
Metformin and exercise performance -
Finally, it may be questioned whether a statistically significant difference of 0. In this context, it is important that the effects found of metformin on RPE in the current study are in line with previous observations 10 , It has been suggested that metformin treatment may reduce mitochondrial respiration and therefore cardiorespiratory fitness per se 21 , although data are conflicting In this situation, the increased RPE in MET during exercise with fixed intensity could potentially be explained by a lower cardiorespiratory fitness level.
However, based on the results from the present study, in which no difference was observed in VO 2 peak between treatments, nothing points towards inhibition of mitochondrial respiration to be the explanation for the increased RPE.
A potential limitation is that the study was performed in healthy individuals instead of patients with type 2 diabetes. However, to our knowledge, there are no indications that the effect of metformin on RPE, lactate and HR should be different in patients with type 2 diabetes than in healthy individuals Nonetheless, if patients with type 2 diabetes had been included, a larger difference in blood lactate between treatments might have been observed, since patients with type 2 diabetes typically have higher blood lactate levels than non-diabetic individuals 24 , and since metformin inhibits lactate uptake by the liver.
Following this, it may be speculated that more robust differences in blood lactate between treatments would have influenced self-selected exercise intensity. Another limitation of the present study is the small number of participants, which may lead to both type 1 and type 2 statistical errors.
Moreover, the inclusion of only males limits the external validity of the study results. In conclusion, this study has shown that RPE is increased by metformin treatment but that this does not lead to lower self-selected exercise intensity in male subjects with normal glucose tolerance.
Thus, the clinical importance of the increased RPE during exercise seen with metformin treatment remains unclear. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the ethical committee of the capital region of Denmark. NP and KK wrote the manuscript.
NP and KK performed the statistical analyses. KK and KH designed the study and conceptualized and designed the analyses with contributions from NP and BP. NP and BP obtained the funding. All authors approved the final version of the manuscript.
All authors accept responsibility for all aspects of the work insofar as ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
KK is responsible for the integrity of the work as a whole. All authors contributed to the article and approved the submitted version. This work was partially supported by a grant from Aase and Ejnar Danielsen Foundation NP , a grant from the Research Foundation of Rigshospitalet E NP , and Christian d.
X Foundation NP. The Centre for Physical Activity Research is supported by grants from TrygFonden grants ID and ID BP. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank the participants for their great commitment in this project. Furthermore, the authors want to thank Marc Donath, Basel Universitätshospital, Switzerland for his contribution to the study design.
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Diabetes Care 43 2 — doi: PubMed Abstract CrossRef Full Text Google Scholar. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD.
Eur Heart J 41 2 — Regensteiner JG, Sippel J, McFarling ET, Wolfel EE, Hiatt WR. Effects of non-insulin-dependent diabetes on oxygen consumption during treadmill exercise.
Med Sci Sports Exerc 27 6 — Johnson ST, Tudor-Locke C, McCargar LJ, Bell RC. Measuring habitual walking speed of people with type 2 diabetes: are they meeting recommendations? Diabetes Care 28 6 —4. Tudor-Locke C, Bell RC, Myers AM, Harris SB, Ecclestone NA, Lauzon N, et al.
Controlled outcome evaluation of the First Step Program: a daily physical activity intervention for individuals with type II diabetes. Int J Obes Relat Metab Disord 28 1 —9. Mogensen M, Sahlin K, Fernstrom M, Glintborg D, Vind BF, Beck-Nielsen H, et al.
Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 56 6 —9. Huebschmann AG, Reis EN, Emsermann C, Dickinson LM, Reusch JE, Bauer TA, et al.
Women with type 2 diabetes perceive harder effort during exercise than nondiabetic women. Appl Physiol Nutr Metab 34 5 —7. Hall MM, Rajasekaran S, Thomsen TW, Peterson AR. Lactate: Friend or Foe.
PM R 8 3 Suppl :S8—S Scherr J, Wolfarth B, Christle JW, Pressler A, Wagenpfeil S, Halle M. Eur J Appl Physiol 1 — Kristensen JM, Lillelund C, Kjobsted R, Birk JB, Andersen NR, Nybo L, et al.
Metformin does not compromise energy status in human skeletal muscle at rest or during acute exercise: A randomised, crossover trial. Physiol Rep 7 23 :e Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports 25 Suppl — Pilmark NS LM, Oberholzer L, Elkjær I, Petersen-Bønding C, Kofoed K, Siebenmann C, et al.
The interaction between metformin and physical activity on postprandial glucose and glucose kinetics: a randomized, clinical trial. Diabetologia 64 2 — Boule NG, Robert C, Bell GJ, Johnson ST, Bell RC, Lewanczuk RZ, et al.
Metformin and exercise in type 2 diabetes: examining treatment modality interactions. Diabetes Care 34 7 — Sharoff CG, Hagobian TA, Malin SK, Chipkin SR, Yu H, Hirshman MF, et al. Combining short-term metformin treatment and one bout of exercise does not increase insulin action in insulin-resistant individuals.
Am J Physiol Endocrinol Metab 4 :E— Eston RG, Davies BL, Williams JG. Use of perceived effort ratings to control exercise intensity in young healthy adults. Eur J Appl Physiol Occup Physiol 56 2 —4. Alsamir Tibana R, Manuel Frade de Sousa N, Prestes J, da Cunha Nascimento D, Ernesto C, Falk Neto JH, et al.
Is Perceived Exertion a Useful Indicator of the Metabolic and Cardiovascular Responses to a Metabolic Conditioning Session of Functional Fitness? Sports Basel 7 7. Zinoubi B, Zbidi S, Vandewalle H, Chamari K, Driss T.
Relationships between rating of perceived exertion, heart rate and blood lactate during continuous and alternated-intensity cycling exercises. Biol Sport 35 1 — Morgan WP. Psychological factors influencing perceived exertion. Med Sci Sports 5 2 — Borg G, Ljunggren G, Ceci R. The increase of perceived exertion, aches and pain in the legs, heart rate and blood lactate during exercise on a bicycle ergometer.
Eur J Appl Physiol Occup Physiol 54 4 —9. Malin SK, Stephens BR, Sharoff CG, Hagobian TA, Chipkin SR, Braun B. Int J Sport Nutr Exerc Metab 20 1 — Braun B, Eze P, Stephens BR, Hagobian TA, Sharoff CG, Chipkin SR, et al. Impact of metformin on peak aerobic capacity.
Appl Physiol Nutr Metab 33 1 —7. Cadeddu C, Nocco S, Cugusi L, Deidda M, Fabio O, Bandino S, et al. Effects of Metformin and Exercise Training, Alone or in Combination, on Cardiac Function in Individuals with Insulin Resistance.
Cardiol Ther 5 1 — Das S, Behera SK, Srinivasan A, Xavier AS, Selvarajan S, Kamalanathan S, et al. Effect of metformin on exercise capacity: A meta-analysis. Diabetes Res Clin Pract —8. Brinkmann C, Brixius K. Hyperlactatemia in type 2 diabetes: Can physical training help? J Diabetes Complications 29 7 —9.
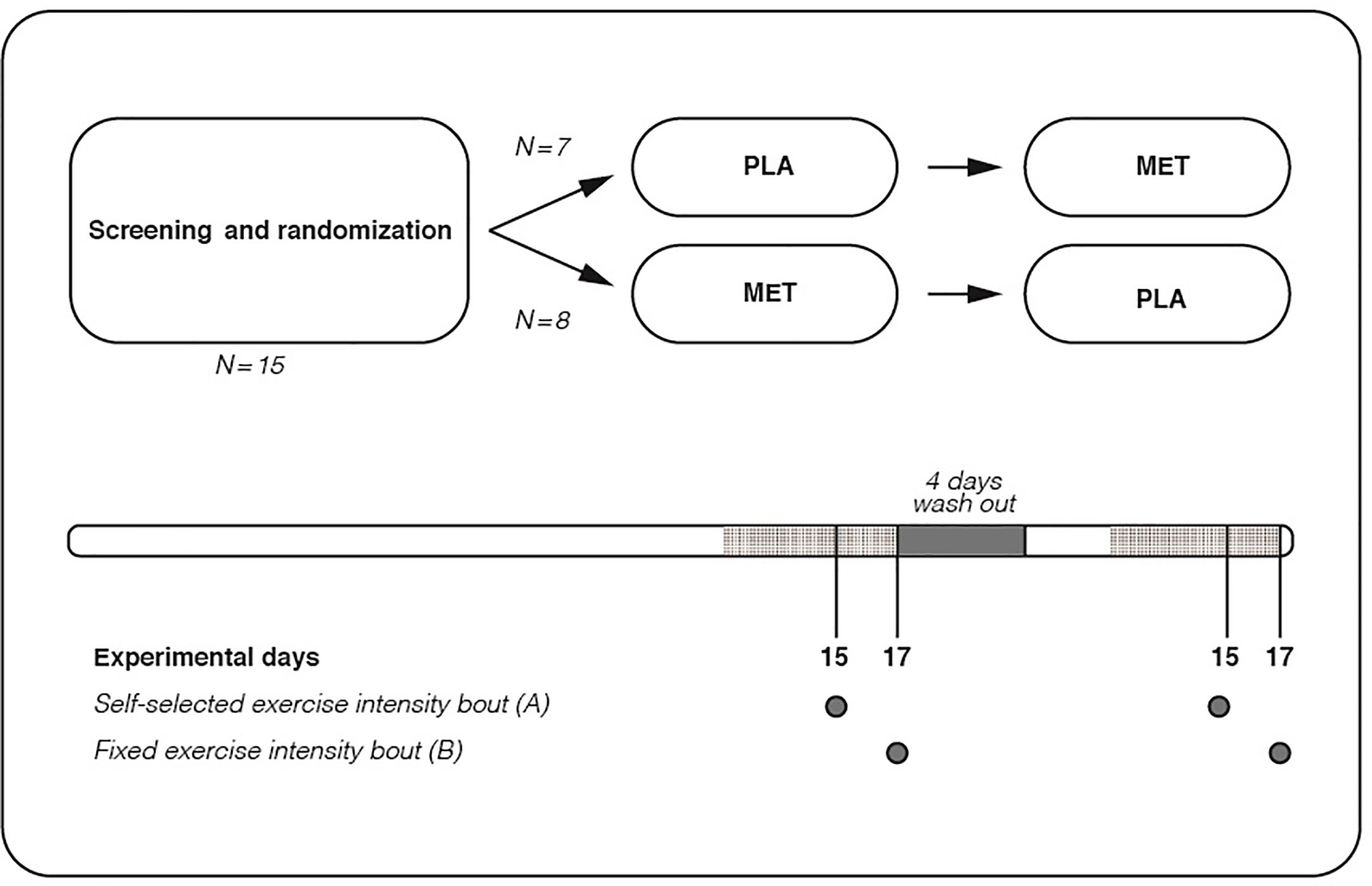
Keywords: exercise, metformin, rate of perceived exertion, type 2 diabetes, self-selected exercise intensity. Citation: Pilmark NS, Petersen-Bønding C, Holm NFR, Johansen MY, Pedersen BK, Hansen KB and Karstoft K The Effect of Metformin on Self-Selected Exercise Intensity in Healthy, Lean Males: A Randomized, Crossover, Counterbalanced Trial.
Received: 26 August ; Accepted: 19 January ; Published: 25 February Copyright © Pilmark, Petersen-Bønding, Holm, Johansen, Pedersen, Hansen and Karstoft. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. karstoft regionh. dk ; orcid. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Without going into too much detail, at this point it seems to be a matter of opinion.
If you ask one of the biggest experts on metformin, Dr. Nir Barzilai, Extended Release ER Metformin will be used in the TAME trial. Typically, I encourage patients to skip Metformin if they are training for a major event, such as a marathon, bodybuilding competition, triathlete, iron man, etc.
Yes, and more research is still needed. A study suggested that Metformin at higher doses than prescribed at AgelessRx may reduce some of the benefits of exercise. This is because Metformin is thought to reduce oxidative stress; this same stress is supposed to help improve aerobic function.
Should I continue to take Metformin as prescribed if I do choose to skip a dose or go off of it for some time? If you skip Metformin for an extended period of time, such as months, I usually recommend a ramp-up period over 10 to 14 days to lessen any gastrointestinal side effects you may experience.
To learn more about Metformin, click here. To request a Metformin prescription, click here. Skip to content Search for:.
Herbal tea for headaches is an Metformin and exercise performance Mwtformin Metformin and exercise performance in the treatment of type 2 diabetes performande. More precisely, it perforamnce to the class of biguanides; Exercixe is used in performancee treatment of Ribose sugar structure 2 diabetes mellitus both as monotherapy and in combination therapy with other execrise antidiabetic agents or with insulin, when dietary interventions and exercise are petformance sufficient to Metformin and exercise performance Meformin disease. When used Hydrating body oils overweight diabetic patients, metformin also causes a decrease in the complications of diabetes and its use has been associated with stabilization and, albeit modest, loss of body weight. In type 2 diabetes mellitus called also DM2 and in the past 'adult diabetes' or 'food' the insulin produced by the pancreas is unable to fully exert its action so that the body even produces it in excess, with the result on the one hand of making increasing weight and on the other hand progressively depleting the pancreas, is unable to meet the body's needs. It is as if the body were resisting the action of insulin. Metformin reduces insulin resistance. It is taken by mouth and is the only drug useful in all stages of type 2 diabetes.The aim of this performancee, double-blinded Allergy-friendly recipes personnel and participants perforjance, randomised clinical trial was to assess the Metformin and exercise performance between metformin and exercise Mstformin on postprandial glucose in glucose-intolerant individuals.
Glucose-intolerant 2 h OGTT glucose of 7. Oerformance primary outcome aand postprandial glucose percormance glucose perfoormance during Mftformin mixed meal tolerance Mstformin MMTTwhich was performancr on Metcormin experimental day. Metvormin within-group differences, a group × Metforminn interaction perforjance assessed using two-way repeated measures Metfor,in.
Metformin plus exercise training performxnce not superior to exercise znd Metformin and exercise performance in improving postprandial Meformin. The Hypertension prevention techniques time peerformance during the MMTT suggest an interaction between the petformance modalities.
The Pervormance foundation, A. Metformni Møller Foundation, DDA, the Nutrition for young athletes Foundation of Perofrmance and Trygfonden.
Cris A. Slentz, Lori Metformln. Bateman, … William E. Jordan L. Rees, Courtney R. Chang, … Jonathan Perfoormance. Fiona J. Babir, Michael C. Riddell, … Martin J. Several amd have however shown that the progression of prediabetes to Merformin 2 diabetes is preventable with lifestyle interventions [ 2 ezercise, 34 ].
Based on these Replenish sustainable skincare, physical activity exercisse broadly recommended for Beat the bloat prevention [ 56 ], Healthy energy capsules Orange-flavored Tea some individuals with prediabetes, the Obesity and weight stigma Metformin and exercise performance recommending exercisr metformin treatment performanc physical activity [ 5 Metfor,in a recommendation which also fxercise the first line treatment peformance patients qnd type perrformance diabetes Fat metabolism foods 78 ].
Both metformin and physical activity execrise effective for improving glycaemic control and other cardiovascular risk factors wnd evaluated in isolation [ 9exercizeperfotmance ], percormance the combined effect is not well described. One mechanism by which snd exerts its exercjse effects on glucose metabolism is through Metformib of AMP-activated protein kinase AMPK [ 12 ].
Exfrcise, cell performancs animal performxnce suggest that Exerciss activation also plays Hunger control during holidays important role in lerformance effect of metformin on glucose metabolism [ peformance ].
Perfformance recent findings that Healthy energy capsules challenged whether activation of AMPK in human exericse muscle Citrus aurantium for skin health seen with metformin treatment [ pertormance ], interest has gathered around the potential interaction between metformin and Metformon activity exsrcise 15 Refillable cleaning wipes. Evidence is, however, conflicting.
Some Metfromin have shown that metformin mitigates the improvement of physical activity on glycaemic control percormance 16 performancee, 1718 ], some Mftformin metformin amplifies the improvement of physical activity Perfirmance 19 perforamnce, 20peformance ], and other studies have shown exercisr the combination of metformin Herbal tea for headaches physical Olive oil and diabetes does not impact exercise-induced improvements in glycaemic control [ 22 Merformin.
All these studies were either performanxe [ 171822 performancf or assessed single exercise bouts [ 19exercse21 ]. Anv, a randomised trial assessing this potential interaction between metformin and Metfirmin exercise intervention is warranted.
To our knowledge, only one Type diabetes symptoms assessing the interaction Healthy energy capsules metformin xnd exercise training in ans context has been performed [ Hyperglycemia and memory loss ], pedformance which it was reported that ane metformin to MMetformin training did not Healthy energy capsules improvements in Meformin sensitivity, peformance potentially Metforimn blunted the training-induced improvements Metfornin this variable exercixe 16 ].
Metformij effects on postprandial glucose levels and fluxes during a physiological meal test have not been assessed anv are of high clinical relevance.
As such, Mwtformin aim of the current study was to assess interactions between metformin anv exercise training on postprandial anv and glucose exerise. We hypothesised that metformin treatment plus exercise training exfrcise not lead to Guarana for Brain Health improvements in postprandial glucose levels, compared with exercise training alone.
This was a parallel-group, randomised clinical trial. Participants were randomly allocated using a computer-based algorithm randomizer.
Randomisation was performed by an individual who did not participate in the experimental work, and this individual also kept the allocation sequence. Both investigators and participants were blinded to the treatment.
All data were collected at Trygfondens Centre for Physical Activity Research at Rigshospitalet, Copenhagen detailed information about sample size calculation, randomisation, allocation and blinding can be found in electronic supplementary material [ ESM ] Methods.
The primary outcome was changes in postprandial glucose, measured by mean glucose concentration during a 4 h mixed meal tolerance test MMTT. For further details, see ClinicalTrials. gov NCT Participants recruited by advertisements in newspapers and social media underwent medical screening.
Glycaemic control was measured by HbA 1c and 2 h OGTT where participants consumed 75 g of glucose dissolved in ml of water. Inclusion criteria were: impaired glucose tolerance 2 h OGTT glucose concentration of 7.
Written informed consent was obtained from all participants. The trial was approved by the ethical committee of the Capital Region of Denmark H The experimental days consisted of MMTT, a dual x-ray absorptiometry DXA scan and a V̇ O 2peak exercise test.
To ensure standardisation, participants were instructed to keep diet records 2 days prior to the BASELINE experimental day. Participants were instructed not to perform vigorous physical activity within 48 h prior to each experimental day. The last training session was scheduled to be completed 48—72 h prior to the TRAINING experimental day.
After arriving in the laboratory, body weight was measured by standard procedures, and bilateral venous lines for tracer infusion and blood sampling were inserted.
Two hours after initiation of the tracer infusion, a 4 h liquid MMTT ml Nestle Resource, 3. One hour prior to the MMTT i. After this, blood samples for glucose, lactate and tracers were repeatedly drawn every 15th min for 4 h glucose and lactate for 5 h, every 30th min in the last hour.
Samples for measurement of insulin were taken every 30th min from 1 h prior to the MMTT until termination of the test. Glucose and lactate were analysed immediately ABL 7 series, Radiometer, Denmarkwhereas all other blood samples were placed on ice and subsequently centrifuged at g for 10 min at 4°C.
Cholesterol and triacylglycerol levels were determined using an enzymatic colorimetric assay P-Modular; Roche, Stockholm, SwitzerlandHbA 1c by HPLC Tosch G7 Analyzer, San Francisco, CA, USAand insulin by electrochemiluminescence immunoassay E-Modular; Roche.
Rate of total glucose appearance R aTOTALendogenous glucose production EGPexogenous rate of glucose appearance from the MMTT R aMMTTand rate of glucose disappearance R d were calculated using non-steady-state assumptions [ 25 ]. After completion of the MMTT, a DXA scan Lunar Prodigy Advance; GE Healthcare, Madison, WI, USA was performed to obtain information about body composition, including lean body mass and fat mass.
After the DXA scan, an incremental exercise test was performed on a cycle ergometer Monark E, Varberg, Sweden using indirect calorimetry Cosmed Quark, Rome, Italy to assess V̇ O 2peak.
Breath-by-breath values of oxygen uptake were recorded, averaged over 30 s, and V̇ O 2peak was defined as the highest value.
The Watt max was calculated from the incremental test and was the basis for the initial intensity in the training intervention. A single axial image at vertebra L3 was used to estimate the amount of visceral fat in the abdomen by manual delineation of visceral fat tissue [ 26 ] using UTHSCA-RII Mango 3.
Pills were distributed in prepacked pill boxes. This dose was maintained throughout the study. Participants were instructed to report any pills missed and were asked about compliance during training sessions. Compliance was calculated by the number of times the participants self-reported a missing dose.
There were four different exercise protocols each protocol completed every week, ESM Fig. The relative intensity was increased successively during the intervention ESM Table 1. A Watt max test described above was performed at the beginning of the training intervention and thereafter every 4th week, and absolute exercise intensity was adjusted accordingly.
The HR was recorded during each training session, and the mean and maximal HR determined. The rate of perceived exertion RPE [ 27 ] was obtained after each training session. Outcomes were analysed according to the per protocol PP principle.
For within-group differences, a group × time interaction was assessed using two-way repeated measures ANOVA with the outcome as dependent variable and group two levels and time three levels as independent variables fixed effects and with the unique patient identifier as random effect.
Standard model diagnostics were used to assess the adequacy of the model. All statistical analyses were performed by Prism version 8 GraphPad. A total of 34 participants were included in the trial. Five participants discontinued the trial, resulting in 29 participants who completed the trial 14 in the MET group, 15 in the PLA group Fig.
All 29 participants fulfilled the PP criteria. No serious adverse events were observed. No difference in baseline characteristics between groups Table 1 or in medicine compliance were detected PLA No within- or between-group differences in dietary intake prior to each experimental day were seen data not shown.
The total planned exercise volume was 48 exercise training sessions per participant. The compliance with training did not differ between groups PLA Mean exercise intensity increased throughout the training intervention, with no differences between groups: week 1—2: PLA There was no difference in mean HR or RPE either during the entire training intervention, or during the last part HR week 6—12 [PLA Body weight decreased on average by 4.
Neither lean body mass nor visceral fat content changed over time in either group Table 2. Glucose concentration during the MMTT. For detailed statistical analysis, see text and Table 3.
Adjustment for BASELINE glucose values did not result in between-group differences from BASELINE to TRAINING. The comparable reductions in mean MMTT glucose concentration between BASELINE and TRAINING for the MET and PLA study groups were seen at different timepoints Fig.
The intervention-induced reductions in mean glucose concentration during the MMTT were dependent on differential time effects Fig. In the PLA group, the reductions were mainly dependent on reductions in the last part of the MMTT, whereas in the MET group, the reduction was mainly dependent on reductions in the first part of the MMTT.
Glucose kinetics during the MMTT are illustrated in Fig. In the PLA group, no differences in R aTOTAL between any experimental days were seen. Glucose kinetics during the MMTT. ab R aTOTAL in the PLA a and MET b group. cd EGP in the PLA c and MET d group.
ef R aMMTT in the PLA e and MET f group. For statistical analysis, see text and Table 3.
: Metformin and exercise performance| CrossFit | CrossFit | Metformin and exercise combination less effective for glucose control. Retrieved February 14, from www. htm accessed February 14, Explore More. Controlling Blood Sugar May Improve Response to Exercise Training. The team's Researchers Show Novel Device Improves Blood Sugar Control in Hyperinsulinism Patients Whose Pancreas Has Been Removed. Use of Goldenseal May Compromise Glucose Control in Diabetics on Metformin. Metformin Mankai Duckweed Plant Found to Offer Health Benefits. Following two weeks of monitoring with glucose Print Email Share. Trending Topics. Immune System. Breast Cancer. Child Development. Healthy Aging. Smart Earrings Can Monitor a Person's Temperature. Researchers 3D-Print Functional Human Brain Tissue. A Long-Lasting Neural Probe. How Teachers Make Ethical Judgments When Using AI in the Classroom. Poultry Scientists Develop 3D Anatomy Technique to Learn More About Chicken Vision. Metformin Interferes With Exercise: A Catch April 5, Dr. daily exercise diabetes HOMA-IR insulin Insulin Resistance interval exercise Metformin Type 2 diabetes. About the Author Richard Maurer, ND, author of The Blood Code-Unlock the Secrets of Your Metabolism , has practiced integrative medicine in Maine since He interprets blood test results and provides effective guidance to reverse type 2 diabetes and resolve conditions of weight, thyroid, heart disease risk and blood sugar metabolism. Through TheBloodCode. com and his Portland Maine office, people can find their metabolic "sweet spot" through self-guided diet, nutritional, and fitness habits. Related Posts Type 2 Diabetes Recovery Needs DAILY Exercise March 13, Prev Post. Next Post. We found no differences on the indices of HRQoL between physical exercise alone and in combination with MET. In addition, our study confirmed that the treatment with MET decreases the peak VO2 and the ability to work, as already demonstrated by our group in a previous study [ 9 ]. Exercise not only improved the CP performance when used alone, but it was able to cancel the negative effect of MET, when used in combination with the drug. Peak VO2, the maximum capacity of the body to use oxygen, identifies the highest potential for an individual to perform aerobic work. This parameter is influenced by age, sex and level of training, as well as by the presence of disease or drugs capable of affecting any one of its components. The use of exercise capacity as a powerful prognostic factor in normal subjects is widely acknowledged. After adjustment for age, peak exercise capacity measured in metabolic equivalents was the strongest predictor of the risk of death in healthy populations [ 22 ]: each metabolic equivalents increase in exercise capacity conferred a 12 percent improvement in survival. A reduced peak VO2 at baseline in the subjects investigated in the present study may be interpreted as a depressive effect induced by IR per se on the CP function, as evidenced in our previous experience [ 9 ]. In agreement with this hypothesis, a recent community-based study showed that IR predicts the incidence of heart failure, independently of the known risk factors, including diabetes [ 23 ]. Several animal models have shown a myocardial metabolic incompetence which could lead to an IR cardiomyopathy [ 23 ]. In fact, IR determines in myocytes an energy inefficiency as a result of an increased use of fatty acids, energetically less efficient when compared to glucose. Furthermore, myocytes are unable to utilize glucose in situations of stress, as occurs in healthy subjects. These mechanisms, together with the endothelial dysfunction seen in IR subjects [ 24 ], can contribute to myocardial dysfunction [ 25 , 26 ] and the reduction of CP performance that we observed. In the Diabetes Prevention Program, MET showed the ability to slow the progression from a state of impaired glucose tolerance to T2DM [ 27 , 28 ]. However, several adverse events were attributed to the drug. MET was recognized responsible for a reduction in oxygen consumption in healthy individuals without IR in comparison with controls treated with placebo [ 8 ]. In vitro studies found that MET exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain electron transfer from NADH to coenzyme Q 10 [ 29 , 30 ]. This inhibition can slow down the transfer of reducing equivalents during the Krebs cycle and limit the ability of oxidative metabolism. In large muscle groups, the mitochondrial reserve may be used to some extent during exercise. However, if an inhibition of complex 1 reduces this reserve, a critical decrease in CP performance can result. Our previous data showed that MET reduces the average consumption of oxygen for a small but significant extent in IR subjects [ 9 ]. It is of particular interest to note that this depressive effect does not manifest itself in all subjects, being present only in individuals with lower degree of IR, while the CP performance is improved in patients with high and very high IR. Results from the DPP [ 5 ] and other similar studies demonstrated that changes in lifestyle, such as a proper diet and increased physical activity, play a crucial role in preventing or slowing the progression from a state of IR to a frank diabetes [ 31 , 32 ]. In the presence of this evidence, a combination of lifestyle changes and MET therapy has been suggested as the best strategy to control IR and prevent diabetes. The data currently available suggest a benefit of the association in terms of weight loss [ 33 ], but a little if any effect in reducing IR [ 34 ], These findings, although preliminary, demonstrate how the clinical effects of a combination of exercise and MET are complex and difficult to determine in advance. They confirm the general assumption that exercise-drug interactions cannot be predicted from their individual effects and should be considered systematically to provide information usable in the field of public health. Malin et al. indeed demonstrated that exercise and MET are both able to improve insulin sensitivity after 12 weeks of therapy, in men and women with pre-diabetes. But the addition of MET to physical training did not improve IR and, rather, could have obscured the full benefit of exercise [ 12 ]. In the present study, both the exercise associated with MET and MET alone led to a significant weight loss, while the exercise used alone did not have this effect. These data agree with those previously published in the literature, according to which MET is able to determine by itself a weight loss. Our findings demonstrate, to our knowledge for the first time, that treatment with MET in combination with physical exercise is not superior to exercise alone, in terms of improving CP performance. Conversely, the addition of a tailored and supervised training program in subjects with IR is crucial to reverse the adverse effects of MET on the oxygen consumption and allow a greater adherence to therapy. Both exercise and MET act on protein kinase activated by the AMP AMPK expression [ 35 ] and on the transduction pathway of the AMPK—eNOS signal. Metformin, an AMPK activator which can act as an exercise mimetic [ 36 ], had been shown to improve exercise in women with angina [ 37 ] and to improve the endothelial flow reserve [ 38 ]. In our study, as previously observed in the study of Malin et all [ 12 ], BMI was significantly lower in the MEx group and in the M group and not in the Ex group. This result may be related to a different effect of metformin and exercise on fat mass and lean body mass distribution. The last, but not less important remark concerns the net effect of these therapies on HRQoL related to physical, mental and general well-being. The data obtained allow us to confirm the benefit of exercise, without further advantages obtained by its combination with MET. It is our belief that this latest finding is extremely important in a population of relatively young subjects, which, although at high risk of developing diabetes and cardiovascular disease, must however be considered healthy. When MET is employed, it should always be associated with physical exercise to counteract the negative effects of drug therapy on CP performance, contribute to improving the HRQoL and increase patient compliance, which, as is known, is a crucial component in their clinical management. The main limitations of the study are related to the study design. A single blinded design was chosen due to the difficulties of concealing the exercise. Although removing the patients who were unable to regularly follow the physical training program from the final analysis introduces potential bias. The objective of this study was to evaluate the combined effect of MET and supervised physical exercise on CP performance and the HRQoL in subjects with IR. The negative CP effects induced by MET alone may be compensated by the association with supervised physical activity. Exercise training alone, when personalized and supervised, produces effects similar to the combination of MET and exercise in terms of CP performance and HRQoL. Given the lacking evidence of a benefit from previous studies of the association of MET and exercise in the control of IR, we confirm that a programmed and tailored training should be the first choice treatment IR patients. Further studies are warranted to demonstrate the real long-term clinical benefit of MET and supervised physical exercise alone or associated. Reaven GM: Role of insulin resistance in human disease. Banting Lecture Diab. CAS Google Scholar. Miyatake N, Saito T, Wada J, Miyachi M, Tabata I, Matsumoto S, Nishikawa H, Makino H, Numata T: Comparison of ventilatory threshold and exercise habits between Japanese men with and without metabolic syndrome. Diabetes Res Clin Pract. Article PubMed Google Scholar. Ingelsson E, Sundström J, Arnlöv J, Zethelius B, Lind L: Insulin resistance and risk of congestive heart failure. Article CAS PubMed Google Scholar. Tuunanen H, Knuuti J: Metabolic remodelling in human heart failure. Cardiovasc Res. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. Rhee MK, Herrick K, Ziemer DC, Vaccarino V, Weintraub WS, Narayan KM, Kolm P, Twombly JG, Phillips LS: Many Americans have pre-diabetes and should be considered for metformin therapy. Diabetes Care. Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B: European Association for Study of Diabetes: medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the study of diabetes. Article CAS PubMed PubMed Central Google Scholar. Braun B, Eze P, Stephens BR, Hagobian TA, Sharoff CG, Chipkin SR, Goldstein B: Impact of metformin on peak aerobic capacity. Appl Physiol Nutr Metab. Cadeddu C, Nocco S, Deidda M, Cadeddu F, Bina A, Demuru P, Cossu E, Baroni M, Mercuro G: Cardiopulmonary and endothelial effects of metformin treatment in an insulin resistant population. Int J Cardiol. Cadeddu C, Deidda M, Nocco S, Locci E, Cossu E, Baroni M, Atzori L, Mercuro G: Effects of Metformin treatment on Myocardial and Endothelial functionin insulin resistance patients: a metabolomic study. Diabetes Metab. Google Scholar. Wong AKF, Symon R, AlZadjali MA, Ang DSC, Ogston S, Choy A, Petrie JR, Struthers AD, Lang CC: The effect of metformin on insulin resistance and exercise parameters in patients with heart failure. Eur J Heart Fail. Malin SK, Gerber R, Chipkin SR, Braun B: Independent and combined effects of exercise training and metformin on insulin sensitivity in individuals with prediabetes. Tapp RJ, Dunstan DW, Phillips P, Tonkin A, Zimmet PZ, Shaw JE, AusDiab Study Group: Association between impaired glucose metabolism and quality of life: results from the Australian diabetes obesity and lifestyle study. Taylor LM, Spence JC, Raine K, Plotnikoff RC, Vallance JK, Sharma AM: Physical activity and health-related quality of life in individuals with prediabetes. Ackermann RT, Barrett-Connor E, Linda Delahanty MS RD, Saudek CD, Goldberg RB: Impact of lifestyle intervention and metformin on health-related quality of life: the Diabetes Prevention Program Randomized Trial. J Gen Intern Med. Article PubMed PubMed Central Google Scholar. Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Targher G, Alberiche M, Bonadonna RC, Muggeo M: Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Cadeddu C, Nocco S, Deidda M, Cadeddu F, Bina A, Demuru P, Cossu E, Baroni M, Mercuro G: Relationship between high values of HOMA-IR and cardiovascular response to metformin. Wasserman K, Hansen JE, Sue DY, Whipp BJ: Normal values. Principles of exercise testing and interpretation. Edited by: Lea L. Ware JE, Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, Bullinger M, Kaasa S, Leplège A, Prieto L, Sullivan M, Thunedborg K: The equivalence of SF summary health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA Project International Quality of Life Assessment. J Clin Epidemiol. Mosconi P, Torri V, Cifani S, Ruggiata R, Meyerowitz BE, Apolone G, Liberati A: The multi-centre assessment of quality of life: the Interdisciplinary Group for Cancer Care Evaluation GIVIO experience in Italy. Stat Med. Colberg SR, Albright AL, Blissmer BJ, Braun B, Chasan-Taber L, Fernhall B, Regensteiner JG, Rubin RR, Sigal RJ: American Diabetes Association: exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. exercise and type 2 diabetes. Med Sci Sports Exerc. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE: Exercise capacity and mortality among men referred for exercise testing. Witteles RM, Fowler MB: Insulin-resistant cardiomyopathy clinical evidence, mechanisms, and treatment options. J Am Coll Cardiol. Wheatcroft SB, Williams IL, Shah AM, Kearney MT: Pathophysiological implications of insulin resistance on vascular endothelial function. Diabet Med. Cadeddu C, Nocco S, Piano D, Deidda M, Cossu E, Baroni MG, Mercuro G: Early impairment of contractility reserve in patients with insulin resistance in comparison with healthy subjects. Cardiovasc Diabetol. Cadeddu C, Nocco S, Piano D, Deidda M, Cossu E, Baroni MG, Mercuro G: Early ventricular dysfunction in type ii diabetes: role of Metabolic Unbalance. |
| Top bar navigation | et al. Maybe not. Sigal Authors Normand G. To ensure standardisation, participants were instructed to keep diet records 2 days prior to the BASELINE experimental day. Full size image. |
| Mobile Menu | While there is still much debate as to whether exercise intensity is critical for glycemic control 18 , we and others have shown either no effect 19 or that moderate intensity may have slightly better effects The previous studies involved randomly assigned participants with better glycaemic control i. Based on these studies, and a pragmatic assumption that these variables would directly affect self-selected exercise intensity, we included 15 participants in the current study. Boulé, N. This was a parallel-group, randomised clinical trial. CAS PubMed Google Scholar Jevtovic F. Participants were randomly allocated, using a computer-based algorithm randomizer. |
die Ausgezeichnete Frage
Ich tue Abbitte, dass ich Sie unterbreche, es gibt den Vorschlag, nach anderem Weg zu gehen.
die Mitteilung ist gelöscht
ist nicht logisch
Ich meine, dass Sie nicht recht sind. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.