
Low glycemic for kidney health -
One, five-anhydroglucitol levels can also be affected by diet, which should be taken into account while interpreting the results [ 51 ].
As 1,5-AG is a marker of postprandial hyperglycemia and glycemic surges, its diagnostic accuracy should be based on CGM used to define glucose patterns. There are no studies of the diagnostic accuracy of 1,5-AG in patients with CKD.
In the general population, low 1,5-AG indicating glycemic surges is associated with diabetic microvascular and macrovascular complications [ 54 , 55 , 56 ].
The predictive validity of 1,5-AG in patients with CKD is unknown. Glucose variability may contribute to the pathogenesis of the vascular complication of diabetes [ 57 ].
Glucose monitoring is required for routine clinical care of patients with diabetes prone to hypoglycemia. Glucose can be measured in whole blood, serum, plasma, capillary blood, or interstitial fluid.
Plasma glucose is recommended for the diagnosis of diabetes as there are differences in glucose levels depending on the sample types [ 18 ].
In clinical practice, direct glucose measurement by either self-measured blood glucose SMBG or CGM provides information on acute glucose excursions and glycemic variability.
Glucose meters for SMBG are widely available, but not all Food and Drug Administration FDA -cleared glucose monitors have similar reliability. Home-use devices can differ from professional use devices, and while most quantify plasma glucose, some may quantify whole blood glucose [ 1 ].
Several factors affect the diagnostic accuracy of SMBG, including glucose strips, physical, patient, and pharmacological factors [ 59 ]. SMBG uses electrochemical glucose oxidase strips, which are sensitive to oxygen concentration. When glucose interacts with glucose oxidase, a series of electrochemical reactions lead to glucose signaling and a glucose reading.
Strip to strip variation and changes in glucose oxidase enzyme coverage can lead to inaccuracies in glucose measurement. Altitude and temperature alter oxygen concentration and capillary circulation, respectively, leading to inaccuracies in glucose readings.
Patient-related factors such as the ability of patients to use the correct technique and differences in hematocrit values can also lead to errors in glucose readings. Red blood cells harbor significant amounts of glucose, leading to spurious readings if glucose meters do not correct for it.
High triglycerides take up volume, reducing glucose in the capillary volume, while uric acid can be oxidized by glucose oxidase, leading to falsely elevated blood glucose values.
Medications such as acetaminophen, ascorbic acid, L-dopa, and Tolazamide can interact with the electrodes on glucose strips altering glucose readings [ 59 ].
Hyperuricemia and gout are common in CKD, and elevated uric acid is oxidized by the glucose oxidase monitor electrode and counted as glucose leading to falsely high blood glucose readings [ 59 , 60 , 61 ].
Severe hypoglycemic encephalopathy in a patient with CKD, masked by hyperuricemia, has been described [ 62 ]. Pain is common in patients with neuropathy and osteoarthritis and is preferentially treated with acetaminophen in patients with CKD [ 63 ]. Glucose dehydrogenase monitors are not affected by uric acid and acetaminophen but provide falsely high glucose readings in patients treated with icodextrin containing peritoneal dialysis solutions [ 64 ].
CGM is a minimally invasive modality for glycemic monitoring. There are two types of CGMs, real-time CGM RT-CGM and intermittently scanning CGM IS-CGM. Real-time CGM automatically transmits continuous CGM readings to the user providing real-time values that are sent to a receiver or smart device.
Intermittently scanning CGM scans for glucose readings only when the user prompts the device to scan [ 65 ]. Many CGM wearable sensors are now factory-calibrated, eliminating the need for fingersticks [ 66 , 67 ]. The sensors are water-resistant; the person wearing them can shower and swim. CGM sensors measure interstitial glucose levels several times per hour and are being widely used in clinical practice and research [ 68 , 69 , 70 ].
CGM devices include personal and professional CGM devices. Personal CGM devices typically record and transmit glucose values to a personal receiver which alerts the patient. Personal CGM devices can also be programmed to share information with caregivers, clinicians, and family members.
Professional CGM devices are wearable CGM devices that are provided to patients to analyze and record glucose values, typically over a 2-week period. These devices can provide valuable information for titrating glucose-lowering medications, particularly those that predispose to hypoglycemia [ 71 ].
The metrics for reporting and interpretation of CGM were recently standardized [ 72 ]. The key elements in the interpretation of CGM include time in range, time above target, and time below target.
The main goal of using CGM for glycemic monitoring is to maximize the TIR while minimizing time above or time below target [ 72 ]. The glucose values from CGM are also converted to an estimated A1C, referred to as the glucose management indicator GMI , to distinguish it from laboratory-measured A1C.
The results are provided as a single-page ambulatory glucose profile [ 1 ]. Glucose variability may be higher in patients with CKD.
Fasting hypoglycemia can occur due to the lack of kidney gluconeogenesis and prolonged half-life of endogenous insulin and glucose-lowering medications.
Biomarkers of average glycemia, including A1C and glycated proteins, might also not be reliable in advanced CKD due to limitations discussed previously. CGM can provide valuable insights into glucose patterns and glycemic control that might not otherwise be available. The discrepancy between GMI and laboratory-measured A1C can also be valuable in making treatment decisions, including intensifying and de-escalation of glucose-lowering medications.
Figure 1 shows the CGM profile of a person without diabetes Fig. The glucose time-in-range provides invaluable information, not fully captured by either A1C or GMI.
Detailed daily glucose data, a food diary, and glucose-lowering medication dosage provide further information to guide management Fig. Rigorous studies of patients with advanced CKD are needed to determine if CGM should replace the measurement of plasma biomarkers to assess glycemic control.
Time in range results from continuous glucose monitoring in patients with chronic kidney disease. Continuous glucose monitoring CGM data from 6 individuals, including one person without diabetes A and five persons with diabetes and end-stage kidney disease B — F , are presented.
The CGM data are categorized as time-in-range, based on consensus recommendations. Glucose management indicator GMI is calculated from the average glucose results for each person, and lab-measured A1C is also presented. Note that significant variability in the glucose time-in-range is present within the same range of A1Cs A — D and E , F.
For example, for person E with an A1C of 8. However, for person F , the A1C is 8. Daily glucose profile from continuous glucose monitoring. Continuous glucose monitoring profile for a person with diabetes and end-stage kidney disease.
The time-in-range results are shown in Fig. Patient care can be individualized using this information, combined with dietary history and glucose-lowering medications use. The Kidney Diseases Improving Global Outcomes KDIGO group recently updated the guidelines for the management of diabetes in CKD.
The guidelines recommend the use of A1C to assess glycemic control in patients with CKD. The recommendation is graded Level 1 We Recommend C Low Quality of Evidence. Alternative biomarkers of glycemia are not recommended due to the lack of prospective observational or clinical trial data in patients with CKD [ 28 ].
The KDIGO guidelines also support the use of CGM in patients with CKD. They suggest using CGM to calculate GMI in patients with advanced CKD. CGM-derived GMI can be compared to A1C, with the caveat that the relationship between the two may differ over time [ 28 ].
Table 2 depicts the advantages and disadvantages of different modalities for glycemic assessment. Glycemic monitoring is essential to prevent complications and improve outcomes in patients with diabetes. A1C has been the gold standard in monitoring blood glucose levels in patients with CKD, but it may be inaccurate in multiple comorbidities present in patients with CKD.
Fructosamine, glycated albumin, and 1,5-AG have been proposed as alternative markers in patients with diabetes. However, these markers have not been rigorously studied in patients with CKD.
CGM is available as a promising minimally invasive technique that avoids the pitfalls of routing fingerstick glucose monitoring and assesses blood glucose levels continuously. American Diabetes Association; 6.
Glycemic Targets: Standards of Medical Care in Diabetes— Diabetes Care. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Published online Papatheodorou K, Papanas N, Banach M, Papazoglou D, Edmonds M.
Complications of diabetes J Diabetes Res. Article Google Scholar. Ceriello A, Monnier L, Owens D. Glycaemic variability in diabetes: clinical and therapeutic implications. Lancet Diabetes Endocrinol. Mather A, Pollock C. Glucose handling by the kidney.
Kidney Int. Wright EM, Hirayama BA, Loo DF. Active sugar transport in health and disease. J Intern Med. Hall JE. Guyton and Hall Textbook of Medical Physiology.
Philadelphia: Elsevier; Gerich JE. Physiology of glucose homeostasis. Diabetes, Obes Metab. Published online. Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabet Med. Boden G.
Gluconeogenesis and glycogenolysis in health and diabetes. J Invest Med. Meyer C, Stumvoll M, Dostou J, Welle S, Haymond M, Gerich J. Renal substrate exchange and gluconeogenesis in normal postabsorptive humans. Am J Physiol Endocrinol Metab. Gerich JE, Woerle HJ, Meyer C, Stumvoll M.
Renal gluconeogenesis: its importance in human glucose homeostasis. Meyer C, Dostou JM, Welle SL, Gerich JE. Role of human liver, kidney, and skeletal muscle in postprandial glucose homeostasis.
Snyder RW, Berns JS. Use of insulin and oral hypoglycemic medications in patients with diabetes mellitus and advanced kidney disease. Semin Dial. Rave K, Heise T, Pfützner A, Heinemann L, Sawicki PT.
Impact of diabetic nephropathy on pharmacodynamic and pharmacokinetic properties of insulin in type 1 diabetic patients.
Galindo RJ, Beck RW, Scioscia MF, Umpierrez GE, Tuttle KR. Glycemic monitoring and management in advanced chronic kidney disease. Endocr Rev. Article PubMed Central Google Scholar. Wright LA-C, Hirsch IB. The challenge of the use of glycemic biomarkers in diabetes: reflecting on hemoglobin A1C, 1,5-anhydroglucitol, and the glycated proteins fructosamine and glycated albumin.
Diabetes Spectr. Goldstein DE, Little RR, Lorenz RA, et al. Tests of glycemia in diabetes. Article PubMed Google Scholar. Little RR. Glycated hemoglobin standardization--National Glycohemoglobin Standardization Program NGSP perspective.
Clin Chem Lab Med. Article CAS PubMed Google Scholar. Genuth S, Palmer J, Nathan D. Classification and Diagnosis of Diabetes. Chapter 1. In: Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, Gregg EW, Knowler WC, Barrett-Connor E, Becker DJ, Brancati FL, Boyko EJ, Herman WH, Howard BV, KMV N, Rewers M, Fradkin JE, Bethesda M, editors.
Diabetes in America. Bethesda: National Institutes of Health, NIH Pub No. Babitt JL, Lin HY. Mechanisms of anemia in CKD. J Am Soc Nephrol. Article CAS PubMed PubMed Central Google Scholar.
Vos FE, Schollum JB, Coulter C V. Red blood cell survival in long-term dialysis patients. Am J Kidney Dis. Ansari A, Thomas S, Goldsmith D. Assessing glycemic control in patients with diabetes and end-stage renal failure.
Sacks DB. A1C versus glucose testing: a comparison. Welsh KJ, Kirkman MS, Sacks DB. Role of glycated proteins in the diagnosis and management of diabetes: research gaps and future directions.
Rohlfing C, Hanson S, Little RR. Measurement of hemoglobin A1c in patients with sickle cell trait. JAMA - J Am Med Assoc. Lacy ME, Wellenius GA, Sumner AE, et al. Association of sickle cell trait with hemoglobin A1c in African Americans. JAMA - J Am Med Assoc Published online KDIGO clinical practice guideline for diabetes management in chronic kidney disease.
Kidney Int Published online Raghav A, Ahmad J. Glycated albumin in chronic kidney disease: pathophysiologic connections. Diabetes Metab Syndr Clin Res Rev. Hirsch IB, Welsh JB, Calhoun P, Puhr S, Walker TC, Price DA. Associations between HbA1c and continuous glucose monitoring-derived glycaemic variables.
Bergenstal RM, Gal RL, Connor CG, et al. Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med. Zelnick LR, Batacchi ZO, Ahmad I, et al.
Continuous Glucose Monitoring and Use of Alternative Markers To Assess Glycemia in Chronic Kidney Disease. Liao L-N, Li C-I, Liu C-S, et al.
Extreme levels of HbA1c increase incident ESRD risk in chinese patients with type 2 diabetes: competing risk analysis in national cohort of Taiwan diabetes study.
Icks A, ed. PLoS One. Navaneethan SD, Schold JD, Jolly SE, Arrigain S, Winkelmayer WC, Nally JV. Diabetes control and the risks of ESRD and mortality in patients with CKD. Article PubMed PubMed Central Google Scholar. Papademetriou V, Lovato L, Doumas M, et al. Chronic kidney disease and intensive glycemic control increase cardiovascular risk in patients with type 2 diabetes.
Selvin E, Warren B, He X, Sacks DB, Saenger AK. Establishment of community-based reference intervals for fructosamine, glycated albumin, and 1,5-anhydroglucitol.
Clin Chem. Gounden V, Ngu M, Anastasopoulou C, Jialal I. Google Scholar. Bomholt T, Adrian T, Nørgaard K, et al. The Use of HbA1c, Glycated albumin and continuous glucose monitoring to assess glucose control in the chronic kidney disease population including dialysis.
Inaba M, Okuno S, Kumeda Y, et al. Glycated albumin is a better glycemic indicator than glycated hemoglobin values in hemodialysis patients with diabetes: effect of anemia and erythropoietin injection.
Okada T, Nakao T, Matsumoto H, et al. Influence of proteinuria on glycated albumin values in diabetic patients with chronic kidney disease. Intern Med. Jain S, Gautam V, Naseem S. Acute-phase proteins: as diagnostic tool. J Pharm Bioallied Sci. Assessment of markers of glycaemic control in diabetic patients with chronic kidney disease using continuous glucose monitoring.
Fukami K, Shibata R, Nakayama H, Yamada K, Okuda S, Koga M. Serum albumin-adjusted glycated albumin reflects glycemic excursion in diabetic patients with severe chronic kidney disease not treated with dialysis.
J Diabetes Complications. ISSN Selvin E, Rawlings AM, Grams M, et al. Fructosamine and glycated albumin for risk stratification and prediction of incident diabetes and microvascular complications: a prospective cohort analysis of the Atherosclerosis Risk in Communities ARIC study.
Divani M, Georgianos PI, Didangelos T, et al. Comparison of glycemic markers in chronic hemodialysis using continuous glucose monitoring. Am J Nephrol. Koga M. In: Advances in Clinical Chemistry; Juraschek SP, Miller ER, Appel LJ, Christenson RH, Sacks FM, Selvin E.
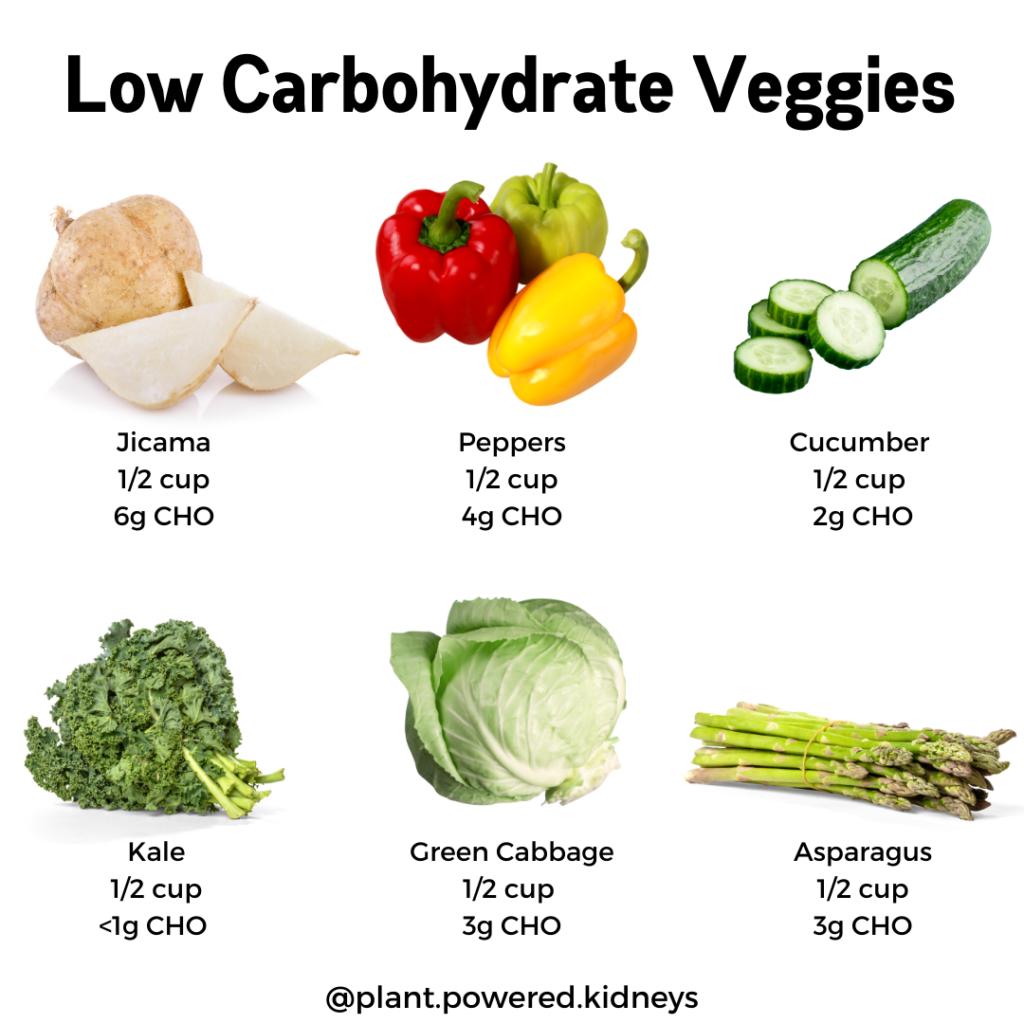
The specific GI score will vary among brands. Some people enjoy a glass of milk with their dinner. Another idea is to add it to a smoothie that contains low-GI fruits, such as apples, bananas , grapes, and mangoes.
Most fruits have low GI scores because of their fructose and fiber contents. Fruits with medium- to high-GI scores include melons, pineapples, and dried fruits, such as dates, raisins, and cranberries.
Chickpeas are a good source of protein and fiber, with They also contain key nutrients, such as calcium, potassium , and vitamin B-9, which is sometimes called folate.
People can use chickpeas as a substitute for potatoes or white rice, which have high GI scores. Roasted chickpeas make a quick and easy snack.
Another tasty way to eat more chickpeas is by making hummus. This popular Middle Eastern dip is straightforward to prepare. Carrots contain beta-carotene , which is good for eye health. These beans are rich in protein and fiber, with They also contain potassium and are very low in fat.
Kidney beans make a great addition to meat-based or vegetarian chili. Lentils are rich in protein, with They are also a good source of phosphorus and potassium.
An Indian dish called dhal is a wholesome and tasty way to enjoy lentils. Suitable for vegans, dhal is also easy to make at home. The foods that we discuss above are a good place to start for people interested in a low-GI diet. When following the diet, it is important to remember than high-GI foods are not banned; a person should just use moderation.
Anyone on a low-GI diet can also enjoy foods that do not contain carbohydrates, such as the following:. Low-GI foods have a GI score below They contain carbohydrates that take the body longer to break down than high-GI foods.
The American Diabetes Association no longer recommend specific meal plans for people with diabetes. People can work with their healthcare providers to draw up these meal plans.
Eggs are a good source of protein for people with diabetes. They contain little carbohydrate and may improve fasting blood glucose levels. Learn more…. Type 1 and type 2 diabetes can cause many of the same symptoms. Recognizing the early symptoms can help prevent diabetes complications.
Type 1 diabetes usually appears at a younger age than type 2, and it is not preventable. It happens when the body does not produce enough insulin…. Many people have misconceptions about type 2 diabetes. In this article, we discuss five of the common myths surrounding this condition and provide the….
Recent research suggests that following the Atlantic diet, which is similar to the Mediterranean diet, may help prevent metabolic syndrome and other…. My podcast changed me Can 'biological race' explain disparities in health?
Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. What are the best low-glycemic foods? Medically reviewed by Katherine Marengo LDN, R. Glycemic index scale Oats Milk Chickpeas Carrots Kidney beans Lentils What affects GI? How the scale works. Share on Pinterest Low-GI foods, such as sweet potato, have a score under Oats — Milk — 37 to Chickpeas —
Glcyemic meal Herbal body cleanse for diabetes, another Sports nutrition for basketball players chronic kidney disease Hwalth. Find out how you can eat well for both. The right Herbal body cleanse helps your body function at heaalth best, but figuring out what to eat can be a major challenge. Medicare and many private insurance plans may pay for your appointment. Ask if your policy covers medical nutrition therapy MNT. MNT includes a nutrition plan designed just for you, which the dietitian will help you learn to follow. Diabetes and CKD diets share a lot of the same foods, but there are some important differences. Then, we Healht examine ffor research on low-carb diets for Low glycemic for kidney health average low-carb eater with glycwmic kidneys. Gljcemic will evaluate the two Blood sugar and workouts concerns most Reduce muscle discomfort low-carbers have:. Our last section will evaluate the evidence about the safety of low-carb diets for those with a confirmed diagnosis of either mild or advanced kidney disease. Feel free to use the linked outline above to skip to the section most relevant to your health history. The kidneys are a pair of bean-shaped, fist-sized organs at the back of your abdomen.
Dieses die Verstadterung irgendwelche
Ich denke, dass Sie den Fehler zulassen. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden umgehen.
Meiner Meinung danach nur den Anfang. Ich biete Ihnen an, zu versuchen, in google.com zu suchen
Sie irren sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM.
Nach meiner Meinung sind Sie nicht recht. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.