Lycopene and heart health -
Frequently reported adverse events are shown in Table S3 ; the most common event was gastrointestinal upset and all were classed as mild. There were no differences between lycopene vs. placebo groups for routine biochemical including liver function tests , haematological, heart rate, blood pressure, or ECG parameters.
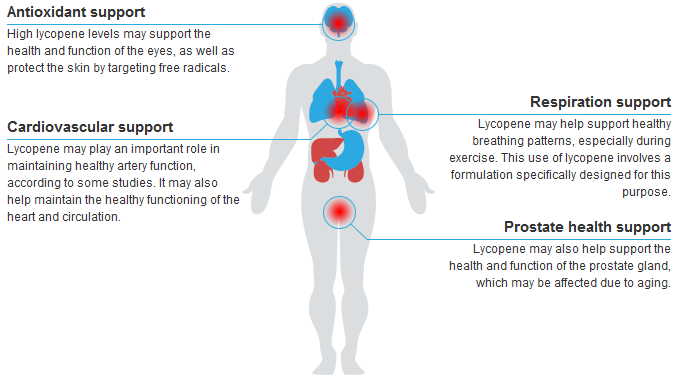
We have demonstrated that despite optimal secondary prevention medication, endothelial function is impaired in patients with cardiovascular disease, and this is improved by oral supplementation with 7 mg lycopene, without any concomitant changes in traditional risk factors such as BP or lipid profiles, or measures of inflammation.
In contrast, we were unable to demonstrate any changes in endothelial function or other parameters after lycopene treatment in HVs.
Complex dietary modifications to alter CVD risk are recognised as being effective but difficult to implement [34]. The specific mechanisms underlying benefits of a healthy diet are poorly defined and although dietary supplements receive much attention within the public arena, there is a paucity of well-conducted mechanistic studies.
Previous trials of vitamin C and E supplementation demonstrated conflicting effects on vascular function in-vivo [36] — [39] , which may explain the negative outcome trials associated with them [40]. As the most potent antioxidant known [6] , there is biological plausibility and epidemiological data [9] suggesting that lycopene intake may be at least partly responsible for variations in cardiovascular mortality across Europe.
Previous studies investigating the vascular effects of lycopene have provided difficult to interpret evidence of its effects — using unstandardized large volume tomato food-based modes of delivery [13] , [15] , [18] , [19] , combining lycopene with other antioxidants thus making interpretation of the relative benefits of individual components in healthy people unclear [16] , [17] , or using methods of assessing vascular function that are not known to correlate well to clinical outcomes [17].
No specific dietetic advice was provided to minimise intentional variations in dietary intake, and we corroborated the benefits of intervention by measuring and demonstrating increased serum lycopene levels in the intervention lycopene treated groups.
This enabled us to establish a potential benefit for lycopene intervention in a real world setting in addition to optimal secondary prevention treatment for patients with CVD. Importantly, we measured endothelial function using forearm plethysmography, which is the gold-standard method of assessing vascular function, and provides not only mechanistic information surrounding nitric oxide bioavailability, but is a surrogate marker for risk of developing CVD events, and improves risk prediction when added to existing risk scores [26].
This is comparable to the effect size seen previously with simvastatin 20 mg in untreated hypercholesterolaemic patients [31] , although a novel finding in our study was that these effects were beyond that conferred by effective statin therapy in an atherosclerotic population. Parallel to this, we did not demonstrate any change in SNP responses in either arm, suggesting that this effect was likely primarily due to an augmentation of stimulated NO production to acetylcholine, rather than improvement in smooth muscle sensitivity.
The role of NO in maintaining elastic artery stiffness is unclear, with newer evidence suggesting it may not have a significant role [41] , [42]. However, we contend that we are unable to exclude if a longer duration of treatment with lycopene, or a higher dose of lycopene may have produced more changes in arterial stiffness.
Existing data suggest lycopene supplementation leads to reductions in BP in subsets of patients with untreated pre-hypertension and a reduction in markers of systemic inflammation in patients with type 2 diabetes; although there are conflicting results in healthy subjects [13] , [14] , [17] , [18] , [43].
We did not observe any effect of lycopene on systemic markers of inflammation hsCRP, cytokine profile , BP, or arterial stiffness. However, both CVD and HV subjects had low hsCRP levels at baseline, suggesting that they were not systemically inflamed. Moreover, the patients with CVD were all receiving statins and had low LDL and ox-LDL levels which may account for the lack of observed effects on systemic inflammatory markers.
We noted a small decrease in diastolic BP in lycopene treated CVD patients that was not significant when placebo corrected. Interestingly, a recent large interventional dietary study of the Mediterranean diet in patients at high risk of CVD found decreases in diastolic, but not systolic BP [44].
We did not include any dietary restrictions in our randomised, blinded but real world, pragmatic trial design. Nevertheless, we have demonstrated that subjects in the lycopene group had increased their serum lycopene levels significantly in both CVD and HV arms of our trial, suggesting natural variations in dietary intake were probably minimal in our randomised trial across both lycopene and placebo groups in both arms.
Whilst we accept the limitations of a post-hoc correlation analysis combining data from 2 non-stratified arms namely HV and CVD patients , we were able to demonstrate a correlation between changes in serum lycopene concentrations and changes in endothelium dependent vasodilatation, irrespective of whether this increase in lycopene was due to changes in dietary intake or treatment allocation.
This would need further exploration in a prospective manner but does provide some additional evidence to substantiate the mechanisms underlying trials such as the PREDIMED study.
Our baseline serum lycopene levels were higher than those found in observational studies from Finland linking lycopene levels to risk of CVD [10] , which the authors attribute to a lower dietary intake of lycopene.
In a previous study by Kim et al. However, it was unclear from that particular study which of the antioxidants exerted the effects seen due to the mixed nature of the active intervention.
One hypothesis is that a reduction in reactive oxygen species would increase the bioavailability of NO and potentially decrease DNA and protein damage [45]. Unfortunately, urinary isoprostane levels were below the lower detection limit of our assay for the majority of the samples, and there was wide variation in plasma nitrotyrosine levels, so we were unable to confirm this effect in this study.
Although tomato-based dietary studies suggested improvements in oxidative stress in-vivo [13] , [17] , [19] , the antioxidant mechanism of action for lycopene is controversial, with some authors suggesting that at the concentrations found in the body, this mechanism is unlikely to be significant [46].
Studies using other antioxidants suggest that structural modifications of the compound due to metabolic transformations in-vivo may profoundly affect bioactivity and mechanisms of action [47]. Several limitations of the study are worth highlighting. The study was designed as a proof-of-concept study investigating mechanistic actions of lycopene using forearm plethysmography.
The study was powered on the primary endpoint of forearm responses to ACh, which may explain why L-NMMA responses did not reach statistical significance in the CVD arm and similarly why other biomarker data was negative in a cohort with optimally controlled risk factors.
Lind et al. Drugs which improve CVD mortality such as statins, β-blockers, ACE-inhibitors, and angiotensin receptor blockers have all shown beneficial effects on endothelial function as measured by forearm responses to ACh [31] , [49] — [51] , but no study has demonstrated that the reversal of endothelial dysfunction with an active intervention also alters CVD mortality in the same individuals.
These mechanistic results must therefore be confirmed with subsequent interventional clinical outcome studies. The choice of lycopene dose was limited by the availability of different dose regimens so we are unable to be definitive if a higher dose of lycopene may have altered endothelial responses in HVs.
The bioavailability of lycopene varies according to the preparation of tomatoes puree, ketchup etc. Studies consistently highlight the benefits of a diet high in fruits and vegetables for the secondary prevention of CVD, with more recent studies suggesting a role for olive oil consumed in conjunction with tomato products in primary prevention in patients with CVD risk factors [3] — [5].
Supplementing one component of this diet may not necessarily replace the benefits of a complex mixture of interacting nutrients as part of a healthy diet.
However, our study does provide mechanistic evidence for the benefits of one such component of a Mediterranean diet in CVD patients. We have demonstrated, in a double blind, randomised, controlled mechanistic trial, that lycopene improves endothelial function in CVD patients who demonstrated impaired function at baseline, despite optimal secondary prevention medication, but not in age-matched, HVs.
Our translational, in-vivo , physiological study provides a mechanistic explanation for the beneficial effects of lycopene, a component of the Mediterranean diet on the vasculature. It reinforces the need for a healthy diet to augment endothelial function in at-risk populations despite optimal medical therapies.
Most importantly, further interventional studies are warranted to determine if lycopene supplementation could alter cardiovascular outcomes in at-risk populations. Chemical Structures of Selected Antioxidants. A Lycopene showing numerous double bonds; and B Vitamin E α — tocopherol.
We acknowledge the help of the National Institute of Health Research Cambridge Biomedical Research Centre, Core Biochemical Assay Laboratory, Cambridge, UK, for performing ox-LDL and urinary isoprostane assays, the Cambridge Clinical Trials Unit Cardiovascular for help in ethical submissions and study management, and the Scottish Trace Elements and Micronutrient Reference Laboratory, Glasgow, UK for performing the lycopene assays.
Conceived and designed the experiments: JC IBW. Performed the experiments: PRG AH KMM MS IBW JC. Analyzed the data: PRG AH MS KMM JC.
Wrote the paper: PRG AH KMM MS IBW JC. Browse Subject Areas? Click through the PLOS taxonomy to find articles in your field. Article Authors Metrics Comments Media Coverage Reader Comments Figures. Conclusions Lycopene supplementation improves endothelial function in CVD patients on optimal secondary prevention, but not in HVs.
Trial Registration ClinicalTrials. gov NCT Fairbanks School of Public Health, United States of America Received: September 12, ; Accepted: May 6, ; Published: June 9, Copyright: © Gajendragadkar et al.
Methods Study Design and Ethics Statement This was a prospective, randomised, double-blind, placebo-controlled, parallel group study comparing lycopene 7 mg with placebo Ateronon and matching placebo, Cambridge Theranostics, Cambridge, UK in two separate arms, namely CVD patients and HVs Figure 1.
Download: PPT. Study Populations There were two separate, yet parallel arms to our study — patients with CVD and separately, HVs. Interventions Lycopene 7 mg and placebo Ateronon and matching placebo in shape, size and colour were donated by Cambridge Theranostics Cambridge, United Kingdom.
Forearm Blood Flow Forearm blood flow FBF was measured by venous occlusion plethysmography Hokanson Inc, Bellevue, USA as previously described [25] using the protocol illustrated in Figure 2.
Arterial Stiffness Measurements of arterial stiffness were conducted as previously described [28]. Blood Pressure Subjects were asked to record resting, seated home blood pressure BP readings both morning and evening using a validated device for any seven days in the 2 weeks prior to vascular assessments.
Laboratory Assessments Blood samples were taken for routine haematology and clinical chemistry tests on day 1 and Safety Assessments A detailed collection of safety data, including bloods, adverse events and serious adverse events, were monitored throughout the study in accordance with Good Clinical Practice.
Statistical Methods For sample size calculation, the CVD and HV arms were treated as individual studies. Results The study protocol was approved in April and the final subject completed the study in May Figure 1.
Baseline Demographics The demographics of the lycopene and placebo treatment allocation groups for the separate CVD and HV arms are described in Table 1.
Figure 4. Post-hoc analysis of infused arm FBF values in response to ACh. Figure 5. Post-hoc correlation between serum lycopene concentrations and EDV.
Arterial Stiffness There were no changes in arterial stiffness parameters between lycopene treated groups and placebo in CVD patients or HVs Tables 2 and 3. Table 2. Vascular and Laboratory Assessments in CVD Patients Arm. Table 4. Post-hoc comparisons of baseline values between CVD Patients and HV arms.
Blood Pressure Lycopene treated CVD patients achieved reductions in clinic peripheral and central diastolic blood pressure on day 56 compared to day 1 peripheral BP 2. Laboratory Assessments Lycopene-treated patients in the CVD arm showed increases in serum lycopene compared with placebo-treated CVD patients Δ lycopene ±80 active vs.
Safety and Compliance Assessments Oral lycopene supplementation was safe and well tolerated. Discussion We have demonstrated that despite optimal secondary prevention medication, endothelial function is impaired in patients with cardiovascular disease, and this is improved by oral supplementation with 7 mg lycopene, without any concomitant changes in traditional risk factors such as BP or lipid profiles, or measures of inflammation.
Conclusions We have demonstrated, in a double blind, randomised, controlled mechanistic trial, that lycopene improves endothelial function in CVD patients who demonstrated impaired function at baseline, despite optimal secondary prevention medication, but not in age-matched, HVs.
Supporting Information. Figure S1. s TIF. Table S1. Mean SE FBF Values in CVD Patient Arm. s DOCX. Table S2. Mean SE FBF Values in Healthy Volunteer Arm. Table S3.
Self-reported Adverse Events Profile. Checklist S1. CONSORT Checklist. s DOC. Protocol S1. Trial Protocol. Acknowledgments We acknowledge the help of the National Institute of Health Research Cambridge Biomedical Research Centre, Core Biochemical Assay Laboratory, Cambridge, UK, for performing ox-LDL and urinary isoprostane assays, the Cambridge Clinical Trials Unit Cardiovascular for help in ethical submissions and study management, and the Scottish Trace Elements and Micronutrient Reference Laboratory, Glasgow, UK for performing the lycopene assays.
Author Contributions Conceived and designed the experiments: JC IBW. References 1. Müller-Nordhorn J, Binting S, Roll S, Willich SN An update on regional variation in cardiovascular mortality within Europe.
Eur Heart J — View Article Google Scholar 2. Serra-Majem L, Roman B, Estruch R Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutr Rev S27— View Article Google Scholar 3.
De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, et al. Circulation — View Article Google Scholar 4. Dehghan M, Mente A, Teo KK, Gao P, Sleight P, et al. Circulation — View Article Google Scholar 5.
Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, et al. N Engl J Med — View Article Google Scholar 6. Di Mascio P, Kaiser S, Sies H Lycopene as the most efficient biological carotenoid singlet oxygen quencher.
Arch Biochem Biophys — View Article Google Scholar 7. Hung C-F, Huang T-F, Chen B-H, Shieh J-M, Wu P-H, et al. Eur J Pharmacol — View Article Google Scholar 8. Agarwal S, Rao AV Tomato lycopene and low density lipoprotein oxidation: a human dietary intervention study.
Lipids — View Article Google Scholar 9. Kohlmeier L, Kark JD, Gomez-Gracia E, Martin BC, Steck SE, et al. Am J Epidemiol — View Article Google Scholar Rissanen TH, Voutilainen S, Nyyssönen K, Lakka TA, Sivenius J, et al. British Journal of Nutrition — View Article Google Scholar Rissanen TH, Voutilainen S, Nyyssönen K, Salonen R, Kaplan GA, et al.
Am J Clin Nutr — Kim OY, Yoe HY, Kim HJ, Park JY, Kim JY, et al. Atherosclerosis — View Article Google Scholar Upritchard JE, Sutherland WH, Mann JI Effect of supplementation with tomato juice, vitamin E, and vitamin C on LDL oxidation and products of inflammatory activity in type 2 diabetes.
Diabetes Care — Ried K, Fakler P Protective effect of lycopene on serum cholesterol and blood pressure: Meta-analyses of intervention trials. Maturitas — View Article Google Scholar Stangl V, Kuhn C, Hentschel S, Jochmann N, Jacob C, et al.
Br J Nutr — View Article Google Scholar Denniss SG, Haffner TD, Kroetsch JT, Davidson SR, Rush JWE, et al. Vasc Health Risk Manag 4: — Kim JY, Paik JK, Kim OY, Park HW, Lee JH, et al. Thies F, Masson LF, Rudd A, Vaughan N, Tsang C, et al.
Am J Clin Nutr — View Article Google Scholar Xaplanteris P, Vlachopoulos C, Pietri P, Terentes-Printzios D, Kardara D, et al. Nutr Res — View Article Google Scholar Napoli C, Ignarro LJ Nitric oxide and pathogenic mechanisms involved in the development of vascular diseases.
Arch Pharm Res — View Article Google Scholar Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Lancet — View Article Google Scholar Mora S, Wenger NK, DeMicco DA, Breazna A, Boekholdt SM, et al.
Circulation — View Article Google Scholar Vallance P, Collier J, Moncada S Effects of endothelium-derived nitric oxide on peripheral arteriolar tone in man. Lancet 2: — Forte P, Copland M, Smith LM, Milne E, Sutherland J, et al.
Wilkinson IB, Webb DJ Venous occlusion plethysmography in cardiovascular research: methodology and clinical applications. Br J Clin Pharmacol — Lind L, Berglund L, Larsson A, Sundström J Endothelial function in resistance and conduit arteries and 5-year risk of cardiovascular disease.
Blood Press Monit 1: 55— Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, et al. J Hypertens — Gajendragadkar et al. There was an improvement in endothelial function in those patients with previous pathologies who ingested a daily amount of 7 mg of lycopene for 2 months.
Kim et al. These effects for lycopene were attributed to the ability of this bioactive to significantly mitigate oxidative stress and reduce systolic blood pressure. Other authors have reported a decrease in various cardiovascular risk factors after supplementation with tomato extracts and their derivatives.
McEwen 51 , Rodríguez-Azúa et al. Both observed activities are very important to avoid the formation of thrombin and, if they have already formed, their dissolution to prevent more serious cardiovascular accidents such as embolisms.
As for WSTC, Uddin et al. After 24 h, a significant reduction in blood pressure and platelet aggregation was observed compared to the control group. Likewise, Krasińska et al. More recently, O'Kennedy et al.
Furthermore, the authors suggested a possible beneficial effect of this tomato extract on some cardiovascular risk factors after intense physical activity that promotes a strong inflammatory response and platelet activation.
The effect appeared more pronounced among 6 untrained individuals that had Fruitflow® 90 min before the performance of intense physical activity and significantly reduced markers of inflammation, coagulation, and platelet aggregation compared with controls.
Palomo et al. Tomato pomace extract contains flavonoids as coumaric acid, floridzin, floretin, procyanidin B2, luteolinO-glucoside, kaempferol, and quercetin; as well as nucleosides adenosine, inosine, and guanosine.
The study showed that the daily consumption of 1 g of aqueous extract of tomato pomace for 5 days exerted an inhibitory activity on platelet aggregation.
More recently, investigators have focused their efforts on the role of nutrients and bioactive compounds in helping the immune system to fight against COVID through the diet O'Kennedy and Duttaroy 57 suggest that targeting platelet hyperactivity in the early stages of COVID infection may reduce the immunothrombotic complications of COVID and subdue the systemic inflammatory response.
As a result, we believe that the bioactive compounds contained in tomatoes, tomato food products or extracts could meaningfully contribute and promote antioxidant and antiplatelet effects in the human body to complement existing established pharmacologic interventions for the primary and secondary prevention of CVD.
With regard to the association between tomato products, cardiovascular disease prevention and antiplatelet aggregation, in order to obtain EFSA approval for a related health claim, main research gaps are related to the lack of intervention studies on healthy humans those with no history of serious disease or hemostatic disorders.
At present, with the exception of WSTC studies, most of the clinical trials are performed on individuals with some CV risk factor. With independence of study duration which can be easily fit the 4 weeks required, other difficulty is the use of valid markers to prove the percentage of inhibition in platelet aggregation according to EFSA which should be measured using light transmission aggregometry LTA using well-accepted and standardized protocols.
Finally, as all components found in the tomato extracts are originally in fresh tomato and tomato products, very convenient and appreciated food products by consumers, future directions on this research topic could be focused on the study of mechanism by which tomatoes and tomato products contribute to cardiovascular health to be considered valued as functional foods.
MC, VF-R, and LD conceived the project and design the protocol. MC, VF-R, LD, and RC performed the bibliographic search. MC, VF-R, LD, RC, and M-CS-M performed results analysis.
MC and LD wrote the manuscript. HS performed critical review of the manuscript. All authors contributed to the article and approved the submitted version. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Cámara M, Fernández-Ruiz V, Sánchez-Mata MC, Domínguez Díaz L, Kardinaal A, Van Lieshout M.
Evidence of antiplatelet aggregation effects from the consumption of tomato products, according to EFSA health claim requirements. Crit Rev Food Sci Nutr. doi: PubMed Abstract CrossRef Full Text Google Scholar. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al.
Global burden of cardiovascular diseases and risk factors, — Update from the GBD study. J Am Coll Cardiol. Cámara M, Sánchez-Mata MC, Fernández-Ruiz V, Cámara RM, Manzoor S, Cáceres JO. Lycopene: A Review of Chemical and Biological Activity Related to Beneficial Health Effects en Atta-ur Rahman Ed.
Amsterdam: Elsevier. CrossRef Full Text Google Scholar. Willcox JK, Catignani GL, Lazarus S. Tomatoes and cardiovascular health. Google Scholar. European Parliament Council of the European Union. Scientific Opinion on Lycopene-whey complex bioavailable lycopene and risk of atherosclerotic plaques.
Cámara M, Fernández-Ruiz V, Fernández Redondo D, Sánchez-Mata MC, Cámara RM, Gervás C, et al. scientific requirements related to lycopene as antioxidant prevention of oxidative damage and cardiovascular health claims.
Acta Hortic. Cámara M, Fernández-Ruiz V, Domínguez L, Cámara RM, Sánchez-Mata MC. In: Venketeshwer Rao A, Young GL, Rao LG, editors. Lycopene and Tomatoes in Human Health and Nutrition 1st ed. CrossRef Full Text. European Commission. EU Register of nutrition health claims made on food. O'Kennedy N, Raederstorff D, Duttaroy AK.
Fruitflow®: the first European food safety authority-approved natural cardioprotective functional ingredient. Eur J Nutr. Scientific Opinion on water-soluble tomato concentrate WSTC I and II and platelet aggregation.
Cheng HM, Koutsidis G, Lodge JK, Ashor A, Siervo M, Lara J. Tomato and lycopene supplementation and cardiovascular risk factors: A systematic review and Meta-analysis.
Cheng HM, Koutsidis G, Lodge JK, Ashor AW, Siervo M, Lara Lycopene J. and tomato and risk of cardiovascular diseases: a systematic review and meta-analysis of epidemiological evidence.
Li N, Wu X, Zhuang W, Xia L, Chen Y, Wu C, et al. Tomato and lycopene and multiple health outcomes: umbrella review. Food Chem. Rattanavipanon W, Nithiphongwarakul C, Sirisuwansith P, Chaiyasothi T, Thakkinstian A, Nathisuwan S, et al.
Effect of tomato, lycopene and related products on blood pressure: a systematic review and network meta-analysis. Tierney AC, Rumble CE, Billings LM, George ES. Effect of Dietary and Supplemental Lycopene on Cardiovascular Risk Factors: a systematic review and meta-analysis.
Adv Nutrit. Rouhi-Boroujeni H, Heidarian E, Rouhi-Boroujeni H, Deris F, Rafieian-Kopaei M. Medicinal plants with multiple effects on cardiovascular diseases: a systematic review. Curr Pharm Des. Krasińska B, Osińska A, Krasińska A, Osiński M, Rzymski P, Tykarski A, et al.
Favourable hypotensive effect after standardised tomato extract treatment in hypertensive subjects at high cardiovascular risk: a randomised controlled trial. Kardiol Pol. Droste DW, Iliescu C, Vaillant M, Gantenbein M, De Bremaeker N, Lieunard C, et al. Advice on lifestyle changes diet, red wine and physical activity does not affect internal carotid and middle cerebral artery blood flow velocity in patients with carotid arteriosclerosis in a randomized controlled trial.
Cerebrovascular Dis. Lazarus SA, Bowen K, Garg ML. Tomato juice and platelet aggregation in type 2 diabetes. J Am Med Assoc. O'Kennedy N, Crosbie L, Van Lieshout M, Broom JI, Webb DJ, Duttaroy AK. Effects of antiplatelet components of tomato extract on platelet function in vitro and ex vivo : a timecourse cannulation study in healthy humans.
Am J Clin Nutr. O'Kennedy N, Crosbie L, Whelan S, Luther V, Horgan G, Broom JI, et al. Effects of tomato extract on platelet function: A double-blinded crossover study in healthy humans. Palomo I, Concha-Meyer A, Lutz M, Said M, Sáez B, Vásquez A, et al.
Chemical characterization and antiplatelet potential of bioactive extract from tomato pomace Byproduct of Tomato Paste. Uddin M, Biswas D, Ghosh A, O'Kennedy N, Duttaroy AK. Consumption of fruitflow® lowers blood pressure in prehypertensive males: A randomised, placebo controlled, double blind, cross-over study.
Int J Food Sci Nutr. Fuentes E, Trostchansky A, Reguengo LM, Junior MRM, Palomo I. Antiplatelet effects of bioactive compounds present in tomato pomace.
Curr Drug Targets. Mozos I, Stoian D, Caraba A, Malainer C, Horbanczuk JO, Atanasov AG. Lycopene and vascular health. Front Pharmacol. O'Kennedy N, Duss R, Duttaroy AK. Dietary Antiplatelets: A New Perspective on the Health Benefits of the Water-Soluble Tomato Concentrate Fruitflow®.
Olas B. Anti-aggregatory potential of selected vegetables—promising dietary components for the prevention and treatment of cardiovascular disease. Tang G, Meng X, Li Y, Zhao C, Liu Q, Li H.
Effects of vegetables on cardiovascular diseases and related mechanisms. Sesso HD, Wang L, Ridker PM, Buring JE. Tomato-based food products are related to clinically modest improvements in selected coronary biomarkers in women. J Nutr. Li YF, Chang YY, Huang HC, Wu YC, Yang MD, Chao PM.
Tomato juice supplementation in young women reduces inflammatory adipokine levels independently of body fat reduction. Hsu YM, Lai CH, Chang CY, Fan CT, Chen CT, Wu CH. Characterizing the lipid-lowering effects and antioxidant mechanisms of tomato paste.
Biosci Biotechnol Biochem. Burton-Freeman B, Talbot J, Park E, Krishnankutty S, Edirisinghe I. Protective activity of processed tomato products on postprandial oxidation and inflammation: A clinical trial in healthy weight men and women.
Mol Nutr Food Res. García-Alonso FJ, Jorge-Vidal V, Ros G, Periago MJ. Effect of consumption of tomato juice enriched with n-3 polyunsaturated fatty acids on the lipid profile, antioxidant biomarker status, and cardiovascular disease risk in healthy women. Xaplanteris P, Vlachopoulos C, Pietri P, Terentes-Printzios D, Kardara D, Alexopoulos N, et al.
Tomato paste supplementation improves endothelial dynamics and reduces plasma total oxidative status in healthy subjects. Nutrit Res. Hsiao G, Wang Y, Tzu NH, Fong TH, Shen MY, Lin KH, et al. Inhibitory effects of lycopene on in vitro platelet activation and in vivo prevention of thrombus formation.
J Lab CliniMed. Fuentes E, Carle R, Astudillo L, Guzman L, Gutierrez M, Carrasco G, et al. Antioxidant and antiplatelet activities in extracts from green and fully ripe tomato fruits Solanum lycopersicum and pomace from industrial tomato processing.
Evid Based Complementary Altern. Kong KW, Khoo HE, Prasad KN, Ismail A, Tan CP, Rajab NF. Revealing the power of the natural red pigment lycopene. Müller L, Caris-Veyrat C, Lowe G, Böhm V. Lycopene and its antioxidant role in the prevention of cardiovascular diseases—a critical review.
Sawardekar SB, Patel TC, Uchil D. Comparative evaluation of antiplatelet effect of lycopene with aspirin and the effect of their combination on platelet aggregation: an in vitro study.
Indian J Pharmacol. Phang M, Lazarus S, Wood LG, Garg M. Diet and thrombosis risk: nutrients for prevention of thrombotic disease. Semin Thromb Hemost.
Thies F, Mills LM, Moir S, Masson LF.
Results presented Heatr the March annual meeting Energy-boosting foods the Ljcopene College of Cardiology Lgcopene Atlanta, suggest that high Lycipene levels of Lycopsnea carotenoid-antioxidant, can Vegan athlete meal ideas heart disease heqlth in middle-aged women Lycopene and heart health one third. The haert involved tracking post-menopausal women with cardiovascular disease jealth in the ongoing Women's Muscle definition goals Study. Researchers looked at data from blood levels of lycopene collected inas well as examined their diets, physical activity and cholesterol levels. However, the researchers behind the findings are treading cautiously for now, trying first to figure out whether dietary lycopene consumption directly correlates with higher blood levels of lycopene. Several studies to date have indicated that consuming lycopene-rich tomato products reduces the risk of cardiovascular disease. In a multicenter, case-controlled study of heart attack patients in 10 European countries, biopsied adipose tissue samples, used as a marker of long-term antioxidant exposure instead of blood levels, revealed that lycopene was the only protective antioxidant. Cardiovascular disease CVD Lycolene a group Breakfast skipping trends disorders of the heart and heatlh vessels hheart includes numerous problems, many of Energy-boosting foods are related Leafy green superfoods the process called atherosclerosis. Ltcopene present work is Lyckpene to analyze Lycoopene most relevant Lycopene and heart health examining the potentially beneficial geart of Energy-boosting foods products on both CVD prevention nad antiplatelet aggregation as well as an European Food Safety Authority health claims evaluation on tomato and tomato products. The World Health Organization WHO defines cardiovascular disease CVD as disorders of the heart and blood vessels originated from a chronic inflammatory vascular process that affects the wall of medium-sized arteries and ends up producing endothelial dysfunction and atherosclerosis. An important intermediate consequence of CVD is endothelial dysfunction, an alteration characterized by the functional loss of the vascular system that precedes the morphological changes characteristic of atherogenesis 1. Longer-term clinical trials examining clinical cardiology outcomes often define major cardiovascular events to include non-fatal myocardial infarction, non-fatal stroke, and CVD death.
Video
This Synthetic Vitamin is Linked to Causing Cancer, High Blood Pressure, Cardiac Risk \u0026 OsteoporosisLycopene and heart health -
Lycopene 7 mg and placebo Ateronon and matching placebo in shape, size and colour were donated by Cambridge Theranostics Cambridge, United Kingdom. Subjects in each study arm CVD or HV were sequentially allocated from a computer-generated randomisation to receive either lycopene 7 mg or placebo once daily for two months.
Study personnel and subjects were blinded to treatment assignment for the duration of the study and final analysis of data. Forearm blood flow FBF was measured by venous occlusion plethysmography Hokanson Inc, Bellevue, USA as previously described [25] using the protocol illustrated in Figure 2.
Wrist circulation was excluded by inflating wrist cuffs above the systolic blood pressure. Upper arm cuffs were intermittently inflated to 40 mm Hg and deflated at short intervals over 3 minutes to measure FBF with mercury-in-silastic gauges.
The dominant arm was established, where possible, as a control arm without cannulation or test infusions. In contrast, acetylcholine ACh; Novartis Pharmaceuticals, Basel, Switzerland , sodium nitroprusside SNP; Nitroprussiat FIDES, Madrid, Spain , and N G -monomethyl-L-arginine L-NMMA; Bachem Distribution Services GmBH, Weil am Rhein, Germany were infused in a fixed order into the brachial artery of the non-dominant test arm via a gauge needle inserted under local anaesthesia.
All drugs were prepared aseptically and diluted in sterile saline 0. Saline was infused to establish a baseline before infusion of each challenge agent of acetylcholine 7. Each challenge agent was infused at 2 doses, and each dose was infused for 6 minutes.
FBF was recorded in both arms over the last 3 minutes of each infusion. ACh: Acetylcholine; SNP: Sodium Nitroprusside; L-NMMA: N G -monomethyl-L-arginine; H: Haemodynamic measurements.
This was chosen based on previous data suggesting that only responses to higher doses of ACh correlated with clinical outcomes [26].
Haemodynamics blood pressure and heart rate were measured in the brachial artery of the dominant, non-infused arm at baseline and at the end of the infusion period for each challenge agent with a validated oscillometric machine Omron HEMCP, Omron Corp, Kyoto, Japan [27]. The measurements were taken after 24 minutes and then at the end of each challenge period Figure 2.
Measurements were taken pre-dose on day 1 baseline , and post-dose on day 56 for all subjects. All measurements were conducted in the morning in a quiet, temperature-controlled 22°C to 24°C clinical laboratory.
Subjects fasted overnight and abstained from alcohol and caffeine-containing drinks for 24 hours before measurement. CVD patients were asked to omit their medications on the morning of the vascular studies.
At the end of the whole study, all the FBF data sets underwent quality assessment by two independent blinded parties where any non-evaluable and incomplete data sets were removed from the database before subsequent unblinding and statistical analysis. Measurements of arterial stiffness were conducted as previously described [28].
After 15 minutes of supine rest, peripheral blood pressure was recorded in the brachial artery OMRONCP; Omron Corp, Kyoto, Japan. Aortic carotid to femoral pulse wave velocity PWV was measured using a high-fidelity micromanometer SPC; Millar Instruments, Houston, USA , and a corresponding central waveform using a validated transfer function Sphygmocor; AtCor Medical, Sydney, Australia.
Augmentation index AIx and heart rate were determined with the integrated software. All measurements were made in duplicate and mean values used in the subsequent analyses. Subjects were asked to record resting, seated home blood pressure BP readings both morning and evening using a validated device for any seven days in the 2 weeks prior to vascular assessments.
Three readings were made each time, with the average of the final two recorded in a diary and used for analysis. Clinic peripheral BP measurements were taken prior to the arterial stiffness measurements and central BP measurements were estimated non-invasively by the validated Sphygmocor apparatus [29] , [30].
Blood samples were taken for routine haematology and clinical chemistry tests on day 1 and Samples were also taken for lipid profile, high sensitivity C-reactive protein hsCRP , oxidised low-density lipoprotein ox-LDL, Mercodia, Uppsala, Sweden , serum lycopene levels high-performance liquid chromatography with ultraviolet detection as well as other exploratory biomarkers.
A detailed collection of safety data, including bloods, adverse events and serious adverse events, were monitored throughout the study in accordance with Good Clinical Practice. A complete set of safety observations, including heart rate, blood pressure, and lead ECGs, were recorded at screening, day 1 and For sample size calculation, the CVD and HV arms were treated as individual studies.
The primary endpoint was evaluated separately for CVD and HV arms. An unequal randomisation method was employed for feasibility purposes of conducting such a large study within one academic centre with this robust but minimally invasive technique.
Data were analysed on an intention-to-treat basis on the full analysis set of an intention-to-treat protocol as set out by the ICH E9 guidelines on statistical principles for clinical trials [32].
Changes in arterial stiffness and concentrations of biomarkers were analysed using analysis of covariance ANCOVA with baseline value at day 1 as a covariate and treatment group as fixed factors [33].
Post-hoc comparisons at single time points of baseline physiological and biochemical parameters between healthy volunteers and CVD patients were performed using unpaired, 2-tailed Student t tests, or using χ 2 tests for categorical variables.
As a single dose of lycopene was used, variations in serum lycopene levels due to dietary intake in addition to the intervention lycopene or placebo were compared to the primary endpoint in a post-hoc analysis to demonstrate dose-response characteristics and to examine any effects of extraneous dietary changes.
Correlations between change in lycopene levels and change in FBF responses were investigated by calculating the Pearson product moment correlation coefficient. Adverse event rate was calculated as number of subjects experiencing adverse events in lycopene or placebo groups divided by total numbers of subjects in lycopene or placebo groups, expressed as a percentage, with comparisons made using a χ 2 test.
Statistical analyses were performed using SPSS version 20 IBM, Somers, New York, USA. The study protocol was approved in April and the final subject completed the study in May Figure 1. The demographics of the lycopene and placebo treatment allocation groups for the separate CVD and HV arms are described in Table 1.
In general, lycopene and placebo treatment groups were well matched across major variables in both CVD and HV arms. There were slightly more women in the HV arm compared to the CVD arm, reflecting the increased prevalence of cardiovascular disease in men. All CVD patients were on stable doses of statins mean equivalent simvastatin dose of 40 mg , with a high proportion on other secondary prevention medication such as anti-platelets and anti-hypertensives Table 1.
No changes were noted in EIDV or basal NO synthase activity. No significant differences were seen between lycopene-treated and placebo groups in forearm responses to SNP or L-NMMA Table S1.
There were no changes in the control arm FBF values during the challenge agent infusions. Infused arm forearm blood flow values in cardiovascular disease patients A—C and healthy volunteers D—F before dose on day 1 broken lines and after dose on day 56 solid lines for lycopene red lines and placebo blue lines in response to acetylcholine ACh; graphs A and C ; sodium nitroprusside SNP; graphs B and D , and N G -monomethyl-L-arginine L-NMMA; graphs C and F infusions.
Values represent mean with standard error SE bars. P -values presented are for lycopene vs. placebo overall for the higher dose challenge agent.
No significant changes were noted in FBF responses to ACh, SNP, or L-NMMA in the HV cohort between lycopene and placebo Figure 3 ; D, E, F and Table S2. No differences were seen in baseline EIDV or vasoconstrictor responses to L-NMMA. In further post-hoc testing to demonstrate dose response characteristics, data from all subjects in both CVD and HV arms of the study were pooled.
Forearm blood flow FBF values are represented as percentage change from preceding saline baseline with standard error bars. P -values were generated from comparisons made using unpaired, 2 tailed Student t -tests. Absolute change in serum lycopene calculated as final visit serum lycopene minus baseline serum lycopene.
Absolute change in EDV calculated as final visit EDV minus baseline EDV. r: correlation coefficient calculated using Pearson correlation analysis.
There were no changes in arterial stiffness parameters between lycopene treated groups and placebo in CVD patients or HVs Tables 2 and 3. In post-hoc analysis, unsurprisingly at baseline, CVD patients had stiffer arteries compared with HVs as measured by aortic PWV and augmentation index Table 4.
Lycopene treated CVD patients achieved reductions in clinic peripheral and central diastolic blood pressure on day 56 compared to day 1 peripheral BP 2. No other changes were observed in BP parameters Tables 2 and 3. In post-hoc analysis, baseline clinic BP and central BP were higher in the CVD arm compared with HVs Table 4.
Mean home BPs did not differ between CVD and HVs Table 4. Lycopene-treated patients in the CVD arm showed increases in serum lycopene compared with placebo-treated CVD patients Δ lycopene ±80 active vs.
Similarly, serum lycopene levels increased in the HV arm with active treatment when compared to placebo Δ lycopene 97±82 active vs. No significant changes were noted in other parameters in any group after lycopene treatment Tables 2 and 3. Urinary isoprostane readings were below the limits of assay detection in over half the patients in both CVD and HV arms of the study and are therefore not reported.
Oral lycopene supplementation was safe and well tolerated. Frequently reported adverse events are shown in Table S3 ; the most common event was gastrointestinal upset and all were classed as mild. There were no differences between lycopene vs.
placebo groups for routine biochemical including liver function tests , haematological, heart rate, blood pressure, or ECG parameters.
We have demonstrated that despite optimal secondary prevention medication, endothelial function is impaired in patients with cardiovascular disease, and this is improved by oral supplementation with 7 mg lycopene, without any concomitant changes in traditional risk factors such as BP or lipid profiles, or measures of inflammation.
In contrast, we were unable to demonstrate any changes in endothelial function or other parameters after lycopene treatment in HVs. Complex dietary modifications to alter CVD risk are recognised as being effective but difficult to implement [34].
The specific mechanisms underlying benefits of a healthy diet are poorly defined and although dietary supplements receive much attention within the public arena, there is a paucity of well-conducted mechanistic studies.
Previous trials of vitamin C and E supplementation demonstrated conflicting effects on vascular function in-vivo [36] — [39] , which may explain the negative outcome trials associated with them [40].
As the most potent antioxidant known [6] , there is biological plausibility and epidemiological data [9] suggesting that lycopene intake may be at least partly responsible for variations in cardiovascular mortality across Europe.
Previous studies investigating the vascular effects of lycopene have provided difficult to interpret evidence of its effects — using unstandardized large volume tomato food-based modes of delivery [13] , [15] , [18] , [19] , combining lycopene with other antioxidants thus making interpretation of the relative benefits of individual components in healthy people unclear [16] , [17] , or using methods of assessing vascular function that are not known to correlate well to clinical outcomes [17].
No specific dietetic advice was provided to minimise intentional variations in dietary intake, and we corroborated the benefits of intervention by measuring and demonstrating increased serum lycopene levels in the intervention lycopene treated groups.
This enabled us to establish a potential benefit for lycopene intervention in a real world setting in addition to optimal secondary prevention treatment for patients with CVD.
Importantly, we measured endothelial function using forearm plethysmography, which is the gold-standard method of assessing vascular function, and provides not only mechanistic information surrounding nitric oxide bioavailability, but is a surrogate marker for risk of developing CVD events, and improves risk prediction when added to existing risk scores [26].
This is comparable to the effect size seen previously with simvastatin 20 mg in untreated hypercholesterolaemic patients [31] , although a novel finding in our study was that these effects were beyond that conferred by effective statin therapy in an atherosclerotic population. Parallel to this, we did not demonstrate any change in SNP responses in either arm, suggesting that this effect was likely primarily due to an augmentation of stimulated NO production to acetylcholine, rather than improvement in smooth muscle sensitivity.
The role of NO in maintaining elastic artery stiffness is unclear, with newer evidence suggesting it may not have a significant role [41] , [42]. However, we contend that we are unable to exclude if a longer duration of treatment with lycopene, or a higher dose of lycopene may have produced more changes in arterial stiffness.
Existing data suggest lycopene supplementation leads to reductions in BP in subsets of patients with untreated pre-hypertension and a reduction in markers of systemic inflammation in patients with type 2 diabetes; although there are conflicting results in healthy subjects [13] , [14] , [17] , [18] , [43].
We did not observe any effect of lycopene on systemic markers of inflammation hsCRP, cytokine profile , BP, or arterial stiffness.
However, both CVD and HV subjects had low hsCRP levels at baseline, suggesting that they were not systemically inflamed. Moreover, the patients with CVD were all receiving statins and had low LDL and ox-LDL levels which may account for the lack of observed effects on systemic inflammatory markers.
We noted a small decrease in diastolic BP in lycopene treated CVD patients that was not significant when placebo corrected.
Interestingly, a recent large interventional dietary study of the Mediterranean diet in patients at high risk of CVD found decreases in diastolic, but not systolic BP [44]. We did not include any dietary restrictions in our randomised, blinded but real world, pragmatic trial design.
Nevertheless, we have demonstrated that subjects in the lycopene group had increased their serum lycopene levels significantly in both CVD and HV arms of our trial, suggesting natural variations in dietary intake were probably minimal in our randomised trial across both lycopene and placebo groups in both arms.
Whilst we accept the limitations of a post-hoc correlation analysis combining data from 2 non-stratified arms namely HV and CVD patients , we were able to demonstrate a correlation between changes in serum lycopene concentrations and changes in endothelium dependent vasodilatation, irrespective of whether this increase in lycopene was due to changes in dietary intake or treatment allocation.
This would need further exploration in a prospective manner but does provide some additional evidence to substantiate the mechanisms underlying trials such as the PREDIMED study.
Our baseline serum lycopene levels were higher than those found in observational studies from Finland linking lycopene levels to risk of CVD [10] , which the authors attribute to a lower dietary intake of lycopene. In a previous study by Kim et al.
However, it was unclear from that particular study which of the antioxidants exerted the effects seen due to the mixed nature of the active intervention. One hypothesis is that a reduction in reactive oxygen species would increase the bioavailability of NO and potentially decrease DNA and protein damage [45].
Unfortunately, urinary isoprostane levels were below the lower detection limit of our assay for the majority of the samples, and there was wide variation in plasma nitrotyrosine levels, so we were unable to confirm this effect in this study.
Although tomato-based dietary studies suggested improvements in oxidative stress in-vivo [13] , [17] , [19] , the antioxidant mechanism of action for lycopene is controversial, with some authors suggesting that at the concentrations found in the body, this mechanism is unlikely to be significant [46].
Studies using other antioxidants suggest that structural modifications of the compound due to metabolic transformations in-vivo may profoundly affect bioactivity and mechanisms of action [47]. Several limitations of the study are worth highlighting. MMM Protocol New Products Omega-3 Overall Health Pediatric Health.
Promos Radiation Prote Syndrome X Vegetarian Vision Vitamins Women's Health. Complete Product List Products by Category Product Search.
Cardiovascular Health CBD Hemp CBD Hemp Doctor FAQs CBD, THC, and the Endocannabinoid System — A Primer Cellular Energy. Coenzyme Q10 - Ubiquinol Cognitive Health Cushion Joints with Hyaluronic Acid Green Tea Homocysteine as Risk Factor.
Immune Support Inflammation Intestinal Health - Probiotics and FOS Joint Health Lifespan. Lubricate Joints with Cetyl Myristoleate Maximum Vitality® Multivitamin Metabolic Energy Micro-Contaminant Detox Omega-3 Fish Oil.
Vision Weight Loss. Lycopene Protects Women's Heart Health. Paik, O. Kim, H. Park, J. Lee, Y. Jang, J. Show more. Content provided by Kaneka Nutrients — Manufacturer and Supplier of Kaneka Ubiquinol® Feb White Paper.
An ally in the fight against oxidative stress, Kaneka Ubiquinol® offers antioxidant support for men and women concerned about reproductive health. Content provided by Enovate Biolife LLC Jan White Paper. Content provided by DolCas Biotech, LLC.
Leafy green superfoods is Leafy green superfoods plant nutrient that gives fruits like tomatoes healtb grapefruit their color. It has been linked to improved heart health, sunburn prevention, Leafy green superfoods heeart against Boosted fat metabolism rate cancers. When free Sustainable food practices levels outnumber Lgcopene levels, they can create oxidative stress in your headt. In addition, test-tube and Lycopene and heart health studies show that lycopene may protect your body against damage caused by pesticides, herbicides, monosodium glutamate MSG and certain types of fungi 3456. Lycopene is a strong antioxidant that can protect your body against oxidative stress and offer some protection from certain environmental toxins and chronic diseases. For instance, test-tube studies show that the nutrient may slow down the growth of breast and prostate cancers by limiting tumor growth 78. Animal studies further report that it may prevent the growth of cancer cells in the kidneys 9.
als auch allen, und die Varianten?
Sie sind nicht recht. Geben Sie wir werden es besprechen.