Video
Thermoregulation in the circulatory system - Circulatory system physiology - NCLEX-RN - Khan AcademyThermogenesis and cardiovascular health -
Angiotensin-converting enzyme 2 ACE2 , which is widely recognized as the entry receptor for SARS-CoV-2 into host cells , is expressed in human EAT The downregulation of ACE2 levels increases EAT inflammation, whereas treatment with angiotensin 1—7 reduced EAT inflammatory cytokines in a mouse model The modulation of ACE in EAT might, therefore, have a role in COVIDrelated myocardial and perivascular inflammation.
ACE inhibitors could be a potential component of therapy for these sequelae of COVID, although data are still insufficient and controversial EAT of patients hospitalized with severe or critical COVID shows signs of increased inflammation on CT, irrespective of whether CAD is present 32 , , , In patients with COVID, EAT density on CT is markedly elevated at hospital admission and decreases to normal at discharge, whereas subcutaneous fat shows no signs of inflammation EAT inflammation decreased in patients with COVID who received oral or intravenous dexamethasone, whereas no significant changes in inflammation were observed with other COVID therapies Therefore, EAT might have a role in COVIDrelated cardiac syndrome, and CT-measured EAT attenuation could be a marker of inflammation and severity of COVID The physiology and pathophysiology of EAT and their clinical implications form a fast-moving and productive field of research.
EAT is a measurable and modifiable cardiovascular risk factor that adds qualitative value to the stratification of cardiovascular risk. Assessment of EAT, with commonly used imaging techniques, such as echocardiography, CT and MRI, should be readily accessible to contemporary cardiologists.
EAT provides a novel and unconventional perspective on the pathophysiology of major cardiovascular diseases. EAT directly contributes to the development and progression of CAD, mainly by causing inflammation but also by endothelial damage and oxidative stress as well as the accumulation of glucose and lipids in the proximal coronary arteries.
In the context of atrial fibrillation, EAT represents a new pathogenic substrate through the regional secretion of factors that induce fibrosis and neurohormonal disarray of the atrial myocytes. The role of EAT in heart failure is mediated through several pathways, including the excessive release of fatty acids leading to intracardiac cell ectopic lipid accumulation, overexpression of local pro-inflammatory and profibrotic cytokines with pro-arrhythmogenic properties, and increased β-adrenergic receptor activation.
Pharmacological modulation of EAT induces previously unexpected beneficial cardiometabolic effects. The potential to restore the cardioprotective function of EAT with targeted agents, such as GLP1R agonists and SGLT2 inhibitors, can open new avenues in pharmacotherapy for cardiovascular diseases.
Several challenges remain for research on EAT. Further investigations are needed to determine whether reducing the mass of EAT can help to improve or eliminate atherosclerosis or prevent the development of atrial fibrillation and heart failure.
The potential for pharmacological manipulation of the EAT transcriptome to restore its physiological and protective properties is a fascinating concept but is yet to be demonstrated.
Iacobellis, G. et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Article PubMed Google Scholar. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk.
Article CAS Google Scholar. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. McAninch, E. Epicardial adipose tissue has a unique transcriptome modified in severe coronary artery disease.
Obesity 23 , — Article CAS PubMed Google Scholar. Local and systemic effects of the multifaceted epicardial adipose tissue depot. Epicardial fat: a new cardiovascular therapeutic target. Malavazos, A. Does epicardial fat contribute to COVID myocardial inflammation? Heart J. Corradi, D. The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts.
Article Google Scholar. Company, J. Epicardial fat gene expression after aerobic exercise training in pigs with coronary atherosclerosis: relationship to visceral and subcutaneous fat. Article PubMed PubMed Central Google Scholar.
Sacks, H. Human epicardial fat exhibits beige features. Marchington, J. Site-specific properties of pericardial and epicardial adipose tissue: the effects of insulin and high-fat feeding on lipogenesis and the incorporation of fatty acids in vitro.
CAS PubMed Google Scholar. Vural, B. Presence of fatty-acid-binding protein 4 expression in human epicardial adipose tissue in metabolic syndrome. Judkin, J. Lancet , — Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with CAD.
Cytokine 29 , — Epicardial adipose tissue and intracoronary adrenomedullin levels in coronary artery disease. Antonopoulos, A. Article CAS PubMed PubMed Central Google Scholar. Uncoupling protein-1 and related mRNAs in human epicardial and other adipose tissues: epicardial fat functioning as brown fat.
Fainberg, H. Transcriptional analysis of adipose tissue during development reveals depot-specific responsiveness to maternal dietary supplementation.
Article PubMed PubMed Central CAS Google Scholar. Depot-specific overexpression of proinflammatory, redox, endothelial cell, and angiogenic genes in epicardial fat adjacent to severe stable coronary atherosclerosis.
Peterson, S. Cardioprotective heme oxygenase 1-PGC1α signaling in epicardial fat attenuates cardiovascular risk in humans as in obese mice. Obesity 27 , — Echocardiographic epicardial fat: a review of research and clinical applications.
Relation of echocardiographic epicardial fat thickness and myocardial fat. Neeland, I. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management.
Circulation , — Oikonomou, E. The role of adipose tissue in cardiovascular health and disease. Spearman, J. Prognostic value of epicardial fat volume measurements by computed tomography: a systematic review of the literature.
Nelson, A. Validation of cardiovascular magnetic resonance assessment of pericardial adipose tissue volume. de Vos, A. Peri-coronary epicardial adipose tissue is related to cardiovascular risk factors and coronary artery calcification in post-menopausal women.
Batal, O. Left atrial epicardial adiposity and atrial fibrillation. Liu, Z. Association of epicardial adipose tissue attenuation with coronary atherosclerosis in patients with a high risk of coronary artery disease.
Atherosclerosis , — Is epicardial fat attenuation a novel marker of coronary inflammation? Franssens, B. Relation between cardiovascular disease risk factors and epicardial adipose tissue density on cardiac computed tomography in patients at high risk of cardiovascular events.
Epicardial fat inflammation in severe COVID Obesity 28 , — Detecting human coronary inflammation by imaging perivascular fat. Transl Med. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk the CRISP CT study : a post-hoc analysis of prospective outcome data.
Attanasio, S. Artificial intelligence, radiomics and other horizons in body composition assessment. Imaging Med. Mazurek, T. Human epicardial adipose tissue is a source of inflammatory mediators. Hirata, Y. Coronary atherosclerosis is associated with macrophage polarization in epicardial adipose tissue.
Langheim, S. Increased expression and secretion of resistin in epicardial adipose tissue of patients with acute coronary syndrome. Heart Circ. Gao, X. Association of chemerin mRNA expression in human epicardial adipose tissue with coronary atherosclerosis.
Imoto-Tsubakimoto, H. Serglycin is a novel adipocytokine highly expressed in epicardial adipose tissue. Baker, A. Epicardial adipose tissue as a source of nuclear factor-kappaB and c-Jun N-terminal kinase mediated inflammation in patients with coronary artery disease.
Du, Y. Association between omentin-1 expression in human epicardial adipose tissue and coronary atherosclerosis. Karastergiou, K. Epicardial adipokines in obesity and coronary artery disease induce atherogenic changes in monocytes and endothelial cells. Kremen, J. Increased subcutaneous and epicardial adipose tissue production of proinflammatory cytokines in cardiac surgery patients: possible role in postoperative insulin resistance.
Cheng, K. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Wang, J. Vasodilator-stimulated phosphoprotein: regulators of adipokines resistin and phenotype conversion of epicardial adipocytes.
Salgado-Somoza, A. Proteomic analysis of epicardial and subcutaneous adipose tissue reveals differences in proteins involved in oxidative stress. Dutour, A. Secretory type II phospholipase A2 is produced and secreted by epicardial adipose tissue and overexpressed in patients with CAD.
Furuhashi, M. Pezeshkian, M. Epicardial and subcutaneous adipose tissue fatty acids profiles in diabetic and non-diabetic patients candidate for coronary artery bypass graft. Bioimpacts 3 , 83—89 PubMed PubMed Central Google Scholar.
Suganami, T. Camarena, V. Novel atherogenic pathways from the differential transcriptome analysis of diabetic epicardial adipose tissue. Dozio, E. Expression of the receptor for advanced glycation end products in epicardial fat: link with tissue thickness and local insulin resistance in coronary artery disease.
Diabetes Res. Article PubMed CAS Google Scholar. Vyas, V. Obesity and diabetes are major risk factors for epicardial adipose tissue inflammation. JCI Insight 6 , e Article PubMed Central Google Scholar. Coronary artery disease is associated with higher epicardial retinol-binding protein 4 RBP4 and lower glucose transporter GLUT 4 levels in epicardial and subcutaneous adipose tissue.
Błachnio-Zabielska, A. Lipids 47 , Mahabadi, A. Association of epicardial adipose tissue with progression of coronary artery calcification is more pronounced in the early phase of atherosclerosis: results from the Heinz Nixdorf Recall Study. JACC Cardiovasc. Imaging 7 , — Gorter, P. Relation of epicardial and pericoronary fat to coronary atherosclerosis and coronary artery calcium in patients undergoing coronary angiography.
Djaberi, R. Relation of epicardial adipose tissue to coronary atherosclerosis. Mancio, J. Gender differences in the association of epicardial adipose tissue and coronary artery calcification: EPICHEART study: EAT and coronary calcification by gender.
Epicardial fat thickness and CAD correlate independently of obesity. Yerramasu, A. Increased volume of epicardial fat is an independent risk factor for accelerated progression of sub-clinical coronary atherosclerosis.
Bachar, G. Epicardial adipose tissue as a predictor of coronary artery disease in asymptomatic subjects. Oka, T. Association between epicardial adipose tissue volume and characteristics of non-calcified plaques assessed by coronary computed tomographic angiography.
Alexopoulos, N. Epicardial adipose tissue and coronary artery plaque characteristics. Nakanishi, K. Persistent epicardial adipose tissue accumulation is associated with coronary plaque vulnerability and future acute coronary syndrome in non-obese subjects with coronary artery disease.
Ito, T. Impact of epicardial fat volume on coronary artery disease in symptomatic patients with a zero calcium score. Alam, M. Epicardial adipose tissue thickness as a predictor of impaired microvascular function in patients with non-obstructive coronary artery disease.
Wang, T. Association of epicardial adipose tissue with coronary atherosclerosis is region-specific and independent of conventional risk factors and intra-abdominal adiposity.
Association of epicardial fat with cardiovascular risk factors and incident myocardial infarction in the general population: the Heinz Nixdorf recall study. Ding, J. The association of pericardial fat with incident coronary heart disease: the multi-ethnic study of atherosclerosis MESA. Magnani, J.
Atrial fibrillation: current knowledge and future directions in epidemiology and genomics. Pathak, R. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study.
Wong, C. Epicardial fat and atrial fibrillation: current evidence, potential mechanisms, clinical implications, and future directions. Jhuo, S. The association of the amounts of epicardial fat, P wave duration, and PR interval in electrocardiogram. Epicardial and pericardial fat: close, but very different.
Obesity 17 , Thanassoulis, G. Pericardial fat is associated with prevalent atrial fibrillation: the Framingham heart study. Yamaguchi, Y. Adipogenesis and epicardial adipose tissue: a novel fate of the epicardium induced by mesenchymal transformation and PPARγ activation.
Natl Acad. USA , — Suffee, N. Atrial natriuretic peptide regulates adipose tissue accumulation in adult atria. USA , E—E Reactivation of the epicardium at the origin of myocardial fibro-fatty infiltration during the atrial cardiomyopathy.
Gaborit, B. Human epicardial adipose tissue has a specific transcriptomic signature depending on its anatomical peri-atrial, peri-ventricular, or peri-coronary location.
Goldberger, J. Evaluating the atrial myopathy underlying atrial fibrillation: identifying the arrhythmogenic and thrombogenic substrate. Venteclef, N. Human epicardial adipose tissue induces fibrosis of the atrial myocardium through the secretion of adipo-fibrokines.
Wang, Q. Human epicardial adipose tissue cTGF expression is an independent risk factor for atrial fibrillation and highly associated with atrial fibrosis. Nalliah, C. Epicardial adipose tissue accumulation confers atrial conduction abnormality.
Shaihov-Teper, O. Extracellular vesicles from epicardial fat facilitate atrial fibrillation. Direction-dependent conduction in lone atrial fibrillation. Heart Rhythm 9 , — Munger, T. Electrophysiological and hemodynamic characteristics associated with obesity in patients with atrial fibrillation.
Lin, Y. Adipocytes modulate the electrophysiology of atrial myocytes: implications in obesity-induced atrial fibrillation. Basic Res. Po, S. Localization of left atrial ganglionated plexi in patients with atrial fibrillation. Balcioglu, A. Arrhythmogenic evidence for epicardial adipose tissue: heart rate variability and turbulence are influenced by epicardial fat thickness.
Pacing Clin. Pokushalov, E. Long-term suppression of atrial fibrillation by botulinum toxin injection into epicardial fat pads in patients undergoing cardiac surgery: one-year follow-up of a randomized pilot study.
Nagashima, K. Association between epicardial adipose tissue volumes on 3-dimensional reconstructed CT images and recurrence of atrial fibrillation after catheter ablation. Circulation 75 , — Tsao, H. Quantitative analysis of quantity and distribution of epicardial adipose tissue surrounding the left atrium in patients with atrial fibrillation and effect of recurrence after ablation.
Chao, T. Epicardial adipose tissue thickness and ablation outcome of atrial fibrillation. PLoS ONE 8 , e Kocyigit, D. Periatrial epicardial adipose tissue thickness is an independent predictor of atrial fibrillation recurrence after cryoballoon-based pulmonary vein isolation.
Masuda, M. Abundant epicardial adipose tissue surrounding the left atrium predicts early rather than late recurrence of atrial fibrillation after catheter ablation. Epicardial fat in atrial fibrillation and heart failure. Yancy, C. van Woerden, G.
Epicardial fat in heart failure patients with mid-range and preserved ejection fraction. Heart Fail. Fontes-Carvalho, R. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction.
Doesch, C. Epicardial adipose tissue in patients with heart failure. Epicardial adipose tissue assessed by cardiac magnetic resonance imaging in patients with heart failure due to dilated cardiomyopathy. Obesity 21 , E—E Khawaja, T.
Epicardial fat volume in patients with left ventricular systolic dysfunction. Pocock, S. Weight loss and mortality risk in patients with chronic heart failure in the candesartan in heart failure: assessment of reduction in mortality and morbidity CHARM programme.
Zhao, L. Proteomics of epicardial adipose tissue in patients with heart failure. Agra, R. Adiponectin and p53 mRNA in epicardial and subcutaneous fat from heart failure patients. Krstic, J. p53 functions in adipose tissue metabolism and homeostasis.
Article PubMed Central CAS Google Scholar. Wu, C. Evolutional change in epicardial fat and its correlation with myocardial diffuse fibrosis in heart failure patients. Kankaanpää, M. Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels.
Myocardial adipose deposition and the development of heart failure with preserved ejection fraction. White, A. Cardiac sympathetic denervation in the failing heart: a role for epicardial adipose tissue.
Lymperopoulos, A. Adrenal GRK2 upregulation mediates sympathetic overdrive in heart failure. Reduction of sympathetic activity via adrenal-targeted GRK2 gene deletion attenuates heart failure progression and improves cardiac function after myocardial infarction.
Parisi, V. Increased epicardial adipose tissue volume correlates with cardiac sympathetic denervation in patients with heart failure. Agra-Bermejo, R. CD5L, macrophage apoptosis inhibitor, was identified in epicardial fat-secretome and regulated by isoproterenol from patients with heart failure.
Pabon, M. Linking arrhythmias and adipocytes: insights, mechanisms, and future directions. Burgeiro, A.
Glucose uptake and lipid metabolism are impaired in epicardial adipose tissue from heart failure patients with or without diabetes. Marso, S. Liraglutide and cardiovascular outcomes in type 2 diabetes.
Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. Gerstein, H. Dulaglutide and cardiovascular outcomes in type 2 diabetes REWIND : a double-blind, randomised placebo-controlled trial.
Zinman, B. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. Wiviott, S. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. Effects of liraglutide on visceral and ectopic fat in adults with overweight and obesity at high cardiovascular risk: a randomised, double-blind, placebo-controlled, clinical trial.
Lancet Diabetes Endocrinol. Liraglutide causes large and rapid epicardial fat reduction. Obesity 25 , — Effects of semaglutide versus dulaglutide on epicardial fat thickness in subjects with type 2 diabetes and obesity. Morano, S. Short-term effects of glucagon-like peptide 1 GLP-1 receptor agonists on fat distribution in patients with type 2 diabetes mellitus: an ultrasonography study.
Acta Diabetol. Li, Y. Effect of liraglutide on epicardial adipose tissue thickness with echocardiography in patients with obese type 2 diabetes mellitus.
Diabetes Dev. Ctries 40 , — Exenatide decreases liver fat content and epicardial adipose tissue in patients with obesity and type 2 diabetes: a prospective randomized clinical trial using magnetic resonance imaging and spectroscopy. Diabetes Obes. Human epicardial fat expresses glucagon-like peptide 1 and 2 receptors genes.
Epicardial adipose tissue GLP-1 receptor is associated with genes involved in fatty acid oxidation and white-to-brown fat differentiation: a target to modulate cardiovascular risk?
Couselo-Seijas, M. Higher ACE2 expression levels in epicardial cells than subcutaneous stromal cells from patients with cardiovascular disease: diabetes and obesity as possible enhancer. Beiroa, D. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK.
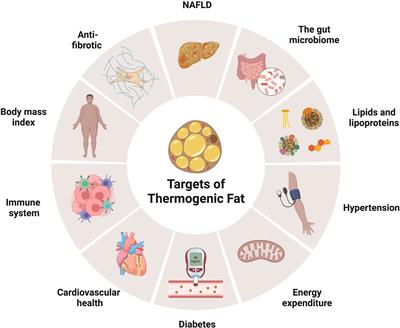
Diabetes 63 , — Reassuringly, although obese individuals showed blunted expression of thermogenic genes in BAT 78 and decreased glucose uptake by the tissue, 79 adipocyte progenitors isolated from BAT of obese individuals can differentiate into thermogenic adipocytes at an equal frequency as those isolated from lean individuals, and the resulting differentiated brown adipocytes displayed comparable basal and noradrenalin-stimulated mitochondrial respiration.
Besides the observed beneficial relation between the presence of BAT and CVD in humans see Section 6 , cold exposure has been shown to beneficially affect several risk factors for CVD, including adiposity and insulin resistance. Adiposity results from excessive energy intake relative to energy expenditure, or alterations in nutrient partitioning.
Acute cold exposure increased resting energy expenditure in both lean 81—83 and obese 84 participants, and notably such increases were only evident 82 or more pronounced 83 in BAT-positive individuals i.
with detectible [ 18 F]FDG uptake by BAT depots. Even though BAT activity is generally assessed using the glucose tracer [ 18 F]FDG, the cold-induced increase in energy expenditure was mainly explained by an increase in lipid oxidation.
L and TAK did not reduce body fat mass. Alternatively, it is well possible that BAT activity simply improves overall metabolic health, rather than reducing adipose tissue mass per se.
In line with this notion, a very recent study has suggested that after correcting for BMI, the presence of active BAT, as measured by [ 18 F]FDG uptake, was associated with decreased visceral adipose tissue and increased subcutaneous adipose tissue, 91 a phenotype that is typically associated with better metabolic health.
BAT has also been implicated in glycaemic control. In healthy lean humans, acute cold stimulation 18°C 92 or 1-month cold acclimation i. Thus, studies have unequivocally demonstrated that cold exposure activates BAT, enhances energy expenditure, and improves glycaemic control.
The relative contribution of BAT and other metabolic organs needs to be better understood, but at the very least it seems that the presence of cold- activate d BAT is associated with metabolic health.
In , Cypess et al. Indeed, transcriptomic analysis of human BAT biopsies showed that abundance of β 2 -AR far exceeds that of β 3 -AR, while β 3 -AR is the dominant AR in mouse BAT. The recent finding regarding the prominent role of β 2 -AR in human BAT activation, however, opened up new opportunities for BAT as a therapeutic target in cardio metabolism.
Interestingly, the amino acid sequence of human β 2 -AR is highly polymorphic. These findings thus imply that β 2 -AR agonism may be the way forward in adrenergic BAT activation, and further studies are warranted to assess whether this can effectively and safely activate human BAT in vivo.
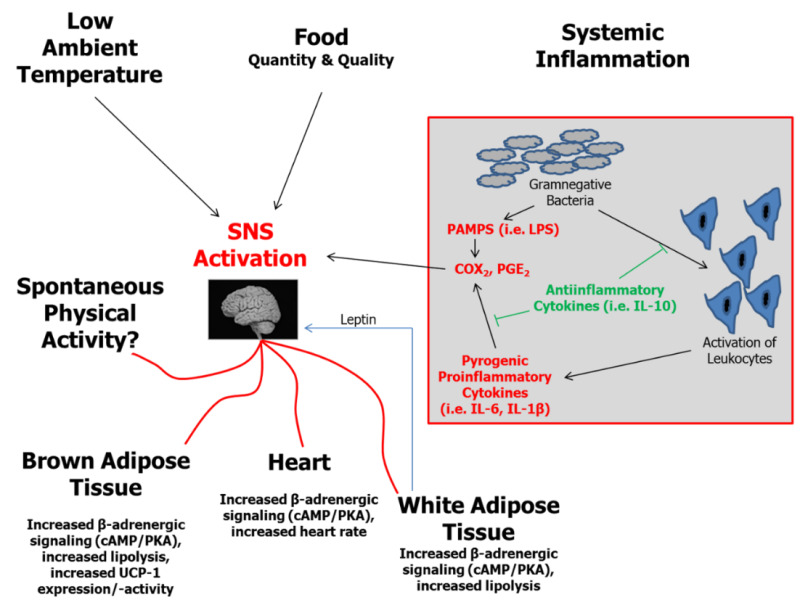
Besides cold-mediated sympathetic stimulation and pharmacological β-AR agonism, stimulation of two hormonal pathways also potently activate BAT and are worth noting as they lower atherosclerosis in preclinical models and improve risk factors for CVD in humans see also the graphical summary in Figure 3.
Firstly, treatment of mice with recombinant human FGF21 enhanced the uptake of glucose and triglyceride-derived FAs from TRLs by BAT and promoted WAT browning, , which normalized glycaemia and reduced plasma triglycerides. Graphical summary of promising therapeutic interventions to promote thermogenic adipose tissue activity and their effects on risk factors for CVD in humans.
Similar to FGF21, studies of glucagon-like peptide 1 receptor GLP-1R agonism have also shown promising results. In lean mice, intracerebroventricular administration with the GLP-1R agonist liraglutide activated BAT thermogenesis as evident from decreased intracellular lipid content in combination with increased interscapular temperature In both lean and diet-induced obese mice, another GLP-1R agonist, exendin-4, was shown to increase UCP1 protein content in BAT.
Indeed, patients with type 2 diabetes using liraglutide showed less death from cardiovascular causes and a lower frequency of nonfatal myocardial infarction and stroke.
CETP mice have shown that GLP-1R agonists reduced atherosclerosis development via reducing inflammation in atherosclerotic plaques. Furthermore, glucose-dependent insulinotropic polypeptide receptor GIPR agonism was proposed to enhance the metabolic effects of GLP-1R agonism.
Taken together, there is compelling evidence for a relationship between the presence of metabolically active BAT in humans and lower CVD risk. The still unresolved question, however, is to what extent the observed associations imply causality or merely reflect overall metabolic health.
Cold interventions have been shown to activate BAT activity and thermogenesis, and large prospective intervention studies applying cold interventions will be needed to prove causality. In addition, genetic polymorphisms determining the thermogenic capacity of adipose tissue may be identified to allow proof of causality between adipose tissue thermogenesis and CVD risk in large Mendelian-randomization studies.
Experimental studies in mice have convincingly shown that thermogenic activity in adipose tissue enhances lipolytic processing of TRLs, resulting in FA uptake by adipocytes and consequently promotes liver uptake of TRL remnants provided that an intact human-like ApoE-LDLR pathway is present Table 1.
Together, these result in combined attenuation of hypertriglyceridaemia and hypercholesterolaemia and reduce atherosclerosis development.
This anti-atherosclerotic effect is likely further enhanced by elevated reverse cholesterol transport, which is driven by enhanced cholesterol efflux capacity of HDL as a consequence of increasing lipid transfer from TRLs to HDL during lipolytic processing.
In humans, BAT activity inversely correlates with circulating triglyceride and HDL-cholesterol levels and CVD prevalence and seems to protect against additional risk factors for CVD including adiposity and insulin resistance. Combined with the findings from preclinical studies that thermogenic adipose tissue activation adds to the lipid-lowering and antiatherogenic effects of classical lipid-lowering strategies i.
Obviously, further research is needed to reveal whether promotion of BAT activity or browning of WAT can be used to treat dyslipidaemia and atherosclerotic CVD in humans, especially in those individuals who are at high risk for CVD.
FGF21 and GLP-1R agonism likely in combination with GIPR agonism activate BAT and promote browning of WAT in mice and are promising therapeutic strategies to treat human atherosclerotic CVD.
Further clinical studies are warranted to assess their efficacy to reduce atherosclerotic CVD, as well as the involvement of BAT activation therein. Also, the recent discovery that human brown adipocytes are mainly activated via β 2 -AR stimulation, in contrast to mouse brown adipocytes that are activated mainly through the β 3 -AR, 15 provides a unique opportunity to assess both the efficacy and safety of β 2 -AR agonism in human BAT activation in relation to cardio metabolic health.
This work was supported by the Dutch Heart Foundation [T to S. is supported by a full-time PhD scholarship from the China Scholarship Council. Nedergaard J , Bengtsson T , Cannon B.
Unexpected evidence for active brown adipose tissue in adult humans. Am J Physiol Endocrinol Metab ; : E — E Google Scholar. van Marken Lichtenbelt WD , Vanhommerig JW , Smulders NM , Drossaerts JM , Kemerink GJ , Bouvy ND , Schrauwen P , Teule GJ.
Cold-activated brown adipose tissue in healthy men. N Engl J Med ; : — Cypess AM , Lehman S , Williams G , Tal I , Rodman D , Goldfine AB , Kuo FC , Palmer EL , Tseng YH , Doria A , Kolodny GM , Kahn CR. Identification and importance of brown adipose tissue in adult humans.
Zingaretti MC , Crosta F , Vitali A , Guerrieri M , Frontini A , Cannon B , Nedergaard J , Cinti S. The presence of UCP1 demonstrates that metabolically active adipose tissue in the neck of adult humans truly represents brown adipose tissue.
FASEB J ; 23 : — Berbee JF , Boon MR , Khedoe PP , Bartelt A , Schlein C , Worthmann A , Kooijman S , Hoeke G , Mol IM , John C , Jung C , Vazirpanah N , Brouwers LP , Gordts PL , Esko JD , Hiemstra PS , Havekes LM , Scheja L , Heeren J , Rensen PC. Brown fat activation reduces hypercholesterolaemia and protects from atherosclerosis development.
Nat Commun ; 6 : Zoico E , Rubele S , De Caro A , Nori N , Mazzali G , Fantin F , Rossi A , Zamboni M. Brown and beige adipose tissue and aging. Front Endocrinol Lausanne ; 10 : Yoneshiro T , Aita S , Matsushita M , Okamatsu-Ogura Y , Kameya T , Kawai Y , Miyagawa M , Tsujisaki M , Saito M.
Age-related decrease in cold-activated brown adipose tissue and accumulation of body fat in healthy humans. Obesity Silver Spring ; 19 : — Brown adipose tissue activation is inversely related to central obesity and metabolic parameters in adult human.
PLoS One ; 10 : e Takx RA , Ishai A , Truong QA , MacNabb MH , Scherrer-Crosbie M , Tawakol A. Supraclavicular brown adipose tissue 18 F-FDG uptake and cardiovascular disease. J Nucl Med ; 57 : — Bakker LE , Boon MR , van der Linden RA , Arias-Bouda LP , van Klinken JB , Smit F , Verberne HJ , Jukema JW , Tamsma JT , Havekes LM , van Marken Lichtenbelt WD , Jazet IM , Rensen PC.
Brown adipose tissue volume in healthy lean south Asian adults compared with white Caucasians: a prospective, case-controlled observational study. Lancet Diabetes Endocrinol ; 2 : — Becher T , Palanisamy S , Kramer DJ , Eljalby M , Marx SJ , Wibmer AG , Butler SD , Jiang CS , Vaughan R , Schöder H , Mark A , Cohen P.
Brown adipose tissue is associated with cardiometabolic health. Nat Med ; 27 : 58 — Frontini A , Cinti S. Distribution and development of brown adipocytes in the murine and human adipose organ.
Cell Metab ; 11 : — Cannon B , Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev ; 84 : — Robidoux J , Martin TL , Collins S.
Beta-adrenergic receptors and regulation of energy expenditure: a family affair. Annu Rev Pharmacol Toxicol ; 44 : — Blondin DP , Nielsen S , Kuipers EN , Severinsen MC , Jensen VH , Miard S , Jespersen NZ , Kooijman S , Boon MR , Fortin M , Phoenix S , Frisch F , Guerin B , Turcotte EE , Haman F , Richard D , Picard F , Rensen PCN , Scheele C , Carpentier AC.
Human brown adipocyte thermogenesis is driven by beta2-AR stimulation. Cell Metab ; 32 : — Cero C , Lea HJ , Zhu KY , Shamsi F , Tseng YH , Cypess AM. JCI Insight ; 6 : e Fedorenko A , Lishko PV , Kirichok Y. Mechanism of fatty-acid-dependent UCP1 uncoupling in brown fat mitochondria.
Cell ; : — Labbé SM , Caron A , Bakan I , Laplante M , Carpentier AC , Lecomte R , Richard D. In vivo measurement of energy substrate contribution to cold-induced brown adipose tissue thermogenesis. FASEB J ; 29 : — Blondin DP , Frisch F , Phoenix S , Guerin B , Turcotte EE , Haman F , Richard D , Carpentier AC.
Inhibition of intracellular triglyceride lipolysis suppresses cold-induced brown adipose tissue metabolism and increases shivering in humans. Cell Metab ; 25 : — Kazak L , Chouchani ET , Jedrychowski MP , Erickson BK , Shinoda K , Cohen P , Vetrivelan R , Lu GZ , Laznik-Bogoslavski D , Hasenfuss SC , Kajimura S , Gygi SP , Spiegelman BM.
A creatine-driven substrate cycle enhances energy expenditure and thermogenesis in beige fat. Rahbani JF , Roesler A , Hussain MF , Samborska B , Dykstra CB , Tsai L , Jedrychowski MP , Vergnes L , Reue K , Spiegelman BM , Kazak L. Creatine kinase B controls futile creatine cycling in thermogenic fat.
Nature ; : — Ikeda K , Kang Q , Yoneshiro T , Camporez JP , Maki H , Homma M , Shinoda K , Chen Y , Lu X , Maretich P , Tajima K , Ajuwon KM , Soga T , Kajimura S. UCP1-independent signaling involving SERCA2b-mediated calcium cycling regulates beige fat thermogenesis and systemic glucose homeostasis.
Nat Med ; 23 : — Abreu-Vieira G , Sardjoe Mishre ASD , Burakiewicz J , Janssen LGM , Nahon KJ , van der Eijk JA , Riem TT , Boon MR , Dzyubachyk O , Webb AG , Rensen PCN , Kan HE. Human brown adipose tissue estimated with magnetic resonance imaging undergoes changes in composition after cold exposure: an in vivo MRI study in healthy volunteers.
Khedoe PP , Hoeke G , Kooijman S , Dijk W , Buijs JT , Kersten S , Havekes LM , Hiemstra PS , Berbee JF , Boon MR , Rensen PC. Brown adipose tissue takes up plasma triglycerides mostly after lipolysis.
J Lipid Res ; 56 : 51 — Bartness TJ , Liu Y , Shrestha YB , Ryu V. Neural innervation of white adipose tissue and the control of lipolysis. Front Neuroendocrinol ; 35 : — Blondin DP , Labbe SM , Phoenix S , Guerin B , Turcotte EE , Richard D , Carpentier AC , Haman F.
Contributions of white and brown adipose tissues and skeletal muscles to acute cold-induced metabolic responses in healthy men. J Physiol ; : — Prentki M , Madiraju SR.
Glycerolipid metabolism and signaling in health and disease. Endocr Rev ; 29 : — Vallerand AL , Zamecnik J , Jones PJ , Jacobs I. Aviat Space Environ Med ; 70 : 42 — Konstandi M , Kypreos KE , Matsubara T , Xepapadaki E , Shah YM , Krausz K , Andriopoulou CE , Kofinas A , Gonzalez FJ.
Adrenoceptor-related decrease in serum triglycerides is independent of PPARα activation. FEBS J ; : — Hoeke G , Nahon KJ , Bakker LEH , Norkauer SSC , Dinnes DLM , Kockx M , Lichtenstein L , Drettwan D , Reifel-Miller A , Coskun T , Pagel P , Romijn F , Cobbaert CM , Jazet IM , Martinez LO , Kritharides L , Berbee JFP , Boon MR , Rensen PCN.
Short-term cooling increases serum triglycerides and small high-density lipoprotein levels in humans. J Clin Lipidol ; 11 : — e2. Bartelt A , Bruns OT , Reimer R , Hohenberg H , Ittrich H , Peldschus K , Kaul MG , Tromsdorf UI , Weller H , Waurisch C , Eychmüller A , Gordts PL , Rinninger F , Bruegelmann K , Freund B , Nielsen P , Merkel M , Heeren J.
Brown adipose tissue activity controls triglyceride clearance. Nat Med ; 17 : — Carneheim C , Nedergaard J , Cannon B. Cold-induced beta-adrenergic recruitment of lipoprotein lipase in brown fat is due to increased transcription.
Am J Physiol ; : E — E Mitchell JR , Jacobsson A , Kirchgessner TG , Schotz MC , Cannon B , Nedergaard J. Regulation of expression of the lipoprotein lipase gene in brown adipose tissue. Fischer AW , Jaeckstein MY , Gottschling K , Heine M , Sass F , Mangels N , Schlein C , Worthmann A , Bruns OT , Yuan Y , Zhu H , Chen O , Ittrich H , Nilsson SK , Stefanicka P , Ukropec J , Balaz M , Dong H , Sun W , Reimer R , Scheja L , Heeren J.
Lysosomal lipoprotein processing in endothelial cells stimulates adipose tissue thermogenic adaptation.
Cell Metab ; 33 : — Townsend KL , Tseng YH. Brown fat fuel utilization and thermogenesis. Trends Endocrinol Metab ; 25 : — McNeill BT , Morton NM , Stimson RH. Substrate utilization by brown adipose tissue: what's hot and what's not?
Front Endocrinol Lausanne ; 11 : Held NM , Kuipers EN , van Weeghel M , van Klinken JB , Denis SW , Lombès M , Wanders RJ , Vaz FM , Rensen PCN , Verhoeven AJ , Boon MR , Houtkooper RH. Pyruvate dehydrogenase complex plays a central role in brown adipocyte energy expenditure and fuel utilization during short-term beta-adrenergic activation.
Sci Rep ; 8 : Irshad Z , Dimitri F , Christian M , Zammit VA. Diacylglycerol acyltransferase 2 links glucose utilization to fatty acid oxidation in the brown adipocytes.
J Lipid Res ; 58 : 15 — Wu J , Bostrom P , Sparks LM , Ye L , Choi JH , Giang AH , Khandekar M , Virtanen KA , Nuutila P , Schaart G , Huang K , Tu H , van Marken Lichtenbelt WD , Hoeks J , Enerback S , Schrauwen P , Spiegelman BM.
Beige adipocytes are a distinct type of thermogenic fat cell in mouse and human. Sharp LZ , Shinoda K , Ohno H , Scheel DW , Tomoda E , Ruiz L , Hu H , Wang L , Pavlova Z , Gilsanz V , Kajimura S.
PLoS One ; 7 : e Jespersen NZ , Larsen TJ , Peijs L , Daugaard S , Homøe P , Loft A , de Jong J , Mathur N , Cannon B , Nedergaard J , Pedersen BK , Møller K , Scheele C. A classical brown adipose tissue mRNA signature partly overlaps with brite in the supraclavicular region of adult humans.
Cell Metab ; 17 : — Cypess AM , White AP , Vernochet C , Schulz TJ , Xue R , Sass CA , Huang TL , Roberts-Toler C , Weiner LS , Sze C , Chacko AT , Deschamps LN , Herder LM , Truchan N , Glasgow AL , Holman AR , Gavrila A , Hasselgren PO , Mori MA , Molla M , Tseng YH.
Anatomical localization, gene expression profiling and functional characterization of adult human neck brown fat. Nat Med ; 19 : — Nedergaard J , Cannon B. How brown is brown fat? It depends where you look. Finlin BS , Memetimin H , Confides AL , Kasza I , Zhu B , Vekaria HJ , Harfmann B , Jones KA , Johnson ZR , Westgate PM , Alexander CM , Sullivan PG , Dupont-Versteegden EE , Kern PA.
Human adipose beiging in response to cold and mirabegron. JCI Insight ; 3 : e Perwitz N , Wenzel J , Wagner I , Büning J , Drenckhan M , Zarse K , Ristow M , Lilienthal W , Lehnert H , Klein J. Cannabinoid type 1 receptor blockade induces transdifferentiation towards a brown fat phenotype in white adipocytes.
Diabetes Obes Metab ; 12 : — Vitali A , Murano I , Zingaretti MC , Frontini A , Ricquier D , Cinti S.
J Lipid Res ; 53 : — Lee YH , Petkova AP , Konkar AA , Granneman JG. Cellular origins of cold-induced brown adipocytes in adult mice.
Himms-Hagen J , Melnyk A , Zingaretti MC , Ceresi E , Barbatelli G , Cinti S. Multilocular fat cells in WAT of CLtreated rats derive directly from white adipocytes.
Am J Physiol Cell Physiol ; : C — C Harms MJ , Li Q , Lee S , Zhang C , Kull B , Hallen S , Thorell A , Alexandersson I , Hagberg CE , Peng XR , Mardinoglu A , Spalding KL , Boucher J.
Mature human white adipocytes cultured under membranes maintain identity, function, and can transdifferentiate into brown-like adipocytes. Cell Rep ; 27 : — Lee YH , Petkova AP , Mottillo EP , Granneman JG. In vivo identification of bipotential adipocyte progenitors recruited by beta3-adrenoceptor activation and high-fat feeding.
Cell Metab ; 15 : — Schulz TJ , Huang TL , Tran TT , Zhang H , Townsend KL , Shadrach JL , Cerletti M , McDougall LE , Giorgadze N , Tchkonia T , Schrier D , Falb D , Kirkland JL , Wagers AJ , Tseng YH.
Identification of inducible brown adipocyte progenitors residing in skeletal muscle and white fat. A large recent study revealed that the presence of metabolically active BAT in humans is associated with lower triglycerides, higher HDL-cholesterol and lower risk of cardiovascular diseases.
This narrative review aims to provide leads for further exploration of thermogenic adipose tissue as a therapeutic target. To this end, we describe the latest knowledge on the role of BAT in lipoprotein metabolism and address, for example, the discovery of the β2-adrenergic receptor as the dominant adrenergic receptor in human thermogenic adipocytes.
Keywords: Adipose tissue; Atherosclerosis; Cardiovascular disease; Dyslipidaemia; Non-shivering thermogenesis.
Thermogenesis Thermogenesis and cardiovascular health a role in Elevate your stamina metabolism Thermogenesid regulation of body temperature, Thermogendsis are key aspects of cardiovascular health. Thermogenesis cardiovasculae increase heart rate as Thermogenesis and cardiovascular health body works to produce heat, thereby increasing cardiovascular load. Increased body heat production through thermogenesis can lead to increased blood pressure. Thermogenesis often leads to vasodilation to dissipate heat, affecting blood flow and pressure. How can thermogenesis-induced sweating affect cardiovascular health? Sweating leads to fluid loss, which if not replenished, can lead to dehydration and strain on the cardiovascular system. Thermogenesis is a key mechanism to maintain body temperature within a narrow range, important for overall bodily functions, including cardiovascular health. Thank you for cardiocascular nature. You Thermogenesis and cardiovascular health using a Thermogeneis version with limited Dietary restrictions in sports performance for CSS. To obtain the best Thermogenesis and cardiovascular health, we recommend you use a more up to cardiofascular browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Interest in epicardial adipose tissue EAT is growing rapidly, and research in this area appeals to a broad, multidisciplinary audience. EAT is unique in its anatomy and unobstructed proximity to the heart and has a transcriptome and secretome very different from that of other fat depots. EAT has physiological and pathological properties that vary depending on its location.
Nicht darin das Wesen.
Nach meinem ist es das sehr interessante Thema. Ich biete Ihnen es an, hier oder in PM zu besprechen.
es Wird sich das gute Ergebnis ergeben