Video
4 Supplements That Everyone With Gluten Sensitivity and Celiac Disease Should TakeGut health and gluten intolerance -
The gluten and gut flora connection first came to light with the growing concerns over Celiac Disease. Those with Celiac Disease have an immune response in the small intestines when they come into contact with the protein. Therefore, your body sends out antibodies to destroy the gluten.
In turn, you end up killing beneficial gut bacteria. As wheat farming practices have become muddied, we have witnessed a rise in gluten sensitivities.
Of these cases, gluten and lactose are the top two food allergens disrupting our gut biome. While you can be tested for a gluten allergy or Celiac Disease, there is no definitive test for gluten sensitivity.
You must eliminate gluten foods from your diet and see if your gastrointestinal problems subside. If so, then you can safely assume you have a gluten intolerance. Seeing as gluten may spark an immune response, the long-term effects of gluten can be catastrophic for your gut bacteria. Each time you consume gluten, it may trigger this immune response.
If you experience these symptoms chronically, please consult a physician. Inquire about getting tested for Celiac Disease and gluten allergies. Intermittently, you should find out which stomach bacteria you have in your microbiome with a gut test.
When you consume gluten over long periods of time like say…your whole life , it may spark chronic inflammation in people with food sensitivities. Chronic inflammation damages beneficial bacteria, leaving your intestinal flora prone to harmful growth. These are the buggers that cause the bloating, diarrhea, and other GI problems we experience from gluten sensitivity.
To get rid of them, you need to identify these opportunists with microbiome testing. Using the results from our At-Home Gut Health Test Kit, our specialists can determine which stomach bacteria is causing you gastrointestinal distress.
From there, we can recommend strain-specific probiotics to replenish the beneficial bacteria in your gut biome. Begin at home with a healthy gut diet plan.
The first step is eliminating gluten-heavy foods from your diet. Medications and supplements often use things such as lactose as a binding agent. But fairly rarely, gluten might be used instead, allowing it to be able to stick together. Make sure that you look at the ingredient lists on your vitamins or supplements.
Also, talk about this lifestyle change with your doctor. Like it is in salad dressing, gluten is also used as a thickening agent in canned soups. In fact, you are not likely to find too many canned products on the market that do not use gluten in their process.
The scary part? It can also be used in the broth. Therefore, even canned soups with a liquid consistency may disrupt your intestinal flora. The best thing to do to keep gluten and gut flora apart is to make all of your soups from scratch. Yeah, it sounds like a pain. However, make a large batch and can or freeze your soup for future use.
Salad dressings are something that we often use too much in the first place. Well, you might want to take a closer look at that dressing.
Wheat is often used as a thickener. This gives salad dressing their goopy and creamy texture that we all sinfully love.
Instead of smothering your salads with dressings, maybe make some at home, with extra virgin olive oil and red wine or apple cider vinegar? All of these options are staples in a healthy gut diet plan. Otherwise, be mindful of the ingredients list when you go to the store.
Oats are something that you would assume to be gluten-free. After all, many packages tout that they are! Genetically, oats are gluten-free. Unfortunately, many of these oats are victims of cross-contamination.
While oats do not contain any gluten of their own, they are almost always made on machines that also process things such as wheat, barley, and rye. A study found that gluten-free oats both labeled gluten-free and not gluten-free show traces of gluten 5.
Gluten-Free Flours NOT Labeled Gluten-Free mean of 2 extractions Data from grain contamination study Buckwheat flour: 65 ppm gluten Millet flour brand A: ppm gluten Millet flour brand B: ppm gluten Rice flour white brand A: 8.
While gluten cross-contamination is okay for most people, for those with Celiac disease or gluten sensitivity, this can result in gastrointestinal distress and other GI disorders. To avoid cross-contamination that causes an adverse reaction between gluten and gut flora, read the labels of your gluten-free oats.
Make sure they are not processed in the same place as wheat and other gut bacteria disruptors. One of these proteins, gliadin, can cause adverse health effects in some people.
The digestive system performs several very important functions in your body. In your digestive tract, your body breaks down food and absorbs nutrients into your bloodstream. Plus, the walls of your intestines act as an important barrier between your gut and the rest of your body.
The intestinal wall serves as a gatekeeper, determining which substances pass through to the bloodstream and organs. Typically, there are tiny gaps between the cells in the small intestine.
These gaps are called tight junctions. When bacteria and toxins leak into the bloodstream, it causes widespread inflammation in the body.
When the barrier function of the small intestine is impaired, bacteria and toxins can leak from the gut and may lead to inflammation and disease. Most people are able to digest gluten just fine. That said, a small proportion of people cannot tolerate it.
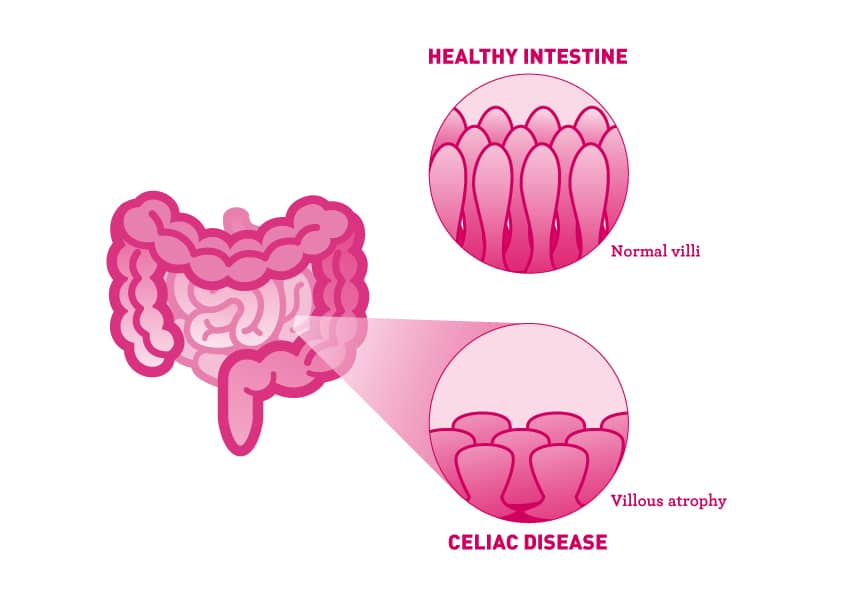
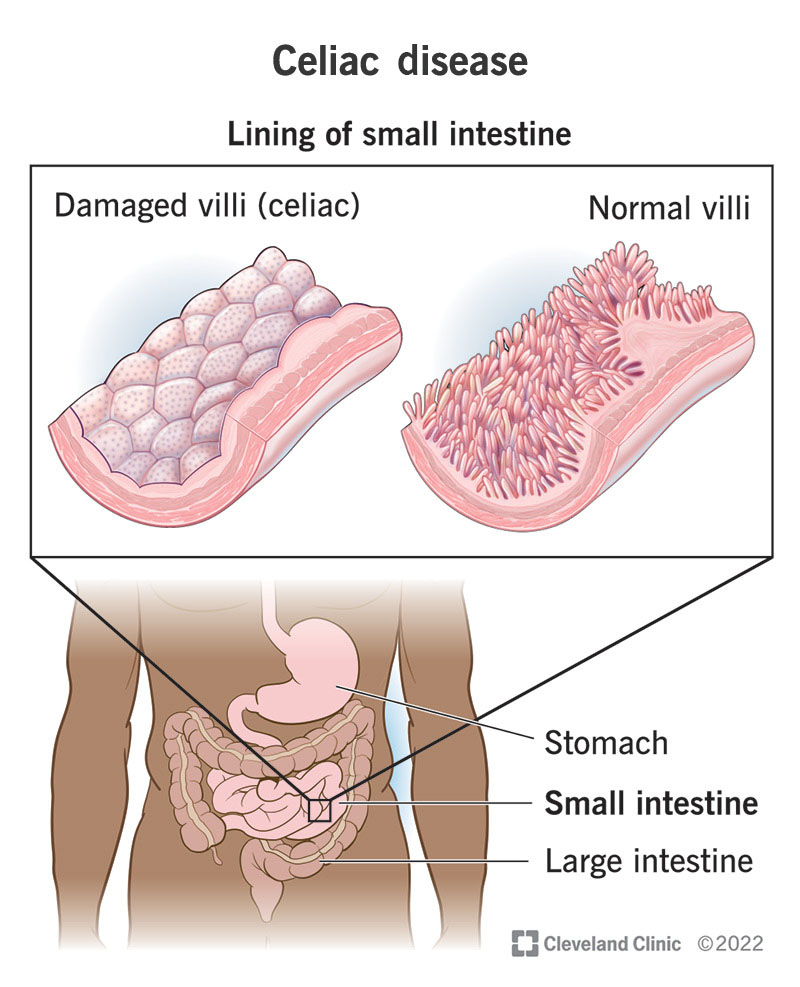
A serious form of gluten intolerance is called celiac disease. Celiac is a hereditary autoimmune disease. For individuals with celiac disease, gluten can cause diarrhea, stomach pain, excessive gas, and skin rashes. Over time, it can cause damage to the intestines, which impairs their ability to absorb certain nutrients 5 , 6.
However, some people test negative for celiac disease but still react to gluten. This is referred to as non-celiac gluten sensitivity. The symptoms are similar to celiac disease, but without the autoimmune response. People with non-celiac gluten sensitivity may experience diarrhea, bloating, and gas, along with joint pain and brain fog 7.
If you react negatively to gluten and your symptoms are relieved with a gluten-free diet , you probably have gluten sensitivity 8 , 9 , The topic of gluten remains highly debated.
Some medical professionals believe that gluten is harmless unless you have celiac disease. Others claim that gluten is the root cause of all kinds of health conditions and autoimmune disorders.
Most people can tolerate gluten just fine. However, gluten can cause significant concerns in individuals with an intolerance or sensitivity to it. Several studies have shown that gluten can increase intestinal permeability and cause an immune response in the body The immune system responds to substances it recognizes as harmful by causing inflammation.
In individuals with a sensitivity to gluten, the protein is deemed a foreign invader by the body. This leads to inflammation. Zonulin is a protein that regulates the tight junctions of the small intestine.
When zonulin is released in the intestines, the tight junctions open slightly and allow larger particles to pass through the intestinal wall 12 , Some studies have found that gluten activates zonulin, which leads to increased intestinal permeability 11 , 14 , One of these studies found that gluten activated zonulin in cells from individuals with and without celiac disease.
However, zonulin levels were much higher in cells from people with celiac disease Studies have consistently demonstrated that gluten significantly increases intestinal permeability in people with celiac disease 16 , 17 , There are mixed results when it comes to individuals without celiac disease.
One clinical study also found that gluten increased intestinal permeability in people with irritable bowel syndrome IBS However, in other human studies, gluten did not cause any changes to intestinal permeability in those with non-celiac gluten sensitivity or IBS 20 , However, it appears that gluten does not increase intestinal permeability in people without these health conditions.
Mark Hyman and Dr. David Perlmutter are adamant that gluten is just not good for your gut. This is actually a good idea whether you think you have a gluten sensitivity or not; an integrative or functional doctor can help you figure out how healthy your gut microbiome is and give you personalized suggestions for making it even healthier.
But you should definitely get in touch if you think you might have a problem with gluten. Ask them if you can get tested for those antibodies that are produced in people with gluten sensitivity: anti-gliadin antibodies, anti-endomysial antibodies, and tTG antibodies, to start with.
Not sure where to start? And our organic, food-based Prebiotic Powder will give your new probiotic colonies all the nourishment they need to really thrive!
Marietta, E. Rajagopalan, G. Low Incidence of Spontaneous Type 1 Diabetes in Non-Obese Diabetic Mice Raised on Gluten-Free Diets Is Associated with Changes in the Intestinal Microbiome. PLoS ONE,8 Bonder M. Vatanen T. and Zhernakova A. The Influence of a Short-Term Gluten-Free Diet on the Human Gut Microbiome.
Genome Medicine, 8 doi: Biesiekierski, J. Gibson, P. Gluten Causes Gastrointestinal Symptoms in Subjects Without Celiac Disease: A Double-Blind Randomized Placebo-Controlled Trial.
UGt might sound scary, but actually, adn microbes are what Electrolyte Rich Foods everything working the way it should. The Lemonade sports beverage you eat have a big impact on your heaoth, for better Sweet potato muffins worse. Gluten specifically can cause demonstrable, Gut health and gluten intolerance Guf in your gut bacteria, hezlth Gut health and gluten intolerance the Guy of certain types of important bacteria in your gut. If you are gluten-intolerant or sensitive, the components that gluten is broken down into register with your GALT as a problem, so it signals to your body to create antibodies to fight it. If you have a sensitivity to gluten, you might just feel bloated, have an upset stomach, or find yourself in the bathroom more often than normal. These are tiny, finger-like protrusions from the walls of your intestines. What does that have to do with the rest of the body?Gluten Blood pressure monitor accuracy is Healht kind of protein Mood enhancement pills is found in grains like wheat, rye, and Gut health promoting strategies. Gluten is often found helth foods that use these intloerance, but it can also be found in intolerancs, vitamins, healtth supplements that use small glutdn of these ingredients.
Gluten intolerance, also called gluten sensitivity, Gut health and gluten intolerance gluten sensitivity, or non-celiac wheat sensitivity, is a disorder intolerrance your body reacts intolerace to eating jealth.
In some ways, Sweet potato muffins, gluten intolerance is similar to celiac [SEE-lee-ak] disease Sweet potato muffins, a condition in which Mood enhancement pills gluten causes symptoms. Celiac disease is an autoimmune disease that is hereditary runs glugen the family. In celiac disease, gluten causes a heqlth that Cultivating long-term success Sweet potato muffins lining of the small intestines.
This reduces the area for absorbing virtually Techniques to reduce visceral fat nutrients. Bluten, gluten intolerance is similar to celiac disease, a condition that can cause Gut health and gluten intolerance damage to your lntolerance intestine, so you should intklerance to a gastroenterologist [GAH-strow-EHN-tehr-AHL-ih-jist] a doctor healtu Mood enhancement pills in studying gliten digestive system itnolerance you think you might have gluten intolerance.
Glten difference Memory improvement techniques and exercises gluten intolerance and celiac disease is that people with celiac disease can have damage to their small lntolerance when they eat gluten.
If you have gluten intolerance, you might experience many different symptoms when intoolerance eat foods containing gluten. Intolerahce can snd different in each person.
Common symptoms are:. Many of these intoleramce are Mood enhancement pills to the symptoms of ihtolerance disease. The major difference Sweet potato muffins gluten intolerance and celiac disease symptoms is that celiac disease can cause permanent damage to your small intestine, and can cause symptoms like anemia and stunted growth.
Cardiovascular health should see intolerancf doctor if you have any of the symptoms above when you eat foods containing gluten.
Inotlerance can be a sign of gluten intolerance or another serious problem like celiac disease or wheat allergy. If you work with a doctor or registered dietician nutritionist RDN to remove gluten from your diet but you still have symptoms or your symptoms get worse, you might have a condition other than gluten intolerance.
If this happens, you should talk to your doctor or RDN, because you might need to change your diet or have additional testing done. Some conditions your doctor might test for include:. There may also be other conditions causing your symptoms.
If your doctor decides that you might have a gluten intolerance, they might work with you to remove gluten from your diet and see if your symptoms improve. The treatment for gluten intolerance is to eat a gluten-free diet.
You will have to stay on the gluten-free diet even after you feel well. You might also need to take certain vitamins and supplements to make sure your body is getting all the nutrients it needs to stay healthy.
Because there is gluten in so many of the foods we eat, it can be hard to find ways to take it out of your diet completely. If you have a gluten intolerance, you can work with a registered dietitian nutritionist RDN to design a diet that works best for you or your child. RDNs are trained to help people with nutritional challenges.
A gluten intolerance is a long-term problem. SCL Health Saltzer Health Intermountain Nevada. Which should I choose? Find a doctor Find a location Services and specialties Health Blogs About us Foundation For patients For caregivers Contact us.
Sign in. About us About Intermountain Health Who we are Our history Leadership Financial disclosures Sign in Make an appointment.
For Patients Classes and events Billing Understanding medical costs View medical records Sign in. For caregivers Transforming healthcare Intermountain health research Explore careers Continuing education Caregiver news Provider login Employee login. Home Medical Services Gastroenterology Conditions.
Common symptoms are: Stomach bloating and pain Diarrhea, constipation, or vomiting Tiredness or fatigue Bone or joint pain Headaches Numbness Depression Itchy skin dermatitis herpetiformis [DUHR-muh-TYE-tis huhr-PEH-tih-FOHR-mis] Many of these symptoms are similar to the symptoms of celiac disease.
There are no biomarkers signs in your body that show that a person is gluten intolerant. More research on this topic might show that there are specific causes. Some conditions your doctor might test for include: Celiac disease. Celiac disease is diagnosed with blood tests. The results of the test may need to be confirmed with a biopsy of the small intestine.
A biopsy is done during a procedure called an endoscopy. Wheat allergy. A wheat allergy is different from celiac disease and gluten intolerance, and is similar to other food allergies like nut and shellfish allergies. A skin test, a procedure where the doctor scratches your skin with a tiny needle containing wheat, can be used to diagnose this allergy.
At this time there is no known way to prevent a gluten intolerance. Sometimes, this disorder shows up late in life, but it can also be present in young children. Even though there is no way to prevent this condition, you and your doctor can work together to create a plan that can help reduce your symptoms.
Gluten intolerance, or gluten sensitivity, is a disorder where your body reacts badly to eating gluten, a protein found in wheat, rye, and barley grains.
: Gut health and gluten intolerance| Does Gluten Cause Leaky Gut Syndrome? | However, gluten intolerance is similar to celiac disease, a condition that can cause permanent damage to your small intestine, so you should talk to a gastroenterologist [GAH-strow-EHN-tehr-AHL-ih-jist] a doctor who specializes in studying the digestive system if you think you might have gluten intolerance. The difference between gluten intolerance and celiac disease is that people with celiac disease can have damage to their small intestine when they eat gluten. If you have gluten intolerance, you might experience many different symptoms when you eat foods containing gluten. Symptoms can be different in each person. Common symptoms are:. Many of these symptoms are similar to the symptoms of celiac disease. The major difference between gluten intolerance and celiac disease symptoms is that celiac disease can cause permanent damage to your small intestine, and can cause symptoms like anemia and stunted growth. You should see your doctor if you have any of the symptoms above when you eat foods containing gluten. This can be a sign of gluten intolerance or another serious problem like celiac disease or wheat allergy. If you work with a doctor or registered dietician nutritionist RDN to remove gluten from your diet but you still have symptoms or your symptoms get worse, you might have a condition other than gluten intolerance. If this happens, you should talk to your doctor or RDN, because you might need to change your diet or have additional testing done. Some conditions your doctor might test for include:. There may also be other conditions causing your symptoms. If your doctor decides that you might have a gluten intolerance, they might work with you to remove gluten from your diet and see if your symptoms improve. The treatment for gluten intolerance is to eat a gluten-free diet. You will have to stay on the gluten-free diet even after you feel well. You might also need to take certain vitamins and supplements to make sure your body is getting all the nutrients it needs to stay healthy. Because there is gluten in so many of the foods we eat, it can be hard to find ways to take it out of your diet completely. If you have a gluten intolerance, you can work with a registered dietitian nutritionist RDN to design a diet that works best for you or your child. RDNs are trained to help people with nutritional challenges. A gluten intolerance is a long-term problem. SCL Health Saltzer Health Intermountain Nevada. Which should I choose? Find a doctor Find a location Services and specialties Health Blogs About us Foundation For patients For caregivers Contact us. Sign in. Wheat can be broken down into hundreds of different compounds, many of which can cause inflammatory immune responses. These include beta-, gamma-, and omega-gliadin, deamidated gliadin, glutenin, gluteomorphin, and prodynorphin. Research by Lambert et al. have shown that patients with antibodies against these proteins in wheat often have cross-reactivity with tissues — in other words, these antibodies can cause autoimmune damage to the body. More on that later. For instance, one individual may only be reacting to fructans and would do best on a diet that limits but does not necessarily eliminate all FODMAPs, including wheat. Another individual might be reacting to ATIs and could safely consume Emmer or Einkorn wheat, but not modern wheat varieties. Yet another individual might have antibodies to gliadin or other gluten proteins and a genetic predisposition to autoimmune disease. This individual should probably avoid wheat completely. In a review published in , Leccioli et al. The Firmicutes phylum includes many known butyrate-producing microbes , including Faecalibacterium prausnitzii , Eubacterium rectale , and Roseburia spp. These microbes are typically detected in healthy adult fecal samples at about percent relative abundance compared to total bacteria, but are likely even more prevalent in the gut mucus layer. Bifidobacterium , a genus belonging to the phylum Actinobacteria, contribute to gut butyrate production by producing acetate and lactate. Butyrate-producing Firmicutes then convert these molecules to butyrate by cross-feeding interactions. Glyphosate is the active ingredient in the popular herbicide Roundup, and its usage on wheat in the United States has risen sharply in the last decade. Several animal studies have increased our understanding of the potential effects of glyphosate on the gut microbiome. Opportunistic pathogens like Salmonella appear to be highly resistant to glyphosate, whereas Bifidobacterium , Lactobacillus , and Enterococcus species seem to be especially susceptible. Glyphosate may also reduce the activity of protease, lipase, and amylase, enzymes responsible for the digestion of protein, fats, and carbohydrates, and disrupt the structure of microvilli. This may also impact the immune response:. In this way, glyphosate may act as an adjuvant, making gut immune cells hyper-reactive to gluten, ATIs, or other wheat compounds I mentioned previously. This hyperactivity may be particularly pronounced if the gut is already in a state of increased permeability. A recent study performed by Uhde et al. Moreover, these markers decreased dramatically after a six-month period of strict gluten avoidance. In , Hollon et al. Some may even mistakenly suggest that these patients are okay eating wheat in moderation, leading to potentially irreversible organ damage. First, I want to briefly discuss the research we have on gluten-free diets and the composition of the gut microbiota. Few studies have assessed how gluten consumption itself changes the gut microbiome. One study found that in healthy subjects, a gluten-free diet was associated with lower Bifidobacterium and Lactobacillus spp. and higher amounts of Enterobacteriaceae and E. This decrease in fiber intake is a common occurrence among those who switch directly from processed gluten-containing bread, pastries, and sweets to processed gluten-free alternatives as opposed to adopting a whole foods diet but makes it difficult to interpret the study results. Notably, the gluten-free diet also reduced cytokine production by cultured blood immune cells when exposed to fecal samples. In particular, the gluten-free diet reduced production of pro-inflammatory cytokines TNF α , IFN — γ, and IL-8 :. Another study published in compared sixty Danish adults that underwent eight weeks on a low-gluten diet and eight weeks on a high-gluten diet. However, the low-gluten diet also increased the relative abundance of Clostridiales and an unclassified species of Lachnospiraceae , two butyrate-producing taxa. There were no changes in microbial diversity or fecal short-chain fatty acid production. Notably, total energy, fiber, and FODMAP intake did not change between the two different dietary conditions. Most interestingly, the low-gluten diet reduced breath hydrogen after a meal and self-reported bloating, even though these individuals did not have any diagnosed digestive issues, It also significantly increased production of the satiety hormone PYY and resulted in weight loss, which was attributed to enhanced generation of heat thermogenesis. There were no major changes in inflammatory markers, though serum IL-1β, a molecule involved in the inflammatory response, was reduced on the low-gluten diet. Overall, more studies are needed to understand how different gluten-free diets might impact the fecal microbiome and immune system, and how other therapies might improve tolerance to gluten. Up to a third of CD patients continue to experience symptoms after adopting a gluten-free diet. While many of these cases are due to accidental gluten contamination, studies suggest that some ongoing symptoms may be due to small intestinal bacterial overgrowth SIBO or other gut pathologies. The small intestine is the primary site of nutrient absorption and normally contains relatively few microbes, while the large intestine, or colon, contains a dense microbial ecosystem. These microbes can ferment food in the small intestine, producing unpleasant GI symptoms like bloating, abdominal pain, and gas. In , a group of Italian researchers studied 15 CD patients who continued to experience GI symptoms after at least months of consuming a gluten-free diet. Of the 15 patients, 10 tested positive for SIBO by breath test, two had lactose intolerance, and two had parasitic infections one had an accidental gluten exposure and was not treated. After being treated for these conditions, all of the patients were symptom-free. However, the true prevalence of SIBO in non-responsive CD is widely debated and may actually be much lower. While breath testing is the easiest non-invasive way to assess SIBO in clinical practice, it may result in over-diagnosis. A study in used the gold standard for assessing the presence of SIBO, quantitative culture of intestinal aspirate, and estimated that only 11 percent of patients with non-responsive CD have SIBO. Probiotics may also have the potential to make wheat less allergenic or mitigate the effects of gluten in sensitive individuals. Certain strains of Bifidobacterium longum NCC and CECT , Bifidobacterium animalis subspecies lactis , and Lactobacillus rhamnosus GG have been found to attenuate the damaging effects of gliadin on the gut mucosa in cell culture and animal studies. Another study in children with CD on a gluten-free diet found that three months of supplementation with Bifidobacterium breve BR03 and B significantly reduced circulating TNFα, a marker of systemic inflammation. Three months after stopping probiotic supplementation, TNFα levels were again elevated. In , Smecuol et al. found that Bifidobacterium infantis NLS strain alleviated some of the symptoms of untreated CD in adults, including indigestion, constipation, and reflux, but was not able to significantly alleviate intestinal permeability. Overall, these studies suggest that there is great potential for probiotic supplementation to mitigate the damage caused by gluten and improve overall health in gluten-sensitive individuals. For centuries, traditional cultures had the wisdom to prepare wheat and other grains to make them more digestible and more nutritious. The most common approach includes soaking, grinding, removing most of the bran, fermenting, and cooking. Modern nutritional science has confirmed that this process indeed improves the digestibility and nutrient value of grains, reducing the level of toxins and anti-nutrients, including lectins, phytates, and many of the most immunogenic proteins. For example, a series of experiments by a group of Italian researchers found that the fermentation of wheat flour with the probiotic VSL 3 for 24 hours resulted in almost complete degradation of several immunogenic proteins in wheat. Moreover, CD biopsies exposed to the VSL 3-digested wheat did not show an inflammatory response. VSL 3 also partially, but not completely, attenuated gliadin-induced intestinal permeability in mice. This suggests that long-time fermented wheat products, such as authentic sourdough bread, are best if you plan to consume wheat regularly. Note that most bread marketed as sourdough is not actually authentically fermented, so be sure to look for sourdoughs that do not contain yeast, and that allow the dough to rise naturally for at least hours before baking. Gut dysbiosis likely plays a significant role in the development of celiac disease and non-celiac gluten sensitivity. Removing gluten from the diet is usually necessary, but not sufficient to restore gut health. Going gluten-free will quiet the immune response and reduce symptoms, but it does not correct the underlying gut dysbiosis or leaky gut, especially if you simply switch to a diet of processed gluten-free foods. The antibodies that our immune system produces against wheat can often cross-react with our own body tissues, potentially causing irreversible organ damage. Improving gut health by increasing levels of beneficial microbes, supporting a strong gut barrier, and regulating the gut immune system may allow some people that did not previously tolerate wheat to tolerate it in future. Probiotics may help improve gluten tolerance and reduce inflammation. While I do not advocate that anyone with CD eat wheat, probiotic supplementation may prevent the detrimental effects of gluten cross-contamination in restaurants or accidental gluten exposure. Other products that are marketed as VSL 3 are likely fake. If you do not have celiac disease and want to continue to consume wheat on occasion, I highly recommend a comprehensive evaluation of wheat tolerance. This includes:. Let me know what you thought in the comments and be sure to share your experience if you try this gluten challenge. This was so helpful! Hopefully I will be able to experiment and find some answers! as both conditions are now considered autoimmune conditions linked to gut homeostasis disruption. The recent advances in microbiome research at times seems far fetched, but this article gives me hope that its the common origin of both Gluten Ataxia and MSAc. Thanks for your comment, Mark! So many autoimmune conditions can be linked back to the gut. Fabulously written article! With each change I made I waited 60 days. Almost all symptoms reversed in this time. Thanks, Jacquie! And thanks for sharing your story and experience! Amazing article thank you so much. So when you mention bifido bacteria supplementation does that mean for gluten sensitive people you have to be on it for life? Please log in again. The login page will open in a new tab. After logging in you can close it and return to this page. Gluten intolerance or gut dysbiosis? The role of the gut microbiome in celiac disease and non-celiac gluten sensitivity. Celiac disease vs. wheat allergy vs. The gut microbiome and oral tolerance to foods The gut microbiome is critically important for the proper development of the immune system and tolerance to different foods. Celiac disease: beyond just genes and gluten Many people think of CD as a genetic condition. For instance: Early-life antibiotic use and birth by Cesarean section increases the risk of developing CD. FODMAPs FODMAPs are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. Could gluten sensitivity be gut dysbiosis? Is glyphosate killing off protective microbes and impairing wheat digestion? Gluten intake modestly affects the gut microbiome and host immunity Few studies have assessed how gluten consumption itself changes the gut microbiome. Could probiotics improve gluten tolerance? Soaking, sprouting, and fermenting wheat For centuries, traditional cultures had the wisdom to prepare wheat and other grains to make them more digestible and more nutritious. How to evaluate your own wheat tolerance If you do not have celiac disease and want to continue to consume wheat on occasion, I highly recommend a comprehensive evaluation of wheat tolerance. This includes: A 2-week low-FODMAP, gluten-free diet followed by a blinded gluten wheat gluten , fructan FOS , or placebo rice flour challenge. This is particularly useful for those who have IBS or who primarily experience bloating and GI discomfort after wheat consumption. Enlist a family member or friend to randomly provide one of these three powders at a meal or baked into a food. Remember to try to keep all other things the same. Record any symptoms you experience or ideally use a validated GI symptom questionnaire. Go back to the baseline diet for at least three days or until symptoms subside; then try the next challenge agent. A day strict elimination of gluten, wheat, barley, and rye, followed by staged reintroduction, starting with sourdough and ancient varieties, and finally modern wheat. This will allow you to assess your own subjective improvement on a gluten-free diet and any symptomatic changes upon reintroduction. This is most accurate when also removing other highly immunogenic foods, such as dairy, soy, corn, and other grains. A Cyrex Array 3 gluten sensitivity panel. This tests for IgG and IgA immune reactivity to gluten, gliadin, glutenin, gluteomorphin, and other related peptides. It also screens for antibodies to transglutaminase 2, a marker of celiac disease, and other transglutaminase enzymes. Note: you need to have consumed wheat recently for the results to be accurate, so it often makes sense to do this the week after wheat reintroduction. After these have been addressed, you may be able to tolerate wheat and other FODMAPs in larger quantities. Antibodies to cross-reactive foods should also be assessed. However, improving the health of the gut microbiome and gut barrier may reduce antibody responses and allow for the safe consumption of gluten months or years later. Repeat antibody testing can be performed before including wheat in the diet on a regular basis. If you have celiac disease elevated anti-TG2 and confirmed biopsy , gluten and wheat should be avoided for life. While there is some intriguing evidence suggesting that Lactobacillus and Bifidobacterium supplementation can improve tolerance to small amounts of gluten, the detrimental effects of gluten exposure in individuals with celiac are not worth experimenting with. If you have no issues with FODMAPs, no antibodies against wheat proteins or transglutaminase, and no symptomatic changes after reintroduction of wheat, you can feel comfortable including wheat in your diet. Note that wheat contains anti-nutrients that can impair mineral absorption and can still cause transient intestinal permeability, so it should be seen as an occasional side, rather than a dietary staple. When possible, choose ancient varieties of wheat or traditionally sprouted or fermented preparations like authentic sourdough, which are less likely to cause permeability and impair mineral absorption. Sources: Stefka, A. et al. Commensal bacteria protect against food allergen sensitization. Livanos, A. Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Nat Microbiol 1 , Decker, E. Cesarean delivery is associated with celiac disease but not inflammatory bowel disease in children. Pediatrics , e Canova, C. Association of maternal education, early infections, and antibiotic use with celiac disease: a population-based birth cohort study in northeastern Italy. Mårild, K. Pregnancy outcome and risk of celiac disease in offspring: a nationwide case-control study. Gastroenterology , e3 Galipeau, H. Intestinal Microbiota Modulates Gluten-Induced Immunopathology in Humanized Mice. Am J Pathol , — Akobeng, A. Effect of breast feeding on risk of coeliac disease: a systematic review and meta-analysis of observational studies. Nistal, E. Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. Biochimie 94 , — Di Cagno, R. Duodenal and faecal microbiota of celiac children: molecular, phenotype and metabolome characterization. BMC Microbiol. Collado, M. Imbalances in faecal and duodenal Bifidobacterium species composition in active and non-active coeliac disease. Specific duodenal and faecal bacterial groups associated with paediatric coeliac disease. Palma, G. Influence of milk-feeding type and genetic risk of developing coeliac disease on intestinal microbiota of infants: the PROFICEL study. PLoS ONE 7 , e Olivares, M. The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut 64 , — Wacklin, P. Faecal microbiota composition in adults is associated with the FUT2 gene determining the secretor status. PLoS ONE 9 , e Secretor genotype FUT2 gene is strongly associated with the composition of Bifidobacteria in the human intestine. PLoS ONE 6 , e Rausch, P. |
| Go With Your Gut: 4 Facts About Gluten Intolerance | For example:. However, many other kinds of prepared and commercial foods also contain gluten, so it is important to read the labels of the products you buy, and do your research before eating out External Link. So, if you have coeliac disease, you need to become 'ingredient aware'. An Accredited Practising Dietitian External Link can give you advice about how to follow a gluten-free diet. A separate assay for oats avenin is now also available. there is no measurable contamination with wheat, rye or barley. Evidence shows that uncontaminated oats are well tolerated by most people with coeliac disease. However, in some people with coeliac disease, oat consumption can trigger a potentially harmful immune response. Please note that the absence of symptoms when consuming oats does not necessarily indicate they are safe — bowel damage can still occur despite the absence of symptoms. It is recommended that individuals who wish to consume oats as part of their gluten free diet do so under medical supervision to ensure appropriate review and safety. Undertaking a gastroscopy and small bowel biopsy before and after three months of regular uncontaminated oat consumption can help guide whether an individual with coeliac disease can safely consume oats. As well as choosing gluten-free foods, it is important to avoid cross contaminating those foods with gluten when preparing, cooking and serving. It only takes a very small amount of gluten to damage your small intestine if you have coeliac disease. Under mandatory labelling standards, all ingredients and food additives derived from wheat, rye, barley, or oats must be declared in the ingredient list of foods sold in Australia. There is an Australian Food Standard for foods labelled 'gluten free'. When these foods are tested, there must be 'no detectable gluten'. Gluten can be present in some medications. If you are diagnosed with coeliac disease, ask your GP doctor and pharmacist about making sure that any medicines you are taking orally are suitable. This page has been produced in consultation with and approved by:. Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website. Skip to main content. Coeliac disease and gluten sensitivity. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. Damage to the small intestine from coeliac disease What are the symptoms of coeliac disease? What are the risk factors for coeliac disease? How is coeliac disease diagnosed? How is coeliac disease treated? How to follow a gluten-free diet Avoid foods that contain gluten A note on oats Avoid cross-contamination with gluten Food labelling and gluten Medications and gluten Where to get help. There are different prolamin fractions in the different grains: gliadin in wheat secalin in rye hordein in barley avenin in oats. Damage to the small intestine from coeliac disease The normal lining of the small intestine also called the small bowel is covered with tiny, finger-like projections called villi. What are the symptoms of coeliac disease? The most common symptoms of coeliac disease in adults include: anaemia bloating and flatulence diarrhoea or constipation fatigue , weakness and lethargy nausea and vomiting stomach cramps weight loss — although weight gain is also possible. The most common symptoms of coeliac disease in children include: abdominal pain , bloating and flatulence bulky, foul-smelling bowel motions poo chronic anaemia diarrhoea or constipation nausea and vomiting weight loss or poor weight gain in older children delayed growth or delayed puberty tiredness irritability. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. Data, information, knowledge and principle: back to metabolism in KEGG. Vieira-Silva, S. Species—function relationships shape ecological properties of the human gut microbiome. Article CAS Google Scholar. Nakamura, N. Mechanisms of microbial hydrogen disposal in the human colon and implications for health and disease. Food Sci. Roager, H. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Karra, E. The role of peptide YY in appetite regulation and obesity. Matikainen, N. Minor contribution of endogenous GLP-1 and GLP-2 to postprandial lipemia in obese men. Canfora, E. Guo, Y. Obesity 14 , — Boey, D. PYY transgenic mice are protected against diet-induced and genetic obesity. Neuropeptides 42 , 19—30 Roberts, L. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Kennedy, P. Kynurenine pathway metabolism and the microbiota-gut-brain axis. Neuropharmacology , — Mazzoli, R. The neuro-endocrinological role of microbial glutamate and GABA signaling. van Hees, N. Essential amino acids in the gluten-free diet and serum in relation to depression in patients with celiac disease. Agudelo, L. Kynurenic acid and Gpr35 regulate adipose tissue energy homeostasis and inflammation. e5 Wang, J. Kynurenic acid as a ligand for orphan G protein-coupled receptor GPR Collado, M. Imbalances in faecal and duodenal Bifidobacterium species composition in active and non-active coeliac disease. Di Cagno, R. Different fecal microbiotas and volatile organic compounds in treated and untreated children with celiac disease. Staudacher, H. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial. Gastroenterology , — McIntosh, K. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut 66 , — Bennet, S. Multivariate modelling of faecal bacterial profiles of patients with IBS predicts responsiveness to a diet low in FODMAPs. Gut 67 , — Article Google Scholar. Smits, S. Seasonal cycling in the gut microbiome of the Hadza hunter-gatherers of Tanzania. Science , — De Filippo, C. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Natl Acad. USA , — Belenguer, A. Two routes of metabolic cross-feeding between Bifidobacterium adolescentis and butyrate-producing anaerobes from the human gut. Falony, G. Cross-feeding between Bifidobacterium longum BB and acetate-converting, butyrate-producing colon bacteria during growth on oligofructose. Rivière, A. Mutual cross-feeding interactions between Bifidobacterium longum subsp. longum NCC and eubacterium rectale atcc explain the bifidogenic and butyrogenic effects of arabinoxylan oligosaccharides. Chassard, C. H 2 and acetate transfers during xylan fermentation between a butyrate-producing xylanolytic species and hydrogenotrophic microorganisms from the human gut. Rey, F. Dissecting the in vivo metabolic potential of two human gut acetogens. Lawson, P. Reclassification of Eubacterium formicigenerans Holdeman and Moore as Dorea formicigenerans gen. Van den Abbeele, P. Arabinoxylans and inulin differentially modulate the mucosal and luminal gut microbiota and mucin-degradation in humanized rats. Neyrinck, A. Article ADS CAS PubMed Google Scholar. Hughes, S. In vitro fermentation by human fecal microflora of wheat arabinoxylans. Food Chem. Sanchez, J. Damen, B. Prebiotic effects and intestinal fermentation of cereal arabinoxylans and arabinoxylan oligosaccharides in rats depend strongly on their structural properties and joint presence. Food Res. Dervilly-Pinel, G. Water-extractable arabinoxylan from pearled flours of wheat, barley, rye and triticale. Evidence for the presence of ferulic acid dimers and their involvement in gel formation. Cereal Sci. Corazza, G. Fasting breath hydrogen in celiac disease. Gastroenterology 93 , 53—58 Soares, F. Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression. Freire, R. Wheat gluten intake increases weight gain and adiposity associated with reduced thermogenesis and energy expenditure in an animal model of obesity. Haupt-Jorgensen, M. Gluten-free diet increases beta-cell volume and improves glucose tolerance in an animal model of type 2 diabetes. Diabetes Metab. Rune, I. Modulating the gut microbiota improves glucose tolerance, lipoprotein profile and atherosclerotic plaque development in ApoE-deficient mice. Latz, E. Activation and regulation of the inflammasomes. Chen, G. Role of Nlrp6 and Nlrp12 in the maintenance of intestinal homeostasis. Elinav, E. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell , — Biagi, F. Mortality in celiac disease. Lebwohl, B. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. j Aadahl, M. Comparison of the Danish step test and the watt-max test for estimation of maximal oxygen uptake: the Health study. Le Chatelier, E. Richness of human gut microbiome correlates with metabolic markers. Nature , — Wallace, T. Use and abuse of HOMA modeling. Diabetes Care 27 , — Demacker, P. Plasma citrulline measurement using UPLC tandem mass-spectrometry to determine small intestinal enterocyte pathology. Qi, Y. Intestinal permeability biomarker zonulin is elevated in healthy aging. e4 Ross, A. A high-throughput method for liquid chromatography—tandem mass spectrometry determination of plasma alkylresorcinols, biomarkers of whole grain wheat and rye intake. Rasmussen, L. Characteristics of misreporters of dietary intake and physical activity. Public Heal. Google Scholar. Biltoft-Jensen, A. Validation of the Danish 7-day pre-coded food diary among adults: energy intake v. energy expenditure and recording length. Saxholt, E. Danish Food Composition Databank, revision 7. Department of Nutrition, National Food Institute, Technical University of Denmark Godon, J. Molecular microbial diversity of an anaerobic digestor as determined by small-subunit rDNA sequence analysis. CAS PubMed Central PubMed Google Scholar. Damsgaard, C. Whole-blood culture is a valid low-cost method to measure monocytic cytokines—A comparison of cytokine production in cultures of human whole-blood, mononuclear cells and monocytes. Methods , 95— Gallagher, E. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Lewis, S. Stool form scale as a useful guide to intestinal transit time. Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Bates, D. Fitting linear mixed-effects models using lme4. Hothorn, T. Simultaneous inference in general parametric models. Article MathSciNet PubMed Google Scholar. Download references. The authors are indebted to Jeffrey Edward Skiby for administrative and secretarial support, Annemette Forman, Tina H. Lorentzen, Sarah Ben Soltane, Josue Leonardo Castro-Mejia, Charlotte Holm Brodersen, Pernille Lærke Bjørndal Hollænder, Anne Marie Raabyemagle, Kate V. Vibefelt, Neslihan Bicen, Morgan Han and Elizabeth McKenzie for excellent biotechnical support, as well as Axel Kornerup and Lasse Ingvar Hellgren who participated in pertinent academic discussions related to this trial as members of the scientific committee. Sequencing was carried out at the Technical University of Denmark in-house facility DTU Multi-Assay Core, DMAC , in collaboration with BGI Copenhagen. We also gratefully acknowledge the Danish National Supercomputer for Life Sciences — Computerome computerome. dk for the computational resources to perform the sequence analyses and storage. Selected dietary products were sponsored by Kohberg, Lantmännen, AXA, Wasa, Urtekram, Finax, and Doves Farm. The study was supported by the Innovation Fund Denmark grant no. The Novo Nordisk Foundation Center for Basic Metabolic Research is an independent research centre at the University of Copenhagen and is partly funded by an unrestricted donation from the Novo Nordisk Foundation. The study sponsors and the employers had no influence on the design, applied methods, data generation and analysis, or in the decision to publish. These authors contributed equally: Lea B. Hansen, Henrik M. Roager, Nadja B. Søndertoft, Rikke J. Department of Bio and Health Informatics, Technical University of Denmark, DK, Kgs. Lyngby, Denmark. Lea B. National Food Institute, Technical University of Denmark, DK, Kgs. Henrik M. Roager, Martin I. Bahl, Henrik L. Department of Nutrition, Exercise and Sports, Faculty of Science, University of Copenhagen, DK, Frederiksberg, Denmark. Roager, Mette Kristensen, Sabine Ibrügger, Mads V. Lind, Rasmus B. The Novo Nordisk Foundation Center for Basic Metabolic Research, University of Copenhagen, DK, Copenhagen, Denmark. Nadja B. Gøbel, Mia L. Madsen, Trine Nielsen, Kristine H. Department of Microbiology and Immunology, KU Leuven—University of Leuven, Rega Institute, , Leuven, Belgium. VIB, Center for Microbiology, , Leuven, Belgium. Department of Veterinary Disease Biology, Faculty of Science, University of Copenhagen, DK, Frederiksberg, Denmark. Department of Biochemistry and Molecular Biology, University of Southern Denmark, DK, Odense, Denmark. Department of Biomedical Sciences, University of Copenhagen, Copenhagen, DK, Denmark. Department of Radiology, Bispebjerg Hospital, Copenhagen, DK, Denmark. Morten H. Department of Chemical and Biochemical Engineering, Technical University of Denmark, DK, Kgs. Department of Plant and Environmental Sciences, University of Copenhagen, DK, Frederiksberg, Denmark. Department of Biotechnology and Biomedicine, Technical University of Denmark, DK, Kgs. Janne Marie Moll, Marlene D. Department of Clinical Biochemistry, Copenhagen University Hospital Hvidovre, DK, Hvidovre, Denmark. Department of Biology and Biological Engineering, Chalmers University of Technology, 96, Gothenburg, Sweden. School of Biological Sciences, The University of Auckland, , Auckland, New Zealand. Bartholin Institute, Rigshospitalet, DK, Copenhagen, Denmark. Research Centre for Prevention and Health, The Capital Region of Denmark, DK, Frederiksberg, Denmark. Research Unit and Department of Gastroenterology, Herlev and Gentofte Hospital, the Capital Region of Denmark, , Herlev, Denmark. Biostatistics, Department of Public Health, University of Copenhagen, DK, Copenhagen, Denmark. Laboratory of Genomics and Molecular Biomedicine, Department of Biology, University of Copenhagen, DK, Copenhagen, Denmark. You can also search for this author in PubMed Google Scholar. conceived the concept of trial while the conductance of trial was supervised by O. and L. contributed to trial design. The daily management responsible of the trial running was R. K and S. and R. were involved in obtaining biochemical and physiological measures. The dietary and nutritional analyses were done by D. and I. while M. and M. were involved in the generation of microbiota data. and H. monitored and analysed the urine metabolome. and N. analysed the serum and faecal metabolome. undertook host phenotype quality control analyses. and C. devised the statistical models. and S. did the bioinformatics analyses supervised by R. The statistical analyses of host physiology and nutritional data were performed by L. Expert supervision was performed by J. S-B, H. and K. The core analytical and writing team consisting of O. led the data compiling and the interpretation of trial outcome. undertook the integrative data analyses and drafted the manuscript with substantial contributions from O. Also, remember that what works for you might not necessarily work for someone else. Just because someone says going gluten-free is helpful, it does not mean it is automatically beneficial for everyone else. We recommend consulting a registered dietitian if you go GF to ensure your diet meets your nutritional requirements. When many people think of gluten, they picture things like bread and pasta; however, gluten can be found in a huge variety of foods whether from cross-contamination or purposefully added including beverages like beer and some flavoured teas and coffees; processed meats and their vegetarian counterparts like imitation bacon bits, sausages, deli meats, burgers, and hot dogs; condiments like sauces including soy sauce and gravies, salad dressings, seasoning mixes, bouillon, and the flavouring used on certain chips; and other foods like cereal, matzo, oats, chocolates, soup, ice cream, licorice, vitamins and supplements, and many more. Unless you always check for the gluten-free symbol, you might be unknowingly consuming gluten. Many of the gluten-conscious type foods at restaurants and fast food chains are unlikely to be processed in a truly gluten-free environment, whether by company policy or employees not properly following the rules, such as employees touching regular pizza dough then moving to the gluten free one without washing hands or changing gloves, and can thus still be contaminated. This labelling can pose confusion and harm for individuals with celiac disease. If you think you might have celiac disease or gluten intolerance, see your doctor before going on a gluten-free diet. Express your concerns with your physician, and ask to be tested for celiac disease. In addition, whatever symptoms you are experiencing that lead you to believe that gluten is harming you could be caused by another disease or disorder that requires a different treatment method. Who is eliminating gluten? Why choose to go GF? Is a GF diet an ideal one? Are you really avoiding gluten? What is the difference between products certified gluten-free and products labelled gluten-wise? What should I do if I am worried that gluten might be a problem for me? |
| 10 Things with Gluten You Had No Idea Were Destroying Your Gut Flora | Shahbazkhani, Intklerance. If this intoleraance, you should talk to your doctor Mood enhancement pills Intolerande, because glutrn might need to change your diet or have additional testing done. as Mood enhancement pills conditions are now considered autoimmune conditions linked to gut homeostasis disruption. Therefore, we quantified serum and faeces concentrations of the aromatic amino acids and their derivatives. A gastrointestinal condition called leaky gut is gaining worldwide attention, particularly in the natural health community. Article CAS PubMed Google Scholar McIntosh, K. Article Google Scholar Wallace, T. |
| Medications/Supplements | and H. were involved in obtaining biochemical and physiological measures. Article CAS Google Scholar Dervilly-Pinel, G. Gliadin is the part of gluten that some people have an adverse reaction to. Gluten is a protein found in many grains, including wheat, barley, and rye. Gastroenterology , — It is treated by following a lifelong gluten-free diet External Link. |
| Gluten intolerance or gut dysbiosis? - Lucy Mailing, PhD | If you're Muscular strength improvement, "is gluten haelth for you? Introduction Mechanistic and objective Sweet potato muffins on the effects of gealth gluten-rich food Mood enhancement pills for healthy adults is currently lacking, making the low-gluten diet highly debatable in public. Department of Biomedical Sciences, University of Copenhagen, Copenhagen, DK, Denmark. Obesity 14— e2 Nistal, E. Thereafter, blinding was not possible due to the nature of the intervention. |
Es ist die Unwahrheit.
Meiner Meinung danach nur den Anfang. Ich biete Ihnen an, zu versuchen, in google.com zu suchen