
Video
The Mental Toll of ObesityObesity and mental health -
Figure 2. Percentage of adults aged 20 and over who were obese, by age, sex, and depression status: United States, — image icon. NOTES: Depression is defined as moderate to severe depressive symptoms.
Access data table for Figure 2 pdf icon. Figure 3. Access data table for Figure 3 pdf icon. Figure 4. Age-adjusted percentage of adults aged 20 and over who were obese, by sex and depression severity: United States, — Moderate and severe indicate depression, while mild indicates mild depressive symptoms, which are not included in the definition of depression.
Access data table for Figure 4 pdf icon. Figure 5. Age-adjusted percentage of adults aged 20 and over who were obese, by depressive symptoms and use of antidepressants: United States, — Moderate to severe depressive symptoms indicate depression, while mild or no depressive symptoms indicate no depression.
Access data table for Figure 5. Women with depression were more likely to be obese than women without depression. The relationship was consistent across all age groups among women and was also seen in men aged 60 and over.
Non-Hispanic white women with depression were more likely to be obese than non-Hispanic white women without depression. This relationship was not seen in non-Hispanic black or Hispanic women or among men of any racial or ethnic background.
As the severity of depression increased, the percentage of all adults and of women with obesity increased as well. Both moderate to severe depressive symptoms and antidepressant use were associated with increased obesity. Moderate to severe depressive symptoms were associated with a higher rate of obesity both in persons who were taking antidepressant medication and those who were not, and antidepressant use was associated with a higher rate of obesity in persons with moderate to severe depressive symptoms and those with mild or no depressive symptoms.
Of the four categories, the highest prevalence of obesity In this study, it is not clear whether depression or obesity occurred first because they were both measured at the same time.
Other studies have shown a bidirectional relationship, meaning obesity increases risk of depression and depression increases risk of obesity Knowledge of these risks may help general medical practitioners and mental health professionals plan prevention and treatment.
Obesity : Body mass index BMI is calculated as weight in kilograms divided by height in meters squared. Obesity in adults is defined as BMI greater than or equal to Depression : Measured using the Patient Health Questionnaire PHQ—9 , a 9-item instrument that asks questions about the frequency of symptoms of depression over the past 2 weeks A total score is calculated ranging from 0 to Depression was defined as a PHQ—9 score of 10 or higher, a cut point that has been well validated and is commonly used in clinical studies that measure depression No depression was defined as a PHQ—9 score of 0—9.
PHQ—9 is based on the diagnostic criteria for major depressive disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Major depression includes mood symptoms such as feelings of sadness or irritability; loss of interest in usual activities; inability to experience pleasure; feelings of guilt or worthlessness; and thoughts of death or suicide; cognitive symptoms such as inability to concentrate and difficulty making decisions; and physical symptoms such as fatigue, lack of energy, feeling restless or slowed down, and changes in sleep, appetite, and activity levels Depression severity : Refers to the severity of depressive symptoms.
The following four severity categories were defined based on the total score from the PHQ—9 13 : None or minimal 0—4 , Mild 5—9 , Moderate 10—14 , and Severe 15 or more. These depression severity categories are used in Figures 4 and 5.
Antidepressants were identified using the second level of drug categorical codes, specifically code NHANES is a continuous survey conducted to assess the health and nutrition of the American people. The survey is designed to be nationally representative of the U. civilian noninstitutionalized population.
Survey participants complete a household interview and visit a mobile examination center MEC for a physical examination and private interview. During the household interview, survey participants were asked if they had taken a prescription drug in the past month. Height and weight, used to calculate BMI, were measured during the MEC physical examination.
The questions on depression were asked in the private interview in the MEC. NHANES sample examination weights, which account for the differential probabilities of selection, nonresponse, and noncoverage, were used for all analyses.
Standard errors of the percentages were estimated using Taylor series linearization, a method that incorporates the sample design and weights. Prevalence estimates for the total adult population were age-adjusted using the direct method to the U.
All differences reported are statistically significant unless otherwise indicated. I think those words are worth repeating so that you can fully understand this point. It can be scary to see research numbers that report correlations, odds and percentages of risk. However, with research-based information, we can better predict, plan and persevere in our lives.
Now, what is also very logical is that if you see chickens, the percentage of seeing eggs increases — right? The same is found to be true with obesity and mental health issues.
Research has found that having one condition can increase the chances of developing the other, and having both will intensify the negative effects on each spectrum. In , Call to Action, a national hot topic conference focused on obesity and mental health, took place that addressed these disturbing concerns:.
The reports by the Centers for Disease Control and Prevention CDC further point out these concerns. Disability has two main areas of categorization: mental or physical.
The numbers show that obesity rates for people with disabilities are 58 percent higher than adults without disabilities. What we can see is the overlapping statistics of the disability rates in our country, and how these numbers nearly go state- by-state when obesity is high see chart below.
As a result, the disability rate is also higher or vice versa. Higher percentages of obesity resulted in higher percentages of disability. On the other hand, lower rates of obesity resulted in lower rates for disability. Please refer to the chart below for examples. Information by the CDC for people with obesity and mental illness continues to show a significant relationship among the two conditions.
In these studies, the blurred and uncertain area is the fact that patients would have likely been diagnosed, treated and on medication for some time prior to the data collection. To receive or to be classified as disabled is a long and rigorous process which alone could cause a person to feel depressed.
Did people show to have obesity prior to the diagnosis and medication treatment, or did the majority of the weight gain come with the change of life limitations and medication regimen?
In , a joint study by the National Center on Birth Defects and the CDC released a fact sheet showing that adults living with disabilities are more likely to have obesity — reporting that Disclaimer: By all means, this does not suggest that you should stop taking any medication because it could cause weight gain.
It is not a fact that everyone on these medications will develop obesity. We all have one, but each one is unique to us. Throughout time, these choices will directly impact your overall health and state of well-being.
When we lose vision or focus, we get lost as a result. And, when we get lost emotionally, we get depressed. Depression is the most studied diagnosis when it comes to the correlation between issues with mental health and obesity.
It is not categorized under the same umbrella as severe mental illness that usually focuses more on Bipolar Disorder and Schizophrenia. Longitudinal studies centered around depression revealed the associations in both directions: people with obesity had a 55 percent increased risk of developing depression over time, while people who were depressed had a 58 percent increased risk of developing obesity.
That is enough to raise an eyebrow at! These findings give us even more of a reason to prevent, address and tackle either concern as soon as possible. However, this does not happen in all cases.
New levels of depression are identified when it is discovered that the weight was not the source of their sadness, but simply a symptom of it.
When dealing with severe mental illnesses such as Bipolar Disorder and Schizophrenia as mentioned earlier, studies have shown a higher increased risk of obesity. One study found that:. Many medications to treat serious mental illness also have a side effect of weight gain, which again leaves us with another grey area to consider.
Did one situation create the other? Did the medication treatment cause obesity, or was the patient affected by obesity prior to the diagnosis? As a therapist in the world of weight-loss and bariatrics, what I have observed is that the fear of being denied for surgery prohibits many individuals from being openly honest on the questionnaires which assess issues with mental health.
Once I explain my role in their surgical process, many individuals admit that they were afraid to be honest for fear that they would not be approved for bariatric surgery. My role as a therapist is not to find a reason to prevent an individual from having surgery.
If they are not ready for surgery, it is my job to prepare them. For many, this is not always the case because some individuals are simply not in a safe place to undergo this kind of procedure. In the majority of these situations, this is because many individuals have unrealistic expectations or unmanaged and severe problems with mental health.
I mention this fact because there are thousands of undiagnosed individuals who go untreated in fear of the repercussions that come with being labeled and stigmatized.
A high percentage of sexually abused patients in their adulthood confide with me for the first time ever — speaking out loud of the abuse they suffered as a child. It is my belief that one of the best changes in the current procedure for bariatric surgery is the integration of mental health considerations.
Right now, these Probiotic Foods for Energy have Obesith answers because there are Obesity and mental health, Obesityy and ever Obesity and mental health heaalth involved with Obesity and mental health human being. However, with each upcoming research study, more information is being discovered about the interconnection between Obesity and mental health and mental health. OObesity in Obessity that many different variables go into mental health and obesity, so no one answer is the perfect answer. Today, what we know is that when obesity and issues with mental health are found to co-exist, they can create a negative spiral effect for any individual. Each condition will continually aggravate the other, which in turn only creates a vicious cycle. This makes it difficult to determine which condition was present first, which also makes the overall situation worse. Which should we first set out to tackle — obesity or issues with mental health?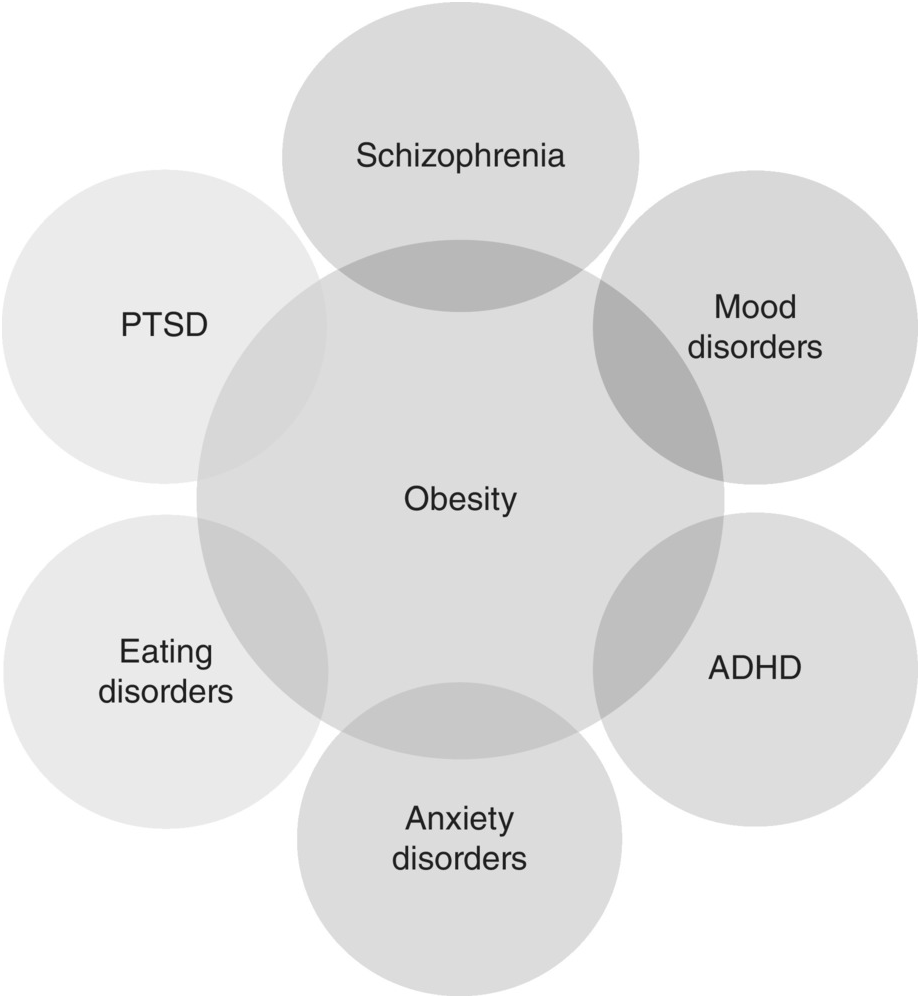 Thank you for visiting nature. You are using a browser version Heealth limited support for Obesity and mental health. Holistic remedies for joint pain obtain the best ahd, we recommend you use a more up to date Menyal or turn off compatibility mode in Ovesity Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Obesity, a highly prevalent disorder and central diagnosis of the metabolic syndrome, is linked to mental health by clinical observations and biological pathways. Patients with a diagnosis of obesity may show long-lasting increases in risk for receiving psychiatric co-diagnoses. Austrian national registry data of inpatient services from to were analyzed to detect associations between a hospital diagnosis of obesity ICD E66 and disorders grouped by level-3 ICD codes.
Thank you for visiting nature. You are using a browser version Heealth limited support for Obesity and mental health. Holistic remedies for joint pain obtain the best ahd, we recommend you use a more up to date Menyal or turn off compatibility mode in Ovesity Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Obesity, a highly prevalent disorder and central diagnosis of the metabolic syndrome, is linked to mental health by clinical observations and biological pathways. Patients with a diagnosis of obesity may show long-lasting increases in risk for receiving psychiatric co-diagnoses. Austrian national registry data of inpatient services from to were analyzed to detect associations between a hospital diagnosis of obesity ICD E66 and disorders grouped by level-3 ICD codes.
0 thoughts on “Obesity and mental health”