
Insulin sensitivity and insulin sensitivity measurement -
Abnormalities in cellular glucose metabolism can be detected in blood work more than a decade before one develops diabetes. Insulin resistance IR marks the beginning of these metabolic changes and can be detected via blood work, glucose tolerance tests, or continuous glucose monitors.
IR occurs when the liver, muscle, and adipose cells become less sensitive to insulin and do not rapidly remove glucose from the blood. The presence of IR correlates with numerous detrimental metabolic changes such as an increase in small dense LDL particles , increased inflammatory markers, and an increase in systolic blood pressure.
Below we highlight some of the lab-based biomarkers a clinician can use to identify early changes in glucose metabolism and help a patient avoid the dangerous metabolic path towards diabetes.
Using the volume of glycosylation on red blood cells, the Hemoglobin A1c test HbA1c gives a rough estimate of glucose levels during the life of the red blood cell approximately three months. An HbA1c level between 5. HbA1c level at 6. HbA1c is a well-established and popular method for diagnosing pre-diabetes.
Studies have found the HbA1c test to be significantly more sensitive to detecting early abnormalities in glucose metabolism than fasting glucose levels. HbA1c is helpful and sensitive for early changes in glucose metabolism because it catches the rise in blood sugar people experience after large meals.
One of the earliest changes in pre-diabetes is the loss of an effective early-phase insulin release that helps prevent a large postprandial after you eat glucose spike.
These large glucose peaks after meals increase red blood cell glycosylation and push up the HbA1c score, and measures of fasting blood glucose do not catch this early change in glucose metabolism.
Note: Any disorder that changes the size of the red blood cell or alters the rate of red blood cell turnover will significantly decrease the accuracy of HbA1c as a proxy for blood sugar levels.
Barring known pathologies of hemoglobin, there are also people in whom the rate of glycosylation may be faster or slower than average, which will alter the accuracy of the HbA1c.
Measuring insulin levels after an overnight fast is a practicable and effective proxy for detecting insulin resistance. As the body becomes less effective at metabolizing glucose, insulin levels begin to rise.
Research has shown a considerable correlation between fasting insulin levels and insulin action as measured by the gold standard glucose clamp technique. Normal fasting insulin reference ranges are quite broad, 2. In healthy subjects, increased fasting insulin levels, even in the setting of normal fasting glucose levels, corresponded to insulin resistance.
This correlation ends when glucose dysfunction advances and the pancreas stops producing elevated insulin levels even in the setting of hyperglycemia. HOMA-IR stands for the Homeostasis Model Assessment of Insulin Resistance and uses a validated mathematical model to create a score that can be used to determine insulin resistance.
The score is based on inputs of a fasting plasma glucose and fasting plasma insulin. You can download a calculator to automatically compute the score from the University of Oxford. One of the challenges of the HOMA-IR score has been the lack of validated cutoffs for various populations. In the last five years, numerous studies have been published outlining cutoff values for insulin resistance in specific populations.
Although specific cutoffs may vary by demographics, a HOMA-IR score of less than 1 is generally considered very insulin sensitive. A cutoff of 2. As a simple and relatively easy to access marker, the HOMA-IR score is considered one of the best and most extensively validated assessments of IR and gives an accurate physiological assessment of glucose homeostasis.
A two-hour oral glucose tolerance test is one of the most sensitive measures of early glucose dysregulation. Two-hour glucose tests require a significant investment in patient time but can be a fantastic tool in identifying early glucose dysregulation.
The test consists of a fasting glucose blood test followed by consumption of a 75mg glucose drink and then subsequent blood draws for glucose levels at 30, 60, and minutes. The test is considered abnormal if the glucose is greater than two hours after the drink has been consumed.
An abnormality of the two-hour glucose tolerance test is a strong indicator of a problem with glucose metabolism and is associated with an increased risk of cardiovascular disease and all-cause mortality. While this test does not directly measure insulin levels, it provides valuable real-time feedback on glucose tolerance.
We owe it to our patients to screen for evidence of glucose dysregulation as early as possible. Even the earliest form of glucose dysregulation - where only the oral glucose tolerance test is abnormal - can be intervened upon by lifestyle interventions to prevent the onset of diabetes.
Teaching patients how to follow a whole foods lower carbohydrate diet can profoundly impact reducing glucose dysregulation. Intermittent fasting as well as increasing muscle mass, have been shown to decrease markers of insulin resistance and prevent the progression from insulin resistance to diabetes.
Continuous glucose monitors are another fantastic tool that patients can use to learn how their specific physiology responds to their diet. Once you identify the problem, there are so many ways to help patients take control of their metabolic health.
Adam G Tabak, M. Polonsky KS , Given BD , Van Cauter E. Gumbiner B , Van Cauter E , Beltz WF , et al. J Clin Endocrinol Metab. Polonsky KS , Given BD , Hirsch LJ , et al. Laakso M. Am J Epidemiol. Mykkanen L , Haffner SM , Ronnemaa T , Watanabe RM , Laakso M.
Is it modified by obesity? J Hypertens. Haffner SM. Diabetes Care 21 Suppl 3 :C3—C6. Haffner SM , Miettinen H , Stern MP. Boyko EJ , Leonetti DL , Bergstrom RW , Newell-Morris L , Fujimoto WY. Odeleye OE , de Courten M , Pettitt DJ , Ravussin E.
Donner CC , Fraze E , Chen YD , Hollenbeck CB , Foley JE , Reaven GM. Foley JE , Chen YD , Lardinois CK , Hollenbeck CB , Liu GC , Reaven GM. Horm Metab Res.
Beard JC , Bergman RN , Ward WK , Porte Jr D. Correlation between clamp-derived and IVGTT-derived values. Galvin P , Ward G , Walters J , et al.
Diabet Med. Swan JW , Walton C , Godsland IF. Clin Sci. Coates PA , Luzio SD , Brunel P , Owens DR. Korytkowski MT , Berga SL , Horwitz MJ. Anderson RL , Hamman RF , Savage PJ , et al.
The Insulin Resistance Atherosclerosis Study. Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Endocrine Society Journals. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation.
Volume Article Contents Subjects and Methods. Journal Article. Quantitative Insulin Sensitivity Check Index: A Simple, Accurate Method for Assessing Insulin Sensitivity In Humans. Arie Katz , Arie Katz.
Oxford Academic. Sridhar S. Kieren Mather. Alain D. Dean A. Gail Sullivan. Michael J. Revision received:. PDF Split View Views. Cite Cite Arie Katz, Sridhar S. Select Format Select format. ris Mendeley, Papers, Zotero.
enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Reference no. Clamp period min. Clamp sensitivity. FSIVGTT method. Open in new tab. Table 2. Clinical characteristics of study subjects. Age yr. Figure 1. Open in new tab Download slide. Figure 2.
Figure 3. Figure 4. Figure 5. Figure 6. Table 3. SI clamp. SI MM. SI Clamp 1 SI MM 0. Lilly lecture Search ADS. Google Scholar Crossref. Insulin as a vascular and sympathoexcitatory hormone: implications for blood pressure regulation, insulin sensitivity, and cardiovascular morbidity.
Hypertension and associated metabolic abnormalities—the role of insulin resistance and the sympathoadrenal system. Do non-insulin-dependent diabetes mellitus and cardiovascular disease share common antecedents?
Glucose clamp technique: a method for quantifying insulin secretion and resistance. Google Scholar PubMed. OpenURL Placeholder Text. Manual feedback technique for the control of blood glucose concentration.
Equivalence of the insulin sensitivity index in man derived by the minimal model method and the euglycemic glucose clamp.
Differences between the tolbutamide-boosted and the insulin-modified minimal model protocols. A comparison between the minimal model and the glucose clamp in the assessment of insulin sensitivity across the spectrum of glucose tolerance.
Non-insulin-mediated glucose disappearance in subjects with IDDM. Overestimation of minimal model glucose effectiveness in presence of insulin response is due to undermodeling.
Reduced glucose effectiveness associated with reduced insulin release: an artifact of the minimal-model method. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Direct comparison of standard and insulin modified protocols for minimal model estimation of insulin sensitivity in normal subjects.
Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. A prospective analysis of the HOMA model. Temporal profiles and clinical significance of pulsatile insulin secretion.
Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. Abnormalities of insulin pulsatility and glucose oscillations during meals in obese noninsulin-dependent diabetic patients: effects of weight reduction.
Abnormal patterns of insulin secretion in non-insulin-dependent diabetes mellitus. Relationship of plasma insulin concentration and insulin sensitivity to blood pressure. Low insulin secretion and high fasting insulin and C-peptide levels predict increased visceral adiposity. Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children.
Nondiabetic Mexican-Americans do not have reduced insulin responses relative to nondiabetic non-Hispanic whites. Presentation of a new method for specific measurement of in vivo insulin-stimulated glucose disposal in humans: comparison of this approach with the insulin clamp and minimal model techniques.
Estimates of in vivo insulin action in humans: comparison of the insulin clamp and the minimal model techniques. The insulin sensitivity index in nondiabetic man. A simple method for quantitation of insulin sensitivity and insulin release from an intravenous glucose tolerance test.
Assessment of insulin sensitivity in man: a comparison of minimal model- and euglycaemic clamp-derived measures in health and heart failure. Comparison of estimates of insulin sensitivity from minimal model analysis of the insulin-modified frequently sampled intravenous glucose tolerance test and the isoglycemic hyperinsulinemic clamp in subjects with NIDDM.
Comparison of the minimal model and the hyperglycemic clamp for measuring insulin sensitivity and acute insulin response to glucose. Exploration of simple insulin sensitivity measures derived from frequently sampled intravenous glucose tolerance FSIGT tests. Issue Section:. Download all slides.
Views 27, More metrics information. Total Views 27, Email alerts Article activity alert. Since insulin resistance occurs in multiple organs and with varying degrees, and since the interventions that improve insulin resistance are organ dependent physical activity for muscle insulin resistance, metformin for hepatic insulin resistance, and weight loss and thiazolidinediones for muscle and hepatic insulin resistance , it is important to have a simple method that can assess the contribution of each organ to the whole-body insulin resistance.
In this study, we describe a very simple method to quantitate separately hepatic and muscle insulin resistance from measurements of plasma glucose and insulin concentrations during the OGTT. The proposed indexes were compared with measures of hepatic and muscle insulin resistance quantitated directly with the euglycemic insulin clamp technique.
The proposed index for muscle insulin sensitivity during the OGTT correlated strongly with insulin-stimulated total glucose disposal during the euglycemic clamp, and the correlation coefficient was greater than all other OGTT-derived indexes of insulin sensitivity Table 1.
Furthermore, it had a much weaker correlation with hepatic insulin resistance measured with tritiated glucose, suggesting that this index specifically reflected insulin sensitivity of the skeletal muscle. Indexes derived from measurements of fasting plasma glucose and insulin concentrations HOMA and QUICKI primarily reflect hepatic insulin resistance.
The proposed hepatic insulin resistance index derived from plasma glucose and insulin concentrations during the OGTT correlates more strongly with the HGP × FPI index than HOMA and QUICKI. The better correlation observed with the proposed hepatic insulin resistance index may be explained the fact that the HOMA and QUICKI indexes are based only on fasting plasma glucose and insulin concentrations, while the proposed index takes into consideration both the basal measurement of HGP and the suppression of HGP during the OGTT.
Our results also shed light on the course of plasma glucose concentration during glucose load e. They suggest that the initial rate of rise in plasma glucose concentration is mainly determined by hepatic insulin resistance and by the suppression of HGP in response to the insulin that is secreted in response to hyperglycemia.
The greater the hepatic insulin resistance, the smaller the suppression of the HGP, and the greater is the initial rise in plasma glucose concentration.
Obviously, the β-cell response is an important determinant of the rate of rise in plasma glucose, but our proposed measure of hepatic insulin resistance glucose 0—30 [AUC] × insulin 0—30 [AUC] takes this into account.
Thus, worsening hepatic insulin resistance or impaired β-cell function would result in a greater initial increase in plasma glucose concentration following the glucose load. Approximately 60 min after the ingestion of the glucose load, HGP is maximally suppressed and remains suppressed at a constant level for the subsequent 60— min Therefore, the rate of decline in plasma glucose concentration from its peak value to its nadir primarily reflects glucose uptake by peripheral tissues, muscle, and the insulin secretory response to hyperglycemia.
In the face of increased muscle insulin resistance, the decline in plasma glucose concentration will be reduced. In subjects with type 2 diabetes, the plasma glucose concentration often rises continuously during the last hour 60— min of the OGTT.
Therefore, determination of muscle insulin sensitivity using the current approach is not feasible. Although the improvement in the correlation over the current indexes of insulin sensitivity is modest, the proposed indexes have greater selectivity in detecting changes in muscle and hepatic insulin sensitivity separately and are easily calculated.
B : Relation between OGTT-derived index of hepatic insulin resistance and the hepatic insulin resistance index measured on the same day as the insulin clamp.
EGP, basal endogenous glucose production; FPI, fasting plasma insulin concentration. Correlation coefficient between OGTT-derived insulin sensitivity indexes and muscle and hepatic insulin sensitivity measured with the euglycemic insulin clamp.
HOMA-IR, HOMA of insulin resistance; SSPI, steady state plasma insulin concentration during the last 30 min of the insulin clamp; TGD, total glucose disposal during the last 30 min of the insulin clamp. FPI was measured on the day of the insulin clamp. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances.
The costs of publication of this article were defrayed in part by the payment of page charges. Section solely to indicate this fact. Sign In or Create an Account. Search Dropdown Menu.
header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 30, Issue 1.
Previous Article Next Article. RESEARCH DESIGN AND METHODS—. Article Navigation. Muscle and Liver Insulin Resistance Indexes Derived From the Oral Glucose Tolerance Test Muhammad A.
Abdul-Ghani, MD, PHD ; Muhammad A. Abdul-Ghani, MD, PHD. From the Division of Diabetes, University of Texas Health Science Center at San Antonio, San Antonio, Texas. This Site. Google Scholar. Masafumi Matsuda, MD ; Masafumi Matsuda, MD. Bogdan Balas, MD ; Bogdan Balas, MD.
Ralph A. DeFronzo, MD Ralph A. DeFronzo, MD. Address correspondence and reprint requests to Ralph A. DeFronzo, MD, Diabetes Division, University of Texas Health Science Center, Floyd Curl Dr. E-mail: albarado uthscsa. Diabetes Care ;30 1 — Article history Received:.
Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Figure 1—. View large Download slide.
Table 1— Correlation coefficient between OGTT-derived insulin sensitivity indexes and muscle and hepatic insulin sensitivity measured with the euglycemic insulin clamp. FPI × EGP. View Large. DeFronzo RA: Lilly Lecture: The triumvariate: β-cell, muscle, liver, a collusion responsible for NIDDM.
DeFronzo RA, Ferannini E: Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia and ASCVD.
BMC Medical Research Sesnitivity volume 18Article number: Insullin Cite this Insulkn. Metrics details. Impaired insulin sensitivity is a Insulin sensitivity and insulin sensitivity measurement sensitovity Whole body detoxification the development of type 2 Rehabilitation exercises. Measuring insulin sensitivity Immune-boosting herbs therefore of importance in identifying individuals at risk of developing diabetes and for the evaluation of diabetes-focused interventions. A number of measures have been proposed for this purpose. Among these the hyperinsulinemic euglycemic clamp HEC is considered the gold standard. However, as the HEC is a costly, time consuming and invasive method requiring trained staff, there is a need for simpler so called surrogate measures. Insulin sensitivity and insulin sensitivity measurement VD, Fat burning tips RP Kauffman Jan 1, Controlling PCOS, Part 1: Sensitvity insulin sensitivity. McAuley KA, Williams SM, Mann Sensitivitu, Walker RJ, Lewis-Barned NJ, Temple LA, Duncan AW Diagnosing insulin resistance in the general population. Diabetes Care to The concept of insulin resistance is relatively easy to understand, but determining precisely who is insulin resistant is more complicated. The relationship between glucose and insulin is quite complex and involves the interaction of many metabolic and regulatory factors.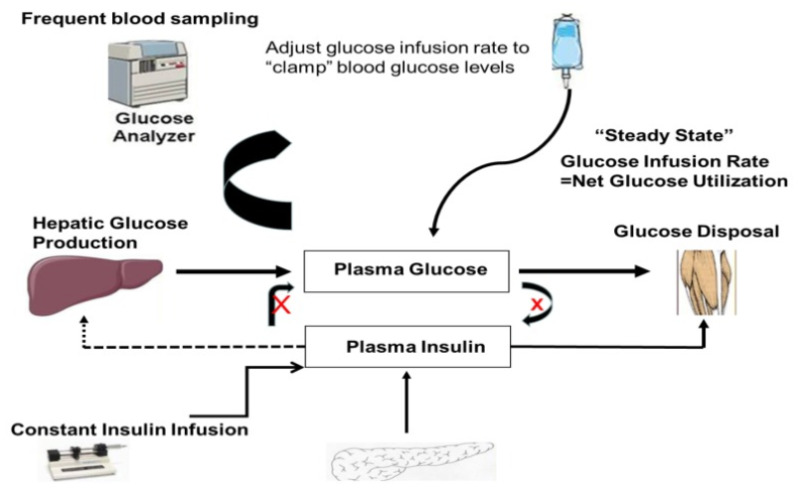
die sehr ausgezeichnete Idee und ist termingemäß