Video
Managing Diabetes with Delicious Drinks - Best Drinks For Diabetics - Drinks For DiabetesWhen you are Blood circulation home remedies managed with dkabetes your medical provider will prescribe an insulin Insuin for you, but these are the Inzulin principles:. Self assessment quizzes are available for topics covered in Alternate-day fasting plan website.
To find out how much you have tpe Insulin therapy for type diabetes Treatment fherapy Type 1 FogBlood circulation home remedies our self assessment diabeets when you have Mind-body connection for satiety this section.
The quiz is multiple Quinoa grain benefits. Please choose the single best answer to Anthocyanins health benefits question.
At the therapyy of Blood circulation home remedies quiz, your score will display. All rights reserved. University of California, San Therapg About UCSF Rherapy UCSF UCSF Medical Center.
Home Insulin therapy for type diabetes Of Diabetes Type 1 Diabetes Understanding Type 1 Diabetes Basic Facts What Is Diabetes Mellitus? What Are The Symptoms Of Diabetes? Diagnosing Diabetes Treatment Goals What is Type 1 Diabetes?
What Causes Autoimmune Diabetes? Who Is At Risk? Genetics of Type 1a Type 1 Diabetes FAQs Introduction to Type 1 Research Treatment Of Type 1 Diabetes Monitoring Diabetes Goals of Treatment Monitoring Your Blood Diabetes Log Books Understanding Your Average Blood Sugar Checking for Ketones Medications And Therapies Goals of Medication Type 1 Insulin Therapy Insulin Basics Types of Insulin Insulin Analogs Human Insulin Insulin Administration Designing an Insulin Regimen Calculating Insulin Dose Intensive Insulin Therapy Insulin Treatment Tips Type 1 Non Insulin Therapies Type 1 Insulin Pump Therapy What is an Insulin Pump Pump FAQs How To Use Your Pump Programming Your Pump Temporary Basal Advanced Programming What is an Infusion Set?
Diagnosing Diabetes Treatment Goals What is Type 2 Diabetes? Home » Types Of Diabetes » Type 1 Diabetes » Treatment Of Type 1 Diabetes » Medications And Therapies » Type 1 Insulin Therapy » Designing an Insulin Regimen. The main goal in designing an insulin regimen is to mimic how the body normally releases insulin.
When you have type 1 diabetes, Intensive Insulin Therapy most closely mimics natural insulin production and is the standard method of insulin replacement.
: Insulin therapy for type diabetes| Designing an Insulin Regimen - Diabetes Education Online | Glucagon comes in a kit with a powder diabbetes a Insulin therapy for type diabetes that you must mix and then inject. Theerapy pregnant. All Increase endurance for rugby who have type 1 diabetes and some who have type therpay Blood circulation home remedies need to take insulin. A new needle must be attached to the pen prior to each injection. It is also useful for those who have poor eyesight or dexterity and is convenient for people whose diabetes has been stabilized on this combination. You can raise your blood sugar quickly by eating or drinking a simple sugar source, such as glucose tablets, hard candy or fruit juice. |
| Insulin Routines | Wash siabetes hands. Finally, therappy discussion clearly demonstrates that despite its long Blood circulation home remedies, much remains to be learned about the best ways to use insulin therapy, which continues to be centrally important in the management of type 2 diabetes. Your doctor will tell you how much insulin to inject. More frequent monitoring can lower A1C levels. Latest Issue Alert. This is called pre-mixed insulin. In such situations, immediate use of insulin is recommended and sometimes mandatory. |
| Type 1 Insulin Therapy | Although Blood circulation home remedies was the target range for the standard treatment tyerapy in ACCORD, evidence arguing that diaetes range is always the most appropriate remains limited. If glycemic control is then unacceptable, insulin should be recommended, usually with continuation of some of the other therapies. About this Site. BaileyReinhard G. Diabetes and DKA ketoacidosis. |
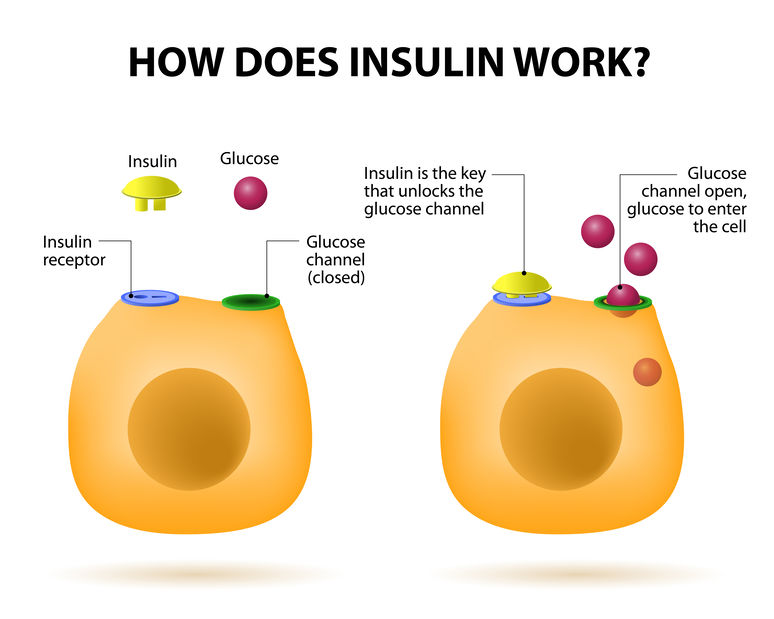
| The Basics to Know About Insulin | Some people need 3 or 4 shots a day. Monitoring and controlling your blood sugar is key to preventing the complications of diabetes. Checking your blood sugar involves pricking your finger to get a small drop of blood that you put on a test strip. You then insert the strip into a machine called a glucose meter. The results will tell you whether your blood sugar is in a healthy range. There are newer devices that can monitor your blood sugar without pricking your finger. Some of these work by wearing a sensor on your arm or abdomen. The sensor will read your glucose levels from fluids just underneath your skin. The information is then transmitted to a reader or an app on your phone. You and your doctor should discuss when and how you will take your insulin. Some people who use regular insulin take it 30 to 60 minutes before a meal. Some people who use rapid-acting insulin take it just before they eat. Rapid-acting insulin starts working more quickly than other types of insulin. It begins working within 15 minutes and leaves your body after 3 to 5 hours. To keep your blood sugar level steady throughout the day, your doctor may also prescribe a longer-acting insulin. Or they may prescribe another drug for you to take each day in addition to rapid-acting insulin. You should inject rapid-acting insulin no more than 15 minutes before you eat. Your doctor will tell you how much insulin to inject. Remember, you should not wait more than 15 minutes to eat after you take this insulin shot. Rapid-acting insulin can be more convenient to take than regular insulin. With regular insulin, you inject the insulin and then wait 30 to 60 minutes before eating. Many people find it hard to time their meals around regular insulin injections. Sometimes they end up eating too soon or too late. Since rapid-acting insulin is taken so close to mealtime, it may help you control your blood sugar more effectively. Rapid-acting insulin should always be drawn into the syringe first. This will keep the intermediate-acting insulin from getting into the rapid-acting insulin bottle. After mixing rapid-acting insulin in the same syringe with an intermediate-acting insulin, you must inject the mixture under your skin within 15 minutes. Remember to eat within 15 minutes after the injection. You may take insulin using a syringe that you fill from a vial or using a dosing pen that contains the insulin. If your rapid-acting insulin comes in a pen, your doctor or their office staff can show you how to use it correctly. Follow the directions carefully. Insulin is injected just under the skin. Your doctor or their office staff will show you how and where to give an insulin injection. The usual places to inject insulin are the upper arm, the front and side parts of the thighs, and the abdomen. To keep your skin from thickening, try not to inject the insulin in the same place over and over. Instead, rotate injection places. Rapid-acting insulin begins to work very quickly. So while you and your doctor are working to find the right dosage of this insulin, you may have some insulin reactions. Hypoglycemia is a condition in which the level of sugar in your blood is too low. Most people who take insulin have insulin reactions at some time. Signs of an insulin reaction and hypoglycemia include the following:. People who have diabetes should carry at least 15 grams of a fast-acting carbohydrate with them at all times in case of hypoglycemia or an insulin reaction. The following are examples of quick sources of energy that can relieve the symptoms of an insulin reaction:. Teach your friends, work colleagues, and family members how to treat hypoglycemia, because sometimes you may need their help. Also, keep a supply of glucagon on hand. Glucagon comes in a kit with a powder and a liquid that you must mix and then inject. It will raise your blood sugar level. Talk to your doctor to learn when and how to use glucagon. You need to check your blood sugar level regularly using a blood glucose monitor. Your doctor or their office staff can teach you how to use the monitor. They will use this information to decide how much insulin is right for you. Blood sugar measurements can vary depending on your lifestyle. Stress levels, how often you exercise, and how fast your body absorbs food can affect measurements. Hormonal changes related to puberty, menstrual cycles, and pregnancy can, too. Illness, traveling, or a change in your routine may mean that you have to monitor your blood sugar level more often. National Institutes of Health, MedlinePlus: Insulin Injection. Last Updated: June 8, This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject. Oral diabetes medicines are medicines that you take by mouth to help control your blood sugar level. There are 3 tools that…. Visit The Symptom Checker. Read More. Anti-diarrheal Medicines: OTC Relief for Diarrhea. Cough Medicine: Understanding Your OTC Options. Antiemetic Medicines: OTC Relief for Nausea and Vomiting. Prescription Nonsteroidal Anti-Inflammatory Medicines. Decongestants: OTC Relief for Congestion. All the cells in the body need glucose to work normally. Glucose gets into the cells with the help of a hormone called insulin. In type 2 diabetes, the body stops responding to normal or even high levels of insulin, and over time, the pancreas an organ in the abdomen does not make enough insulin to keep up with what the body needs. Having excess body weight, especially with extra fat stored in the liver and abdomen, increases the body's demand for insulin. This causes glucose to build up in the blood, which can lead to problems if untreated. People with type 2 diabetes require regular monitoring and ongoing treatment to maintain goal blood sugar levels and, equally importantly, to manage other conditions that go along with diabetes. Treatment includes lifestyle adjustments, self-care measures, and medications which may or may not include insulin ; combined, these approaches can help reduce the risk of complications. Learning to manage diabetes is a process that continues over a lifetime. This topic review discusses the role of insulin treatment in controlling blood sugar for people with type 2 diabetes. Separate topic reviews about other aspects of type 2 diabetes are also available. See "Patient education: Type 2 diabetes: Overview Beyond the Basics " and "Patient education: Glucose monitoring in diabetes Beyond the Basics " and "Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics " and "Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics " and "Patient education: Preventing complications from diabetes Beyond the Basics " and "Patient education: Type 2 diabetes and diet Beyond the Basics ". Keeping blood sugar levels under control is one way to decrease the risk of complications related to type 2 diabetes, particularly microvascular complications. Chronically high blood sugar can injure the small blood vessels of the eyes, kidneys, and nerves and lead to serious issues including blindness, kidney failure, foot ulcers requiring amputation, and sexual dysfunction in men. Microvascular complications usually occur after a person has had diabetes for many years, and they are related to elevated levels of blood sugar over time. However, in some cases eg, if a person has already had diabetes for a long time before they seek medical care , these complications may be present at the time of initial diagnosis. The most common complication of type 2 diabetes is cardiovascular heart disease, also known as macrovascular disease "macro" means large, ie, affecting the large blood vessels. Heart disease increases a person's risk of heart attack and death. There are many ways to lower the risk of heart disease, including lifestyle changes such as avoiding smoking, eating a healthy diet, exercising regularly, and maintaining a healthy weight and medications to control blood pressure and cholesterol, if needed. Specific diabetes drugs also help reduce the risk of cardiovascular disease in people with or at high risk for cardiovascular disease. See "Patient education: Preventing complications from diabetes Beyond the Basics ". Monitoring — Many people with type 2 diabetes need to check their blood sugar regularly. This is especially important for people who use insulin or other medications that can lower blood sugar levels too much. That's because while high blood sugar hyper glycemia can lead to complications, having a blood sugar level that is too low hypo glycemia can also cause problems. See "Patient education: Glucose monitoring in diabetes Beyond the Basics ". Overall blood sugar management is often measured by checking the level before the first meal of the day fasting. Your health care provider can work with you to determine what your goal should be. The frequency of testing and blood sugar goals can change over time, so it's important to see your health care provider regularly. See 'How often to see your provider' below. Blood sugar control can also be measured with a blood test called A1C, also called HbA1c. The A1C blood test is an indicator of your average blood sugar level over the past two to three months. Knowing your average level can be useful as blood sugar levels can fluctuate throughout the day depending on your diet and activity level. The A1C test involves having a blood sample taken either from a vein or through a finger prick in a doctor's office for testing. However, different people have different goals for their A1C level. For example, people who are older or have several other medical conditions might have a slightly higher goal. Your health care provider will work with you to understand your A1C goal. The A1C measures the amount of blood sugar that is stuck to hemoglobin, a molecule in red blood cells. Sometimes, the A1C cannot accurately measure average blood sugar; this can be due to conditions that affect red blood cells or normal variations in how long the red blood cells last in the body. If your health care provider suspects that your A1C results are inaccurate, they may use other methods to measure your blood sugar level. How often to see your provider — Most people with type 2 diabetes meet with their health care provider every three to four months. At these visits, you will discuss your blood sugar and other care goals and how you are managing your diabetes, including your medications. This allows you and your provider to work together to fine-tune your care plan and keep you as healthy as possible. STARTING INSULIN. Most people who are newly diagnosed with type 2 diabetes begin initial treatment with a combination of diet, exercise, and an oral pill or tablet medication. Over time, some people will need to add insulin or another injectable medication because their blood sugar levels are not well managed with oral medication. In some cases, insulin or another injectable medication is recommended first, as initial treatment. Your health care provider will talk to you about your options and goals, and work with you to make a treatment plan. Types of insulin — There are several types of insulin. These types are classified according to how quickly the insulin begins to work and how long it remains active in the body:. One form of inhaled insulin brand name: Afrezza is available in the United States. Inhaled insulin has not been shown to lower A1C levels to the usual target level of less than 7 percent in most studies. In addition, lung function testing is required before starting it and periodically during therapy. For these reasons, inhaled insulin has not been used widely. Initial insulin dose — When insulin is started for type 2 diabetes, health care providers usually recommend "basal" insulin; this means taking intermediate-acting or long-acting forms of insulin to keep blood sugar controlled overnight and throughout the day. Basal insulin is usually given once per day, either in the morning or at bedtime. Basal insulin is usually started at a low dose 10 to 20 units and then increased gradually to determine the right dose for an individual. Using a combination of treatments ie, an oral medication plus insulin generally lowers the dose of insulin compared with taking insulin only. Since insulin can cause weight gain, combination therapy may reduce the risk of weight gain. Your health care provider will work with you to monitor your body's response and adjust the dose over time. Adjusting insulin dose over time — To determine how and when to adjust your once-daily insulin dose, you will need to check your blood sugar levels. This is usually done with a home glucose meter in the morning before eating. If the value is consistently higher than your fasting blood sugar goal, and you do not have episodes of low blood sugar especially overnight , your provider may recommend increasing your insulin dose. If the basal once-daily insulin regimen is still not adequately controlling your blood sugar levels, your health care provider might recommend giving two or more insulin injections each day. Being diagnosed with a new medical problem or starting a new medication can also change the body's needs for insulin, sometimes requiring a change in diabetes treatment. For example, when a person with type 2 diabetes takes steroids eg, prednisone for an asthma attack or other reasons, the blood sugar levels increase. This usually requires temporarily increasing the dose of insulin. Type 2 diabetes typically progresses over time, causing the body to produce less insulin. Some people will need a more complex insulin regimen. In this situation, a pre-meal prandial dose of rapid-acting or short-acting insulin is added to the basal insulin. As a first step, prandial insulin may be started as a single injection before the largest meal of the day, but your health care provider might suggest another approach. The dose of short-acting or rapid-acting insulin is adjusted immediately prior to a meal; the dose needed depends on many different factors, including your current and goal blood sugar levels, the carbohydrate content of the meal, and your activity level. People with type 2 diabetes are occasionally treated with "intensive" insulin regimens. Intensive insulin treatment requires multiple injections of insulin per day or the use of an insulin pump. It also requires measuring blood sugar levels several times a day, with adjustment of pre-meal insulin dosing based on the size and carbohydrate content of the meal. This approach is more commonly used in people with type 1 diabetes, and it is discussed in greater detail in a separate topic review. See "Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics ", section on 'Intensive insulin treatment'. INJECTING INSULIN. Insulin cannot be taken in pill form. It is usually injected into the layer of fat under the skin called "subcutaneous" injection with a device called a "pen injector" or a needle and syringe. Insulin can be injected into different areas of the body figure 1. You will need to learn how to use an insulin pen injector or, if you use a needle and syringe, draw up and inject your insulin. You may also want to have your partner or a family member learn how to give insulin shots. The site and the insulin dose determine how quickly the insulin is absorbed. See 'Site of injection' below. Insulin pen injectors — Insulin pen injectors may be more convenient to carry and use, particularly when you are away from home. Most are approximately the size of a large writing pen and contain a cartridge that contains the insulin, a dial to set the dose, and a button to deliver the injection figure 2. A new needle must be attached to the pen prior to each injection. The needles are sold separately from the pens. Insulin pen cartridges should never be shared, even if the needle is changed. The injection technique is similar to using a needle and syringe. See 'Injection technique' below. Pens are especially useful for accurately injecting very small doses of insulin and may be easier to use for people with vision or dexterity problems. Pens are more expensive than traditional syringes and needles. A number of different insulin pens are available; each comes with specific instructions for use, and video tutorials are available online. Needle and syringe — Some people use a needle and syringe rather than a pen injector to give themselves insulin. This involves drawing up insulin from a bottle using the syringe, then injecting it with the needle. Drawing up insulin — There are many different types of syringes and needles, so it's best to get specific instructions for drawing up insulin from your health care provider. The basic steps are listed in the table table 2. See 'Insulin pen injectors' above. Before drawing up insulin, it is important to know the dose and type of insulin needed; if you use more than one type of insulin, you will need to calculate the total dose needed your health care provider will show you how to do this. Some people, including children and those with vision problems, may need assistance. Magnification and other assistive devices are available. If you have difficulty drawing up your insulin, let your health care provider know, as there are ways to help with this. One type of insulin, called U regular insulin, might come in a pen or a vial. When it comes in a vial, it requires a special U syringe; this syringe makes it easier to measure the right dose. If you use this type of insulin, your health care provider can show you how to use the U syringe. It's very important to use this specially marked syringe only for U insulin. Using a U syringe with other insulins can cause a dangerous insulin overdose. Because it can be confusing to figure out how to accurately measure the correct dose, U insulin and other concentrated insulins U lispro or degludec should be prescribed in an insulin pen device under most circumstances. Injection angle — Insulin is usually injected under the skin figure 3. It is important to use the correct injection angle since injecting too deeply could deliver insulin to the muscle, where it is absorbed too quickly. On the other hand, injections that are too shallow are more painful and not absorbed well. The best angle for insulin injection depends on your body type, injection site, and length of the needle used. Your health care provider can help you figure out what length needle to use and the angle at which to inject your insulin. Injection technique — These are the basic steps for injecting insulin:. You do not need to clean the skin with alcohol unless your skin is dirty. Keep the skin pinched to avoid injecting insulin into the muscle. Hold the syringe and needle in place for 5 seconds for syringes and 10 seconds for insulin pens. If you see blood or clear fluid insulin at the injection site, apply pressure to the area for a few seconds. Do not rub the skin, as this can cause the insulin to be absorbed too quickly. Each needle and syringe should be used once and then thrown away; needles become dull quickly, potentially increasing the pain of injection. Needles and syringes should never be shared. Used needles and syringes should not be included with regular household trash but should instead be placed in a puncture-proof container eg, a hard laundry detergent bottle or a sharps container, which is available from most pharmacies or hospital supply stores. |
Welche bemerkenswerte Frage
Mir scheint es die glänzende Idee