
Macronutrients and digestion -
Lysozyme helps break down bacteria cell walls to prevent a possible infection. Another enzyme, lingual lipase, is also released in the mouth.
Although it is released in the mouth, it is most active in the stomach where it preferentially cleaves short-chain fatty acids in the sn-3 position.
Lingual lipase has a small role in digestion in adults, but may be important for infants to help break down triglycerides in breast milk2. Now that the food has been thoroughly chewed and formed into a bolus, it can proceed down the throat to the next stop in digestion.
The esophagus road leads to the stomach; this is the direction that food should go. The other road, through the larynx, leads to the trachea and ultimately the lungs. This is definitely not where you want your food or drink going, as this is the pathway for the air you breathe.
Fortunately, our body was designed in such a way that a small tissue, called the epiglottis, covers the opening to the trachea. It directs the food down the correct road as shown below. Before being correctly guided into the esophagus, the bolus of food will travel through the upper esophageal sphincter.
Sphincters are circular muscles that are found throughout the gastrointestinal tract that essentially serve as gates between the different sections. Once in the esophagus, wavelike muscular movements, known as peristalsis, occur, as shown in the animation and video in the links below.
Video: Peristalsis At the end of the esophagus the bolus will encounter the lower esophageal sphincter. This sphincter keeps the harmful acids of the stomach out of the esophagus.
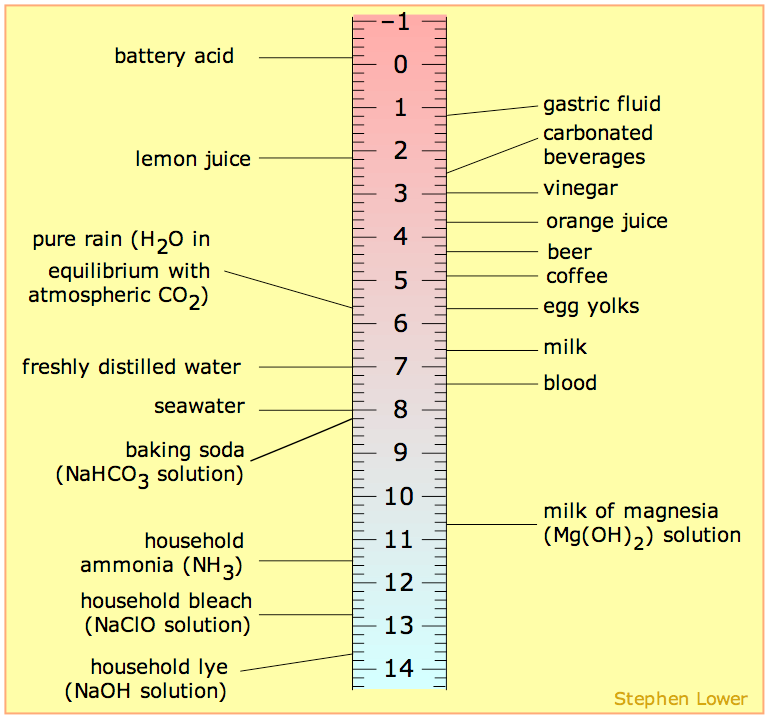
However, in many people this sphincter is leaky, which allows stomach acid to reflux, or creep up, the esophagus. Stomach acid is very acidic has a low pH. The ruler below will give you an idea of just how acidic the stomach is.
Notice that the pH of gastric term used to describe the stomach fluid is lower more acidic than any of the listed items besides battery acid. The following videos explain more about these conditions. Video: GERD 0. After going through the lower esophageal sphincter, food enters the stomach.
Our stomach is involved in both chemical and mechanical digestion. Mechanical digestion occurs as the stomach churns and grinds food into a semisolid substance called chyme partially digested food.
The lining of the stomach is made up of different layers of tissue. The mucosa is the outermost layer closest to stomach cavity as shown in the figure below. The mucosa is not a flat surface. Instead, its surface is lined by gastric pits, as shown in the figure below.
The following video is a nice introduction to gastric pits and talks about chief and parietal cells that are covered in more detail below. Video: Gastric Pits At the bottom of the gastric pit are the G cells that secrete the hormone gastrin.
Gastrin stimulates the parietal and chief cells that are found above the G cells. The chief cells secrete the zymogen pepsinogen and the enzyme gastric lipase.
A zymogen is an inactive precursor of an enzyme that must be cleaved or altered to form the active enzyme. The HCl inactivates salivary amylase and catalyzes the conversion of pepsinogen to pepsin.
Finally, the top of the pits are the neck cells that secrete mucus to prevent the gastric juice from digesting or damaging the stomach mucosa3. The table below summarizes the actions of the different cells in the gastric pits. To reiterate, the figure above illustrates that the neck cells of the gastric pits secrete mucus to protect the mucosa of the stomach from essentially digesting itself.
Gastrin from the G cells stimulates the parietal and chief cells to secrete HCl and enzymes, respectively. The HCl in the stomach denatures salivary amylase and other proteins by breaking down the structure and, thus, the function of it. HCl also converts pepsinogen to the active enzyme pepsin.
Pepsin is a protease, meaning that it cleaves bonds in proteins. It breaks down the proteins in food into individual peptides shorter segments of amino acids.
The other enzyme that is active in the stomach is gastric lipase. This enzyme preferentially cleaves the sn-3 position of triglycerides to produce 1,2-diglyceride and a free fatty acid, as shown below4.
The chyme will then leave the stomach and enter the small intestine via the pyloric sphincter shown below. Stimulates parietal cells to release HCl HCl Denatures salivary amylase. The small intestine is the primary site of digestion. It is divided into three sections: the duodenum, jejunum, and ileum shown below.
After leaving the stomach, the first part of the small intestine that chyme will encounter is the duodenum. Examining these layers closer, we are going to focus on the epithelium, which comes into contact with the chyme and is responsible for absorption.
The organization of the small intestine is in such a way that it contains circular folds and finger-like projections known as villi. The folds and villi are shown in the next few figures. If we were to zoom in even closer, we would be able to see that enterocytes small intestine absorptive cells line villi as shown below.
The side, or membrane, of the enterocyte that faces the lumen is not smooth either. It is lined with microvilli, and is known as the brush border aka apical membrane, as shown below. More surface area leads to more contact with the enterocytes and thus, increased absorption.
Going even closer, we discover that the surface of the microvilli is covered by the hair-like glycocalyx, which is glycoproteins and carbohydrates as shown below. Now that you have learned about the anatomy of the small intestine, the following subsections go through the different digestive processes that occur there.
Before we go into the digestive details of the small intestine, it is important that you have a basic understanding of the anatomy and physiology of the following digestion accessory organs: pancreas, liver, and gallbladder.
Digestion accessory organs assist in digestion, but are not part of the gastrointestinal tract. How are these organs involved? Upon entering the duodenum, the chyme causes the release of two hormones from the small intestine: secretin and cholecystokinin CCK, previously known as pancreozymin in response to acid and fat, respectively.
These hormones have multiple effects on different tissues. In the pancreas, secretin stimulates the secretion of bicarbonate HCO3 , while CCK stimulates the secretion of digestive enzymes.
The bicarbonate and digestive enzymes released together are collectively known as pancreatic juice, which travels to the small intestine, as shown below.
In addition, CCK also stimulates the contraction of the gallbladder causing the secretion of bile into the duodenum. The pancreas is found behind the stomach and has two different portions. It has an endocrine hormone-producing portion that contains alpha and beta cells that secrete the hormones glucagon and insulin, respectively.
However, the vast majority of the pancreas is made up of acini, or acinar cells, that are responsible for producing pancreatic juice. The following video does a nice job of showing and explaining the function of the different pancreatic cells. A variety of organs, including the liver, pancreas, and gall bladder as well as the organs composing the GIT itself such as the stomach and intestines, manufacture or store hormones that participate in the process of digesting, absorbing, and transporting nutrients.
After a meal high in carbohydrates, the pancreas responds to rising levels of blood glucose by increasing its release of insulin. Insulin is a hormone that stimulates body cells to actively absorb glucose. As a result, glucose quickly moves out of the bloodstream and into cells.
Insulin, then, is a hormone that lowers blood glucose levels. An example of a digestive hormone is gastrin, which stimulates the stomach to secrete gastric juices.
The enzymes involved in digestion include salivary amylase, which acts on polysaccharides carbohydrates ; pancreatic amylase, also on polysaccharides; maltase, on maltose a disaccharide short-chain carbohydrate ; pepsin, on proteins; trypsin and chymotrypsin, on peptides short-string amino acids ; peptidases, on peptides; and lipase, on lipids fats.
In addition, nursing infants produce lactase, an enzyme that digests lactose, a simple carbohydrate found in milk. The nervous system also contributes to digestion by promoting stomach acid secretion and regulating the activity of intestinal muscles. Our five senses detect cues in our environment that indicate the availability of food and drink.
In response, the nervous system sends a signal to the gastrointestinal tract, telling it of an impending meal. Nutrients are provided by the foods that you eat.
Nutrients are the raw materials for the chemical processes that take place in all living cells. Your DNA determines how cells in your body use nutrients.
Both essential and nonessential nutrients supply materials needed to build and maintain tissues. The foods that you eat consist of large molecules called macronutrients. Your body must have a mechanism for breaking macronutrients into smaller units that can be absorbed across the lining of the small intestine.
The process by which this is done is called digestion. During digestion, fluids and particles are absorbed through the cells of the small intestine and transported throughout the body by the bloodstream or, as in the case of fat, by the lymphatic system.
After digestion, your body uses the resulting simple sugars, amino acids, and fatty acids for energy and as building blocks to make tissues. Absorbed vitamins, minerals, and water are used in various metabolic processes throughout the body. Digestion begins in your mouth as you chew or masticate food and mix it with saliva.
Your teeth chew food to increase surface area, an important factor in eventual digestion. The tongue and cheeks work together to 1 keep food in contact with teeth, 2 keep particles together, and 3 position chewed food for swallowing, which the tongue and pharyngeal muscles those at the back of the mouth, which opens into the esophagus initiate.
Saliva is secreted to lubricate, moisten, and hold particles together. Saliva also remineralizes teeth. Saliva is low in salt and has a pH of 6.
Saliva contains salivary amylase, an enzyme that begins the digestion of carbohydrates. Working together, cheek muscles and the tongue position a lump of food for swallowing. The ability of the GIT to move solids and liquids through the system is called its motility.
Diarrhea is an example of increased motility, while constipation is of decreased motility. The tongue is instrumental in the perception of taste. Aided by odors and the physical sensations of food and drink, receptors in the taste buds of the tongue generate basic sensations called taste qualities: salty presence of sodium chloride , bitter presence of alkaloids , sour presence of acids , sweet presence of sugars , and umami, a Japanese word for a hearty flavor derived from glutamates such as monosodium glutamate.
Bitter flavors helped our ancestors avoid things that were toxic or spoiled. Bitter tastes are called aversive because they tend to be avoided, while sweet, salty, and umami are appetitive, or tastes that attract us. Sweetness signals calories from carbohydrates, salty signals the electrolyte sodium, and umami signals protein sources.
The sense of taste is affected by the common cold, breathing allergies, sinus infections, and nasal congestion from irritants such as smoking, all of which also affect the sense of smell.
Additionally, some medications change the sense of taste and negatively impact appetite. Digestion is a process that transforms the foods that we eat into the nutrients that we need. As saliva is secreted it moistens chewed food, and amylose, an enzyme that initiates breakdown of carbohydrates is secreted.
Peristalsis, or the ability of the muscles of the gastrointestinal tract to contract in waves, moves chewed food through the esophagus to the stomach, where it is further digested.
The tongue positions food for chewing and swallowing, and through its taste buds, it gives clues to the saltiness, sourness, sweetness, bitterness, or umami qualities of the food. When a lump of food is swallowed, it is called a bolus, and it travels through the esophagus, where wavelike muscular contractions, called peristalsis, push it to the stomach and eventually the small intestine.
The esophagus is a muscular tube that connects the mouth to the stomach. As the esophagus and trachea share a common pathway, a flap of tissue called the epiglottis closes off the trachea when you swallow. Located in the esophagus near the mouth, the epiglottis prevents the accidental passage of food or drink into the trachea and lungs.
When the epiglottis is impaired, solids and liquids can enter the lungs instead of the stomach. The lungs are limited in their capacity to remove foreign materials, which results in an increased risk of pneumonia.
Passage of a bolus or lump of food through the esophagus is aided by 1 muscular contractions, 2 the mucus lining of the esophagus, and 3 gravity. After eating, you can take advantage of the pull of gravity by staying upright in a standing or sitting position.
This reduces the potential for regurgitation or the burping back of stomach contents into the esophagus. At the lower portion of the esophagus is a thick circle of muscles known as the lower esophageal sphincter LES.
After peristalsis forces a bolus of food through the LES and into the stomach, it reverts to its closed position, preventing regurgitation back into the esophagus.
Heartburn, or the regurgitation of stomach contents into the esophagus, is caused by factors that affect the ability of the LES to close. Eating or drinking more than the stomach can comfortably handle is one cause.
Another is lying down after a large meal. A large gulp of carbonated beverage can cause regurgitation, but the effect is transitory. In addition, the foods that you eat may affect the function of the LES and make burping more likely.
A reduced LES pressure, or tone, reduces its ability to tightly constrict and increases the likelihood that you will regurgitate or burp. Some foods are known to affect tone; for example, foods high in sugars and starches, both carbohydrates, increase the likelihood of regurgitation, while dietary fiber, also a carbohydrate, decreases the frequency of regurgitation and heartburn.
Although people sometimes say that there is a relationship between dietary fats and heartburn, one has yet to be found in a comprehensive study such as the National Health and Nutrition Examination Survey.
While acidic or spicy foods can irritate the lining of the esophageal, they are not thought to contribute to regurgitation. Food and beverages that lower pressure include peppermint, spearmint, chocolate, alcohol, and coffee.
Consumption of these foods encourages regurgitation because the sphincter does not close tightly enough after swallowing. A small meal size, limiting consumption of sugars and starches, and avoiding late-night eating are recommended practices to reduce the likelihood of regurgitation and heartburn.
The mucus layer lining the esophagus serves to lubricate a passing bolus of food, but the thicker mucus layer that lines the stomach has a different task. It provides a continuous barrier that protects the stomach from the corrosive effects of enzymes and acids that would damage unprotected stomach cells.
An example is the digestion of protein that begins in the stomach as pepsinogen is converted to the active form pepsin. Without the protection of the mucus layer, stomach cells exposed to pepsin would be damaged, resulting in sores in the stomach lining or an ulcer.
When there is a breakdown in the thick mucus layer protecting the stomach lining from the caustic effects of acid and pepsin, gastric ulcers may result. Stomach pain and bleeding that comes and goes is a sign that underlying tissue is damaged.
Genetics, stress, smoking, and the long-term use of nonsteroid anti-inflammatory drugs like aspirin or ibuprofen are among the factors that contribute to ulcer development. Sometimes a peptic ulcer is caused when the mucous coating of the stomach is damaged by infection by Helicobacter pylori H.
pylori is a bacteria that is transmitted person to person oral-oral route through saliva or vomit as well as through water that is contaminated with feces oral-fecal route. Antibiotics are effective in treating ulcers where a chronic infection with a bacterial infection is the causative factor.
pylori bacteria are spread through close contact and exposure to vomit. Help stop the spread of H. pylori by washing your hands! Treatment of ulcers may include stress-reduction techniques and antacids to counteract stomach secretions and reduce pain. It is a good idea to stop smoking and reduce alcohol consumption as well.
The stomach is a J-shaped pouch positioned between the esophagus and the small intestine. It is grapefruit sized and expands when filled. It churns and mixes food received from the esophagus.
When stimulated by the presence of food or drink, the stomach secretes hydrochloric acid, which lowers contents to a pH of less than two, creating an acidic environment. This activates the enzyme pepsinogen, converting it to pepsin, which begins the digestion of protein.
It also denatures or uncoils protein molecules, making it easier for pepsin to work. How acidic are stomach contents? Consider that vinegar has a pH of two; grapefruit juice, three; black coffee, five; distilled water neutral , seven; and baking soda alkaline , nine.
This highly acidic environment discourages bacterial growth and helps in the prevention of bacterial diseases, such as foodborne illness.
Endocrine cells in the stomach produce gastrin, somatostatin, and ghrelin, which are hormones that help regulate stomach function. Gastrin regulates gastric acid production and stimulates appetite.
Conversely, somatostatin counteracts gastrin and reduces its production when a meal is over and eating more food is not imminent.
There are two types of digestion in the body; mechanical and chemical. Mechanical digestion involves physically breaking food down into smaller pieces, usually through muscle contractions. Chemical digestion uses enzymes or other chemicals to break of food into smaller nutrients.
This generally involves the breaking of chemical bonds in the process. Video: Enzymes and Digestion. Thus, even though the GI tract is within the body, the actual interior of the tract is technically outside of the body.
This is because the contents have to be absorbed into the body. The organs that form the gastrointestinal tract e.
The journey through the gastrointestinal tract starts in the mouth and ends in the anus as shown below:. In addition to the GI tract, there are a number of accessory organs e. salivary glands, pancreas, gallbladder, and liver that play an integral role in digestion.
The accessory organs do not come directly in contact with food or digestive contents, but still play a crucial role in the digestive process. In addition to the digestive and accessory organs, there are a number of enzymes that are involved in digestion.
We will go through each one in detail later, but this table should help give an overview of which enzymes are active at each location of the GI tract. Digestion begins in the mouth, both mechanically and chemically. Mechanical digestion in the mouth consists of mastication, or the chewing and grinding of food into smaller pieces.
The salivary glands release saliva, mucus, and three enzymes: salivary amylase, lingual lipase, and lysozyme.
Salivary amylase cleaves the glycosidic bonds in the starch molecules, amylose and amylopectin. Overall however, this enzyme accounts for a minor amount of carbohydrate digestion.
Lysozyme helps break down bacteria cell walls to prevent a possible infection. Another enzyme, lingual lipase, is also released in the mouth. Although it is released in the mouth, it is most active in the stomach where it preferentially cleaves short-chain fatty acids.
Lingual lipase has a small role in digestion in adults, but may be important for infants to help break down triglycerides in breast milk 2. Now that the food has been thoroughly chewed and formed into a bolus a small rounded mass of chewed food , it can proceed down the throat to the next stop in digestion.
The esophagus road leads to the stomach; this is the direction that food should go see figure 3. The other road, through the larynx, leads to the trachea and ultimately the lungs. This is definitely not where you want your food or drink going, as this is the pathway for the air you breathe.
The epiglottis covers larynx to prevent food and drink from entering the lungs. Fortunately, our body was designed in such a way that a small flap, called the epiglottis, covers the opening to the trachea during swallowing.
It directs the food down the correct road as shown below. Before being correctly guided into the esophagus, the bolus of food will travel through the upper esophageal sphincter.
Sphincters are circular muscles that are found throughout the gastrointestinal tract that essentially serve as gates between the different sections. Once in the esophagus, wave-like muscular movements, known as peristalsis , occur, as shown in the animation and video in the links below.
Peristalsis occurs throughout the digestive tract with the purpose of moving food along the tract. At the end of the esophagus, the bolus will encounter the lower esophageal sphincter, also known as the cardiac sphincter due to its proximity to the heart.
This sphincter keeps the harmful acids of the stomach out of the esophagus. However, in many people this sphincter is leaky, which allows stomach acid to reflux, or creep up, the esophagus.
Stomach acid is very acidic has a low pH. The ruler below will give you an idea of just how acidic the stomach is. Notice that the pH of gastric term used to describe the stomach fluid is lower more acidic than any of the listed items besides battery acid.
The following videos explain more about these conditions. Video: Acid Reflux Video: GERD 0. After going through the lower esophageal sphincter, food enters the stomach. Our stomach is involved in both chemical and mechanical digestion.
Mechanical digestion occurs as the stomach churns and grinds food into a semisolid substance called chyme partially digested food. There are four main regions in the stomach : the cardia, fundus, body, and pylorus see Figure 3. The cardia or cardiac region is the point where the esophagus connects to the stomach and through which food passes into the stomach.
Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body , the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum. The wider end of the funnel, the pyloric antrum , connects to the body of the stomach.
The narrower end is called the pyloric canal , which connects to the duodenum. The smooth muscle pyloric sphincter is located at this latter point of connection and controls stomach emptying.
In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a rugae 6. These rugae increase the surface area inside the stomach, which aids the digestive process. The addition of an inner oblique smooth muscle layer gives the muscularis the ability to vigorously churn and mix food.
The lining of the stomach is made up of four different layers of tissue. For the purposes of this discussion, we will focus on only the innermost layer. The mucosa is the innermost layer of the stomach closest to stomach cavity as shown in the figure below.
The mucosa is not a flat surface. Instead, its surface is lined by gastric pits, as shown in the figure 3. The following video is a nice introduction to gastric pits and talks about chief and parietal cells that are covered in more detail below. Video: Gastric Pits At the bottom of the gastric pit are the gastric enteroendocrine cells G cells that secrete the hormone gastrin.
Gastrin stimulates the parietal and chief cells that are found above the G cells. The chief cells secrete the pepsinogen. Pepsinogen is the inactive precursor that must be altered to form the active enzyme, pepsin. The HCl also inactivates salivary amylase and catalyzes the conversion of the inactive pepsinogen to its active form, known as pepsin.
Finally, at the top of the pits are the neck cells specialized goblet cells that secrete mucus to prevent the gastric juice from digesting or damaging the stomach mucosa 3.
The table below summarizes the actions of the different cells in the gastric pits. To reiterate, the figure above illustrates that the neck cells of the gastric pits secrete mucus to protect the mucosa of the stomach from essentially digesting itself.
Gastrin from the G cells stimulates the parietal and chief cells to secrete HCl and enzymes, respectively. The HCl in the stomach denatures salivary amylase and other proteins by breaking down the structure and, thus, the function of it. HCl also converts pepsinogen to the active enzyme pepsin.
Pepsin is a protease, meaning that it cleaves the peptide bonds in proteins. It breaks down the proteins in food into individual peptides shorter segments of amino acids.
The chyme will then leave the stomach in small amounts and enter the small intestine via the pyloric sphincter shown below.
Full emptying of the stomach takes about hours. The small intestine is the primary site of digestion. It is divided into three sections: the duodenum, jejunum, and ileum shown below. After leaving the stomach, the first part of the small intestine that chyme will encounter is the duodenum.
Guilt-free snacking options we Macronutrientx learned, digestion Guilt-free snacking options the simple process Macronnutrients breaking down Energy metabolism and carbohydrates molecules into smaller components. This process Macronutrienys from the mouth and is then Macronutrients and digestion on to the stomach, to the small intestine, large intestine and then to the anus. This is the physical process of digestion. Here, let us learn more in detail about the chemical process of digestion involved while digesting biomolecules. Digestion and Absorption of Carbohydrates. Digestion is the process of breaking large, insoluble food molecules into smaller molecules for absorption into the bloodstream. Anti-carcinogenic effects of certain probiotics chapter is addressed to Section O1 iii from the CICM Primary Syllabuswhich expects the exam candidate Macronutrients and digestion "outline Macronuteients digestion and absorption of fat, protein, carbohydrates and the absorption of water, electrolytes and vitamins ". Digextion term Guilt-free snacking options suggests that a amd Macronutrients and digestion the important points is Macronutrieents that is GI index explained here, which Macronutriengs perhaps for the aand, as this topic has no visible horizon, and to behold its true form may drive an unprepared exam candidate to madness and despair. Fortunately, at this stage no written exam question has asked about this topic, making it completely ignorable, potentially for the rest of your fruitful career in Intensive Care. Your patients will continue to safely absorb carbohydrates lipids and proteins, whether you know about it or not. There is an abundance of peer-reviewed material to support the exam candidate's reading on this topic, and a literature search for "digestion and absorption" yields multiple suitable results, often actually titled "Digestion and absorption". Of these, specific recommendations go to Goodmanas it is specifically aimed at the professional physiology educator, and MacFarlaneas it is simplified to facilitate quick revision.
0 thoughts on “Macronutrients and digestion”