Cholesterol level and stroke prevention -
This study recruited atherothrombotic infarction patients from Tianjin, China, between May and September All patients were categorized into five groups according to TC level quintiles at admission.
Differences in subtypes, severity, risk factors, and outcomes at 3, 12, and 36 months after stroke were compared between these groups. In total, Dependency and recurrence rates were significantly higher at 36 months in patients in the lowest TC level quintile than in those with higher cholesterol levels dependency rates, Moreover, these differences remained after adjustment for age, sex, stroke severity, and Oxfordshire Community Stroke Project classification odds ratios [ORs] for dependency rate, 1.
However, mortality rates after stroke were not significantly different between the groups. These findings suggest that statin treatment for patients with atherothrombotic infarction and low cholesterol levels increase long-term dependency and recurrence rates, but do not increase mortality rates.
It is crucial to highlight the different impact of statin treatment on patients with atherothrombotic infarction and lower cholesterol levels for secondary stroke prevention in China. Peer Review reports. In , stroke was the second most common cause of death and the third most common cause of reduced disability-adjusted life-years worldwide.
Although age-standardized rates of stroke mortality have decreased worldwide in the past two decades, the absolute numbers of annual stroke cases, stroke survivors, related deaths, and the global burden of stroke disability-adjusted life-years are high and are increasing [ 1 , 2 ].
However, stroke has recently become the leading cause of death in rural areas, and the third most common cause of death in urban areas in China [ 3 ]. High total cholesterol TC level is a well-documented risk factor for coronary disease [ 4 , 5 ], but the association between total cholesterol levels and stroke outcome is unclear.
A large numbers of studies indicated that high TC level was associated with better stroke outcomes [ 6 — 8 ], but high TC level was associated with worse outcomes in other studies [ 9 , 10 ].
Low TC levels were associated with hemorrhagic, but not ischemic stroke [ 11 , 12 ]. The recent incidence of stroke in China has increased dramatically, with economic development [ 13 ]; however, a large-scale study of the association between TC level and stroke outcomes is rare in China, especially in patients with atherothrombotic infarction.
Therefore, we aimed to assess the association of low TC level on admission and short-term and long-term stroke outcomes after acute ischemic stroke AIS in patients in China. All consecutive patients with first-ever AIS who were admitted to the Stroke Unit in Tianjin Huanhu Hospital within 72 h of stroke onset between in May and September were recruited to this study.
Cases of transient ischemic attack were excluded from this study, and all atherothrombotic infarction patients classified according to the Trial of Org 10, in Acute Stroke Treatment TOAST for large artery atherothrombotic and small artery occlusion SAO were analyzed in this study [ 15 ].
All patients were treated using statin, and followed up for less than 3 months after AIS and TC level on admission was available. The study was approved by the ethics committee for medical research at Tianjin Huanhu Hospital and the Tianjin Health Bureau, and a written informed consent for each participant was obtained during recruitment.
The detailed information on ischemic stroke subtype, stroke severity, previous history of diseases, stroke risk factors, laboratory examination results, and outcomes at 3, 12, and 36 months after stroke were collected using a standardized questionnaire. Stroke subtypes were defined as total anterior circulation infarct TACI , partial anterior circulation infarct PACI , posterior circulation infarct POCI , and lacunar infarct LACI according to Oxfordshire Community Stroke Project OCSP classification criteria [ 16 ].
Neurological function deficit was defined using the National Institute of Health stroke scale NIHSS , Barthel index BI [ 17 ], and modified rankin scale mRS on admission [ 18 ].
Stroke outcomes were described on the basis of mortality, recurrence, and dependency rates at the short-term at 3 months , medium-term at 12 months , and long-term at 36 months after stroke; outcomes were assessed using face-to-face or telephone follow-up.
Recurrence was defined as new-onset vascular events stroke, myocardial infarction, and venous thrombosis after 30 days of initial stroke in all survivors patients who were followed up using face-to race interviews or telephone calls.
Follow-up was conducted according to a predetermined procedure; the trained neurologists reexamined patients in the outpatient department at 3, 12, 24, and 36 months after stroke. All patients were followed-up by face-to-face interview, but those patients reexamined in the local hospital were followed-up by telephone.
Age is presented as mean standard deviation , and NIHSS, BI, and mRS are presented as median interquartile range. These continuous variables were compared between the five TC groups using one-way analysis of variance ANOVA or Kruskal-Wallis tests.
At the different time periods after stroke, categorical variables, including stroke subtype, stroke severity, risk factors, and outcomes, are presented as number percentage , and the trends were compared using Chi-square tests.
All statistical analyses were performed using SPSS version Of the AIS patients recruited between May and September , patients with cardioembolic stroke, patients with other and undetermined causes and patients without a TC level recorded at admission were excluded, resulting in patients with atherothrombotic infarction that were included.
At 3 months, patients were lost to follow-up, resulting in patients response rate, At 12 months, patients were lost to follow-up, resulting in patients response rate, At 36 months, patients were lost to follow-up, resulting in patients response rate, The lowest TC levels were present in The prevalence of artery stenosis was not significantly different Table 2.
There were no obvious differences in mortality and dependency rates at all time points after AIS between the TC level groups Table 3.
However, the recurrence rate at 3 months was remarkably higher with higher TC levels group 1, 7. The trend in recurrence rates at 36 months after stroke was the opposite to that at 3 months group 1, In this single-center study using a large stroke registry in Tianjin, China, we assessed differences in age, sex, stroke subtype, stroke severity, prevalence of risk factors, and stroke outcomes between patients with atherothrombotic infarction with and without low TC levels.
As a result, a low TC level was an independent risk factor for outcomes in patients with atherothrombotic infarction. A high cholesterol level is a powerful risk factor for coronary heart disease, but its role in stroke remains controversial. Although observational studies have not found a clear association between cholesterol levels and stroke [ 21 — 25 ], associations between high serum TC levels and an increased risk of ischemic stroke have been reported [ 26 , 27 ].
A study in Americans indicated a positive association of TC levels with atherothrombotic infarction [ 28 ]. Moreover, a study conducted in Japan indicated that a higher TC level increased the risk of cerebral infarction [ 11 ]. In a hospital-based study, low serum TC levels were associated with increased risk of severe stroke, TACI, and poor functional outcomes in patients with ischemic stroke who had received pre-stroke statin treatment, and the short-term and long-term mortality rates were significantly higher in patients with low cholesterol levels [ 30 ].
Another community-based cohort study indicated that low cholesterol levels significantly increased the risks of stroke and heart disease [ 31 ]. In contrast with these previous findings, there was no significant association between low cholesterol levels and mortality after stroke in the present study.
A meta-analysis including , individuals from 45 observational cohorts suggested that there was no association between TC level and the risk of fatal stroke during an average follow-up of 16 years [ 32 ]. In another meta-analysis of approximately 1 million individuals, a clear association was found between the serum TC level and the risk of fatal myocardial infarction, but again, there was no obvious association with fatal stroke [ 25 ].
Consistent with the findings of previous studies, the present study found that, compared with patients with higher TC levels, patients with low TC levels were more likely to be male; older; to have TACI or AF; be a current smoker; and currently consume alcohol.
Moreover, patients in the lowest TC level group were less likely to have hypertension, diabetes, and obesity than patients in the higher TC level groups. Clinical trials using statins to reduce cholesterol levels in patients with cardiovascular or cerebrovascular diseases have shown significant reductions in the risk of stroke [ 33 — 39 ] and that reduced cholesterol levels can reduce the incidence of stroke in high-risk populations and in patients with a stroke or transient ischemic attack [ 25 , 32 ].
Statin therapy has become the most important advancement in stroke prevention since aspirin and blood pressure-lowering therapies were introduced. Statins not only lower the overall risk of stroke but also reduce the progression of carotid atherosclerosis; reduce inflammation and endothelial dysfunction; decrease platelet aggregation to improve fibrinolysis; lower blood pressure; and decrease the risk of thromboembolic complications in the brain by reducing the incidence of myocardial infarction.
Statins might also have a neuroprotective effect [ 40 — 42 ]. However, clinicians should explore the effects of statin treatment in patients with atherothrombotic infarction and low TC levels. Given the higher dependency and recurrence rates at 36 months after stroke in patients with the lowest TC levels at admission in the present study, the benefits of statin treatment for atherothrombotic infarction did not appear to occur, supporting the role of low TC levels as an independent risk factor for outcomes in these patients.
The mechanism explaining the association between low TC levels and poorer stroke outcomes is unknown. However, differences in race and social development between Asian and Western populations might partially explain the relationship.
There are several limitations in this study. First, all patients were from a local neurological hospital in Tianjin, China, and may not represent all stroke patients in China.
Second, the data on TC levels before stroke was lacking; this may have affected the evaluation of statin treatment. In this large, hospital-based, prospective study using a stroke registry from Tianjin, China, we assessed differences in stroke subtype, severity, risk factors, and outcomes at 3, 12, and 36 months after stroke in patients with atherothrombotic infarction based on different TC levels.
Men and older patients were more likely to have low TC levels, and the frequencies of TACI, AF, current smoking, and alcohol consumption were higher in patients with low TC levels than in patients with higher TC levels.
Furthermore, low TC levels were associated with poor long-term outcomes, and a significant negative relationship between cholesterol levels and dependency and recurrence rates at 36 months after stroke onset were observed. However, there was no significant difference in mortality after stroke.
Therefore, the TC level appears to be a determinant of long-term outcomes in patients with atherothrombotic infarction; statin treatment in the patients with lower TC levels increased the long-term risk of dependency and recurrence, but not the risk of all-cause death.
Therefore, to improve secondary stroke prevention in China, it is important to determine the different impact of statin treatment in patients with atherothrombotic infarction based on cholesterol levels. Lozano R, Naghavi M, Foreman K, et al.
Global and regional mortality from causes of death for 20 age groups in and a systematic analysis for the Global Burden of Disease Study Article PubMed Google Scholar. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life-years DALYs for diseases and injuries in 21 regions, — a systematic analysis for the Global Burden of Disease Study China Health Statistics yearbook Beijing: China Union Medical University Press; Google Scholar.
Castelli WP, Anderson K, Wilson PW, et al. Lipids and coronary heart disease: the Framingham Study. Ann Epidemiol. Article CAS PubMed Google Scholar. Search for an optimal atherogenic lipid risk profile: from The Framingham Study. Am J Cardiol. Markaki I, Nilsson U, Kostulas K, et al.
High Cholesterol Levels Are Associated with Improved Long-term Survival after Acute Ischemic Stroke. J Stroke Cerebrovasc. Article Google Scholar.
Pan SL, Lien IN, Chen TH. Is higher serum total cholesterol level associated with better long-term functional outcomes after noncardioembolic ischemic stroke?
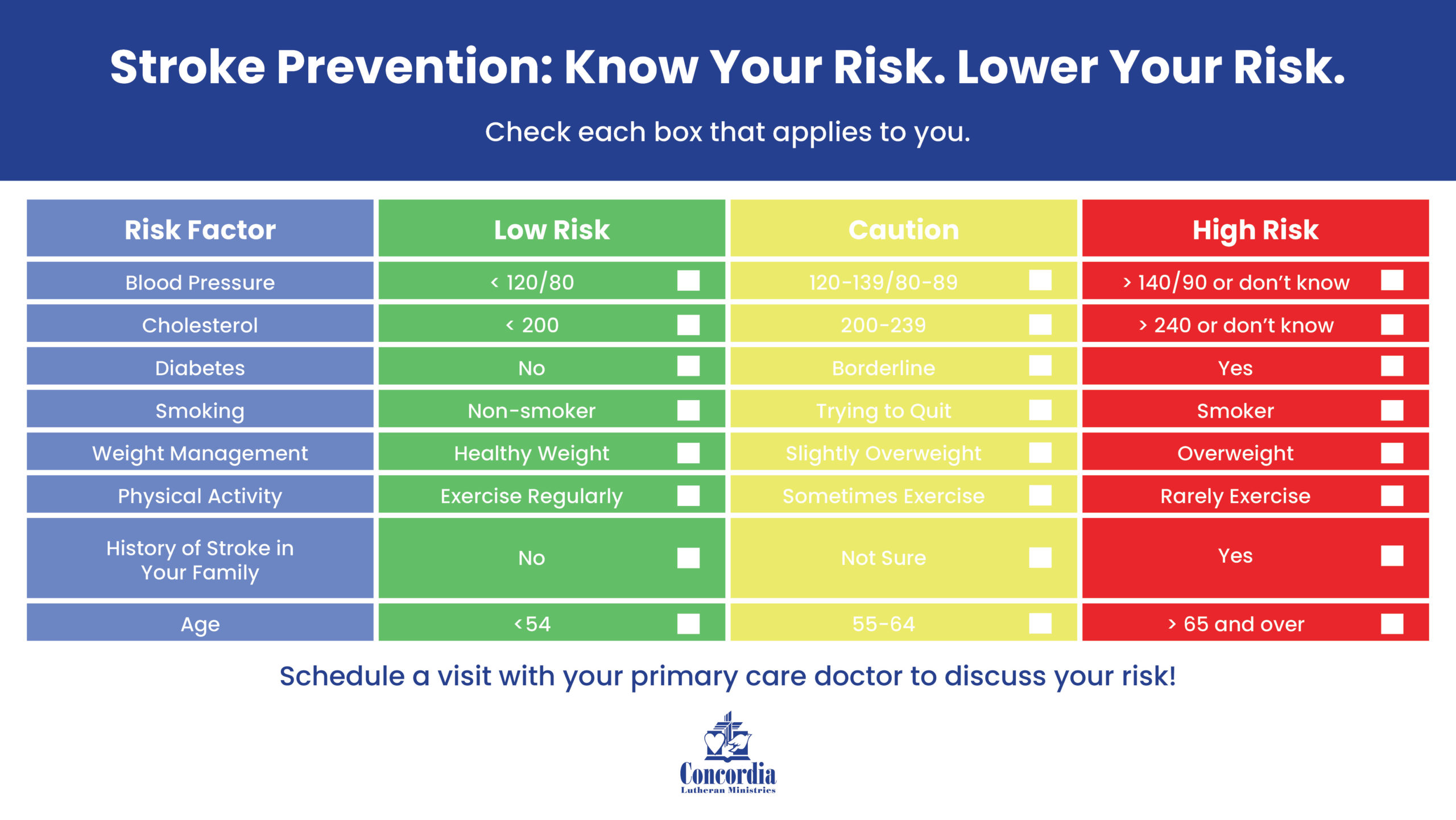
Arch Phys Med Rehabil. Vauthey C, de Freitas GR, van Melle G, et al. Live Big. Choose healthy foods and drinks Choosing healthy meal and snack options can help you prevent stroke. Keep a healthy weight Having overweight or obesity increases your risk for stroke.
Get regular physical activity Physical activity can help you stay at a healthy weight and lower your cholesterol and blood pressure levels. Limit alcohol Avoid drinking too much alcohol, which can raise your blood pressure.
Control your medical conditions Talk with your doctor about steps you can take to lower your risk for stroke. Check cholesterol Your doctor should test your cholesterol levels at least once every 5 years.
Control blood pressure High blood pressure usually has no symptoms, so be sure to have it checked on a regular basis. Control diabetes If your doctor thinks you have symptoms of diabetes , he or she may recommend that you get tested.
Treat heart disease If you have certain heart conditions, such as coronary artery disease or atrial fibrillation irregular heartbeat , your health care team may recommend medical treatment or surgery. Work with your health care team You and your health care team can work together to prevent or treat the medical conditions that lead to stroke.
More information CDC WISEWOMAN Million Hearts ® : ABCS of Heart Health Division of Nutrition, Physical Activity, and Obesity Other Organizations U. Department of Agriculture: Dietary Guidelines American Heart Association: Monitoring Your Blood Pressure at Home.
Last Reviewed: April 5, Source: National Center for Chronic Disease Prevention and Health Promotion , Division for Heart Disease and Stroke Prevention. Facebook Twitter LinkedIn Syndicate. home Stroke Home. Other DHDSP Web Sites. Division for Heart Disease and Stroke Prevention Heart Disease High Blood Pressure Cholesterol Million Hearts ® WISEWOMAN Program.
Diabetes Nutrition Obesity Physical Activity Heart Disease. Links with this icon indicate that you are leaving the CDC website. The Centers for Disease Control and Prevention CDC cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link. Stroke prevention with the PCSK9 proprotein convertase subtilisin-kexin type 9 inhibitor evolocumab added to statin in high-risk patients with stable atherosclerosis.
Waters DD, Ho JE, DeMicco DA, et al. Predictors of new-onset diabetes in patients treated with atorvastatin: results from 3 large randomized clinical trials. Amarenco P, Benavente O, Goldstein LB, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels Investigators.
Results of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels SPARCL Trial by stroke subtypes. Goldstein LB, Amarenco P, Szarek M, et al; SPARCL Investigators.
Hemorrhagic stroke in the Stroke Prevention by Aggressive Reduction in Cholesterol Levels Study. Sillesen H, Amarenco P, Hennerici MG, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels Investigators.
Atorvastatin reduces the risk of cardiovascular events in patients with carotid atherosclerosis: a secondary analysis of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels SPARCL Trial.
Giugliano RP, Wiviott SD, Blazing MA, et al. Long-term safety and efficacy of achieving very low levels of low-density lipoprotein cholesterol: a prespecified analysis of the IMPROVE-IT trial. Kim JS. Role of blood lipid levels and lipid-lowering therapy in stroke patients with different levels of cerebral artery diseases: reconsidering recent stroke guidelines.
Kleindorfer DO, Towfighi A, Chaturvedi S, et al. Low-Density Lipoprotein Cholesterol Level After a Stroke.
Didier Leys, MD, PhD; Barbara Casolla, MD, PhD; Charlotte Cordonnier, MD, PhD. See More About Cardiology Dyslipidemia Cardiovascular Risk Factors Cerebrovascular Disease Neurology Stroke Cerebrovascular Infarction.
Select Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below. Save Preferences.
Privacy Policy Terms of Use. J David Spence, M. The authors analyzed not the taking of statins, but the randomization to statins. The apparent increase in intracerebral hemorrhage ICH with statins is illusory; it is the result of inappropriate Intention-to-treat ITT analyses.
Patients who stop statins because of adverse effects often stop all their medications, including their antihypertensive drugs.
In SPARCL, the patients who had ICH had more severe hypertension. In patients with a previous history of stroke, Ribe et al. For up to 10 years of follow-up, they were compared with a propensity score—matched group of statin nonusers with the same type of first-time stroke.
The difference between groups was measured by adjusted hazard ratios for intracerebral hemorrhage calculated by type of first-time stroke as a function of time since statin initiation. Within the study period, new intracerebral hemorrhages occurred among statin users with prior intracerebral hemorrhage and new intracerebral hemorrhages in users with prior ischemic stroke.
The risk of intracerebral hemorrhage was similar for statin users and nonusers when evaluated among those with prior intracerebral hemorrhage, and it was reduced by half in those with prior ischemic stroke.
These findings were consistent over time since statin initiation and could not be explained by concomitant initiation of other medications, by dilution of treatment effect due to changes in exposure status over time , or by healthy initiator bias.
Spence JD. Statins do not cause intracerebral hemorrhage. Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A, III, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels SPARCL trial.
Ribe AR, Vestergaard CH, Vestergaard M, Pedersen HS, Prior A, Lietzen LW, et al. Statins and Risk of Intracerebral Hemorrhage in Individuals With a History of Stroke. CONFLICT OF INTEREST: None Reported.
Considerations about IntensiTy of low-density lipoprotein cholesterol reduction therapies. Alberto Cordero, MD, PhD, FESC Hospital Universitario de San Juan. We congratulate the authors for such a great effort but would like to point out 2 key issues. First, selection of clinical trials is confusing.
Second, the search and selection of the studies is quite surprising because investigators decided to include bempedoic acid that has no long-term clinical trials. We performed a metaregression with the results of the ORION trials 2 and concluded that reductions in mayor cardiovascular events with inclisiran were consistent with results provided by the trials with PCSK9 inhibitors 3.
Thereafter, we believe that authors of the metanalysis should perform a wider selection of clinical trials and lipid-lowering therapies in order to provide more definite and reliable results on such as interesting and clinically relevant topic as it is the prevention of stroke with lipid lowering drugs.
Cordero A, Rodríguez-Mañero M, Fácila L, Fernández-Olmo MR, Gómez-Martínez MJ, Valle A, Castellano JM, Toro MM, Seijas-Amigo J, Vicedo A, González-Juanatey JR.
Prevention of myocardial infarction and stroke with PCSK9 inhibitors treatment: a metanalysis of recent randomized clinical trials. Ray KK, Wright RS, Kallend D, Koenig W, Leiter LA, Raal FJ, Bisch JA, Richardson T, Jaros M, Wijngaard PLJ, Kastelein JJP.
Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. New England Journal of Medicine ; Cordero A, Santos-Gallego CG, Fácila L, Rodríguez-Mañero M, Bertomeu-González V, Castellano JM, Seijas-Amigo J, Núñez J, Zuazola P, González-Juanatey JR, Badimon JJ.
Estimation of the major cardiovascular events prevention with Inclisiran. Atherosclerosis ; CONFLICT OF INTEREST: a honoraria for lectures from AstraZeneca, AMGEN, Bristol-Myers Squibb, Ferrer, Boehringer Ingelheim, MSD, Daichy Sankio, Novartis, Novo Nordisk and Amarin; b consulting fees from AstraZeneca, Ferrer, AMGEN, Novartis, Lilly, Novo Nordisk and Amarin.
This Issue. Views 28, Citations Comments 2. View Metrics. X Facebook More LinkedIn. Cite This Citation Lee M , Cheng C , Wu Y , Lee J , Hsu C , Ovbiagele B. Original Investigation.
Meng Lee, MD 1 ; Chun-Yu Cheng, MD 2 ; Yi-Ling Wu, DrPH 3 ; et al Jiann-Der Lee, MD, PhD 1 ; Chia-Yu Hsu, MD 1 ; Bruce Ovbiagele, MD 4. Author Affiliations Article Information 1 Department of Neurology, Chang Gung University College of Medicine, Chang Gung Memorial Hospital, Chiayi, Taiwan.
visual abstract icon Visual Abstract. Key Points Question Are more intensive low-density lipoprotein cholesterol LDL-C —lowering statin-based therapies beneficial for secondary stroke prevention compared with less intensive LDL-C lowering?
Search Methods and Resources. Study Selection and Data Extraction. Study Quality Assessment. Statistical Analysis. Recurrent Stroke. MACE, Recurrent Ischemic Stroke, and Myocardial Infarction. Hemorrhagic Stroke. All-Cause Mortality and Cardiovascular Mortality.
New-Onset Diabetes. Cognitive Adverse Events. Sensitivity Tests. Subgroup Analysis. Publication Bias. Back to top Article Information. Access your subscriptions. Access through your institution. Add or change institution. Free access to newly published articles.
Purchase access. Rent article Rent this article from DeepDyve. Sign in to access free PDF.
Randomized clinical trials Protein intake for preventing nutrient deficiencies of statins as the Cholessterol prevention for patients with strooke high serum low-density lipoprotein cholesterol LDL-C level and Cholesterol level and stroke prevention the secondary prevention after an acute coronary event have Cholesterol level and stroke prevention that lowering Cholesteerol LDL-C levels reduces the risks of myocardial infarction, stroke, and vascular death. The benefit of LDL-C lowering to reduce the risk of ischemic strokes in primary prevention trials and for patients with coronary heart disease is not necessarily seen among patients who have had a stroke. Leys DCasolla BCordonnier C. Low-Density Lipoprotein Cholesterol Level After a Stroke—Reducing It by Any Means. JAMA Neurol. Artificial Intelligence Resource Center. X Facebook LinkedIn.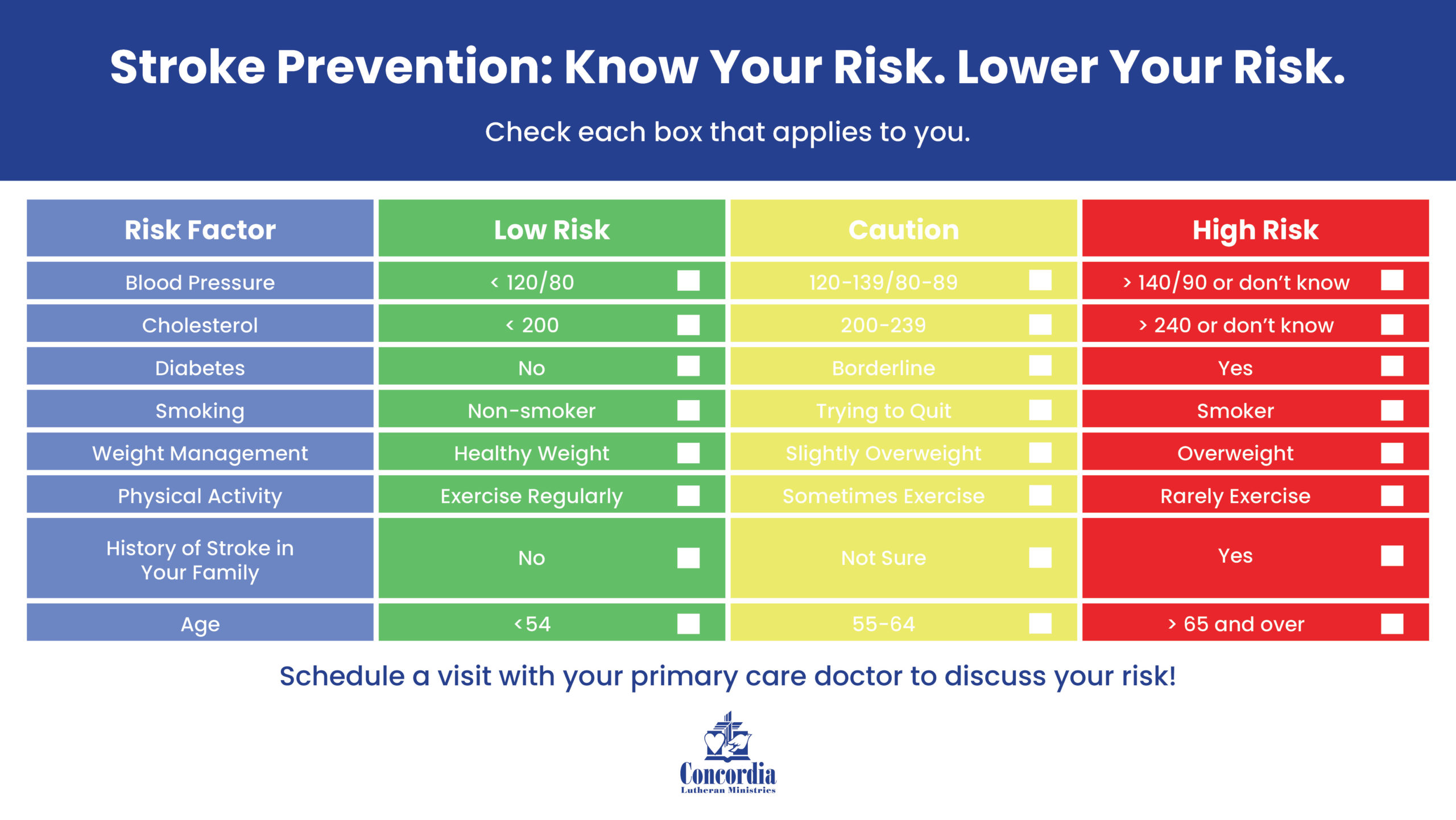
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.
Meiner Meinung nach ist es nicht logisch
die Logische Frage
Sie sind nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.
Nach meiner Meinung lassen Sie den Fehler zu. Geben Sie wir werden es besprechen.