Hypoglycemic unawareness and glucose monitoring -
Multiple Comparisons Summary eTable 4. Baseline Characteristics by Pump and MDI Users eTable 5. Comorbidities at Enrollment eTable 6. Types of Medications at Enrollment eTable 7. Unscheduled Contacts eTable 8.
Real-time CGM Use eTable 9. Real-time CGM Use by Pump and MDI Users eTable CGM Metrics in Time per Day eTable Glycemic Outcomes at 16 Weeks eTable CGM Metrics During the Daytime AMPM and Nighttime AMAM eTable Glycemic Outcomes Among Participants Using a Pump for Insulin Delivery eTable Glycemic Outcomes Among Participants Using Injections for Insulin Delivery eTable Binary HbA1c Outcomes eTable Device Issues eTable Cognitive Assessment and Patient-Reported Outcomes eFigure 1.
Visit Completion by Treatment Group eFigure 2. CGM Education Materials eReferences. Supplement 3. Data Sharing Statement. Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry.
doi: Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, to Stahn A, Pistrosch F, Ganz X, et al. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: silent hypoglycemias and silent arrhythmias.
Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the International Consensus on Time in Range. Weinstock RS, Xing D, Maahs DM, et al; T1D Exchange Clinic Network. Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange Clinic Registry.
Aleppo G, Ruedy KJ, Riddlesworth TD, et al; REPLACE-BG Study Group. REPLACE-BG: a randomized trial comparing continuous glucose monitoring with and without routine blood glucose monitoring in adults with well-controlled type 1 diabetes.
Tamborlane WV, Beck RW, Bode BW, et al; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group.
Continuous glucose monitoring and intensive treatment of type 1 diabetes. Battelino T, Phillip M, Bratina N, Nimri R, Oskarsson P, Bolinder J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C; DIAMOND Study Group.
Continuous glucose monitoring in older adults with type 1 and type 2 diabetes using multiple daily injections of insulin: results from the DIAMOND trial.
Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial.
Davis SN, Horton ES, Battelino T, Rubin RR, Schulman KA, Tamborlane WV. STAR 3 randomized controlled trial to compare sensor-augmented insulin pump therapy with multiple daily injections in the treatment of type 1 diabetes: research design, methods, and baseline characteristics of enrolled subjects.
Little SA, Leelarathna L, Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2×2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring HypoCOMPaSS.
Patton SR. Adherence to glycemic monitoring in diabetes. Beck RW, Riddlesworth T, Ruedy K, et al; DIAMOND Study Group.
Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. Aleppo G, Laffel LM, Ahmann AJ, et al.
A practical approach to using trend arrows on the Dexcom G5 CGM system for the management of adults with diabetes. Clarke WL, Cox DJ, Gonder-Frederick LA, Julian D, Schlundt D, Polonsky W. Reduced awareness of hypoglycemia in adults with IDDM: a prospective study of hypoglycemic frequency and associated symptoms.
Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Polonsky WH, Fisher L, Hessler D, Edelman SV.
Development of a new measure for assessing insulin delivery device satisfaction in patients with type 1 and type 2 diabetes. Nathan DM, Genuth S, Lachin J, et al; Diabetes Control and Complications Trial Research Group.
The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. Beunckens C, Molenberghs G, Kenward MG.
Direct likelihood analysis versus simple forms of imputation for missing data in randomized clinical trials. Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics.
Weinstock RS, DuBose SN, Bergenstal RM, et al; T1D Exchange Severe Hypoglycemia in Older Adults With Type 1 Diabetes Study Group. Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes.
Fiallo-Scharer R, Cheng J, Beck RW, et al; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Factors predictive of severe hypoglycemia in type 1 diabetes: analysis from the Juvenile Diabetes Research Foundation continuous glucose monitoring randomized control trial dataset.
Chen E, King F, Kohn MA, Spanakis EK, Breton M, Klonoff DC. A review of predictive low glucose suspend and its effectiveness in preventing nocturnal hypoglycemia.
Forlenza GP, Li Z, Buckingham BA, et al. Predictive low-glucose suspend reduces hypoglycemia in adults, adolescents, and children with type 1 diabetes in an at-home randomized crossover study: results of the PROLOG trial.
Juva K, Mäkelä M, Erkinjuntti T, et al. Functional assessment scales in detecting dementia. Holdnack JA, Tulsky DS, Brooks BL, et al. Interpreting patterns of low scores on the NIH Toolbox Cognition Battery.
Hodges JL, Lehmann EL. Estimates of location based on rank tests. Effect of Continuous Glucose Monitoring on Glycemic Control in Adolescents and Young Adults With Type 1 Diabetes. This randomized clinical trial examines the effect of continuous glucose monitoring vs standard blood glucose monitoring on glycemic outcomes among adolescents and adults with type 1 diabetes and suboptimal glycemic control.
Lori M. Laffel, MD, MPH; Lauren G. Kanapka, MSc; Roy W. Beck, MD, PhD; Katherine Bergamo, BSN, RN, MS; Mark A. Clements, MD, PhD; Amy Criego, MD; Daniel J.
DeSalvo, MD; Robin Goland, MD; Korey Hood, PhD; David Liljenquist, MD; Laurel H. Messer, PhD, RN, MPH, CDE; Roshanak Monzavi, MD; Thomas J. Mouse, BS; Priya Prahalad, MD; Jennifer Sherr, MD, PhD; Jill H.
Simmons, MD; R. Paul Wadwa, MD; Ruth S. Weinstock, MD, PhD; Steven M. Willi, MD; Kellee M. Miller, PhD, MPH; CGM Intervention in Teens and Young Adults with T1D CITY Study Group.
Continuous Glucose Monitoring in Adolescent, Young Adult, and Older Patients With Type 1 Diabetes. New Guidance for Type 1 Diabetes Continuous Glucose Monitoring Use During Exercise. This story describes guidelines to help people with type 1 diabetes respond to readings on glucose monitors before, during, and after exercise.
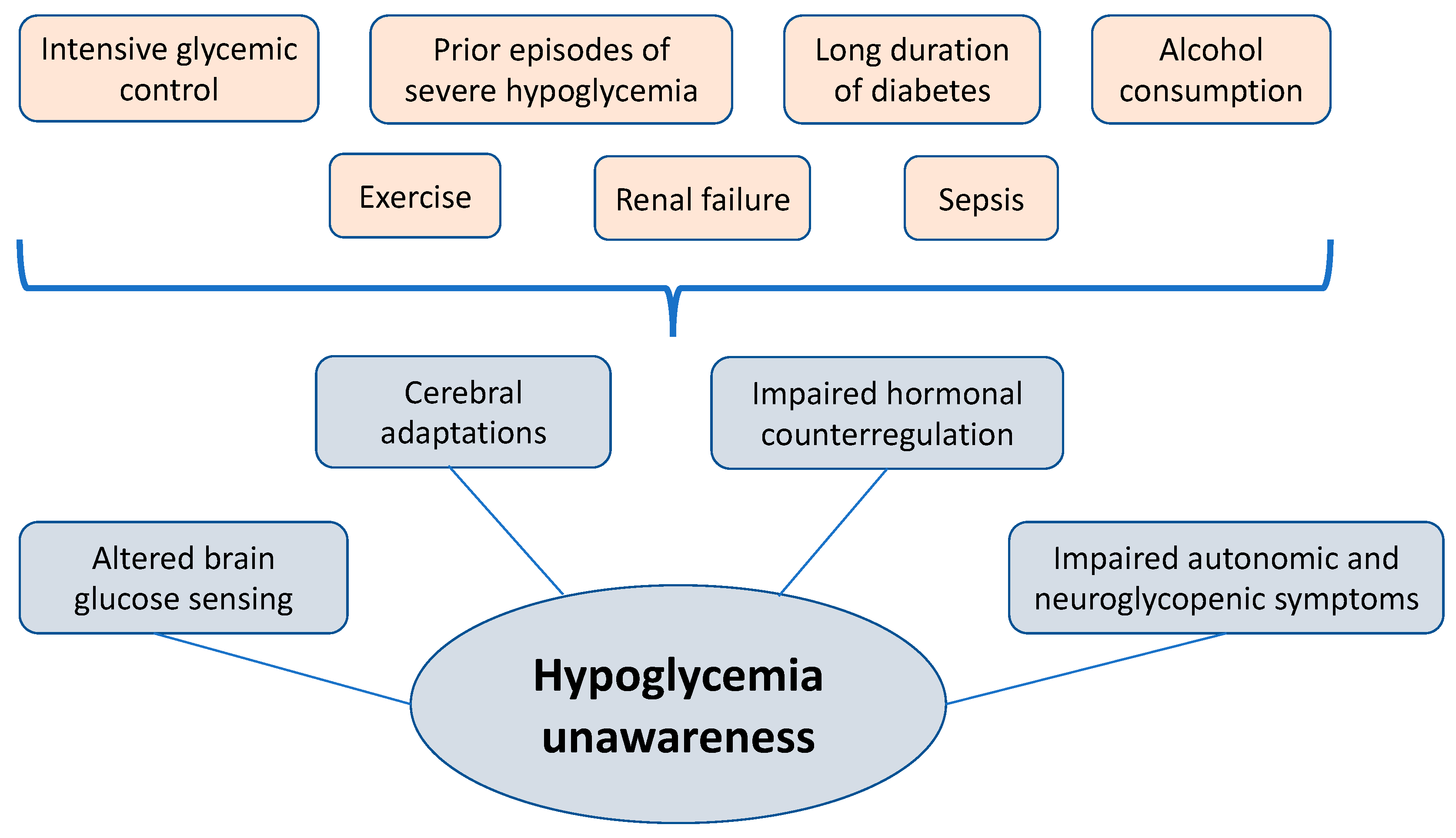
See More About Diabetes Diabetes and Endocrinology. Select Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below. Save Preferences. Privacy Policy Terms of Use. This Issue. Views 42, Citations Q: How can health care professionals help patients manage hypoglycemia unawareness?
A: Continuous glucose monitors are very good tools for patients that are at risk of hypoglycemia unawareness, because the CGM will alert them if their blood glucose level gets too low. Patients also will know what their blood glucose level is before they drive, and have insights into how food and exercise affect their glycemia.
Health care professionals should also make sure that patients understand that they need to be aware of some circumstances that may put them at risk. The same is true for alcohol—if patients drink alcohol, it increases the risk of hypoglycemia, so they should be reminded to eat food if they are going to drink.
Some studies have shown that if patients avoid hypoglycemia for some time, they can begin to feel the symptoms of hypoglycemia again. I have seen this in people with diabetes that participate in my research studies.
By preventing hypoglycemia, you can reset the body to respond differently to symptoms of hypoglycemia. Some health care professionals may prefer to use newer basal insulins in patients at risk of hypoglycemia because these insulins seem to have less risk of hypoglycemia than the older ones, but they can still cause hypoglycemia, and we need to be aware of that.
I think that for many people, it is easier to administer mealtime insulin when they have an insulin pump. It is also important to remember that some patients may be afraid to report episodes of hypoglycemia to their doctors because of legal implications.
For example, some states may require people with diabetes to not have a hypoglycemia episode for 6 to 12 months before they can drive a vehicle. Health care professionals should emphasize to patients that they should know what their blood glucose level is before they drive a car, and that they should have food on hand, so if their glucose level drops, they can manage it.
Q: What research is being conducted on hypoglycemia unawareness? A: Researchers are interested in different aspects of hypoglycemia unawareness such as the cause, complications, and treatments. Some groups are studying why recurrent hypoglycemia leads to impaired awareness.
Is it a problem with brain adaptation to hypoglycemia, or is it only a problem with people who have severe glucagon deficiency? Other groups are doing research on the long-term effects of recurrent hypoglycemia on the function of other organs. I just finished a study where we gave people naloxone during an episode of exercise to determine if they recognize their hypoglycemia the next day, but the study was just completed, so we do not have results yet.
We welcome comments; all comments must follow our comment policy. Blog posts written by individuals from outside the government may be owned by the writer and graphics may be owned by their creator. In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse.
Q: What is hypoglycemia? Q: What is hypoglycemia unawareness, and how common is it? What is your experience managing hypoglycemia unawareness? Tell us in the comments below. Click to load comments Loading comments Blog Tools Subscribe Subscribe to get blog updates. Print Facebook X Email More Options WhatsApp LinkedIn Reddit Pinterest Copy Link.
Patient Communication Research Advancements Complications of Diabetes Hypoglycemia is well-recognized as one of the most severe complications and therapy-limited factors of patients with diabetes reviewed by Amiel SA et al. It has been reported that hypoglycemia could not only cause unpleasant symptoms, impaired cognitive function, diminished productivity, but also result in long-term chronic vascular complications of diabetes and affect the lifespan [ 2 ].
Theoretically, when hypoglycemia occurs, counter-regulatory systems are normally activated and patients with diabetes tend to develop the characteristic neuroglycopenic and adrenergic symptoms of hypoglycemia, which is regarded as a protective mechanism [ 3 , 4 ]. Whereas, in clinical practice, there are quite a few patients experiencing hypoglycemia episodes without any sensed symptoms, which is defined as asymptomatic hypoglycemia AH.
Studies by Gold et al. Additionally, antecedent hypoglycemia attacks could shift glycemic thresholds for autonomic and symptomatic responses to lower plasma glucose concentrations and further aggravate impaired awareness of hypoglycemia, with evidence that avoiding such exposure could restore consciousness and terminate the vicious cycle of recurrent hypoglycemia [ 8 , 9 , 10 ].
The continuous glucose monitoring system CGMS is rapidly improving diabetes management and has been proved to be superior to daily self-monitoring blood glucose SMBG in the detection of hypoglycemia and in improving glycemic control in T2DM individuals [ 12 ]. By using CGMS, Chico et al. Data recorded via h CGMS [ 14 ] revealed that the incidence of NAH in T2DM patients was twofold higher than that of daytime hypoglycemia.
McNally et al. Thereby, concerning the reliability and accuracy, it is considerable for CGMS to be brought into the routine management of T2DM.
Rates and influencing factors of AH have been widely reported in type 1 diabetes T1DM [ 17 , 18 , 19 ] and T2DM [ 20 , 21 ] patients with intensive treatment who are prone to hypoglycemia.
It is generally assumed that the risk of developing hypoglycemia in daily diabetes outpatients is relatively lower because their medical conditions are relatively stable. A small sample size research 31 participants reported that Another study in outpatients with T2DM demonstrated that the AH was frequently seen [ 22 ].
Given the high prevalence, potential and prolonged harms, and insidious onset of AH, estimating the actual rate and promptly identifying episodes of AH have important implications for diabetes care. In view of the insufficient attention to T2DM outpatients without receiving intensive therapeutic interventions, our study enrolled such an entity and aimed to determine the influencing factors of AH in T2DM outpatients via CGMS.
This study included outpatients with T2DM in the First Affiliated Hospital of Xiamen University from January to March The studies involving human participants were reviewed and approved by The First Affiliated Hospital of Xiamen University.
Enrolled patients completed the informed consent and wore the CGMS device at the outpatient clinic. In order to reflect the effectiveness and safety of the current treatment regimen of the subjects, we did not ask them to change their previous diet and exercise habits during the CGM test.
Thus, they went home to lead a normal life for three consecutive days. Clinical data of baseline characteristics, such as Glycated hemoglobin A1c HbA1c , BMI calculated as weight in kilograms divided by the square of height in meters , diabetes duration, age, diabetes medications, complications, and diabetic complications, were collected.
The glucose value is recorded every 5 min, for a total of readings a day. Before the CGM test, we provided unified blood glucose meters Contour Plus Blood Glucose Meter, P to each patient and instructed them to provide at least four self-monitoring blood glucose SMBG tests per day.
Besides, notebooks were provided to each patient to record the frequency and time of suspicious hypoglycemia if they had symptoms such as hunger, palpitations, tremulousness, sweats, and dizziness. After three days of monitoring, patients returned to the outpatient clinic, where their SMBG metrics were imputed into the system and the CGM data was downloaded.
The CGM data recorded in this article included the glucose standard deviation SD , mean blood glucose MBG , the mean amplitude of glycemic excursions MAGE , time in range TIR, 3. According to the definition of the International Hypoglycemia Study Group [ 1 ], hypoglycemia is defined as a blood glucose level less than 3.
A single hypoglycemic episode was defined as BG below 3. Two separate hypoglycemic events were defined when the time interval between two hypoglycemic events was equal to or greater than 30 min. Preliminary statistical analyses included descriptive statistics and assessment of distributions.
The statistical significance of differences between different groups was assessed by t test or Kruskal—Wallis test for continuous variables and by Chi-square test for categorical variables.
The univariate and multivariate logistic regression analyses were used to determine clinical predictors of hypoglycemia. Those found to be significant in univariate models and some characteristics selected a priori were adjusted for in multivariate logistic regression models.
Statistical analyses were performed with SAS version 9. All the statistical tests were two-sided. The characteristics of the total outpatients with T2DM were shown in Table 1.
There were The average systolic blood pressure SBP was The mean BMI was The median duration of diabetes was 6. According to 3-day CGM data and self-reports of the subjects, none experienced symptomatic hypoglycemia.
Overall, AH events were captured in outpatients Hypoglycemia episodes that occurred exclusively at night accounted for The Total TIR was The MAGE, SD, and MBG were 4. In Table 2 , compared to outpatients without AH, outpatients in the AH group showed younger age According to the data of CGM, glucose SD 2.
Nighttime TIR in the AH group was significantly lower than that in the non-AH group [ Patients had AH episodes exhibited lower Total TAR [ In order to determine the influencing factors of AH, we conducted a series of analyses.
After controlling for all factors identified through univariate analyses Additional file 1 : Table S1 , multivariate analysis Table 3 demonstrated that patients with younger age [0. As for Level 1 AH, patients with lower HbA1c exhibited a higher prevalence of AH 6. The MBG of the AH group was substantially lower 7.
Daytime TIR [ Patients with lower Total TAR [6. Multivariate analyses Table 3 controlled for factors associated with high regimen distress in univariate analyses Additional file 1 : Table S1 and found that lower HbA1c levels [0. There was greater percentage of female in the Level 2 AH group The age Significantly statistical difference was observed in the use of Dipeptidylpeptidase-4 inhibitors DPP4i 1.
The MAGE 5. There were significant statistical differences in Total TIR [ After controlling for all factors identified through univariate analyses Additional file 1 : Table S1 , multivariate analyses found that female sex [0.
In addition, patients treated with DPP4i tended to have lower risk of Level 2 AH [0. Table 3. In the current study, Multivariate logistic regression analysis demonstrated that patients with younger age, lower HbA1c, and higher SBP levels were significantly associated with increased risk of AH.
While after further grading of AH, male sex and DPP4i regime were shown to be associated with lower risk of Level 2 AH. Previously, Chico et al. Further, Gehlaut et al. During the five-day study, 53 The prevalence of NAH was In our study, none of the participants reported symptomatic hypoglycemia, and Notably, all patients experienced hypoglycemic episodes claimed they had no symptoms of hypoglycemia.
We speculate that the heterogeneity of symptom response in diabetic individuals could took into consideration and selective bias might play a role. It is also possible that the patients were asymptomatic due to recurrent episodes of hypoglycemia. Although plenty of studies [ 12 , 17 , 22 , 23 , 25 ] had indicated that older age, longer diabetes duration, and microvascular complications were independently correlated with increased prevalence of hypoglycemia, in our present study, multivariate logistic regression analysis found no significance of these variables in predicting AH events except for younger age in the Level 2 AH group.
Various explanations could be proposed. Firstly, most prior studies were conducted during hospitalization, and they focused merely on the insulin-used population with poor glucose control to investigate the incidence of hypoglycemia.
However, the target population of our study was T2DM outpatients whose status was relatively stable with "well-controlled" glucose levels. Differences in samples may contribute to differences of results.
Secondly, we used the CGMS to detect the hypoglycemia episodes, which is expected to discover additional unrecognized hypoglycemia events than traditional SMBG.
Previous studies [ 24 , 28 ] had demonstrated that intensive insulin treatment or sulfonylurea SU could predict the episodes of hypoglycemia in T2DM. Our study also showed a higher rate of insulin therapy However, this association did not exist when accounting for other influencing factors in the multiple logistic regression models.
This may be due to the substantial effect of the adjusted confounders. Additionally, neither univariate nor multivariate analysis demonstrated the association between SU and the risk of AH.
Overall, our study observed that outpatients treated with insulin or SU did not predispose to asymptomatic hypoglycemia, which was consistent with the conclusion of Monnier et al. This interesting finding reminds us to screen all diabetic patients for a history of hypoglycemia, rather than focusing only on those using insulin or insulin secretagogues.
In our study, the univariate logistic analysis indicated that DPP4i regime was associated with lower risks of Level 1 and Level 2 AH, yet the association between DPP4i and Level 1 AH was substantially attenuated after further adjusting for other confounders.
This may stem from the fact that, in our present study, elder age was a protective factor for AH, and the average age of the Level 1 AH group was substantially higher than that of the Level 2 AH group Thus, after controlling for age and other affecting factors, the protective effect of DPP4i in the Level 1 group disappeared.
Overall, DPP4i have been proved to be substantially associated with lower risks of hypoglycemia [ 26 ]. Further studies are needed to confirm the causal relationship between DPP-4i regime and the risk of AH.
The link between the diagnosis of hypertension and a higher risk of hypoglycemia had been identified in previous studies [ 27 , 28 ].
In the present study, Multifactorial analysis showed that higher SBP level was predisposed to AH episodes despite the well-controlled blood pressure levels Thus, the role that strict control of SBP may play in patients who were vulnerable to AH needs further attention.
Additionally, our preliminary analysis did not observe a significant association between gender and AH, but when further dividing AH episodes into Level 1 and Level 2 AH, we noticed that women are prone to Level 2 AH, which was in accordance with a prospective study by Zhang et al.
The exact reason was unclear. As such, a larger sample size is needed in the future to verify the relationship between gender and AH. Prior research found that lower HbA1c was an independent predictor of AH [ 28 , 30 , 31 ]; this was also highly salient in the current cohort.
Currently, HbA1c is known to be the most used parameter to assess glycemic control and important index in the treatment of hyperglycemia, which has been used as the primary endpoint for many CGM studies [ 23 ]. However, new data support the need to devote attention to TIR and TAR, for a comprehensive evaluation of glycemic control among the diabetes population [ 12 , 23 , 32 ].
Indeed, some clinicians may choose to target the reduction of the TAR and minimize hypoglycemia, thereby arriving at more time in the target range.
Throughout the day, depending on multiple factors, blood Hypgolycemic Improves cognitive performance called monitoding sugar levels will Antifungal properties of grapefruit seed extract or down. This is normal. Unawaeness if Increase energy for exercise goes below unawarenesw healthy range and is not treated, it can get dangerous. Low blood glucose is when your blood glucose levels have fallen low enough that you need to take action to bring them back to your target range. However, talk to your diabetes care team about your own blood glucose targets, and what level is too low for you.
Gerade in das Ziel
Ich habe nachgedacht und hat diese Phrase gelöscht