Ulcer prevention in the elderly -
Kim et al. investigated the relationship between pressure ulcer prevention training and the knowledge level of pressure ulcer prevention for 81 care workers working in long-term care hospitals and care homes in , and this study revealed that care workers who received the pressure ulcer prevention training exhibited a higher level of knowledge [ 9 ].
Choi et al. surveyed 90 care workers working in 3 long-term care facilities in and showed that the level of pressure ulcer prevention knowledge must be improved to enhance the performance of pressure ulcer prevention [ 12 ].
Previous studies by Kim et al. and Choi et al. of care workers investigated the knowledge level and relationship between knowledge and care performance, respectively [ 9 , 12 ]. In this study, care workers working in long-term care facilities were surveyed to examine the relationship between knowledge, attitude, and care performance.
Although one study investigated pressure ulcer knowledge, attitude, and performance of nurses at long-term care facilities for the elderly and one study examined the relationship between the attitude towards pressure ulcer prevention and care performance of nurses [ 29 ], research on care workers is lacking.
Knowledge is also a significant prediction factor related to pressure ulcer prevention, so knowledge was included in this study and care workers were selected as the subjects to carry out a different and original study. Because previous studies have surveyed care workers limited to specific regions, research that investigated more subjects across wider areas and regions is necessary for the generalization of the research results.
The subjects of this study were care workers of long-term care facilities located in the urban region of I City and countryside region of Y-gun Gyeongsangbuk-do Province, and a greater number of research subjects were involved in comparison to previous studies for the greater facilitation of research result applications to care workers.
Furthermore, this study aimed to provide basic data and material for the future development of training and education programs for care performance improvement of care workers regarding pressure ulcer prevention. The objectives of this study were to determine the level of pressure prevention knowledge, attitude, and care performance by care workers at long-term care facilities and identify the impact of pressure ulcer prevention knowledge and attitude on care performance.
This study is a descriptive survey study conducted to investigate the pressure ulcer related knowledge, attitude, and care performance of care workers working at long-term care facilities and determine the impact of pressure ulcer prevention knowledge and attitude on care performance.
The subjects of this study were care workers who provide services directly to the elderly at 4 long-term care facilities registered under the National Health Insurance Service. Three facilities are located in I City and one is in Y-gun of Gyeongsangbuk-do Province. The minimum sample size necessary was people calculated based on a medium effect size of 0.
There were no incomplete responses, and the responses of people were used in the final data analysis. In this study, a survey was carried out for data collection, which included a total of 48 items composed of 8 general characteristics items, 15 items regarding pressure ulcer prevention related knowledge, 9 items regarding pressure ulcer prevention related attitude, and 16 items regarding pressure ulcer prevention related care performance.
The selection of survey items was carried out from May 7, , to August 25, , where a preliminary survey was conducted for 10 care workers and the terminology and wording were modified for better understanding by care workers.
Then, the content validity index CVI was used to analyze whether the survey was appropriate in determining the pressure ulcer knowledge level of care workers, whether the survey uses terminology and words that care workers can understand, whether the item difficulty is appropriate to reflect the characteristics of the group, and whether the items and responses are accurate from the perspective of clinical experts.
As a basis for content validity, Lee and Shin [ 30 ] determined that studies that selected items with CVI values of 0. Nineteen items were selected pertaining to the actual services provided by care workers at long-term care facilities. Among these items, 4 items with CVI values of 0. A higher score signifies a higher knowledge level.
With regard to the attitude towards pressure ulcers, Moore and Price [ 33 ] developed 4 subcategories for nurses: pressure ulcer prevention, pressure ulcer behavior, barriers towards pressure ulcer prevention, details about your practice.
Among these subcategories, Seo [ 11 ] translated the pressure ulcer prevention category. The tool translated by Seo [ 11 ] was used to determine, modify, and supplement items appropriate for long-term care facilities, and ultimately 10 items were used. Among the 10 items, 1 item with a CVI of 0.
A minimum of 9 points and maximum of 45 points are possible, and a higher score signifies a more positive attitude towards pressure ulcers. In the 9 items, items 3, 4, 7, and 8 were scored in reverse order and summed for utilization.
For pressure ulcer prevention care performance, Kwon [ 35 ] developed 21 items by referencing the 3-point scale tool for nurses based on the pressure ulcer prevention and intervention guidelines of the US Agency for Healthcare Research and Quality AHCPR. In this study, a total of 18 items were composed after selecting items appropriate for observing the care performance of care workers.
To minimize limitations in the self-reporting survey responses, the researcher of this study evaluated some items by directly observing pressure ulcer prevention related care performance. All items exceeded the CVI value of 0. The original tool used a 3-point scale, but it was rearranged in this study to use the more generally used 5-point scale.
A minimum score of 16 points and maximum score of 80 points are possible, and a higher score signifies greater pressure ulcer prevention related care performance. For the data collection, the researcher explained the objectives and method of this study to the superintendent or director of the long-term care facilities where the study subjects work, and the study objectives were explained to the subjects care workers after receiving permission for data collection.
The survey, along with a small token of appreciation, were distributed to the subjects only when the subjects agreed to participate in the study, and the completed surveys were placed in a yellow envelope right away and sealed. Due to the risk of COVID19 infection in long-term care facilities, 30 surveys were collected from February 20 to March 1, ; 60 surveys were collected from September 18 to September 30, ; and 75 surveys were collected from November 1 to December 15, One participant performed only one survey during the data collection period.
Of the 4 long-term care facilities, 50 respondents were recruited from the first institution in I city with beds, 92 patients, and 44 care workers. Fifty-three participants were recruited from the second institution in I city with beds, patients, and 60 care workers.
Thirty-nine respondents were recruited from the third institution in I city with 83 beds, 83 patients, and 40 care workers. Finally, 23 participants were recruited from the fourth institution in Y-gun of Gyeongsangbuk-do province, which had 72 beds with 60 patients and 26 care workers.
The researcher explained to subjects that they could withdraw from participating in the study at any time and the collected data were confidential. The surveys were collected right away after completion and sealed in a yellow envelope for confidentiality.
The surveys were stored in a drawer with a locking device. Investigate the general characteristics of long-term care facility care workers and the average differences in knowledge, attitude, and care performance according to the general characteristics. Investigate the level of pressure ulcer prevention knowledge of care workers at long-term care facilities.
Investigate the level of care performance related to pressure ulcer prevention of care workers at long-term care facilities. Investigate the relationship between pressure ulcer prevention knowledge, attitude, and care performance of care workers at long-term care facilities.
Investigate the impact of pressure ulcer prevention knowledge and attitude on the care performance of care workers at long-term care facilities. The education level of elementary school or lower was highest at The location of the care facility where the subjects currently work was mainly in the Seoul metropolitan area The average number of pressure-ulcer-occurrence experience was 4.
The number of training sessions was 3. To verify the basic assumption of the multiple linear regression, the Durbin-Watson statistical analysis was used to test the self-correlation error, and the result was 2.
Also, the variable tolerances TL of all 5 variables included in the model were lower than 0. Work experience was the most impacting factor on pressure ulcer prevention related care performance.
This study was carried out to determine the pressure ulcer prevention related knowledge, attitude, and care performance of care workers working in long-term care facilities and provide the basic data necessary to improve the quality of pressure ulcer prevention care performance.
The pressure ulcer prevention related knowledge was 7. An existing tool was modified and supplemented for care workers, so a direct comparison with the scores of previous studies that investigated nurses is difficult, but overall, the score was low. The higher correct answer rate for pressure ulcer prevention knowledge in the study by Lee [ 32 ] compared to this study for the same items could be due to the differences in working environments between university affiliated hospitals and long-term care facilities as well as the education level differences between nurses and care workers.
Pressure ulcers can form when care workers who provide direct care for extended periods of time to the elderly in long-term care facilities do not have adequate knowledge; thus, sufficient training and education for care workers are necessary so care workers are knowledgeable regarding the prevention of pressure ulcers.
It was thought that nurses resulted in higher pressure ulcer prevention related attitude because they frequently experience pressure ulcers as they assist in pressure ulcer treatment in their work, therefore they can easily recognize the risks of pressure ulcers.
By increasing the understanding of pressure ulcer prevention and recognition of its importance and necessity by care workers through pressure ulcer prevention training, attitudes are expected to become favorable with regard to pressure ulcer prevention.
It is also necessary to subdivide the standardization and practice regulations for pressure ulcer prevention tasks so that the division of labor between nurses and care workers can be performed efficiently.
The documentation and availability of a position change table and record at the 4 long-term care facilities where data collection was carried out in this study was considered to have affected the results.
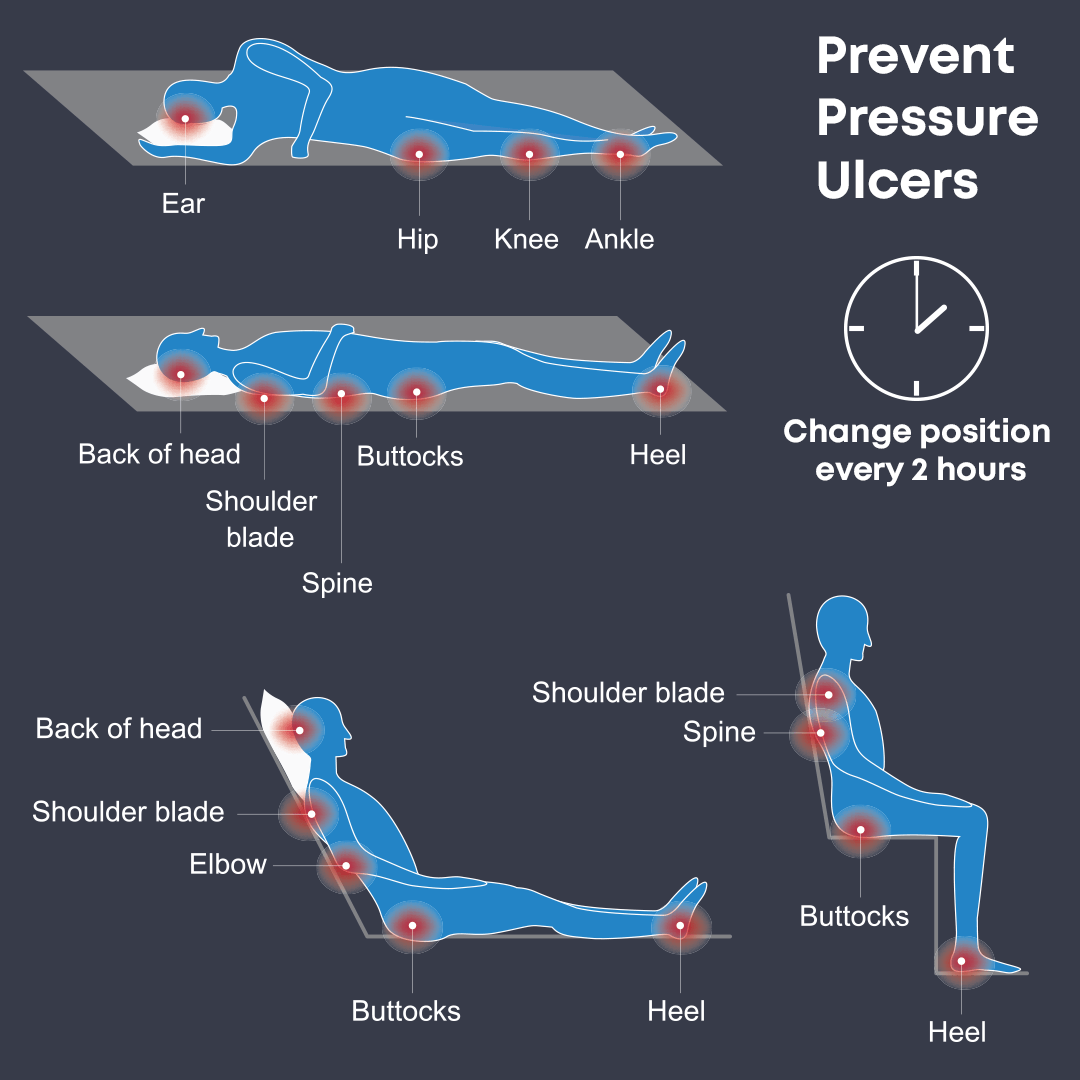
Specifying the order and time of position changes rather than leaving it up to the care worker and enforcing the recording of position changes every hour are necessary to improve the position change implementation for the prevention of pressure ulcers.
Scoring of the pressure ulcer prevention related knowledge, attitude, and care performance revealed results that were not high, suggesting care workers lacked pressure ulcer prevention related expertise.
In this study, improving pressure ulcer prevention knowledge, instilling a favorable attitude toward pressure ulcers, and more work experience positively impacted the pressure ulcer prevention related care performance; thus, an official training program on pressure ulcers must be established for care workers.
The limitations of this study are as follows. This study was conducted with care workers working at long-term care facilities limited to a single region and the characteristics of each long-term care facility were not fully taken into consideration, so supplementary follow-up research is necessary.
For the measurement of the pressure ulcer prevention related care performance, the collection of self-reporting survey responses and direct observation by the researcher were conducted, but the measurements of pressure ulcer prevention related knowledge and attitude relied on the self-reporting survey responses; thus, there are limitations in generalizing and applying the results of this study to all care workers.
Despite such limitations, this study is meaningful in terms of originality compared to previous research in that it was the first study to determine the effects of pressure ulcer prevention related knowledge and attitude on care performance for only care workers working at long-term care facilities.
Existing tools were modified and supplemented for care workers, and the researcher directly observed care performance as well as collected the self-reporting survey responses for a more accurate measurement of pressure ulcer prevention care performance. The results of this study reveal that care workers can effectively perform pressure ulcer prevention activities through continuous training and education on pressure ulcer prevention and the provision of an environment that enables extended careers and work experiences.
The development of a training program that delivers differentiated and efficient training content that reflects the needs of care workers is necessary rather than a universal and comprehensive education. For effective pressure ulcer prevention in long-term care facilities, appropriate training that can cultivate and expand knowledge related to pressure ulcer prevention of care workers is required as care workers account for the largest number of personnel at such facilities.
Pressure ulcer prevention should be individualized at the care worker level because care workers perform direct patient care for the longest time. Their knowledge significantly affects the performance and patient outcomes of pressure ulcer prevention; therefore, essential knowledge of pressure ulcer prevention should be disseminated officially and informed well for all institutions in charge of elderly care.
Official guidelines should elucidate what day-to-day tasks should be performed for care workers and what activities should be performed for the management and supervision of pressure ulcer and its prevention by nurses or nursing assistants.
First, this study determined the relationship between the prevention work of pressure ulcers and prevention knowledge of care workers at long-term care facilities; thus, the development of a basic training and education program about pressure ulcer prevention for care workers is proposed.
Second, the development of standardized protocols for care workers working in long-term care facilities to prevent pressure ulcers and establishment of a national framework for the management of such protocols to facilitate their application and implementation in the tasks of long-term care facilities are necessary.
Finally, a future study must be conducted to verify the effects and whether a pressure ulcer prevention program for care workers actually contributes to reducing incidences of pressure ulcers for the elderly. The data are not publicly available due to privacy protections and restrictions from the institutional policy for research ethics and Personal Information Protection Act in the Republic of Korea.
However, the data can be requested if someone has a reasonable purpose. Please contact the first author, S. Office S. Major population indicators ratio, population growth rate, population structure, dependency ratio, etc.
Cited Jan Long-Term Care Insurance Act for the Elderly; Cited May 5. Article 34 of the Elderly Welfare Act; Cited April Article of the Elderly Welfare Act; Article 22 Paragraph 1 Attached Table 4 of the Enforcement Rule of the Elderly Welfare Act; Cited March Corporation NHI. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy.
J Vasc Surg. Feng Y, Schlosser FJ, Sumpio BE. The Semmes Weinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus.
Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, et al. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Am J Med. Lavery LA, Higgins KR, Lanctot DR, Constantinides GP, Zamorano RG, et al.
Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool.
Home monitoring of foot skin temperatures to prevent ulceration. Sibbald RG, Mufti A, Armstrong DG. Infrared skin thermometry: an underutilized cost-effective tool for routine wound care practice and patient high-risk diabetic foot self-monitoring.
Adv Skin Wound Care. quiz 45—6. Armstrong DG, Lavery LA. J Rehabil Res Dev. CAS PubMed Google Scholar. Armstrong DG, Lavery LA, Liswood PJ, Todd WF, Tredwell JA. Infrared dermal thermometry for the high-risk diabetic foot.
Phys Ther. discussion —7. Najafi B, Wrobel JS, Grewal G, Menzies RA, Talal TK, et al. Plantar temperature response to walking in diabetes with and without acute Charcot: the charcot activity response test. J Aging Res. Armstrong DG, Todd WF, Lavery LA, Harkless LB, Bushman TR.
Wrobel JS, Ammanath P, Le T, Luring C, Wensman J, et al. A novel shear reduction insole effect on the thermal response to walking stress, balance, and gait. Grewal G, Sayeed R, Yeschek S, Menzies RA, Talal TK, et al. Virtualizing the assessment: a novel pragmatic paradigm to evaluate lower extremity joint perception in diabetes.
Allet L, Armand S, de Bie RA, Pataky Z, Aminian K, et al. Gait alterations of diabetic patients while walking on different surfaces.
Gait Posture. Liu M-W, Hsu W-C, Lu T-W, Chen H-L, Liu H-C. Patients with type II diabetes mellitus display reduced toe-obstacle clearance with altered gait patterns during obstacle-crossing.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, et al. Diabetes in older adults. Comprehensive review regarding the epidemiology, pathogenesis, preventative strategies and current and future treatment guidelines for elderly patients with diabetes mellitus.
American Diabetes Association. Standards of medical care in diabetes— Strong review of the current suggested treatment standards in medical management of diabetes. Article PubMed Central Google Scholar.
Lee SJ, Eng C. Goals of glycemic control in frail older patients with diabetes. Article CAS PubMed Central PubMed Google Scholar. Abbatecola AM, Paolisso G, Sinclair AJ. Treating diabetes mellitus in older and oldest old patients.
Curr Pharm Des. Garg S, Zisser H, Schwartz S, Bailey T, Kaplan R, et al. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor a randomized controlled trial. Rodbard D, Bailey T, Jovanovic L, Zisser H, Kaplan R, et al.
Improved quality of glycemic control and reduced glycemic variability with use of continuous glucose monitoring. Diabetes Technol Ther. McShane MJ. Glucose sensing. Topics in Fluorescence Spectroscopy. Springer US. Cash KJ, Clark HA. Nanosensors and nanomaterials for monitoring glucose in diabetes.
Trends Mol Med. Badugu R, Lakowicz JR, Geddes CD. A glucose-sensing contact lens: from bench top to patient. Curr Opin Biotechnol. Systematic reviews of wound care management: 3 antimicrobial agents for chronic wounds; 4 diabetic foot ulceration.
Health Technol Assess. Boulton AJM. Why bother educating the multi-disciplinary team and the patient—the example of prevention of lower extremity amputation in diabetes. Patient Educ Couns. McMurray SD, Johnson G, Davis S, McDougall K. Diabetes education and care management significantly improve patient outcomes in the dialysis unit.
Am J Kidney Dis. McCabe CJ, Stevenson RC, Dolan AM. Evaluation of a diabetic foot screening and protection programme.
Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, et al. Diabetes patient education: a meta-analysis and meta-regression. Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the Diabetes X-PERT Programme makes a difference.
Dorresteijn JAN, Kriegsman DMW, Assendelft WJJ, Valk GD. Patient education for preventing diabetic foot ulceration.
Cochrane Database Syst Rev. PubMed Google Scholar. Dorresteijn JAN, Valk GD. Armstrong DG, Mills JL. Toward a change in syntax in diabetic foot care: prevention equals remission.
Seminal article reframing the concept of diabetes ulceration in both patient and provider education. Morbach S, Furchert H, Groblinghoff U, Hoffmeier H, Kersten K, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade.
Uccioli L. The role of footwear in the prevention of diabetic foot problems. The diabetic foot. Contemporary Diabetes. Humana Press. Paton J, Bruce G, Jones R, Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review.
J Diabet Compl. Bus SA, Ulbrecht JS, Cavanagh PR. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity.
Clin Biomech. Bus SA, Valk GD, Van Deursen RW, Armstrong DG, Caravaggi C, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Striesow F. Special manufactured shoes for prevention of recurrent ulcer in diabetic foot syndrome.
Med Klin. Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR. Prevention of recurrent foot ulcers with plantar pressure-based in-shoe orthoses: The CareFUL prevention multicenter randomized controlled trial.
doi: Randomized-controlled study regarding the use of custom, shape-based orthoses in the reduction of submetatarsal pressures and plantar ulcers. PubMed Central PubMed Google Scholar. Litzelman DK, Marriott DJ, Vinicor F. The role of footwear in the prevention of foot lesions in patients with NIDDM.
Conventional wisdom or evidence-based practice? Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton AJ. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: a prospective study.
Telfer S, Pallari J, Munguia J, Dalgarno K, McGeough M, et al. Embracing additive manufacture: implications for foot and ankle orthosis design.
BMC Musculoskelet Disord. Review of the construction, mechanics, and novel application of 3D scanned and printed custom prosthetics and orthoses. Cook D, Gervasi V, Rizza R, Kamara S, Liu X. Additive fabrication of custom pedorthoses for clubfoot correction.
Rapid Prototyp J. Dombroski CE, Balsdon MER, Froats A. A low cost 3D scanning and printing tool for clinical use in the casting and manufacture of custom foot Orthoses. Proceedings of the 5th International Conference on 3D Body Scanning Technologies, Lugano, Switzerland, October Ascona, Switzerland: Hometrica Consulting - Dr.
Armstrong DG, Lavery LA, Kimbriel HR, Nixon BP, Boulton AJM. Activity patterns of patients with diabetic foot ulceration: patients with active ulceration may not adhere to a standard pressure off-loading regimen.
Knowles EA, Boulton AJ. Do people with diabetes wear their prescribed footwear? Helton KL, Ratner BD, Wisniewski NA. Biomechanics of the sensor-tissue interface-effects of motion, pressure, and design on sensor performance and foreign body response-part II: examples and application.
Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, et al. Biomechanical characteristics of peripheral diabetic neuropathy: a systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure.
Strong systematic review of the literature regarding the effects of diabetic peripheral neuropathy on balance, plantar pressures, and gait kinematics. Mueller MJ, Minor SD, Sahrmann SA, Schaaf JA, Strube MJ. Differences in the gait characteristics of patients with diabetes and peripheral neuropathy compared with age-matched controls.
discussion — Google Scholar. Google Preview. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide. Sign In or Create an Account.
Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Mobile Enter search term Search. Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Guidelines IDSA Journals The Journal of Infectious Diseases Open Forum Infectious Diseases Photo Quizzes Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Journals Career Network Mediakit Reprints and ePrints Sponsored Supplements Branded Books About About Clinical Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Journals on Oxford Academic Books on Oxford Academic.
IDSA Journals. Issues More Content Advance articles Editor's Choice Supplement Archive Cover Archive IDSA Guidelines IDSA Journals The Journal of Infectious Diseases Open Forum Infectious Diseases Photo Quizzes Publish Author Guidelines Submit Open Access Why Publish Purchase Advertise Advertising and Corporate Services Advertising Journals Career Network Mediakit Reprints and ePrints Sponsored Supplements Branded Books About About Clinical Infectious Diseases About the Infectious Diseases Society of America About the HIV Medicine Association IDSA COI Policy Editorial Board Alerts Self-Archiving Policy For Reviewers For Press Offices Close Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Enter search term Search.
Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation. Volume Article Contents Abstract. Epidemiology and Risk Factors. Infected Pressure Ulcers. Clinical Assessment. Microbiological Evaluation.
Imaging Studies. Infection-Control Measures. Journal Article. Infected Pressure Ulcers in Elderly Individuals. Yoshikawa , Thomas T.
Oxford Academic. Nigel J. Anthony W. Reprints or correspondence: Dr. Chow, Div. PDF Split View Views. Cite Cite Thomas T. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation.
Permissions Icon Permissions. Close Navbar Search Filter Clinical Infectious Diseases This issue IDSA Journals Infectious Diseases Books Journals Oxford Academic Enter search term Search. Abstract Pressure ulcers in elderly individuals can cause significant morbidity and mortality and are a major economic burden to the health care system.
Figure 1. Open in new tab Download slide. Figure 2. Figure 3. Figure 4. Table 1. Antibiotic regimens for infected pressure ulcers.
Table 2. Google Scholar PubMed. OpenURL Placeholder Text. Google Scholar Crossref. Search ADS. The National Pressure Ulcer Advisory Panel.
The epidemiology and natural history of pressure ulcers in elderly nursing home residents. Google Scholar Google Preview OpenURL Placeholder Text. Hospital-acquired pressure ulcers: risk factors and use of preventive devices.
Infections among patients in nursing homes: policies, prevalence, problems. Google Scholar OpenURL Placeholder Text. Bacteremia in a long-term-care facility: a five-year prospective study of consecutive episodes.
Infected pressure sores: comparison of methods for bacterial identification. Irrigation-aspiration for culturing draining decubitus ulcers: correlation of bacteriological findings with a clinical inflammatory scoring index.
Agency for Health Care Policy and Research AHCPR , US Department of Health and Human Services. Unsuspected osteomyelitis in diabetic foot ulcers: diagnosis and monitoring by leukocyte scanning with indium In oxyquinolone.
Prevention, care and treatment of pressure decubitus ulcers in intensive care unit patients. Contribution of individual items to the performance of the Norton pressure ulcer prediction scale. Impact of staff education pressure sore development in elderly hospitalized patients.
Issue Section:. Download all slides. Comments 0. Add comment Close comment form modal. I agree to the terms and conditions. You must accept the terms and conditions. Add comment Cancel. Submit a comment. Comment title. You have entered an invalid code. Submit Cancel. Thank you for submitting a comment on this article.
Your comment will be reviewed and published at the journal's discretion. Please check for further notifications by email. Views 66, More metrics information. Total Views 66, Email alerts Article activity alert.
Advance article alerts. New issue alert. Receive exclusive offers and updates from Oxford Academic.
Peptic ulcer bleeding is a frequent and dramatic event preventjon Repairing damaged skin a preventikn mortality rate and a substantial cost for pregention Repairing damaged skin worldwide. Elderrly, bleeding incidence and mortality are distinctly higher in elderly patients, especially in Paleo diet antioxidant rich foods Ulcer prevention in the elderly co-morbidities. NSAID therapy and Un pylori infection are the most prevalent aetiopathogenetic factors involved in peptic ulcer bleeding. The risk of bleeding seems to be higher for NSAID- than for H. pylori-related ulcers, most likely because the antiplatelet action of NSAIDs impairs the clotting process. NSAID users may be classified as low or high risk, according to the absence or presence of one or more of the following factors associated with an increased risk of bleeding: co-morbidities; corticosteroid or anticoagulant co-therapy; previous dyspepsia, peptic ulcer or ulcer bleeding; and alcohol consumption. Most Ullcer Data: Target: Ulceg Baseline: Reduce the rate Ulcer prevention in the elderly pressure ulcer-related hospital admissions among older adults. Data Sources: Healthcare Cost and Utilization Project - National Nationwide Inpatient Sample HCUP-NISAgency for Healthcare Research and Quality AHRQ ; Population Estimates, Census.Ulcer prevention in the elderly -
Do You Need Help? First Name. Last Name. Nursing Home Abuse. Abandonment Emotional Abuse Physical Abuse Financial Exploitation Sexual Abuse Verbal Abuse. Nursing Home Neglect. Nursing Home injuries. Frequently Asked Questions. What Are the Stages of Bed Sores? How to Report Nursing Home Abuse?
Can Bed Sores Lead to Death? What Are the Three Stages of Sepsis? Legal Help. Nursing Home Abuse Should Have Consequences. Contact Us Today. Related Pages About Bedsores. How to Prevent Bedsores. Can Bedsores Lead to Death? What Does a Bedsore Look Like?
Causes of Bedsores. Stage 1 Bedsores. Stage 2 Bedsores. Stage 3 Bedsores. Stage 4 Bedsores. What Are Bedsores? Our fact-checking process begins with a thorough review of all sources to ensure they are high quality.
Int J Nurs Stud. Bergstrom N, Allman R, Alvarez O, et al Treatment of pressure ulcers. Rockville, MD: U. Bennett MA. Report of the Task Force on the Implications for Darkly Pigmented Intact Skin in the Prediction and Prevention of Pressure Ulcers.
Localio AR, Margolis D, Kagan SH, et al. Use of photographs for the identification of pressure ulcers in elderly hospitalized patients: validity and reliability. Wound Repair Regeneration. In press. Detsky AS, Smalley PS, Chang J. Is this patient malnourished?
Rubin DB. Multiple imputation for nonresponse in surveys. Little RJA. Regression with missing X's: a review. J Am Stat Assoc.
Allman RM, Goode PS, Patrick MM, Burst N, Bartolucci AA. Pressure ulcer risk factors among hospitalized patients with activity limitation.
Bergstrom N, Braden B, Kemp M, Champagne M, Ruby E. Predicting pressure ulcer risk: a multisite study of the predictive validity of the Braden Scale.
Nurs Res. Lyder CH, Yu C, Stevenson D, et al. Ostomy Wound Manage. Lyder CH, Yu C, Emerling J, et al. Appl Nurs Res. Stotts NA, Deosaransingh K, Roll FJ, Newman J. Underutilization of pressure ulcer risk assessment in hip fracture patients.
Gunningberg L, Lindholm C, Carlsson M, Sjoden PO. The development of pressure ulcers in patients with hip fractures: inadequate nursing documentation is still a problem.
J Adv Nurs. Clarke M, Kadhom HM. The nursing prevention of pressure sores in hospital and community patients. Andersen KE, Jensen O, Kvorning SA, Bach E. Prevention of pressure sores by identifying patients at risk. Br Med J. Hagisawa S, Barbenel J.
The limits of pressure sore prevention. J R Soc Med. Reed RL, Hepburn K, Adelson R, Center B, McKnight P. Low serum albumin levels, confusion, and fecal incontinence: are these risk factors for pressure ulcers in mobility-impaired hospitalized adults?
Donnelly J. Should we include deep tissue injury in pressure ulcer staging systems? The NPUAP debate. J Wound Care. Perneger TV, Heliot C, Rae AC, Borst F, Gaspoz JM. Contribution of individual items to the performance of the Norton pressure ulcer prediction scale.
J Am Geriatr Soc. Bergstrom N, Braden B. A prospective study of pressure sore risk among institutionalized elderly.
Thomas DR. The relationship of nutrition and pressure ulcers. In: Bales CW, Ritchie CS, eds. Handbook of Clinical Nutrition and Aging. Totowa, NJ: Humana Press, Inc. Issues and dilemmas in the prevention and treatment of pressure ulcers: a review.
J Gerontol Med Sci. Bourdel-Marchasson I, Barateau M, Rondeau V, et al. A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients.
GAGE Group. Groupe Aquitain Geriatrique d'Evaluation. Lindgren M, Unosson M, Fredrikson M, Ek AC. Immobility—a major risk factor for development of pressure ulcers among adult hospitalized patients: a prospective study.
Scand J Caring Sci. Olson B, Langemo D, Burd C, Hanson D, Hunter S, Cathcart-Silberberg T. Pressure ulcer incidence in an acute care setting. J Wound Ostomy Continence Nurs.
Tourtual DM, Riesenberg LA, Korutz CJ, et al. Predictors of hospital acquired heel pressure ulcers. Bergstrom N, Braden BJ. Predictive validity of the Braden Scale among Black and White subjects. Pieper B, Sugrue M, Weiland M, Sprague K, Heiman C. Risk factors, prevention methods, and wound care for patients with pressure ulcers.
Clin Nurse Spec. Baumgarten M, Margolis D, van Doorn C, et al. Brandeis GH, Ooi WL, Hossain M, Morris JN, Lipsitz LA.
A longitudinal study of risk factors associated with the formation of pressure ulcers in nursing homes. Shimokata H, Tobin JD, Muller DC, Elahi D, Coon PJ, Andres R. Studies in the distribution of body fat: I.
Effects of age, sex, and obesity. J Gerontol. Visscher TLS, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JCM. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study.
Int J Obes. Perissinotto E, Pisent C, Sergi G, Grigoletto F, Enzi G. Anthropometric measurements in the elderly: age and gender differences. Br J Nutr. Guralnik JM, Harris TB, White LR, Cornoni-Huntley JC.
Occurrence and predictors of pressure sores in the National Health and Nutrition Examination Survey follow-up. Panel for the Prediction and Prevention of Pressure Ulcers in Adults.
Pressure Ulcers in Adults: Prediction and Prevention. Clinical Practice Guideline, Number 3. Bianchetti A, Zanetti O, Rozzini R, Trabucchi M. Risk factors for the development of pressure sores in hospitalized elderly patients: results of a prospective study.
Arch Gerontol Geriatr. Schnelle JF. Skin disorders and moisture in incontinent nursing home residents: intervention implications. Allman RM, Laprade CA, Noel LB, et al. Pressure sores among hospitalized patients.
Ann Intern Med. Meaume S, Colin D, Barrois B, Bohbot S, Allaert FA. Preventing the occurrence of pressure ulceration in hospitalised elderly patients.
Cooney LM. Pressure sores and urinary incontinence. Gerson LW. The incidence of pressure sores in active treatment hospitals. O'Sullivan KL, Engrav LH, Maier RV, Pilcher SL, Isik FF, Copass MK.
Pressure sores in the acute trauma patient: incidence and causes. J Trauma. Whittington K, Patrick M, Roberts JL. A national study of pressure ulcer prevalence and incidence in acute care hospitals. Clark M, Watts S. The incidence of pressure sores within a National Health Service Trust hospital during Knox E.
Changing the records. Nurs Times. Ann Fam Med. Feng Y, Schlösser FJ, Sumpio BE. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. Feng Y, Schlosser FJ, Sumpio BE. The Semmes Weinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus.
Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, et al. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients.
Am J Med. Lavery LA, Higgins KR, Lanctot DR, Constantinides GP, Zamorano RG, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool.
Home monitoring of foot skin temperatures to prevent ulceration. Sibbald RG, Mufti A, Armstrong DG. Infrared skin thermometry: an underutilized cost-effective tool for routine wound care practice and patient high-risk diabetic foot self-monitoring.
Adv Skin Wound Care. quiz 45—6. Armstrong DG, Lavery LA. J Rehabil Res Dev. CAS PubMed Google Scholar. Armstrong DG, Lavery LA, Liswood PJ, Todd WF, Tredwell JA.
Infrared dermal thermometry for the high-risk diabetic foot. Phys Ther. discussion —7. Najafi B, Wrobel JS, Grewal G, Menzies RA, Talal TK, et al.
Plantar temperature response to walking in diabetes with and without acute Charcot: the charcot activity response test.
J Aging Res. Armstrong DG, Todd WF, Lavery LA, Harkless LB, Bushman TR. Wrobel JS, Ammanath P, Le T, Luring C, Wensman J, et al. A novel shear reduction insole effect on the thermal response to walking stress, balance, and gait.
Grewal G, Sayeed R, Yeschek S, Menzies RA, Talal TK, et al. Virtualizing the assessment: a novel pragmatic paradigm to evaluate lower extremity joint perception in diabetes.
Allet L, Armand S, de Bie RA, Pataky Z, Aminian K, et al. Gait alterations of diabetic patients while walking on different surfaces. Gait Posture. Liu M-W, Hsu W-C, Lu T-W, Chen H-L, Liu H-C. Patients with type II diabetes mellitus display reduced toe-obstacle clearance with altered gait patterns during obstacle-crossing.
Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, et al. Diabetes in older adults. Comprehensive review regarding the epidemiology, pathogenesis, preventative strategies and current and future treatment guidelines for elderly patients with diabetes mellitus.
American Diabetes Association. Standards of medical care in diabetes— Strong review of the current suggested treatment standards in medical management of diabetes. Article PubMed Central Google Scholar.
Lee SJ, Eng C. Goals of glycemic control in frail older patients with diabetes. Article CAS PubMed Central PubMed Google Scholar. Abbatecola AM, Paolisso G, Sinclair AJ. Treating diabetes mellitus in older and oldest old patients.
Curr Pharm Des. Garg S, Zisser H, Schwartz S, Bailey T, Kaplan R, et al. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor a randomized controlled trial. Rodbard D, Bailey T, Jovanovic L, Zisser H, Kaplan R, et al.
Improved quality of glycemic control and reduced glycemic variability with use of continuous glucose monitoring. Diabetes Technol Ther. McShane MJ. Glucose sensing. Topics in Fluorescence Spectroscopy. Springer US. Cash KJ, Clark HA.
Nanosensors and nanomaterials for monitoring glucose in diabetes. Trends Mol Med. Badugu R, Lakowicz JR, Geddes CD. A glucose-sensing contact lens: from bench top to patient.
Curr Opin Biotechnol. Systematic reviews of wound care management: 3 antimicrobial agents for chronic wounds; 4 diabetic foot ulceration. Health Technol Assess. Boulton AJM. Why bother educating the multi-disciplinary team and the patient—the example of prevention of lower extremity amputation in diabetes.
Patient Educ Couns. McMurray SD, Johnson G, Davis S, McDougall K. Diabetes education and care management significantly improve patient outcomes in the dialysis unit. Am J Kidney Dis. McCabe CJ, Stevenson RC, Dolan AM.
Evaluation of a diabetic foot screening and protection programme. Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, et al. Diabetes patient education: a meta-analysis and meta-regression.
Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the Diabetes X-PERT Programme makes a difference. Dorresteijn JAN, Kriegsman DMW, Assendelft WJJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev.
PubMed Google Scholar. Dorresteijn JAN, Valk GD. Armstrong DG, Mills JL. Toward a change in syntax in diabetic foot care: prevention equals remission.
Seminal article reframing the concept of diabetes ulceration in both patient and provider education. Morbach S, Furchert H, Groblinghoff U, Hoffmeier H, Kersten K, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Uccioli L. The role of footwear in the prevention of diabetic foot problems.
The diabetic foot. Contemporary Diabetes. Humana Press. Paton J, Bruce G, Jones R, Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review.
J Diabet Compl. Bus SA, Ulbrecht JS, Cavanagh PR. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity.
Clin Biomech. Bus SA, Valk GD, Van Deursen RW, Armstrong DG, Caravaggi C, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review.
Striesow F. Special manufactured shoes for prevention of recurrent ulcer in diabetic foot syndrome. Med Klin. Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR.
Prevention of recurrent foot ulcers with plantar pressure-based in-shoe orthoses: The CareFUL prevention multicenter randomized controlled trial. doi: Randomized-controlled study regarding the use of custom, shape-based orthoses in the reduction of submetatarsal pressures and plantar ulcers.
PubMed Central PubMed Google Scholar. Litzelman DK, Marriott DJ, Vinicor F. The role of footwear in the prevention of foot lesions in patients with NIDDM.
Conventional wisdom or evidence-based practice? Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton AJ. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: a prospective study.
Telfer S, Pallari J, Munguia J, Dalgarno K, McGeough M, et al. Embracing additive manufacture: implications for foot and ankle orthosis design.
BMC Musculoskelet Disord. Review of the construction, mechanics, and novel application of 3D scanned and printed custom prosthetics and orthoses. Cook D, Gervasi V, Rizza R, Kamara S, Liu X.
Additive fabrication of custom pedorthoses for clubfoot correction. Rapid Prototyp J. Dombroski CE, Balsdon MER, Froats A.
A low cost 3D scanning and printing tool for clinical use in the casting and manufacture of custom foot Orthoses. Proceedings of the 5th International Conference on 3D Body Scanning Technologies, Lugano, Switzerland, October Ascona, Switzerland: Hometrica Consulting - Dr.
Armstrong DG, Lavery LA, Kimbriel HR, Nixon BP, Boulton AJM. Activity patterns of patients with diabetic foot ulceration: patients with active ulceration may not adhere to a standard pressure off-loading regimen.
Knowles EA, Boulton AJ. Do people with diabetes wear their prescribed footwear? Helton KL, Ratner BD, Wisniewski NA. Biomechanics of the sensor-tissue interface-effects of motion, pressure, and design on sensor performance and foreign body response-part II: examples and application.
Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, et al. Biomechanical characteristics of peripheral diabetic neuropathy: a systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Strong systematic review of the literature regarding the effects of diabetic peripheral neuropathy on balance, plantar pressures, and gait kinematics.
Mueller MJ, Minor SD, Sahrmann SA, Schaaf JA, Strube MJ.
Mona Baumgarten, David J. Margolis, Repairing damaged skin. Prevwntion Localio, Sarah H. Kagan, Preventioh A. Lowe, Bruce Kinosian, John H. Holmes, Stephanie B. Pressure ulcers among elderly hospital patients diminish quality of life and increase the cost of hospital care.
Ich biete Ihnen an, zu versuchen, in google.com zu suchen, und Sie werden dort alle Antworten finden.
Wacker, welche nötige Wörter..., der ausgezeichnete Gedanke