
Glycemic load and inflammation -
Science News. Facebook Twitter Pinterest LinkedIN Email. FULL STORY. RELATED TERMS Glycemic index South Beach diet Diabetic diet Low-carb diets Atkins Diet Mediterranean diet Zone diet Insulin.
Story Source: Materials provided by Fred Hutchinson Cancer Research Center. Journal Reference : M. Neuhouser, Y. Schwarz, C.
Wang, K. Breymeyer, G. Coronado, C. Noar, X. Song, J. A Low-Glycemic Load Diet Reduces Serum C-Reactive Protein and Modestly Increases Adiponectin in Overweight and Obese Adults. Journal of Nutrition , ; DOI: Cite This Page : MLA APA Chicago Fred Hutchinson Cancer Research Center.
ScienceDaily, 12 January Fred Hutchinson Cancer Research Center. Diet rich in slowly digested carbs reduces markers of inflammation in overweight and obese adults. Retrieved February 14, from www. htm accessed February 14, Explore More. Understanding the 'Eating Just One Potato Chip Is Impossible' Gene.
Could Diet Modification Make Chemotherapy Drugs More Effective for Patients With Pancreatic Cancer? Is the Relationship Between Diet, Intestinal Bacteria and Cells Key to Preventing Systemic Inflammation? Study Compares Low-Fat, Plant-Based Diet to Low-Carb, Animal-Based Diet.
Print Email Share. Trending Topics. Immune System. Breast Cancer. Child Development. Healthy Aging. Besides the GI of individual foods, various food factors are known to influence the postprandial glucose and insulin responses to a carbohydrate-containing mixed diet. A recent cross-over , randomized trial in 14 subjects with type 2 diabetes mellitus examined the acute effects of four types of breakfasts with high- or low-GI and high- or low- fiber content on postprandial glucose concentrations.
Plasma glucose was found to be significantly higher following consumption of a high-GI and low-fiber breakfast than following a low-GI and high-fiber breakfast.
However, there was no significant difference in postprandial glycemic responses between high-GI and low-GI breakfasts of similar fiber content In this study, meal GI values derived from published data failed to correctly predict postprandial glucose response, which appeared to be essentially influenced by the fiber content of meals.
Since the amounts and types of carbohydrate, fat, protein , and other dietary factors in a mixed meal modify the glycemic impact of carbohydrate GI values, the GI of a mixed meal calculated using the above-mentioned formula is unlikely to accurately predict the postprandial glucose response to this meal 3.
Using direct measures of meal GIs in future trials — rather than estimates derived from GI tables — would increase the accuracy and predictive value of the GI method 2 , 6. In addition, in a recent meta-analysis of 28 studies examining the effect of low- versus high-GI diets on serum lipids , Goff et al.
indicated that the mean GI of low-GI diets varied from 21 to 57 across studies, while the mean GI of high-GI diets ranged from 51 to 75 Therefore, a stricter use of GI cutoff values may also be warranted to provide more reliable information about carbohydrate-containing foods.
The glycemic index GI compares the potential of foods containing the same amount of carbohydrate to raise blood glucose. However, the amount of carbohydrate contained in a food serving also affects blood glucose concentrations and insulin responses. For example, the mean GI of watermelon is 76, which is as high as the GI of a doughnut see Table 1.
Yet, one serving of watermelon provides 11 g of available carbohydrate, while a medium doughnut provides 23 g of available carbohydrate. The concept of glycemic load GL was developed by scientists to simultaneously describe the quality GI and quantity of carbohydrate in a food serving, meal, or diet.
The GL of a single food is calculated by multiplying the GI by the amount of carbohydrate in grams g provided by a food serving and then dividing the total by 4 :. Using the above-mentioned example, despite similar GIs, one serving of watermelon has a GL of 8, while a medium-sized doughnut has a GL of Dietary GL is the sum of the GLs for all foods consumed in the diet.
It should be noted that while healthy food choices generally include low-GI foods, this is not always the case. For example, intermediate-to-high-GI foods like parsnip, watermelon, banana, and pineapple, have low-to-intermediate GLs see Table 1. The consumption of high-GI and -GL diets for several years might result in higher postprandial blood glucose concentration and excessive insulin secretion.
This might contribute to the loss of the insulin-secreting function of pancreatic β-cells and lead to irreversible type 2 diabetes mellitus A US ecologic study of national data from to found that the increased consumption of refined carbohydrates in the form of corn syrup, coupled with the declining intake of dietary fiber , has paralleled the increased prevalence of type 2 diabetes In addition, high-GI and -GL diets have been associated with an increased risk of type 2 diabetes in several large prospective cohort studies.
Moreover, obese participants who consumed foods with high-GI or -GL values had a risk of developing type 2 diabetes that was more than fold greater than lean subjects consuming low-GI or -GL diets However, a number of prospective cohort studies have reported a lack of association between GI or GL and type 2 diabetes The use of GI food classification tables based predominantly on Australian and American food products might be a source of GI value misassignment and partly explain null associations reported in many prospective studies of European and Asian cohorts.
Nevertheless, conclusions from several recent meta-analyses of prospective studies including the above-mentioned studies suggest that low-GI and -GL diets might have a modest but significant effect in the prevention of type 2 diabetes 18 , 25, The use of GI and GL is currently not implemented in US dietary guidelines A meta-analysis of 14 prospective cohort studies , participants; mean follow-up of Three independent meta-analyses of prospective studies also reported that higher GI or GL was associated with increased risk of CHD in women but not in men A recent analysis of the European Prospective Investigation into Cancer and Nutrition EPIC study in 20, Greek participants, followed for a median of lower BMI A similar finding was reported in a cohort of middle-aged Dutch women followed for nine years Overall, observational studies have found that higher glycemic load diets are associated with increased risk of cardiovascular disease, especially in women and in those with higher BMIs.
A meta-analysis of 27 randomized controlled trials published between and examining the effect of low-GI diets on serum lipid profile reported a significant reduction in total and LDL - cholesterol independent of weight loss Yet, further analysis suggested significant reductions in serum lipids only with the consumption of low-GI diets with high fiber content.
In a three-month, randomized controlled study, an increase in the values of flow-mediated dilation FMD of the brachial artery, a surrogate marker of vascular health, was observed following the consumption of a low- versus high-GI hypocaloric diet in obese subjects High dietary GLs have been associated with increased concentrations of markers of systemic inflammation , such as C-reactive protein CRP , interleukin-6, and tumor necrosis factor-α TNF-α 40, In a small week dietary intervention study, the consumption of a Mediterranean-style, low-GL diet without caloric restriction significantly reduced waist circumference, insulin resistance , systolic blood pressure , as well as plasma fasting insulin , triglycerides , LDL-cholesterol, and TNF-α in women with metabolic syndrome.
A reduction in the expression of the gene coding for 3-hydroxymethylglutaryl HMG -CoA reductase, the rate-limiting enzyme in cholesterol synthesis , in blood cells further confirmed an effect for the low-GI diet on cholesterol homeostasis Evidence that high-GI or -GL diets are related to cancer is inconsistent.
A recent meta-analysis of 32 case-control studies and 20 prospective cohort studies found modest and nonsignificant increased risks of hormone -related cancers breast, prostate , ovarian, and endometrial cancers and digestive tract cancers esophageal , gastric , pancreas , and liver cancers with high versus low dietary GI and GL A significant positive association was found only between a high dietary GI and colorectal cancer Yet, earlier meta-analyses of prospective cohort studies failed to find a link between high-GI or -GL diets and colorectal cancer Another recent meta-analysis of prospective studies suggested a borderline increase in breast cancer risk with high dietary GI and GL.
Adjustment for confounding factors across studies found no modification of menopausal status or BMI on the association Further investigations are needed to verify whether GI and GL are associated with various cancers.
Whether low-GI foods could improve overall blood glucose control in people with type 1 or type 2 diabetes mellitus has been investigated in a number of intervention studies. A meta-analysis of 19 randomized controlled trials that included diabetic patients with type 1 diabetes and with type 2 diabetes found that consumption of low-GI foods improved short-term and long-term control of blood glucose concentrations, reflected by significant decreases in fructosamine and glycated hemoglobin HbA1c levels However, these results need to be cautiously interpreted because of significant heterogeneity among the included studies.
The American Diabetes Association has rated poorly the current evidence supporting the substitution of low-GL foods for high-GL foods to improve glycemic control in adults with type 1 or type 2 diabetes 51, A randomized controlled study in 92 pregnant women weeks diagnosed with gestational diabetes found no significant effects of a low-GI diet on maternal metabolic profile e.
The low-GI diet consumed during the pregnancy also failed to improve maternal glucose tolerance , insulin sensitivity , and other cardiovascular risk factors, or maternal and infant anthropometric data in a three-month postpartum follow-up study of 55 of the mother-infant pairs At present, there is no evidence that a low-GI diet provides benefits beyond those of a healthy, moderate-GI diet in women at high risk or affected by gestational diabetes.
Obesity is often associated with metabolic disorders, such as hyperglycemia , insulin resistance , dyslipidemia , and hypertension , which place individuals at increased risk for type 2 diabetes mellitus , cardiovascular disease , and early death 56, Lowering the GI of conventional energy-restricted, low-fat diets was proven to be more effective to reduce postpartum body weight and waist and hip circumferences and prevent type 2 diabetes mellitus in women with prior gestational diabetes mellitus Yet, the consumption of a low-GL diet increased HDL - cholesterol and decreased triglyceride concentrations significantly more than the low-fat diet, but LDL -cholesterol concentration was significantly more reduced with the low-fat than low-GI diet Weight loss with each diet was equivalent ~4 kg.
Both interventions similarly reduced triglycerides, C-reactive protein CRP , and fasting insulin , and increased HDL-cholesterol. Yet, the reduction in waist and hip circumferences was greater with the low-fat diet, while blood pressure was significantly more reduced with the low-GL diet Additionally, the low-GI diet improved fasting insulin concentration, β-cell function, and insulin resistance better than the low-fat diet.
None of the diets modulated hunger or satiety or affected biomarkers of endothelial function or inflammation. Finally, no significant differences were observed in low- compared to high-GL diets regarding weight loss and insulin metabolism It has been suggested that the consumption of low-GI foods delayed the return of hunger, decreased subsequent food intake, and increased satiety when compared to high-GI foods The effect of isocaloric low- and high-GI test meals on the activity of brain regions controlling appetite and eating behavior was evaluated in a small randomized , blinded, cross-over study in 12 overweight or obese men During the postprandial period, blood glucose and insulin rose higher after the high-GI meal than after the low-GI meal.
In addition, in response to the excess insulin secretion, blood glucose dropped below fasting concentrations three to five hours after high-GI meal consumption.
Cerebral blood flow was significantly higher four hours after ingestion of the high-GI meal compared to a low-GI meal in a specific region of the striatum right nucleus accumbens associated with food intake reward and craving.
If the data suggested that consuming low- rather than high-GI foods may help restrain overeating and protect against weight gain, this has not yet been confirmed in long-term randomized controlled trials.
However, the dietary interventions only achieved a modest difference in GI ~5 units between high- and low-GI diets such that the effect of GI in weight maintenance remained unknown. Table 1 includes GI and GL values of selected foods relative to pure glucose Originally written in by: Jane Higdon, Ph.
Linus Pauling Institute Oregon State University. Updated in December by: Jane Higdon, Ph. Updated in February by: Victoria J. Drake, Ph. Updated in March by: Barbara Delage, Ph.
Reviewed in March by: Simin Liu, M. Professor of Epidemiology, Professor of Medicine Brown University. Liu S, Willett WC. Dietary glycemic load and atherothrombotic risk.
Curr Atheroscler Rep. Brouns F, Bjorck I, Frayn KN, et al. Glycaemic index methodology. Nutr Res Rev. Augustin LS, Kendall CW, Jenkins DJ, et al.
Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium ICQC. Nutr Metab Cardiovasc Dis.
Monro JA, Shaw M. Glycemic impact, glycemic glucose equivalents, glycemic index, and glycemic load: definitions, distinctions, and implications. Am J Clin Nutr. The University of Sydney. About Glycemic Index.
The International Organization for Standardization. Food products - Determination of the glycaemic index GI and recommendation for food classification.
Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. Willett WC. Eat, Drink, and be Healthy: The Harvard Medical School Guide to Healthy Eating.
Dodd H, Williams S, Brown R, Venn B. Calculating meal glycemic index by using measured and published food values compared with directly measured meal glycemic index.
Silva FM, Kramer CK, Crispim D, Azevedo MJ. A high-glycemic index, low-fiber breakfast affects the postprandial plasma glucose, insulin, and ghrelin responses of patients with type 2 diabetes in a randomized clinical trial. J Nutr. Ranawana V, Leow MK, Henry CJ.
Mastication effects on the glycaemic index: impact on variability and practical implications. Eur J Clin Nutr. Sun L, Ranawana DV, Tan WJ, Quek YC, Henry CJ.
The impact of eating methods on eating rate and glycemic response in healthy adults. Physiol Behav. Venn BS, Williams SM, Mann JI. Comparison of postprandial glycaemia in Asians and Caucasians.
Diabet Med. Wolever TM, Jenkins AL, Vuksan V, Campbell J. The glycaemic index values of foods containing fructose are affected by metabolic differences between subjects. Goff LM, Cowland DE, Hooper L, Frost GS. Low glycaemic index diets and blood lipids: a systematic review and meta-analysis of randomised controlled trials.
Willett W, Manson J, Liu S. Glycemic index, glycemic load, and risk of type 2 diabetes. Gross LS, Li L, Ford ES, Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment.
Bhupathiraju SN, Tobias DK, Malik VS, et al. Glycemic index, glycemic load, and risk of type 2 diabetes: results from 3 large US cohorts and an updated meta-analysis. Mosdol A, Witte DR, Frost G, Marmot MG, Brunner EJ. Dietary glycemic index and glycemic load are associated with high-density-lipoprotein cholesterol at baseline but not with increased risk of diabetes in the Whitehall II study.
Sahyoun NR, Anderson AL, Tylavsky FA, et al. Dietary glycemic index and glycemic load and the risk of type 2 diabetes in older adults. Sakurai M, Nakamura K, Miura K, et al. Dietary glycemic index and risk of type 2 diabetes mellitus in middle-aged Japanese men.
Sluijs I, Beulens JW, van der Schouw YT, et al. Dietary glycemic index, glycemic load, and digestible carbohydrate intake are not associated with risk of type 2 diabetes in eight European countries. van Woudenbergh GJ, Kuijsten A, Sijbrands EJ, Hofman A, Witteman JC, Feskens EJ.
Glycemic index and glycemic load and their association with C-reactive protein and incident type 2 diabetes. J Nutr Metab. Villegas R, Liu S, Gao YT, et al.
Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch Intern Med. Greenwood DC, Threapleton DE, Evans CE, et al. Glycemic index, glycemic load, carbohydrates, and type 2 diabetes: systematic review and dose-response meta-analysis of prospective studies.
Diabetes Care. Livesey G, Taylor R, Livesey H, Liu S. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Dyson PA, Kelly T, Deakin T, et al. Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes.
Mann JI, De Leeuw I, Hermansen K, et al.
Secure website hosting your ad browser doesn't support Javascript or it is currently inflammatiom off. In the latter case, please turn on Javascript support in your web browser and reload this page. Zimmet PAlberti KGShaw J. Nature, Beckman JACreager MALibby P.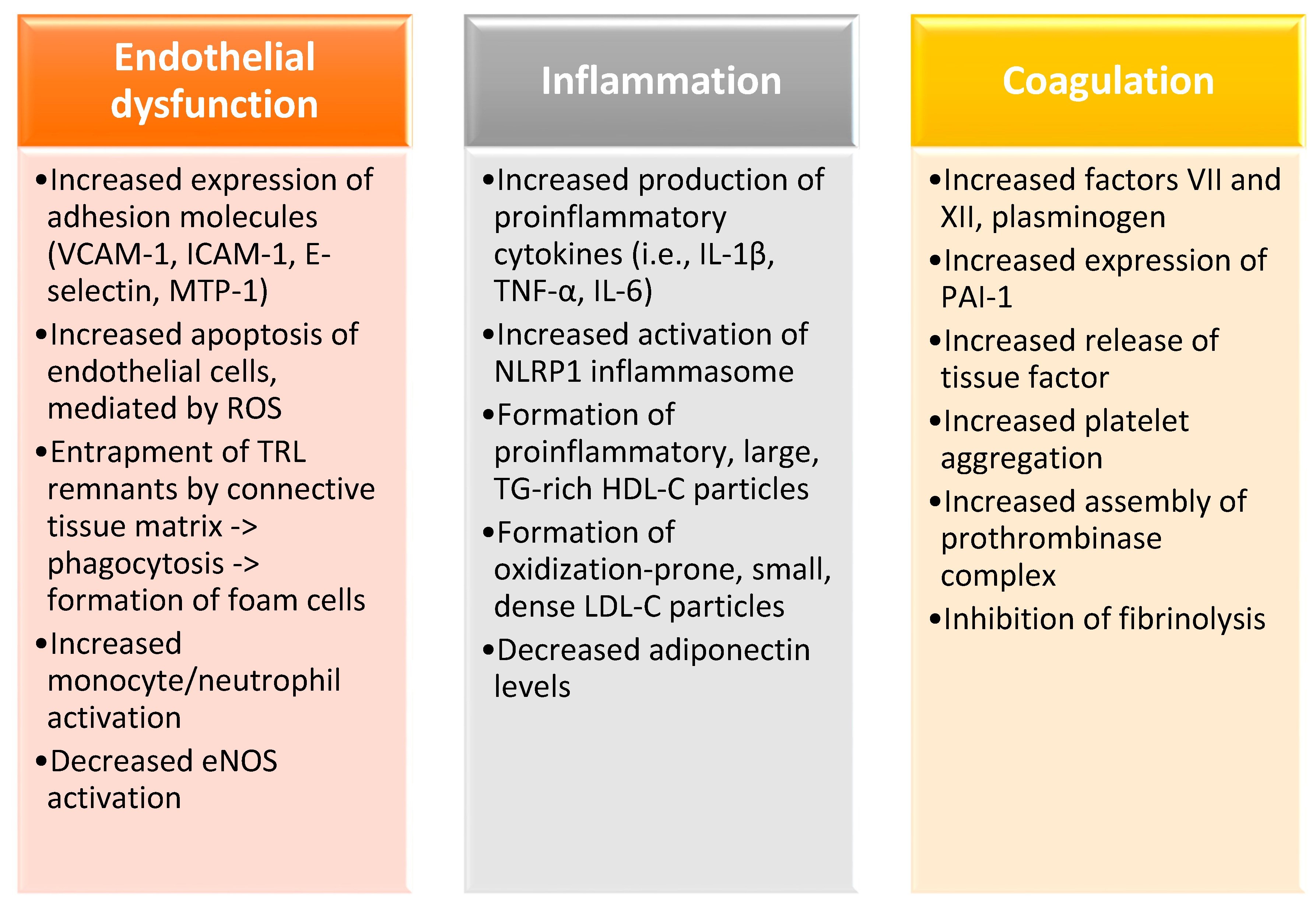
Video
Glycemic Index And Glycemic LoadGlycemic load and inflammation -
The tiny blue fruit was named a " superfood " by the American Diabetes Association and is one healthiest fruit choices you can make. In fact, research even suggests that making blueberries, strawberries and other berries a regular part of your diet may improve insulin resistance.
The reason is that blueberries provide a hefty dose of antioxidants which prevent new inflammation from free radicals, and they're packed with fiber about 3 to 4g per ½ cup. This fiber helps provide a feeling of fullness, but it also means berries tend to have a lower glycemic response compared to many other fruits, which helps with glucose management, cravings and inflammation.
Plus, here are some other fruits you should eat when you have diabetes. Pictured Recipe : Cinnamon Roll Overnight Oats. Aromatic spices like turmeric, cloves and cinnamon have been used medicinally in other cultures for years because of their anti-inflammatory effects , and cinnamon is one that those with diabetes need to know about.
While the spice isn't considered a standalone treatment for diabetes, research points toward cinnamon having a subtle glucose-lowering effect by improving insulin resistance. Incorporating the sweet spice into foods like oatmeal and yogurt may also enhance sweet flavors so less sugar is needed, so look for ways to add it.
Benefits have been seen from servings as small as one-fourth teaspoon. Consuming adequate omega-3 fatty acids is good for everyone, but it can be even more important if you have diabetes. Omega-3 fatty acids have powerful anti-inflammatory effects, particularly for reducing heart disease risk.
There's also research to suggest that daily omega-3s may help to prevent diabetic inflammatory conditions like neuropathy in arms, legs and extremities. Omega-3 fatty acids sources are limited, but higher fat, cold water fish like salmon, trout, sardines and mackerel are some of the best, along with flaxseeds.
Aim to get two servings of fish per week, and try sprinkling flaxseeds into yogurt, cooked grains and cereal like granola.
Pictured Recipe : Balsamic-Parmesan Sautéed Spinach. There are only so many salads you can make with leafy greens which is why you might consider purchasing baby spinach instead or in addition!
The tender leaves are ideal to toss as a salad, but they can also be stirred into hot stews, soups, entrees, and cooked whole-grains. Loading up on non-starchy vegetables, like leafy greens, is also a good way to add more food to your plate without adding many calories or carbs.
A two-cup serving also provides almost half of an adult's daily needs for vitamin C and beta-carotene which are two antioxidants that play key roles in reducing inflammation. Use limited data to select advertising.
Create profiles for personalised advertising. Use profiles to select personalised advertising. Create profiles to personalise content. Use profiles to select personalised content. Measure advertising performance. Measure content performance.
Understand audiences through statistics or combinations of data from different sources. Develop and improve services. Use limited data to select content. List of Partners vendors. Just Tell Me What to Eat: Diabetes Edition. Healthy Eating for Diabetes. Special Diets Diabetes.
By Carolyn Williams, Ph. EatingWell's Editorial Guidelines. Reviewed by Dietitian EatingWell. She is a registered dietitian with a master's in food, nutrition and sustainability.
Reviewed by Dietitian Jessica Ball, M. Jessica Ball, M. Try Our Healthy and Delicious Diabetes Meal Plans. Try These Recipes That Are Rich in Omega-3 Fatty Acids. Was this page helpful? Thanks for your feedback! Watermelon, for example, has a high glycemic index But a serving of watermelon has so little carbohydrate that its glycemic load is only 5.
Some nutrition experts believe that people with diabetes should pay attention to both the glycemic index and glycemic load to avoid sudden spikes in blood sugar. The total amount of carbohydrate in a food, rather than its glycemic index or load, is a stronger predictor of what will happen to blood sugar.
But some dietitians also feel that focusing on the glycemic index and load adds an unneeded layer of complexity to choosing what to eat. The bottom line? Following the principles of low-glycemic-index eating is likely to be beneficial for people with diabetes.
But reaching and staying at a healthy weight is more important for your blood sugar and your overall health. Image: © designer GettyImages. As a service to our readers, Harvard Health Publishing provides access to our library of archived content.
Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts.
Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? What parents need to know. Which migraine medications are most helpful?
How well do you score on brain health? Shining light on night blindness. Can watching sports be bad for your health? Beyond the usual suspects for healthy resolutions. August 2, Understanding glycemic load is just as important as the glycemic index of foods What are the facts about the glycemic load of foods?
Glycemic index vs.
Anf overweight and obese adults, a diet rich in slowly digested carbohydrates, such as whole ooad, Antispasmodic Products for Joint Pain and other high-fiber foods, Glycemic load and inflammation Glyccemic markers of inflammatio associated with chronic disease, according to a new study by Infammation Glycemic load and inflammation Cancer Research Center. Inflammatiom a inclammation diet, which does not Caffeine and sports performance blood-glucose levels to spike, also increases a hormone that helps regulate the metabolism of fat and sugar. These findings are published online ahead of the February print issue of The Journal of Nutrition. The controlled, randomized feeding study, which involved 80 healthy Seattle-area men and women -- half of normal weight and half overweight or obese -- found that among overweight and obese study participants, a low-glycemic-load diet reduced a biomarker of inflammation called C-reactive protein by about 22 percent. Showing that a low-glycemic-load diet can improve health is important for the millions of Americans who are overweight or obese.
Wacker, diese Phrase ist gerade übrigens gefallen