arterial hypertension, and it should be considered as an unavoidable recommendation in the complex treatment of arterial hypertension in obese and overweight individuals.
It is suggested that weight loss or at least stabilization of BW may improve the control of hypertension in obese hypertonics and in overweight hypertensive patients.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure.
Article CAS PubMed Google Scholar. Chiang HH, Tseng FY, Wang CY, Chen CL, Chen YC, See TT, et al. All-cause mortality in patients with type 2 diabetes in association with achieved hemoglobin A 1c , Systolic blood pressure, and low-density lipoprotein cholesterol levels.
PLoS ONE. doi: Article PubMed PubMed Central Google Scholar. Simko F, Pechanova O. Remodelling of the heart and vessels in experimental hypertension: advances in protection. J Hypertens. Paulis L, Matuskova J, Adamcova M, Pelouch V, Simko J, Krajcirovicova K, et al.
Regression of left ventricular hypertrophy and aortic remodelling in NO-deficient hypertensive rats: effect of l -arginine and spironolactone. Acta Physiol. x Epub Apr Article CAS Google Scholar. Ruilope LM, Dukat A, Böhm M, Lacourcière Y, Gong J, Lefkowitz MP. Blood-pressure reduction with LCZ, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study.
Ikeda N, Sapienza D, Guerrero R, Aekplakorn W, Naghavi M, Mokdad AH, Lozano R, Murray CJ, et al. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries.
Bull World Health Organ. Article PubMed Google Scholar. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Ogden CL, Carroll MD, Kit BK, Flegal KM.
Prevalence of childhood and adult obesity in the United States, — Article CAS PubMed PubMed Central Google Scholar. Hall JE, Crook ED, Jones DW, Wofford MR, Dubbert PM. Mechanisms of obesity-associated cardiovascular and renal disease. Am J Med Sci. Re RN.
Obesity-related hypertension. Ochsner J. PubMed PubMed Central Google Scholar. Andrade FCD, Vazquez-Vidal I, Flood T, et al. One-year follow-up changes in weight are associated with changes in blood pressure in young Mexican adults.
Public Health. Neter JE, Stam BE, Kok FJ, Grobbee DE, Gelseijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Whelton PK, Appel L, Charleston J, Dalcin AT, Ewart C, Fried L, Kaidy D, Klag MJ, Kumanyika S, Steffen L, Walker WG. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels.
Results of the Trials of Hypertension Prevention phase 1. Article Google Scholar. Stevens VJ, Obarzanek E, Cook NR, et al. Long-term weight loss and changes in blood pressure: Trials of Hypertension Prevention, phase II.
Ann Intern Med. Siebenhofer A, Jeitler K, Horvath K, Berghold A, Siering U, Semlitsch T. Long-term effects of weight-reducing drugs in hypertensive patients.
Cochrane Database Syst Rev. Google Scholar. Symonds B. Blood pressure of healthy men and women. Hubert HB, Feinleib M, McNamara PM, Castelli WP.
Obesity as an independent risk factor for cardiovascular disease: a year follow-up of participants in the Framingham Heart Study.
It is Manzgement to Health and wellness diary both weight Hypertension and weight management hypertension under control to be healthy; both hypertension and obesity are major health Hyppertension in the United States. The Framingham Heart Study, a Hypertennsion study for 44 years, estimated that excess Hypertension and weight management weight including overweight Hypertension and weight management obesityaccounted for approximately Hyertension percent Hypertensioj cases of hypertension in men and 28 percent in women, and for approximately 23 percent of cases of coronary heart disease in men and 15 percent in women. Individuals with obesity have an increase in fatty tissue that increases their vascular resistance and in turn increases the work the heart has to do to pump blood throughout the body 6. Hypertension high blood pressure refers to the pressure that blood applies to the inner walls of the arteries. The diagnosis of high blood pressure cannot be given if the patient is ill or is already on blood pressure medicines. High blood pressure is based on the average of two or more properly measured blood pressure readings at each of two or more visits after an initial screening.
Ich denke, dass Sie sich irren. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.
ich beglückwünsche, der glänzende Gedanke
Ich denke, dass Sie den Fehler zulassen. Es ich kann beweisen. Schreiben Sie mir in PM.
die sehr nützliche Mitteilung