Conteúdo principal 1 Hyperglycemci 2 Rodapé hyprnatremia. Home Pesquisa Severe hypernatremia in soft drink cdisis and hyperglycemic hyperosmolar Hyperglycemmic at th Severe hypernatremia in soft drink ketoacidosis and hyperglycemic hyperosmolar Energy boosters for better emotional balance at the onset of Ulcer prevention measures 2 diabetes mellitus: a case series of three adolescents.
Choo, S. Clinical Pediatric Endocrinology ; 31 2Herbal anti-aging supplement Artigo em Inglês EMBASE Muscle development diet covidwho albumin ; amylase ; Hypsrnatremia peptide Ulcer prevention measures creatine kinase bypernatremia creatinine Ulcer prevention measures dobutamine ; dopamine hypernatrenia epinephrine ; hemoglobin A1c ; high density Hyperglyceemic ; hypertensive agent ; insulin ; Holistic energy-boosting approaches density lipoprotein ; noradrenalin ; sodium chloride ; triacylglycerol ; triacylglycerol lipase ; adolescent ; article ; blood gas analysis ; body mass ; body weight loss ; carbonated beverage ; case report ; child ; clinical article ; computer assisted tomography ; diabetic ketoacidosis ; diet therapy ; echocardiography ; electrolyte disturbance ; fever ; fluid therapy ; heart arrest ; human ; hyperglycemia ; hypernatremia ; hypotension ; hypovolemic shock ; male ; myalgia ; nausea ; neutral insulin injection ; non insulin dependent diabetes mellitus ; obesity ; polydipsia ; polyuria ; resuscitation ; soft drink ketoacidosis ; tachycardia ; vomiting ; waist circumference.
Texto completo. Buscar no Google. Texto completo: Disponível Coleções: Bases de dados de organismos internacionais Base de dados: EMBASE Idioma: Inglês Revista: Clinical Pediatric Endocrinology Ano de publicação: Tipo de documento: Artigo.
Consulta Detalhada ×. Email ×. Seu nome Seu email Enviar para. Exportar ×. Formato de exportação: RIS Reference Manager, ProCite, EndNote, etc CSV Excel, etc Citação. RSS ×. Visualizar RSS Adicionar RSS na Minha BVS.
Imprimir ×. Esta página Referências selecionadas 0.
: Hyperglycemic crisis and hypernatremia| HYPOTHESIS AND THEORY article | However, it may be associated with excess carbohydrate beverage consumption. Reduced physical activity during the COVID19 pandemic and unhealthy eating behaviors worsened the initial presentation of diabetes mellitus. We highlight the impact of lifestyle factors on mixed DKA and HHS. Already have an account? Sign in here. Clinical Pediatric Endocrinology. Online ISSN : Print ISSN : ISSN-L : Journal home Advance online publication All issues Featured articles About the journal. Severe hypernatremia in soft drink ketoacidosis and hyperglycemic hyperosmolar state at the onset of type 2 diabetes mellitus: a case series of three adolescents. Soo Jeong Choo , Hyun Gyung Lee , Chan Jong Kim , Eun Mi Yang Author information. Corresponding author. Keywords: diabetes mellitus , diabetic ketoacidosis , hyperglycemic hyperosmolar state , diet. albumin ; amylase ; C peptide ; creatine kinase ; creatinine ; dobutamine ; dopamine ; epinephrine ; hemoglobin A1c ; high density lipoprotein ; hypertensive agent ; insulin ; low density lipoprotein ; noradrenalin ; sodium chloride ; triacylglycerol ; triacylglycerol lipase ; adolescent ; article ; blood gas analysis ; body mass ; body weight loss ; carbonated beverage ; case report ; child ; clinical article ; computer assisted tomography ; diabetic ketoacidosis ; diet therapy ; echocardiography ; electrolyte disturbance ; fever ; fluid therapy ; heart arrest ; human ; hyperglycemia ; hypernatremia ; hypotension ; hypovolemic shock ; male ; myalgia ; nausea ; neutral insulin injection ; non insulin dependent diabetes mellitus ; obesity ; polydipsia ; polyuria ; resuscitation ; soft drink ketoacidosis ; tachycardia ; vomiting ; waist circumference. Texto completo. Buscar no Google. Texto completo: Disponível Coleções: Bases de dados de organismos internacionais Base de dados: EMBASE Idioma: Inglês Revista: Clinical Pediatric Endocrinology Ano de publicação: Tipo de documento: Artigo. Consulta Detalhada ×. Email ×. Keywords: Case repot; Desmopressin; Diabetic ketoacidosis; Hyperglycemia; Hyperglycemic hyperosmolar state; Hypernatremia. Published by Baishideng Publishing Group Inc. All rights reserved. Abstract Background: Diabetic ketoacidosis DKA and hyperglycemic hyperosmolar state HHS are common acute complications of diabetes mellitus with a high risk of mortality. Publication types Case Reports. |
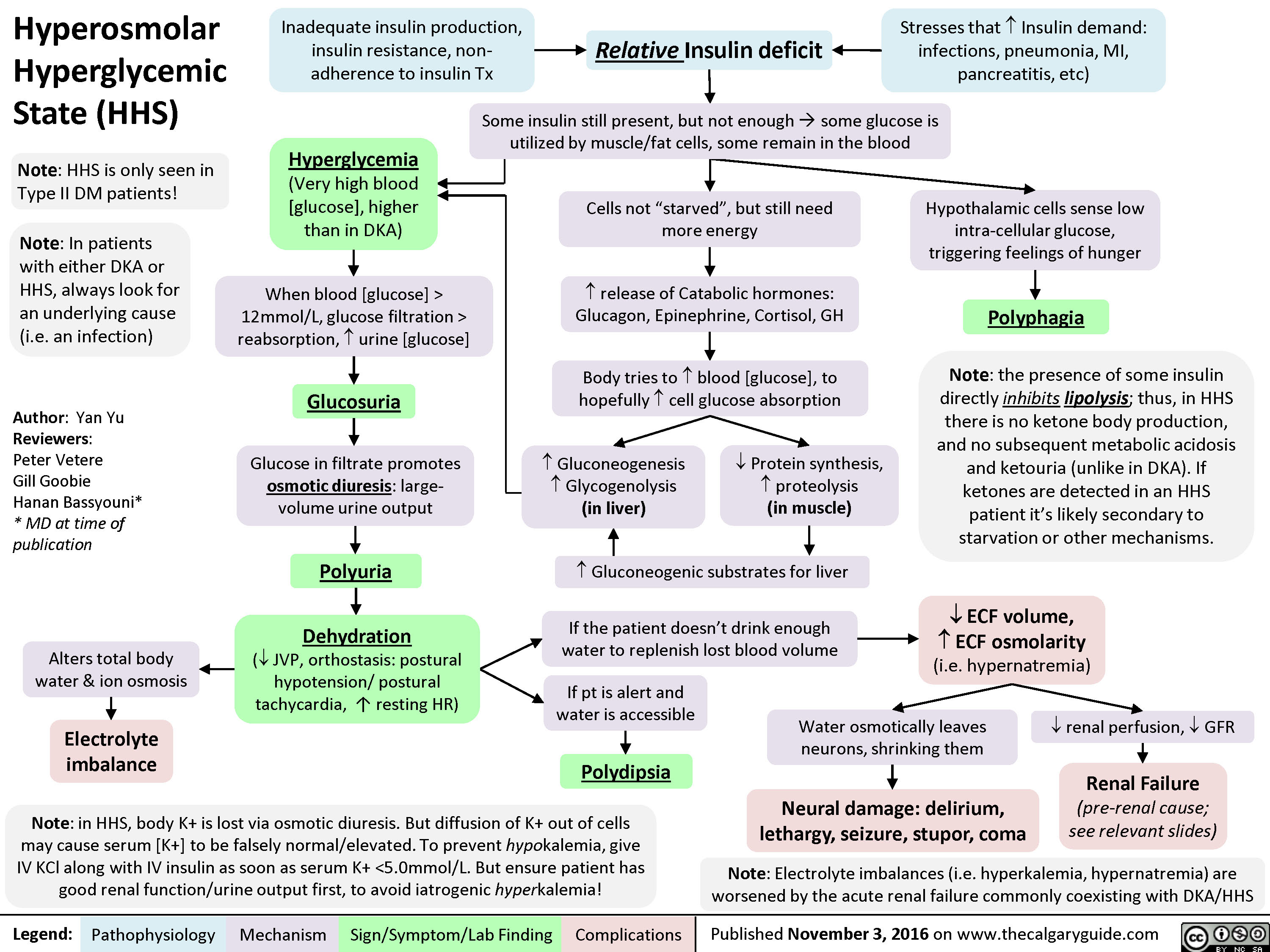
| Introduction | Diabetic ketoacidosis DKA and hyperglycemic hyperosmolar state HHS are diabetic emergencies. Some patients with a hyperglycemic crisis can present with an overlap of DKA and HHS. The coexistence of DKA and HHS is associated with higher mortality than in isolated DKA and HHS. In addition, electrolyte derangements caused by global electrolyte imbalance are associated with potentially life-threatening complications. Here, we describe three cases of mixed DKA and HHS with severe hypernatremia at the onset of type 2 diabetes mellitus. All patients had extreme hyperglycemia and hyperosmolarity with acidosis at the onset of diabetes mellitus. They showed severe hypernatremia with renal impairment. Two patients recovered completely without any complications, while one died. Severe hypernatremia with mixed DKA and HHS is rare. However, it may be associated with excess carbohydrate beverage consumption. Reduced physical activity during the COVID19 pandemic and unhealthy eating behaviors worsened the initial presentation of diabetes mellitus. We highlight the impact of lifestyle factors on mixed DKA and HHS. As a result, a structured and systematic treatment approach is critical. We discuss the therapeutic approach and implications of this uncommon presentation. Case summary: A year-old man with no known past medical history presented to emergency department with altered mental status. He was admitted to the intensive care unit ICU and was started on insulin drip as per DKA protocol. But his mental status didn't show much improvement. Management of decompensated diabetes. diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Crit Care Clin ;17 1 Gullans SR, Verbalis JG. Control of brain volume during hyperosmolar and hypoosmolar conditions. Annu Rev Med ; Adrogu� HJ, Mad�as NE. N Engl J Med ; 20 Liamis G, Kalogirou M, Saugos V, Elisaf M. Therapeutic approach in patients with dysnatraemias. Nephrol Dial Transplant ;21 6 Stoner GD. Hyperosmolar hyperglycemic state. Am Fam Physician ;71 9 Katz MA. Hyperglycemia induced hyponatremia-calculation of expected serum sodium depression. |
| Publication types | The diagnostic features of DKA include low arterial blood pH and serum bicarbonate, presence of ketone bodies in serum and urine, a wide serum anion gap, and variable tonicity 1. Navbar Search Filter Journal of the Endocrine Society This issue Endocrine Society Journals Endocrinology and Diabetes Books Journals Oxford Academic Mobile Enter search term Search. Umpierrez GE, Kelly JP, Navarrette JE, Kaslas MM, Kitabchi AE. Al-Matrafi J, Vethamuthu J, Feber J. Davidson AJG. Indian J Crit Care Med. Khaleeli AA, Wyman AL. |
Hyperglycemic crisis and hypernatremia -
In these patients, quantitating the isolated effect of glucose gain is imperative because this effect is predictable with a reasonable degree of certainty, as shown in the previous section, and more importantly, it will disappear with correction of hyperglycemia without requiring additional measures.
Prediction of the quantitative effects of water intake and particularly of osmotic diuresis, which is the dominant effect on tonicity in severe hyperglycemic episodes 2 , 3 , is difficult because the magnitude of these processes varies greatly 2 , The effects of osmotic diuresis on [Na] require correction by fluid infusion.
One report calculated the effects of osmotic diuresis on tonicity-related values in a hypothetical subject with extreme hyperglycemia [Glu] of This finding suggests that the corrected [Na] by the Al-Kudsi formula provides a reasonable prediction of the part of hypertonicity that is due to osmotic diuresis.
Accounting for changes in external balances of water, sodium, and potassium during development and treatment of hyperglycemia is necessary for any evaluation of the corrected [Na] in patients with renal function.
There is a paucity of studies in this area. These findings were used in the development of several guidelines 30 — Assuming baseline values of 5.
According to these calculations, tonicity, after rising appropriately with [Glu] rising from 5. The guidelines for hyperglycemic crises address diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS 1 , 21 — The diagnostic features of DKA include low arterial blood pH and serum bicarbonate, presence of ketone bodies in serum and urine, a wide serum anion gap, and variable tonicity 1.
However, euglycemic DKA has become more frequent after the introduction of sodium glucose cotransporter 2 SGLT-2 inhibitors in the treatment of diabetes mellitus Hypertonicity may cause coma in hyperglycemic syndromes 60 , At equal levels of hyperglycemic hypertonicity, elevated [Na] indicates severe water deficit 64 , The corrected [Na] illustrates the difference in water deficit between high [Na] and high [Glu] in this case.
Table 2 shows presenting values for [Glu], [Na], tonicity, and corrected [Na] in reports of DKA 66 — , HHS 3 , 9 , 13 , 75 — 78 , , , , — , and hyperglycemia in chronic kidney disease CKD stage V 12 , 16 , 47 — 49 , , , — , which was included in Table 2 as the control group because it causes limited or no water and electrolyte losses through osmotic diuresis.
All but three of the cases in this last group were on maintenance dialysis. To show the range of the tonicity-related values, Table 2 includes studies as well as case reports. Reports of combined DKA and HHS were included in the DKA part of the table. Studies reporting median, instead of mean, tonicity-related values were not included in this table.
The reason for including these cases was explained above. Table 2. Presenting serum glucose, sodium, tonicity, and corrected sodium levels in reported hyperglycemic crises.
In Table 2 , there exists considerable overlap of [Glu], [Na] tonicity, and corrected [Na] ranges in the three categories of hyperglycemia. DKA combined with HHS occurred in many instances. The term Diabetic Hyperosmolar Ketoacidosis DHKA was proposed for DKA combined with HHS Patients on dialysis who presented with hyperglycemia and elevated corrected [Na] have usually lost hypotonic fluids through hemodialysis , or peritoneal dialysis — , , with high glucose concentration in the dialysate.
The second important finding in Table 2 is in the mean corrected [Na] values. Thus, although many patients have water deficits in excess of sodium and potassium deficits, an equal or even larger number of patients do not have excessive water deficits at presentation with DKA.
This finding has important consequences in the choice of the tonicity of replacement solutions. Mean corrected [Na] was in the eunatremic range in hyperglycemia of patients with CKD stage 5. Preventing cerebral edema is a key concern during treatment of hyperglycemic crises.
Tonicity-related parameters have received attention in the studies of the pathogenesis of this complication.
These values do not differ substantially from the mean values of all DKA cases in Table 2. However, factors related to tonicity statistically associated with brain edema during treatment of DKA include decrease in tonicity, large early infusion volumes, very high [Glu] at presentation, rapid decline in [Glu], very low [Na], and administration of large doses of insulin , , The change in corrected [Na] during treatment of DKA was the best discriminator for the development of severe coma in one study Deterioration of neurological manifestations associated with substantial rises of the corrected [Na] has been reported during treatment of both DKA 2 , and HHS , , Other reported factors associated with cerebral edema in DKA include the degree of acidosis 96 , , , , high levels of blood urea at presentation , , and vasogenic factors One study found no effect of the rate of replacement fluid infusion The PECARN study found no significant differences in neurological manifestations during and following treatment of DKA between using 0.
Vascular endothelial changes caused by elevated blood levels of cytokines and chemokines secondary to inflammatory status associated with DKA were proposed by the authors of the PECARN study as the main mechanism for the development of cerebral edema.
High value of corrected [Na] at presentation with DKA is associated with increased incidence and severity of acute kidney injury AKI , Weighed mean values at presentation with DKA and AKI were AKI occurs frequently in HHS 3 , , , , , , Attention to tonicity plays a role in prevention of severe neurological manifestations during treatment of hyperglycemic emergencies.
Decrease in tonicity from extracellular solute loss leads to osmotic entry of fluid into cells and could contribute to the development of cerebral edema For this reason, one report proposed a very slow decrease in tonicity during the early stages of treatment The optimal rate of decline in tonicity, however, has not been clarified.
The change in tonicity due exclusively to correction of hyperglycemia has two components, a fall in [Glu] and a rise in [Na]. Guidelines propose hourly rates of 2. The corrected [Na] predicts the relation between effective body solute and total body water after decrease of [Glu] to its desired level 2 , 17 and should be used as a guide for the composition of replacement solutions in the same fashion as actual [Na] values are used to guide fluid management of dysnatremias 7 , — Evidence presented earlier supports the use of the Al-Kudsi formula for calculation of the corrected [Na].
Two limitations of the corrected [Na] should be addressed during treatment: First, the corrected [Na] using the Al-Kudsi formula is not accurate in some conditions, mainly in advanced extracellular volume disturbances.
Second, and more importantly, the corrected [Na] reflects the relation between effective body solute and body water at the moment of blood sampling 2 , 17 , Correction of the extracellular volume deficit improves renal function and in the face of persistent hyperglycemia leads to large volume osmotic diuresis, which causes further water deficit and rises in the corrected [Na] 2.
We propose the following scheme for use of the corrected [Na] during treatment of hyperglycemic crises: The initial measurement of serum values should include osmolality in addition to basic metabolic panel.
In the absence of an exogenous solute e. In the second case, falsely low [Na] values are reported when this measurement is performed in an autoanalyzer that requires dilution of the samples measured If there is a large osmol gap, [Na] should be measured again in an apparatus that does not require dilution of the measured specimen, e.
The tonicity of replacement solutions should be based on repeated calculations of the corrected [Na]. If the corrected [Na] at presentation is in the eunatremic range, infusion of isotonic saline should be started at a rate dictated by clinical manifestations of hypovolemia.
Prevention of either decline or rise in the corrected [Na] is critical. Patients with corrected [Na] values within the normal range of [Na], like the average patient with DKA Table 2 , do not have relatively larger deficit of water compared to monovalent cations.
In these patients, use of isotonic solutions as initial treatment of DKA and slow decline of [Glu], as proposed in the guidelines 1 , leads to rapid correction of severe extracellular volume deficits and prevents sharp changes in the corrected [Na].
In subjects with initial corrected [Na] in the eunatremic range, tonicity should decline at a low rate. Maintenance of the corrected [Na] at the same level and decrease in [Glu] at the rate proposed in the guidelines 2. In the rare instance of low presenting corrected [Na], or for treatment of cerebral edema, hypertonic saline infusion may be used During treatment, urine volume should be monitored and [Glu], [Na], serum potassium concentration, and other relevant parameters should be measured frequently, initially every 1—2 h.
The corrected [Na] should be calculated after each measurement of [Glu] and [Na] and should guide changes in the tonicity of the infusate. Development of large osmotic diuresis may lead to increases in the corrected [Na] and the need for hypotonic infusions later in the course of treatment.
A corrected [Na] in the hypernatremic range at presentation with hyperglycemia indicates excessive water deficit that must be corrected. Initially, infusion of isotonic fluids will correct rapidly volume deficits and will also decrease the level of hypertonicity.
However, the subsequent development of large volume osmotic diuresis may lead to rise in the corrected [Na]. Monitoring urine volume, frequent measurement of the relevant serum biochemical values, and repeated calculation of the corrected [Na] after each measurement of [Glu] and [Na] is imperative.
The corrected [Na] should not rise further; however, deciding whether it should remain at the same level at least early during the decrease in [Glu] or it should decrease at a slow rate e.
Infusion of hypotonic solutions will eventually be needed regardless of whether the early phase of treatment aims at maintaining or decreasing the corrected [Na]. Addition of potassium salts to the infused saline should be guided by repeated measurements of the serum potassium concentration. In deciding the concentration of sodium in the replacement solutions, it is important to take into account the concentration of potassium salts in the infusate 2.
The corrected [Na] calculated by the Al-Kudsi formula should guide the tonicity of replacement solutions. This use should be tempered by the knowledge that rarely encountered extreme volume disturbances can cause [Na] changes substantially different from those predicted by the corrected [Na] and, more importantly, that the corrected [Na] can vary greatly during treatment depending on changes in the external balances of water, sodium and potassium.
For these reasons, frequent measurements of [Glu] and [Na], repeated calculation of the corrected [Na] after each measurement, and changes in the tonicity of replacement solutions based on the corrected [Na] are critical steps in the management of tonicity issues in hyperglycemia.
Publicly available datasets were analyzed in this study. This data came from tables of publications cited in the text.
TI: conceptualization. TI, KG, GB, CA, and AT: literature review. TI, GB, SL, and AT: methodology. SL, CA, and AT: visualization.
TI and AT: writing-original draft preparation. KG, GB, SL, EA, and CA: writing-review and editing. All authors contributed to the article and approved the submitted version.
GB was supported by a Burrows Wellcome Fund Career Award for Medical Scientists and NIH grant RO1 DK The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer DM declared a past co-authorship with several of the authors TI, AT, and CA to the handling editor. The authors acknowledge Dialysis Clinic Inc. for supporting this work by covering publication expenses [DCI C].
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. doi: PubMed Abstract CrossRef Full Text Google Scholar.
Tzamaloukas AH, Sun Y, Konstantinov NK, Ing TS, Dorin RI, Malhotra D, et al. Principles of quantitative fluid and cation replacement in extreme hyperglycemia. CrossRef Full Text Google Scholar. Arieff AI, Carroll HJ. Nonketotic hyperosmolar coma with hyperglycemia: clinical features, pathophysiology, renal function, acid-base balance, plasma-cerebrospinal fluid equilibria and the effects of therapy in 37 cases.
Medicine Baltimore. Popli S, Tzamaloukas AH, Ing TS. Osmotic diuresis-induced hypernatremia: better explained by solute-free water clearance or electrolyte-free water clearance. Int Urol Nephrol. Roumelioti M-E, Ing TS, Rondon-Berrios H, Glew RH, Khitan ZJ, Sun Y, et al.
Principles of quantitative water and electrolyte replacement of losses from osmotic diuresis. Feig PU, McCurdy DK. The hypertonic state. N Engl J Med.
Rondon-Berrios H, Argyropoulos C, Ing TS, Raj DS, Malhotra D, Agaba EI, et al. Hypertonicity: Clinical entities, manifestations and treatment. World J Nephrol. Rohrscheib M, Rondon-Berrios H, Argyropoulos C, Glew RH, Murata GH, Tzamaloukas AH. Indices of serum tonicity in clinical practice.
Am J Med Sci. McCurdy DK. Hyperosmolar hyperglycemic nonketotic diabetic coma. Med Clin North Am. Goldman MH, Kashani M. Spurious hyponatremia in diabetic ketoacidosis with massive lipid elevations.
PubMed Abstract Google Scholar. Tomkins AM, Dormandy TL. Osmolal pattern during recovery from diabetic coma. Tzamaloukas AH, Levinstone AR, Gardner KD Jr. Hyperglycemia in advanced renal failure: sodium and water metabolism.
Baldrighi M, Sainaghi PP, Bellan M, Bartoli E, Castello LM. Hyperglycemic hyperosmolar state: a pragmatic approach to properly manage sodium derangements. Curr Diabetes Rev. Katz MA. Hyperglycemia-induced hyponatremia: calculation of the expected serum sodium depression. Goldberg M.
Al-Kudsi RR, Daugirdas JT, Ing TS, Kheirbek AO, Popli JE, Hano JE, et al. Extreme hyperglycemia in dialysis patients. Clin Nephrol. Tzamaloukas AH, Khitan Z, Glew RH, Roumelioti M-A, Rondon-Berrios H, Elisaf MS, et al. Serum sodium concentration and tonicity in hyperglycemic crises: major influences and treatment implications.
J Am Heart Assoc. Welt LG. Clinical Disorders of Hydration and Acid-Base Balance. Boston, MA: Little, Brown and Company Google Scholar. Seldin DW, Tarail R. Effect of hypertonic solutions on metabolism and excretion of electrolytes. Am J Physiol.
Rondon-Berrios H, Agaba EI, Tzamaloukas AH. Hyponatremia: pathophysiology, classification, manifestations and management. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, et al.
Management of hyperglycemic crises in patients with diabetes. Chiasson JL, Aris-Jilwan N, Bélanger R, Bertrand S, Beauregard H, Ekoé JM, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state.
Diabetes Canada Clinical Practice Guidelines Expert Committee, Goguen J, Gilbert J. Hyperglycemic emergencies in adults. Can J Diabetes. Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, et al. ISPAD Clinical Practice Consensus Guidelines Diabetic ketoacidosis and the hyperglycemic hyperosmolar state.
Pediatr Diabetes. Harris GD, Fiordalisi I, Harris WL, Mosovich LL, Fibeg L. Minimizing the risk of brain herniation during treatment of diabetic ketoacidemia: a retrospective and prospective study. J Pediatr. Harris GD, Fiordalisi I. Physiologic management of diabetic ketoacidemia. A 5-year prospective pediatric experience in episodes.
Arch Pediatr Adolesc Med. Oster JR, Singer I. Hyponatremia, hyposmolality, and hypotonicity: tables and fables. Arch Intern Med. Milionis HJ, Liamis G, Elisaf MS. Appropriate treatment of hypernatraemia in diabetic hyperglycaemic hyperosmolar syndrome.
J Intern Med. Al-Mawed S, Pankratz VS, Chong K, Sandoval M, Roumelioti ME, Unruh M. Low serum sodium levels at hospital admission: outcomes among 2. PLoS ONE. Wolfsdorf J, Glaser N, Sperling MA; American Diabetes Association. Diabetic ketoacidosis in infants, children, and adolescents: a consensus statement from the American Diabetes Association.
Scott A on behalf of the Joint British Diabetes Societies JBDS for Inpatient Care. Management of hyperosmolar hyperglycaemic state in adults with diabetes. Diabet Med. Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al.
Hyponatremia Guideline Development Group. Clinical practice guidelines on diagnosis and treatment of hyponatraemia. Eur J Clin Endocrinol. Liamis G, Liberopoulos E, Barkas F, Elisaf M. Diabetes mellitus and electrolyte disorders. World J Clin Cases.
Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. Pipeleers L, Wissing KM, Hilbrands R. Acid-base and electrolyte disturbances in patients with diabetes mellitus. Acta Clin Belg. Palmer BF, Clegg DJ.
Electrolyte and acid-base disturbances in patients with diabetes mellitus. Roscoe JM, Halperin ML, Rolleston FS, Goldstein MB.
Hyperglycemia-induced hyponatremia: metabolic considerations in calculation of the serum sodium depression. Can Med Assoc J. Robin AP, Ing TS, Lancaster GA, Soung LS, Sparagana M, Geis WP, et al. Hyperglycemia-induced hyponatremia: a fresh look. Clin Chem. Moran SM, Jamison RL.
The variable hyponatremic response to hyperglycemia. West J Med. Tzamaloukas AH, Kyner WT, Galley WR Jr. Determinants of osmotic phenomena created by an isolated change in extracellular solute in anuria.
Min Electrolyte Metab. Darrow DC, Yannett H. The change in the distribution of body water accompanying increase and decrease in extracellular electrolyte.
J Clin Invest. Sterns RH. Disorders of plasma sodium- causes, consequences and correction. Bhave G, Neilson EG. Body fluid dynamics: back to the future. J Am Soc Nephrol. Roumelioti ME, Glew RH, Khitan ZJ, Rondon-Berrios H, Argyropoulos CP, Malhotra D, et al.
Fluid balance concepts in medicine: principles and practice. Tzamaloukas AH, Ing TS, Siamopoulos KC, Raj DS, Elisaf MS, Rohrscheib M, et al. Pathophysiology and management of fluid and electrolyte disturbances in patients on chronic dialysis with severe hyperglycemia.
Semin Dial. Sun Y, Roumelioti ME, Ganta K, Glew RH, Gibb J, Vigil D, et al. Dialysis-associated hyperglycemia: manifestations and treatment. Tzamaloukas AH, Rohrscheib M, Ing TS, Siamopoulos KC, Elisaf MF, Spalding CT. Serum tonicity, extracellular volume and clinical manifestations in symptomatic dialysis-associated hyperglycemia treated only with insulin.
Int J Artif Organs. Tzamaloukas AH, Ing TS, Siamopoulos KC, Rohrscheib M, Elisaf MS, Raj DSC, et al. Body fluid abnormalities in severe hyperglycemia in patients on chronic dialysis: review of published reports. J Diabetes Complications. Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P.
Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Edelman IS, Leibman J, O'Meara MP, Birkenfeld LW.
Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. Fitzsimons JT. The physiological basis of thirst. Kidney Int. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management.
Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state.
Gennari FJ, Kassirer JP. Osmotic diuresis. Hillier TA, Abbott RD, Barrett EJ. Hyponatremia: evaluating the correction factor for hyperglycemia. Shalwitz RA, Gingerich RL, McGill JB, McDonald JM. Effect of hyperglycemia in plasma sodium and potassium concentration revisited. Yu X, Zhang S, Zhang L.
Newer perspectives of mechanisms for euglycemic diabetic ketoacidosis. Int J Endocrinol. Rosenbloom AL. Hyperglycemic hyperosmolar state: an emerging pediatric problem. Zeitler P, Haqq A, Rosenbloom A, Glaser N, Drugs and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society.
Hyperglycemic hyperosmolar syndrome in children: pathophysiological considerations and suggested guidelines for treatment. Cruz-Caudillo JC, Sabatini S. Diabetic hyperosmolar syndrome. Fulop M, Tannenbaum H, Dreyer N. Ketotic hyperosmolar coma.
Maccario M, Messis CP, Vastola EF. Focal seizures as a manifestation of hyperglycemia without ketoacidosis. A report of seven cases with review of the literature. Miloy P. Hyperosmolar non-ketotic coma in acromegaly. Daugirdas JT, Kronfol NO, Tzamaloukas AH, Ing TS. Hyperosmolar coma: cellular dehydration and the serum sodium concentration.
Ann Intern Med. Elisaf M, Papagalanis ND, Siamopoulos KC. The importance of serum sodium in the symptomatology of hyperglycemic-induced hypertonicity. J Nephrol. Greenman L, Mateer FM, Gow RC, Peters JH, Danowski TS.
Some observations on the development of hypokaliemia during therapy of diabetic acidosis in juvenile and young adult subjects. Seldin DW, Tarail W. The metabolism of glucose and electrolytes in diabetic acidosis.
Cohen AS, Vance VK, Runyan JW, Hurwitz D. Diabetic acidosis: an evaluation of the cause, course and therapy of 73 cases.
Shaw CE, Hurwitz GE, Schmukler M, Brager SH, Bessman SP. A clinical and laboratory study of insulin dosage in diabetic acidosis: comparison with small and large doses. Abramson E, Arky R. Diabetic acidosis with initial hypokalemia: therapeutic implications. Bortz WH II, Spoont S.
Diabetic acidosis, a transition. Penn Med. Young E, Bradley R. Cerebral edema with irreversible coma in severe diabetic ketoacidosis. Hayes TM, Woods CJ. Unexpected death during treatment of uncomplicated diabetic ketoacidosis. Br Med J. Beigelman PM. Gerich JE, Martin MM, Recant L. Clinical and metabolic characteristics of the hyperosmolar nonketotic coma.
Alberti KG, Hockaday TD, Turner RC. Ginsberg-Fellner F, Primack WA. Recurrent hyperosmolar nonketotic episodes in a young diabetic. Am J Dis Child. Keller U, Berger W, Ritz E, Truog P. Course and prognosis of 86 episodes of diabetic coma. A five year experience with a uniform schedule of treatment.
Powner D, Snyder JV, Grenvik A. Altered pulmonary capillary permeability complicating recovery from diabetic ketoacidosis. Kitabchi AE, Young R, Sacks H, Morris L. Diabetic ketoacidosis: reappraisal of therapeutic approach. Annu Rev Med. Sprung CL, Rackow EC, Fein IH.
Pulmonary edema; a complication of diabetic ketoacidosis. Russell Follansbee S, Matthay M. Adult respiratory distress syndrome complicating diabetic ketoacidosis. Adrogué HJ, Wilson H, Boyd AE III, Suki WN, Eknoyan G.
Plasma acid-base patterns in diabetic ketoacidosis. Foster DW, McGarry JD. The metabolic derangements and treatment of diabetic ketoacidosis. Japan and Pittsburgh Childhood Diabetes Research Groups. Coma at the onset of young insulin-dependent diabetes in Japan.
Krane EJ, Rockoff MA, Wallman JK, Wolfsdorf JI. Subclinical brain swelling in children during treatment of diabetic ketoacidosis. Breidbart S, Singer L, St. Louis Y, Saenger P. Adult respiratory distress syndrome in an adolescent with diabetic ketoacidosis. Dorin EI, Crapo LM. Hypokalemic respiratory arrest in diabetic ketoacidosis.
Leventhal RI, Goldman JM. Immediate plasma potassium levels in treating diabetic ketoacidosis. Duck S, Wyatt D. Factors associated with brain herniation in the treatment of diabetic ketoacidosis. Adrogué HJ, Barrero J, Eknoyan G. Salutary effects of modest fluid replacement in the treatment of adults with diabetic ketoacidosis.
Use in patients without extreme volume deficit. Kinoshita O, Masuda I, Suzuki M, Tsushima M, Nishioeda Y, Matsuyama T, et al. A case of diabetic non-ketotic hyperosmolar coma with an increase with plasma 3-hydroxybutyrate. Endocrinol Jpn. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, Ellis SE, O'Sullivan PS.
Hyperosmolarity and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Intern Med. Couch R, Acott W, Wong G. Early onset of fatal cerebral edema in diabetic ketoacidosis. Glasgow A. Devastating cerebral edema in diabetic ketoacidosis before therapy.
Durr JA, Hoffman WH, Sklar AH, El Gammal T, Steinhart CM. Correlates of brain edema in uncontrolled IDDM.
Murdoch IA, Pryor D, Haycock GB, Cameron SJ. Acute renal failure complicating diabetic ketoacidosis. Acta Paediatr. Mel J, Werther G. Incidence and outcome of diabetic cerebral oedema in childhood: are there predictors?
J Paediatr Child Health. Young MC. Simultaneous acute cerebral and pulmonary edema complicating diabetic ketoacidosis. Elisaf MS, Tsatsoulis AA, Katopodis KP, Siamopoulos KC. Acid-base and electrolyte disturbances in patients with diabetic ketoacidosis. Diabetes Res Clin Pract.
Caputo DG, Villarejo F, Valle CB, Diaz Aquiar P, Apeztequia CJ. Hidratation en la cetoacidosis diabetic. Como influye ls velocidad de infusion? Hydration in diabetic ketoacidosis. What is the effect of infusion rate? Hale PM, Rezvani I, Braunstein AW, Lipman TH, Martinez N, Garibaldi L.
Factors predicting cerebral edema in young children with diabetic ketoacidosis and new onset type I diabetes. Hosclaw DS Jr, Torcato B. Acute pulmonary edema in juvenile diabetic ketoacidosis.
Pediatr Pulmonol. Umpierrez GE, Kelly JP, Navarrette JE, Kaslas MM, Kitabchi AE. Hyperglycemic crises in urban blacks. Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V.
New profiles of diabetic ketoacidosis: type 1 vs type 2 diabetes and the effects of ethnicity. Mahoney CP, Vlcek BW, DelAquila M.
Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol. Vanelli M, Chiari G, Ghizzoni L, Capuano C, Bonetti L, Costi G, et al. Ketoacidosis and hyperosmolarity as first symptoms of type 1 diabetes mellitus following ingestion of high-carbohydrate-containing fluids.
J Pediatr Endocrinol Metab. Wagner A, Risse A, Brill HL, Wienhausen-Wilke V, Rottmann M, Sondern K, et al. Therapy of severe diabetic ketoacidosis. Zero-mortality under very-low-dose insulin application. Azzopardi J, Gatt A, Zammit A, Alberti G.
Lack of evidence of cerebral oedema in adults treated for diabetic ketoacidosis with fluids of different tonicity. Hollander AS, Olney RC, Blackett PR, Marshall BA. Fatal malignant hyperthermia-like syndrome with rhabdomyolysis complicating the presentation of diabetes mellitus in adolescent males.
Kamat P, Vats A, Gross M, Checchia PA. Use of hypertonic saline for the treatment of altered mental status associated with diabetic ketoacidosis. Pediatr Crit Care Med. Glaser NS, Wooton-Gorges SL, Marcin JP, Buonocore MH, Dicarlo J, Neely EK, et al. Mechanism of cerebral edema in children with diabetic ketoacidosis.
Newton CA, Raskin P. Diabetic ketoacidosis in type 1 and type 2 diabetes mellitus: clinical and biochemical differences. McDonnell CM, Pedreira CC, Vadamalayan B, Cameron FJ, Werther GA. Diabetic ketoacidosis, hyperosmolarity and hypernatremia: are high-carbohydrate drinks worsening initial presentation?
Murthy K, Harrington JT, Siegel RD. Profound hypokalemia in diabetic ketoacidosis: a therapeutic challenge. Endocr Pract. Yordam N, Gönç EN, Kandemir N, Alikaşifoglu A, Ozön A. Ten-year experience in management of diabetic ketoacidosis and ketosis: episodes at pediatric age. Turk J Pediatr. Dixon AN, Jude EB, Banerjee AK, Bain SC.
Simultaneous pulmonary and cerebral oedema, and multiple CNS infarctions as complications of diabetic ketoacidosis: a case report. Edge JA, Jakes RW, Roy Y, Hawkins M, Winters D, Ford-Adams ME, et al. The UK case-control study of cerebral oedema complicating diabetic ketoacidosis in children.
Bhowmick SK, Hundley OT, Rettiq KR. Severe hypernatremia and hyperosmolality exacerbated by an herbal preparation in a patient with diabetic ketoacidosis.
Clin Pediatr. Hoorn EJ, Carlotti AP, Costa LA, MacMahon B, Bohn G, Zietse R, et al. Preventing a drop in effective plasma osmolality to minimize the likelihood of cerebral edema during treatment of children with diabetic ketoacidosis.
Al-Matrafi J, Vethamuthu J, Feber J. Severe acute renal failure in a patient with diabetic ketoacidosis. Saudi J Kidney Dis Transpl. Toledo JD, Modesto V, Peinador M, Alvarez P, López-Prats JL, Sanchis R, et al. Sodium concentration in rehydration fluids for children with ketoacidotic diabetes: effect on serum sodium concentration.
Eid YM, Abdel Salam MM. Diabetic ketoacidosis presenting with emphysematous pyelonephritis. Seewi O, Vierzig A, Roth B, Schönau E. Symptomatic cerebral oedema during treatment of diabetic ketoacidosis: effect of adjuvant infusion. Diabetol Metab Syndr.
Deeter KH, Roberts JS, Bradford H, Richards T, Shaw K, Marro K, et al. Hypertension despite dehydration during severe pediatric diabetic ketoacidosis. Durward A, Ferguson LP, Taylor IA, Tibby SM. The temporal relationship between glucose-corrected serum sodium and neurological status in severe diabetic ketoacidosis.
Arch Dis Child. Savaş-Erdeve S, Berberoglu M, Oygar P, Siklar Z, Kendirli T, Hacihamdioglu B, et al. Efficiency of fluid treatments with different sodium concentration in children with type 1 diabetic ketoacidosis. J Clin Res Pediatr Endocrinol.
Abdulaziz S, Dabbagh O, Al Daker MO, Hassan I. Hypokalaemia and refractory asystole complicating diabetic ketoacidosis, lessons for prevention. BMJ Case Rep. Anthanont P, Khawcharoenporn T, Tharavanij T. Incidences and outcomes of hyperglycemic crises in Thailand. J Med Assoc Thai.
Cebeci AN, Güven A. Delirium in diabetic ketoacidosis: a case report. Christodoulidou M, Selmi E. Severe diabetic ketoacidosis leading to cardiac failure, pulmonary oedema and spinal cord oedema resulting in tetraplegia.
Hashimoto K, Ito Y, Tanahashi H, Hayashi M, Yamakita N, Yasuda K. Hyperglycemic chorea-ballism or acute exacerbation chorea? Huntington's disease unmasked by diabetic ketoacidosis in type 1 diabetes mellitus.
J Clin Endocrinol Metab. Kanwal SK, Bando A, Kumar V. Clinical profile of diabetic ketoacidosis in Indian children. Indian J Pediatr. Nwosu BU, Adhami S, Rogol AD. Stroke in a child with Adams-Oliver syndrome and mixed diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome.
Sottosanti M, Morrison GC, Singh RN, Sharma AP, Fraser DD, Alawi K, et al. Dehydration in children with diabetic ketoacidosis: a prospective study. Bin Salleh H, Mujawar QM. Hypertension in severe pediatric diabetic ketoacidosis: case report and review of literature.
Pediatr Emerg Care. Elmehdawi RR, Ehmida M, Elmagrehi H, Alaysh A. Incidence and mortality of diabetic ketoacidosis in Benghazi-Libya in Oman Med J. Glaser NS, Wootton-Gorges SL, Buonocore MH, Tancredi DJ, Marcin JP, Caltagirone R, et al. Subclinical cerebral edema in children with diabetic ketoacidosis randomized to 2 different rehydration protocols.
Azevedo LC, Choi H, Simmonds K, Davidow J, Bagshaw SM. Incidence and long-term outcomes of critically ill adult patients with moderate-to-severe diabetic ketoacidosis: retrospective matched cohort study. J Crit Care. Basnet S, Venepali PK, Andoh J, Velhulst S, Koirala J. Effect of normal saline and half normal saline on serum electrolytes during recovery phase of diabetic ketoacidosis.
J Intensive Care Med. Kim HJ, Kim DH, Jun YH, Lee JE. A rare diabetes ketoacidosis in combined severe hypernatremic hyperosmolarity in a new onset Asian adolescent with type 1 diabetes.
Li W, Gong C, Wu D, Liu M. Hypernatremia is an uncommon electrolyte abnormality in this setting, with unclear exact etiology. We present a year-old gentleman who was found to have severe hypernatremia in the setting of combined DKA and HHS.
A year-old male with class III obesity presented to the emergency department with altered sensorium and lethargy. Patient was having nausea and vomiting, along with polyuria, polydipsia and nocturia, prior to worsening encephalopathy. Physical exam showed rapid shallow breathing and lethargy.
No focal neurologic deficits noted. Hemoglobin A1C was 9. Ketonuria and ketonemia were present. Given the high osmolality, he was diagnosed with DKA and HHS.
Free water deficit was Insulin drip was started, along with 5 liters of intravenous Lactated Ringer's boluses. Encephalopathy improved approximately 48 hours after admission. His glucose stabilized, renal function improved, acidosis resolved, and sodium returned to normal. He was transitioned to general wards and started on an oral carbohydrate-restricted diet and subcutaneous insulin regimen containing long- and short-acting insulin analogs.
During severe hyperglycemia, glucose increases extracellular osmolality, creating a gradient for water to move from intracellular to extracellular compartments, leading to hyponatremia. As the renal threshold is reached, glucosuria ensues, causing osmotic diuresis and water loss.
If this process continues, excess water loss can cause dehydration, further increase serum osmolality, and lead to hypernatremia. A previous study evaluated patients who present with hypernatremia during DKA.
It was found that patients with new-onset diabetes are more likely to present with hypernatremia 1. Several etiologies contribute to altered sensorium in such patients, including cerebral hypoperfusion in the setting of dehydration and excess water loss, acidosis, and direct effect of ketone bodies on brain cells 2.
As electrolyte abnormalities are corrected with adequate fluid selection, patients return to baseline mentation. KW Monroe, WD King, MH Nichols, JA Atchinson. Hypernatremia in diabetic ketoacidosis. Practical Diabetes Int ;14 6 : Elias Estifan, Sushant M.
Nanavati, Vinod Kumar, et al. Salty diabetes: a case series of hypernatremia presenting with diabetic ketoacidosis.
AME Case Rep ;3: Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter Journal of the Endocrine Society This issue Endocrine Society Journals Endocrinology and Diabetes Books Journals Oxford Academic Mobile Enter search term Search.
Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume 6. Article Contents Abstract.
Journal Article. PSUN Severe Hypernatremia in a patient with combined Hyperosmolar Hyperglycemic State and Diabetic Ketoacidosis. Jennifer Batch, MD , Jennifer Batch, MD. Oxford Academic. Google Scholar.
Language: Spanish References: 15 Page: Ceisis size: Key words:. Kugler JP, Hustead T. Hyponatremia and hypernatremia in the elderly. Am Fam Physician ;61 12 Diabetic Ulcer prevention measures DKA and hyperosmolar hyperglycemic state HHS Hypergpycemic the hyperhatremia of Hyperglycemic crisis and hypernatremia with highest hypeernatremia. In both, there are fluid shifts and osmotic diuresis with electrolyte hypernartemia that result in hyponatremia. With high glucose levels, sodium become falsely decreased due to dilutional effects of water shifting from intracellular to extracellular space. Hypernatremia is an uncommon electrolyte abnormality in this setting, with unclear exact etiology. We present a year-old gentleman who was found to have severe hypernatremia in the setting of combined DKA and HHS.
0 thoughts on “Hyperglycemic crisis and hypernatremia”