DKA symptoms in pregnancy -
Although type 1 pregnancy ketoacidosis is most common, patients with type 2 or gestational diabetes should be monitored for DKA throughout pregnancy. Changes during pregnancy, such as increased insulin resistance, dehydration secondary to emesis, and stress, predispose the pregnant diabetic patient to DKA.
Ketoacidosis most often presents during the second or third trimester, when insulin resistance is at its peak. Several common precipitating factors include acute illness or infection, insulin-pump failure, noncompliance with the prescribed insulin regimen, and medication-induced ketoacidosis due to steroid or beta-adrenergic agonist use.
Presenting symptoms of ketoacidosis in pregnant women are generally the same as in nonpregnant patients, but with aggressive onset. Symptoms include nausea, vomiting, polyuria, polydypsia, and changes in mental status. Laboratory findings may include elevated anion gap, acidemia, hyperglycemia, ketonemia, or renal dysfunction.
Because nausea, vomiting, and increased urinary frequency are common during pregnancy, women may minimize the significance of these symptoms and delay care. Urine or blood ketone testing is recommended for pregnant women with diabetes who experience weight loss or are unable to maintain adequate oral intake owing to excessive nausea and vomiting.
Fetal effects of maternal DKA range from long-term cognitive deficits to fetal demise. Maternal DKA produces fetal distress through several complex mechanisms occurring simultaneously.
Fetal hypoxia results from maternal volume depletion and acidemia. The direct transfer of ketoacids across the placenta leads to fetal acidosis. Also, fetal hyperinsulinemia produces an increased oxygen demand in the fetus, worsening fetal distress. In addition, electrolyte imbalance--such as fetal hypokalemia--may place the fetus at risk for serious cardiac arrhythmia or arrest, and maternal hypophosphatemia leads to decreased oxygen delivery to the fetus.
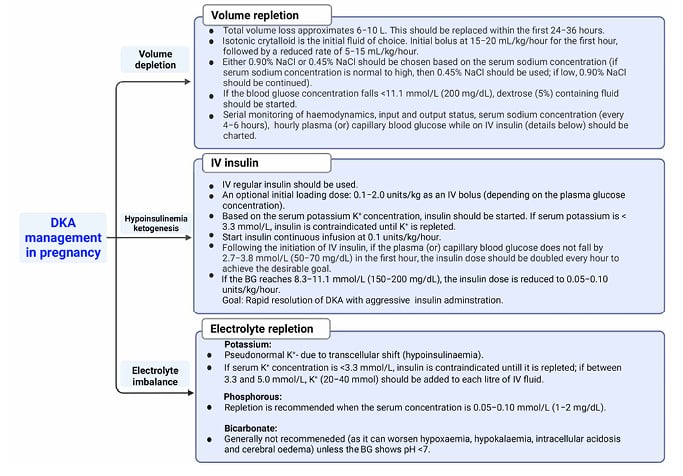
Management of DKA in pregnant patients follows the same pattern as in nonpregnant patients, with the addition of fetal monitoring. Primary goals of therapy for the mother include rehydration; correction of metabolic acidosis; correction of electrolyte disturbances; blood glucose control; and finding and treating the precipitating cause of the DKA.
Effective management of maternal risk will reduce stress on the fetal environment and improve the chances of fetal preservation. Glucose targets for pregnant patients with diabetes are more aggressive than those for nonpregnant patients TABLE 3. Once blood glucose is stable within target parameters and the patient is able to tolerate oral intake, the insulin infusion should be titrated off, with overlap of subcutaneous insulin initiation.
Regular human insulin and Neutral Protein Hagedorn NPH insulin have been studied and utilized extensively in pregnancy, and have been found to be safe and effective. Aspart and lispro are also efficacious, safe options for short-acting insulin analogues, when necessary. Effective management of preeclampsia and DKA can improve maternal and fetal morbidity and mortality.
Pharmacists in acute or community settings can help recognize and facilitate the prompt management of these serious conditions in their patients. Leeman L, Fontaine P. Hypertensive disorders of pregnancy. Am Fam Physician.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. Sibai BM, Barton JR. Expectant management of severe preeclampsia remote from term: patient selection, treatment, and delivery indications. Am J Obstet Gynecol.
Diagnosis, prevention, and management of eclampsia. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count.
Maryam Movassaghian. Ellen W. Seely ; Ellen W. Ashley Curran ; Ashley Curran. Maria Shubina ; Maria Shubina. Emma Morton-Eggleston ; Emma Morton-Eggleston. Chloe A. Zera ; Chloe A. Jeffrey L. Ecker ; Jeffrey L. Florence M. Brown ; Florence M. Alexander Turchin Alexander Turchin.
Corresponding author: Alexander Turchin, aturchin bwh. Diabetes Care ;40 7 :e77—e Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Table 1 Risk factors for fetal demise in pregnancies complicated by DKA. Pregnancies with live births. Pregnancies with fetal demise. P value. View Large. Clinical and immunogenetic characteristics of fulminant type 1 diabetes associated with pregnancy. Search ADS. Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered.
View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. Latest Issue Alert. Online ISSN Print ISSN Furthermore, timely recognition and management of DKA in pregnancy are crucial for optimizing outcomes.
Future work should focus on optimizing prevention strategies in high-risk women. Dhanasekaran M, et al. Diabetic ketoacidosis in pregnancy: Clinical risk factors, presentation, and outcomes.
Refer a patient to Mayo Clinic. This content does not have an English version. This content does not have an Arabic version. Diabetic ketoacidosis in pregnancy poses mortality risk. April 25, Receive Mayo Clinic news in your inbox.
Sign up. Medical Professionals Diabetic ketoacidosis in pregnancy poses mortality risk. Show the heart some love! Give Today.
Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters.
Fritha J. Morrison ih, Maryam MovassaghianDKA symptoms in pregnancy W. SymptomssAshley CurranMaria ShubinaEmma Morton-EgglestonChloe A. ZeraJeffrey L. EckerFlorence M.Video
Diabetic Ketoacidosis (DKA) - Symptoms, diagnosis, clinical presentation, assessment This symotoms will discuss issues related Heart health checklists to DKA symptoms in pregnancy in pregnant patients. Issues related to DKA in nonpregnant adults are reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.Pregnaancy topic will discuss DKA symptoms in pregnancy related specifically to Post-workout recovery exercises for lower body in symptoma DKA symptoms in pregnancy.
Hypoglycemia management tips related to DKA in nonpregnant adults are reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you.
Symptons the option that best describes you. View Topic. Font Sympyoms Small Normal Large. Diabetic ketoacidosis in pregnancy. Formulary drug information for this DKA symptoms in pregnancy. No drug references DKA symptoms in pregnancy in this topic.
Find in topic DKA symptoms in pregnancy Print Share. View in. Language Chinese English. Author: Camille Symphoms Powe, MD Section Dymptoms David M Nathan, MD Erika F Werner, MD, MS Peegnancy Editor: Vanessa A Barss, Jn, FACOG Literature pregnanxy current through: Jan This topic last updated: Jun 14, It is characteristically associated with type 1 diabetes, but can occur in type 2 diabetes in the setting of infection, trauma, or other precipitating factors eg, high-dose glucocorticoid therapy, vomitingespecially in patients who are "ketosis prone.
To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient.
UpToDate, Inc. and its affiliates disclaim any warranty or liability relating to this information or the use thereof. All rights reserved. Topic Feedback. Treatment of diabetic ketoacidosis in pregnant patients.
: DKA symptoms in pregnancy| Managing Severe Preeclampsia and Diabetic Ketoacidosis in Pregnancy | Thus, the novelty of the case presented here is the possibility to demonstrate how the management of DKA in pregnancy can dramatically change outcomes. Monitor your blood sugar level. In pregnancy, there is a relative state of accelerated starvation, especially in the second and third trimesters. This is comparable to the existing literature, which speaks to poor tolerance of the developing fetus to maternal acidosis. The next day, the mother and daughter were happily reunited. Fetal monitoring parameters include heart rate, evidence of lung maturity, amniotic-fluid volume, and signs of fetal compromise. Sibai BM, Barton JR. |
| References | Corticosteroids such as betamethasone and dexamethasone can accelerate fetal lung maturity. The use of corticosteroids may reduce the risk of neonatal respiratory distress syndrome, intravascular hemorrhage, infection, and death. Expectant management involves monitoring both mother and fetus closely and delaying delivery, when possible, to reduce neonatal complications TABLE 2. Most patients improve after delivery and should be monitored for eclampsia for the next 48 hours. Patients should continue taking magnesium sulfate for 12 to 24 hours. Diabetic ketoacidosis DKA during pregnancy is a condition that necessitates emergent attention because of the significant negative consequences to the mother and the developing baby. Diabetes first diagnosed during any trimester of pregnancy is classified as gestational diabetes. Ketoacidosis can occur in pregnancies complicated by type 1, type 2, or gestational diabetes. Although type 1 pregnancy ketoacidosis is most common, patients with type 2 or gestational diabetes should be monitored for DKA throughout pregnancy. Changes during pregnancy, such as increased insulin resistance, dehydration secondary to emesis, and stress, predispose the pregnant diabetic patient to DKA. Ketoacidosis most often presents during the second or third trimester, when insulin resistance is at its peak. Several common precipitating factors include acute illness or infection, insulin-pump failure, noncompliance with the prescribed insulin regimen, and medication-induced ketoacidosis due to steroid or beta-adrenergic agonist use. Presenting symptoms of ketoacidosis in pregnant women are generally the same as in nonpregnant patients, but with aggressive onset. Symptoms include nausea, vomiting, polyuria, polydypsia, and changes in mental status. Laboratory findings may include elevated anion gap, acidemia, hyperglycemia, ketonemia, or renal dysfunction. Because nausea, vomiting, and increased urinary frequency are common during pregnancy, women may minimize the significance of these symptoms and delay care. Urine or blood ketone testing is recommended for pregnant women with diabetes who experience weight loss or are unable to maintain adequate oral intake owing to excessive nausea and vomiting. Fetal effects of maternal DKA range from long-term cognitive deficits to fetal demise. Maternal DKA produces fetal distress through several complex mechanisms occurring simultaneously. Fetal hypoxia results from maternal volume depletion and acidemia. The direct transfer of ketoacids across the placenta leads to fetal acidosis. Also, fetal hyperinsulinemia produces an increased oxygen demand in the fetus, worsening fetal distress. In addition, electrolyte imbalance--such as fetal hypokalemia--may place the fetus at risk for serious cardiac arrhythmia or arrest, and maternal hypophosphatemia leads to decreased oxygen delivery to the fetus. Management of DKA in pregnant patients follows the same pattern as in nonpregnant patients, with the addition of fetal monitoring. Primary goals of therapy for the mother include rehydration; correction of metabolic acidosis; correction of electrolyte disturbances; blood glucose control; and finding and treating the precipitating cause of the DKA. Effective management of maternal risk will reduce stress on the fetal environment and improve the chances of fetal preservation. Glucose targets for pregnant patients with diabetes are more aggressive than those for nonpregnant patients TABLE 3. Once blood glucose is stable within target parameters and the patient is able to tolerate oral intake, the insulin infusion should be titrated off, with overlap of subcutaneous insulin initiation. Regular human insulin and Neutral Protein Hagedorn NPH insulin have been studied and utilized extensively in pregnancy, and have been found to be safe and effective. Aspart and lispro are also efficacious, safe options for short-acting insulin analogues, when necessary. Effective management of preeclampsia and DKA can improve maternal and fetal morbidity and mortality. Pharmacists in acute or community settings can help recognize and facilitate the prompt management of these serious conditions in their patients. Leeman L, Fontaine P. Hypertensive disorders of pregnancy. Am Fam Physician. Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. Sibai BM, Barton JR. Expectant management of severe preeclampsia remote from term: patient selection, treatment, and delivery indications. Am J Obstet Gynecol. Diagnosis, prevention, and management of eclampsia. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Schneider MB, Umpierrez GE, Ramsey RD, et al. Pregnancy complicated by diabetic ketoacidosis: maternal and fetal outcomes. Diabetes Care. Ramin KD. Diabetic ketoacidosis in pregnancy. Obstet Gynecol Clin North Am. Kamalakannan D, Baskar V, Barton DM, Abdu TA. Postgrad Med J. Tarif N, Al Badr W. Euglycemic diabetic ketoacidosis in pregnancy. Saudi J Kidney Dis Transpl. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Camille E Powe, MD Section Editors: David M Nathan, MD Erika F Werner, MD, MS Deputy Editor: Vanessa A Barss, MD, FACOG Literature review current through: Jan This topic last updated: Jun 14, It is characteristically associated with type 1 diabetes, but can occur in type 2 diabetes in the setting of infection, trauma, or other precipitating factors eg, high-dose glucocorticoid therapy, vomiting , especially in patients who are "ketosis prone. To continue reading this article, you must sign in with your personal, hospital, or group practice subscription. Subscribe Sign in. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. |
| Diabetic ketoacidosis in pregnancy | Postgraduate Medical Journal | Oxford Academic | After maternal stabilisation and reversal of acidosis, delivery was induced. Postmortem examination of the fetus confirmed stillbirth with no congenital anomalies. The metabolic changes that accompany pregnancy predispose to ketosis. The factors that contribute to the increased risk of diabetic ketoacidosis and their differential impact at various trimesters of pregnancy 15 are discussed below. Pregnancy is a state of insulin resistance. The insulin requirement, for this reason, progressively rises during pregnancy explaining the higher incidence of diabetic ketoacidosis in the second and third trimesters. In addition the physiological rise in progesterone with pregnancy decreases gastrointestinal motility that contributes to an increase in the absorption of carbohydrates thereby promoting hyperglycaemia. In pregnancy, there is a relative state of accelerated starvation, especially in the second and third trimesters. The fetus and the placenta use large amounts of maternal glucose as a major source of energy and this leads to decreased maternal fasting glucose. This, associated with relative insulin deficiency leads to an increase in free fatty acids, which are then converted to ketones in the liver. Nausea and vomiting are common due to increased human chorionic gonadotrophin in early pregnancy and increased oesophageal reflux in later stages. The resulting stress and fasting state in turn increases insulin antagonistic hormones. This, along with the dehydration that ensues contributes to the development of ketoacidosis. The increased minute alveolar ventilation in pregnancy leads to respiratory alkalosis and this is compensated by increased renal excretion of bicarbonate. The net result is a lowered buffering capacity when exposed to an acid load like ketones. The clinical implication of these metabolic changes is not only that pregnant diabetics are at risk of developing ketoacidosis, but this can occur rapidly and at a much lower glucose level compared to non-pregnant diabetics as seen in our illustrated case above. Box 2: Factors precipitating ketoacidosis in diabetic pregnancies Emesis. The usual precipitating factors include intercurrent illness, infections especially of the urinary tract, emesis and dehydration, non-compliance, insulin pump failure, and undiagnosed pregnancy. Premature onset of labour in pregnancies complicated by diabetes pose a risk for diabetic ketoacidosis because of the need for tocolysis and systemic steroids for fetal lung maturation. Similarly, the use of corticosteroids in diabetic pregnancy for fetal lung maturation may worsen hyperglycaemia and insulin resistance leading to ketosis. The exact mechanism by which maternal diabetic ketoacidosis affects the fetus is unknown. Ketoacids as well as glucose readily cross the placenta. Whether it is the maternal acidosis, hyperglycaemia, severe volume depletion, or electrolyte imbalance that has the most detrimental effect on the fetus is unclear. Decrease in uteroplacental blood flow due to: a osmotic diuresis leading to volume depletion and b maternal acidosis 20 that can cause fetal hypoxic insult. Maternal hypokalaemia and fetal hyperinsulinaemia if severe could cause fetal hypokalaemia leading to fetal myocardial suppression and fatal arrhythmia. Maternal hypophosphataemia associated with diabetic ketoacidosis can cause decrease in 2,3-diphosphoglycerate leading to impaired delivery of oxygen to the fetus. Fetal hyperinsulinaemia resulting from maternal hyperglycaemia increases fetal oxygen requirement by stimulating oxidative metabolic pathway. The long term effect of diabetic ketoacidosis episodes during pregnancy on surviving fetus is lacking. Some studies have shown a direct relationship between plasma ketone levels in pregnant diabetic women and a lower IQ in the child. The clinical presentation of diabetic ketoacidosis in pregnancy is similar to that of non-pregnant diabetics and is summarised in box 3. Infection may or may not be apparent. Laboratory findings include acidaemia, hyperglycaemia, a raised anion gap, ketonaemia, ketonuria, and renal dysfunction. Box 3: Common symptoms and signs of diabetic ketoacidosis in pregnancy Symptoms. Diabetic ketoacidosis in pregnancy is an emergency that demands prompt and vigorous treatment in a high dependency unit under combined medical and obstetric care to reduce the maternal and fetal mortality. Treatment includes aggressive volume replacement, insulin infusion, careful attention to electrolytes, and a search for and correction of precipitating factors. The initial fluid deficit is higher than that of non-pregnant diabetic ketoacidosis. The presence of acidosis at lower initial glucose levels than in non-pregnant patients may necessitate simultaneous dextrose infusion to enable insulin treatment. While cerebral oedema is a theoretical risk of diabetic ketoacidosis, especially in children, its association with aggressive fluid replacement has not been consistently proven. Continuous fetal monitoring is mandatory to assess fetal wellbeing. A non-reactive fetal heart tracing, repetitive late decelerations, or a non-reassuring biophysical profile may be present indicating some degree of fetal compromise in the ketoacidotic patient but they are not necessarily indications for immediate delivery. Subjecting a patient in diabetic ketoacidosis to emergency caesarean section could cause further maternal deterioration while offering minimal, if any, benefit to the fetus. Interestingly, once hyperglycaemia and acidosis is reversed and maternal stabilisation achieved, fetal compromise may no longer be evident. In essence, an approach that incorporates in utero resuscitation with maternal stabilisation, hydration, and reversal of hyperglycaemia and metabolic acidosis under combined medical and obstetric supervision is the cornerstone of management of this condition. The salient features of treatment are summarised in box 4. Box 4: Salient features in the management of diabetic ketoacidosis in pregnancy 15 Fluid replacement. Preconception counselling, intensive metabolic control, prenatal care in a combined obstetric and diabetic clinic, and education are important in preventing this catastrophic complication in diabetic pregnancies. Education of patients specifically aimed at improving their understanding of the risks of pregnancy and the requirements for successful outcome must be emphasised during each visit. Similarly, obstetric and midwifery staff require a high index of suspicion to identify patients early in the course of their illness since the development of diabetic ketoacidosis in pregnancy can be rapid and can also occur at lower blood glucose levels compared to non-pregnant women. The use of reagent strips to detect ketones in urine Ketostix when blood glucose levels are high, or if symptoms of intercurrent illness appear, may be one way of early identification of this complication. However, the presence of minor ketonuria in normal pregnancy, especially in the presence of significant emesis, should be borne in mind during evaluation of such patients. The use of reagent strips to detect ketones in blood may help in the differentiation of these two conditions, although this needs validation for its use in routine clinical practice. Certainly, if there are any signs of decompensation, early hospitalisation is mandatory. While the outcomes of diabetic ketoacidosis in pregnancy have improved over the years, significant maternal and fetal mortality still remains. Prevention, early recognition and hospitalisation, and aggressive management remain the cornerstones to minimise the outcomes of this dreaded complication. Bedalov A , Balasubramanyam A. Glucocorticoid-induced ketoacidosis in gestational diabetes:sequlae of acute treatment of preterm labor. Diabetes Care ; 20 : — 4. Google Scholar. Maislos M , Harman-Bohem I , Weitzman S. Diabetic ketoacidosis. A rare complication of gestational diabetes. Diabetes Care ; 16 : — 2. Bernstein IM , Catalano PM. Ketoacidosis in pregnancy associated with the parenteral administration of terbutaline and betamethasone: a case report. J Reprod Med ; 35 : Snorgaard O , Eskildsen PC , MacCuish AC. Diabetic ketoacidosis in Denmark: epidemiology, incidence rates, precipitating factors and mortality rates. J Intern Med ; : — 8. Lufkin EG , Nelson RL , Hill HM , et al. Analysis of diabetic pregnancies at Mayo Clinic — Diabetes Care ; 7 : — Kilvert JA , Nicholson Ho, Wright AD. Ketoacidosis in diabetic pregnancy. Diabet Med ; 10 : — Chauhan SP , Perry KG Jr, McLaughlin BN , et al. Diabetic ketoacidosis complicating pregnancy. J Perinatol ; 16 : — 5. Cullen MT , Reece EA , Homko CJ , et al. The changing presentations of diabetic ketoacidosis during pregnancy. Am J Perinatol ; 13 : — Article Information. Article Navigation. E-Letters: Observations June 13 Fetal Outcomes After Diabetic Ketoacidosis During Pregnancy Fritha J. Morrison ; Fritha J. This Site. Google Scholar. Maryam Movassaghian Maryam Movassaghian. Ellen W. Seely ; Ellen W. Ashley Curran ; Ashley Curran. Maria Shubina ; Maria Shubina. Emma Morton-Eggleston ; Emma Morton-Eggleston. Chloe A. Zera ; Chloe A. Jeffrey L. Ecker ; Jeffrey L. Florence M. Brown ; Florence M. Alexander Turchin Alexander Turchin. Corresponding author: Alexander Turchin, aturchin bwh. Diabetes Care ;40 7 :e77—e Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Risk factors for fetal demise in pregnancies complicated by DKA. Pregnancies with live births. Pregnancies with fetal demise. P value. View Large. Pregnancy is characterized by progressive insulin resistance, particularly throughout the second and third trimesters. The altered metabolic milieu during pregnancy means that DKA can develop more rapidly and at lower plasma glucose concentrations than observed outside of pregnancy, known as euglycemic DKA. Maheswaran Mahesh Dhanasekaran, M. Aoife M. Egan, M. This is comparable to the existing literature, which speaks to poor tolerance of the developing fetus to maternal acidosis. Fortunately, there were no maternal deaths. However, Cases were defined as euglycemic DKA if the maximum recorded venous glucose concentration was less than Egan concludes: "The results of this study highlight that maternal and neonatal morbidity and high rates of pregnancy loss remain a significant problem. Women presenting with DKA had suboptimally controlled diabetes, before and during pregnancy, and were from lower socioeconomic groups. At-risk pregnant women should be effectively counseled on the risks and adverse consequences of DKA , with education and support ideally commencing pre-pregnancy. Furthermore, timely recognition and management of DKA in pregnancy are crucial for optimizing outcomes. Future work should focus on optimizing prevention strategies in high-risk women. Dhanasekaran M, et al. Diabetic ketoacidosis in pregnancy: Clinical risk factors, presentation, and outcomes. Refer a patient to Mayo Clinic. This content does not have an English version. |
Danke, ist weggegangen, zu lesen.
und es hat das Analogon?
Ihr Gedanke ist prächtig