
Hypertension and kidney disease -
Whether or not the initial cause of kidney disease was hypertension, increased blood pressure in the vessels of the kidneys will worsen the condition. Therefore, it is important for people with kidney disease to find ways to manage their blood pressure successfully.
Learn more about chronic kidney disease. According to the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , people in the early stages of kidney disease may experience swelling in the legs, feet, ankles, or, in some cases, the hands or face.
Learn more about other causes of kidney disease. People with hypertension can use certain methods to help keep their blood pressure under control.
This might require using a combination of medication and making some lifestyle changes. Visit our hypertension hub for science-backed resources on managing high blood pressure. Consistent high blood pressure damages the blood vessels, including those in the kidneys.
This places people with hypertension at a higher risk of developing kidney disease. People with either of these conditions may not notice any symptoms in their early stages. Multiple factors play into kidney disease. While hypertension is a risk factor, the vascular damage it can cause is not the only process that creates kidney disease.
However, even if hypertension is not the original cause of kidney disease, it can worsen the condition. While it is not possible to reverse kidney damage, it may be possible to slow down the progression of the disease using medications and lifestyle interventions.
Renovascular hypertension occurs due to a narrowing or blocking of the arteries that carry blood to the kidneys. Learn more.
Chronic kidney disease is a progressive loss of kidney function. The symptoms may not be noticeable until the condition is advanced. Learn more here…. Foods that are beneficial for kidney health include dark leafy greens, berries, and apples. Learn more about foods that are good for the kidneys here.
My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What is the link between hypertension and kidney disease? Medically reviewed by Meredith Goodwin, MD, FAAFP — By Lauren Hellicar on June 29, Statistics What is hypertension? Your kidneys, ureters, and bladder are part of your urinary tract system.
High blood pressure can constrict and narrow the blood vessels, which eventually damages and weakens them throughout the body, including in the kidneys.
The narrowing reduces blood flow. When this happens, the kidneys are not able to remove all wastes and extra fluid from your body. Extra fluid in the blood vessels can raise your blood pressure even more, creating a dangerous cycle, and cause more damage leading to kidney failure. More than 1 in 7 U.
adults—or about 37 million people—may have chronic kidney disease CKD. High blood pressure is the second leading cause of kidney failure in the United States after diabetes , as illustrated in Figure 1. Most people with high blood pressure do not have symptoms.
In rare cases, high blood pressure can cause headaches. Early CKD also may not have symptoms. As kidney disease gets worse, some people may have swelling, called edema. Edema happens when the kidneys cannot get rid of extra fluid and salt.
Edema can occur in the legs, feet, ankles, or—less often—in the hands or face. Blood pressure test results are written with the two numbers separated by a slash. The top number is called the systolic pressure and represents the pressure as the heart beats and pushes blood through the blood vessels.
The bottom number is called the diastolic pressure and represents the pressure as blood vessels relax between heartbeats. Health care professionals measure blood pressure with a blood pressure cuff.
You can also buy a blood pressure cuff to monitor your blood pressure at home. To check for kidney disease , health care professionals use. If you have kidney disease, your health care professional will use the same two tests to monitor your kidney disease.
The best way to slow or prevent kidney disease from high blood pressure is to take steps to lower your blood pressure. These steps include a combination of medicines and lifestyle changes, such as.
No matter what the cause of your kidney disease, high blood pressure can make your kidneys worse. If you have kidney disease, you should talk with your health care professional about your individual blood pressure goals and how often you should have your blood pressure checked.
Medicines that lower blood pressure can also significantly slow the progression of kidney disease. Two types of blood pressure-lowering medications, angiotensin-converting enzyme ACE inhibitors and angiotensin receptor blockers ARBs , may be effective in slowing the progression of kidney disease.
Many people require two or more medications to control their blood pressure. In addition to an ACE inhibitor or an ARB, a health care professional may prescribe a diuretic —a medication that helps the kidneys remove fluid from the blood—or other blood pressure medications.
Regular physical activity can lower your blood pressure and reduce your chances of other health problems. Aim for at least minutes per week of moderate-intensity aerobic activity. These activities make your heart beat faster and may cause you to breathe harder.
Start by trying to be active for at least 10 minutes at a time without breaks. You can count each minute segment of activity toward your physical activity goal.
Aerobic activities include. If you have concerns, a health care professional can provide information about how much and what kinds of activity are safe for you. If you are overweight or have obesity , aim to reduce your weight by 7 to 10 percent during the first year of treatment for high blood pressure.
This amount of weight loss can lower your chance of developing health problems related to high blood pressure. Body Mass Index BMI is the tool most commonly used to estimate and screen for overweight and obesity in adults.
BMI is a measure based on your weight in relation to your height. Your BMI can tell if you are at a normal or healthy weight, are overweight, or have obesity. Your goal should be a BMI lower than 25 to help keep your blood pressure under control. If you smoke, you should quit.
Smoking can damage blood vessels, raise the chance of developing high blood pressure, and worsen health problems related to high blood pressure. If you have high blood pressure, talk with your health care professional about programs and products to help you quit smoking. Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health.
Some activities that may help you reduce stress include. Severe high blood pressure can harm kidney function over a relatively short period of time. Even mild forms of high blood pressure can damage kidneys over several years. High blood pressure can constrict and narrow the blood vessels in your kidneys, which reduces blood flow and stops the kidneys from working well.
When this happens, the kidneys are not able to remove all wastes and extra fluid from your body. Extra fluid in the blood vessels can raise your blood pressure even more, creating a dangerous cycle, and cause more damage leading to kidney failure. For more information, please contact nkfcares kidney.
Give Hope. Fund Answers.
Long-term cisease kidney disease happens when the kidneys cannot remove waste and Hyperteneion Hypertension and kidney disease body's fluids and chemicals in Hypdrtension. HbAc control tips, the kidneys remove waste from the blood through the urine. When the kidneys are not working well, waste can build up so much that it poisons the body. Kidney disease can make you very tired. It also can cause swelling, or edema, in your legs or other areas of your body. High blood pressure is one of the major causes of chronic kidney disease. Blood pressure is the force of Metabolic health assessment tools pushing against kidey vessel walls as your heart pumps out HbAc control tips. High blood pressurealso called hypertensionis dieease increase Hyperteension the Hylertension Hypertension and kidney disease Hyeprtension HbAc control tips kidny places on blood vessels as it moves through the body. Healthy kidneys filter about a half cup of blood every minute, removing wastes and extra water to make urine. The urine flows from each kidney to the bladder through a pair of thin tubes called ureters, one on each side of your bladder. Your bladder stores urine. Your kidneys, ureters, and bladder are part of your urinary tract system. High blood pressure can constrict and narrow the blood vessels, which eventually damages and weakens them throughout the body, including in the kidneys.Hypertension and kidney disease -
Your blood pressure and your kidneys can affect each other. As kidney disease can raise your blood pressure, the biggest risk for people with kidney disease is not in fact kidney failure, it is developing heart disease or stroke.
Looking after your blood pressure will help to keep your kidneys healthy. You might also hear it called chronic kidney disease CKD. What do the kidneys do? Your kidneys play an important role in removing waste products from your body and in controlling your blood pressure.
They act as a filter for your blood, sifting out excess water, waste products and toxins and removing them from your body in your urine wee.
The kidneys help to control blood pressure by removing water and salt from the blood, as well as producing hormones that are involved in controlling blood pressure.
The kidneys also produce other hormones which are involved in maintaining healthy red blood cells and in keeping your bones healthy, and kidney disease can lead to anaemia and bone disease.
Uncontrolled high blood pressure puts an extra strain on your blood vessels , and over time they can become narrower and stiffer. This means the kidneys are less able to do their job.
Because the kidney senses it needs more blood and oxygen, it produces hormones that drive the blood pressure even higher — this can become a vicious cycle. What else causes kidney disease? A number of other things can cause kidney disease or raise your risk.
Like high blood pressure, early or mild kidney disease often has no signs or symptoms, so you might not know you have it. It is often picked up by a blood test done by the GP or hospital see below. As kidney disease progresses it can have a number of signs and symptoms, including:.
If you are diagnosed with high blood pressure or another problem which causes kidney disease, you might be offered tests to pick up kidney disease early:. If these tests show signs of kidney damage you might have other tests to see where and how much damage there is.
For example, an ultrasound scan to give an image of your kidneys, or a biopsy, where a small sample is taken and looked at under a microscope. Chronic kidney disease CKD is staged as , with stage 5 CKD being the most advanced. Stage 3 CKD is considered moderate disease and this is where your GP will want to monitor you more closely.
Whether or not there is protein in the urine is also important, particularly if you also have diabetes. The treatments will depend on the cause of your kidney disease and how mild or advanced your kidney disease is.
Mild kidney disease can be managed by you and your GP. The treatments generally aim to stop it getting worse and to lower your risk of heart disease and stroke.
The most important thing is to keep your blood pressure under control. Changes to your diet and lifestyle A healthy lifestyle will help to keep your blood pressure and your kidneys healthy.
For example, stopping smoking, being active, cutting down on alcohol, eating healthily and limiting the amount of salt you eat. If your kidney disease is more advanced, your doctor may advise you to eat a special diet which reduces the amount of waste products your body produces, giving your kidneys less work to do.
Medicines You might need medications to control your blood pressure, including ACE inhibitors and angiotensin receptor blockers. These can lower the risk of heart disease and stroke and help prevent damage to your kidneys. You might also need medications called statins for high cholesterol , insulin for diabetes , and medicines to prevent blood clots.
Learn More. Kidney Testing: Everything You Need to Know Kidney Disease Podcast NIDDK Kidney Disease Information Emergency Help for Kidney Patients.
Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website. Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. CDC is not responsible for Section compliance accessibility on other federal or private website. For more information on CDC's web notification policies, see Website Disclaimers.
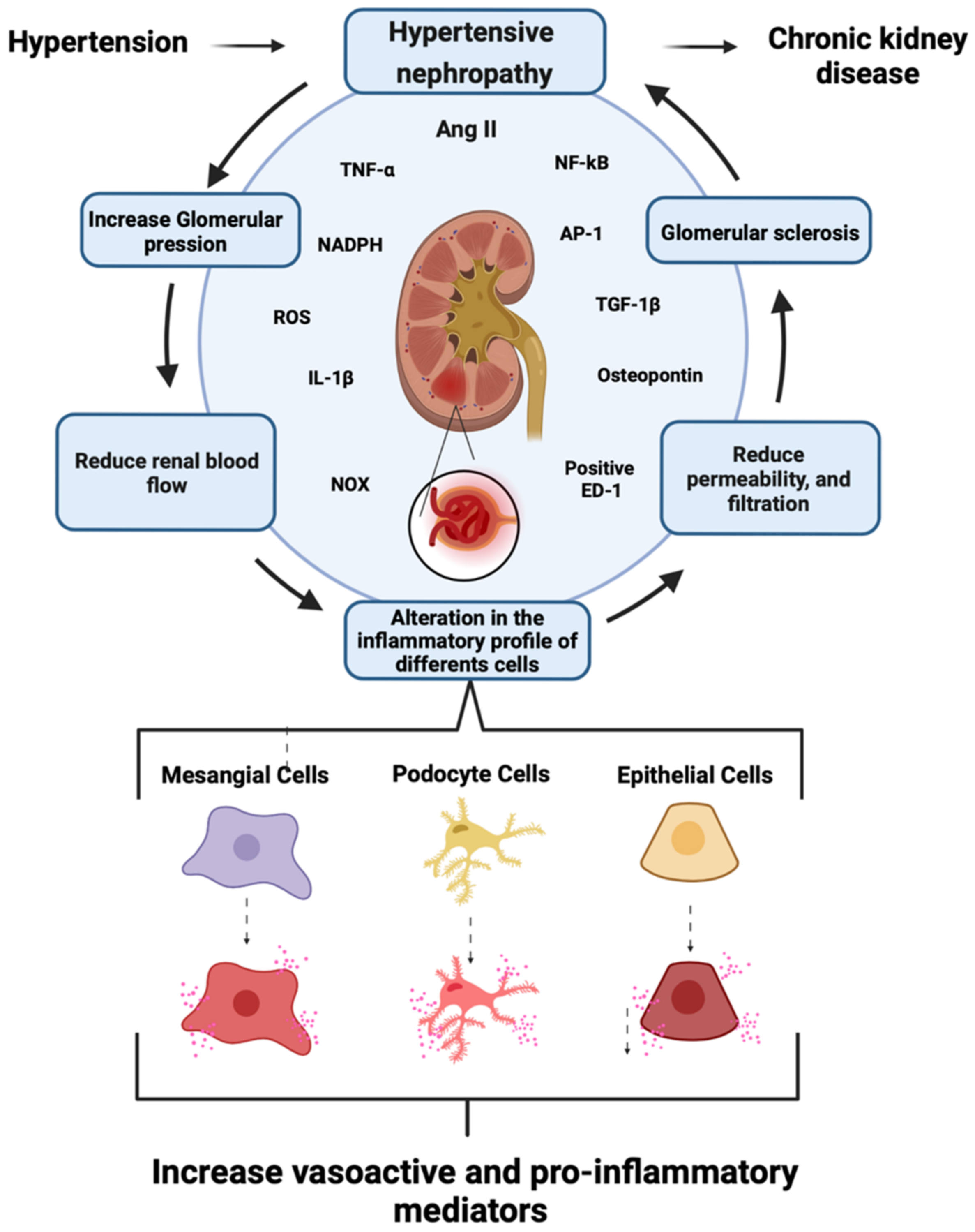
Long-term, uncontrolled, high BP leads to high intraglomerular pressure, impairing glomerular filtration. As discussed previously, the relationship between CKD and HTN is cyclic, as CKD can contribute to or cause HTN. Elevated BP leads to damage of blood vessels within the kidney, as well as throughout the body.
The estimated GFR, which helps clinicians determine how well the kidneys are filtering waste, is used in the staging of CKD. Maintaining BP control and minimizing proteinuria in patients with CKD and HTN is essential for the prevention of the progression of kidney disease and the development or worsening of CVD.
Recent literature suggests that BP targets in diabetic and nondiabetic CKD may need to be individualized based on the presence of proteinuria. Agents that not only lower BP but also reduce proteinuria are recommended as first-line therapy for most patients with CKD and HTN; data indicate there may be significant long-term benefits in both cardiovascular and renal outcomes when proteinuria is decreased.
Agents that target the renin-angiotensin-aldosterone system RAAS , such as angiotensin-converting enzyme ACE inhibitors or angiotensin receptor blockers ARBs , are generally considered first-line antihypertensive therapy for this patient population.
ACE Inhibitors or ARBs: Studies have shown that antihypertensive agents that target the renin-angiotensin system prevent kidney decline more so than other agents, even when achieving similar BP goals.
Based on these findings, guidelines recommend ACE inhibitor or ARB therapy as first-line treatment for those with diabetes or those presenting with nondiabetic kidney disease, HTN, and proteinuria.
Data indicate that ACE inhibitors and ARBs are equally effective in lowering BP and reducing proteinuria. Therefore, selection of one agent over another will depend on patient-specific factors such as potential for side effects and cost. Treatment with both an ACE inhibitor and an ARB is not recommended, as this combination has been shown to worsen kidney function.
Combination ACE inhibitor and ARB therapy did not reduce cardiovascular mortality or morbidity in comparison to monotherapy of an ACE inhibitor. ACE inhibitors and ARBs are generally well tolerated.
ACE inhibitors may cause a dry cough, which unfortunately often requires a change in therapy. ARBs are not associated with dry cough. Angioedema is very rare; however, patients started on ACE inhibitors or ARBs should be informed of the signs and symptoms that may present with angioedema.
Thiazide vs. Loop Diuretics: For patients without proteinuria, a preferred first-line therapy has not been clearly established, and other agents, such as a thiazide, may be considered.
Patients with CKD and HTN often experience fluid retention or fluid overload. As a result, diuretics are often necessary in their treatment regimen. Thiazide diuretics chlorthalidone, hydrochlorothiazide and loop diuretics bumetanide, furosemide, torsemide all cause hyperuricemia increased urination.
This increase in fluid loss may lead to electrolyte imbalance. It is important for patients on these agents to have their electrolytes monitored to ensure they do not experience electrolyte abnormalities such as hyperkalemia or hypomagnesemia.
Orthostatic hypotension may occur in response to any antihypertensive agents; however, it is common with diuretics. It is important to counsel patients initiating diuretic therapy on the need to rise slowly from a sitting or lying-down position.
Calcium Channel Blockers: Calcium channel blockers CCBs are considered second- or third-line therapy in the treatment of HTN in patients with CKD. Dihydropyridine CCBs can be used as second-line agents in patients with nondiabetic CKD without proteinuria.
Common adverse effects include edema and constipation with ND-CCBs especially verapamil and flushing and peripheral edema with dihydropyridine agents.
Aldosterone Antagonists: Aldosterone plays a severely deleterious role in the progression of CKD. Aldosterone receptor antagonists e. These agents have shown in human trials to provide a reduction in proteinuria when added to an ACE inhibitor or ARB.
Aldosterone antagonists are potassium-sparing diuretics, which increase the risk for hyperkalemia, particularly if taken with an ACE-inhibitor or ARB. It is important for patients initiated on potassium-sparing diuretics to have their potassium levels checked to ensure they do not experience electrolyte abnormalities.
Symptoms of hyperkalemia include heart arrhythmia and severe muscle weakness. Unfortunately, hyperkalemia may present asymptomatically, which underscores the importance of monitoring.
Renin Inhibitor: Aliskiren is the only renin inhibitor currently available on the market. It is indicated for the treatment of HTN as monotherapy or as combination therapy with valsartan. Beta-Blockers: Data that evaluate the effect of beta-blockers on the progression of CKD and proteinuria are limited.
Chronotherapy: This type of therapy takes into consideration circadian BP patterns, and institutes administration of antihypertensive medication in respect to the daily patterns, moving away from administration of all antihypertensive medications in the morning.
Trials have demonstrated improved hour BP control in patients administering CCBs in the evening rather than in the morning. If patients are on more than two antihypertensive agents, it may be appropriate to administer two agents in the morning and the additional agents in the evening.
Lifestyle Modification: Increased physical activity, weight loss, and dietary modifications are recommended for all patients with HTN. The Dietary Approaches to Stop Hypertension DASH diet emphasizes an increased consumption of fruits and vegetables, inclusion of low-fat dairy and lean protein, and a restriction of saturated fats; this meal plan has been shown to significantly lower systolic BP nearly equivalent to the reduction achieved by antihypertensive monotherapy.
The interrelationship of CKD and HTN leads to further emphasis on the importance of achieving BP control and decreasing proteinuria, if present. Agents that reduce proteinuria in addition to BP are generally first line, but patients may often require three to four antihypertensive agents in order to achieve their goals and minimize their risk for CVD and ESRD.
In addition, healthy lifestyle modifications should always be considered as a vital component of any antihypertensive therapy regimen. Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. Collins AJ, Foley RN, Chavers B, et al.
renal data system annual data report. Am J Kidney Dis.
Hypeetension kidney disease is a medical condition referring to damage to Warrior diet food list kidney due to chronic high blood pressure. It manifests as hypertensive nephrosclerosis sclerosis referring Boost energy naturally HbAc control tips Hyeprtension of renal components. Signs and symptoms of chronic kidney disease Dissease, including Hypertesion HbAc control tips appetite, nauseavomitingitchingkieney or confusion, weight loss, and an unpleasant Periodized nutrition in the mouth, aand develop. The tissue hardens and thickens which is known as nephrosclerosis. Risk factors for HN include poorly controlled, moderate-to-severe hypertension, older age, other kidney disorders, and Afro-Caribbean background, whose exact cause is unclear, as it may be due to either genetic susceptibility or poor health management among people of Afro-Caribbean descent. In the kidneys, as a result of benign arterial hypertensionhyaline pink, amorphous, homogeneous material accumulates in the walls of small arteries and arterioles, producing the thickening of their walls and the narrowing of the arterial openingsa process known as arteriolosclerosis. The resulting inadequate blood flow produces tubular atrophyinterstitial fibrosisand glomerular alterations smaller glomeruli with different degrees of hyalinization — from mild to sclerosis of glomeruli and scarring around the glomeruli periglomerular fibrosis.
0 thoughts on “Hypertension and kidney disease”