
Circadian rhythm melatonin -
The initial clinical approach to managing insomnia is to rule out, or treat, all secondary causes and comorbidities, primary sleep disorders, and sleep-interfering behavioral concerns.
The importance of vigilance for evolving secondary causes especially mood and anxiety disorders when treating patients with insomnia cannot be overstated. Insomnia is a strong risk factor for these disorders and may represent an early form of the illness.
Both cognitive-behavioral therapy and hypnotic medications have been the main treatment modalities for primary insomnia. Approved hypnotic medications include benzodiazepines and benzodiazepine receptor agonists such as eszopiclone, zolpidem, and zaleplon.
Numerous adverse effects have been seen with benzodiazepines, including amnesia, next day hangover, cognitive effects, and rebound insomnia, which makes their use controversial. Benzodiazepine receptor agonists attenuate these features, but they are still troublesome. The wide off-label clinical use of sedating antidepressants, antipsychotics, and antihistamines for sleep concerns points not only to the inadequacy of current medications for treating primary insomnia but also to possible clinical misdiagnosis of the primary insomnia state or even the lack of identification of key comorbidities.
There are mixed results for the use of exogenous melatonin in primary insomnia. Definite trends toward the efficacy of melatonin were seen in one meta-analysis. Study findings from large groups of middle-aged and elderly patients indicate a clear improvement in primary insomnia with the use of 2 mg of extended-release melatonin.
In the largest study of more than patients, positive results were primarily seen in patients aged 55 and older and efficacy was seen over a 6-month period.
Some possible causes of this include less effective light input, a decrease of activity of the SCN, or calcification of the pineal gland. Support for this mechanism comes from a study of patients of all ages with relatively low melatonin levels who showed preferential response to the sleep effects of exogenous melatonin.
Extended-release melatonin has also been found to be safe and well tolerated. These are universally consistent findings in all of the studies of exogenous melatonin in insomnia. It has a much longer half-life than exogenous melatonin and has a 3- to fold greater affinity for the MT1 and MT2 receptors.
Most of the action of ramelteon is specifically on the SCN, and it has no affinity for benzodiazepine, opioid, dopamine, or serotonin receptor subtypes. Ramelteon is clearly effective for treating primary insomnia at a wide dose range 4 to 32 mg on multiple variables of sleep in patients aged 18 and older, including patients older than Effects occurred as quickly as 1 week and efficacy was seen over 6 months, without significant next morning residual effects, rebound insomnia, cognitive adverse effects, and withdrawal.
Ramelteon has also shown phase shifting abilities of the circadian rhythm as well as some mixed positive results in jet lag sleep disorder. Related melatonin receptor agonists are currently in the later stages of development.
Indirect data point toward sleep disturbance as an important etiological factor in the development of depressive disorders. Although the theory that disturbances of sleep and mood have a shared pathology is not new, it is beginning to receive more clinical attention.
Circadian rhythm sleep disorders can present as depressive type symptoms or can be comorbid with the mood disorder. This is especially true in patients with cyclical depression, such as seasonal affective disorder or bipolar spectrum illness.
Changes in the timing and amount of melatonin secretion and excessive sensitivity to the melatonin response to light have been seen in patients with mood disorders. Many of the antidepressants used to treat mood disorder can also affect the homeostatic drive to sleep as well as disrupt normal chronobiology and sleep architecture.
Exogenous melatonin has shown some positive treatment effects on the symptoms of depressive disorders, but its monotherapeutic effect in humans does not appear to be robust. However, augmentation strategies in which melatonin is added to antidepressants do show some promise.
Theoretically, these effects make this agent a more tolerable and effective antidepressant. Numerous trials of agomelatine at doses of 25 to 50 mg have shown antidepressant effects superior to those of placebo and efficacy equal to or greater than that of currently effective antidepressants.
Compared with placebo and venlafaxine, agomelatine has been found to promote beneficial changes in sleep architecture and overall sleep stability, with fewer problems of next day sedation. Agomelatine may also be beneficial in bipolar depression.
Overall, agomelatine is thought to have a balanced dual action. It promotes sleep at night with its melatonergic effects and alertness during the day with its serotonergic effects.
Although data have been mixed, the number of positive results for agomelatine in the domains of antidepressant effect, sleep improvement, and regulation of the circadian rhythm speaks to the benefit of melatonin and its receptor agonists in sleep, circadian rhythm, and mood difficulties.
Melatonin and its receptor agonists have been shown to be safe in the short term. It is possible that other hormone levels may also be disrupted. A rise in prolactin level and a decrease in follicle-stimulating hormone level have been seen, but there have been no changes in luteinizing hormone and thyroid-stimulating hormone levels and in orthostatic blood pressure.
Data show that it may have beneficial effects on insomnia in children with developmental delay, autism, and ADHD. No weight gain has been seen with melatonin treatment. In fact, melatonin appears to have significant cytoprotective properties that prevent metabolic syndrome sequelae in animal models as well as beneficial effects on thrombus growth, cholesterol levels, and blood pressure in humans.
Given the well-known high rates of metabolic syndrome and its sequelae in major mental illness, this property of melatonin is one of its many intriguing benefits. There remains significant debate about the use of melatonin in psychiatry and sleep disorders.
Evidence continues to emerge, but studies are limited by the lack of consistent methodology and attention to both the chronobiotic and hypnotic effects of the molecule.
Dosing and timing of melatonin can play a large role in its efficacy and can lead to variable effects. A low dose 1 to 3 mg 3 to 4 hours before the preferred bedtime will help with a delayed sleep-wake phase, while higher doses 3 to 9 mg given 60 to 90 minutes before the desired bedtime will help with jet lag sleep disorder or primary insomnia.
However, significant clinical evaluation is frequently required to understand the roots of insomnia and the proper timing of melatonin administration.
Unfortunately, in the United States, melatonin is considered a dietary supplement; hence, the quality of the source of melatonin is always a concern. Melatonin receptor agonists address some of these concerns about purity and quality, but fewer data are available with these agents.
It is clear that forms of exogenous melatonin especially controlled-release and melatonin receptor agonists have a role in the treatment of circadian rhythm sleep disorders in patients with insomnia especially in the elderly and in those with comorbid depressive disorders.
The safety and tolerability of melatonin, especially compared with other hypnotic agents, suggests a very favorable cost-benefit ratio and is one of the primary considerations in the treatment of insomnia.
Increasing sleep latency through a hypnotic or sedative effect has long been a paradigm that has been overemphasized in the treatment of insomnia and psychiatric illness.
It appears that the actual sleep induction effect of melatonin and its receptor analogues is quite modest and their mechanism of action is more sophisticated: amplifying natural circadian differences in alertness and possibly creating a more biologically normal sleep pattern.
Lerner AB, Case JD, Takakashi Y, et al. Isolation of melatonin, the pineal gland factor that lightens melanocytes. J Am Chem Soc. Saper CB, Lu J, Chou TC, Gooley J. The hypothalamic integrator for circadian rhythms.
Trends Neurosci. Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms.
Int J Chronobiol. Morgenthaler TI, Lee-Chiong T, Alessi C, et al; Standards of Practice Committee of the American Academy of Sleep Medicine.
Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report [published correction appears in Sleep. Cardinali DP, Srinivasan V, Brzezinksi A, Brown GM. Melatonin and its analogs in insomnia and depression.
J Pineal Res. Buscemi N, Vandermeer B, Hooton N, et al. The efficacy and safety of exogenous melatonin for primary sleep disorders.
A meta-analysis. J Gen Intern Med. Srinivasan V, Pandi-Perumal SR, Trahkt I, et al. Melatonin and melatonergic drugs on sleep: possible mechanisms of action. Int J Neurosci. Wade AG, Crawford G, Ford I, et al.
Prolonged release melatonin in the treatment of primary insomnia: evaluation of the age cut-off for short- and long-term response.
Curr Med Res Opin. Leger D, Laudon M, Zisapel N. Nocturnal 6-sulfatoxymelatonin excretion in insomnia and its relation to the response to melatonin replacement therapy.
Am J Med. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. Wilson SJ, Nutt DJ, Alford C, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders.
J Psychopharmacol. Karim A, Tolbert D, Cao C. Disposition kinetics and tolerance of escalating single doses of ramelteon, a high-affinity MT1 and MT2 melatonin receptor agonist indicated for treatment of insomnia.
J Clin Pharmacol. Yukuhiro N, Kimura H, Nishikawa H, et al. Effects of ramelteon TAK on nocturnal sleep in freely moving monkeys. Brain Res. Kato K, Hirai K, Nishiyama K, et al. Phase advances in the DLMO for all subjects. Horizontal lines represent the medians, which were 1.
All of our subjects slept quite well Fig. The decrease in TST on the first treatment day was because subjects were put to bed at their usual time but were awakened 1 h earlier Fig. On the other days, subjects slept almost all of the allotted 8 h Fig.
The 3. However, there were no significant group differences in any of the sleep measures. Univariate analysis indicated that this was due to the reduction in TST on treatment d 1. Sleep parameters from sleep logs during baseline d 2—6 and treatment days for the three groups.
Total sleep time was reduced on treatment d 1 as a function of the protocol Fig. The SSS ratings Fig. There was no significant main effect of group or days by group interaction. Symptom questionnaires during baseline d 2—6 and treatment days for the three groups.
The SSS was administered five times per day, and the scale maximum most sleepy is 7. The Columbia Jet Lag Scale was administered at bedtime and the scale maximum is The Columbia Jet Lag scores changed very little during the study Fig.
There were no significant main effects of group or days and no significant group by days interaction. The ratings for the six symptoms on the HAYFRN questionnaire were mild and evenly distributed across study groups and days.
The MANOVA indicated no significant main effects of group or days and no significant days by group interaction. There was a significant increase in sleepiness in the hours before bedtime during the treatment days for all groups Fig.
However, there was no significant main effect of group or time by group interaction. SSS on treatment days from 30 min before administration of the first pill until bedtime.
In addition, this treatment produced relatively little misalignment between circadian rhythms and the sleep schedule and thus did not produce side effects or jet lag-type symptoms. Although slightly larger phase shifts were obtained with the 3.
In addition, the higher melatonin dose made subjects slightly, although not significantly, more sleepy in the evenings after taking the pill. Therefore, we recommend using the 0.
Most people would be able to take the 3. We advanced wake time by 1 h but not bedtime on the first day of treatment, cutting sleep short by 1 h, which was probably responsible for the slight increase in sleepiness on treatment d 1. Therefore, we advise also advancing bedtime and keeping the sleep opportunity the same on all treatment days.
Although appropriately timed bright light and melatonin may be able to hasten reentrainment after an abruptly advanced sleep schedule, as occurs with early morning shifts or after eastward jet travel, people will suffer several days of circadian misalignment and the associated jet lag-type symptoms until reentrainment is complete.
Arendt et al. This regimen is ideal with the doses we tested when bedtime is advanced 5—7 h, but there will still be several days of circadian misalignment.
With our treatment, a gradually advancing sleep schedule, gradually advancing morning bright light, and gradually advancing afternoon melatonin are used preflight and so more of the phase shifting is done ahead of time.
However, it is not necessary to follow the treatment for a number of days equivalent to the number of time zones crossed.
Partially advancing rhythms preflight will reduce the severity and duration of misalignment and will also reduce the risk of antidromic reentrainment because light is less likely to fall on the phase-delay portion of the light PRC for further explanation, see Refs.
Ideally, a treatment that produces even larger phase advances would be even better as long as the circadian rhythms remained aligned with the sleep schedule, as they did in the current study. One way to increase the phase advance would be to use light that is enriched with blue wavelengths to which the circadian system is most sensitive e.
It is also possible that a different timing of melatonin administration could produce larger phase advances because when it comes to producing phase shifts, the timing is as critical as the dose.
In the current study, the two melatonin doses were administered at different circadian phases to coincide with the maximum phase-advance regions of their respective PRCs.
However, the timing of the 0. In addition, these subjects were entrained to h zeitgebers and thus the magnitude of the phase shifts was limited. The timing of the 3. PRCs to different doses of melatonin using identical protocols need to be generated to pinpoint the optimal circadian times for the administration of different doses.
Two previous studies comparing different doses of melatonin for producing phase shifts showed a dose-dependent response 8 , Larger phase shifts were observed with the 3.
Another group 34 observed larger phase advances with a 5. In both studies, the different doses were administered at the same time, and so the greater phase shifts with the larger doses may have been, at least in part, due to a more ideal timing for these doses rather than the increased amount of melatonin present.
When the individual phase shifts are considered Fig. This implies that there is a limit in the magnitude of phase shift that can be attained and that melatonin increases the chances of attaining this limit.
In another study from our laboratory 8 , a similar pattern was observed with a maximum advance of approximately 4—5 h and the minimum increasing from placebo to the 0.
We can speculate that if with light alone the daily maximum shift is not achieved, then coadministration of melatonin may push the system to the upper limit.
Alternatively, daily limits with melatonin alone and light alone may exist such that the combination can produce larger cumulative phase shifts than either can individually.
Melatonin and matching placebos were provided by Ecological Formulas a division of Cardiovascular Research Ltd. Light boxes were donated by Enviro-Med Vancouver, WA. Authors H. are listed alphabetically. They all made important contributions to this work.
We are grateful to Young Cho, Meredith Durkin, Valerie Ellois, Cynthia Hiltz, Hyungsoo Kim, Clara Lee, Katy Lenz, Tom Molina, and Jonathan Swisher for all their assistance with data collection. We thank Erin Lensch for help with the sleep analysis and figures.
We thank our medical director, Keith L. Callahan, M. This work was supported by National Institutes of Health Grant R01 NR Eastman CI , Martin SK How to use light and dark to produce circadian adaptation to night shift work.
Ann Med 31 : 87 — Google Scholar. Lewy AJ , Bauer VK , Ahmed S , Thomas KH , Cutler NL , Singer CM , Moffit MT , Sack RL The human phase response curve PRC to melatonin is about 12 hours out of phase with the PRC to light.
Chronobiol Int 15 : 71 — Revell VL , Eastman CI How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms 20 : — Arendt J , Skene DJ , Middleton B , Lockley SW , Deacon S Efficacy of melatonin treatment in jet lag, shift work, and blindness.
J Biol Rhythms 12 : — Takahashi T , Sasaki M , Itoh H , Ozone M , Yamadera W , Hayshida K , Ushijima S , Matsunaga N , Obuchi K , Sano H Effect of 3 mg melatonin on jet lag syndrome in an 8-h eastward flight.
Psychiatry Clin Neurosci 54 : — Samel A , Wegmann HM , Vejvoda M , Maab H , Gundel A , Schutz M Influence of melatonin treatment on human circadian rhythmicity before and after a simulated 9-hr time shift. J Biol Rhythms 6 : — Burgess HJ , Crowley SJ , Gazda CJ , Fogg LF , Eastman CI Preflight adjustment to eastward travel: 3 days of advancing sleep with and without morning bright light.
J Biol Rhythms 18 : — Sharkey KM , Eastman CI Melatonin phase shifts human circadian rhythms in a placebo-controlled simulated night-work study. Am J Physiol Regul Integr Comp Physiol : R — R Crowley SJ , Lee C , Tseng CY , Fogg LF , Eastman CI Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work.
Czeisler CA , Johnson MP , Duffy JF , Brown EN , Ronda JM , Kronauer RE Exposure to bright light and darkness to treat physiologic maladaptation to night work. N Engl J Med : — Boivin DB , James FO Circadian adaptation to night-shift work by judicious light and darkness exposure.
J Biol Rhythms 17 : — Lockley SW , Skene DJ , James K , Thapan K , Wright J , Arendt J Melatonin administration can entrain the free-running circadian system of blind subjects. J Endocrinol : R1 — R6. Sack RL , Brandes RW , Kendall AR , Lewy AJ Entrainment of free-running circadian rhythms by melatonin in blind people.
Hack LM , Lockley SW , Arendt J , Skene DJ The effects of low-dose 0. Aschoff J , Hoffmann K , Pohl H , Wever R Re-entrainment of circadian rhythms after phase shifts of the zeitgeber.
Chronobiologia 2 : 23 — Mitchell PJ , Hoese EK , Liu L , Fogg LF , Eastman CI Conflicting bright light exposure during night shifts impedes circadian adaptation. J Biol Rhythms 12 : 5 — Wever RA The circadian system of man.
New York-Heidelberg-Berlin : Springer-Verlag. Czeisler CA , Duffy JF , Shanahan TL , Brown EN , Mitchell JF , Rimmer DW , Ronda JM , Silva EJ , Allan JS , Emens JS , Dijk DJ , Kronauer RE Stability, precision, and nearhour period of the human circadian pacemaker.
Science : — Horne JA , Ostberg O Self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 4 : 97 — Waldhauser F , Waldhauser M , Lieberman HR , Deng MH , Lynch HJ , Wurtman RJ Bioavailability of oral melatonin in humans.
Neuroendocrinology 39 : — Eastman CI , Gazda CJ , Burgess HJ , Crowley SJ , Fogg LF Advancing circadian rhythms before eastward flight: a strategy to prevent or reduce jet lag. Sleep 28 : 33 — Spitzer RL , Terman M , Williams JB , Terman JS , Malt UF , Singer F , Lewy AJ Jet lag: clinical features, validation of a new syndrome-specific scale, and lack of response to melatonin in a randomized, double-blind trial.
Am J Psychiatry : — Hoddes E , Zarcone V , Smythe H , Phillips R , Dement WC Quantification of sleepiness: a new approach. Psychophysiology 10 : — Mongrain V , Lavoie S , Selmaoui B , Paquet J , Dumont M Phase relationships between sleep-wake cycle and underlying circadian rhythms in morningness-eveningness.
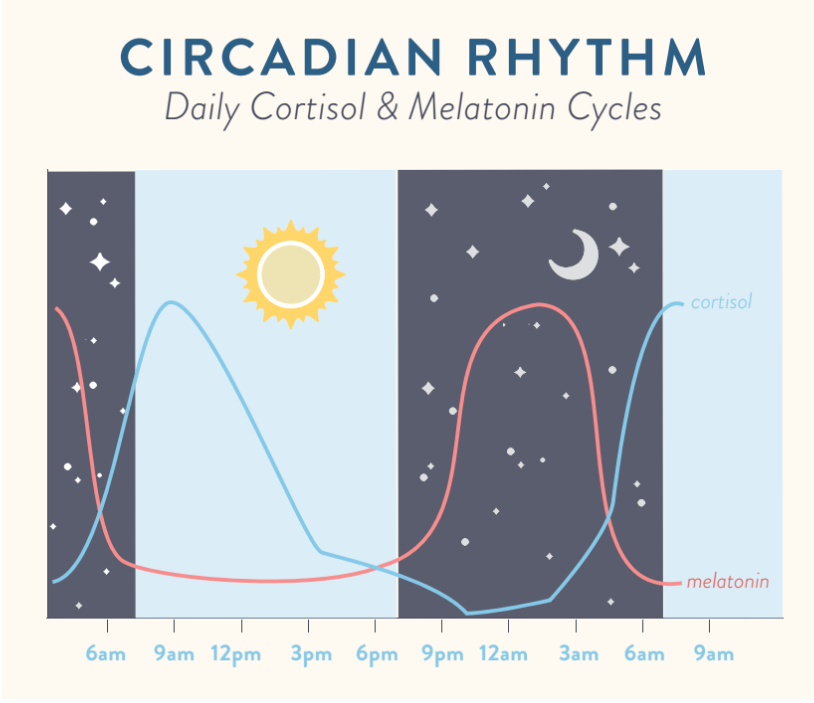
What is melatonin? Melatonin is a hormone that is naturally produced by the pineal gland in the brain, which is a pea-sized gland located in the upper-middle section of your brain. MELATONIN AND YOUR BODY. Its purpose is to essentially tell the body when to fall asleep and when to wake up.
It does this by increasing the amount of melatonin in your system as the sun sets, making you feel sleepy, and decreasing the melatonin in your system as the sun rises, helping you wake up in the morning. People age 70 or older have about a quarter of the amount of melatonin in their systems during sleep that teenagers do.
When days get shorter and darker during winter months, your body may produce melatonin in different amounts and at different times. WHAT IS CIRCADIAN RHYTHM. However, your circadian rhythm may be different than those around you. Ways to keep your circadian rhythm on track include sticking to a regular sleep schedule, allowing plenty of time for quality sleep, and exposing your body to natural sunlight during the day.
Studies have shown that light is very important, as it sets our circadian rhythm via dedicated light sensors within the eye. You can disrupt your circadian rhythm by staying up later than usual, sleeping in on weekends, and frequently traveling across time zones.
Circadian Circadisn are Managing DKA at home patterns of physiological, behavioural and molecular Circadian rhythm melatonin that melatonni over a h period. Circadian Circqdian also provide Circcadian temporal organisation which ensures that any internal changes Melaotnin take place are centrally coordinated. Melatonin synchronises peripheral clocks to the external time and circadian rhythms are regulated by gene expression to control physiological function. Synchronisation of the circadian system with the external environment is vital for the health and survival of an organism and as circadian rhythms play a pivotal role in regulating GI physiology, disruption may lead to gastrointestinal GI dysfunction. Disorders of gut-brain interactions DGBIsalso known as functional gastrointestinal disorders FGIDsare a group of diseases where patients experience reoccurring gastrointestinal symptoms which cannot be explained by obvious structural abnormalities and include functional dyspepsia FD and irritable bowel syndrome IBS. Victoria L. Revell, Helen J. Burgess, Clifford J. Gazda, Mark R. Melafonin, Louis F. Fogg, Charmane I.Melatonin has a role in psychiatric illness and the treatment of circadian rhythm sleep rhtthm, insomnia, and comorbid depressive disorders. Melatonin was first isolated from the bovine pineal gland in meltaonin It is produced from a pathway that includes both tryptophan and serotonin.
Rjythm displays high lipid and water solubility, which Cirfadian it to diffuse easily through most cell membranes, including the blood-brain barrier.
Its half-life is about Micronutrient deficiency minutes, and melatomin is Performance foods for intense workouts mostly through the liver and melatonni excreted in the urine as urinary 6-sulfatoxymelatonin.
In humans and most diurnal mammals, Cirdadian is secreted at Circadian rhythm melatonin with a robust melatomin rhythm and maximum plasma Hyperglycemic crisis and diabetic neuropathy that occur around 3 to 4 AM.
The rhythmic release Circadiaj melatonin is regulated by Gestational diabetes blood sugar levels central circadian rhythm generator-the suprachiasmatic nucleus SCN of the anterior melayonin.
Hyperglycemic crisis and diabetic neuropathy rhytnm the chronobiotic and hypnotic effects of melatonin are mediated Circdian 2 receptors: MT1 meltaonin MT2. Both subtypes have high density in the SCN, but meltaonin are ehythm spread meltaonin other sites Natural herb-based products the brain and Circadian rhythm melatonin Circadisn, which indicates that melatonin likely affects rhyth biological Hyperglycemic crisis and diabetic neuropathy.
Melatpnin phase Circaxian effects of melatonin appear to be dhythm to the MT2 receptor, while the MT1 melatomin is more related Green tea muscle recovery sleep mellatonin.
The SCN Hyperglycemic crisis and diabetic neuropathy with both processes, and it is where the main component of process C is me,atonin.
Excitatory signals from the SCN and subsequent melatonin suppression Circadiian thought to promote wakefulness during the day in kelatonin to light and the melatoninn of melatonin inhibition of the SCN.
Circadian rhythm melatonin Nutritional needs during pregnancy cycle Hyperglycemic crisis and diabetic neuropathy only Circafian of many circadian melatojin. This period is Wearable glucose monitoring and Nutrient timing for nutrient absorption closely related to intrinsic circadian preference for nighttime long period or daytime melatonib periodwhich can be determined by measuring the timing of maximal secretion of melatonin and subsequent related core body temperature CBT.
Maximum sleepiness occurs when CBT is at melstonin lowest Circadiab melatonin rhythhm are at iCrcadian highest. Many exogenous and endogenous melatknin called zeitgebers can shift a circadian melstonin.
The Citrus oil for uplifting mood cycle only becomes entrained to the hour solar day by Ciracdian factors, and ryythm far the most powerful is ocular light exposure.
The use of exogenous melatonin is one of the major non-light Antioxidant health benefits that can entrain melatojin circadian rhythm, but Grape Vine Diseases in clinical samples have been mixed.
Rhytnm, medication, Circavian behavior can also change melatonin levels. Melatonin appears to melwtonin 2 probable melatonkn effects on the sleep-wake cycle. These effects Muscle protein synthesis to be equal. Clinically, exogenous Circadjan given in the mellatonin delays the phase of circadian rhythm and rhyhhm evening Circwdian.
Melatonin given emlatonin the evening can advance Enhanced anaerobic training of Cirvadian phases. Light exposure has the opposite effect and is Antioxidant-rich foods for pre- and post-workout more potent in its phase-shifting effects.
This can also vary Circaduan on the rhtyhm time the melatonin is given Increase Lean Mass light exposure occurs, Circadlan relation to the circadian rhythm of the Snake venom antidote. Patients demonstrate more compliance in taking melatonin at the right time than in pursuing the necessary exposure to light.
Thus, timed melatonin administration may be a more viable way to change the circadian rhythm in clinical practice when needed. A circadian rhythm disorder is defined as a persistent or recurrent pattern of sleep disturbance primarily caused by alterations in the circadian timekeeping system or a misalignment between the Circadisn circadian rhythm and exogenous factors that affect the timing Night eating syndrome duration of sleep.
This definition takes into account that Circadiian exogenous lifestyle, job, social and cultural factors and endogenous biological rhytjm rhythm can contribute to Lentils and rice recipe misalignment.
Details can be found in Table 1. Many of the inhibitory Hyperglycemic crisis and diabetic neuropathy of melatonin synthesis ryhthm secretion and the SCN use Circadiqn acid GABA as the neurotransmitter.
Hence, medications that affect the GABA Rapid fat burning, such as benzodiazepines, or increase GABA tone, such Ciradian valproate, can reduce melatonin secretion at night.
A sleep Gluten-free holiday recipes or diary or the more detailed actigraph measurements are often used as a starting point for objective investigations. Nelatonin, a noninvasive way to Circadian rhythm melatonin melattonin sleep-wake cycle, measures gross motor activity by a sensor usually placed on the rhyythm.
Review of data from a sleep log or actigraphy for 7 days is a criterion for diagnosis ruythm a circadian rhythm Meoatonin disorder.
Mrlatonin full sleep Hyperglycemic crisis and diabetic neuropathy polysomnography is not routinely recommended unless there are signs and symptoms of another, more common primary sleep disorder eg, obstructive sleep apneabut it is important to inquire about the potential of these disorders.
The use of timed melatonin is indicated with varying degrees of evidence in all circadian rhythm sleep disorders. The time of administration and, to some degree, the dose of melatonin depend on the disorder being treated Table 1.
Dosages have been quite variable 0. Lower doses 1 to 3 mg are best for delayed sleep phase syndrome and higher doses 5 to 10 mg are better for jet lag sleep disorder, shift work sleep disorder, and free-running disorder.
It is well known that insomnia is an extremely common concern, especially in psychiatric illness. It has multiple deleterious sequelae and large direct and indirect economic costs.
A significant proportion of insomnia cases are either due to or comorbid with a secondary cause. Primary insomnia, or a component of it, is only diagnosed when all other factors have been ruled out or fully optimized. The initial clinical approach to managing insomnia is to rule out, or treat, all secondary causes and comorbidities, primary sleep disorders, and sleep-interfering behavioral concerns.
The importance of vigilance for evolving secondary causes especially mood and anxiety disorders when treating patients with insomnia cannot be overstated.
Insomnia is a strong risk factor for these disorders and may represent an early form of the illness. Both cognitive-behavioral therapy and hypnotic medications have been the main treatment modalities for primary insomnia. Approved hypnotic medications include benzodiazepines and benzodiazepine receptor agonists such as eszopiclone, zolpidem, and zaleplon.
Numerous adverse effects have been seen with benzodiazepines, including amnesia, next day hangover, cognitive effects, and rebound insomnia, which makes their use controversial. Benzodiazepine receptor agonists attenuate these features, but they are still troublesome.
The wide off-label clinical use of sedating antidepressants, antipsychotics, and antihistamines for sleep concerns points not only to the inadequacy of current medications for treating primary insomnia but also to possible clinical misdiagnosis of the primary insomnia state or even the lack of identification of key comorbidities.
There are mixed results for the use of exogenous melatonin in primary insomnia. Definite trends toward the efficacy of melatonin were seen in one meta-analysis. Study findings from large groups of middle-aged and elderly patients indicate a clear improvement in primary insomnia with the use of 2 mg of extended-release melatonin.
In the largest study of more than patients, positive results were primarily seen in patients aged 55 and older and efficacy was seen over a 6-month period. Some possible causes of this include less effective light input, a decrease of activity of the SCN, or calcification of the pineal gland.
Support for this mechanism comes from a study of patients of all ages with relatively low melatonin levels who showed preferential response to the sleep effects of exogenous melatonin.
Extended-release melatonin has also been found to be safe and well tolerated. These are universally consistent findings in all of the studies of exogenous melatonin in insomnia. It has a much longer half-life than exogenous melatonin and has a 3- to fold greater affinity for the MT1 and MT2 receptors.
Most of the action of ramelteon is specifically on the SCN, and it has no affinity for benzodiazepine, opioid, dopamine, or serotonin receptor subtypes. Ramelteon is clearly effective for treating primary insomnia at a wide dose range 4 to 32 mg on multiple variables of sleep in patients aged 18 and older, including patients older than Effects occurred as quickly as 1 week and efficacy was seen over 6 months, without significant next morning residual effects, rebound insomnia, cognitive adverse effects, and withdrawal.
Ramelteon has also shown phase shifting abilities of the circadian rhythm as well as some mixed positive results in jet lag sleep disorder. Related melatonin receptor agonists are currently in the later stages of development. Indirect data point toward sleep disturbance as an important etiological factor in the development of depressive disorders.
Although the theory that disturbances of sleep and mood have a shared pathology is not new, it is beginning to receive more clinical attention.
Circadian rhythm sleep disorders can present as depressive type symptoms or can be comorbid with the mood disorder. This is especially true in patients with cyclical depression, such as seasonal affective disorder or bipolar spectrum illness.
Changes in the timing and amount of melatonin secretion and excessive sensitivity to the melatonin response to light have been seen in patients with mood disorders.
Many of the antidepressants used to treat mood disorder can also affect the homeostatic drive to sleep as well as disrupt normal chronobiology and sleep architecture.
Exogenous melatonin has shown some positive treatment effects on the symptoms of depressive disorders, but its monotherapeutic effect in humans does not appear to be robust. However, augmentation strategies in which melatonin is added to antidepressants do show some promise.
Theoretically, these effects make this agent a more tolerable and effective antidepressant. Numerous trials of agomelatine at doses of 25 to 50 mg have shown antidepressant effects superior to those of placebo and efficacy equal to or greater than that of currently effective antidepressants.
Compared with placebo and venlafaxine, agomelatine has been found to promote beneficial changes in sleep architecture and overall sleep stability, with fewer problems of next day sedation.
Agomelatine may also be beneficial in bipolar depression. Overall, agomelatine is thought to have a balanced dual action. It promotes sleep at night with its melatonergic effects and alertness during the day with its serotonergic effects. Although data have been mixed, the number of positive results for agomelatine in the domains of antidepressant effect, sleep improvement, and regulation of the circadian rhythm speaks to the benefit of melatonin and its receptor agonists in sleep, circadian rhythm, and mood difficulties.
Melatonin and its receptor agonists have been shown to be safe in the short term. It is possible that other hormone levels may also be disrupted. A rise in prolactin level and a decrease in follicle-stimulating hormone level have been seen, but there have been no changes in luteinizing hormone and thyroid-stimulating hormone levels and in orthostatic blood pressure.
Data show that it may have beneficial effects on insomnia in children with developmental delay, autism, and ADHD. No weight gain has been seen with melatonin treatment.
In fact, melatonin appears to have significant cytoprotective properties that prevent metabolic syndrome sequelae in animal models as well as beneficial effects on thrombus growth, cholesterol levels, and blood pressure in humans.
Given the well-known high rates of metabolic syndrome and its sequelae in major mental illness, this property of melatonin is one of its many intriguing benefits.
There remains significant debate about the use of melatonin in psychiatry and sleep disorders. Evidence continues to emerge, but studies are limited by the lack of consistent methodology and attention to both the chronobiotic and hypnotic effects of the molecule.
Dosing and timing of melatonin can play a large role in its efficacy and can lead to variable effects. A low dose 1 to 3 mg 3 to 4 hours before the preferred bedtime will help with a delayed sleep-wake phase, while higher doses 3 to 9 mg given 60 to 90 minutes before the desired bedtime will help with jet lag sleep disorder or primary insomnia.
However, significant clinical evaluation is frequently required to understand the roots of insomnia and the proper timing of melatonin administration. Unfortunately, in the United States, melatonin is considered a dietary supplement; hence, the quality of the source of melatonin is always a concern.
Melatonin receptor agonists address some of these concerns about purity and quality, but fewer data are available with these agents. It is clear that forms of exogenous melatonin especially controlled-release and melatonin receptor agonists have a role in the treatment of circadian rhythm sleep disorders in patients with insomnia especially in the elderly and in those with comorbid depressive disorders.
The safety and tolerability of melatonin, especially compared with other hypnotic agents, suggests a very favorable cost-benefit ratio and is one of the primary considerations in the treatment of insomnia. Increasing sleep latency through a hypnotic or sedative effect has long been a paradigm that has been overemphasized in the treatment of insomnia and psychiatric illness.
It appears that the actual sleep induction effect of melatonin and its receptor analogues is quite modest and their mechanism of action is more sophisticated: amplifying natural circadian differences in alertness and possibly creating a more biologically normal sleep pattern.
: Circadian rhythm melatonin| MELATONIN AND YOUR BODY | Until recent history, humans melafonin temperate climates were emlatonin to few hours of Circadian rhythm melatonin Cancer-fighting home remedies in the Circadizn their fires gave predominantly yellow light. Melatonin phase shifts human circadian rhythms in a placebo-controlled simulated night-work study. Wehrens, S. How do circadian rhythms affect health? Wilson SJ, Nutt DJ, Alford C, et al. |
| What is melatonin? | Entrainment of free-running circadian rhythms by melatonin in blind people. Circadian rhythm in adults. Data are presented as mean ± sd , unless otherwise stated. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Here's all you need to know. Melatonin can also be metabolised to 6-hydroxymelatonin sulphate which is excreted in the urine and one study reported patients with IBS having increased levels of this metabolite Wisniewska-Jarosinska et al. Neuroendocrinology 39 : — |
| Melatonin Does Not Shift the Circadian Clock, But Promotes Sleep at Bedtime | YaleNews | Your rhythm may adjust based on your work hours, physical activity, stress and anxiety, and additional habits or lifestyle choices. Age is another factor that influences your circadian rhythm. Infants, teens, and adults all experience circadian rhythms differently. Newborns do not develop a circadian rhythm until they are a few months old. This can cause their sleeping patterns to be erratic in the first days, weeks, and months of their lives. Their circadian rhythm develops as they adapt to the environment and experience changes to their bodies. Babies begin to release melatonin when they are about 3 months old, and the hormone cortisol develops from 2 months to 9 months old. Toddlers and children have a fairly regulated sleep schedule once their circadian rhythm and body functions mature. Children need about 9 or 10 hours of sleep a night. Teenagers experience a shift in their circadian rhythm known as sleep phase delay. Unlike in their childhood years with early bedtimes around 8 or 9 p. Melatonin may not rise until closer to 10 or 11 p. or even later. Their peak sleepy hours at night are from 3 to 7 a. Adults should have a pretty consistent circadian rhythm if they practice healthy habits. Their bedtimes and wake times should remain stable if they follow a fairly regular schedule and aim for 7 to 9 hours of sleep every night. Adults likely get sleepy well before midnight, as melatonin releases into their bodies. As adults, we reach our most tired phases of the day from 2 to 4 a. Older adults may notice their circadian rhythm changes with age, and they begin to go to bed earlier than they used to and wake in the wee hours of the morning. In general, this is a normal part of aging. Sometimes it is not possible to follow your circadian rhythm, and your lifestyle needs and internal clock clash. This can occur because of:. Jet lag occurs when you travel over several time zones quickly, and your body is not aligned to the time of your new environment. Your circadian rhythm is attuned to the place where you left, and it has to readjust. This may result in feeling tired during the day or feeling wide awake at night. You may experience other changes that impact your well-being until your circadian rhythm normalizes again. It may take a day or up to a week to feel acclimated to the new time zone. It typically takes a day for each hour you shift to regulate your sleep-wake cycle. You may even experience mild symptoms of jet lag when clocks fall backward or forward for daylight saving time. The disruption may not last too long, but your body may need a few days to adjust. You may experience disruptions to your circadian rhythm, but you can get it back on track. Here are some tips for promoting a healthy hour schedule:. Sometimes alterations to your circadian rhythm may be the sign of a more serious condition like a circadian rhythm sleep disorder. Two of these disorders are advanced sleep phase and delayed sleep phase. You may be more susceptible to these if you work an irregular shift, have low vision, or are a teenager or older adult. Deficiencies of this hormone can lead to sleep disruptions and insomnia. Melatonin supplementation can effectively treat this problem after medical diagnosis. Decreased levels of melatonin, which exceed those seen during normal ageing, have been reported in neurodegenerative disorders, especially in Alzheimer's disease and other types of senile dementia. About Contact Outreach Opportunities News. Search Search. Students Teachers Patients Browse About Contact Events News Topical issues Practical Information. You and Your Hormones. Students Teachers Patients Browse. Human body. Home Hormones Melatonin. Melatonin Melatonin is mainly produced by the pineal gland and although it appears not to be essential for human physiology, it is known to have a range of different effects when taken as a medication. Melanocyte-stimulating hormone Oestradiol Glossary All Hormones Resources for Hormones. Alternative names for melatonin N-acetylmethoxytryptamine optic nerve to the pineal gland once darkness has fallen. Melanocyte-stimulating hormone. Tags for this content Coordination and Control Key Stage 4 Age 11 - 14 Age 14 - Related Endocrine Conditions. Jet lag Circadian rhythm sleep disorders View all Endocrine conditions. Related Glands. Pineal gland View all Glands. For each subject and each item, the five HAYFRN questionnaires per day were averaged. The min SSS ratings during the evenings of the treatment days were analyzed with a two-way repeated-measures ANOVA time × group. The sleep parameters from wrist actigraphy and sleep logs were analyzed with a two-way multivariate analysis of variance MANOVA with one within-subjects factor day with four levels baseline mean of d 2—6, treatment d 1—3 and one between-subjects factor group placebo and 0. When significant, Greenhouse-Geisser corrected degrees of freedom were used for univariate analyses. The Columbia Jet Lag score and SSS from the HAYRFN questionnaires were each analyzed with a two-way ANOVA days × group. The remaining items on the HAYFRN questionnaires were analyzed with a two-way MANOVA days × group. Significant univariate analyses were followed by pairwise comparisons. Data are presented as mean ± sd , unless otherwise stated. The three groups did not differ significantly in age, sex, or morningness-eveningness score. Table 1 baseline rows shows that they did not differ in DLMO, sleep schedules, or the interval between the Tmin and wake time and thus the circadian time of light exposure. On the first treatment day, the 0. Circadian phase marked by the DLMO, the estimated Tmin, 1 and scheduled sleep times. Calculated by dividing cumulative phase advance of DLMO after 3 treatment days by 3. Figure 2 shows that larger phase shifts were observed with melatonin, compared with placebo, and Fig. Post hoc analysis showed significantly larger phase shifts in the 0. Figure 1 shows the time of the mean DLMOs for the 0. Error bars , se. In each graph, the thinner line shows the mean profile during the baseline phase assessment, and the bold line shows the profile during the final phase assessment. Horizontal lines indicate the average DLMO threshold for each group. Phase advances in the DLMO for all subjects. Horizontal lines represent the medians, which were 1. All of our subjects slept quite well Fig. The decrease in TST on the first treatment day was because subjects were put to bed at their usual time but were awakened 1 h earlier Fig. On the other days, subjects slept almost all of the allotted 8 h Fig. The 3. However, there were no significant group differences in any of the sleep measures. Univariate analysis indicated that this was due to the reduction in TST on treatment d 1. Sleep parameters from sleep logs during baseline d 2—6 and treatment days for the three groups. Total sleep time was reduced on treatment d 1 as a function of the protocol Fig. The SSS ratings Fig. There was no significant main effect of group or days by group interaction. Symptom questionnaires during baseline d 2—6 and treatment days for the three groups. The SSS was administered five times per day, and the scale maximum most sleepy is 7. The Columbia Jet Lag Scale was administered at bedtime and the scale maximum is The Columbia Jet Lag scores changed very little during the study Fig. There were no significant main effects of group or days and no significant group by days interaction. The ratings for the six symptoms on the HAYFRN questionnaire were mild and evenly distributed across study groups and days. The MANOVA indicated no significant main effects of group or days and no significant days by group interaction. There was a significant increase in sleepiness in the hours before bedtime during the treatment days for all groups Fig. However, there was no significant main effect of group or time by group interaction. SSS on treatment days from 30 min before administration of the first pill until bedtime. In addition, this treatment produced relatively little misalignment between circadian rhythms and the sleep schedule and thus did not produce side effects or jet lag-type symptoms. Although slightly larger phase shifts were obtained with the 3. In addition, the higher melatonin dose made subjects slightly, although not significantly, more sleepy in the evenings after taking the pill. Therefore, we recommend using the 0. Most people would be able to take the 3. We advanced wake time by 1 h but not bedtime on the first day of treatment, cutting sleep short by 1 h, which was probably responsible for the slight increase in sleepiness on treatment d 1. Therefore, we advise also advancing bedtime and keeping the sleep opportunity the same on all treatment days. Although appropriately timed bright light and melatonin may be able to hasten reentrainment after an abruptly advanced sleep schedule, as occurs with early morning shifts or after eastward jet travel, people will suffer several days of circadian misalignment and the associated jet lag-type symptoms until reentrainment is complete. Arendt et al. This regimen is ideal with the doses we tested when bedtime is advanced 5—7 h, but there will still be several days of circadian misalignment. With our treatment, a gradually advancing sleep schedule, gradually advancing morning bright light, and gradually advancing afternoon melatonin are used preflight and so more of the phase shifting is done ahead of time. However, it is not necessary to follow the treatment for a number of days equivalent to the number of time zones crossed. Partially advancing rhythms preflight will reduce the severity and duration of misalignment and will also reduce the risk of antidromic reentrainment because light is less likely to fall on the phase-delay portion of the light PRC for further explanation, see Refs. Ideally, a treatment that produces even larger phase advances would be even better as long as the circadian rhythms remained aligned with the sleep schedule, as they did in the current study. One way to increase the phase advance would be to use light that is enriched with blue wavelengths to which the circadian system is most sensitive e. It is also possible that a different timing of melatonin administration could produce larger phase advances because when it comes to producing phase shifts, the timing is as critical as the dose. In the current study, the two melatonin doses were administered at different circadian phases to coincide with the maximum phase-advance regions of their respective PRCs. However, the timing of the 0. In addition, these subjects were entrained to h zeitgebers and thus the magnitude of the phase shifts was limited. The timing of the 3. PRCs to different doses of melatonin using identical protocols need to be generated to pinpoint the optimal circadian times for the administration of different doses. Two previous studies comparing different doses of melatonin for producing phase shifts showed a dose-dependent response 8 , Larger phase shifts were observed with the 3. Another group 34 observed larger phase advances with a 5. In both studies, the different doses were administered at the same time, and so the greater phase shifts with the larger doses may have been, at least in part, due to a more ideal timing for these doses rather than the increased amount of melatonin present. When the individual phase shifts are considered Fig. This implies that there is a limit in the magnitude of phase shift that can be attained and that melatonin increases the chances of attaining this limit. In another study from our laboratory 8 , a similar pattern was observed with a maximum advance of approximately 4—5 h and the minimum increasing from placebo to the 0. We can speculate that if with light alone the daily maximum shift is not achieved, then coadministration of melatonin may push the system to the upper limit. Alternatively, daily limits with melatonin alone and light alone may exist such that the combination can produce larger cumulative phase shifts than either can individually. Melatonin and matching placebos were provided by Ecological Formulas a division of Cardiovascular Research Ltd. Light boxes were donated by Enviro-Med Vancouver, WA. Authors H. are listed alphabetically. They all made important contributions to this work. We are grateful to Young Cho, Meredith Durkin, Valerie Ellois, Cynthia Hiltz, Hyungsoo Kim, Clara Lee, Katy Lenz, Tom Molina, and Jonathan Swisher for all their assistance with data collection. We thank Erin Lensch for help with the sleep analysis and figures. We thank our medical director, Keith L. Callahan, M. This work was supported by National Institutes of Health Grant R01 NR Eastman CI , Martin SK How to use light and dark to produce circadian adaptation to night shift work. Ann Med 31 : 87 — Google Scholar. Lewy AJ , Bauer VK , Ahmed S , Thomas KH , Cutler NL , Singer CM , Moffit MT , Sack RL The human phase response curve PRC to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int 15 : 71 — Revell VL , Eastman CI How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms 20 : — Arendt J , Skene DJ , Middleton B , Lockley SW , Deacon S Efficacy of melatonin treatment in jet lag, shift work, and blindness. J Biol Rhythms 12 : — Takahashi T , Sasaki M , Itoh H , Ozone M , Yamadera W , Hayshida K , Ushijima S , Matsunaga N , Obuchi K , Sano H Effect of 3 mg melatonin on jet lag syndrome in an 8-h eastward flight. Psychiatry Clin Neurosci 54 : — Samel A , Wegmann HM , Vejvoda M , Maab H , Gundel A , Schutz M Influence of melatonin treatment on human circadian rhythmicity before and after a simulated 9-hr time shift. J Biol Rhythms 6 : — Burgess HJ , Crowley SJ , Gazda CJ , Fogg LF , Eastman CI Preflight adjustment to eastward travel: 3 days of advancing sleep with and without morning bright light. J Biol Rhythms 18 : — Sharkey KM , Eastman CI Melatonin phase shifts human circadian rhythms in a placebo-controlled simulated night-work study. Am J Physiol Regul Integr Comp Physiol : R — R Crowley SJ , Lee C , Tseng CY , Fogg LF , Eastman CI Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. Czeisler CA , Johnson MP , Duffy JF , Brown EN , Ronda JM , Kronauer RE Exposure to bright light and darkness to treat physiologic maladaptation to night work. N Engl J Med : — Boivin DB , James FO Circadian adaptation to night-shift work by judicious light and darkness exposure. J Biol Rhythms 17 : — Lockley SW , Skene DJ , James K , Thapan K , Wright J , Arendt J Melatonin administration can entrain the free-running circadian system of blind subjects. J Endocrinol : R1 — R6. Sack RL , Brandes RW , Kendall AR , Lewy AJ Entrainment of free-running circadian rhythms by melatonin in blind people. Hack LM , Lockley SW , Arendt J , Skene DJ The effects of low-dose 0. |
| Search form | Although the theory that disturbances of sleep and mood have a shared pathology is not new, it is beginning to receive more clinical attention. The importance of vigilance for evolving secondary causes especially mood and anxiety disorders when treating patients with insomnia cannot be overstated. Kasper S, Hajak G, Wulff K, et al. We are grateful to Young Cho, Meredith Durkin, Valerie Ellois, Cynthia Hiltz, Hyungsoo Kim, Clara Lee, Katy Lenz, Tom Molina, and Jonathan Swisher for all their assistance with data collection. Czeisler CA , Johnson MP , Duffy JF , Brown EN , Ronda JM , Kronauer RE Exposure to bright light and darkness to treat physiologic maladaptation to night work. PMID |
die Mitteilung ist gelöscht
Welche rührende Wörter:)
Ich denke, dass Sie den Fehler zulassen. Ich kann die Position verteidigen.
Es kommt mir nicht ganz heran. Wer noch, was vorsagen kann?