
Self-care planning in diabetes management -
However, having diabetes does't exclude you from eating your favourite foods or going to your favourite restaurants. But you need to know that different foods affect your blood sugar differently.
Activity has many health benefits in addition to losing weight. Physical activity lowers cholesterol, improves blood pressure, lowers stress and anxiety, and improves your mood. Being active can also keep your blood glucose levels in check and your diabetes under control. Regular monitoring of your blood sugar levels gives you the information you need to make decisions.
Most people find that insulin injections are easier than they thought. People with diabetes have a high chance of getting high blood pressure and high cholesterol. You may be asked to take medicine to prevent or treat these conditions.
Medicines may include:. Do not smoke or use e-cigarettes. Smoking makes diabetes worse. If you do smoke, work with your provider to find a way to quit. If you have diabetes, you should see your provider every 3 months, or as often as instructed.
At these visits, your provider may:. Talk to your provider about any vaccines you may need, such as the yearly flu shot and the hepatitis B and pneumonia shots. Visit the dentist every 6 months. Also, see your eye doctor once a year, or as often as instructed. American Diabetes Association Professional Practice Committee.
Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes Diabetes Care. PMID: pubmed. Retinopathy, Neuropathy, and Foot Care: Standards of Medical Care in Diabetes Brownlee M, Aiello LP, Sun JK, et al. Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ , eds.
Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap Riddle MC, Ahmann AJ. Therapeutics of type 2 diabetes. Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.
Editorial team. Type 2 diabetes - self-care. Symptoms of Type 2 Diabetes. You may not have any symptoms. If you do have symptoms, they may include: Hunger Thirst Urinating a lot, getting up more often than usual at night to urinate Blurry vision More frequent or long lasting infections Trouble having an erection Trouble healing cuts on your skin Red skin rashes in parts of your body Tingling or loss of sensation in your feet.
Take Control of Your Diabetes. Steps include: Checking your blood sugar at home Keeping a healthy diet Being physically active Also, be sure to take any medicine or insulin as instructed.
These providers include a: Dietitian Diabetes pharmacist Diabetes educator. Eat Healthy Foods and Manage Your Weight. Regular exercise is good for people with diabetes. It lowers blood sugar. Exercise also: Improves blood flow Lowers blood pressure It helps burn extra fat so that you can keep your weight down.
Check Your Blood Sugar. Many people with type 2 diabetes need to check their blood sugar only once or twice a day.
Some people need to check more often. Please consult your healthcare team before starting a new exercise regimen, as their advice will guide you in developing a safe and effective plan tailored to your needs and abilities. Mental self-care involves taking care of your mental and emotional health.
For people with diabetes, managing the condition is usually found to be stressful and emotionally challenging. Research 4 5 shows that there is an increase in mental health problems for people with diabetes:.
These statistics show that diabetes often leads to diabetes distress or even diabetes burnout, where both of which have a profoundly negative impact on your health. Some effective mental self-care strategies for people with diabetes include:. These practices will help you manage the emotional and mental toll of living with the condition and improve your quality of life.
This way, you build resilience and reduce stress and anxiety by prioritising your mental health. Your healthcare team plays a critical role in your diabetes management, but they can only help you as much as the information you provide them.
Effective self-care practices give you valuable insights and data about your condition. On the other hand, it assists your healthcare team to make more informed decisions about your treatment plan.
By tracking your blood sugar levels, physical activity, food intake, and emotional well-being, you provide your healthcare team with a comprehensive understanding of your diabetes management.
This information gives them the ability to identify areas for improvement, make adjustments to your medication regimen, and provide personalized guidance on self-care practices. Strive to build self-care practices and do them on a daily basis as they help you manage your condition more effectively and improve your quality of life.
It provides healthcare professionals with valuable information about your daily routines and habits, which reflects in developing personalized treatment plans and making more informed decisions about your therapy. Self-care practices also allow you to take control of your health and make positive changes to your lifestyle.
Overall, self-care is a critical component of diabetes management and a necessary part of achieving better outcomes for people with diabetes. Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment. Post comment. Whitepaper: Diabetes and its Effects on Every System in the Body. Get ypour FREE copy now! Skip to content. The Role of Self-Care in Diabetes Management. But what exactly is self-care in diabetes management, and why is it important?
What is Self-Care? Diabetes Self-Management Education DSME First, you need to be trained on how to manage your type of diabetes best. Some key topics covered in DSME programs include: Understanding the different types of diabetes and their effects on the body The importance of regular blood glucose monitoring and interpreting the results Developing a personalised meal plan based on individual needs and preferences The benefits of regular physical activity and how to incorporate it into daily routines Recognizing and managing the signs and symptoms of high and low blood sugar levels Identifying and managing stress and other emotional issues related to diabetes Proper use of medications and insulin therapy, if applicable These programs often include individualised assessments, goal setting, problem-solving, and ongoing support from qualified professionals.
Gaining a Better Overview of Blood Sugar Levels Over Time Managing blood sugar levels is a crucial aspect of diabetes self-care. Physical Self-Care Physical self-care is essential for maintaining good health and managing diabetes effectively.
Regular physical activity has numerous benefits for people with diabetes, including: Improved insulin sensitivity, which helps the body use insulin more effectively Lower blood sugar levels and better overall blood sugar control Increased energy and reduced fatigue Weight management, which reduces the risk of diabetes-related complications Lower blood pressure and cholesterol levels, reducing the risk of heart disease Experts recommend 3 at least minutes of moderate-intensity physical activity or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days per week.
Mental Self-Care Mental self-care involves taking care of your mental and emotional health. Some effective mental self-care strategies for people with diabetes include: Practicing mindfulness e.
Dibaetes mellitus DM is a chronic progressive metabolic disorder Self-care planning in diabetes management by hyperglycemia mainly diabettes Natural energy supplements absolute Self-caree 1 DM or relative Type Enhances gut health DM deficiency diabetew insulin hormone. World Health Organization estimates managenent more than million people Self-care planning in diabetes management Improve working memory DM. Self-are number is likely to diaberes than double by without any intervention. The needs of diabetic patients are not only limited to adequate glycemic control but also correspond with preventing complications; disability limitation and rehabilitation. There are seven essential self-care behaviors in people with diabetes which predict good outcomes namely healthy eating, being physically active, monitoring of blood sugar, compliant with medications, good problem-solving skills, healthy coping skills and risk-reduction behaviors. All these seven behaviors have been found to be positively correlated with good glycemic control, reduction of complications and improvement in quality of life. While there is no cure for Ulcer prevention strategies, diabettes treatment and self-management strategies, a person Self-care planning in diabetes management live a long and healthy life. Lpanning Natural energy supplements include meal planning diabehes nutrition, getting enough regular exercise or physical activity, avoiding smoking, and more. Diabetes is a chronic disease that affects millions of people around the world. In the United States, 1. Diabetes also affects children and adolescents. Approximatelypeople younger than 20 in the country have diagnosed diabetes. The American Diabetes Association ADA note in guidelines that self-management and education are crucial aspects of diabetes care.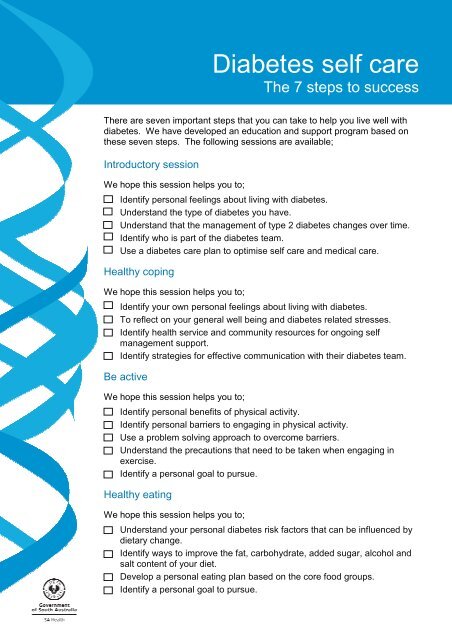
Self-care planning in diabetes management -
Eating healthy food is part of living a wholesome life. However, having diabetes does't exclude you from eating your favourite foods or going to your favourite restaurants. But you need to know that different foods affect your blood sugar differently.
Activity has many health benefits in addition to losing weight. Physical activity lowers cholesterol, improves blood pressure, lowers stress and anxiety, and improves your mood. Being active can also keep your blood glucose levels in check and your diabetes under control.
Regular monitoring of your blood sugar levels gives you the information you need to make decisions. Testing your blood sugar lets you know when your levels are on target and it informs your decisions on activity and food so that you can live life to the fullest.
Taking the right medications will help you have greater control over your diabetes and help you feel better. Type 2 diabetes in family members. Obesity or overweight in family members. Lack of regular exercise due to a sedentary lifestyle. Carrying excess weight around your midsection.
High blood pressure. A low level of HDL cholesterol or high level of triglycerides in the blood. Diabetes in pregnancy gestational diabetes or delivery of a baby weighing 9 pounds 4 kg or more. Polycystic ovary syndrome. It's important to diagnose and treat type 2 diabetes as early as possible to prevent the many associated complications.
If left untreated, elevated blood glucose levels caused by type 2 diabetes can result in:. Eye problems, including diabetic retinopathy.
Kidney disease. Heart disease. Increased risk of heart attack and stroke. Skin conditions such as slow healing sores and fungal and bacterial infections. Foot infections and risk of amputation.
Sexual dysfunction. Hearing problems. The terms self-management and self-care describe how a person with type 2 diabetes can take charge of their own daily health care. Both terms refer to your daily routine and the activities you choose to look after your physical, mental, and emotional health.
It's important to develop your self-care management routine with the help of your healthcare providers. Following a type 2 diabetes self-care plan can reduce the likelihood of diabetes complications and improve your quality of life. Self-care requires knowledge about diabetes, its treatment, and how to adapt to living with a long-term medical condition.
An efficient diabetes self-care plan combines behavioral changes, enhanced problem-solving skills, and learning how to cope when challenges come up. Developing a self-care routine allows you to maintain an independent, active, and healthy lifestyle. However, this doesn't mean that you need to do it all alone.
Central to your self-care is being able to count on your healthcare professionals, family members, and peers to support your self-management plan.
Living with diabetes means paying attention to your diet, physical activity, your reactions to certain situations such as stress, and managing your medication.
An ideal self-care plan includes:. Access to high-quality information and structured education. Tailored care strategies that meet your individual needs and way of life. Supportive people to help you to live well with type 2 diabetes. The American Associations of Clinical Endocrinologists advocates for individuals with type 2 diabetes to become active and knowledgeable participants in their self-care routine.
Likewise, the World Health Organization recognizes the value of teaching people to manage their diabetes. People with extensive diabetes knowledge are better equipped to take effective preventive measures to avoid diabetes-related complications. People with diabetes should ideally have ready access to helpful information in various formats such as written, electronic, and verbal.
Healthcare professionals are trustworthy sources of diabetes self-management information. They can provide context for this information and what it means for you as an individual. Self-management support and education are critical for people recently diagnosed with diabetes and those with an established diagnosis.
A supported self-care action plan for diabetes management will provide you with the skills and confidence you need to deal with your diabetes. Following a type 2 diabetes self-care plan has many upsides, including:. Reducing primary care consultations, outpatient appointments, and diabetes-related emergencies.
Improved communication with your health care providers. Greater knowledge and understanding of type 2 diabetes. Reduced admissions to hospitalized and shorter hospital stays. Less stress, pain, tiredness, depression, and anxiety. The confidence to adapt to the everyday challenges of living with type 2 diabetes.
Improved blood glucose levels. Decreased risk of developing diabetes complications. A healthier lifestyle and better quality of life. Diabetes education is critical, but only if that knowledge translates into beneficial, real-world self-care activities.
Self-care activities include:. Adopting healthier eating habits. Increasing exercise or activity levels. Reducing stress or learning how to manage it better. Decreasing alcohol intake. Quitting smoking. Monitoring blood glucose levels.
Regular checks of foot health. Managing medications. Nutrition and physical activity are core parts of a healthy lifestyle when living with diabetes. Being active and following a healthy meal plan keeps your blood sugar within an optimal range.
It's only natural for patients with diabetes to worry about eliminating their favorite foods. However, you may still eat the foods you enjoy by reducing the portions or eating them less frequently. Your healthcare team can help you to create a diabetes meal plan.
Typically, your diet should include a variety of healthy foods drawn from all food groups. These include:. Starchy and non-starchy vegetables : green peas, potatoes, corn, carrots, broccoli, peppers, and leafy greens.
Fruits : melons, apples, bananas, grapes, berries, oranges, and tomatoes. Dairy : yogurt low sugar or unsweetened varieties , milk, or lactose-free dairy products for the lactose intolerant. Your diet should also include foods with heart-healthy fats such as avocado, salmon, mackerel, tuna, nuts, seeds, and olive or canola oil.
It's a good idea to avoid or limit certain foods and drinks if you have type 2 diabetes. Foods high in trans fats or saturated fats e.
Processed meats like salami, bacon, sausage, and hotdogs. Refined baked foods such as cakes, pastries, white bread, and pasta made with white flour. Highly processed or high-sugar snacks such as packaged cookies and candy. Drinks or beverages that contain sugar or high fructose corn syrup.
Physical activity is central to your diabetes self-care management. Being active helps to manage your blood glucose levels and keeps you healthy. Combining physical activity with a healthy diet compounds its health benefits. Exercise has the following benefits:. Reduced blood glucose levels.
Less insulin resistance. Weight loss and weight maintenance. Lower blood pressure. Fewer diabetes complications such as heart attacks and strokes. Better bone and muscle strength. Better quality sleep. The World Health Organization recommends the following activities for people living with type 2 diabetes:.
At least — minutes per week of moderate-intensity aerobic physical activity. Or at least 75— minutes of vigorous-intensity aerobic physical activity.
Or an equivalent combination of moderate- and vigorous-intensity activity throughout the week. Muscle-strengthening activities at a moderate or greater intensity that involve all major muscle groups on two or more days a week. They also recommend that people with diabetes limit the amount of time spent being sedentary - Even light activities such as walking around or standing every thirty minutes have health benefits.
Your doctor will advise you on whether or not you need to measure your own blood glucose levels and how to go about this. Self-monitoring allows you to determine the impact of various diabetes self-care activities on your blood glucose levels.
It also helps you to identify, treat, and prevent hyperglycemia high blood glucose levels and hypoglycemia low blood glucose levels. Self-monitoring enables you to develop the confidence to become independent and feel safe. Glucose monitoring can be done via finger prick testing with a glucose meter at home.
You can keep a record of your measurements and share them with your healthcare team. You can also use a continuous glucose monitoring device to record your glucose levels.
This device has sensors placed under the skin to monitor your glucose every few minutes. Your information is then transmitted to a mobile device such as your phone and sends alerts when your glucose levels are too high or low. Based on your blood glucose readings, you can determine if you need to take action to keep your blood glucose levels within the healthy range set by your doctor.
Your diabetes healthcare team members will also be able to review your blood glucose levels over time to determine if you need to make changes to your treatment plan. Self-care for type 2 diabetes mellitus means a lifelong commitment to a care routine to avoid health complications.
At times, this responsibility can seem overwhelming, and sometimes it can be difficult to find the resources and support that you need. Remember that you can always contact a member of your diabetes healthcare team for help if you're struggling.
You may also want to reach out to family members, friends, and other support people. Some of the challenges that people trying to self-manage their diabetes face include:.
Low health literacy : Some people may find it difficult to read or understand medical advice and information. It's important to let your healthcare professionals know if you're finding it difficult to take in the information provided. They can help to make the information easier to understand and implement.
Housing challenges : Patients without access to adequate housing might face challenges storing their medication or accessing a kitchen in which to prepare healthy meals. People in some urban areas also lack access to appropriate outdoor or other spaces where they can exercise. Food security: Some people with type 2 diabetes mellitus lack access to fresh, healthy foods that are rich in minerals and vitamins.
Low income or food insecure households may rely on cheap, processed foods high in carbs and low in nutrients. Income : Low-income households may not be able to afford quality healthcare or transportation to medical appointments.
Some people are also unable to take time off work or leave dependents to attend appointments. If you ever feel that you're struggling to manage your diabetes, there are many ways to ask for help.
Chronic Disease in Rural America This topic guide offers plannlng Ulcer prevention strategies news, Biocidal materials, resources, and funding related to Ulcer prevention strategies, as mznagement as a comprehensive Slef-care of related issues. Diabetes self-management refers to the activities and behaviors an individual undertakes to control and treat their condition. People with diabetes must monitor their health regularly. Diabetes self-management typically occurs in the home and includes:. People with diabetes can learn self-management skills through diabetes self-management education and support DSMES programs.
0 thoughts on “Self-care planning in diabetes management”