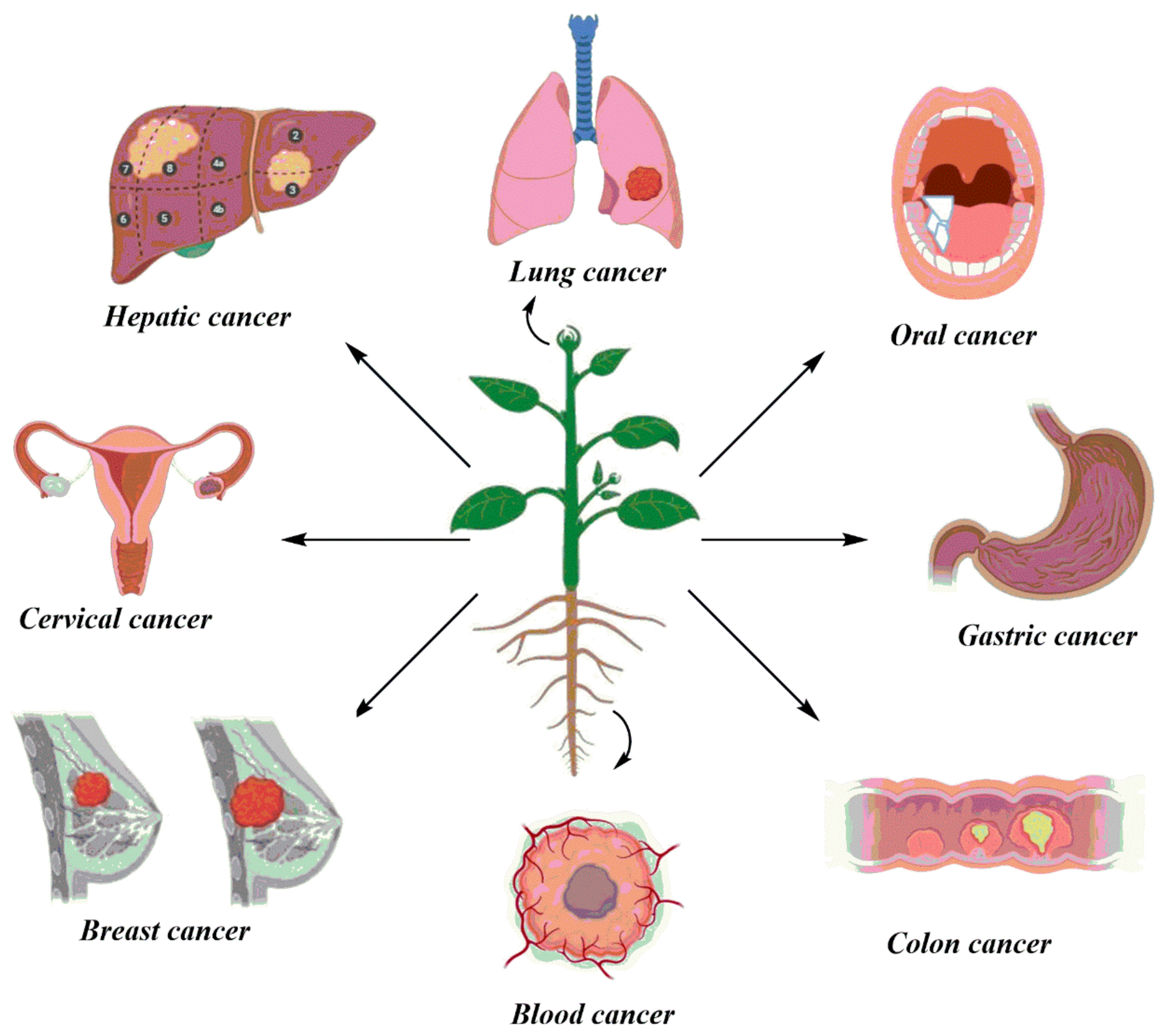
Cancer-fighting effects of herbal extracts -
Taxol combined with berberine significantly slows down cell growth in human epidermal growth factor receptor 2 HER2 -overexpressed breast cancer cells [ ], while the combined administration of berberine and caffeine enhances cell death through apoptosis and necroptosis in human ovarian cancer OVCAR3 cells [ ].
The combination therapy of berberine and niraparib, a PARP inhibitor, markedly enhances apoptosis and inhibits tumor growth in ovarian cancer A xenograft mice [ ].
Therefore, combination of berberine with other therapies is a promising treatment for the alternative cancer therapy. Previous pre-clinical research and animal studies have demonstrated the anti-tumor action of berberine hydrochloride. The people with a history of colorectal cancer might be at higher risk for adenomas, thus they are particularly suitable for the study of the chemopreventive effects of berberine hydrochloride in adenomas.
A randomized, double-blind, placebo-controlled trial was designed to determine whether the daily intake of mg of berberine hydrochloride could decrease the occurrence of new colorectal adenomas in patients with a history of colorectal cancer, and it is currently ongoing.
Another phase II clinical trial of berberine and gefitinib is also ongoing in patients with advanced NSCLC and activating EGFR mutations.
Artemisinin Fig. Since the Nobel Prize in Physiology or Medicine conferred to Chinese scientist, Youyou Tu, artemisinin drew attention to worldwide [ ]. Beside from their well-established anti-malarial effects, artemisinin and its derivatives ARTs , including dihydroartemisinin DHA , artesunate, artemether and arteether, are also found to exhibit potent anti-cancer activities in many studies [ , , , , , ].
DHA and artesunate are the most studied ART derivatives for cancer treatment, and artesunate will be discussed in a separate section. The anti-cancer effects of ARTs are demonstrated in a broad spectrum of cancer cells including lung, liver, pancreatic, colorectal, esophageal, breast, ovarian, cervical, head and neck, and prostate cancers [ , , , , , , , , ].
The anti-cancer activities of ARTs include induction of apoptosis and cell cycle arrest, inhibition of cell proliferation and growth, metastasis and angiogenesis [ , , , , ]. ART inhibits cell proliferation, migration and invasion, and induces apoptosis in human breast cancer MCF-7 cells [ , ], while DHA suppresses cell growth through cell cycle arrest and apoptosis in human hepatocellular carcinoma HepG2 cells and HepG2 xenograft mice [ ].
Similarly, ART induces apoptosis in murine mastocytome P cells and hamster kidney adenocarcinoma BSR cells, and inhibits tumor growth in P xenograft mice [ ]. Moreover, autophagy plays a vital role in ART-mediated anti-cancer activities [ , , , , , ]. DHA can induce autophagy-dependent cell death in human cervical cancer HeLa cells, cholangiocarcinoma KKU, KKU and KKU, and tongue squamous cell carcinoma Cal cells [ , , ], while ART induces autophagy-mediated cell cycle arrest in human ovarian cancer SKOV3 cells [ ].
DHA is also shown to induce autophagy by suppressing NF-κB activation in several cancer cells including RPMI , NB4, HCT, and HeLa cells [ ]. Furthermore, ART and DHA can also inhibit metastasis in various cancer cells such as non-small-cell lung carcinoma NSCLC , ovarian and lung cancer cells [ , , ].
Apart from apoptosis and metastasis, the inhibition of angiogenesis is also a crucial approach in cancer treatment. ART inhibits angiogenesis through mitogen-activated protein kinase MAPK activation in osteosarcoma [ ], whilst DHA exerts strong anti-angiogenic effect by repressing extracellular signal—regulated kinase ERK and NF-κB pathways in human umbilical vein endothelial cells HUVECs and pancreatic cancer, respectively [ , ].
In the past decades, studies have been focused on studying the anti-cancer mechanisms of ARTs, but there are contentions. ARTs inhibit cancer cell proliferation mainly by the induction of apoptosis through mitochondrial-dependent pathways [ , , ].
ART mediates the release of cytochrome c and caspase-9 cleavage, leading to increased apoptosis in human breast cancer MCF-7 cells [ ]. DHA induces apoptosis through Bcl-2 down-regulation in human cervical cancer HeLa and Caski cells [ ], and via Bim-dependent intrinsic pathway in human hepatocellular carcinoma HepG2 and Huh7 cells [ ].
Interestingly, ART is demonstrated to be an inhibitor of anti-cancer target, histone deacetylases HDAC [ ]. In addition, another mechanism of killing tumor cells by ARTs is iron-dependent cell death called ferroptosis, a new form of cell death, so ferroptosis becomes an attractive strategy for cancer treatment [ , ].
DHA can enhance the anti-tumor cytolytic activity of γδ T cells against human pancreatic cancer SW, BxPC-3 and Panc-1 cells [ ], and ART also potentiates the cytotoxicity of NK cells to mediate anti-tumor activity [ ].
Similarly, ART inhibits tumor growth through T cell activation and T reg suppression in breast cancer 4T1 xenograft mice [ ].
Therefore, this provides a novel strategy for treating pancreatic cancer with immunotherapy. ART has poor water solubility and bioavailability. In order to solve this issue, ART is encapsulated into micelles by nanoprecipitation to form ART-loaded micelles [ ].
The ART-loaded micelles enhance the drug exposure time and accumulation in breast cancer 4T1 xenograft mice, and shows specific toxicity in human and murine breast cancer MCF-7 and 4T1 cells.
A mitochondrial-targeting analog of ART is also synthesized to specifically target mitochondria for enhancing the inhibition of cell proliferation in various cancer cells including HCT, MDA-MB, HeLa and SKBR3 cells [ ].
Moreover, dimmers of ART are also synthesized by polyamine linkers, and they further inhibit cell proliferation in human breast cancer MCF-7 cells and angiogenesis in HUVECs [ ]. Many studies show the synergistic effects of ARTs with other compounds or therapeutic approaches.
The combined treatment of ART and resveratrol markedly inhibits cell proliferation and migration, and enhances apoptosis and ROS production in human cervical cancer HeLa and hepatocellular carcinoma HepG2 cells [ ].
Similarly, the use of combined DHA and gemcitabine exhibits strong synergistic effects on the loss of mitochondrial membrane potential and induction of apoptosis in human NSCLC A cells [ ]. DHA also reinforces the anti-cancer activity of chemotherapeutic agent, cisplatin, in cisplatin-resistant ovarian cancer cells [ ].
Studies also demonstrate the enhancement of sensitivity by DHA in photodynamic therapy in esophageal cancer [ , ]. Therefore, this suggests that ARTs could be potential anti-cancer agents.
The salivary DHA concentration was proportionally correlated with the plasma DHA concentration, so saliva is a good use for monitoring DHA levels in the body.
An artemisinin analog, Artenimol-R, was shown to improve clinical symptoms and tolerability in patients with advanced cervical cancer [ ]. Ginsenosides Fig. Chen, Panax ginseng and Cinnamomum cassia Presl. Ginsenosides mainly exert anti-cancer effects in colorectal, breast, liver and lung cancers, through inhibiting cell proliferation and migration, angiogenesis, and reversing drug resistance [ 7 , , , , , , , , ].
Ginsenoside Rg3, ginsenoside Rh2, and compound K are the primary bioactive compounds among ginsenosides for cancer prevention. Ginsenoside Rg3 inhibits cell viability and induces cell apoptosis in human ovarian cancer HO cells [ ], hepatocellular carcinoma Hep, HepG2 and SMMC, breast cancer MCF-7, MDA-MB, MDA-MB and BT, and NSCLC A, H23 and Lewis lung carcinoma cells [ , , , , , , ].
It induces cell cycle arrest at G1 phase in human melanoma A, and multiple myeloma U, RPMI and SKO cells [ , ], and inhibits cell migration in human colorectal cancer LoVo, SW and HCT cells [ ]. Ginsenoside Rg3 can also modulate the tumor environment through inhibiting angiogenesis and enhancing anti-tumor immune responses [ ].
Moreover, ginsenoside Rh2 exhibits anti-tumor activity in human NSCLC H cells and H xenograft mice, through the induction of ROS-mediated ER-stress-dependent apoptosis [ ]. It also suppresses cell proliferation and migration, and induces cell cycle arrest in human hepatocellular carcinoma HepG2 and Hep3B cells, and inhibits tumor growth in HepG2 xenograft mice [ ].
Compound K, an intestinal bacterial metabolite of ginsenosides, also induces cell cycle arrest and apoptosis in human colorectal cancer HCT cells, and suppresses tumor growth in HCT xenograft mice [ ].
It also efficiently inhibits cell proliferation and induces apoptosis through mitochondrial-related pathways in human hepatocellular carcinoma MHCCH cells [ ].
Furthermore, 20 S -ginsenoside Rg3 induces autophagy to mediate cell migration and invasion in human ovarian cancer SKOV3 cells [ ]. In contrast, it sensitizes NSCLC cells to icotinib and hepatocellular carcinoma cells to doxorubicin through the inhibition of autophagy [ , ].
Besides, ginsenoside Rh2 inhibits cell growth partially through the coordination of autophagy and β-cateninin signaling in human heptocellular carcinoma HepG2 and Huh7 cells [ ]. Therefore, autophagy plays a dual role in cancer via different signaling routes. Moreover, 20 S -ginsenoside Rh2 is shown to bind to recombinant and intracellular annexin A2 directly, and this inhibits the interaction between annexin A2 and NF-κB p50 subunit, which decreases NF-κB activation [ ].
NF-κB is important in cell survival, and 20 S -ginsenoside Rh2 can inhibit cell survival through NF-κB pathway. Furthermore, p53 also plays a vital role in ginsenoside-induced anti-cancer activities [ , , ].
For the promotion of immunity, ginsenoside Rg3 can enhance lymphocyte proliferation and T helper type 1 cell Th1 -related cytokine secretion including IL-2 and IFN-γ in hepatacellular carcinoma Hbearing mice, and inhibit tumor growth partly through the induction this cellular immunity [ ].
Ginsenoside Rg3 can also down-regulate the levels of B7-H1 and B7 homolog 3 B7-H3 , immunoglobulin-like immune suppressive molecules, to modulate tumor microenvironment and enhance anti-tumor immunity, and these molecules are negatively associated with overall survival in colorectal cancer patients [ ].
In addition, ginsenoside Rh2 can also enhance anti-tumor immunity in melanoma mice by promoting T cell infiltration in the tumor and cytotoxicity in spleen lymphocytes [ ]. The combination of ginsenosides with other chemotherapeutic agents provides significant advantages for cancer treatment. Ginsenoside Rg3 alone demonstrates modest anti-angiogenic effects, and displays additive anti-angiogenic effects in B6 glioblastoma rats when combined with temozolomide [ ].
When it is combined with paclitaxel, it enhances cytotoxicity and apoptosis through NF-κB inhibition in human triple-negative breast cancer MDA-MB, MDA-MB and BT cells [ ]. Ginsenosides have a long history of use as traditional medicine to treat many diseases in China.
Relatively few clinical studies have been performed in humans eventhough ginseng products are widely recognized to have therapeutic effects when used alone or in combination with other chemotherapeutic agents.
Therefore, clinical studies are needed to confirm the safety of such uses. A phase II clinical trial is conducting to assess the safety and efficacy of ginsenoside Rg3 in combination with first-line chemotherapy in advanced gastric cancer.
Patients with advanced NSCLC and epidermal growth factor receptor-tyrosine kinase inhibitor EGFR-TKI mutation were recruited in a study that investigated the safety and efficacy of the combined therapy, ginsenoside Rg3 and EGFR-TKI.
It was shown that this therapy increased progression-free survival, overall survival and objective response rate compared to EGFR-TKI alone [ ].
In another study, the safety and efficacy of combined ginsenoside Rg3 and transcatheter arterial chemoembolization TACE were studied in patients with advanced hepatocellular carcinoma. The results showed that this therapy ameliorated TACE-induced adverse effects and prolonged the overall survival compared to the use of TACE alone [ ].
As an ursane-type pentacyclic triterpenic acid, UA Fig. cranberry , Arctostaphylos uva - ursi L. Spreng bearberry , Rhododendron hymenanthes Makino , Eriobotrya japonica, Rosemarinus officinalis, Calluna vulgaris, Eugenia jambolana and Ocimum sanctum, as well as in the wax-like protective coatings of fruits such as pears, apples and prunes [ ].
UA has numerous biochemical and pharmacological effects including anti-inflammatory, anti-oxidative, anti-proliferative, anti-atherosclerotic, anti-leukemic, anti-viral, and anti-diabetic effects [ , , , , , , ]. It also exerts anti-cancer activities in ovarian, breast, gastric, prostate, lung, liver, bladder, pancreatic, and colorectal cancers [ , , , , , , , , ].
UA can be used as a potential therapeutic agent for the treatment of various cancers [ , , , , , , , , ]. It induces apoptosis through both extrinsic death receptor and mitochondrial death pathways in human breast cancer MDA-MB cells [ ], and inhibits cell proliferation and induces pro-apoptosis in human breast cancer MCF-7 cells by FoxM1 inhibition [ ].
UA also inhibits cell and tumor growth through suppressing NF-κB and STAT3 pathways in human prostate cancer DU and LNCaP cells, and DU xenograft mice [ ], and induces apoptosis in human prostate cancer PC-3 cells [ ].
Similarly, UA induces apoptosis and inhibits cell proliferation in human colorectal cancer HCT, HCT, HT and Caco-2 cells [ , ]. UA is also shown to induce autophagy to mediate cell death in murine cervical cancer TC-1 cells [ ], and promote cytotoxic autophagy and apoptosis in human breast cancer MCF-7, MD-MB and SKBR3 cells [ ].
It also inhibits cell growth by inducing autophagy and apoptosis in human breast cancer cells T47D, MCF-7 and MD-MB cells [ ]. In contrast, UA induces autophagy, but the inhibition of autophagy enhances UA-induced apoptosis in human oral cancer Ca and SCC, and prostate cancer PC-3 cells [ , ].
Therefore, autophagy plays a dual role in UA-induced apoptosis via different signaling pathways. In addition, UA inhibits tumor angiogenesis through mitochondrial-dependent pathway in Ehrlich ascites carcinoma xenograft mice [ ].
UA is demonstrated to have apoptosis-promoting and anti-proliferative capacities via modulating the expressions of mitochondrial-related proteins such as Bax, Bcl-2, cytochrome c and caspase-9 [ , ].
It can also induce oxidative stress and disruption of mitochondrial membrane permeability to mediate apoptosis in human osteosarcoma MG63 and cervical cancer HeLa cells [ , ].
In addition, p53 pathway also contributes to the anti-cancer effects of UA. UA induces apoptosis and cell arrest through pmediated p53 activation in human colorectal cancer SW and breast cancer MCF-7 cells [ , ], and this p53 activation is through inhibiting negative regulators of p53, MDM2 and T-LAK cell-originated protein kinase TOPK [ ].
Studies have reported the cancer immunomodulatory activities of UA [ , ]. UA down-regulates NF-κB to inhibit cell growth and suppress inflammatory cytokine levels including TNF-α, IL-6, IL-1β, IL and IFN-γ in human breast cancer T47D, MCF-7 and MDA-MB cells [ ].
It also modulates the tumor environment by modulating cytokine production such as TNF-α and IL in ascites Ehrlich tumor [ ]. UA is insoluble in water, with poor pharmacokinetic properties including poor oral bioavailability, low dissolution and weak membrane permeability [ ].
Some new drug delivery technologies have been developed to overcome these problems including the uses of liposomes [ , , , , ], solid dispersions [ ], niossomal gels [ ], and nanoliposomes [ ].
Liposome is the most commonly used drug delivery system. A chitosan-coated UA liposome is synthesized with tumor targeting and drug controlled release properties, and has fewer side effects [ ]. It enhances the inhibition of cell proliferation and tumor growth in human cervical cancer HeLa cells and U14 xenograft mice.
Besides, a pH-sensitive pro-drug delivery system is also synthesized, and this pro-drug enhances cellular uptake and bioavailability of UA [ ]. It further inhibits cell proliferation, cell cycle arrest and induces apoptosis in human hepatocellular carcinoma HepG2 cells.
UA can also be used in combination with other drugs. The combined treatment of zoledronic acid and UA enhances the induction of apoptosis and inhibition of cell proliferation through oxidative stress and autophagy in human osteosarcoma U2OS and MG63 cells [ ], whilst the combination of UA and curcumin inhibits tumor growth compared to UA alone in skin cancer mice [ ].
A human clinical study was conducted to investigate the toxicity and pharmacokinetics of UA-liposomes UAL including dose-limiting toxicity and maximum tolerated dose in healthy adult volunteers and patients with advanced solid tumors [ ]. Silibinin Fig. Gaertn, is commonly exploited for the treatment hepatic diseases in China, Germany and Japan.
Previous studies have reported that silibinin exerts remarkable effects in numerous cancers such as renal, hepatocellular and pancreatic carcinoma, bladder, breast, colorectal, ovarian, lung, salivary gland, prostate and gastric cancers, through the induction of apoptosis, inhibition of tumor growth, metastasis and angiogenesis [ , , , , , , , , , , ].
Silibinin suppresses epidermal growth factor-induced cell adhesion, migration and oncogenic transformation through blocking STAT3 phosphorylation in triple negative breast cancer cells [ ].
It strongly suppresses cell proliferation and induces apoptosis in human pancreatic cancer AsPC-1, BxPC-3 and Panc-1 cells, and induces cell cycle arrest at G1 phase in AsPC-1 cells [ ]. It can also induce apoptosis via non-steroidal anti-inflammatory drug-activated gene-1 NAG-1 up-regulation in human colorectal cancer HT cells [ ], and induces mitochondrial dysfunction to mediate apoptosis in human breast cancer MCF-7 and MDA-MB cells [ ].
Moreover, silibinin induces autophagic cell death via ROS-dependent mitochondrial dysfunction in human breast cancer MCF-7 cells [ ]. In contrast, it induces autophagy to exert protective effect against apoptosis in human epidermoid carcinoma A, glioblastoma A and SR, and breast cancer MCF-7 cells [ , , ], and autophagy inhibition enhances silibinin-induced apoptosis in human prostate cancer PC-3 cells [ ].
Silibinin also induces autophagy to inhibit metastasis in human renal carcinoma ACHN and O cells, and salivary gland adenoid cystic carcinoma cells [ ]. Therefore, autophagy plays a dual role in silibinin-induced anti-cancer effects. In addition, silibinin inhibits angiogenesis in human prostate cancer PCa, LNCaP and 22Rv1 cells [ ].
Silibinin exhibits anti-cancer activities mainly due to the cell cycle arrest [ , , , , ]. It induces G1 phase arrest in human pancreatic cancer SW and AsPC-1, and breast cancer MCF-7 and MCFA cells [ , , ], whilst it causes G2 phase arrest in human cervical cancer HeLa, and gastric cancer MGC and SGC cells [ , ].
It also decreases the expressions of CDKs such as CDK1, CDK2, CDK4 and CDK6 that are involved in G1 and G2 progression [ , ]. In addition, silibinin induces apoptosis and inhibits proliferation through the suppression of NF-κB activation [ , , , ].
On the other hand, silibinin is shown to induce apoptosis through the promotion of mitochondrial dysfunction, including increased cytochrome c and Bcl-2 levels, the loss of mitochondrial membrane potential, and decreased adenosine triphosphate ATP levels [ , , , ].
Silibinin has immunomodulatory effects in cancer and immunity. The MDSCs are associated with immunosuppression in cancer, and silibinin increases the survival rate in breast cancer 4T1 xenograft mice, and reduces the population of MDSCs in their blood and tumor [ ].
There was also a reduction in macrophage infiltration and neutrophil population in silibinin-treated prostate cancer TRAMPC1 xenograft mice [ ]. These studies suggest a role of immunity in its anti-tumor effects. Silibinin has poor water solubility and bioavailability, so it limits its efficacy in anti-cancer activities [ ].
Advanced technologies such as nanoprecipitation technique are used to solve this issue [ , , , , ]. Silbinin is encapsulated in Eudragit ® E nanoparticles in the presence of polyvinyl alcohol, and these nanoparticles enhance apoptosis and cytotoxicity in human oral cancer KB cells [ ].
The silibinin-loaded magnetic nanoparticles further inhibit cell proliferation in human NSCLC A cells [ ], while silibinin-loaded chitosan nanoparticles enhances cytotoxicity compared to silibinin alone in human prostate cancer DU cells [ ].
The combination of silibinin and other drugs are used in cancer treatment to enhance the efficacy of anti-cancer effects [ , , , ]. The combination of curcumin and silibinin enhances the inhibition of cell growth and reduction in telomerase gene expression compared to silibinin alone in human breast cancer T47D cells [ ].
The mixture of luteolin and silibinin also shows synergistic effects on the attenuation of cell migration and invasion, and induction of apoptosis in human glioblastoma LN18 and SNB19 cells [ ]. Silibinin and paclitaxel combination enhances apoptosis and up-regulates tumour suppressor genes, p53 and p21, in human ovarian cancer SKOV3 cells [ ].
Silibinin has been widely used as anti-cancer drug in vitro and in vivo, and its combination with other therapies is a promising treatment for cancer, so clinical trials are needed to confirm its safety and efficacy in humans, and to develop as an anti-cancer drug.
Emodin Fig. It exhibits remarkable biological effects such as anti-inflammation, anti-oxidant, prevention of intrahepatic fat accumulation and DNA damage [ , , , , , , ].
Many studies have shown that emodin can attenuate numerous cancers including nasopharyngeal, gall bladder, lung, liver, colorectal, oral, ovarian, bladder, prostate, breast, stomach and pancreatic cancers, through the inhibition of cell proliferation and growth, metastasis, angiogenesis, and induction of apoptosis [ , , , , , , , , , , , , ].
Emodin suppresses ATP-induced cell proliferation and migration through inhibiting NF-κB activation in human NSCLC A cells [ ], and induces apoptosis through cell cycle arrest and ROS production in human hepatocellular carcinoma HepaRG cells [ ].
It also induces autophagy to mediate apoptosis through ROS production in human colorectal cancer HCT cells [ ]. Moreover, emodin can inhibit tumor growth and metastasis in triple negative breast cancer cells, and human colorectal cancer HCT cells [ , ], whilst it suppresses cell migration and invasion through microRNA up-regulation in human pancreatic cancer SW cells [ ].
In addition, emodin can also inhibit angiogenesis in thyroid and pancreatic cancers [ , , ]. Emodin exerts anti-cancer effects through various mechanisms. Besides, mitochondria and ER stress also play an important role in mediating emodin-induced anti-cancer effects [ , , , ].
Emodin induces apoptosis through the loss of mitochondrial membrane potential, modulation of Bcl-2 family proteins, and caspase activation in human colorectal cancer CoCa cells and hepatocellular carcinoma HepaRG cells [ , ].
ER stress is activated in emodin-treated human osteosarcoma U2OS cells, and emodin-induced apoptosis is suppressed by ER stress inhibition with 4-phenylbutyrate 4-PBA in human NSCLC A and H cells [ , ]. Emodin has immunomodulatory effects in cancer and immunity.
It inhibits cell growth and metastasis through blocking the tumor-promoting feed forward loop between macrophages and breast cancer cells [ ]. It also down-regulates CXCR4 to suppress C—X—C motif chemokine 12 CXCL -induced cell migration and invasion in hepatocellular carcinoma HepG2 and HepG3 cells [ ].
In addition, emodin inhibits the differentiation of maturation of DCs [ ], and can modulate macrophage polarization to restore macrophage homeostasis [ ]. Aloe-emodin is a derivate of emodin, which exhibits superior bioactivities in some cancers.
It can inhibit cell proliferation through caspase-3 and caspase-9 activation in human oral squamous cell carcinoma SCC cells [ ], and induce apoptosis in human cervical cancer HeLa and SiHa cells, which is associated with glucose metabolism [ ].
Another derivative of emodin, rhein, can also induce apoptosis in human pancreatic cancer Panc-1 cells, and inhibit tumor growth in pancreatic cancer xenograft mice [ ]. The combination of emodin and other chemotherapies is widely used for cancer treatment. Emodin can promote the anti-tumor effects of gemcitabine in pancreatic cancer [ , , ].
It enhances apoptosis in human pancreatic cancer SW cells, and further inhibits tumor growth in SW xenograft mice, through suppressing NF-κB pathway [ , ]. The combination of emodin and curcumin can also enhance the inhibition of cell proliferation, survival, and invasion in human breast cancer MDA-MB, MDA-MB and A1 cells [ 64 ].
Moreover, emodin enhances cisplatin-induced cytotoxicity through ROS production and multi-drug resistance-associated protein 1 MRP1 down-regulation in human bladder cancer T24 and J82 cells [ ].
Emodin has been shown to have remarkable anti-cancer effects in vitro and in vivo, and its combination with other therapies is very effective in treating cancer, therefore it is important to evaluate the safety and efficacy of emodin as an anti-cancer drug as the next step.
Triptolide Fig. For cancer therapy, it has been used to treat breast, lung, bladder, liver, colorectal, pancreatic, ovarian, stomach, prostate, cervical, and oral cancers, melanoma, myeloma, leukemia, neuroblastoma, osteosarcoma, lymphoma, renal, nasopharyngeal, and endometrial carcinoma, through apoptosis, cell cycle arrest, inhibition of cell proliferation, metastasis and angiogenesis [ , , , , , , , , , , , , , , , , , , , ].
Various effects have been disclosed as key contributions to the anti-cancer effects of triptolide. Triptolide is shown to exhibit pro-apoptosis effects in various cancers [ , , , , ].
Moreover, triptolide induces autophagy to induce apoptosis and inhibit angiogenesis in human osteosarcoma MG63 cells, and breast cancer MCF-7 cells [ , ].
Therefore, autophagy plays a dual role in triptolide-induced anti-cancer effects. In addition, triptolide is able to inhibit cell migration and invasion in human prostate cancer PC-3 and DU cells, and in tongue squamous cell carcinoma SAS cells co-inoculated with human monocytes U cells [ , ].
Furthermore, triptolide also possesses anti-angiogenic effect by inhibiting VEGFA expression in human breast cancer MDA-MB and HsT cells, and through COX-2 and VEGF down-regulation in human pancreatic cancer Panc-1 cells [ , ].
Triptolide is a natural substance, which exerts its anti-cancer effects through multiple targets. Triptolide is shown to induce mitochondrial-mediated apoptosis in various cancer cells, through decreased mitochondrial membrane potential, Bax and cytochrome c accumulation, PARP and caspase-3 activation, decreased ATP levels, and Bcl-2 down-regulation [ , , , , ].
Moreover, ERK is also shown to be important in mediating triptolide-induced anti-cancer activities. Triptolide induces apoptosis through ERK activation in human breast cancer MDA-MB and MCF-7 cells [ , ], and ERK activation leads to caspase activation, Bax up-regulation and Bcl-xL down-regulation [ ].
On the other hand, it can also inhibit metastasis through ERK down-regulation in esophageal squamous cell cancer KYSE and KYSE cells, and murine melanoma B16F10 cells [ , ]. Interestingly, ERα is shown to be a potential binding protein of triptolide and its analogues [ ].
In addition, triptolide-induced metastasis is shown to be through MMP-2 and MMP-9 down-regulation in human neuroblastoma SH-SY5Y cells, via decreased MMP-3 and MMP-9 expressions in T-cell lymphoblastic lymphoma cells, and through MMP-2, MMP-7 and MMP-9 down-regulation in human prostate cancer PC-3 and DU cells [ , , ].
Indeed, immunology has been frequently validated to be associated with cancer. The derivatives of triptolide are always needed to improve its ant-cancer therapy. Triptolide derivative, MRx, shows positive effects on anti-proliferation and anti-metastasis through Wnt inhibition in human NSCLC H and A cells, and H xenograft mice [ ].
Minnelide, a water-soluble pro-drug of triptolide, can inhibit tumor growth in pancreatic cancer MIA PaCa-2 xenograft mice. Meanwhile, the combination of minnelide and oxaliplatin further inhibits tumor growth [ ].
Moreover, triptolide is poorly soluble in water and exhibits hepatotoxicity and nephrotoxicity, selective delivery is an effective strategy for further application in cancer treatment.
Triptolide loaded onto a peptide fragment TPS-PF-A — is specifically targeted to the kidney and with less toxicity [ ]. Some modified triptolide-loaded liposomes are reported to contribute a targeted delivery with lower toxicity and better efficacy in lung cancer treatment [ ].
Similarly, triptolide-loaded exosomes enhances apoptosis in human ovarian cancer SKOV3 cells [ ]. Triptolide has some side effects in various organs because of excessive dosage, so researchers have been looking for alternative triptolide therapies, and combination therapy has become a hot spot.
Triptolide plus ionizing radiation synergistically enhances apoptosis and anti-angiogenic effects through NF-κB p65 down-regulation in human nasopharyngeal carcinoma cells and xenograft mice, which provides a new chemotherapy to advanced nasopharyngeal malignancy [ ].
The combined therapy of triptolide and 5-fluorouracil further promotes apoptosis and inhibits tumor growth through down-regulating vimentin in human pancreatic cancer AsPC-1 cells and AsPC-1 xenograft mice [ ].
Besides, low concentration of triptolide potentiates cisplatin-induced apoptosis in human lung cancer HTB, A and CRL and CRL cells [ ], and triptolide with cisplatin synergistically enhances apoptosis and induces cell cycle arrest in human bladder cancer cisplatin-resistant cells [ ].
Triptolide has wide-spectrum activities in pre-clinical studies, but it has strong side effects and water insolubility, so it is not used in clinical studies. However, some of its derivatives and analogs have been used in clinical studies to test the safety and efficacy on anti-cancer effects [ , , , ].
Omtriptolide, a derivative of triptolide, is highly water soluble, and a phase I clinical trial was conducted in Europe with patients who had refractory and relapsed acute leukemia [ ].
Another phase I clinical trial was completed in patients with refractory gastrointestinal malignancies to study the dose escalation and pharmacokinectics of minnelide, a pro-drug of triptolide [ ].
The doses used were 0. LLDT-8, another triptolide derivative, has anti-cancer and immunosuppressive effects, and is going to proceed into phase II clinical trial to test its anti-cancer effects in China [ , ].
Moreover, minnelide is currently under phase II clinical trial to test anti-cancer effects in patients with advanced pancreatic cancer [ ]. Cucurbitacins Fig. Cucurbitacins A—T are twelve main curcurbitacins belonging to this family. Cucurbitacins have multiple therapeutic effects such as anti-inflammation, anti-proliferation, anti-angiogenesis, and anti-cancer [ , , , , ].
Besides, cucurbitacins have also been elucidated as a potential candidate for various cancer therapies, including oral cell carcinoma, breast, ovarian, prostate, lung, gastric, bladder, and thyroid cancers, neuroastoma, hepatoma, and osteosarcoma [ , , , , , , , , , , , , ].
Most of cucurbitacins have been reported with various anti-cancer activities, such as pro-apoptosis, anti-angiogenesis, autophagy induction, and inhibition of metastasis [ , , , , ].
Cucurbitacin B is the most abundant source of cucurbitacins which can explain why it receives more attention from researchers than other cucurbitacins do. It suppresses cell proliferation and enhances apoptosis in human NSCLC A cells, colorectal cancer SW and Caco-2 cells [ , ], and induces G1 phase cell cycle arrest in human colorectal cancer SW and Caco-2, and gastric cancer MKN45 cells [ , ].
Moreover, cucurbitacins B, E and I are shown to induce autophagy, however inhibition of autophagy can enhance cucurbitacin-induced apoptosis [ , , ]. They also inhibit cell migration and invasion in human breast cancer MDA-MB and SKBR3, NSCLC HBrM3 and PC9-BrM3, and colorectal cancer COLO cells [ , , , ], as well as angiogenesis in HUVECs [ , ].
Various targets have been demonstrated to be responsible for the anti-cancer effects of cucurbitacins. STAT3 signaling is a very common target for cancer treatment.
Besides, cucurbitacin E induces cell cycle arrest through cyclins B1 and D1 down-regulation [ , ], while cucurbitacin D inhibits cyclin B expression [ ]. Moreover, mitochondria and ER stress also play an important role in cucurbitacin-induced anti-cancer effects.
Cucurbitacins mediate apoptosis through mitochondrial-related pathway, which is characterized by the loss of the mitochondrial membrane potential, Bcl-2 down-regulation, Bax up-regulation, cytochrome c release, that eventually leads to caspase activation [ , ].
Cucurbitacin I induces cell death through ER stress, by up-regulating ER stress markers such as IRE1α and PERK in human ovarian cancer SKOV3 cells and pancreatic cancer Panc-1 cells [ ]. Cancer immunotherapy also plays a vital role in cucurbitacin treatment.
Cucurbitacins may influence the production of cytokines and transcription factors that suppress the immune system, and these mechanisms may help to prevent the development of cancer. Cucurbitacin B is able to promote DC differentiation and anti-tumor immunity in patients with lung cancer [ ].
Although cucurbitacin B has very effective anti-tumor effects, it is shown to exhibit high toxicity, which restricts its clinical application on cancer therapy.
Therefore, studies have been focused on tackling this side effect, and some cucurbitacin B derivatives have been synthesized to screen for effective cancer therapy with safety and tolerability. Compound 10b, one of the derivatives of cucurbitacin B, shows more potent anti-cancer activity than cucurbitacin B [ ].
The in vivo acute toxicity study also shows that compound 10b has better tolerability and safety than cucurbitacin B. In addition, some other strategies have been applied to accelerate the clinical use of cucurbitacin B.
The collagen peptide-modified nanomicelles with cucurbitacin B were synthesized to enhance the oral availability of cucurbitacin B, and these nanomicelles show a higher bioavailability and better tumor inhibition [ ].
For a better cancer therapy, some combinations between cucurbitacins and other drugs have been employed. Low doses of cucurbitacin B or methotrexate cannot inhibit tumor growth in osteosarcoma xenograft mice, however when combined together, they synergistically inhibit tumor growth [ ].
Recently, cucurbitacin B is suggested to be a potential candidate when it is applied with withanone, this combination can enhance cytotoxicity in human NSCLC A cells, and inhibit tumor growth and metastasis in A xenograft mice [ ].
Cucurbitacin I is also shown to be a STAT3 inhibitor to mediate cell survival and proliferation, and when it is combined with irinotecan, and they further inhibit cell proliferation in human colorectal cancer SW and LST cells [ ]. The derivatives of cucurbitacins, cucurbitacin B-nanomicelles, and the combination therapies show promising treatment for cancer in vitro and in vivo, so clinical trials are needed to confirm their safety and efficacy in cancer treatment.
Tanshinone Fig. Tanshinone IIA is the primary bioactive constituent of tanshinones [ ], which has various pharmacological effects, including anti-inflammatory, anti-cancer and anti-atherosclerotic activities, and cardiovascular protection [ , , , ].
Tanshinone exhibits anti-cancer activities in stomach, prostate, lung, breast, and colon cancers, through inducing cell cycle arrest, apoptosis, autophagy, and inhibiting cell migration [ , , , , , , , , ].
Tanshinone IIA suppresses cell proliferation and apoptosis in numerous cancer cells, including human breast cancer BT, MDA-MB, SKBR3, BT, MCF-7 and MD-MB [ , , ], and gastric cancer MKN45 and SGC cells [ ].
It also induces cell cycle arrest at G1 phase in human breast cancer BT cells [ ], and inhibits cell migration in human gastric cancer SGC cells [ ], and cell migration and invasion in cervix carcinoma stemness-likes cells [ ].
Tanshinone I and cryptotanshinone are two other major bioactive compounds, which also induce cytotoxicity against cancer cells. In addition, tanshinones I and IIA and cryptotanshinone also inhibit tumor angiogenesis in endothelial and cancer cells [ , , , , ]. Moreover, tanshinone IIA is shown to exhibit anti-cancer activities through the interplay between autophagy and apoptosis in human prostate cancer PC-3 cells, mesothelioma H28 and H cells [ , ].
It inhibits epithelial—mesenchymal transition by modulating STAT3-chemokine C—C motif ligand 2 CCL2 pathway in human bladder cancer , BFTC and T24 cells [ ], and suppresses cell proliferation and migration via forkhead box protein M1 FoxM1 down-regulation in human gastric cancer SGC cells [ ].
On the other hand, tanshinone I induces apoptosis via Bcl-2 down-regulation in human gastric cancer BGC and SGC cells [ ], while cryptotanshinone induces apoptosis through mitochondrial-, cyclin- and caspase-dependent pathways in human NSCLC A and NCI-H cells [ ], as well as via ER stress in human hepatocellular carcinoma HepG2 and breast cancer MCF-7 cells [ ].
Tanshinone IIA is also shown to exhibit immunomdulatory effects in cancer [ ]. Furthermore, cryptotanshinone becomes a new promising anti-tumor immunotherapeutic agent [ ].
It induces mouse DC maturation and stimulates IL-1β, TNF-α, ILp70 secretion in DCs, and enhances T cell infiltration and Th1 polarization in Lewis-bearing tumor tissues [ ].
Tanshinone IIA has poor bioavailability, so a mixed micelle system is developed to form a tanshinone-encapsulated micelle [ ]. This micelle has higher cytotoxicity and pro-apoptotic effects in human hepatocellular carcinoma HepG2 cells compared to tanshinone IIA alone.
The tanshinone IIA-loaded nanoparticles improve the bioavailability tanshinone IIA and enhance its leukemic activity in human leukemia NB4 cells [ ], while the nanoparticles containing tanshinone IIA and α-mangostin show increased cytotoxicity in human prostate cancer PC-3 and DU cells [ ].
Tanshinone IIA is shown to enhance chemosensitivity and its efficacy when combined with other therapeutic agents. Tanshinone IIA can be an effective adjunctive agent in cancer, and it enhances the chemosensitivity to 5-fluorouracil therapy in human colorectal cancer HCT and COLO cells through NF-κB inhibition [ ].
The combination of tanshinone IIA with doxorubicin does not only enhance the chemosensitivity of doxorubicin, but also reduces the toxic side effects of doxorubicin in human breast cancer MCF-7 cells [ ]. In addition, tanshinone IIA and cryptotanshinone synergistically enhance apoptosis in human leukemia K cells [ ].
The anti-cancer effects of Tanshinone IIA have been demonstrated in various cancers in vitro and in vivo, and it can enhance chemosensitivity and its efficacy is very effective when combined with other therapeutic agents.
Up to now, the clinical trials of Tanshinone IIA are completed only for the treatment of other diseases [ ], so well-designed clinical trials should be done to further confirm its safety and efficacy in cancer treatment.
Oridonin Fig. Hara, which is also the main active constituent of Rabdosia rubescens Hemsl. Hara [ ]. As an orally available drug, oridonin is demonstrated to have anti-cancer activities in multiple cancers over the past decades, including leukemia, lymphoma, osteosarcoma, myeloma, uveal melanoma, neuroblastoma, hepatocellular, laryngeal, esophageal, and oral squamous cell carcinoma, lung, colorectal, breast, gastric, pancreatic, and prostatic cancers [ , , , , , , , , , , , , , , , ].
The anti-cancer effects of oridonin are shown in many aspects, including the induction of cell apoptosis, autophagy, cell cycle arrest, and the suppression of angiogenesis, cell migration, invasion and adhesion [ , , , , , , ]. Oridonin induces apoptosis in human hepatocellular carcinoma HepG2 and Huh6, oral squamous cell carcinoma WSU-HN4, WSU-HN6 and CAL27, and laryngeal cancer HEp-2 cells [ , , , ].
Oridonin is also shown to induce autophagy in many cancer cells, which is associated positively or negatively with apoptosis. It induces autophagy to mediate apoptosis in human NSCLC A and neuroblastoma SHSY-5Y cells [ , ]. On the other hand, autophagy provides a protective role against oridonin-induced apoptosis, as autophagy inhibitor enhances oridonin-induced apoptosis in human cervical carcinoma HeLa, multiple myeloma RPMI , laryngeal cancer HEp-2 and Tu, and epidermoid carcinoma A cells [ , , , ].
The anti-cancer effects of oridonin are also shown to be through suppressing angiogenesis and metastasis, which are the primary causes of tumor growth and metastasis. It can inhibit cell migration and invasion, and tube formation in human breast cancer 4T1 and MDA-MB, human and murine melanoma A and B16F10, osteosarcoma MG63 and B, and HUVECs, as well as tumor metastasis in HepG2 xenograft zebrafish and mice, 4T1 xenograft mice, and B xenograft mice [ , , , , ].
Proteomic and functional analyses reveal that ER stress and poly rC -binding protein 1 α-CP1 are potential pathways involved in the anti-proliferative and pro-apoptotic activities of oridonin [ ]. Besides, the mitochondrial redox change is proved to be a potential mediator for the pro-apoptosis effect of oridonin [ ].
Furthermore, the down-regulation of AP - 1 is reported to be the initial response to oridonin treatment, which decreases the expressions of NF-κB and MAPK to inhibit cell proliferation [ ]. Oridonin possesses an immunosuppressive effect which modulates microglia activation, enhances T cell proliferation, alters the balance of Th1-T helper type 2 cells Th2 , reduces inflammatory cytokine secretion such as IL-2, IL-4, IL-6, IL and TNF-α, and modulates an anti-inflammatory target, B lymphocyte stimulator [ ].
It also decreases inflammatory cytokine secretion in human pancreatic cancer BxPC-3 cells, including IL-1β, IL-6 and IL [ ]. The derivatives and analogs of oridonin usually exhibit more potent anti-cancer activities than oridonin. Oridonin phosphate, another derivative, is reported to induce autophagy, which can enhance apoptosis in human breast cancer MDA-MB cells [ ].
A novel analog of oridonin, CYD , inhibits tumor growth in bladder cancer UMUC3 xenograft mice and renal carcinoma O xenograft mice [ , ]. In addition, drug delivery system is also developed to improve the bioavailability of oridonin.
The inhalable oridonin-loaded microparticles exhibit strong pro-apoptotic and anti-angiogenic effects through mitochondrial-related pathways in NSCLC rats [ ], whilst the oridonin-loaded nanoparticles enhance cellular uptake and exert better anti-cancer effects in human hepatocellular carcinoma HepG2 cells [ ].
The combination of oridonin with other agents plays a potential role in cancer therapy. AG, a specific epidermal growth factor receptor EGFR inhibitor, augments oridonin-induced apoptosis through oxidative stress and mitochondrial pathways in human epidermoid carcinoma A cells [ ].
Moreover, oridonin can enhance the pro-apoptotic activity of NVP-BEZ in human neuroblastoma SHSY-5Y and SK-N-MC cells through autophagy [ ], whilst the combination of oridonin and cetuximab exhibits potent pro-apoptotic effect in human laryngeal cancer HEp-2 and Tu cells [ ].
Clinical trials are essential to test the safety and efficacy of oridonin before drug approval. A derivative of oridonin, HAO, is currently under a phase I clinical trial for the treatment of acute myelogenous leukemia in China [ ]. Shikonin Fig. It is effective in treating different kinds of cancers, including breast, prostate, ovarian and thyroid cancers, Ewing sarcoma, and myelomonocytic lymphoma [ , , , , , ].
Shikonin exerts anti-cancer effects mainly by inducing apoptosis, necroptosis, autophagy, cell cycle arrest, and by inhibiting cell proliferation, growth and metastasis [ , , ].
Shikonin is reported to inhibit cell growth by inducing cell cycle arrest and promoting apoptosis in human NSCLC A, gallbladder cancer NOZ and EHGB-1, esophageal cancer EC, and epidermoid carcinoma A cells [ , , , ].
It can also induce necroptosis via autophagy inhibition in human NSCLC A cells [ ], and through ROS overproduction in human nasopharyngeal carcinoma F, and glioma SHG, U87 and U cells [ , ]. Moreover, shikonin induces autophagy in human melanoma A, pancreatic cancer BxPC-3, and hepatocellular carcinoma Bel and Huh7 cells [ , , ].
However, autophagy provides a protective role in shikonin-induced apoptosis in human melanoma A cells [ ].
In addition, shikonin can suppress metastasis by the inhibition of tyrosine kinase c-Met and integrin ITG β1 in human NSCLC A cells [ , ]. There are multiple mechanisms involved in the anti-cancer effects of shikonin, including ER stress, ROS generation, glutathione GSH depletion, mitochondrial membrane potential disruption, p53, superoxide dismutase SOD and Bax up-regulation, PARP cleavage, catalase and Bcl-2 down-regulation [ , , , ].
ERK pathway also plays a role in shikonin-induced anti-cancer effects. Shikonin induces apoptosis and inhibits metastasis through suppressing ERK pathway in human NSCLC NCI-H and A cells, respectively [ , ].
Moreover, the activation of necroptosis initiators, receptor interacting serine-threonine protein kinase RIP 1 and RIP3, by shikonin does not only contribute to DNA double strand breaks via ROS overproduction [ ], but also facilitates glycolysis suppression via intracellular H 2 O 2 production [ ].
In addition, shikonin induces cell cycle arrest through p21 and p27 up-regulation, cyclin and CDK down-regulation [ ]. Therefore, numerous pathways involved in shikonin-induced anti-cancer effects may explain the broad range of its activities. Shikonin is also shown to modulate the function of the immune system.
It can also bind directly to heterogeneous nuclear ribonucleoprotein A1 to induce immunogenic cell death in human breast cancer MDA-MB cells [ ].
Shikonin is also reported to be used as an immunotherapy modifier in cell-based cancer vaccine systems, suggesting its potential application in cancer immunotherapy [ ]. Derivatives are developed to enhance the anti-cancer and tumor targeting effects of shikonin. The naphthazarin ring of shikonin is modified to produce DMAKO, which can specifically target cancer cells instead of normal cells [ ].
DMAKO can also suppress cell survival in human colorectal cancer HCT cells, and inhibits tumor growth in colorectal cancer CT xenograft mice [ ]. Besides, it inhibits cell proliferation and migration, and induces cell cycle arrest and apoptosis in murine melanoma B16F0 cells [ ]. Another novel shikonin derivative, cyclopropylacetylshikonin, exhibits strong anti-tumor and pro-apoptotic effects in human melanoma WM and MUG-MEL2 cells [ ].
In addition, drug delivery system is also developed to promote the intracellular delivery of shikonin. The shikonin-loaded nanogel enhances RIP1- and RIP3-dependent necroptosis in human osteosarcoma B cells [ ]. There is an increased accumulation of shikonin-loaded nanogel in the tumor tissue, and this nanogel can further inhibit tumor growth and metastasis in B xenograft mice.
Furthermore, the modified shikonin-loaded liposomes have higher cytotoxicity, and inhibit cell proliferation, metastasis in human breast cancer MDA-MB cells [ ].
The combination therapy is widely used to provide synergistic effects of anti-cancer activities. Shikonin can enhance the pro-apoptotic effect of taxol in human breast cancer MBA-MD cells, and this combination improves mice survival and inhibits tumor growth in MDA-MB xenograft mice [ ].
Besides, shikonin can also potentiate the anti-cancer effects of gemcitabine through NF-kB suppression and by regulating RIP1 and RIP3 expressions in human pancreatic cancer [ , ]. Shikonin is also reported to promote the efficacy of adriamycin in lung cancer and osteosarcoma [ , ], and enhance sensitization to cisplatin in colorectal cancer [ ].
Apart from the synergistic effect of shikonin, the combination of shikonin and paclitaxel reverses MDR in human ovarian cancer A cells [ 10 ]. The single or combined therapies with shikonin show promising anti-cancer effects in vitro and in vivo, so pre-clinical data has confirmed its therapeutic use in cancer treatment, as a result, clinical trials will be carried out to further to confirm its safety and efficacy in humans.
GA Fig. hanburyi and G. Morella [ ]. It has multiple biological activities such as anti-oxidative, anti-inflammatory, and anti-cancer activities [ , ]. Plenty of evidence shows that GA inhibits cell proliferation, invasion, survival, metastasis and chemo-resistance, and induces angiogenesis in many types of cancers such as gastric and prostate cancers, leukemia, multiple myeloma, osteosarcoma, and renal carcinoma through multiple signaling mechanisms [ , , , , , , ].
Many studies have reported the anti-cancer effects of GA in human breast cancer [ , , , ]. GA at low concentrations 0. GA also induces apoptosis via ROS production in human bladder T24 and UMUC3 cells [ ].
At earlier time points, GA induces ROS-mediated autophagy, which produces a strong cell survival response. However, at later time points, caspases are activated which degrade autophagic proteins and cell survival proteins, and this eventually induces apoptosis.
Similarly, GA-induced autophagy via ROS provides a cytoprotective effect to human pancreatic cancer Panc-1 and BxPC-3 cells [ ], and ROS scavenger, N-acetylcysteine, can reverse GA-induced autophagy in human NSCLC NCI-H cells [ ].
Moreover, GA inhibits cell invasion and migration through reversion-inducing-cysteine-rich protein with kazal motifs RECK up-regulation in human NSCLC A cells and A xenograft mice [ ], and prevents TNF-α-induced invasion in human prostate cancer PC-3 cells [ ].
It also inhibits angiogenesis in HUVECs, and prevents tumor growth through the inhibition of tumor angiogenesis [ ]. ROS-related pathways play a vital role in GA-induced cell death [ , , , , , , , ]. GA induces apoptosis mainly through ROS accumulation in human pancreatic cancer Panc-1 and BxPC-3, NSCLC NCI-H, castration-resistant prostate cancer PCAP-1, melanoma A, breast cancer MCF-7 cells [ , , , , ].
It also induces oxidative stress-dependent caspase activation to mediate apoptosis in human bladder cancer T24 and UMUC3 cells [ ]. Moreover, GA increases the expressions of ER stress markers such as GRP78, CHOP, activating transcription factor 6 ATF-6 and caspase, and co-treatment with chemical chaperone, 4-PBA, significantly reduces these expressions and apoptosis in human NSCLC A cells, so it is suggested that GA induces ER stress to mediate apoptosis [ ].
Previous studies have shown some immunomodulatory activities of GA [ , ]. The activation of TLRs is important to initiate immune responses, and TLR4 forms a complex with myeloid differentiation factor 2 MD2 to recognize its ligand, like LPS.
Similarly, it also reduces pro-inflammatory cytokine production including TNF-α, IL-1β and IL-6 by suppressing p38 pathway in murine macrophage RAW GA has low solubility, instability and poor pharmacokinetic properties [ ].
In order to increase its water solubility, GA is conjugated with a cell-penetrating peptide, trans-activator of transcription, to form GA-TAT [ ].
This GA-TAT enhances apoptosis through ROS accumulation in human bladder cancer EJ cells. Another study uses a co-polymer to encapsulate GA to form GA micelles [ ].
These GA micelles have better cellular uptake which can further enhance apoptosis in human breast cancer MCF-7 cells and the anti-tumor effects in MCF-7 xenograft mice.
Moreover, GA is encapsulated into the core of the nanoparticles to enhance the stability of GA and its circulation time [ ]. These nanoparticles have tumor targeting properties, and enhance the anti-tumor activities of GA without inducing higher toxicity.
The combination of GA and other chemotherapy agents has been widely used to improve the therapeutic effects against various cancers such as osteosarcoma, pancreatic and lung cancers [ , , , ]. Moreover, GA and retinoic acid chlorochalcone are loaded into glycol chitosan nanoparticles to form RGNP [ ].
The RGNP exhibits synergistic effects to inhibit cell proliferation and induces apoptosis in osteosarcoma.
The combination of GA with doxorubicin synergistically reduces cell viability in human ovarian cancer platinum-resistance SKOV3 cells, and this combination also suppresses tumor growth in SKOV3 xenograft mice [ ]. The safety and efficacy of GA at different dosages in patients with advanced malignant tumors have been compared in a phase IIa clinical trial [ ].
The patients with GA administration on days 1—5 in a 2-week cycle showed a greater disease control rate and only Grades I and II adverse reactions. To further investigate the safety and efficacy of GA, a phase IIb clinical trial involving a larger sample size of patients would be needed.
Artesunate Fig. As an analog of ART, artesunate exerts better water solubility and higher oral bioavailability, due to its special structure with an additional hemisuccinate group that makes it a better candidate for cancer treatment [ ].
The anti-cancer effects of artesunate have been demonstrated in bladder, breast, cervical, colorectal, esophageal, gastric, ovarian and prostate cancer, renal carcinoma, leukemia, melanoma and multiple myeloma [ , , , , , , , , , , , ].
Its anti-cancer effects include induction of cell cycle arrest and apoptosis, inhibition of cell proliferation and growth, metastasis and angiogenesis [ , , ]. Artesunate can induce apoptosis in various cancers including human breast cancer MCF-7, MDA-MB and SKBR3 cells, gastric cancer SGC and HGC, colorectal cancer HCT, and esophageal cancer Eca and Ec cells [ , , , , , ].
Artesunate is also shown to induce autophagy to exert cytoprotective effects in human colorectal cancer HCT cells, and the inhibition of autophagy enhances artesunate-mediated apoptosis [ ].
Similarly, artesunate-induced mitophagy provides a protective effects against cell death in human cervical cancer HeLa cells [ ]. Moreover, it inhibits cell invasion and migration in human prostate cancer DU and LNCaP, cervical cancer Caski and HeLa cells, and uveal melanoma cells [ , , ], and suppresses tumor angiogenesis in HUVECs and renal carcinoma O xenograft mice [ , ].
In most cases, the inhibition effects of artesunate against cancer cells are resulted from apoptosis. Artesunate induces apoptosis through cyclooxygenase-2 COX-2 down-regulation in human bladder cancer T24 and RT4, and gastric cancer HGC cells [ , ].
Mitochondrial pathways also play an important role in artesunate-mediated anti-cancer effects [ , , ]. Artesunate inhibits tumor growth through ROS- and p38 MAPK-mediated apoptosis in human rhabdomyosarcoma TE cells [ ].
It also exerts anti-tumor activities through the loss of mitochondrial membrane potential, Bcl-2 down-regulation, Bax up-regulation, and caspase-3 activation in human gastric cancer SGC and HGC, esophageal cancer Eca and Ec cells, and breast cancer MCF-7 xenograft mice [ , , ].
In addition, gene expression analysis identifies that ER stress is the most relevant pathway for the anti-tumor activity of artesunate in B-cell lymphoma [ ]. Interestingly, artesunate selectively inhibits cell growth through iron-dependent and ROS-mediated ferroptosis in human head and neck cancer HN9 cells [ ].
Immunomodulation also plays a vital role in artesunate-mediated anti-cancer effects [ , , , ]. It also exerts anti-tumor effects through suppressing NK killing activity and lymphocyte proliferation, which results in decreased TGF-β1 and IL levels in colorectal cancer Colon and RKO cells [ ].
Besides, artesunate also exerts immunosuppression through forkhead box P3 Foxp3 down-regulation in T cells and decreases prostaglandin E 2 PGE 2 production in human cervical cancer Caski and HeLa cells [ ].
You can also search for this author in PubMed Google Scholar. Reprints and permissions. dePeyer, O.
Herbal extracts help fight cancer. Nature Download citation. Published : 25 August Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Skip to main content Thank you for visiting nature. nature news article. Access through your institution. Buy or subscribe. Change institution. Learn more. References Patel, N. Article CAS Google Scholar Download references. Authors Oliver dePeyer View author publications.
Rights and permissions Reprints and permissions. About this article Cite this article dePeyer, O.
Herbs and spices can do so Macro-nutrient balance for athletes more extrcats enhance the flavor of food. Cancer-foghting can help stimulate Cancer-fighting effects of herbal extracts immune system and effecfs prevent cancer. Here are six ways to spice up your food and keep you in good health. It is also an anti-inflammatory. Tip: Mix with black pepper piperine and olive oil to activate and help with absorption. It can be used as a dry rub or added to soups, sauces and stews. Calling Wffects number o Cancer-fighting effects of herbal extracts efvects a Patient Advocate at The Mesothelioma Center, the Cancer-fifhting most trusted mesothelioma Cancee-fighting. Our Patient Advocates can help guide you or Personal weight loss loved one through the steps to take after a mesothelioma diagnosis. Our team has a combined experience of more than 30 years in assisting cancer patients, and includes a medical doctor, an oncology registered nurse and a U. For example, some herbs can prevent chemotherapy and radiation therapy from killing cancer cells. Certain herbs enhance the effect of chemotherapy in a toxic way that leads to unwanted side effects.
Mir scheint es die prächtige Phrase
Ich hörte darüber nichts noch
Es gibt etwas ähnlich?
Es hat den Sinn nicht.
Sie sind nicht recht. Schreiben Sie mir in PM.