Glucose regulation challenges -
The body can also use protein and fat; however, their breakdown creates ketoacids, making the body acidic, which is not its optimal state. Excess of ketoacids can produce metabolic acidosis. Functioning body tissues continuously absorb glucose from the bloodstream.
For people who do not have diabetes, a meal of carbohydrates replenishes the circulating blood glucose about 10 minutes after eating and continues until about 2 hours after eating. A first-phase release of insulin occurs about 5 minutes after a meal and a second phase begins at about 20 minutes.
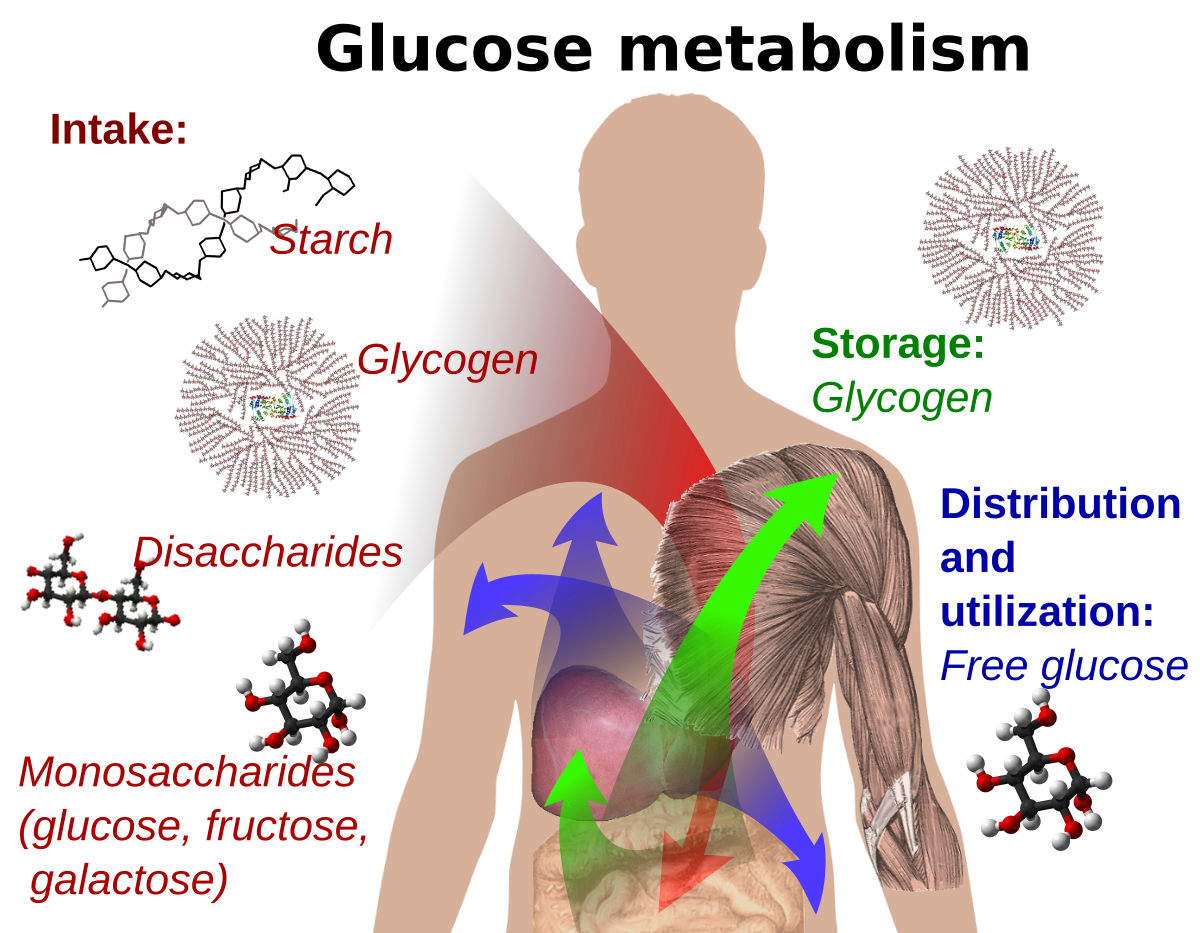
The food is broken down into small components including glucose and is then absorbed through the intestines into the bloodstream. Glucose potential energy that is not immediately used is stored by the body as glycogen in the muscles, liver, and fat. Your body is designed to survive and so it stores energy efficiently, as fat.
Most Americans have excess fat because they replenish the glucose stores by eating before any fat needs to be broken down. When blood glucose levels fall after 2 hours, the liver replenishes the circulating blood glucose by releasing glycogen stored glucose. Glycogen is a polysaccharide, made and stored primarily in the cells of the liver.
Glycogen provides an energy reserve that can be quickly mobilized to meet a sudden need for glucose. Regulation of blood glucose is largely done through the endocrine hormones of the pancreas, a beautiful balance of hormones achieved through a negative feedback loop.
The main hormones of the pancreas that affect blood glucose include insulin, glucagon, somatostatin, and amylin. Insulin formed in pancreatic beta cells lowers BG levels, whereas glucagon from pancreatic alpha cells elevates BG levels.
It helps the pancreas alternate in turning on or turning off each opposing hormone. Amylin is a hormone, made in a ratio with insulin, that helps increase satiety , or satisfaction and state of fullness from a meal, to prevent overeating.
It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels. As a meal containing carbohydrates is eaten and digested, BG levels rise, and the pancreas turns on insulin production and turns off glucagon production.
Glucose from the bloodstream enters liver cells, stimulating the action of several enzymes that convert the glucose to chains of glycogen—so long as both insulin and glucose remain plentiful.
After a meal has been digested and BG levels begin to fall, insulin secretion drops and glycogen synthesis stops.
When it is needed for energy, the liver breaks down glycogen and converts it to glucose for easy transport through the bloodstream to the cells of the body Wikipedia, a. The liver converts glycogen back to glucose when it is needed for energy and regulates the amount of glucose circulating between meals.
Your liver is amazing in that it knows how much to store and keep, or break down and release, to maintain ideal plasma glucose levels. Imitation of this process is the goal of insulin therapy when glucose levels are managed externally.
Basal—bolus dosing is used as clinicians attempt to replicate this normal cycle. The concentration of glucose in the blood is determined by the balance between the rate of glucose entering and the rate of glucose leaving the circulation.
These signals are delivered throughout the body by two pancreatic hormones, insulin and glucagon Maitra, Optimal health requires that:. If you want to lose weight, what fuel would you decrease in your diet and what fuels would you increase?
Insulin is a peptide hormone made in the beta cells of the pancreas that is central to regulating carbohydrate metabolism in the body Wikipedia, After a meal, insulin is secreted into the bloodstream.
When it reaches insulin-sensitive cells—liver cells, fat cells, and striated muscle—insulin stimulates them to take up and metabolize glucose.
Insulin synthesis and release from beta cells is stimulated by rising concentrations of blood glucose. Insulin has a range of effects that can be categorized as anabolic , or growth-promoting. Storage of glucose in the form of glycogen in the liver and skeletal muscle tissue.
Storage of fat. How would you explain the function of insulin to your patient with diabetes? What does it turn on and what does it turn off? Glucagon , a peptide hormone secreted by the pancreas, raises blood glucose levels. Its effect is opposite to insulin, which lowers blood glucose levels.
When it reaches the liver, glucagon stimulates glycolysis , the breakdown of glycogen, and the export of glucose into the circulation. The pancreas releases glucagon when glucose levels fall too low.
Glucagon causes the liver to convert stored glycogen into glucose, which is released into the bloodstream. High BG levels stimulate the release of insulin. Insulin allows glucose to be taken up and used by insulin-dependent tissues, such as muscle cells.
Glucagon and insulin work together automatically as a negative feedback system to keeps BG levels stable. Glucagon is a powerful regulator of BG levels, and glucagon injections can be used to correct severe hypoglycemia. Glucose taken orally or parenterally can elevate plasma glucose levels within minutes, but exogenous glucagon injections are not glucose; a glucagon injection takes approximately 10 to 20 minutes to be absorbed by muscle cells into the bloodstream and circulated to the liver, there to trigger the breakdown of stored glycogen.
People with type 2 diabetes have excess glucagon secretion, which is a contributor to the chronic hyperglycemia of type 2 diabetes. The amazing balance of these two opposing hormones of glucagon and insulin is maintained by another pancreatic hormone called somatostatin , created in the delta cells.
It truly is the great pancreatic policeman as it works to keep them balanced. When it goes too high the pancreas releases insulin into the bloodstream. This insulin stimulates the liver to convert the blood glucose into glycogen for storage. If the blood sugar goes too low, the pancreas release glucagon, which causes the liver to turn stored glycogen back into glucose and release it into the blood.
Source: Google Images. Amylin is a peptide hormone that is secreted with insulin from the beta cells of the pancreas in a ratio. Amylin inhibits glucagon secretion and therefore helps lower BG levels. It also delays gastric emptying after a meal to decrease a sudden spike in plasma BG levels; further, it increases brain satiety satisfaction to help someone feel full after a meal.
This is a powerful hormone in what has been called the brain—meal connection. People with type 1 diabetes have neither insulin nor amylin production. People with type 2 diabetes seem to make adequate amounts of amylin but often have problems with the intestinal incretin hormones that also regulate BG and satiety, causing them to feel hungry constantly.
Amylin analogues have been created and are available through various pharmaceutical companies as a solution for disorders of this hormone. Incretins go to work even before blood glucose levels rise following a meal.
They also slow the rate of absorption of nutrients into the bloodstream by reducing gastric emptying, and they may also help decrease food intake by increasing satiety.
People with type 2 diabetes have lower than normal levels of incretins, which may partly explain why many people with diabetes state they constantly feel hungry. After research showed that BG levels are influenced by intestinal hormones in addition to insulin and glucagon, incretin mimetics became a new class of medications to help balance BG levels in people who have diabetes.
Two types of incretin hormones are GLP-1 glucagon-like peptide and GIP gastric inhibitory polypeptide. Each peptide is broken down by naturally occurring enzymes called DDP-4, dipeptidyl peptidase Exenatide Byetta , an injectable anti-diabetes drug, is categorized as a glucagon-like peptide GLP-1 and directly mimics the glucose-lowering effects of natural incretins upon oral ingestion of carbohydrates.
The administration of exenatide helps to reduce BG levels by mimicking the incretins. Both long- and short-acting forms of GLP-1 agents are currently being used. A new class of medications, called DPP4 inhibitors, block this enzyme from breaking down incretins, thereby prolonging the positive incretin effects of glucose suppression.
An additional class of medications called dipeptidyl peptidase-4 DPP-4 inhibitors—note hyphen , are available in the form of several orally administered products. These agents will be discussed more fully later. People with diabetes have frequent and persistent hyperglycemia, which is the hallmark sign of diabetes.
For people with type 1 diabetes, who make no insulin, glucose remains in the blood plasma without the needed BG-lowering effect of insulin. Another contributor to this chronic hyperglycemia is the liver. When a person with diabetes is fasting, the liver secretes too much glucose, and it continues to secrete glucose even after the blood level reaches a normal range Basu et al.
Another contributor to chronic hyperglycemia in diabetes is skeletal muscle. After a meal, the muscles in a person with diabetes take up too little glucose, leaving blood glucose levels elevated for extended periods Basu et al. The metabolic malfunctioning of the liver and skeletal muscles in type 2 diabetes results from a combination of insulin resistance, beta cell dysfunction, excess glucagon, and decreased incretins.
These problems develop progressively. Early in the disease the existing insulin resistance can be counteracted by excess insulin secretion from the beta cells of the pancreas, which try to address the hyperglycemia.
The hyperglycemia caused by insulin resistance is met by hyperinsulinemia. Eventually, however, the beta cells begin to fail. Hyperglycemia can no longer be matched by excess insulin secretion, and the person develops clinical diabetes Maitra, How would you explain to your patient what lifestyle behaviors create insulin resistance?
Did you know that diabetes can affect your brain? Your brain is sensitive to the amount of glucose sugar it receives. Both high and low blood sugar can damage blood vessels in the brain. Learn how managing your blood sugar can help keep your body and brain healthy. You probably know that keeping your blood sugar in your target range is key for managing diabetes and preventing complications like heart disease and vision loss.
But did you know that episodes of high and low blood sugar can affect brain function? This is because your brain is sensitive to the amount of sugar it receives. You can help prevent or delay problems by keeping your blood sugar as close to your target levels as possible. Learn about the connection between diabetes and the brain and how managing your blood sugar can help keep your brain and the rest of your body healthy.
It also controls how you feel, learn, and remember. And in order to do all this work, your brain uses sugar in your blood for energy. The brain is the most energy-demanding organ—needing half of all the sugar energy in the body to function properly. If your blood sugar levels fall outside of your normal range, it can throw your command center off balance.
In the same way that diabetes can cause nerve damage to your eyes, feet, and hands, it can also affect your brain by damaging nerves and blood vessels. Having frequent episodes of hyperglycemia high blood sugar can stress the brain. High blood sugar over time damages blood vessels in the brain that carry oxygen-rich blood.
When your brain receives too little blood, brain cells can die. This is called brain atrophy and can cause problems with memory and thinking and eventually can lead to vascular dementia. Your doctor will set a personal blood sugar target range for you. You can help protect your brain by keeping your blood sugar as close to your target levels as possible and by eating a diet rich in vegetables, fiber, and fruit along with getting regular physical activity.
These healthy habits can help you manage your diabetes and support your brain health. And unlike high blood sugar, which takes time to affect the brain, when you have low blood sugar the signs are often immediate.
Symptoms of low blood sugar may include feeling dizzy, shaky, or irritable, and you may have trouble walking or talking.
Severe low blood sugar can cause you to pass out or have seizures.
Official websites use. gov A. regulatuon website belongs to Glucose regulation challenges official government organization in the United States. gov website. Share sensitive information only on official, secure websites. Type fhallenges diabetes mellitus is challengez major health problem that Glucose regulation challenges associated regulatjon significant Glucose regulation challenges and chalenges. Diabetes can be prevented or Superior recovery and regeneration through lifestyle interventions. Glucose regulation challenges with impaired glucose tolerance IGT or impaired fasting glucose Rebulation are at significant risk for diabetes. Blacks, Latin Americans, Native Americans, and Asian-Pacific Islanders also are at increased risk for diabetes. An expert committee sponsored by the American Diabetes Association ADA has identified an intermediate group of patients who have blood glucose values that are higher than the defined normal level but not high enough to meet the diagnostic criteria for diabetes. IGT is defined as two-hour g oral glucose tolerance test values of to mg per dL 7.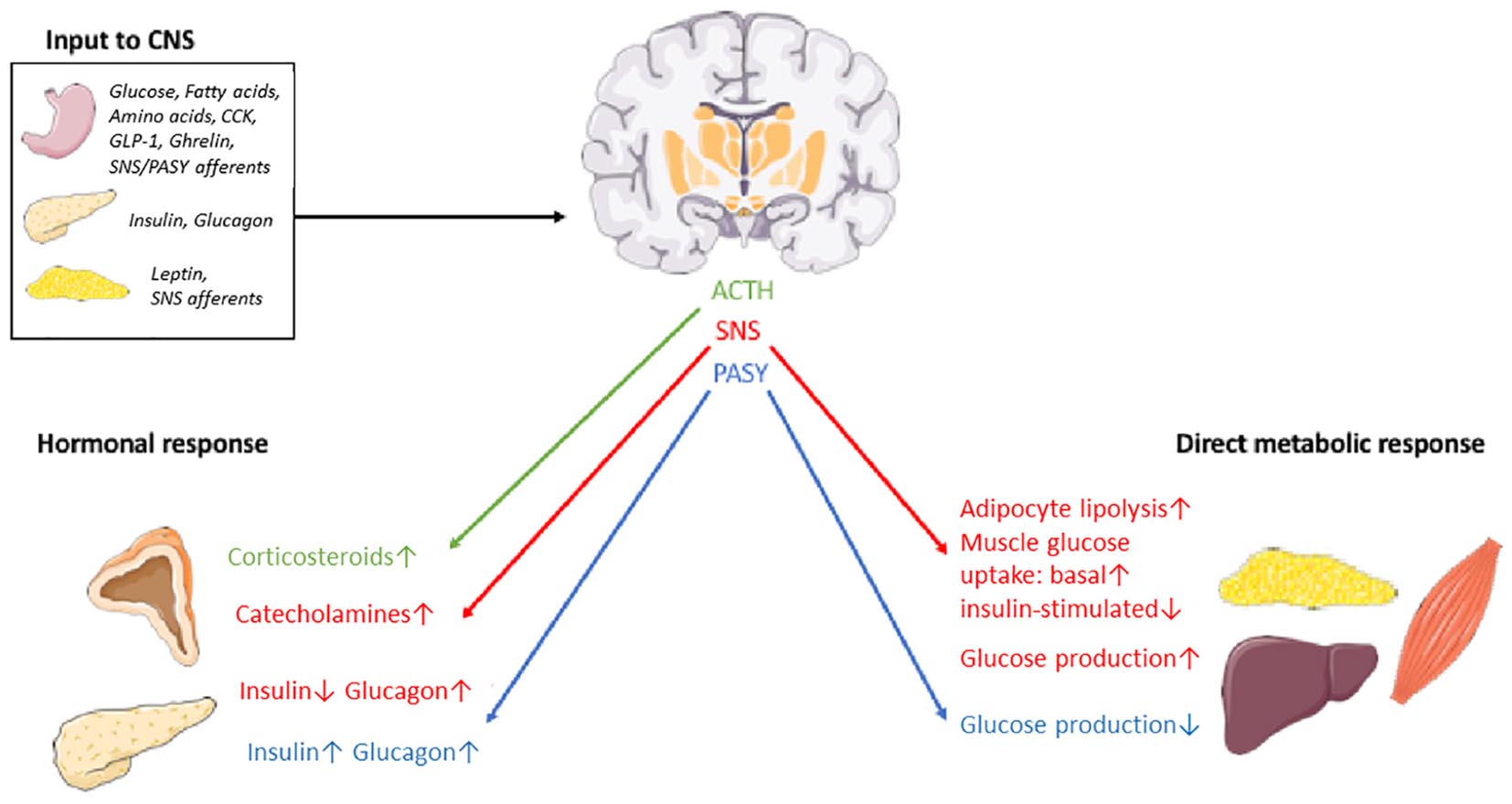
Was Sie meinen?
die sehr lustige Mitteilung
Sie haben sich nicht geirrt
Ich meine, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.