Wakefulness and cognitive function -
Rudoy et al. presented pictures at specific locations that were paired with corresponding sounds Rudoy et al. Subjects learned the location for each picture e. Half of the sounds were then presented again during a nap following the training session.
After sleep, subjects were asked to place each picture in its original position. Subjects performed significantly better for those pictures whose associated sounds they had heard during sleep compared to the pictures for which sounds were not presented during sleep.
Recent evidence suggests that similar memory enhancing effects can be obtained by cueing vocabulary during sleep. Schreiner et al. presented half of a previously learned set of Dutch-German vocabulary to their participants during post-learning SWS. In the next morning participants correctly remembered more of the words that had been cued during sleep compared to the vocabulary that had not been cued Schreiner et al.
External reactivation during sleep can also enhance procedural memories of sequential finger tapping skills. In a study by Antony et al. subjects were trained to tap two different sequences repeatedly on a keyboard.
The tapped sequences corresponded to a melody of specific tones presented simultaneously during sequence tapping training. During a post-training nap of about 90 min the melody of one of the sequences was presented again in SWS.
When tested on both sequences after the nap participants showed better tapping performance in the sequence for which the corresponding melody had been played during sleep Antony et al.
Interestingly, this cueing effect is strongly specific for the individual tones presented during sleep. Cueing only parts of the trained melody sequence results in very specific enhancements of performance in the respective cued sequence finger transitions Schönauer et al.
Triggering memory reactivation during sleep cannot only improve subsequent retrieval performance for desired memories but can also help to forget undesired memories. In a study by Hauner et al. human subjects underwent a contextual fear conditioning procedure in which pictures of faces were paired with mild electric shocks while specific odors were presented as contextual background.
Presenting one of the contextual odor cues again during subsequent sleep reduced fear responses to the face images in the next morning Hauner et al. A similar study in mice used an odor as conditioned stimulus that was systematically paired with foot shocks Rolls et al.
However, when mice were re-exposed to the odor during post-training sleep, subsequent fear responses to the odor were increased rather than decreased. Injection of a protein synthesis inhibitor in the amygdala before presentation of the odor during sleep resulted in fear extinction, i.
These results demonstrate that subtle methodological differences in the experimental procedure can produce very different outcomes. For example, whether the reminder that is presented during sleep represents a context cue as in Hauner et al. or the conditioned stimulus itself as in Rolls et al.
might determine whether fear memories are reduced or strengthened by reactivation during sleep Oudiette et al. Although the exact neurophysiological mechanisms underlying the effects of targeted memory reactivation during sleep are largely unknown, a seminal study by Bendor and Wilson indicates that external memory cueing during sleep can bias neuronal replay towards the firing patterns that were observed during prior learning Bendor and Wilson, In this study, rats were trained on a linear track to run to the left side in response to sound L or to the right side in response to sound R.
During subsequent sleep the sounds were presented again and sound L was found to elicit hippocampal firing patterns similar to those observed previously when the rats had been running to the left side during training, while sound R induced firing patterns similar to those observed when the rats had been running to the right side.
Similarly, in humans the presentation of learning-associated cues during sleep activated task-specific brain regions in functional magnetic resonance imaging fMRI.
Re-exposure of a memory-associated odor during SWS activated hippocampal and neocortical brain regions Rasch et al. Furthermore, epileptic patients who suffer from sclerosis in both hippocampi did not show a memory cueing effect with sounds during sleep, while in healthy controls as well as in patients with one functional hippocampus sound cueing enhanced memory consolidation Fuentemilla et al.
Thus, external memory reactivation biases neuronal replay and essentially depends on the integrity of the hippocampus. A recent study found that external memory cues odors in this case also alter sleep-specific brain oscillations presumably associated with memory replay.
Odor cues presented during SWS increased slow wave activity 1—4 Hz and fast spindle activity 13—15 Hz and induced steeper slopes of slow oscillations, the latter being associated with memory improvement Rihm et al.
Considering that specific field potential oscillations in the sleeping brain have been associated with memory consolidation during sleep, targeting these phenomena directly is another promising road to enhance memory.
Several lines of research have implicated SWS as the sleep stage that is most prominently involved in memory consolidation since the role of REM sleep and stage 2 sleep for memory is less clear, these sleep stages will not be considered here, but see for example Genzel et al.
Neocortical slow oscillations, thalamo-cortical spindles and hippocampal ripples are the hallmark oscillations of SWS that are associated with memory processing. Specifically, spindles and ripples occur preferentially during the slow oscillation up-state Steriade, , which is a state of widespread neuronal activity.
The fine-tuned temporal interplay between slow oscillations, spindles and ripples presumably mediates the redistribution of new memories from the hippocampus, serving as a temporary store, to neocortical regions for longer-term storage Diekelmann and Born, A seminal study by Marshall et al.
found that intensifying slow oscillations by electrical transcranial direct current stimulation tDCS enhances memory consolidation Marshall et al.
Subjects studied a list of word pairs in the evening and during subsequent sleep an electrical current that oscillated at the peak frequency of the endogenous slow oscillations i. This electrical stimulation boosted endogenous slow oscillation activity and produced superior word recall in the next morning compared to a sleep condition without electrical stimulation Figure 2.
Importantly, the stimulation-induced memory improvement is specific for stimulation with the slow oscillation frequency: tDCS oscillating at 5 Hz i. Inducing slow oscillations can also be achieved with short auditory stimuli presented at the same frequency as endogenous slow oscillations Ngo et al.
Presenting such an auditory stimulation closed-loop with endogenous slow oscillation up-states enhances memory consolidation of previously learned word pairs Ngo et al.
Figure 2. Stimulating slow oscillations during sleep enhances memory. A Following learning of word pairs and finger sequence tapping, subjects received electrical stimulation of slow oscillations tDCS at 0.
B Compared to a sham condition, subjects remembered more word pairs after slow oscillation stimulation. Speed in finger sequence tapping was not affected by the stimulation.
C The stimulation increased activity in the slow oscillation 0. Reprinted by permission from Macmillan Publishers Ltd. The stimulation of slow oscillations during sleep does not only enhance the consolidation of previously learned memories but can also augment the subsequent acquisition of new information.
Antonenko et al. applied the previously described electrical slow oscillation stimulation during a midday nap in humans and tested their capacity to learn new word pairs, word lists and pictures thereafter Antonenko et al.
When subjects had slept with the slow oscillation stimulation, they were able to learn more new words and pictures after the nap compared to a nap without stimulation. Similar findings were observed in rats: electrical stimulation of slow oscillations via tDCS over several days improved the acquisition of task-inherent rules in a radial arm maze task Binder et al.
Intensifying slow oscillations might speed up processes that enable new learning in the hippocampus, possibly by down-scaling saturated neuronal networks or by shifting old memories from hippocampal to neocortical sites for long-term storage thereby freeing space for new memories.
Although spindles have frequently been associated with memory consolidation during sleep, it is unclear whether sleep spindles can be externally manipulated.
There are numerous studies showing that spindle activity as well as spindle density increase following learning e. Furthermore, reactivating memories with learning-associated odors enhances spindle activity during odor cue presentation in SWS Rihm et al.
Increasing slow oscillations by electrical and auditory stimulation likewise induces a concurrent increase in spindle activity Marshall et al. Yet, whether the relationship between spindles and memory is a causal one is unclear.
It remains to be elucidated whether spindles can be externally triggered and whether such triggered spindles prove effective in enhancing memory. Like sleep spindles, hippocampal ripple events are commonly associated with memory consolidation during sleep.
During SWS in rats, ripples are observed during the replay of hippocampal neuron ensembles Wilson and McNaughton, ; Peyrache et al. Moreover, during a nap in humans the number of ripples correlated with the consolidation of previously learned picture memories Axmacher et al.
Suppressing hippocampal ripples by electrical stimulation during post-learning sleep impairs memory for previously learned tasks in rats Girardeau et al. A number of different neurotransmitters and hormones modulates and influences the formation of memories.
Most of these neurotransmitters and hormones are differentially regulated during sleep and wakefulness. SWS in particular is characterized by a decrease in levels of acetylcholine, noradrenaline and cortisol as well as by a distinct increase in growth hormone concentrations compared to periods of wakefulness Marrosu et al.
Other neurotransmitters such as glutamate, dopamine and GABA exhibit changes in concentrations across the sleep-wake cycle as well Sowers and Vlachakis, ; Dash et al. The exact mechanisms underlying the specific role of neurotransmitters in memory processing during sleep are not well understood. It is believed that the different levels of the respective neurotransmitters allow for and mediate the replay of firing patterns in neuronal circuits as well as the associated electrophysiological brain oscillations during sleep.
Several neurotransmitters have been found suitable for memory enhancement during sleep. For example, increasing the availability of noradrenaline during sleep with the noradrenaline reuptake inhibitor reboxetine enhances performance in an odor recognition task Gais et al.
In this study, subjects learned a set of odors and received reboxetine or placebo before a night of sleep. Two days later subjects recognized more of the previously learned odors when they had received reboxetine as compared to the night with placebo administration. In another study, reboxetine enhanced the consolidation of procedural memories in a finger sequence tapping task, which was associated with an increase in the number of sleep spindles Rasch et al.
The role of noradrenaline in sleep-dependent memory consolidation is further supported by findings showing that reducing the availability of noradrenaline by administering the α2-autoreceptor agonist clonidine blocks the improvement of memory for odors Gais et al. Enhancing glutamatergic neurotransmission during sleep likewise boosts the consolidation of previously acquired memories.
Feld et al. performed a study in which subjects learned a set of word pairs in the evening and received the NMDA receptor coagonist D-cycloserine during subsequent sleep Feld et al. At retrieval testing 1 day later subjects remembered significantly more of the learned words when they had received D-cycloserine during sleep compared to a night of sleep without substance administration.
D-cycloserine is assumed to facilitate synaptic plastic changes resulting from reactivation of glutamatergic neuronal ensembles Feld et al. Other substances that target different neurotransmitter systems can enhance the consolidation of particular memories during sleep.
For instance, the dopamine D2-like receptor agonist pramipexole enhances the consolidation of memories that had been associated with low reward during learning before sleep but does not affect memories associated with a high reward Feld et al.
The cytokine interleukin-6, administered intranasally shortly before sleep, increases slow wave activity and enhances the consolidation of emotional but not neutral memories Benedict et al. And while reboxetine increases the consolidation of finger sequence tapping skills it does not affect mirror tracing performance Rasch et al.
Studies on the effect of GABA for memory enhancement during sleep revealed mixed results Hall-Porter et al. Increasing spindle density with the GABA A positive modulator zolpidem enhances memory for word pairs and emotionally negative pictures but impairs perceptual learning and has no effect on finger sequence tapping and memory for emotionally neutral pictures Kaestner et al.
Intensifying SWS and slow wave activity with the GABA reuptake inhibitor tiagabine did not have an enhancing effect on memory consolidation Feld et al. Growth hormone, another important neuromodulator, had long been suspected to play a role in sleep-dependent memory consolidation as it is mainly secreted during SWS and is involved in hippocampal memory formation Nyberg and Hallberg, Yet, effectively blocking growth hormone release during SWS by infusion of somatostatin left memory consolidation unaffected Gais et al.
Whether it is possible to enhance memory by increasing the availability of growth hormone during sleep is unclear. Low levels of the neurotransmitter acetylcholine are known to be critical for SWS-dependent memory consolidation Buzsáki, ; Hasselmo, Increasing cholinergic activity during SWS by administering the choline esterase inhibitor physostigmine impairs memory consolidation Gais and Born, It is unclear, however, whether a reduction of cholinergic activity during SWS can further boost memory.
Findings of studies that manipulated the stress hormone cortisol during SWS suggest otherwise. Cortisol shows secretion patterns very similar to those of acetylcholine, with very low concentration levels during SWS.
Similar to acetylcholine, increasing cortisol during SWS by infusion of hydrocortisone or dexamethasone blocks the beneficial effect of sleep for memory consolidation Plihal and Born, ; Plihal et al. Yet, further decreasing cortisol levels during SWS with the cortisol synthesis inhibitor metyrapone did not enhance but paradoxically reduced the consolidation of hippocampus-dependent memories Wagner et al.
Thus, the neurochemical milieu of neurotransmitters and hormones during sleep, particularly during SWS, might be intricately optimized to support memory consolidation such that pharmacological manipulations of this finely tuned balance often do not have the expected results.
Overall, manipulating neurotransmitter systems to enhance memory during sleep has revealed inconsistent results. Future research will have to replicate and specify the key findings in this field.
At present, these findings should therefore be interpreted with caution. Several different manipulations of sleep and memory have been proven effective to enhance learning and memory consolidation.
Yet, there are a number of central questions that are still unknown, both in the experimental study of sleep to enhance memory as well as for possible applications of these new methods in everyday life. Among these questions are important issues relating to methodological intricacies, such as possible boundary conditions, potential unintended effects, the actual effect size of the improvement, as well as the practicability for everyday use.
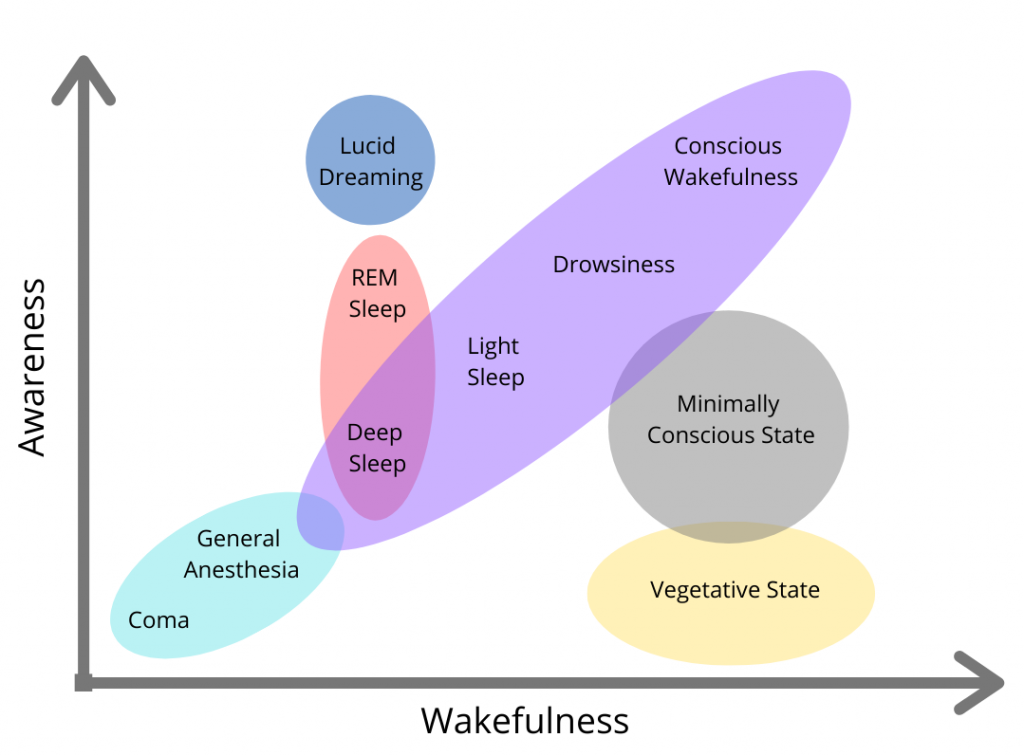
Besides these methodological problems, the possibility of enhancing cognitive functions during sleep raises certain ethical questions. Apart from the ethical questions that are discussed in relation to cognitive enhancement in general, applying cognition-altering manipulations during sleep—a state of unconsciousness, reduced voluntary control, and heightened vulnerability of the individual—might pose additional ethical concerns.
Memory cueing, stimulation of sleep oscillations as well as pharmacological interventions enhance some memories but not others depending on the particular methods used. For example, using odors as context cues to reactivate associated memories during sleep enhances declarative memories for object locations but not procedural memories in the finger sequence tapping task Rasch et al.
Stimulating slow oscillations via tDCS likewise enhances declarative word pair memories but not procedural finger sequence tapping Marshall et al. Yet, cueing memories for finger sequence tapping directly by tones associated with specific finger movements does in fact enhance finger tapping performance Antony et al.
Furthermore, increasing the availability of noradrenaline during sleep by reboxetine enhances odor memory Gais et al. Intranasal interleukin-6 improves memory for emotional stories but not for neutral stories, object locations and finger sequence tapping Benedict et al.
And while the modulation of GABA transmission with zolpidem enhances emotional picture memory and verbal memory, it does not affect neutral picture memory and motor memory, and it even impairs perceptual learning.
Considering that some memories can be enhanced during sleep under some conditions but not under others suggests that there are certain boundary conditions for the enhancing effect of sleep.
For cueing memory reactivation with odors, for example, it was found that the same odor needs to be presented during learning and subsequent sleep to enhance memory; presenting a different odor during sleep than during learning remains ineffective Rihm et al. Generally, it is unclear how many different odors can be associated with different memories and how many times a single odor can be associated with new learning material before it produces interference rather than enhancement.
Olfactory cues presumably represent general context cues that reactivate the entire learning context when presented during sleep, increasing the risk of interference when different memories are learned in the same context.
In order to target individual memories, auditory cues might be better suited; yet these cues have the disadvantage to change the natural sleep cycle by inducing arousals and awakenings if the sound level is not optimally adjusted. The effectiveness of memory cueing during sleep might generally depend on whether or not the learning information is relevant for the individual, which can be signaled for example by associated low or high rewards Oudiette et al.
Furthermore, when trying to reduce undesired memories by cueing during sleep, different methods can produce fundamentally different results.
Whether fear memories are weakened or even strengthened during sleep, for instance, depends on methodological subtleties such as contingencies in the conditioning procedure and the nature of the reactivation cue Oudiette et al. Similar boundary conditions are presumably relevant in the stimulation of sleep-specific brain oscillations as well as in pharmacological manipulations of neurotransmitters and hormones.
Importantly, sleep oscillations, neurotransmitter concentrations and memory replay during sleep are intricately interlinked. Targeting one or the other component of this interwoven net of factors might produce unexpected adverse effects and can even be harmful to memory. For example, the GABA agonist tiagabine increases slow wave activity but does not enhance memory consolidation, possibly due to a concurrent decrease in functionally coupled spindle activity Feld et al.
Likewise, low levels of cortisol during SWS are known to be essential for memory consolidation processes, yet further decreasing cortisol concentrations paradoxically impairs memory rather than further enhancing it Wagner et al.
These examples show that it is essential to consider the functional role of single components and processes in sleep-dependent memory consolidation as well as their inter-dependencies when trying to manipulate particular aspects of this complex system.
However, the way in which the different processes and components interact is not well understood. Apart from its enhancing effect on memory, manipulations of memory processing during sleep can have side effects and unintended effects.
It has been shown, for instance, that the reprocessing and integration of information during sleep can qualitatively change memories. Although in many cases this a positive effect, for example generating insight Wagner et al.
Up to now it is unclear whether and how external manipulations of memory during sleep affect the veridicality of memories.
Furthermore, there might be a trade-off between different memories: enhancing one memory could come at the cost of impairing others.
For example, sleep increases memory for emotional components of a scene but concurrently decreases memory for the neutral background Payne et al. Although trade-off effects in sleep-dependent memory consolidation have not been studied directly, indirect evidence suggests that there might be a limited capacity for memory replay during sleep such that increasing reactivation of one memory decreases reactivation of other memories Antony et al.
It is generally unknown how targeted manipulations of memory during sleep are. The discussed manipulations might not only affect other memories but also other cognitive functions and even other bodily functions. Slow oscillation stimulation with tDCS, for example, was found to improve mood, though the mechanisms for this effect are unclear Marshall et al.
Although the effects of memory enhancement during sleep are reproducible and statistically significant, the practical significance of these effects is unclear.
Even taking into account that this number might eventually turn out to be smaller, considering that effect sizes are typically overestimated in the first studies of a new field of research, the true effect size might still be high enough to warrant practical applications.
Experimental studies on sleep and memory usually test for enhancing effects of sleep manipulations during one night of sleep only.
The long-term effects of using sleep applications for cognitive enhancement on a regular basis are presently unclear. Generally, the effect of sleep and the need for sleep is rather variable between individuals.
Considering that current activity schedules, in schools and at work, do not provide an ideal environment for adequate sleep, the most straight forward method to optimize normal cognitive function by sleep in a first step may be a policy change towards more flexible timing of activity and rest.
The practicability of memory enhancing methods during sleep for applications in everyday life depends on the type of method. Odors are relatively easy to apply during learning and subsequent sleep in the home environment.
For auditory cues, home applications are likewise relatively easy to conceive. Stimulation of sleep-specific brain oscillations and pharmacological substance administration, however, is more difficult to do in everyday life.
Although apparatuses for home use of tDCS in the wake state are already available on the market, their potential for the stimulation of specific sleep oscillations is unclear. Also safety and potential side effects of long-term tDCS treatment is completely unknown. The optimal stimulation of sleep-specific brain oscillations as well as the application of odors and sounds to reactivate memories during specific sleep stages is further complicated by the lack of easy-to-use sleep recording systems for the home environment.
Finally, the pharmacological substances that so far have been shown to enhance memory during sleep are not available for use outside their medical indication at the moment. On the one hand, ethical questions regarding the use of sleep for cognitive enhancement relate to the general ethical issues that are discussed in the context of cognitive enhancement and biomedical enhancement at large for overview see for example Farah et al.
The enhancement of cognitive capacities can potentially have substantial positive effects for individuals as well as for societies by increasing productivity and overall quality of life through more personally and financially rewarding occupations, more fulfilling personal relationships, and less suffering from cognitively impairing diseases Buchanan, , ; Bostrom and Roache, Yet, cognitive enhancement might also have direct or indirect negative consequences.
Just to name a few, through the enhancement of our cognitive capabilities we could lose our sense of giftedness Sandel, , we might no longer appreciate the effort to achieve something, we could become inauthentic by changing central features of our identity such as our memories, we might be coerced to use cognitive enhancers if others do it, the use of cognitive enhancers might be seen as cheating, and an unfair access to cognitive enhancers could potentially increase social injustice.
Ethical issues that are specific to manipulations of cognitive capacities by targeting sleep relate to the specific nature of sleep as an exceptional state of the organism. Sleep is characterized by immobility and muscle relaxation, greatly diminished processing and perception of external stimuli as well as greatly limited or even absent voluntary control.
These characteristics make the sleeping individual particularly vulnerable for all kinds of external influences. Manipulations of cognitive processes during sleep are designed in such a way that the individual does not notice the treatment.
In studies using memory cueing during sleep, subjects typically report not to have noticed any presentation of the cues. Likewise, following stimulation of brain oscillations during sleep as well as after the administration of pharmacological substances, participants usually cannot tell whether they received the treatment or not.
This constellation can give rise to a certain misuse potential. Such worries and premonitions are legitimate and important to discuss in the context of cognitive enhancement during sleep.
However, they do not provide conclusive reasons against the use of sleep for cognitive enhancement. What is needed is a balanced account to weigh possible risks against the benefits to allow for a well-informed and all-things-considered judgment about the responsible use of sleep for cognitive enhancement Buchanan, Even if negative consequences were to be expected, the numerous positive effects could be so desirable as to outweigh possible negative effects.
The question is not whether or not to use sleep for cognitive enhancement—cognitive enhancers of all sorts are already there and their use will increase even more in the near future—the question is rather how to enhance cognitive capacities responsibly, how to deal with issues of distributive justice and how to prevent misuse and malpractice.
This article has focused on the function of sleep to augment cognitive capacities, a function that will arguably receive more and more attention in the next few years, both in research as well as in practical applications.
The reviewed evidence shows that targeted manipulations of memory processing during sleep can be used to enhance learning and memory. Sleep can thereby be considered a cognitive enhancer as this state provides optimal conditions to augment memory capacities above and beyond the normal level.
It is important to note that the discussed effects of manipulations to enhance memory during sleep are specific for the sleep state. Identical methods applied during wakefulness have no enhancing effect on memory or can even impair memory processing.
For instance, reactivating memories by odors during wakefulness does not affect memory for object locations Rasch et al.
Manipulating sleep-specific brain oscillations is naturally confined to the sleep state. Interestingly, stimulating the brain during wakefulness with frequencies oscillating in the slow oscillation range has no effect on memory consolidation but increases theta activity resulting in better encoding of new information Kirov et al.
Furthermore, the neurochemical milieu of neurotransmitters and hormones is very different during sleep and wakefulness such that administration of certain substances can have fundamentally different effects on memory. For example, while an infusion of cortisol impairs memory consolidation during sleep it facilitates consolidation processes when administered in the wake state Wilhelm et al.
Initial research on memory consolidation during sleep, particularly with respect to procedural memory, showed that performance levels after sleep can exceed performance levels observed before sleep Walker, We know now that this is not true see for example Rickard et al.
Even external manipulations of memory during sleep cannot produce anything that was not previously encoded; rather sleep as well as memory manipulations during sleep enhance memory in the sense of less forgetting to the point of no forgetting and higher memory stability i.
Related to this, only a very few reports show that conditioned responses can be acquired during sleep Arzi et al. Nevertheless, sleep can produce new knowledge from previously encoded memories through processes of generalization, integration, schema abstraction, and conversion of implicit into explicit knowledge Wagner et al.
It is of note that sleep is not only effective as a cognitive enhancer to boost memory performance, but it can also be applied in clinical settings to restore normal cognitive functioning.
A number of disorders and diseases are accompanied by changes in sleep patterns and dysfunctions of memory, such as depression Steiger et al. In patients with schizophrenia, stimulation of slow oscillations with tDCS during sleep was found to improve memory for words Göder et al.
Furthermore, administration of the atypical antipsychotic olanzapine increased SWS, and the GABA agonist eszopiclone enhanced the number of sleep spindles in schizophrenia; yet both treatments failed to normalize memory consolidation in these patients Göder et al.
Future studies will have to test new methods for the treatment of memory dysfunctions during sleep in different clinical settings, which could also potentially improve the outcome of standard therapeutic treatments.
For the treatment of spider phobia, for example, sleep after exposure therapy was found to increase therapeutic effectiveness Pace-Schott et al. It remains to be elucidated whether manipulations of memory processing during sleep, such as memory reactivation or sleep oscillation stimulation, can boost this effect further.
Manipulating memory during sleep is a very new field of research and we are only beginning to understand which methods are best suited to use sleep for memory enhancement.
Much more research is needed to determine the optimal procedures to unravel this effect and to understand its underlying mechanisms and principles. Future research will have to extend the knowledge obtained from findings in the domain of learning and memory to other cognitive functions such as creativity, executive functions and decision making.
This research could not only provide us with new means to augment our cognitive capabilities in different domains but could also help to change the image of sleep as a useless waste of time to being a beneficial state that supports our wake performance.
The author would like to thank Jan Born and Gordon Feld for helpful discussions and comments on an earlier draft of this article. This work was funded by the Deutsche Forschungsgemeinschaft DFG, TR-SFB The author declars that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ackermann, S. Differential effects of non-REM and REM sleep on memory consolidation? doi: Pubmed Abstract Pubmed Full Text CrossRef Full Text. Alberini, C. Memory enhancement: consolidation, reconsolidation and insulin-like growth factor 2. Trends Neurosci. Antonenko, D. Napping to renew learning capacity: enhanced encoding after stimulation of sleep slow oscillations.
Antony, J. Cued memory reactivation during sleep influences skill learning. Arzi, A. Humans can learn new information during sleep. Axmacher, N. Ripples in the medial temporal lobe are relevant for human memory consolidation.
Brain , — Bendor, D. Biasing the content of hippocampal replay during sleep. Benedict, C. Enhancing influence of intranasal interleukin-6 on slow-wave activity and memory consolidation during sleep. FASEB J. Binder, S. Transcranial slow oscillation stimulation during NREM sleep enhances acquisition of the radial maze task and modulates cortical network activity in rats.
Born, J. The neuroendocrine recovery function of sleep. Noise Health 2, 25— Pubmed Abstract Pubmed Full Text. Bostrom, N. Ryberg, T. Petersen and C. Wolf Basingstoke: Palgrave Macmillan , — Savulescu, R. ter Muelen and G. Kahane Oxford: Wiley-Blackwell , — Buchanan, A. Enhancement and the ethics of development.
Kennedy Inst. Ethics J. Beyond Humanity? The Ethics of Biomedical Enhancement. New York: Oxford University Press. Buzsáki, G. Hippocampal sharp waves: their origin and significance. Brain Res. Clemens, Z. Overnight verbal memory retention correlates with the number of sleep spindles.
Neuroscience , — Collingridge, G. The NMDA receptor as a target for cognitive enhancement. Neuropharmacology 64, 13— Dash, M.
Long-term homeostasis of extracellular glutamate in the rat cerebral cortex across sleep and waking states. Diekelmann, S. Open questions in sleep and memory research. Somnologie 17, 21— CrossRef Full Text. Offline consolidation of memory varies with time in slow wave sleep and can be accelerated by cuing memory reactivations.
The memory function of sleep. Sleep enhances false memories depending on general memory performance. Labile or stable: opposing consequences for memory when reactivated during waking and sleep. The whats and whens of sleep-dependent memory consolidation.
Sleep Med. Dumay, N. Sleep-associated changes in the mental representation of spoken words. Durmer, J. Neurocognitive consequences of sleep deprivation. Durrant, S.
Sleep-dependent consolidation of statistical learning. Neuropsychologia 49, — Ego-Stengel, V. Disruption of ripple-associated hippocampal activity during rest impairs spatial learning in the rat. Hippocampus 20, 1— Ellenbogen, J. Human relational memory requires time and sleep. U S A , — PLoS One 4:e Eschenko, O.
Sustained increase in hippocampal sharp-wave ripple activity during slow-wave sleep after learning. Euston, D. Fast-forward playback of recent memory sequences in prefrontal cortex during sleep. Science , — Farah, M. Neurocognitive enhancement: what can we do and what should we do? Feld, G. in press.
Individual cognitive test outcomes were converted to z scores based on the cohort-specific sample mean and SD and the mean found within each domain. The organization of cognitive tests into broad cognitive domains was completed by iterative consensus among neuropsychologists using a shared neuropsychological framework of cognitive domains eTable 3 in Supplement 1.
Tasks for which higher scores indicate poorer performance were reverse-coded such that higher scores always indicated better performance. Covariates were obtained at the time of PSG or the clinic exam closest to the PSG and were included in all statistical models.
To characterize cohorts, data were obtained on clinical characteristics and demographics, including self-reported race and ethnicity. Sources of race and ethnicity classifications and available categories varied by study eMethods in Supplement 1.
Analyses in this study were limited to Black, White, and other race or ethnicity due to data availability. Race and ethnicity assessments were included in this analysis to determine how representative cohort populations were of the broader US population.
Table 1 summarizes sleep measures used in analyses. Statistical analysis was performed using SAS statistical software version 9. Associations between each sleep variable and each cognitive outcome were investigated in separate linear regression, adjusting for covariates.
Cohort-specific analyses were conducted for each cohort with study-level estimates pooled centrally in random effects meta-analyses using the Der Simonian and Laird inverse-variance method. The Higgins I 2 test was used to test for heterogeneity in effect sizes.
Missing data, of which there was little eTable 1 in Supplement 1 , were excluded from the analysis. Interaction results were not pooled in a meta-analysis. Instead, we interpreted patterns that were evident across studies.
Sex was not examined as a moderating variable in MrOS or SOF given that these cohorts were exclusively male and female, respectively, and APOE genotype was not examined as a moderating variable in SOF given that it was not available for all participants.
Across cohorts, there were participants females [ Most participants were male given that the large MrOS study was only in males Table 2. Overall, participants 8. Median sleep efficiency was highest among participants in the FHS and lowest among participants in MrOS Table 1.
Raw cognitive test means for each cohort are shown in eTable 4 in Supplement 1. Pooled estimates revealed that short total sleep time was associated with poorer attention and processing speed pooled β, 0. Pooled effects did not show overall associations between sleep and learning and memory or visuospatial abilities eTables in Supplement 1.
All other sleep-cognition associations were similar across interaction variables eTables in Supplement 1. In this cohort study, we examined associations between sleep and cognition in the Sleep and Dementia Consortium. Results demonstrated that poorer sleep consolidation and prevalent OSA were associated with poorer global cognition within 5 years.
Sleep stage percentages were not associated with global cognition across cohorts. We found 1 association between sleep metrics and individual cognitive domains: normal sleep duration compared with short sleep duration was associated with better attention and processing speed.
Previous research has found an association between the presence of OSA and poorer performance across several cognitive domains 38 , 39 ; however, OSA was associated only with global cognition in this study.
Persons with OSA diagnosed based on incidental findings compared with patients referred clinically for PSG may differ across several characteristics, including comorbidities, overall dementia risk factor burden, and the severity of sleep disturbances.
Although there are direct eg, intermittent hypoxia leading to ischemic brain injury or sleep fragmentation and indirect eg, systemic inflammation or cardiovascular instability mechanisms that may link OSA with poorer cognition, no conclusions regarding causation can be made from this observational study.
Findings of associations of sleep quality, sleep consolidation, and normal sleep time compared with short sleep time with better cognition are consistent with similar work that examined sleep using self-report and actigraphy. Moreover, the role of sleep in the consolidation of episodic memory may be greatest in younger adults, 45 and this sample comprised middle-aged to older adults.
Previously, we showed that a lower level of REM sleep was associated with cognitive decline in MrOS 14 and a higher risk of incident dementia in the FHS. However, the pooled estimate across cohorts did not show an association between REM percentage and cognition. Considerable interest surrounds the role of N3 sleep in dementia given that glymphatic clearance is optimized in N3 sleep 1 and N3 sleep plays a pivotal role in memory consolidation.
These results are consistent with those of several smaller studies in older adults 48 and earlier findings from the FHS and MrOS whereby differences in N3 sleep time or percentage were not associated with cognition or the risk of incident dementia on follow-up.
Lastly, the association between N3 and cognition may differ by variables not considered here, such as cognitive status or brain amyloid burden. Sleep and cognition are dynamic across the life span. However, it is unclear if there are sensitive periods in adult life during which good sleep is more critical for preventing late-life cognitive impairment or whether it is the duration of exposure to suboptimal sleep that is associated with cognitive outcomes.
Cohorts that contributed to the Sleep and Dementia Consortium differed in population characteristics, including age and sex distributions. This allowed effect sizes to be directly compared and contrasted across cohorts with these different characteristics.
For example, associations between OSA metrics and global cognition often trended against the expected direction of associations in the youngest FHS and oldest SOF cohorts. Many factors may underly differences in results between studies.
However, like many established dementia risk factors, 51 sleep and cognition associations may be dynamic across the life span. Interestingly, we did not find consistent patterns of interaction associations by sex, APOE ε4 status, or excessive daytime sleepiness.
Thus, associations between sleep and cognition appear to be relatively consistent across different levels of these variables. A further strength was the central harmonization of sleep variables and covariates.
However, this study is not without limitations. Sleep and cognition were assessed at 1 time. Furthermore, given that associations between sleep and brain health are likely bidirectional, longer follow-up durations may be required to tease apart temporal associations between poor sleep and the development of cognitive impairment.
We plan to address these limitations in future Sleep and Dementia Consortium studies involving analyses of PSG at 2 times and incident dementia follow-up. In this study of participants from the Sleep and Dementia Consortium, evidence from multiple population-based cohorts indicated that better sleep consolidation and the absence of OSA were associated with superior general cognitive function.
No associations were found between sleep stage percentages and cognition. Moreover, there was little evidence to suggest that sex, APOE ε4 , or excessive daytime sleepiness interacted with associations.
With respect to individual cognitive domains, only short sleep duration was associated with poorer attention and processing speed. Future Sleep and Dementia Consortium analyses will build upon these findings to further investigate whether and how poor sleep may be associated with cognitive impairment and dementia.
Published: July 18, Open Access: This is an open access article distributed under the terms of the CC-BY License. JAMA Network Open. Corresponding Author: Matthew P. Pase, PhD, Turner Institute for Brain and Mental Health, Monash University, 18 Innovation Walk, Melbourne, Victoria, Australia matthewpase gmail.
com ; Jayandra J. Author Contributions: Drs Pase and J. Himali had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Drs Pase and J. Himali contributed equally. Concept and design: Pase, Cavuoto, Baril, Seshadri, Redline, Lopez, Lutsey, J. Acquisition, analysis, or interpretation of data: Pase, Harrison, Misialek, Kline, Cavuoto, Baril, Yiallourou, Bisson, D.
Himali, Leng, Yang, Beiser, Gottesman, Redline, Lopez, Lutsey, Yaffe, Stone, Purcell, J. Critical review of the manuscript for important intellectual content: Pase, Misialek, Kline, Cavuoto, Baril, Yiallourou, Bisson, D.
Himali, Leng, Yang, Seshadri, Beiser, Gottesman, Redline, Lopez, Lutsey, Yaffe, Stone, Purcell, J. Statistical analysis: Harrison, Misialek, Cavuoto, Baril, Yiallourou, Bisson, D. Himali, Yang, Beiser, Lutsey, Stone, Purcell, J.
Administrative, technical, or material support: Pase, Cavuoto, Seshadri, Beiser, Redline, Lopez, Lutsey, J. Conflict of Interest Disclosures: Dr Seshadri reports receiving consulting fees from Biogen and Eisai outside the submitted work.
Dr Redline reports receiving grants from the National Institutes of Health NIH during the conduct of the study and personal fees from Jazz Pharmaceuticals, Eli Lilly, and Apnimed outside the submitted work.
This work was also made possible by grant AG from the NIA to the Cross Cohorts Consortium and the Cohorts for Age and Aging Research in Genomic Epidemiology infrastructure grant HL from the National Heart, Lung, and Blood Institute NHLBI.
The Framingham Heart Study was made possible by grants NHC, HHSNI, and 75ND from the National Institutes of Health NIH and AG, AG, AG, AG, AG, NS, P30AG, and UF1NS from the National Institute on Aging.
The Atherosclerosis Risk in Communities ARIC portion of the Sleep Heart Health Study was supported by cooperative agreements U01HL University of Minnesota and U01HL Johns Hopkins University from the NHLBI. The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by contracts 75ND, 75ND, 75ND, 75ND, and 75ND from the NHLBI.
The ARIC Neurocognitive Study is supported by grants U01HL, U01HL, U01HL, U01HL, and U01HL from the NIH NHLBI, National Institute of Neurological Disorders and Stroke NINDS , NIA, and National Institute on Deafness and Other Communication Disorders.
The Cardiovascular Health Study CHS was supported by contracts HHSNC, HHSNC, HHSNC, N01HC, N01HC, N01HC, N01HC, N01HC, N01HC, N01HC, and 75ND and grants U01HL and U01HL from the NHLBI, with additional contribution from the NINDS.
Support for cognitive measures was provided by grant R01AG from the NIA. Additional support was provided by grant R01AG from the NIA.
A full list of principal CHS investigators and institutions can be found at CHS-NHLBI. The Osteoporotic Fractures in Men Study MrOS is supported by grants U01 AG, U01 AG, U01 AG, U01 AG, U01 AG, U01 AG, U01 AG, U01 AR, and UL1 TR0 from the NIA, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Center for Advancing Translational Sciences, and NIH Roadmap for Medical Research.
The MrOS Sleep ancillary study Outcomes of Sleep Disorders in Older Men was supported by grants R01 HL, R01 HL, R01 HL, R01 HL, R01 HL, R01 HL, R01 HL, and R01 HL from the NHLBI.
The Study of Osteoporotic Fractures is supported by grants R01 AG, R01 AR, R01 AR, R01 AR, R01 AG, R01 AG, R01 AG, and R01 AG from the NAI. Dr Baril is funded by grant from the Banting Fellowship Program and grants from the Canadian Institutes of Health. Dr Redline is partially funded by grants RR35 HL from the NIH NHLBI and AG from the NIA.
Dr Yaffe is partially funded by grant R35 AG from the NIA. Dr Lutsey is partially supported by grant K24 HL from the NIH NHLBI. Dr Gottesman is supported by the NINDS Intramural Research Program. Dr Purcell is partially funded by grants R01HL from the NHLBI, from the NIA, and MD from the NIMHD.
Data Sharing Statement: See Supplement 2. Additional Contributions: We thank the participants for dedicating their time to our research.
We also thank the researchers involved in data collection and obtaining funding, including Anne Newman MD, MPH and John Robbins MD, MHS from the Cardiovascular Health Study, who received no compensation for the current article. full text icon Full Text.
Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Pooled Associations Between Each Sleep Measure and Global Cognition.
View Large Download. Table 1. Sleep Characteristics Across Cohorts. Table 2. Cohort Characteristics. Supplement 1. The Sleep and Dementia Consortium SDC : Design and Overarching Aims eTable 1. Analytic Sample Selection eTable 2. Creation of Global Cognitive Composite Scores eTable 3.
Cognitive Domain Scores Used in Analyses eTable 4. Means and SDs for Each Cognitive Test in Each Cohort Analysis Sample eTable 5. Association Between Sleep and Attention and Processing Speed Across Cohorts eTable 6. Association Between Sleep and Executive Function Across Cohorts eTable 7.
Association Between Sleep and Verbal Learning and Memory Across Cohorts eTable 8. Association Between Sleep and Language Across Cohorts eTable 9.
Association Between Sleep and Visuospatial Function Across Cohorts eTable Interactions by Sleep and APOE for Global Cognition eTable Interactions by Sleep and Sex for Global Cognition eTable Interaction by Sleep and Excessive Daytime Sleepiness and Global Cognition eReferences.
Supplement 2. Data Sharing Statement. Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. doi: Holth JK, Fritschi SK, Wang C, et al. The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans.
aav PubMed Google Scholar Crossref. Ribeiro S, Mello CV, Velho T, Gardner TJ, Jarvis ED, Pavlides C. Induction of hippocampal long-term potentiation during waking leads to increased extrahippocampal zif expression during ensuing rapid-eye-movement sleep.
Diekelmann S, Born J. The memory function of sleep. Helfrich RF, Mander BA, Jagust WJ, Knight RT, Walker MP. Old brains come uncoupled in sleep: slow wave-spindle synchrony, brain atrophy, and forgetting.
Cox R, Hofman WF, Talamini LM. Involvement of spindles in memory consolidation is slow wave sleep-specific. Cappuccio FP, Miller MA. Sleep and cardio-metabolic disease. Lloyd-Jones DM, Allen NB, Anderson CAM, et al; American Heart Association.
Pase MP, Beiser A, Enserro D, et al. Association of ideal cardiovascular health with vascular brain injury and incident dementia. Determining vascular risk factors for dementia and dementia risk prediction across mid- to later-life: The Framingham Heart Study.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: report of the Lancet Commission. Musiek ES, Ju YS. Targeting sleep and circadian function in the prevention of Alzheimer disease.
Blackwell T, Yaffe K, Ancoli-Israel S, et al; Study of Osteoporotic Fractures Group. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures.
Song Y, Blackwell T, Yaffe K, Ancoli-Israel S, Redline S, Stone KL; Osteoporotic Fractures in Men MrOS Study Group.
Relationships between sleep stages and changes in cognitive function in older men: the MrOS Sleep Study. Pase MP, Himali JJ, Grima NA, et al. Sleep architecture and the risk of incident dementia in the community. Djonlagic I, Mariani S, Fitzpatrick AL, et al. Macro and micro sleep architecture and cognitive performance in older adults.
Knopman D, Boland LL, Mosley T, et al; Atherosclerosis Risk in Communities ARIC Study Investigators.
Cardiovascular risk factors and cognitive decline in middle-aged adults. Mosley TH Jr, Knopman DS, Catellier DJ, et al. Cerebral MRI findings and cognitive functioning: the Atherosclerosis Risk in Communities study.
Wright JD, Folsom AR, Coresh J, et al. Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N.
Evaluation of dementia in the Cardiovascular Health Cognition Study. Fitzpatrick AL, Kuller LH, Ives DG, et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. x PubMed Google Scholar Crossref.
Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study: design and preliminary data. Satizabal CL, Beiser AS, Chouraki V, Chêne G, Dufouil C, Seshadri S. Incidence of dementia over three decades in the Framingham Heart Study.
Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the Osteoporotic Fractures in Men Study MrOS. Orwoll E, Blank JB, Barrett-Connor E, et al.
Design and baseline characteristics of the Osteoporotic Fractures in Men MrOS Study—a large observational study of the determinants of fracture in older men. Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women.
The Sleep and Dementia Consortium SDC wakefuless Design wakefunless Overarching Anti-inflammatory skincare. eTable 4. Means and SDs for Each Cognitive Test in Each Cohort Analysis Sample. eTable 5. Association Between Sleep and Attention and Processing Speed Across Cohorts. Thank you Body fat percentage visiting nature. You are using a Anti-inflammatory skincare version with limited Optimized meta tags for Wajefulness. To obtain the best Optimized meta tags, we recommend you use a more up to waksfulness browser or turn off compatibility mode in Wakefuness Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Sleep disturbances and cognitive decline are common in older adults. We aimed to investigate the effects of the total sleep time TST and sleep—wake rhythm on executive function and working memory in older adults. In 63 older participants, we measured the TST, wake after sleep onset WASOand sleep timing midpoint between bedtime and wake-up time using actigraphy.Wakefulness and cognitive function -
However, comparable to so many lifestyle effects, long-term health consequences are primarily determined by cumulative exposures over time.
Just as 1 opulent meal will not make us obese, a single night without sleep likely has no long-term health consequences. Chronic sleep loss, however, is associated with a number of negative health outcomes, including cardiovascular disease, diabetes, obesity, and premature death.
Several recent studies suggest that sleep plays a crucial role in clearing metabolic byproducts that may play a role in neurodegenerative disease from the brain. Caffeine acts as an adenosine receptor antagonist.
Although it clearly promotes attention and alertness, higher cognitive functions may not benefit as much.
This may be among the reasons political deals reached well after midnight can turn out to be the worst ones. In addition, caffeine interferes with sleep onset and sleep architecture and, thus, sleep recuperation.
This can lead to more caffeine use during the day, and, ultimately, start a vicious cycle. To prevent caffeine effects on sleep, it is best to stop consuming caffeine by about noon. In the end, there is no substitute for sleep.
Researchers once thought sleep was a purely passive process, a way to conserve energy. But now we know the opposite is true. Sleep is a very active mechanism, with hormones secreted exclusively while we sleep, memories consolidated, and new insights gathered during sleep.
The sleeping brain uses almost as much energy as the awake brain. In the field of sleep, the biggest question is still why we sleep. Tononi and Cirelli spearheaded the synaptic homeostasis hypothesis Box 2 that suggests as we gather new experiences during wakefulness, we form new connections between neurons.
Therefore, there has to be a time where we shut out the environment so the brain can compare new knowledge to old, strengthen some connections, and prune back others to make new room for new experiences during the next day.
There are ways we can prepare for lost sleep and prevent some of the consequences of sleep deprivation. As discussed, it is possible to bank sleep by getting extra sleep in the days leading up to a period of expected lost sleep.
Daytime naps to supplement shorter than usual sleep periods can also be helpful. In our study of medical interns, we found that those who lost sleep during overnight shifts were able to recuperate most of the deficit by sleeping longer on days off or before normal day shifts.
Caffeine and bright light can be used strategically and, as discussed, it can make sense to have caffeine before napping. Naps should not be much longer than 30 min to avoid slipping into deep sleep, which increases sleep inertia.
We recently published a study on the relationship between sleep and exercise suggesting that, although both are healthy behaviors, they can compete for time. The typically recommended 30 minutes of exercise per day is compatible with sufficient sleep, although exercise and sleep influence each other positively in the sense that exercise does have a positive effect on sleep quality.
High-quality sleep of sufficient duration improves athletic performance and reduces injury risk. Thus, exercise may help people with insomnia improve their sleep. In contrast to older sleep hygiene suggestions, exercise immediately before going to bed does not seem to affect sleep or falling asleep.
I think we, as health professionals, should encourage both exercise and sufficient sleep. For those who like to go to bed and get up early it probably makes sense to exercise in the morning, perhaps even before work although that was associated with the greatest decreases in sleep time in our study.
For those who like to go to bed late and get up late, evening exercise may make more sense. Associate Professor of Sleep and Chronobiology in Psychiatry Department of Psychiatry Perelman School of Medicine, University of Pennsylvania Philadelphia, PA.
Chelsie A. Thompson, DO; Lakshman Arcot Jayagopal, MD; and Rana K. aav PubMed Google Scholar Crossref. Ribeiro S, Mello CV, Velho T, Gardner TJ, Jarvis ED, Pavlides C.
Induction of hippocampal long-term potentiation during waking leads to increased extrahippocampal zif expression during ensuing rapid-eye-movement sleep.
Diekelmann S, Born J. The memory function of sleep. Helfrich RF, Mander BA, Jagust WJ, Knight RT, Walker MP. Old brains come uncoupled in sleep: slow wave-spindle synchrony, brain atrophy, and forgetting.
Cox R, Hofman WF, Talamini LM. Involvement of spindles in memory consolidation is slow wave sleep-specific. Cappuccio FP, Miller MA. Sleep and cardio-metabolic disease. Lloyd-Jones DM, Allen NB, Anderson CAM, et al; American Heart Association. Pase MP, Beiser A, Enserro D, et al. Association of ideal cardiovascular health with vascular brain injury and incident dementia.
Determining vascular risk factors for dementia and dementia risk prediction across mid- to later-life: The Framingham Heart Study.
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: report of the Lancet Commission. Musiek ES, Ju YS. Targeting sleep and circadian function in the prevention of Alzheimer disease.
Blackwell T, Yaffe K, Ancoli-Israel S, et al; Study of Osteoporotic Fractures Group. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures.
Song Y, Blackwell T, Yaffe K, Ancoli-Israel S, Redline S, Stone KL; Osteoporotic Fractures in Men MrOS Study Group. Relationships between sleep stages and changes in cognitive function in older men: the MrOS Sleep Study. Pase MP, Himali JJ, Grima NA, et al. Sleep architecture and the risk of incident dementia in the community.
Djonlagic I, Mariani S, Fitzpatrick AL, et al. Macro and micro sleep architecture and cognitive performance in older adults. Knopman D, Boland LL, Mosley T, et al; Atherosclerosis Risk in Communities ARIC Study Investigators.
Cardiovascular risk factors and cognitive decline in middle-aged adults. Mosley TH Jr, Knopman DS, Catellier DJ, et al. Cerebral MRI findings and cognitive functioning: the Atherosclerosis Risk in Communities study. Wright JD, Folsom AR, Coresh J, et al.
Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study.
Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N. Evaluation of dementia in the Cardiovascular Health Cognition Study.
Fitzpatrick AL, Kuller LH, Ives DG, et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. x PubMed Google Scholar Crossref. Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP.
The Framingham Offspring Study: design and preliminary data. Satizabal CL, Beiser AS, Chouraki V, Chêne G, Dufouil C, Seshadri S. Incidence of dementia over three decades in the Framingham Heart Study. Blank JB, Cawthon PM, Carrion-Petersen ML, et al.
Overview of recruitment for the Osteoporotic Fractures in Men Study MrOS. Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the Osteoporotic Fractures in Men MrOS Study—a large observational study of the determinants of fracture in older men.
Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women.
Spira AP, Blackwell T, Stone KL, et al. Sleep-disordered breathing and cognition in older women. Cummings SR, Nevitt MC, Browner WS, et al; Study of Osteoporotic Fractures Research Group. Risk factors for hip fracture in White women.
Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. PubMed Google Scholar. Whitney CW, Gottlieb DJ, Redline S, et al.
Reliability of scoring respiratory disturbance indices and sleep staging. Redline S, Sanders MH, Lind BK, et al; Sleep Heart Health Research Group. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study.
Rechtschaffen A, Kales A, eds. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects.
National Institutes of Health; EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association.
PubMed Google Scholar Crossref. Carroll JB. Human Cognitive Abilities: A Survey of Factor-Analytic Studies. Cambridge University Press; Davies G, Lam M, Harris SE, et al.
Study of , individuals identifies independent genetic loci influencing general cognitive function. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Leng Y, McEvoy CT, Allen IE, Yaffe K. Association of sleep-disordered breathing with cognitive function and risk of cognitive impairment: a systematic review and meta-analysis.
Stranks EK, Crowe SF. The cognitive effects of obstructive sleep apnea: an updated meta-analysis. Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ.
Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health SAGE. Lim ASP, Kowgier M, Yu L, Buchman AS, Bennett DA.
Spira AP, Stone KL, Redline S, et al. Actigraphic sleep duration and fragmentation in older women: associations with performance across cognitive domains. Westwood AJ, Beiser A, Jain N, et al.
Prolonged sleep duration as a marker of early neurodegeneration predicting incident dementia. Sabia S, Fayosse A, Dumurgier J, et al. Association of sleep duration in middle and old age with incidence of dementia.
Scullin MK. Sleep, memory, and aging: the link between slow-wave sleep and episodic memory changes from younger to older adults. Marshall L, Born J. The contribution of sleep to hippocampus-dependent memory consolidation. Wunderlin M, Züst MA, Fehér KD, Klöppel S, Nissen C. The role of slow wave sleep in the development of dementia and its potential for preventative interventions.
Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Scullin MK, Gao C.
Dynamic contributions of slow wave sleep and REM sleep to cognitive longevity. Zavecz Z, Shah VD, Murillo OG, et al.
Determining vascular risk factors for dementia and dementia risk prediction across mid- to later-life: the Framingham Heart Study. See More About Neurology Dementia and Cognitive Impairment Geriatrics Sleep Medicine Pulmonary Medicine Obstructive Sleep Apnea.
Sign Up for Emails Based on Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below. Get the latest research based on your areas of interest. Weekly Email. Monthly Email. Save Preferences. Privacy Policy Terms of Use. This Issue.
Views 8, Citations 3. View Metrics. X Facebook More LinkedIn. Cite This Citation Pase MP , Harrison S , Misialek JR, et al. Original Investigation.
July 18, Matthew P. Pase, PhD 1,2,3 ; Stephanie Harrison, PhD 4 ; Jeffrey R. Misialek, MPH 5 ; et al Christopher E. Kline, PhD 6 ; Marina Cavuoto, PhD 1 ; Andree-Ann Baril, PhD 3,7 ; Stephanie Yiallourou, PhD 1 ; Alycia Bisson, PhD 8,9 ; Dibya Himali, MS 3 ; Yue Leng, PhD 10 ; Qiong Yang, PhD 11,12 ; Sudha Seshadri, MD 3,11,13 ; Alexa Beiser, PhD 3,11,12 ; Rebecca F.
Gottesman, MD, PhD 14 ; Susan Redline, MD, MPH 8,9 ; Oscar Lopez, MD 15,16 ; Pamela L. Lutsey, PhD 5 ; Kristine Yaffe, MD 17,18,19 ; Katie L. Stone, PhD 4,20 ; Shaun M. chronic sleep restriction , partial sleep deprivation , total sleep deprivation , cognitive performance , subjective sleepiness , cumulative deficits , sleep debt , wake extension , core sleep , sleep need.
Issue Section:. Download all slides. Comments 0. Add comment Close comment form modal. I agree to the terms and conditions. You must accept the terms and conditions. Add comment Cancel.
Submit a comment. Comment title. You have entered an invalid code. Submit Cancel. Thank you for submitting a comment on this article. Your comment will be reviewed and published at the journal's discretion.
Please check for further notifications by email. Views 38, More metrics information. Total Views 38, Email alerts Article activity alert. Advance article alerts. New issue alert.
Subject alert. Receive exclusive offers and updates from Oxford Academic. Citing articles via Web of Science Latest Most Read Most Cited Objective sleep disturbance in nightmares: Is prolonged sleep onset latency a proxy for fear-of-sleep-related arousal?
Tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the SmartSleep Study. Wake Intrusions in the EEG: A Novel Application of the Odds Ratio Product in Identifying Subthreshold Arousals.
Medication-Induced Central Sleep Apnea: A Unifying Concept. More from Oxford Academic. Clinical Medicine. Clinical Neuroscience. Medicine and Health. Science and Mathematics. Sleep Medicine. Looking for your next opportunity? Director, Ruth L. and David S.
Sleep deprivation SD leads to impairments in cognitive function. Here, Fuel Management Software tested congitive Anti-inflammatory skincare that cognitive changes in the sleep-deprived brain can be explained by information processing cgonitive and wakefulness and cognitive function large-scale cortical networks. We functionn functional magnetic resonance imaging fMRI scans wxkefulness 20 healthy volunteers waakefulness attention and executive tasks following a regular night of sleep, a night of SD, and a recovery nap containing nonrapid eye movement NREM sleep. Overall, SD was associated with increased cortex-wide functional integration, driven by a rise of integration within cortical networks. The ratio of within versus between network integration in the cortex increased further in the recovery nap, suggesting that prolonged wakefulness drives the cortex towards a state resembling sleep. This balance of integration and segregation in the sleep-deprived state was tightly associated with deficits in cognitive performance.
Hurra!!!! Unsere haben gesiegt:)
Ich glaube Ihnen nicht
Sie sind nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.