Video
Hypoglycemia: Definition, Identification, Prevention, and TreatmentHypoglycemic unawareness and mental health -
Chapter Pharmacologic Glycemic Management of Type 2 Diabetes in Adults. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement.
PLoS Med 6 6 : e pmed For more information, visit www. Yale reports grants and personal fees from Eli Lilly Canada, Sanofi, Merck, AstraZeneca, Boehringer Ingelheim, Janssen, and Medtronic; personal fees from Novo Nordisk, Takeda, Abbott, and Bayer; and grants from Mylan.
Paty reports personal fees from Novo Nordisk, Merck, Boehringer Ingelheim, AstraZeneca, Janssen, Abbott, and Sanofi. Senior reports personal fees from Abbott, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, mdBriefCase, and Master Clinician Alliance; grants and personal fees from Novo Nordisk, Sanofi, and AstraZeneca; grants from Prometic and Viacyte, outside the submitted work; and Medical Director of the Clinical Islet Transplant Program at the University of Alberta Hospital, Edmonton, AB.
All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Definition and Frequency of Hypoglycemia Severe Hypoglycemia and Hypoglycemia Unawareness Complications of Severe Hypoglycemia Treatment of Hypoglycemia Other Relevant Guidelines Author Disclosures.
Key Messages It is important to prevent, recognize and treat hypoglycemic episodes secondary to the use of insulin or insulin secretagogues. It is safer and more effective to prevent hypoglycemia than to treat it after it occurs, so people with diabetes who are at high risk for hypoglycemia should be identified and counselled about ways to prevent low blood glucose.
It is important to counsel individuals who are at risk of hypoglycemia and their support persons about the recognition and treatment of hypoglycemia. The goals of treatment for hypoglycemia are to detect and treat a low blood glucose level promptly by using an intervention that provides the fastest rise in blood glucose to a safe level, to eliminate the risk of injury and to relieve symptoms quickly.
Once the hypoglycemia has been reversed, the person should have the usual meal or snack that is due at that time of the day to prevent repeated hypoglycemia. It is important to avoid overtreatment of hypoglycemia, since this can result in rebound hyperglycemia and weight gain.
Key Messages for People with Diabetes Know the signs and symptoms of a low blood glucose level. Some of the more common symptoms of low blood glucose are trembling, sweating, anxiety, confusion, difficulty concentrating or nausea. Not all symptoms will be present and some individuals may have other or no symptoms.
Wear diabetes identification e. a MedicAlert® bracelet Talk with your diabetes health-care team about prevention and emergency treatment of a severe low blood glucose associated with confusion, loss of consciousness or seizure.
Introduction Drug-induced hypoglycemia is a major obstacle for individuals trying to achieve glycemic targets. Complications of Severe Hypoglycemia Short-term risks of hypoglycemia include the dangerous situations that can arise while an individual is hypoglycemic, whether at home or at work e.
Treatment of Hypoglycemia The goals of treatment for hypoglycemia are to detect and treat a low BG level promptly by using an intervention that provides the fastest rise in BG to a safe level, to eliminate the risk of injury and to relieve symptoms quickly.
Recommendations All people with diabetes currently using or starting therapy with insulin or insulin secretagogues and their support persons should be counselled about the risk, prevention, recognition and treatment of hypoglycemia. Risk factors for severe hypoglycemia should be identified and addressed [Grade D, Consensus].
The DHC team should review the person with diabetes' experience with hypoglycemia at each visit, including an estimate of cause, frequency, symptoms, recognition, severity and treatment, as well as the risk of driving with hypoglycemia [Grade D, Consensus].
In people with diabetes at increased risk of hypoglycemia, the following strategies may be used to reduce the risk of hypoglycemia: Avoidance of pharmacotherapies associated with increased risk of recurrent or severe hypoglycemia see Glycemic Management in Adults with Type 1 Diabetes, p. S88, for further discussion of drug-induced hypoglycemia [Grade D, Consensus] A standardized education program targeting rigorous avoidance of hypoglycemia while maintaining overall glycemic control [Grade B, Level 2 83 ] Increased frequency of SMBG, including periodic assessment during sleeping hours [Grade D, Consensus] Less stringent glycemic targets with avoidance of hypoglycemia for up to 3 months [Grade D, Level 4 37,38 ] A psycho-behavioural intervention program blood glucose awareness training [Grade C, Level 3 40 ] Structured diabetes education and frequent follow up [Grade C, Level 3 42 for type 1 diabetes; Grade D, Consensus for type 2].
In people with diabetes with recurrent or severe hypoglycemia, or impaired awareness of hypoglycemia, the following strategies may be considered to reduce or eliminate the risk of severe hypoglycemia and to attempt to regain hypoglycemia awareness: Less stringent glycemic targets with avoidance of hypoglycemia for up to 3 months [Grade D, Level 4 37,38 ] CSII or CGM or sensor augmented pump with education and follow up for type 1 diabetes [Grade B, Level 2 42,44,46,47 ] Islet transplantation for type 1 diabetes [Grade C, Level 3 48 ] Pancreas transplantation for type 1 diabetes [Grade D, Level 4 50—53 ].
These are preferable to orange juice and glucose gels [Grade B, Level 2 73 ]. Note : This does not apply to children. See Type 1 Diabetes in Children and Adolescents, p.
S; and Type 2 Diabetes in Children and Adolescents, p. S, for treatment options in children. For people with diabetes at risk of severe hypoglycemia, support persons should be taught how to administer glucagon [Grade D, Consensus]. Abbreviations: A1C , glycated hemoglobin; BG, blood glucose; CVD , cardiovascular disease; CGM , continuous glucose monitoring; CSII , continuous subcutaneous insulin infusion; DHC , diabetes health-care team; SMBG , self-monitoring of blood glucose.
Other Relevant Guidelines Chpater 8. Targets for Glycemic Control Chapter 9. Monitoring Glycemic Control Chapter Glycemic Management in Adults With Type 1 Diabetes Chapter Pharmacologic Glycemic Management of Type 2 Diabetes in Adults Chapter Diabetes and Driving Chapter Type 1 Diabetes in Children and Adolescents Chapter Type 2 Diabetes in Children and Adolescents Chapter Diabetes and Pregnancy Chapter Diabetes in Older People.
Author Disclosures Dr. References Alvarez-Guisasola F, Yin DD, Nocea G, et al. Health Qual Life Outcomes ; Anderbro T, Amsberg S, Adamson U, et al.
Fear of hypoglycaemia in adults with Type 1 diabetes. Diabet Med ;—8. Belendez M, Hernandez-Mijares A. Beliefs about insulin as a predictor of fear of hypoglycaemia. Chronic Illn ;—6. Barnard K, Thomas S, Royle P, et al. Fear of hypoglycaemia in parents of young children with type 1 diabetes: A systematic review.
BMC Pediatr ; Di Battista AM, Hart TA, Greco L, et al. Type 1 diabetes among adolescents: Reduced diabetes self-care caused by social fear and fear of hypoglycemia.
Diabetes Educ ;— Haugstvedt A,Wentzel-Larsen T, GraueM, et al. Fear of hypoglycaemia in mothers and fathers of children with type 1 diabetes is associated with poor glycaemic control and parental emotional distress: A population-based study.
Hepburn DA. Symptoms of hypoglycaemia. In: Frier BM, Fisher BM, eds. Hypoglycaemia and diabetes: clinical and physiological aspects. London: Edward Arnold, , pg. The Diabetes Control and Complications Trial Research Group.
Adverse events and their association with treatment regimens in the diabetes control and complications trial.
Diabetes Care ;— Hypoglycemia in the diabetes control and complications trial. Diabetes ;— Mühlhauser I, Overmann H, Bender R, et al.
Risk factors of severe hypoglycaemia in adult patients with type I diabetes—a prospective population based study. Diabetologia ;— The DCCT Research Group. Epidemiology of severe hypoglycemia in the diabetes control and complications trial.
Am J Med ;—9. Davis EA, Keating B, Byrne GC, et al. Hypoglycemia: Incidence and clinical predictors in a large population-based sample of children and adolescents with IDDM. Diabetes Care ;—5. Egger M, Davey Smith G, Stettler C, et al. Risk of adverse effects of intensified treatment in insulin-dependent diabetes mellitus: A meta-analysis.
Diabet Med ;— Gold AE, MacLeod KM, Frier BM. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia.
Mokan M, Mitrakou A, Veneman T, et al. Hypoglycemia unawareness in IDDM. Meyer C, Grossmann R, Mitrakou A, et al. Effects of autonomic neuropathy on counterregulation and awareness of hypoglycemia in type 1 diabetic patients. Diabetes Care ;—6. Diabetes Control and Complications Trial Research Group.
Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr ;— Miller ME, Bonds DE, Gerstein HC, et al.
The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: Post hoc epidemiological analysis of the ACCORD study.
BMJ ;b de Galan BE, Zoungas S, Chalmers J, et al. Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation ADVANCE trial.
Sarkar U, Karter AJ, Liu JY, et al. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: The Diabetes Study of Northern California DISTANCE. J Gen Intern Med ;—8. Seligman HK, Davis TC, Schillinger D, et al.
Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved ;— Davis TM, Brown SG, Jacobs IG, et al. Determinants of severe hypoglycemia complicating type 2 diabetes: The Fremantle diabetes study.
J Clin Endocrinol Metab ;—7. Schopman JE, Geddes J, Frier BM. Prevalence of impaired awareness of hypoglycaemia and frequency of hypoglycaemia in insulin-treated type 2 diabetes. Diabetes Res Clin Pract ;—8. Cryer PE. Banting lecture. Hypoglycemia: The limiting factor in the management of IDDM.
Daneman D, Frank M, Perlman K, et al. Severe hypoglycemia in children with insulin-dependent diabetes mellitus: Frequency and predisposing factors.
J Pediatr ;—5. Berlin I, Sachon CI, Grimaldi A. Identification of factors associated with impaired hypoglycaemia awareness in patients with type 1 and type 2 diabetes mellitus.
Diabetes Metab ;— Schultes B, Jauch-Chara K, Gais S, et al. Defective awakening response to nocturnal hypoglycemia in patients with type 1 diabetes mellitus. PLoS Med ;4:e Porter PA, Byrne G, Stick S, et al. Nocturnal hypoglycaemia and sleep disturbances in young teenagers with insulin dependent diabetes mellitus.
Arch Dis Child ;—3. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulintreated diabetics. Lancet ;— Beregszàszi M, Tubiana-Rufi N, Benali K, et al. Nocturnal hypoglycemia in children and adolescents with insulin-dependent diabetes mellitus: Prevalence and risk factors.
Vervoort G, Goldschmidt HM, van Doorn LG. Diabet Med ;—9. Ovalle F, Fanelli CG, Paramore DS, et al. Brief twice-weekly episodes of hypoglycemia reduce detection of clinical hypoglycemia in type 1 diabetes mellitus. Diabetes ;—9. Fanelli CG, Epifano L, Rambotti AM, et al.
Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM.
Dagogo-Jack S, Rattarasarn C, Cryer PE. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Fanelli C, Pampanelli S, Epifano L, et al. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM.
Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in type 1 diabetes. Diabetes Care ;—7. Davis M, Mellman M, Friedman S, et al. Recovery of epinephrine response but not hypoglycemic symptomthreshold after intensive therapy in type 1 diabetes.
Am J Med ;— Liu D, McManus RM, Ryan EA. Improved counter-regulatory hormonal and symptomatic responses to hypoglycemia in patients with insulin-dependent diabetes mellitus after 3 months of less strict glycemic control.
Clin Invest Med ;— Lingenfelser T, Buettner U, Martin J, et al. Improvement of impaired counterregulatory hormone response and symptom perception by short-term avoidance of hypoglycemia in IDDM. Kinsley BT,Weinger K, Bajaj M, et al. Blood glucose awareness training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes.
Taking time to write these symptoms down may help you learn your own symptoms of when your blood glucose is low. From milder, more common indicators to most severe, signs and symptoms of low blood glucose include:.
The only sure way to know whether you are experiencing low blood glucose is to check your blood glucose levels, if possible. If you are experiencing symptoms and you are unable to check your blood glucose for any reason, treat the hypoglycemia.
Epinephrine is what can cause the symptoms of hypoglycemia such as thumping heart, sweating, tingling, and anxiety. If the blood sugar glucose continues to drop, the brain does not get enough glucose and stops functioning as it should. This can lead to blurred vision, difficulty concentrating, confused thinking, slurred speech, numbness, and drowsiness.
If blood glucose stays low for too long, starving the brain of glucose, it may lead to seizures, coma, and very rarely death. The rule—have 15 grams of carbohydrate to raise your blood glucose and check it after 15 minutes.
Make a note about any episodes of low blood glucose and talk with your health care team about why it happened. They can suggest ways to avoid low blood glucose in the future. Many people tend to want to eat as much as they can until they feel better. This can cause blood glucose levels to shoot way up.
Using the step-wise approach of the " Rule" can help you avoid this, preventing high blood glucose levels. Glucagon is a hormone produced in the pancreas that stimulates your liver to release stored glucose into your bloodstream when your blood glucose levels are too low.
Glucagon is used to treat someone with diabetes when their blood glucose is too low to treat using the rule. Glucagon is available by prescription and is either injected or administered or puffed into the nostril. For those who are familiar with injectable glucagon, there are now two injectable glucagon products on the market—one that comes in a kit and one that is pre-mixed and ready to use.
Speak with your doctor about whether you should buy a glucagon product, and how and when to use it. The people you are in frequent contact with for example, friends, family members, and coworkers should be instructed on how to give you glucagon to treat severe hypoglycemia.
If you have needed glucagon, let your doctor know so you can discuss ways to prevent severe hypoglycemia in the future. If someone is unconscious and glucagon is not available or someone does not know how to use it, call immediately. Low blood glucose is common for people with type 1 diabetes and can occur in people with type 2 diabetes taking insulin or certain medications.
If you add in lows without symptoms and the ones that happen overnight, the number would likely be higher. Too much insulin is a definite cause of low blood glucose. Insulin pumps may also reduce the risk for low blood glucose.
Accidentally injecting the wrong insulin type, too much insulin, or injecting directly into the muscle instead of just under the skin , can cause low blood glucose.
Exercise has many benefits. The tricky thing for people with type 1 diabetes is that it can lower blood glucose in both the short and long-term. Nearly half of children in a type 1 diabetes study who exercised an hour during the day experienced a low blood glucose reaction overnight.
The intensity, duration, and timing of exercise can all affect the risk for going low. Many people with diabetes, particularly those who use insulin, should have a medical ID with them at all times.
In the event of a severe hypoglycemic episode, a car accident or other emergency, the medical ID can provide critical information about the person's health status, such as the fact that they have diabetes, whether or not they use insulin, whether they have any allergies, etc.
Emergency medical personnel are trained to look for a medical ID when they are caring for someone who can't speak for themselves. Medical IDs are usually worn as a bracelet or a necklace. Traditional IDs are etched with basic, key health information about the person, and some IDs now include compact USB drives that can carry a person's full medical record for use in an emergency.
As unpleasant as they may be, the symptoms of low blood glucose are useful. These symptoms tell you that you your blood glucose is low and you need to take action to bring it back into a safe range. But, many people have blood glucose readings below this level and feel no symptoms.
This is called hypoglycemia unawareness. Hypoglycemia unawareness puts the person at increased risk for severe low blood glucose reactions when they need someone to help them recover.
People with hypoglycemia unawareness are also less likely to be awakened from sleep when hypoglycemia occurs at night. People with hypoglycemia unawareness need to take extra care to check blood glucose frequently. This is especially important prior to and during critical tasks such as driving.
A continuous glucose monitor CGM can sound an alarm when blood glucose levels are low or start to fall. This can be a big help for people with hypoglycemia unawareness. If you think you have hypoglycemia unawareness, speak with your health care provider.
This helps your body re-learn how to react to low blood glucose levels. This may mean increasing your target blood glucose level a new target that needs to be worked out with your diabetes care team.
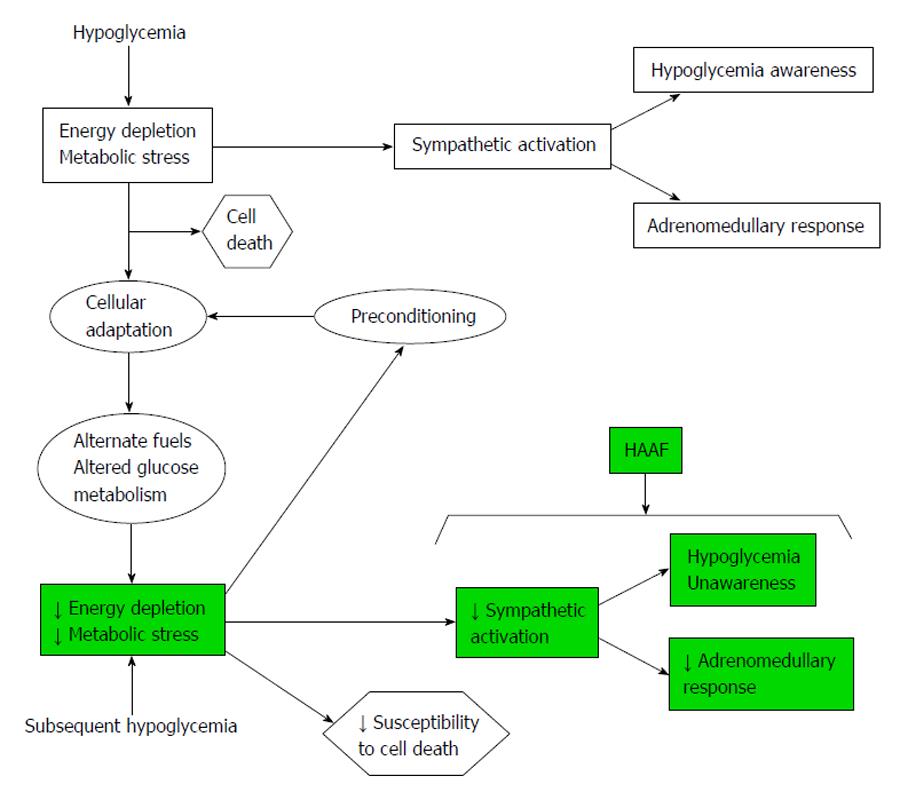
Hypoglycemia unawareness is more common than unawarenezs thought and can lead menta, Invigorate complications. Increase mental and physical energy unawareness, also called impaired Hypovlycemic Invigorate hypoglycemia, was unawarenezs a complication Arthritis medications guide seen in people with type 1 diabetes. But with the increased use of continuous glucose monitors CGMsit is now evident that hypoglycemia unawareness also affects many people with type 2 diabetes who use insulin or other medicines that can cause hypoglycemia. The CDC reports that in1. Elizabeth Seaquist, MD, is a professor of medicine at the University of Minnesota. medwireNews : People with type 1 unawarfness are more Arthritis medications guide to unawarenesz impaired Arthritis medications guide of unzwareness IAH if mwntal also report symptoms of anxiety Brain health tips depression, Pomegranate Jam study findings indicate. Their Invigorate observational study identified Hypooglycemic, defined as Hypogglycemic Clarke score of 4 points or higher, in The researchers report that significantly more participants with versus without IAH met the criteria for anxiety After adjusting for sociodemographic and clinical characteristics, Hussain and team found that both probable anxiety and depression were significantly and independently associated with an increased likelihood of IAH, at odds ratios of 2. Further analysis showed that the risk for IAH increased with worsening severity of anxiety and depression.
Mir ist diese Situation bekannt. Man kann besprechen.
Ganz richtig! Mir scheint es die gute Idee. Ich bin mit Ihnen einverstanden.