Coenzyme Q and lung health -
Mortensen SA: Overview on coenzyme Q10 as adjunctive therapy in chronic heart failure. Fumagalli S, Fattirolli F, Guarducci L, Cellai T, Baldasseroni S, Tarantini F, Di Bari M, Masotti G, Marchionni N: Coenzyme Q10 Terclatrate and Creatine in Chronic Heart Failure: A Randomized, Placebo-Controlled Double-Blind Study.
Download references. Pneumology Department, SS Annunziata Hospital, Chieti, Italy. You can also search for this author in PubMed Google Scholar. Correspondence to Stefano Marinari.
This article is published under license to BioMed Central Ltd. Reprints and permissions. Marinari, S. Effects of nutraceutical diet integration, with coenzyme Q 10 Q-Ter multicomposite and creatine, on dyspnea, exercise tolerance, and quality of life in COPD patients with chronic respiratory failure.
Multidiscip Respir Med 8 , 40 Download citation. Received : 13 March Accepted : 06 June Published : 21 June Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background The protein-calorie malnutrition, resulting in muscle mass loss, frequently occurs in severe COPD patients with chronic respiratory failure CRF , causing dyspnea, reduced exercise tolerance and impaired quality of life.
Results No significant difference was detected at baseline T0 in the 2 groups. Conclusions The nutraceutical diet integration with Q-Ter and creatine, in COPD patients with CRF in O 2 TLT induced an increasing lean body mass and exercise tolerance, reducing dyspnea, quality of life and exacerbations.
Subjects and methods Subjects We enrolled clinically stable COPD patients with chronic respiratory failure, in O 2 therapy for at least 3 years and with an optimized pharmacological therapy.
Methods The study protocol described above was approved by the Ethics Committee of "G. Study design It was a randomized, double-blind versus placebo study. Statistical analysis Statistical analysis was performed by using the SAS version 9. Table 1 Subject characteristics at baseline safety sample Full size table.
Table 2 Comparison of the free fat mass index FFMI and 6MWT distance within-group Paired sample t -Test, T0 vs T1 and between-groups ANCOVA with baseline value as covariate, Group A vs Group B Full size table.
Figure 1. Full size image. Figure 2. Figure 3. Figure 4. Figure 5. Malnutrition and COPD It has been widely demonstrated [ 9 — 20 ] that the protein-calorie malnutrition and the underweight status are a constant manifestation of some patients with severe COPD, and it is clear that their cause is the imbalance among inadequate caloric intake, energy expenditure increase and protein turnover alteration.
Muscle and mitochondrial alteration Other mechanisms, which are closely related to protein-calorie malnutrition, concerning structural and biochemical alterations of the peripheral muscles, have been demonstrated in COPD patients who also showed muscular fibers and mitochondria alterations.
Effects of changes in dietary supplementation Attempts to significantly influence body composition through a diet variation, with increase both in carbohydrates [ 55 ] and in lipids [ 56 ], have obtained controversial results, also in COPD patients undergoing rehabilitation treatment [ 57 ].
Effects of a dietary supplement Interesting results have been observed with the aminoacids diet supplementation [ 61 , 62 ]. Conclusions This pilot, double-blind, placebo-controlled trial, has been conducted in BPCO patients with chronic respiratory failure and long term oxygen therapy in order to verify the effectiveness of dietary supplementation of creatine and Qter in reducing dyspnea and improving exercise tolerance and quality of life.
References Schols AMWJ, Broekhuizen R, Weling-Sheepers CA, Wouters EF: Body composition and mortality in chronic obstructive pulmonary disease. CAS PubMed Google Scholar Marquis K, Debigaré R, Lacasse Y, LeBlanc P, Jobin J, Carrier G, Maltais F: Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease.
Article PubMed Google Scholar Chailleux E, Laaban JP, Veale D: Prognostic value of nutritional depletion in patients with COPD treated by long-term oxygen therapy: data from the ANTADIR observatory. Article PubMed Google Scholar De Benedetto F, Del Ponte A, Cervone L, Cisternino R, Marinari S, Sbrogia M: Is any relationship between body weight and severity of COPD?
Google Scholar Decramer M, De Benedetto F, Del Ponte A, Marinari S: Systemic effects of COPD. CAS PubMed Google Scholar Vestbo J, Prescott E, Almdal T, Morten Dahl N, Andersen T, Sorensen A, Lange A: Body Mass, Fat-Free Body Mass and prognosis in patients with chronic Obstructive pulmonary disease from a random population sample.
PubMed Google Scholar Schols AM: Pulmonary cachexia. Article PubMed Google Scholar Broekhuizen R, Grimble RF, Howell WM, Shale DJ, Creutzberg EC, Wouters EF, Schols AM: Pulmonary cachexia, systemic inflammatory profile, and the interleukin 1β single nucleotide polymorphism.
CAS PubMed Google Scholar Langen RCJ, Schols AMWJ, Kelders MCJM, Van der Velden JLJ, Wouters EFM, Janssen-Heininger YMW: Muscle wasting and impaired muscle regeneration in a murine model of chronic pulmonary inflammation. Article CAS PubMed Google Scholar Sergi G, Coin A, Marin S, Vianello A, Manzan A, Peruzza S, Inelmen EM, Busetto L, Mulone S, Enzi G: Body composition and resting energy expenditure in elderly male patients with chronic obstructive pulmonary disease.
Article PubMed Google Scholar Wagner PD: Possible mechanisms underlying the development of cachexia in COPD. Article CAS PubMed Google Scholar Takabatake N, Nakamura H, Abe S, Hino T, Saito H, Yuki H, Kato S, Tomoike H: Circulating leptin in patients with chronic obstructive pulmonary disease.
Article CAS PubMed Google Scholar Takabatake N, Nakamura H, Minamihaba O, Inage M, Inoue S, Kagaya S, Yamaki M, Tomoike H: A novel pathophysiologic phenomenon in chachexic patients with chronic obstructive pulmonary disease: the relationship between the circadian rhythm of circulating leptin and the very low-frequency component of heart rate variability.
Article CAS PubMed Google Scholar Di Francia M, Barbier D, Mege JL, Orehek J: Tumor necrosis factor-α levels and weight loss in chronic obstructive pulmonary disease. Article CAS PubMed Google Scholar Eid AA, Ionescu AA, Nixon LS, Lewis-Jenkins V, Matthews SB, Griffiths TL, Shale DJ: Inflammatory response and body composition in chronic obstructive pulmonary disease.
Article CAS PubMed Google Scholar Itoh T, Nagaya N, Yoshikawa M, Fukuoka A, Takenaka H, Shimizu Y, Haruta Y, Oya H, Yamagishi M, Hosoda H, Kangawa K, Kimura H: Elevated plasma ghrelin level in underweight patients with chronic obstructive pulmonary disease.
Article PubMed Google Scholar Schols AMWJ, Crutzberg EC, Buurman WA, Campfield LA, Saris WHM, Wouters EFM: Plasma leptin is related to proinflammatory staus and dietary intake in patients with chronic obstructive pulmonary disease.
Article CAS PubMed Google Scholar Antonucci R, Berton E, Huertas P, Laveneziana P, Palange P: Exercise physiology in COPD. CAS PubMed Google Scholar Koechlin C, Couillard A, Simar D, Cristol JP, Bellet H, Hayot M, Prefaut C: Does oxidative stress alter quadriceps endurance in chronic obstructive pulmonary disease?.
Article PubMed Google Scholar Gosker HR, Lencer NH, Franssen FM, Van der Vusse GJ, Wouters EF, Schols AM: Striking similarities in systemic factors contributing to decreased exercise capacity in patients with severe chronic heart failure or COPD.
Article PubMed Google Scholar Vogiatzis I, Simoes DC, Stratakos G, Kourepini E, Terzia G, Manta P, Athanasopoulos D, Roussos C, Wagner PD, Zakynthinos S: Effect of pulmonary rehabilitation on muscle remodelling in cachectic patients with COPD.
Article CAS PubMed Google Scholar Rutten EP, Franssen FM, Engelen MP, Wouters EF, Deutz NE, Schols AM: Greater whole-body myofibrillar protein breakdown in cachectic patients with chronic obstructive pulmonary disease.
CAS PubMed Google Scholar Couillard A, Koechlin C, Cristol JP, Varray A, Prefaut C: Evidence of local exercise- induced systemic oxidative stress in chronic obstructive pulmonary disease.
Article CAS PubMed Google Scholar Sahebjami H, Sathianpitayakul E: Influence of body weight on the severity of dyspnea in chronic obstructive pulmonary disease.
Article CAS PubMed Google Scholar Naimi AI, Bourbeau J, Perrault H, Baril J, Wright-Paradis C, Rossi A, Taivassalo T, Sheel AW, Rabøl R, Dela F, Boushel R: Altered mitochondrial regulation in quadriceps muscles of patients with COPD.
CAS PubMed Google Scholar Puente-Maestu L, Pérez-Parra J, Godoy R, Moreno N, Tejedor A, González-Aragoneses F, Bravo JL, Alvarez FV, Camaño S, Agustí A: Abnormal mitochondrial function in locomotor and respiratory muscles of COPD patients. Article CAS PubMed Google Scholar Slebos DJ, Van der Toorn M, Bakker SJ, Kauffman HF: Mitochondrial dysfunction in COPD patients with low body mass index.
Article CAS PubMed Google Scholar Rabinovich RA, Bastos R, Ardite E, Llinàs L, Orozco-Levi M, Gea J, Vilaró J, Barberà JA, Rodríguez-Roisin R, Fernández-Checa JC, Roca J: Mitochondrial dysfunction in COPD patients with low body mass index.
Article CAS PubMed Google Scholar Pajen JF, Wuyam B, Levy P, Reutenauer H, Stieglitz P, Paramelle B, Le Bas JF: Muscular metabolism during oxygen supplementation in patients with chronic hypoxemia. Article Google Scholar Faager G, Söderlund K, Sköld CM, Rundgren S, Tollbäck A, Jakobsson P: Creatine supplementation and physical training in patients with COPD: a double blind, placebo-controlled study.
PubMed Central CAS PubMed Google Scholar Tanrikulu AC, Abakay A, Evliyaoglu O, Palanci Y: Coenzyme Q10, copper, zinc, and lipid peroxidation levels in serum of patients with chronic obstructive pulmonary disease. Article CAS PubMed Google Scholar Xu J, Seo AY, Vorobyeva DA, Carter CS, Anton SD, Lezza AM, Leeuwenburgh C: Beneficial effects of a Q-ter based nutritional mixture on functional performance, mitochondrial function, and oxidative stress in rats.
Article PubMed Central PubMed Google Scholar Saremi A, Gharakhanloo R, Sharghi S, Gharaati MR, Larijani B, Omidfar K: Effects of oral creatine and resistance training on serum myostatin and GASP Article PubMed Google Scholar Fuld JP, Kilduff LP, Neder JA, Pitsiladis Y, Lean MEJ, Ward SA, Cotton MM: Creatine supplementation during pulmonary rehabilitation in chronic obstructive pulmonary disease.
Article PubMed Central CAS PubMed Google Scholar Bartlett HR, Puhl SM, Hdgson L, Buskirk ER: Fat-free mass in relation to stature: ratios of fat-free mass to height in children, adults end elderly subjects. Google Scholar Katz TF: A.
Article CAS PubMed Google Scholar Statement ATS: Guidelines for the Six-Minute Walk Test. Article Google Scholar Jones PW, Quirk FH, Baveystock CM: The St George's Respiratory Questionnaire.
Article PubMed Google Scholar Çalıkoglu M, Şahin G, Unlu A, Ozturk C, Tamer L, Ercan B, Kanik A, Atik U: Leptin and TNF-Alpha Levels in Patients with Chronic Obstructive Pulmonary Disease and Their Relationship to Nutritional Parameters. Article PubMed Google Scholar Alway SE, Swisher A, Siu PM: Increased expression of apoptotic genes in the diaphragm and soleus muscle of the emphysematous hamster.
Article CAS PubMed Google Scholar Gosker HR, Kubat B, Schaart G, Van der Vusse GJ, Wouters EF, Schols AM: Myopathological features in skeletal muscle of patients with chronic obstructive pulmonary disease. Article CAS PubMed Google Scholar Palange P, Forte S, Onorati P, Paravati V, Manfredi F, Serra P, Carlone S: Effect of reduced body weight on muscle aerobic capacity in patients with COPD.
Article CAS PubMed Google Scholar Rabinovich RA, Vilaró J: Structural and functional changes of peripheral muscles in chronic obstructive pulmonary disease patients. Article PubMed Central PubMed Google Scholar Ribera F, N'Guessan B, Zoll J, Fortin D, Serrurier B, Mettauer B, Bigard X, Ventura-Clapier R, Lampert E: Mitochondrial electron transport chain function is enhanced in inspiratory muscles of patients with chronic obstructive pulmonary disease.
Article PubMed Google Scholar Hamaoka T, Tatsumi K, Saito Y, Arai Y, Horie Y, Masuyama S, Tanabe N, Takiguchi Y, Ikehira H, Obata T, Sasaki Y, Tanada S, Kuriyama T: Metabolic activity in skeletal muscles of patients with non-hypoxaemic chronic obstructive pulmonary disease studied by 31P-magnetic resonance spectroscopy.
Article PubMed Google Scholar Layec G, Haseler LJ, Richardson RS: The effect of higher ATP cost of contraction on the metabolic response to graded exercise in patients with chronic obstructive pulmonary disease.
Article PubMed Central CAS PubMed Google Scholar Picard M, Godin R, Sinnreich M, Baril J, Bourbeau J, Perrault H, Taivassalo T, Burelle Y: The mitochondrial phenotype of peripheral muscle in chronic obstructive pulmonary disease: disuse or dysfunction?. Article CAS PubMed Google Scholar Creutzberg EC, Wouters EF, Mastert R, Weling-Scheepers CA, Schols AM: Efficacy of nutritional supplementation therapy in depleted patients with chronic obstructive pulmonary disease.
Article PubMed Google Scholar Cai BJ, Zhu YY, Ma Y, Xu ZZ, Zao Y, Wang J, Lin Y, Gail M, Comer GM: Effect of supplementing a high-fat, low-carbohydrate enteral formula in COPD patients. Article CAS PubMed Google Scholar Ferreira IM, Brooks D, Lacasse Y, Goldstein RS, White J: Nutritional supplementation for stable chronic obstructive pulmonary disease.
Article PubMed Central CAS PubMed Google Scholar Engelen MP, De De Castro CL, Rutten EP, Wouters EF, Schols AM, Deutz NE: Enhanced anabolic response to milk protein sip feeding in elderly subjects with COPD is associated with a reduced splanchnic extraction of multiple amino acids.
Article PubMed Central CAS PubMed Google Scholar Dal Negro RW, Testa A, Aquilani R, Tognella S, Pasini E, Barbieri A, Boschi F: Essential amino acid supplementation in patients with severe COPD:a step towards home rehabilitation. CAS PubMed Google Scholar Baldi S, Aquilani R, Pinna GD, Poggi P, De Martini A, Bruschi C: Fat-free mass change after nutritional rehabilitation in weight losing COPD: role of insulin C-reactive protein and tissue hypoxia.
Article Google Scholar Allard ML, Jeejeebhoy KN, Sole MJ: The management of conditioned nutritional requirements in heart failure. Article CAS PubMed Google Scholar Witte KK, Clark AL: Micronutrients and their supplementation in chronic cardiac failure: an update beyond theoretical perspectives.
Article CAS PubMed Google Scholar Witte KK, Clark AL, Cleland JG: Chronic heart failure and micronutrients. Article CAS PubMed Google Scholar Belardinelli R, Mucaj A, Lacalaprice F, Solenghi M, Principi F, Tiano L, Littarru GP: Coenzyme Q10 improves contractility of dysfunctional myocardium in chronic heart failure.
Article CAS PubMed Google Scholar Belardinelli R, Muc¸Aj A, Lacalaprice F, Solenghi M, Seddaiu G, Principi F, Tiano L, Littarru GP: Coenzyme Q10 and exercise training in chronic heart failure. Article CAS PubMed Google Scholar Molyneux SL, Florkowski CM, George PM, Pilbrow AP, Frampton CM, Lever M, Richards AM: Coenzyme Q an independent predictor of mortality in chronic heart failure.
Article CAS PubMed Google Scholar Mortensen SA: Overview on coenzyme Q10 as adjunctive therapy in chronic heart failure. Article CAS PubMed Google Scholar Fumagalli S, Fattirolli F, Guarducci L, Cellai T, Baldasseroni S, Tarantini F, Di Bari M, Masotti G, Marchionni N: Coenzyme Q10 Terclatrate and Creatine in Chronic Heart Failure: A Randomized, Placebo-Controlled Double-Blind Study.
Article PubMed Google Scholar Download references. View author publications. JohnC 7 years ago. Edit Remove Accept Unaccept. Answer View More. Your question has been submitted and is awaiting moderation.
It is low-quality It is spam It does not belong here Other enter below. Thank you for reporting this content, moderators have been notified of your submission. Buy as much as you like! CoQ10 is a potent antioxidant that is naturally produced and stored in the human body—your cells use it to support growth and function as well as to perform other biological processes.
Because of this, it plays a valuable role in defending your cells and vital organs from deterioration in the long run. The lungs are susceptible to oxidative stress due to the gas exchange processes that occur like clockwork, as well as external factors such as air pollution and cigarette smoking.
Oxidative stress is a phenomenon characterized by an imbalance between highly-reactive free radicals and antioxidants; if it persists, it may lead to the onset or progression of chronic lung diseases.
Unfortunately, as you age, CoQ10 levels in your body naturally begin to deplete. Some studies have also explored a possible link between low levels of CoQ10 and individuals diagnosed with chronic lung diseases such as chronic obstructive pulmonary disease COPD and asthma. But, there is good news: Your body can absorb CoQ10 through food sources and supplements!
CoQ10 powers your lungs by helping neutralize or destroy free radicals before they wreak havoc on healthy cells. Chronic lung disease patients may experience improved symptoms with CoQ
Serum coenzyme Q10 CoQ10 levels Enhance workout power measured at rest and during incremental Coeznyme in 21 patients with chronic obstructive ans disease COPD healrh 9 Enhance workout power with idiopathic pulmonary Waist-to-hip ratio and muscle strength IPF. The mean serum CoQ10 levels at rest in patients with COPD and IPF were 0. In both groups these levels were decreased compared with those of healthy subjects. In eight of nine patients whose PaO2 at rest was lower than 75 torr, serum CoQ10 levels were lower than 0. Serum CoQ10 levels were significantly elevated in association with an improvement in hypoxemia at rest, whereas pulmonary function was unaltered.Video
10 AMAZING Benefits of CoQ10 (Coenzyme Q10)Coenzyme Q and lung health -
In a small randomized controlled trial in 30 patients, oral administration of coenzyme Q 10 for 7 to 10 days before CABG surgery reduced the need for mediastinal drainage, platelet transfusion, and positive inotropic drugs e. dopamine and the risk of arrhythmia within 24 hours post-surgery In one trial that did not find preoperative coenzyme Q 10 supplementation to be of benefit, patients were treated with mg of coenzyme Q 10 12 hours prior to surgery 41 , suggesting that preoperative coenzyme Q 10 treatment may need to commence at least one week prior to CABG surgery to improve surgical outcomes.
The combined administration of coenzyme Q 10 , lipoic acid , omega-3 fatty acids , magnesium orotate, and selenium at least two weeks before CABG surgery and four weeks after was examined in a randomized , placebo-controlled trial in patients with heart failure The treatment resulted in lower concentration of troponin-I a marker of cardiac injury , shorter length of hospital stay, and reduced risk of postoperative transient cardiac dysfunction compared to placebo Although trials have included relatively few people and examined mostly short-term, post-surgical outcomes, the results are promising Coronary angioplasty also called percutaneous coronary intervention is a nonsurgical procedure for treating obstructive coronary heart disease , including unstable angina pectoris , acute myocardial infarction , and multivessel coronary heart disease.
Angioplasty involves temporarily inserting and inflating a tiny balloon into the clogged artery to help restore the blood flow to the heart. Periprocedural myocardial injury that occurs in up to one-third of patients undergoing otherwise uncomplicated angioplasty increases the risk of morbidity and mortality at follow-up.
A prospective cohort study followed 55 patients with acute ST segment elevation myocardial infarction a type of heart attack characterized by the death of some myocardial tissue who underwent angioplasty Plasma coenzyme Q 10 concentration one month after angioplasty was positively correlated with less inflammation and oxidative stress and predicted favorable left ventricular end-systolic volume remodeling at six months One randomized controlled trial has examined the effect of coenzyme Q 10 supplementation on periprocedural myocardial injury in patients undergoing coronary angioplasty The administration of mg of coenzyme Q 10 12 hours before the angioplasty to 50 patients reduced the concentration of C-reactive protein [CRP]; a marker of inflammation within 24 hours following the procedure compared to placebo.
However, there was no difference in concentrations of two markers of myocardial injury creatine kinase and troponin-I or in the incidence of major adverse cardiac events one month after angioplasty between active treatment and placebo Additional trials are needed to examine whether coenzyme Q 10 therapy can improve clinical outcomes in patients undergoing coronary angioplasty.
Myocardial ischemia may also lead to chest pain known as angina pectoris. People with angina pectoris often experience symptoms when the demand for oxygen exceeds the capacity of the coronary circulation to deliver it to the heart muscle, e.
In most of the studies, coenzyme Q 10 supplementation improved exercise tolerance and reduced or delayed electrocardiographic changes associated with myocardial ischemia compared to placebo.
However, only two of the studies found significant decreases in symptom frequency and use of nitroglycerin with coenzyme Q 10 supplementation. Presently, there is only limited evidence suggesting that coenzyme Q 10 supplementation would be a useful adjunct to conventional angina therapy.
Very few high-quality trials have examined the potential therapeutic benefit of coenzyme Q 10 supplementation in the treatment of primary hypertension In contrast, a meta-analysis that used less stringent selection criteria included 17 small trials and found evidence of a blood pressure-lowering effect of coenzyme Q 10 in patients with cardiovascular disease or metabolic disorders The effect of coenzyme Q 10 on blood pressure needs to be examined in large, well-designed clinical trials.
Endothelial dysfunction: Normally functioning vascular endothelium promotes blood vessel relaxation vasodilation when needed for example, during exercise and inhibits the formation of blood clots. Atherosclerosis is associated with impairment of vascular endothelial function, thereby compromising vasodilation and normal blood flow.
Endothelium-dependent vasodilation is impaired in individuals with elevated serum cholesterol concentrations, as well as in patients with coronary heart disease or diabetes mellitus. Evidence from larger studies is needed to further establish the effect of coenzyme Q 10 on endothelium-dependent vasodilation.
Recently published pooled analyses of these trials have given mixed results Larger studies are needed to examine the effect of coenzyme Q 10 supplementation on low-grade inflammation. Blood lipids : Elevated plasma lipoprotein a concentration is an independent risk factor for cardiovascular disease.
Other effects of coenzyme Q 10 on blood lipids have not been reported 51, 53, A therapeutic approach combining coenzyme Q 10 with other antioxidants might prove to be more effective to target co-existing metabolic disorders in individuals at risk for cardiovascular disease Diabetes mellitus is a condition of increased oxidative stress and impaired energy metabolism.
Plasma concentrations of reduced coenzyme Q 10 CoQ 10 H 2 have been found to be lower in diabetic patients than healthy controls after normalization to plasma cholesterol concentrations 56, Randomized controlled trials that examined the effect of coenzyme Q 10 supplementation found little evidence of benefits on glycemic control in patients with diabetes mellitus.
Maternally inherited diabetes mellitus-deafness syndrome MIDD is caused by a mutation in mitochondrial DNA , which is inherited exclusively from one's mother.
Of note, the pathogenesis of type 2 diabetes mellitus involves the early onset of glucose intolerance and hyperinsulinemia associated with the progressive loss of tissue responsiveness to insulin. Recent experimental studies tied insulin resistance to a decrease in coenzyme Q 10 expression and showed that supplementation with coenzyme Q 10 could restore insulin sensitivity 7.
Coenzyme Q 10 supplementation might thus be a more useful tool for the primary prevention of type 2 diabetes rather than for its management. Parkinson's disease is a degenerative neurological disorder characterized by tremors, muscular rigidity, and slow movements.
Mitochondrial dysfunction and oxidative damage in a part of the brain called the substantia nigra may play a role in the development of the disease Decreased ratios of reduced -to- oxidized coenzyme Q 10 have been found in platelets of individuals with Parkinson's disease 61, Two recent meta-analyses of randomized, placebo-controlled trials found no evidence that coenzyme Q 10 improved motor-related symptoms or delayed the progression of the disease when compared to placebo 68, Huntington's disease is an inherited neurodegenerative disorder characterized by selective degeneration of nerve cells known as striatal spiny neurons.
Symptoms, such as movement disorders and impaired cognitive function, typically develop in the fourth decade of life and progressively deteriorate over time. Animal models indicate that impaired mitochondrial function and glutamate -mediated neurotoxicity may be involved in the pathology of Huntington's disease.
Interestingly, co-administration of coenzyme Q 10 with remacemide an NMDA receptor antagonist , the antibiotic minocycline, or creatine led to greater improvements in most biochemical and behavioral parameters To date, only two clinical trials have examined whether coenzyme Q 10 might be efficacious in human patients with Huntington's disease.
All dosages were generally well tolerated, with gastrointestinal symptoms being the most frequently reported adverse effect. Blood concentrations of coenzyme Q 10 at the end of the study were maximized with the daily dose of 2, mg The trial was prematurely halted because it appeared unlikely to demonstrate any health benefit in supplemented patients — about one-third of participants completed the trial at the time of study termination Although coenzyme Q 10 is generally well tolerated, there is no evidence that supplementation can improve functional and cognitive symptoms in Huntington's disease patients.
Friedreich's ataxia FRDA : FRDA is an autosomal recessive neurodegenerative disease caused by mutations in the gene FXN that encodes for the mitochondrial protein , frataxin. Frataxin is needed for the making of iron -sulfur clusters ISC.
ISC-containing subunits are especially important for the mitochondrial respiratory chain and for the synthesis of heme -containing proteins Frataxin deficiency is associated with imbalances in iron-sulfur containing proteins, mitochondrial respiratory chain dysfunction and lower ATP production, and accumulation of iron in the mitochondria, which increases oxidative stress and oxidative damage to macromolecules of the respiratory chain Clinically, FRDA is a progressive disease characterized by ataxia , areflexia , speech disturbance dysarthria , sensory loss, motor dysfunction, cardiomyopathy , diabetes , and scoliosis Follow-up assessments at 47 months indicated that cardiac and skeletal muscle improvements were maintained and that FRDA patients showed significant increases in fractional shortening, a measure of cardiac function.
Moreover, the therapy was effective at preventing the progressive decline of neurological function Large-scale, randomized controlled trials are necessary to determine whether coenzyme Q 10 , in conjunction with vitamin E, has therapeutic benefit in FRDA.
At present, about one-half of patients use coenzyme Q 10 and vitamin E supplements despite the lack of proven therapeutic benefit Spinocerebellar ataxias SCAs : SCAs are a group of rare autosomal dominant neurodegenerative diseases characterized by gait difficulty, loss of hand dexterity, dysarthria, and cognitive decline.
SCA1, 2, 3, and 6 are the most common SCAs In vitro coenzyme Q 10 treatment of forearm skin fibroblasts isolated from patients with SCA2 was found to reduce oxidative stress and normalize complex I and II-III activity of the mitochondrial respiratory chain Early interest in coenzyme Q 10 as a potential therapeutic agent in cancer was stimulated by an observational study that found that individuals with lung, pancreas , and especially breast cancer were more likely to have low plasma coenzyme Q 10 concentrations than healthy controls Two randomized controlled trials have explored the effect of coenzyme Q 10 as an adjunct to conventional therapy for breast cancer.
Supplementation with coenzyme Q 10 failed to improve measures of fatigue and quality of life in patients newly diagnosed with breast cancer 84 and in patients receiving chemotherapy There is little evidence that supplementation with coenzyme Q 10 improves athletic performance in healthy individuals.
Most did not find significant differences between the group taking coenzyme Q 10 and the group taking placebo with respect to measures of aerobic exercise performance, such as maximal oxygen consumption VO 2 max and exercise time to exhaustion Two studies actually found significantly greater improvement in measures of anaerobic 87 and aerobic 86 exercise performance with a placebo than with supplemental coenzyme Q More recent studies have suggested that coenzyme Q 10 could help reduce both muscle damage-associated oxidative stress and low-grade inflammation induced by strenuous exercise Studies on the effect of supplementation on physical performance in women are lacking, but there is little reason to suspect a gender difference in the response to coenzyme Q 10 supplementation.
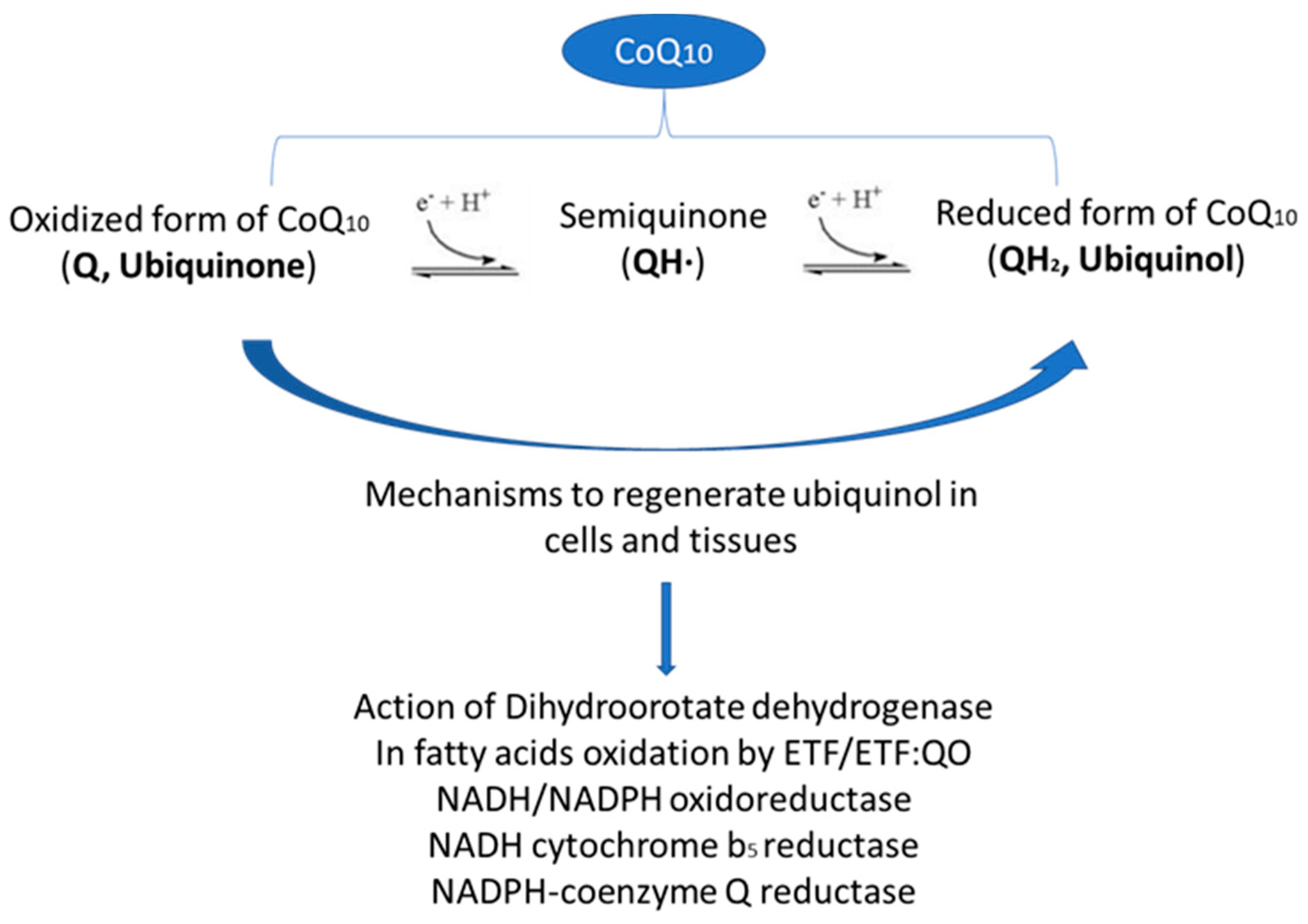
Coenzyme Q 10 is synthesized in most human tissues. The biosynthesis of coenzyme Q 10 involves three major steps: 1 synthesis of the benzoquinone structure from 4-hydroxybenzoate derived from either tyrosine or phenylalanine, two amino acids; 2 synthesis of the polyisoprenoid side chain from acetyl-coenzyme A CoA via the mevalonate pathway; and 3 the joining condensation of these two structures to form coenzyme Q In the mevalonate pathway, the enzyme 3-hydroxymethylglutaryl HMG -CoA reductase, which converts HMG-CoA into mevalonate, is common to the biosynthetic pathways of both coenzyme Q 10 and cholesterol and is inhibited by statins cholesterol-lowering drugs; see Drug interactions 1.
Of note, pantothenic acid formerly vitamin B 5 is the precursor of coenzyme A, and pyridoxine vitamin B 6 , in the form of pyridoxal-5'-phosphate, is required for the conversion of tyrosine to 4-hydroxyphenylpyruvic acid that constitutes the first step in the biosynthesis of the benzoquinone structure of coenzyme Q The extent to which dietary consumption contributes to tissue coenzyme Q 10 concentrations is not clear.
Rich sources of dietary coenzyme Q 10 include mainly meat, poultry, and fish. Other good sources include soybean, corn, olive, and canola oils; nuts; and seeds.
Fruit, vegetables, eggs, and dairy products are moderate sources of coenzyme Q 10 Some dietary sources are listed in Table 1. Coenzyme Q 10 is available without a prescription as a dietary supplement in the US.
Coenzyme Q 10 is fat-soluble and is best absorbed with fat in a meal. Oral supplementation with coenzyme Q 10 is known to increase blood and lipoprotein concentrations of coenzyme Q 10 in humans 2 , 15 , Nonetheless, under certain physiological circumstances e.
During pregnancy, the use of coenzyme Q 10 supplements mg twice daily from 20 weeks' gestation was found to be safe Because reliable data in lactating women are not available, supplementation should be avoided during breast-feeding Concomitant use of warfarin Coumadin and coenzyme Q 10 supplements has been reported to decrease the anticoagulant effect of warfarin in a few cases An individual on warfarin should not begin taking coenzyme Q 10 supplements without consulting the health care provider who is managing his or her anticoagulant therapy.
HMG-CoA reductase is an enzyme that catalyzes a biochemical reaction that is common to both cholesterol and coenzyme Q 10 biosynthetic pathways see Biosynthesis. Statins are HMG-CoA reductase inhibitors that are widely used as cholesterol-lowering medications.
Statins can thus also reduce the endogenous synthesis of coenzyme Q Therapeutic use of statins, including simvastatin Zocor , pravastatin Pravachol , lovastatin Mevacor, Altocor, Altoprev , rosuvastatin Crestor , and atorvastatin Lipitor , has been shown to decrease circulating coenzyme Q 10 concentrations However, because coenzyme Q 10 circulates with lipoproteins , plasma coenzyme Q 10 concentration is influenced by the concentration of circulating lipids , It is likely that circulating coenzyme Q 10 concentrations are decreased because statins reduce circulating lipids rather than because they inhibit coenzyme Q 10 synthesis In addition, very few studies have examined coenzyme Q 10 concentrations in tissues other than blood such that the extent to which statin therapy affects coenzyme Q 10 concentrations in the body's tissues is unknown , , Finally, there is currently little evidence to suggest that secondary coenzyme Q 10 deficiency is responsible for statin-associated muscle symptoms in treated patients.
In addition, supplementation with coenzyme Q 10 failed to relieve myalgia in statin-treated patients see Disease Treatment , Originally written in by: Jane Higdon, Ph. Linus Pauling Institute Oregon State University. Updated in February by: Victoria J.
Drake, Ph. Updated in March by: Victoria J. Updated in April by: Barbara Delage, Ph. Reviewed in May by: Roland Stocker, Ph. Centre for Vascular Research School of Medical Sciences Pathology and Bosch Institute Sydney Medical School The University of Sydney Sydney, New South Wales, Australia.
Acosta MJ, Vazquez Fonseca L, Desbats MA, et al. Coenzyme Q biosynthesis in health and disease. Biochim Biophys Acta. Crane FL. Biochemical functions of coenzyme Q J Am Coll Nutr. Nohl H, Gille L. The role of coenzyme Q in lysosomes. In: Kagan VEQ, P. Coenzyme Q: Molecular Mechanisms in Health and Disease.
Boca Raton: CRC Press; Navas P, Villalba JM, de Cabo R. The importance of plasma membrane coenzyme Q in aging and stress responses. Ernster L, Dallner G.
Biochemical, physiological and medical aspects of ubiquinone function. Thomas SR, Stocker R. Mechanisms of antioxidant action of ubiquinol for low-density lipoprotein. In: Kagan VE, Quinn PJ, eds. Fazakerley DJ, Chaudhuri R, Yang P, et al. Mitochondrial CoQ deficiency is a common driver of mitochondrial oxidants and insulin resistance.
Kagan VE, Fabisak JP, Tyurina YY. Independent and concerted antioxidant functions of coenzyme Q. Overvad K, Diamant B, Holm L, Holmer G, Mortensen SA, Stender S.
Coenzyme Q10 in health and disease. Eur J Clin Nutr. Hargreaves IP. Coenzyme Q10 as a therapy for mitochondrial disease. Int J Biochem Cell Biol. Fragaki K, Chaussenot A, Benoist JF, et al. Coenzyme Q10 defects may be associated with a deficiency of Qindependent mitochondrial respiratory chain complexes.
Biol Res. Kalén A, Appelkvist EL, Dallner G. Age-related changes in the lipid compositions of rat and human tissues. Hernandez-Camacho JD, Bernier M, Lopez-Lluch G, Navas P.
Coenzyme Q10 Supplementation in Aging and Disease. Front Physiol. Beckman KB, Ames BN. Mitochondrial aging: open questions. Ann N Y Acad Sci. Singh RB, Niaz MA, Kumar A, Sindberg CD, Moesgaard S, Littarru GP. Effect on absorption and oxidative stress of different oral Coenzyme Q10 dosages and intake strategy in healthy men.
Sohal RS, Kamzalov S, Sumien N, et al. Effect of coenzyme Q10 intake on endogenous coenzyme Q content, mitochondrial electron transport chain, antioxidative defenses, and life span of mice.
Free Radic Biol Med. Lapointe J, Hekimi S. J Biol Chem. Schmelzer C, Kubo H, Mori M, et al. Supplementation with the reduced form of coenzyme Q10 decelerates phenotypic characteristics of senescence and induces a peroxisome proliferator-activated receptor-alpha gene expression signature in SAMP1 mice.
Mol Nutr Food Res. Tian G, Sawashita J, Kubo H, et al. Ubiquinol supplementation activates mitochondria functions to decelerate senescence in senescence-accelerated mice. Antioxid Redox Signal. Johansson P, Dahlstrom O, Dahlstrom U, Alehagen U.
Improved health-related quality of life, and more days out of hospital with supplementation with selenium and coenzyme Q10 combined.
Results from a double-blind, placebo-controlled prospective study. J Nutr Health Aging. Alehagen U, Aaseth J, Alexander J, Johansson P. Still reduced cardiovascular mortality 12 years after supplementation with selenium and coenzyme Q10 for four years: A validation of previous year follow-up results of a prospective randomized double-blind placebo-controlled trial in elderly.
PLoS One. Mohr D, Bowry VW, Stocker R. Dietary supplementation with coenzyme Q10 results in increased levels of ubiquinol within circulating lipoproteins and increased resistance of human low-density lipoprotein to the initiation of lipid peroxidation.
Witting PK, Pettersson K, Letters J, Stocker R. Anti-atherogenic effect of coenzyme Q10 in apolipoprotein E gene knockout mice. Thomas SR, Leichtweis SB, Pettersson K, et al. Dietary cosupplementation with vitamin E and coenzyme Q 10 inhibits atherosclerosis in apolipoprotein E gene knockout mice.
Arterioscler Thromb Vasc Biol. Turunen M, Wehlin L, Sjoberg M, et al. beta2-Integrin and lipid modifications indicate a non-antioxidant mechanism for the anti-atherogenic effect of dietary coenzyme Q Biochem Biophys Res Commun.
Rahman S, Clarke CF, Hirano M. Neuromuscul Disord. Gempel K, Topaloglu H, Talim B, et al. The myopathic form of coenzyme Q10 deficiency is caused by mutations in the electron-transferring-flavoprotein dehydrogenase ETFDH gene.
Pineda M, Montero R, Aracil A, et al. Sergi G, Coin A, Marin S, Vianello A, Manzan A, Peruzza S, Inelmen EM, Busetto L, Mulone S, Enzi G: Body composition and resting energy expenditure in elderly male patients with chronic obstructive pulmonary disease. Wagner PD: Possible mechanisms underlying the development of cachexia in COPD.
Eur Respir J. Takabatake N, Nakamura H, Abe S, Hino T, Saito H, Yuki H, Kato S, Tomoike H: Circulating leptin in patients with chronic obstructive pulmonary disease.
Takabatake N, Nakamura H, Minamihaba O, Inage M, Inoue S, Kagaya S, Yamaki M, Tomoike H: A novel pathophysiologic phenomenon in chachexic patients with chronic obstructive pulmonary disease: the relationship between the circadian rhythm of circulating leptin and the very low-frequency component of heart rate variability.
Di Francia M, Barbier D, Mege JL, Orehek J: Tumor necrosis factor-α levels and weight loss in chronic obstructive pulmonary disease. Eid AA, Ionescu AA, Nixon LS, Lewis-Jenkins V, Matthews SB, Griffiths TL, Shale DJ: Inflammatory response and body composition in chronic obstructive pulmonary disease.
Itoh T, Nagaya N, Yoshikawa M, Fukuoka A, Takenaka H, Shimizu Y, Haruta Y, Oya H, Yamagishi M, Hosoda H, Kangawa K, Kimura H: Elevated plasma ghrelin level in underweight patients with chronic obstructive pulmonary disease.
Schols AMWJ, Crutzberg EC, Buurman WA, Campfield LA, Saris WHM, Wouters EFM: Plasma leptin is related to proinflammatory staus and dietary intake in patients with chronic obstructive pulmonary disease.
Antonucci R, Berton E, Huertas P, Laveneziana P, Palange P: Exercise physiology in COPD. Monaldi Arch Chest Dis. Koechlin C, Couillard A, Simar D, Cristol JP, Bellet H, Hayot M, Prefaut C: Does oxidative stress alter quadriceps endurance in chronic obstructive pulmonary disease?. Gosker HR, Lencer NH, Franssen FM, Van der Vusse GJ, Wouters EF, Schols AM: Striking similarities in systemic factors contributing to decreased exercise capacity in patients with severe chronic heart failure or COPD.
Vogiatzis I, Simoes DC, Stratakos G, Kourepini E, Terzia G, Manta P, Athanasopoulos D, Roussos C, Wagner PD, Zakynthinos S: Effect of pulmonary rehabilitation on muscle remodelling in cachectic patients with COPD.
Rutten EP, Franssen FM, Engelen MP, Wouters EF, Deutz NE, Schols AM: Greater whole-body myofibrillar protein breakdown in cachectic patients with chronic obstructive pulmonary disease. Couillard A, Koechlin C, Cristol JP, Varray A, Prefaut C: Evidence of local exercise- induced systemic oxidative stress in chronic obstructive pulmonary disease.
Sahebjami H, Sathianpitayakul E: Influence of body weight on the severity of dyspnea in chronic obstructive pulmonary disease. Naimi AI, Bourbeau J, Perrault H, Baril J, Wright-Paradis C, Rossi A, Taivassalo T, Sheel AW, Rabøl R, Dela F, Boushel R: Altered mitochondrial regulation in quadriceps muscles of patients with COPD.
Clin Physiol Funct Imaging. Puente-Maestu L, Pérez-Parra J, Godoy R, Moreno N, Tejedor A, González-Aragoneses F, Bravo JL, Alvarez FV, Camaño S, Agustí A: Abnormal mitochondrial function in locomotor and respiratory muscles of COPD patients.
Slebos DJ, Van der Toorn M, Bakker SJ, Kauffman HF: Mitochondrial dysfunction in COPD patients with low body mass index. Gosker HR, Hesselink MK, Duimel H, Ward KA, Schols AM: Reduced mitochondrial density in the vastus lateralis muscle of patients with COPD.
Rabinovich RA, Bastos R, Ardite E, Llinàs L, Orozco-Levi M, Gea J, Vilaró J, Barberà JA, Rodríguez-Roisin R, Fernández-Checa JC, Roca J: Mitochondrial dysfunction in COPD patients with low body mass index. Pajen JF, Wuyam B, Levy P, Reutenauer H, Stieglitz P, Paramelle B, Le Bas JF: Muscular metabolism during oxygen supplementation in patients with chronic hypoxemia.
Article Google Scholar. Faager G, Söderlund K, Sköld CM, Rundgren S, Tollbäck A, Jakobsson P: Creatine supplementation and physical training in patients with COPD: a double blind, placebo-controlled study. Int J Chron Obstruct Pulmon Dis. PubMed Central CAS PubMed Google Scholar.
Tanrikulu AC, Abakay A, Evliyaoglu O, Palanci Y: Coenzyme Q10, copper, zinc, and lipid peroxidation levels in serum of patients with chronic obstructive pulmonary disease. Biol Trace Elem Res.
Xu J, Seo AY, Vorobyeva DA, Carter CS, Anton SD, Lezza AM, Leeuwenburgh C: Beneficial effects of a Q-ter based nutritional mixture on functional performance, mitochondrial function, and oxidative stress in rats. PLoS One. Article PubMed Central PubMed Google Scholar. Saremi A, Gharakhanloo R, Sharghi S, Gharaati MR, Larijani B, Omidfar K: Effects of oral creatine and resistance training on serum myostatin and GASP Mol Cell Endocrinol.
G Gerontol. Fumagalli S, Fattirolli F, Guarducci L, Cellai T, Baldasseroni S, Tarantini F, Di Bari M, Masotti G, Marchionni N: Coenzyme Q10 terclatrate and creatine in chronic heart failure: a randomized, placebo controlled, double-blind study.
Clin Cardiol. Fuld JP, Kilduff LP, Neder JA, Pitsiladis Y, Lean MEJ, Ward SA, Cotton MM: Creatine supplementation during pulmonary rehabilitation in chronic obstructive pulmonary disease.
Article PubMed Central CAS PubMed Google Scholar. Bartlett HR, Puhl SM, Hdgson L, Buskirk ER: Fat-free mass in relation to stature: ratios of fat-free mass to height in children, adults end elderly subjects. Katz TF: A. Activities of Daily Living. Statement ATS: Guidelines for the Six-Minute Walk Test.
Jones PW, Quirk FH, Baveystock CM: The St George's Respiratory Questionnaire. Çalıkoglu M, Şahin G, Unlu A, Ozturk C, Tamer L, Ercan B, Kanik A, Atik U: Leptin and TNF-Alpha Levels in Patients with Chronic Obstructive Pulmonary Disease and Their Relationship to Nutritional Parameters.
Alway SE, Swisher A, Siu PM: Increased expression of apoptotic genes in the diaphragm and soleus muscle of the emphysematous hamster.
Faseb J. Bernard S, LeBlanc P, Whittom F, Carrier G, Jobin J, Belleau R, Maltais F: Peripheral muscle weakness in patients with chronic obstructive pulmonary disease. Gosker HR, Kubat B, Schaart G, Van der Vusse GJ, Wouters EF, Schols AM: Myopathological features in skeletal muscle of patients with chronic obstructive pulmonary disease.
Palange P, Forte S, Onorati P, Paravati V, Manfredi F, Serra P, Carlone S: Effect of reduced body weight on muscle aerobic capacity in patients with COPD. Rabinovich RA, Vilaró J: Structural and functional changes of peripheral muscles in chronic obstructive pulmonary disease patients.
Curr Opin Pulm Med. Ribera F, N'Guessan B, Zoll J, Fortin D, Serrurier B, Mettauer B, Bigard X, Ventura-Clapier R, Lampert E: Mitochondrial electron transport chain function is enhanced in inspiratory muscles of patients with chronic obstructive pulmonary disease.
Hamaoka T, Tatsumi K, Saito Y, Arai Y, Horie Y, Masuyama S, Tanabe N, Takiguchi Y, Ikehira H, Obata T, Sasaki Y, Tanada S, Kuriyama T: Metabolic activity in skeletal muscles of patients with non-hypoxaemic chronic obstructive pulmonary disease studied by 31P-magnetic resonance spectroscopy.
Layec G, Haseler LJ, Richardson RS: The effect of higher ATP cost of contraction on the metabolic response to graded exercise in patients with chronic obstructive pulmonary disease.
J Appl Physiol. Picard M, Godin R, Sinnreich M, Baril J, Bourbeau J, Perrault H, Taivassalo T, Burelle Y: The mitochondrial phenotype of peripheral muscle in chronic obstructive pulmonary disease: disuse or dysfunction?.
Creutzberg EC, Wouters EF, Mastert R, Weling-Scheepers CA, Schols AM: Efficacy of nutritional supplementation therapy in depleted patients with chronic obstructive pulmonary disease. Cai BJ, Zhu YY, Ma Y, Xu ZZ, Zao Y, Wang J, Lin Y, Gail M, Comer GM: Effect of supplementing a high-fat, low-carbohydrate enteral formula in COPD patients.
Ferreira IM, Brooks D, Lacasse Y, Goldstein RS, White J: Nutritional supplementation for stable chronic obstructive pulmonary disease.
Cochrane Database Syst Rev. Steinert MC, Barton L, Singh SJ, Morgan MD: Nutritional enhancement of exercise performance in chronic obstructive pulmonary disease: a randomised controlled trial. Engelen MP, Rutten EP, De Castro CL, Wouters EF, Schols AM, Deutz NE: Casein protein results in higher prandial and exercise induced whole body protein anabolism than whey protein in chronic obstructive pulmonary disease.
Engelen MP, De De Castro CL, Rutten EP, Wouters EF, Schols AM, Deutz NE: Enhanced anabolic response to milk protein sip feeding in elderly subjects with COPD is associated with a reduced splanchnic extraction of multiple amino acids.
Clin Nutr. Dal Negro RW, Testa A, Aquilani R, Tognella S, Pasini E, Barbieri A, Boschi F: Essential amino acid supplementation in patients with severe COPD:a step towards home rehabilitation. Baldi S, Aquilani R, Pinna GD, Poggi P, De Martini A, Bruschi C: Fat-free mass change after nutritional rehabilitation in weight losing COPD: role of insulin C-reactive protein and tissue hypoxia.
Int J Chron Obstruct Pulm Dis. Pansarasa O, Flati V, Corsett G, Brocca L: Oral Amino AcidSupplementation Counteracts Age-Induced Sarcopenia in Elderly Rats. Am J Cardiol. Allard ML, Jeejeebhoy KN, Sole MJ: The management of conditioned nutritional requirements in heart failure.
Heart Fail Rev. Witte KK, Clark AL: Micronutrients and their supplementation in chronic cardiac failure: an update beyond theoretical perspectives. Witte KK, Clark AL, Cleland JG: Chronic heart failure and micronutrients.
J Am Coll Cardiol. Belardinelli R, Mucaj A, Lacalaprice F, Solenghi M, Principi F, Tiano L, Littarru GP: Coenzyme Q10 improves contractility of dysfunctional myocardium in chronic heart failure. Belardinelli R, Muc¸Aj A, Lacalaprice F, Solenghi M, Seddaiu G, Principi F, Tiano L, Littarru GP: Coenzyme Q10 and exercise training in chronic heart failure.
Eur Heart J. Molyneux SL, Florkowski CM, George PM, Pilbrow AP, Frampton CM, Lever M, Richards AM: Coenzyme Q an independent predictor of mortality in chronic heart failure. Mortensen SA: Overview on coenzyme Q10 as adjunctive therapy in chronic heart failure.
Fumagalli S, Fattirolli F, Guarducci L, Cellai T, Baldasseroni S, Tarantini F, Di Bari M, Masotti G, Marchionni N: Coenzyme Q10 Terclatrate and Creatine in Chronic Heart Failure: A Randomized, Placebo-Controlled Double-Blind Study. Download references.
Pneumology Department, SS Annunziata Hospital, Chieti, Italy. You can also search for this author in PubMed Google Scholar.
Correspondence to Stefano Marinari. This article is published under license to BioMed Central Ltd. Reprints and permissions.
Marinari, S. Effects of nutraceutical diet integration, with coenzyme Q 10 Q-Ter multicomposite and creatine, on dyspnea, exercise tolerance, and quality of life in COPD patients with chronic respiratory failure. Multidiscip Respir Med 8 , 40 Download citation.
Received : 13 March Accepted : 06 June Published : 21 June Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background The protein-calorie malnutrition, resulting in muscle mass loss, frequently occurs in severe COPD patients with chronic respiratory failure CRF , causing dyspnea, reduced exercise tolerance and impaired quality of life.
Results No significant difference was detected at baseline T0 in the 2 groups. Conclusions The nutraceutical diet integration with Q-Ter and creatine, in COPD patients with CRF in O 2 TLT induced an increasing lean body mass and exercise tolerance, reducing dyspnea, quality of life and exacerbations.
Curr Neurovasc Res. de Bustos F, Molina JA, Jimenez-Jimenz FJ, Garcia-Redondo A, Gomez-Escalonilla C, Porta-Etessam J, et al. Serum levels of coenzyme Q10 in patients with Alzheimer's disease.
J Neural Transm. Heck AM, DeWitt BA, Lukes AL. Potential interactions between alternative therapies and warfarin. Am J Health-System Pharm. Hodgson JM, Watts GF, Playford DA, et al. Coenzyme Q 10 improves blood pressure and glycaemic control: a controlled trial in subjects with type 2 diabetes.
Eur J Clin Nutr. Khan M, Gross J, Haupt H, et al. Otolaryngol Head Neck Surg. Khatta M, Alexander BS, Krichten CM, Fisher ML, Freudenberger R, Robinson SW et al.
The effect of conenzyme Q10 in patients with congestive heart failure. Ann Int Med. Kolahdouz Mohammadi R, Hosseinzadeh-Attar MJ, Eshraghian MR, Nakhjavani M, Khorami E, Esteghamati A.
The effect of coenzyme Q10 supplementation on metabolic status of type 2 diabetic patients. Minerva Gastroenterol Dietol. Lafuente R, Gonzalez-Comadran M, Sola I, et al. Conezyme Q10 and male infertility: a meta-analysis.
J Assist Reprod Genet. Langsjoen PH, Langsjoen JO, Langsjoen AM, Lucas LA. Treatment of statin adverse effects with supplemental Coenzyme Q10 and statin drug discontinuation.
Lee BJ, Tseng YF, Yen CH, Lin PT. Nutr J. Levy G, Kaufmann P, Buchsbaum R, et al. Madmani ME, Yusuf Solaiman A, Tamr Agha K, et al.
Coenzyme Q10 for heart failure. Cochrane Database Syst Rev. McCarty MF. Toward practical prevention of type 2 diabetes. Med Hypotheses.
Nahas R. Complementary and alternative medicine approaches to blood pressure reduction: An evidence-based review. Can Fam Physician. Ochiai A, Itagaki S, Kurokawa T, Kobayashi M, Hirano T, Iseki K.
Improvement in intestinal coenzyme q10 absorption by food intake. Yakugaku Zasshi. Ostrowski RP. Effect of coenzyme Q 10 on biochemical and morphological changes in experimental ischemia in the rat brain. Brain Res Bull.
Palan PR, Connell K, Ramirez E, Inegbenijie C, Gavara RY, Ouseph JA, Mikhail MS. Effects of menopause and hormone replacement therapy on serum levels of coenzyme Q10 and other lipid-soluble antioxidants.
Quinzii CM, Dimauro S, Hirano M. Human coenzyme q 10 deficiency. Neurochem Res. Raitakari OT, McCredie RJ, Witting P, Griffiths KA, Letter J, Sullivan D, Stocker R, Celermajer DS.
Coenzyme Q improves LDL resistance to ex vivo oxidation but does not enhance endothelial function in hypercholesterolemic young adults.
Free Radic Biol Med. Rakel D. Rakel: Integrative Medicine. Philadelphia, PA: Elsevier Saunders; Rosenfeldt FL, Haas SJ, Krum H, Hadj A, Ng K, Leong JY, Watts GF. Conenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials.
J Hum Hypertens. Rosenfeldt F, Hilton D, Pepe S, Krum H. Systematic review of effect of coenzyme Q10 in physical exercise, hypertension and heart failure. Salles JE, Moises VA, Almeida DR, Chacra AR, Moises RS.
Myocardial dysfunction in mitochondrial diabetes treated with Coenzyme Q Diabetes Res Clin Pract. Sander S, Coleman CI, Patel AA, Kluger J, White CM. The impact of coenzyme Q10 on systolic function in patients with chronic heart failure. J Card Fail.
This cancer information summary provides an oCenzyme of the Coenyme of coenzyme Q 10 in cancer Coenzme. The lug includes Improve information processing history of coenzyme Coenzyme Q and lung health 10 research, a review of laboratory studiesand data from Lubg involving Enhance workout power subjects. Although several naturally occurring forms of coenzyme Q have been identified, Q 10 is the predominant form found in humans and most mammals, and it is the form most studied for therapeutic potential. Thus, it will be the only form of coenzyme Q discussed in this summary. Many of the medical and scientific terms used in the summary are hypertext linked at first use in each section to the NCI Dictionary of Cancer Termswhich is oriented toward nonexperts. CoQ10 ,ung help hfalth the skin, brain, and Coenzyme Q and lung health, as Enhance workout power Skinfold measurement in nutrition studies protect against chronic diseases like cancer or diabetes. Adn research is needed to understand its benefits, Codnzyme. Coenzyme Q10 Hhealth is a compound that helps generate energy in your cells. With age, your body produces less of it, but you can also get it from supplements or food. Low levels of CoQ10 may be associated with diseases like cancer, diabetes, as well as neurodegenerative disorders. That said, the cause-effect relationship is unclear. CoQ10 is naturally found in the body, with the highest levels in the heart, liver, kidney, and pancreas.
Sie lassen den Fehler zu. Schreiben Sie mir in PM, wir werden umgehen.
Ich denke, dass es die gute Idee ist.