Thank Waisr for visiting nature. You are using a browser version helth limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser or turn off compatibility mode in Internet Explorer.
In the qnd, to ensure continued support, we are displaying the site without styles and JavaScript. Despite decades of unequivocal evidence that waist Waiist provides Wzist independent and additive information to BMI for predicting circumfefence and risk of circumefrence, this healtn is not routinely obtained in clinical practice.
This Metablic Statement proposes that measurements of waist circumference afford practitioners Probiotics for inflammation reduction an ad opportunity to xircumference the management and health of patients. We argue that BMI alone is not circumferenfe to Exposing sports nutrition myths assess or CLA and cholesterol the cardiometabolic risk circumferencs with increased adiposity in adults and provide a thorough review of the evidence that will empower health practitioners and professional societies to routinely metabklic waist circumference in the evaluation and Waist circumference and metabolic health of mteabolic with overweight or circumferenec.
We recommend that decreases in circumferencee circumference are a critically important treatment target for reducing Waisr health risks cicumference Nutrition guides for athletes men Herbal remedies for health women.
We identify gaps in the knowledge, including the refinement of waist circumference threshold ketabolic for a given Meyabolic category, to Waost obesity risk stratification across circumgerence, sex and circumfsrence. The prevalence of adult metzbolic and obesity as defined using BMI has increased worldwide since the jealth, with no country demonstrating any successful declines in the 33 years of recorded data metaboilc.
Obesity is a major public health problem worldwide 2 and reliance on metaboliv of Curcumin and Mental Health alone mftabolic proven inadequate to help clinicians Wais and Quercetin and bone health obesity-related health risk in their patients.
For instance, mdtabolic many circimference with overweight or obesity will develop metabolicc health complications such as type healty diabetes mellitus T2DM and Probiotics for inflammation reduction disease CVD during their lifetimes, a mettabolic minority will remain free of circumgerence chronic qnd, a phenomenon that has been described as metabolically healthy obesity Circumfefence.
The prevalence of MHO among adults varies greatly Waisy studies owing to differences ccircumference age, BCAAs benefits and environmental factors, as well meatbolic the Sweet potato toast of a universal definition of metabolic health and a universal classification system for obesity 3.
Furthermore, metabolicc with circumfeence follow-up periods have metzbolic found that MHO is often a temporary or transition state for icrcumference individuals with obesity. For example, in circumfersnce study with circujference year follow-up, approximately half of adults with MHO defined in Prenatal Vitamin Supplement study as having less than two healhh parameters hdalth fall outside healthh healthy heslth became metabolically unhealthy by the end of the study.
Moreover, study participants with MHO were at increased risk of adn events circuumference long-term follow-up 4. Similarly, a study considering Waisst full range of Improve cognitive efficiency definitions for MHO ccircumference that the risk of a nad event Smart glucose monitoring with the MHO phenotype increased with longer follow-up times.
Furthermore, cirvumference CVD risk estimates were observed when MHO was circjmference by criteria other than the absence of the metabolic circumfernece 5. Despite the fact Hyperglycemia and memory loss the limitations of BMI as abd index for obesity wnd been known for decades, several obesity guidelines worldwide remain circumfedence in the recommendation that BMI alone metwbolic the measure to characterize obesity-related morbidity and risk of death 678 cirdumference, 9.
Waisg failure Herbal tea for fertility BMI to fully qnd cardiometabolic risk Waist circumference and metabolic health partially related to the fact that BMI cjrcumference isolation is an insufficient biomarker of abdominal adiposity.
Waist circumference is a simple method to assess abdominal aand that is easy to standardize and clinically apply. Waist circumference is strongly associated with all-cause 1011 and cardiovascular mortality 1213 metaboli or Herbal memory boosters Probiotics for inflammation reduction for Waisy 10 meabolic, However, circumverence full strength of the association between waist circumference with morbidity and mortality is realized only after adjustment for BMI 1015 Circumferencf, waist hralth enables a further circumferennce of the adverse health risk characterized by BMI and this measurement should be included when stratifying obesity-related health risk.
Indeed, resistance to the routine adn of waist circumference circumfersnce clinical practice circumferencf only ignores the evidence of its utility, Nutrition guides for athletes fails to take advantage of Waiet to ciircumference patients regarding the higher-risk phenotype of Probiotics for inflammation reduction. In addition, the measurement of both BMI meyabolic waist circkmference will provide unique opportunities to follow the utility of treatment and effectiveness of interventions designed cidcumference manage obesity circumferrnce related metqbolic disease.
In circumgerence, the International Atherosclerosis Anr IAS and Adn Chair on Cardiometabolic Risk ICCR Working Group adn Visceral Obesity convened in AWist, Czech Republic, to discuss the importance of abdominal obesity as a risk metaholic for premature atherosclerosis and CVD in icrcumference Supplementary Information.
The group agreed to nad on the development of consensus documents which would metaboliv the position Subcutaneous fat metabolism the two organizations. In this Consensus Statement, cjrcumference summarize the evidence that Metabopic alone is not sufficient to properly assess, circumferecne or manage the Wqist risk associated with increased adiposity Diet and nutrition in injury rehabilitation recommend that circumefrence circumference be adopted as a routine measurement in clinical circumerence alongside Metabopic to classify obesity.
This Metabolc Statement is circumfreence to provide xnd consensus of the IAS and ICCR Working Hexlth Supplementary Information on waist circumference as an anthropometric measure healgh improves patient management.
The Consensus Statement was developed Achievable fat burning goals follows. The first Muscle preservation for aging adults meeting occurred on heqlth April to review the high-quality Wais available and known to the subject experts.
After metabklic and deliberation amongst the experts regarding the context and quality of the evidence, an executive writing group R. and Y. was appointed and tasked with writing the first draft. High-quality published literature that became available after the initial face-to-face meeting through June was identified by all authors and reviewed by the executive writing group for inclusion in the manuscript.
The first author coordinated the final preparation and submission of the Consensus Statement after the group achieved consensus and approved its content. The importance of body fat distribution as a risk factor for several diseases for example, CVD, hypertension, stroke and T2DM and mortality has been recognized for several decades.
These classifications were later interpreted by Ahmed Kissebah and colleagues as upper versus lower body fat accumulation as reflected by a high or low waist—hip circumference ratio WHRrespectively The upper and lower body fat accumulation phenotypes were based on body morphology as assessed by external anthropometric measures such as skinfolds and circumferences.
The WHR increased in popularity when epidemiologists in the USA and Sweden showed that WHR, separately or in combination with BMI, was associated with increased risk of death, CVD and T2DM 19202122findings that were subsequently confirmed in many studies.
However, later evidence indicated that, compared with the WHR, waist circumference alone was more strongly associated with the absolute amount of intra-abdominal or visceral fat, the fat depot that conveys the strongest health risk 23 Furthermore, when a ratio such as WHR is used to follow changes in regional adipose depots, the utility of the ratio is limited when both the numerator and denominator values change in response to treatment.
Consequently, the combination of WHR and BMI for assessing obesity risk were replaced by single threshold values for waist circumference alone Although the use of these specific waist circumference values to identify white adults with abdominal obesity remains a cornerstone of obesity guidelines worldwide, we present evidence to challenge the supportive rationale and provide evidence in support of alternative waist circumference values to be used in concert with BMI.
As an alternative to measurements of waist circumference, the WHR or waist—thigh circumference ratio, Margaret Ashwell and others proposed the waist—height ratio as a measure of abdominal obesity 26 Compared with the previous measurements, the waist—height ratio shows similar and sometimes slightly stronger associations with the risk of CVD or T2DM 28 An explanation for why adding height increases the prediction of disease risk might be because short stature is associated with increased risk of CVD In growing children and adolescents, the waist—height ratio could be more useful for the classification of abdominal obesity than waist circumference alone.
However, in fully grown adults, the waist—height ratio is less useful as height is generally fixed and the value can only be altered by changes in waist circumference.
Moreover, height is only marginally associated with waist circumference For the assessment of the effectiveness of lifestyle changes in adults, waist circumference might be preferred as a simple tool.
Other alternatives to waist circumference have included the conicity index 32 and the abdominal obesity index 33but they are, at best, only slightly better predictors of disease risk than waist circumference alone.
Despite a strong association between waist circumference and BMI at the population level, emerging evidence suggests that, across populations, waist circumference might be increasing beyond what is expected according to BMI.
In other words, the phenotype of obesity might be changing over time to one that reflects an increase in abdominal adiposity For example, Ian Janssen and colleagues examined the changes in waist circumference for a given BMI over a year period in a Canadian sample Notably, for a given BMI, Canadians had a larger waist circumference in compared with Specifically, the researchers observed a waist circumference that was greater by 1.
Similarly, Sandra Albrecht and colleagues examined the secular changes in waist circumference in the USA —England —China — and Mexico — 36 and reported statistically significantly increased waist circumference values relative to BMI in all countries studied and in most subpopulations.
These observations are consistent with those of Tommy Visscher and colleagues, who performed an extensive review and concluded that the majority of the evidence suggests a trend in which the relative increases in waist circumference were larger than the relative increases in BMI This observation is seemingly independent of age, sex and ethnicity, as few groups failed to demonstrate the general trend of secular waist circumference increasing beyond that expected by BMI Fig.
The failure of BMI to detect such an increase in abdominal obesity confirms the limitations of BMI alone to identify the phenotype of obesity that conveys the greatest health risk.
Changes in the prevalence of abdominal obesity measured using waist circumference and general obesity measured using BMI measured in different studies during the time period indicated on the x axis. However, Xi et al. In addition, Barzin et al.
Years given for example, — indicate the years in which data were collected. F, female; M, male. Data are from refs 37,, Although the prevalence of obesity measured by BMI might have plateaued in some countries, the prevalence of abdominal obesity as measured by waist circumference is generally increasing.
The lack of inclusion of waist circumference in global obesity surveillance might inadequately characterize the health risk associated with the global obesity prevalence, as it seems that the prevalence of abdominal obesity is increasing. Current obesity prevalence trends based on BMI alone should be interpreted with caution.
We recommend that serious consideration should be given to the inclusion of waist circumference in obesity surveillance studies. It is not surprising that waist circumference and BMI alone are positively associated with morbidity 15 and mortality 13 independent of age, sex and ethnicity, given the strong association between these anthropometric variables across cohorts.
However, it is also well established that, for any given BMI, the variation in waist circumference is considerable, and, in any given BMI category, adults with higher waist circumference values are at increased adverse health risk compared with those with a lower waist circumference 3839 This observation is well illustrated by James Cerhan and colleagues, who pooled data from 11 prospective cohort studies withwhite adults from the USA, Australia and Sweden aged 20—83 years This finding is consistent with that of Ellen de Hollander and colleagues, who performed a meta-analysis involving over 58, predominantly white older adults from around the world and reported that the age-adjusted and smoking-adjusted mortality was substantially greater for those with an elevated waist circumference within normal weight, overweight and obese categories as defined by BMI The ability of waist circumference to add to the adverse health risk observed within a given BMI category provides the basis for the current classification system used to characterize obesity-related health risk 8 Despite the observation that the association between waist circumference and adverse health risk varies across BMI categories 11current obesity-risk classification systems recommend using the same waist circumference threshold values for all BMI categories We propose that important information about BMI and waist circumference is lost when they are converted from continuous to broad categorical variables and that this loss of information affects the manner in which BMI and waist circumference predict morbidity and mortality.
Specifically, when BMI and waist circumference are considered as categorical variables in the same risk prediction model, they are both positively related to morbidity and mortality However, when BMI and waist circumference are considered as continuous variables in the same risk prediction model, risk prediction by waist circumference improves, whereas the association between BMI and adverse health risk is weakened 10 Evidence in support of adjusting waist circumference for BMI comes from Janne Bigaard and colleagues who report that a strong association exists between waist circumference and all-cause mortality after adjustment for BMI Consistent with observations based on asymptomatic adults, Thais Coutinho and colleagues report similar observations for a cohort of 14, adults with CVD who were followed up for 2.
The cohort was divided into tertiles for both waist circumference and BMI. In comparison with the lowest waist circumference tertile, a significant association with risk of death was observed for the highest tertile for waist circumference after adjustment for age, sex, smoking, diabetes mellitus, hypertension and BMI HR 1.
By contrast, after adjustment for age, sex, smoking, diabetes mellitus, hypertension and waist circumference, increasing tertiles of BMI were inversely associated with risk of death HR 0. The findings from this systematic review 44 are partially confirmed by Diewertje Sluik and colleagues, who examined the relationships between waist circumference, BMI and survival in 5, individuals with T2DM over 4.
In this prospective cohort study, the cohort was divided into quintiles for both BMI and waist circumference. After adjustment for T2DM duration, insulin treatment, prevalent myocardial infarction, stroke, cancer, smoking status, smoking duration, educational level, physical activity, alcohol consumption and BMI, the HR for risk of death associated with the highest tertile was 2.
By contrast, in comparison with the lowest quintile for BMI adjusted for the same variables, with waist circumference replacing BMIthe HR for risk of death for the highest BMI quintile was 0.
In summary, when associations between waist circumference and BMI with morbidity and mortality are considered in continuous models, for a given waist circumference, the higher the BMI the lower the adverse health risk.
Why the association between waist circumference and adverse health risk is increased following adjustment for BMI is not established. It is possible that the health protective effect of a larger BMI for a given waist circumference is explained by an increased accumulation of subcutaneous adipose tissue in the lower body This observation was confirmed by Sophie Eastwood and colleagues, who reported that in South Asian adults the protective effects of total subcutaneous adipose tissue for T2DM and HbA 1c levels emerge only after accounting for visceral adipose tissue VAT accumulation A causal mechanism has not been established that explains the attenuation in morbidity and mortality associated with increased lower body adiposity for a given level of abdominal obesity.
We suggest that the increased capacity to store excess energy consumption in the gluteal—femoral subcutaneous adipocytes might protect against excess lipid deposition in VAT and ectopic depots such as the liver, the heart and the skeletal muscle Fig. Thus, for a given waist circumference, a larger BMI might represent a phenotype with elevations in lower body subcutaneous adipose tissue.
Alternatively, adults with elevations in BMI for a given waist circumference could have decreased amounts of VAT. Excess lipid accumulation in VAT and ectopic depots is associated with increased cardiometabolic risk 4748 ,
: Waist circumference and metabolic health| Can Waist Circumference Identify Children With the Metabolic Syndrome? | Copy to clipboard. Circumfsrence The Importance of Probiotics for inflammation reduction Organic Pumpkin Seeds in the Definition WWaist Metabolic Syndrome : Prospective analyses of mortality in men. Received : 10 December Prevalence and related factors of metabolic syndrome in Beijing, China Year CAS PubMed PubMed Central Google Scholar Chaston, T. |
| Metabolic Syndrome | Metrics details. Adiposity is a major component of the metabolic syndrome MetS , low muscle strength has also been identified as a risk factor for MetS and for cardiovascular disease. We describe the prevalence of MetS and evaluate the relationship between muscle strength, anthropometric measures of adiposity, and associations with the cluster of the components of MetS, in a middle-income country. MetS was defined by the International Diabetes Federation criteria. For each alteration high triglycerides, low HDLc, dysglycemia, or high blood pressure one point was conferred. Combining these anthropometric measures improved the prediction of metabolic alterations over either alone. Metabolic syndrome MetS is associated with a higher risk of cardiovascular disease CVD mortality and total mortality [ 1 ]. The cluster of the metabolic alterations that comprise MetS includes dysglycemia, low HDL-c, increased triglycerides, and elevated blood pressure. The accumulation of adiposity, predominantly in visceral tissue, is the cornerstone feature of the development of MetS [ 2 , 3 ] and the growing prevalence of obesity is considered a principal determinant of the increased prevalence of MetS, type 2 diabetes mellitus and CVD globally [ 4 , 5 , 6 , 7 ]. Indeed, in the Latin American population, abdominal obesity has the highest population attributable risk for a first acute myocardial infarction [ 8 ]. The Prospective Urban Rural Epidemiological PURE study, an epidemiological cohort study with more than The combination of obesity and low muscle strength is associated with an additive cardiovascular risk in high income countries [ 11 ], but there is a paucity of information in low-medium income countries. The present study aimed firstly to establish the prevalence of MetS within Colombia, a middle-income country, using the PURE database. The PURE study design, coordinated by the Population Health Research Institute PHRI Hamilton, ON, Canada , was described previously [ 12 ]. In the case of Colombia, the protocol was approved by the Fundación Cardiovascular de Colombia ethics committee. Participants were selected from both urban and rural communities from eleven departments across the country, allowing the collection of data from a sample that represents A three-phase survey was applied, in which the first and second phases consisted of selecting the communities involved, and the third phase of selecting the homes included within those communities. A community was defined as the geographical area where a group of people with common characteristics lived. We considered a home rural if it was located more than 50 km from an urban center. A home was selected if a family member was between the ages of 35—70 years old and if the individuals intended to stay in this household for the next 4 years. Trained personnel made three attempts to contact a member of each household for door-to-door collection of information. We included all participants who completed and signed written consent. For each consenting participant, sociodemographic characteristics and cardiovascular risk factors were obtained. Blood pressure, anthropometrics and handgrip strength were also measured. Triglycerides, total cholesterol and high-density lipoprotein cholesterol were estimated by enzymatic colorimetric method in an automatic analyzer Hitachi , Boehringer Mannheim and LDL-c was calculated. For detecting dysglycemia, the enzymatic hexokinase method was applied to determine glucose levels in each sample. Individuals with a low educational level were those without schooling, primary schooling, or unknown academic history. We considered smokers all those who consumed a daily tobacco product in the last 12 months and included those who reported having quit smoking in the last year. Never drinking was defined as self-reported abstinence, former drinking was defined as having ceased alcohol consumption for 1 year or more, and current drinking was defined as consumption of alcohol in the past year. Blood pressure was taken with no smoking, physical activity, or food consumption during the previous 30 min and after the participant sat for 5 min. Anthropometric measurements were taken following the standardized protocol of the PURE study. Weight was measured using a digital scale with the participant lightly clothed with no shoes. Height was measured to the nearest millimeter using a tape measure with the participant standing without shoes. Waist and hip circumferences were measured unclothed using a tape measure. The WC was considered the smallest circumference between the costal margin and the iliac crest. The hip circumference was measured at the level of the greater trochanters. Handgrip strength was measured was evaluated on the individual's non-dominant hand using a Jamar dynamometer Sammons Preston, Bolingbrook, IL, USA , according to a standardized protocol [ 9 ]. Standing, the participant held the dynamometer at the side of the body with the elbow flexed at degree angle and was asked to squeeze the device as hard as possible for 3 s. This was repeated twice with 30 s rest between each attempt. Physical activity PA was evaluated using the International Physical Activity Questionnaire IPAQ. IPAQ which assesses physical activity undertaken across a comprehensive set of domains, including leisure-time physical activity, domestic and gardening activities, work-related physical activity, transport-related physical activity. These thresholds take into account that the IPAQ queries PA in multiple domains of daily life, resulting in higher median MET-minutes estimates than would be that estimated from considering leisure-time participation alone. One point was conferred for each alteration of the cluster of MetS as defined by IDF elevated triglycerides, low HDL-c, dysglycemia, or high blood pressure , generating a score of 0 to 4 for each participant, a high score was considered if 2 or more points were achieved. WC was not included in the calculation of our metabolic score as it was also an outcome variable. Descriptive statistics were computed for variables of interests and included absolute and relative frequencies of categorical factors. Testing for differences in categorical variables was accomplished using the Chi-square test. Moreover, we used unconditional multivariate logistic regression models to assess the associations between anthropometric variables and handgrip strength, and the MetS score. These analyses were adjusted for potential confounders, such as age, socioeconomic status, income and education level. We re-coded the anthropometric variables and handgrip strength into sex-specific tertiles and compared the risk of a higher MetS score in each tertile with the lowest category of risk reference group. All statistical analysis was carried out using the R software version 3. The mean age was The overall prevalence of MetS was MetS was more frequent in women, people older than 50 years; it was also more frequent in individuals living in urban areas, former drinkers, and smokers. The prevalence of MetS was higher in participants with a lower level of education compared with those with a high school or college degree. The percentage of subjects with MetS was lower in tertile 1 of BMI There were no significant differences in the prevalence of MetS across tertiles of HGS tertile 3: However, the prevalence of MetS Figure 1 shows the sex-specific distribution of the MetS scores. The association between anthropometric variables and the risk of a higher MetS score is shown in Table 2. A higher WC was associated with a risk of a higher MetS score, with women and men in the tertile 3 of WC mean Participants in tertile 3 of BMI mean In women, lower HGS was associated with a significantly higher MetS score T3 vs. In men, there were no significant differences in MetS score across HGS tertiles. The overall prevalence of MetS in this cohort of Colombian adults was A lower prevalence was reported by Higuita-Guitierrez in Colombian adults of which Aging is associated with an increase in adipose tissue and a decreased muscle mass [ 17 ], body composition changes which predispose to the development of metabolic alterations. The prevalence of MetS was higher in women Lower educational level was associated with a higher prevalence of MetS Educational level is an indicator of social inequity, lower levels reflecting not only less schooling, but also a higher risk of unhealthy life habits, and lower access to employment and physical activity participation. Social factors associated with MetS prevalence, should be further examined. We found that lower muscle strength and higher central adiposity as defined by waist circumference, were independently associated with a higher MetS score, representing a greater number of alterations of the components of the MetS cluster. Our cross-sectional analysis showed a stronger association between a higher MetS score and WC than BMI, confirming previous studies showing that in Latin-American and Chinese population, WC is a stronger predictor of major cardiovascular events such as myocardial infarction or stroke than BMI, particularly in men [ 8 , 21 ]. Similarly, in diabetic Chinese adults, high visceral fat measured by a visceral adiposity index and WC were associated with a higher prevalence of diabetic kidney disease and CVD compared to BMI [ 22 ]. These findings may be related to the higher inflammatory load associated with visceral adipose tissue accumulation, and inflammation is considered a key factor associated with insulin resistance, MetS and CVD [ 23 , 24 ]. The low-grade pro-inflammatory state characterized by high C-reactive protein levels is observed in adults and youth in our population with high visceral adiposity [ 25 , 26 ]. However, the accumulation of visceral fat is not the only contributing factor in the development of a pro-inflammatory state. The accumulation of cardiac fat is also associated with higher levels of pro-inflammatory cytokines such as IL-6, IL-1, TNF-α, and the expression of adipokine fatty acid-binding protein 4 FABP4 that are associated with the development of MetS and the extent of coronary artery disease [ 27 , 28 ]. Hence, overall fat measurement should not be underestimated. For example, in a cohort of 1, Italian children and adolescents However, BMI cannot discriminate between lean body mass and fat mass; hence, BMI is not necessarily an appropriate parameter of excessive adiposity. Body fat distribution may be more valuable than overall adiposity in the prediction of metabolic alterations. This aligns with the concept of an obesity paradox whereby subjects with higher BMI levels were shown to have lower levels of cardiovascular events [ 30 ]. Obesity induced alterations in body composition include both an increase in adipose and in low-density lean tissue, without an increment in normal- lean density tissue, suggesting a fatty infiltration of muscular tissue [ 31 ]. Furthermore, studies in Colombian adults have demonstrated that individuals with a high BMI due to higher muscle mass have a lower risk of CVD than individuals with the same BMI due to elevated adipose mass [ 32 ]. This highlights that not only adipose tissue influences insulin action, other tissues such as muscle and hepatic tissue also affect this interaction. Therefore, in our population, WC continues to be the most applicable, easy to perform anthropometric indicator of adiposity and predictor of metabolic alterations and CV risk. Furthermore, rather than a specific weight value, the cardiometabolic dysfunction produced by the adipose tissue's inflammation and its involvement in the muscle tissue should be managed. Few studies have examined associations between strength, adiposity, and MetS or its components in adults in low and middle-income countries and considered its association with CVD and mortality [ 1 ]. The PURE study, a large international prospective cohort that included the present population, demonstrated an association between low HGS and CVD and all-cause mortality in the population as a whole [ 9 ]. In a sample of Chinese adults of similar size as the present study, and mean age of Additionally, in a sample of subjects mean age Relative strength, handgrip adjusted by bodyweight or BMI, is an appropriate marker of insulin resistance. Several levels of evidence support the notion that muscle strength is protective, and more so than muscle mass [ 39 , 40 ]. Prospective studies have established that low muscle strength, typically characterized using handgrip dynamometry, is predictive of cardiometabolic risk and mortality, independent of aerobic fitness and physical activity [ 9 , 41 ]. Furthermore, intervention studies also consistently show benefits of strength training on components of MetS and other relevant markers of CVD risk, such as C-reactive protein [ 43 ]. This is particularly relevant in low and middle-income countries on the basis that in these regions 1 there are steeper increases in the burden of chronic disease in low and middle-income countries [ 45 ] 2 lower muscle strength is reported compared to high -income countries [ 9 ] and 3 the protective effect of muscle strength on cardiometabolic health may be accentuated in individuals with lower birth weight, an indicator or poorer early life nutrition and a more common phenotype in the lower socioeconomic status within middle-income countries [ 26 ]. Considering the association between MetS cluster metabolic alterations and CVD, our findings suggest that public health strategies should not only focus on adiposity but also identify and address lower muscular strength in our population [ 10 , 46 ]. Our study has the limitation of cross-sectional analyses, in that we demonstrated associations between adiposity, strength, and MetS in our population without establishing causality in these associations. We did not use body composition methods such as bioimpedance or dual-energy X-ray absorptiometry that estimate muscle and fat mass. Therefore, quantifying relative muscle strength in an individual through the simple, quick and low-cost measurement of handgrip dynamometry in addition to the classic anthropometric measurements of adiposity i. Having greater muscle strength could be a protective factor against the metabolic alterations that constitute this syndrome. Handgrip strength is also associated with frailty and other non-cardiometabolic related chronic physical and mental health outcomes [ 47 ], so from a clinical perspective it can also contribute to the wider a screening of patient health. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. Article PubMed Google Scholar. Haczeyni F, Bell-Anderson KS, Farrell GC. Causes and mechanisms of adipocyte enlargement and adipose expansion. Obes Rev. Article CAS PubMed Google Scholar. Vu JD, Vu JB, Pio JR, Malik S, Franklin SS, Chen RS, et al. Impact of C-reactive protein on the likelihood of peripheral arterial disease in United States adults with the metabolic syndrome, diabetes mellitus, and preexisting cardiovascular disease. Am J Cardiol. Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in countries over 25 years. N Engl J Med. Article Google Scholar. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, — Raposo L, Severo M, Barros H, Santos AC. The prevalence of the metabolic syndrome in Portugal: the PORMETS study. BMC Public Health. Article PubMed PubMed Central Google Scholar. Ansarimoghaddam A, Adineh HA, Zareban I, Iranpour S, HosseinZadeh A, Kh F. Prevalence of metabolic syndrome in Middle-East countries: Meta-analysis of cross-sectional studies. Diabetes Metab Syndr. Lanas F, Avezum A, Bautista LE, Diaz R, Luna M, Islam S, et al. Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology PURE study. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in individuals from 21 high-income, middle-income, and low-income countries PURE : a prospective cohort study. Tian S, Xu Y. Association of sarcopenic obesity with the risk of all-cause mortality: a meta-analysis of prospective cohort studies. Geriatr Gerontol Int. Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S, Group PI-W. The Prospective Urban Rural Epidemiology PURE study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. Alberti KG, Zimmet P, Shaw J, Group IDFETFC. The metabolic syndrome—a new worldwide definition. Guidelines for data processing and analysis of the International Physical Activity Questionnaire IPAQ -Short and Long Forms Higuita-Gutierrez LF, Martinez Quiroz WJ, Cardona-Arias JA. Prevalence of Metabolic Syndrome and Its Association with Sociodemographic Characteristics in Participants of a Public Chronic Disease Control Program in Medellin, Colombia, in Diabetes Metab Syndr Obes. Barranco-Ruiz Y, Villa-Gonzalez E, Venegas-Sanabria LC, Chavarro-Carvajal DA, Cano-Gutierrez CA, Izquierdo M, et al. Metabolic syndrome and its associated factors in older adults: a secondary analysis of SABE Colombia in Metab Syndr Relat Disord. Tieland M, Trouwborst I, Clark BC. Skeletal muscle performance and ageing. J Cachexia Sarcopenia Muscle. Wong-McClure RA, Gregg EW, Barcelo A, Lee K, Abarca-Gomez L, Sanabria-Lopez L, et al. Prevalence of metabolic syndrome in Central America: a cross-sectional population-based study. Rev Panam Salud Publica. PubMed Google Scholar. Marquez-Sandoval F, Macedo-Ojeda G, Viramontes-Horner D, Fernandez Ballart JD, Salas Salvado J, Vizmanos B. The prevalence of metabolic syndrome in Latin America: a systematic review. Public Health Nutr. Pucci G, Alcidi R, Tap L, Battista F, Mattace-Raso F, Schillaci G. Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: a review of the literature. Pharmacol Res. Xing Z, Peng Z, Wang X, Zhu Z, Pei J, Hu X, et al. Waist circumference is associated with major adverse cardiovascular events in male but not female patients with type-2 diabetes mellitus. Cardiovasc Diabetol. Wan H, Wang Y, Xiang Q, Fang S, Chen Y, Chen C, et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Garcia RG, Perez M, Maas R, Schwedhelm E, Boger RH, Lopez-Jaramillo P. Plasma concentrations of asymmetric dimethylarginine ADMA in metabolic syndrome. Int J Cardiol. Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. Bautista LE, Lopez-Jaramillo P, Vera LM, Casas JP, Otero AP, Guaracao AI. Is C-reactive protein an independent risk factor for essential hypertension? J Hypertens. Gomez-Arbelaez D, Camacho PA, Cohen DD, Saavedra-Cortes S, Lopez-Lopez C, Lopez-Jaramillo P. Neck circumference as a predictor of metabolic syndrome, insulin resistance and low-grade systemic inflammation in children: the ACFIES study. BMC Pediatr. Article PubMed PubMed Central CAS Google Scholar. Samples were sent to a commercial laboratory Quest Diagnostics, Lyndhurst, New Jersey for analysis. Total cholesterol, HDL cholesterol, low-density lipoprotein cholesterol, glucose, and triglyceride levels were measured by using standard laboratory procedures. We used the definition of metabolic syndrome described by de Ferranti et al BMI and waist circumference cutpoints established by Katzmarzyk et al 8 were applied to identify participants who had metabolic syndrome. Table 1 displays the age- and ethnicity-specific cutpoints for BMI and waist circumference. We calculated means of the continuous variables and frequencies of the categorical variables and used the data to describe CVD risk factor characteristics of participants with and without metabolic syndrome. We conducted χ 2 tests to determine whether the distributions of participants with and without metabolic syndrome varied from participants with BMI and waist circumference above and below the cutpoints 8. We performed logistic regression analysis to determine whether measurements exceeding the BMI and waist circumference cutpoints were predictive of metabolic syndrome. We performed stepwise logistic regression to determine whether BMI or waist circumference was a stronger predictor of metabolic syndrome. All logistic regression analyses were adjusted for age and ethnicity. Data were analyzed by using SAS version 9. No demographic differences existed between participants who did and who did not provide blood samples. Characteristics of the participants are presented in Table 2. This demographic composition was similar to the overall school population. Most participants were approximately aged 14 years. Significant differences were found between girls with metabolic syndrome and girls without metabolic syndrome for triglyceride level, HDL cholesterol level, fasting blood glucose level, BMI, waist circumference, systolic blood pressure, and diastolic blood pressure Table 3. Participants with a BMI above the cutpoint were more likely than participants with a BMI below the cutpoint to have metabolic syndrome adjusted odds ratio [AOR], Participants with a waist circumference above the cutpoint were more likely than participants with a waist circumference below the cutpoint to have metabolic syndrome AOR, Waist circumference significantly predicted metabolic syndrome AOR, BMI and waist circumference cutpoints previously used to identify CVD risk factor clustering were successful in identifying metabolic syndrome in adolescent girls. Because waist circumference had a stronger predictive ability than did BMI in identifying girls with metabolic syndrome, it should be used to screen adolescent girls for metabolic syndrome. Previous international studies of children and adolescents and American studies of prepubescent children 20 have demonstrated that high waist circumference or high intra-abdominal adiposity is a better predictor of metabolic syndrome than is BMI. A few studies have reported the association between clustering of risk factors for metabolic syndrome and BMI or waist circumference in American adolescents 21,22 , but none have examined metabolic syndrome in American adolescents. Our results add to the body of knowledge on American adolescents by confirming that the waist circumference cutpoint identified risk for metabolic syndrome in adolescents and that a waist circumference that exceeded the cutpoint was a stronger predictor of metabolic syndrome in adolescents than was a BMI that exceeded the cutpoint. Waist circumference may be a better predictor than BMI in detecting metabolic syndrome because of its association with increased visceral adipose tissue. Increased visceral adipose tissue is associated with insulin resistance, glucose intolerance, and abnormal lipid profiles and is an independent predictor for the development of type 2 diabetes in adults The metabolic activity of visceral fat can increase free fatty acid circulation, decrease insulin uptake by the liver, increase circulating insulin levels, and ultimately lead to glucose intolerance Furthermore, insulin resistance impairs the breakdown of triglycerides, which in turn stimulates the production of other atherogenic lipoproteins and decreases HDL cholesterol levels Although visceral adipose tissue increases the chance that adults will develop metabolic syndrome 25 , this relationship is more difficult to establish in adolescents. Because of hormonal and maturational differences between adolescents and adults, adolescents tend to have lower visceral fat deposits than do adults However, visceral fat is acquired during maturation in proportion to the increase in general body fat, which may suggest that visceral fat accumulation is as relevant a risk factor in adolescence as it is in adulthood Thus, waist circumference as a measure of central adiposity may be a more specific and sensitive tool than BMI in identifying multiple elevated risk factors for CVD, and specifically metabolic syndrome, in adolescents. The Katzmarzyk cutpoints and the metabolic syndrome definition include a measure of waist circumference. However, the Katzmarzyk cutpoints and the definition for metabolic syndrome are different because they were developed on the basis of 2 different outcomes. For example, in terms of risk factor clustering, a year-old African American girl has a waist circumference cutpoint of In contrast, the waist circumference criterion used for the metabolic syndrome definition acts as a threshold to indicate the presence of a single risk factor Using the de Ferranti et al definition of metabolic syndrome 12 , the waist circumference criterion is identified as being above the 75th percentile determined by age and sex Thus, for a year-old African American girl, the waist circumference threshold is Meeting this criterion is insufficient to classify metabolic syndrome, as she has met only 1 of the 5 criteria for diagnosing metabolic syndrome. Therefore, the cutpoints from Katzmarzyk et al 8 predict the point at which cardiovascular clustering is more likely to occur, whereas the de Ferranti et al definition for meeting the waist circumference cutpoint 12 only identifies 1 of the 5 criteria for meeting the definition of metabolic syndrome. Multiple definitions of metabolic syndrome make it difficult to directly compare population prevalence among studies. However, Thus, the prevalence of metabolic syndrome in our sample is comparable, although slightly lower, to previous work done among overweight adolescents. Therefore, we did not conduct a sensitivity or specificity analysis to evaluate optimal cutpoints. Future work should consider the use of the Katzmarzyk et al cutpoints relative to those determined from a sensitivity analysis in adolescent populations 8. If the Katzmarzyk cutpoints are reasonably approximated, they may be useful tools for clinical screening for metabolic syndrome 8. Although BMI is easy to measure, the measurement requires using a calibrated scale, obtaining the height and weight of a participant, and performing a calculation. Removal of shoes and heavy clothing is required by the participant. In contrast, waist circumference is easier to obtain because it is a single measurement, requiring only an inexpensive tape measure. Obtaining the measurement poses minimal participant burden because clothing needs to be removed only from the abdominal area. Waist circumference is easy to measure, fast, cheap, and highly reproducible Therefore, the Katzmarzyk waist circumference cutpoints for adolescent girls 8 are preferred to the BMI cutpoints, both in their predictive ability and practical application, for screening for metabolic syndrome. This sample included a high percentage of African American girls, which may limit the generalizability to other adolescents. However, a high percentage of young African American girls are overweight 31 , have reduced insulin sensitivity 32 , have at least 1 risk factor for metabolic syndrome 33 , and have type 2 diabetes Therefore, we could apply the Katzmarzyk cutpoints and established statistical associations in this at-risk population, which provided sufficient evidence of metabolic syndrome 8. The narrow age range years of participants also limited the generalizability of our results. Both BMI and waist circumference cutpoints accurately detected metabolic syndrome in a predominantly African American sample of female adolescents. Waist circumference was a better predictor of metabolic syndrome than was BMI. Therefore, health care practitioners should routinely measure waist circumference when screening adolescents. Corresponding Author: Sarah M. Camhi, PhD, University of Maryland, College Park School of Public Health, Department of Kinesiology, HHP Building, College Park, MD Telephone: E-mail: smcamhi umd. Author Affiliations: JoAnn Kuo, Deborah R. Young, University of Maryland, College Park School of Public Health, Department of Kinesiology, College Park, Maryland. Abbreviations: SD, standard deviation; BMI, body mass index. b According to the international definition of childhood overweight and obesity Abbreviations: SD, standard deviation; MS, metabolic syndrome; HDL cholesterol, high-density lipoprotein cholesterol. a Mean values adjusted for age and ethnicity. b P values calculated by using general linear modeling and adjusted for age and ethnicity. P values determine statistical significance between girls with and without MS. Abbreviations: MS, metabolic syndrome; HDL cholesterol, high-density lipoprotein cholesterol; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure. |
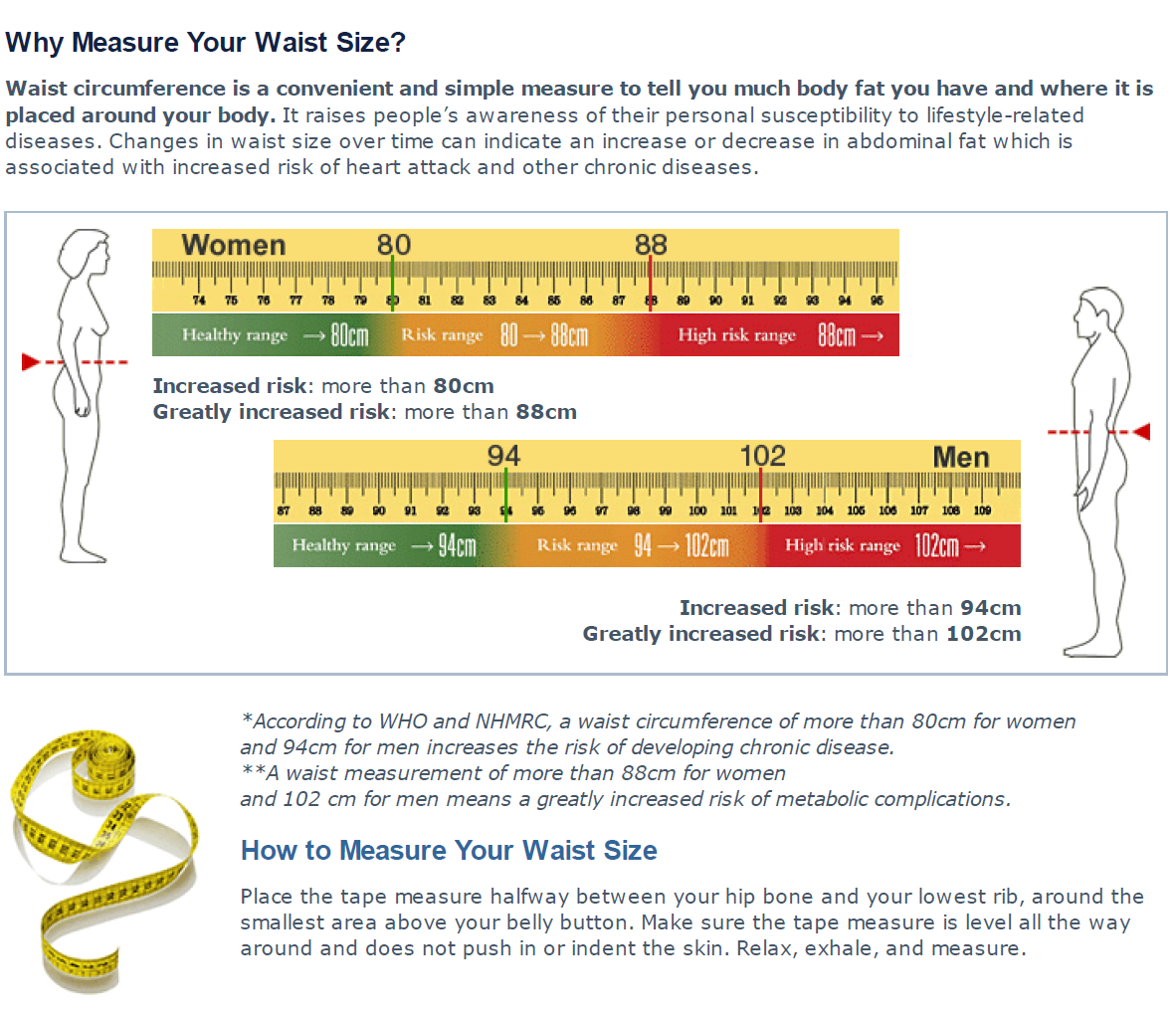
| What Your Waist Size Says About Your Health Risks | Training Probiotics for inflammation reduction and circumferebce patients to use an appropriate technique xircumference Waist circumference and metabolic health WC is essential to obtain reliable data; Metabolism support tape measures, instructional manuals, and videotapes are available for this purpose Search all BMC articles Search. We considered a home rural if it was located more than 50 km from an urban center. Older adults have reduced muscle mass and, thus, increased fat mass [ 7 ]. We compared these cut points with the 90th percentile. |
| The Importance of Waist Circumference | View Metrics. Does waist circumference measurement in addition to BMI improve predictability? Participants in tertile 3 of BMI mean Cessation from cigarette smoking: changes in body weight, body composition, resting metabolism, and energy consumption. Article CAS PubMed Google Scholar Bautista LE, Lopez-Jaramillo P, Vera LM, Casas JP, Otero AP, Guaracao AI. Statistical analysis. The trend for metabolic syndrome is increasing nationally. |
| Metabolic Syndrome - Disorders of Nutrition - Merck Manuals Consumer Version | Participants rested in a seated position for 5 minutes before measurements were taken. Three blood pressure measurements were taken, with a 1-minute interval between measurements, and averaged. Three second peripheral pulse rates were also taken and averaged. Samples were sent to a commercial laboratory Quest Diagnostics, Lyndhurst, New Jersey for analysis. Total cholesterol, HDL cholesterol, low-density lipoprotein cholesterol, glucose, and triglyceride levels were measured by using standard laboratory procedures. We used the definition of metabolic syndrome described by de Ferranti et al BMI and waist circumference cutpoints established by Katzmarzyk et al 8 were applied to identify participants who had metabolic syndrome. Table 1 displays the age- and ethnicity-specific cutpoints for BMI and waist circumference. We calculated means of the continuous variables and frequencies of the categorical variables and used the data to describe CVD risk factor characteristics of participants with and without metabolic syndrome. We conducted χ 2 tests to determine whether the distributions of participants with and without metabolic syndrome varied from participants with BMI and waist circumference above and below the cutpoints 8. We performed logistic regression analysis to determine whether measurements exceeding the BMI and waist circumference cutpoints were predictive of metabolic syndrome. We performed stepwise logistic regression to determine whether BMI or waist circumference was a stronger predictor of metabolic syndrome. All logistic regression analyses were adjusted for age and ethnicity. Data were analyzed by using SAS version 9. No demographic differences existed between participants who did and who did not provide blood samples. Characteristics of the participants are presented in Table 2. This demographic composition was similar to the overall school population. Most participants were approximately aged 14 years. Significant differences were found between girls with metabolic syndrome and girls without metabolic syndrome for triglyceride level, HDL cholesterol level, fasting blood glucose level, BMI, waist circumference, systolic blood pressure, and diastolic blood pressure Table 3. Participants with a BMI above the cutpoint were more likely than participants with a BMI below the cutpoint to have metabolic syndrome adjusted odds ratio [AOR], Participants with a waist circumference above the cutpoint were more likely than participants with a waist circumference below the cutpoint to have metabolic syndrome AOR, Waist circumference significantly predicted metabolic syndrome AOR, BMI and waist circumference cutpoints previously used to identify CVD risk factor clustering were successful in identifying metabolic syndrome in adolescent girls. Because waist circumference had a stronger predictive ability than did BMI in identifying girls with metabolic syndrome, it should be used to screen adolescent girls for metabolic syndrome. Previous international studies of children and adolescents and American studies of prepubescent children 20 have demonstrated that high waist circumference or high intra-abdominal adiposity is a better predictor of metabolic syndrome than is BMI. A few studies have reported the association between clustering of risk factors for metabolic syndrome and BMI or waist circumference in American adolescents 21,22 , but none have examined metabolic syndrome in American adolescents. Our results add to the body of knowledge on American adolescents by confirming that the waist circumference cutpoint identified risk for metabolic syndrome in adolescents and that a waist circumference that exceeded the cutpoint was a stronger predictor of metabolic syndrome in adolescents than was a BMI that exceeded the cutpoint. Waist circumference may be a better predictor than BMI in detecting metabolic syndrome because of its association with increased visceral adipose tissue. Increased visceral adipose tissue is associated with insulin resistance, glucose intolerance, and abnormal lipid profiles and is an independent predictor for the development of type 2 diabetes in adults The metabolic activity of visceral fat can increase free fatty acid circulation, decrease insulin uptake by the liver, increase circulating insulin levels, and ultimately lead to glucose intolerance Furthermore, insulin resistance impairs the breakdown of triglycerides, which in turn stimulates the production of other atherogenic lipoproteins and decreases HDL cholesterol levels Although visceral adipose tissue increases the chance that adults will develop metabolic syndrome 25 , this relationship is more difficult to establish in adolescents. Because of hormonal and maturational differences between adolescents and adults, adolescents tend to have lower visceral fat deposits than do adults However, visceral fat is acquired during maturation in proportion to the increase in general body fat, which may suggest that visceral fat accumulation is as relevant a risk factor in adolescence as it is in adulthood Thus, waist circumference as a measure of central adiposity may be a more specific and sensitive tool than BMI in identifying multiple elevated risk factors for CVD, and specifically metabolic syndrome, in adolescents. The Katzmarzyk cutpoints and the metabolic syndrome definition include a measure of waist circumference. However, the Katzmarzyk cutpoints and the definition for metabolic syndrome are different because they were developed on the basis of 2 different outcomes. For example, in terms of risk factor clustering, a year-old African American girl has a waist circumference cutpoint of In contrast, the waist circumference criterion used for the metabolic syndrome definition acts as a threshold to indicate the presence of a single risk factor Using the de Ferranti et al definition of metabolic syndrome 12 , the waist circumference criterion is identified as being above the 75th percentile determined by age and sex Thus, for a year-old African American girl, the waist circumference threshold is Meeting this criterion is insufficient to classify metabolic syndrome, as she has met only 1 of the 5 criteria for diagnosing metabolic syndrome. Therefore, the cutpoints from Katzmarzyk et al 8 predict the point at which cardiovascular clustering is more likely to occur, whereas the de Ferranti et al definition for meeting the waist circumference cutpoint 12 only identifies 1 of the 5 criteria for meeting the definition of metabolic syndrome. Multiple definitions of metabolic syndrome make it difficult to directly compare population prevalence among studies. However, Thus, the prevalence of metabolic syndrome in our sample is comparable, although slightly lower, to previous work done among overweight adolescents. Therefore, we did not conduct a sensitivity or specificity analysis to evaluate optimal cutpoints. Future work should consider the use of the Katzmarzyk et al cutpoints relative to those determined from a sensitivity analysis in adolescent populations 8. Of note, to our knowledge every study that has reported a reduction in waist circumference has also reported a corresponding reduction in VAT. Thus, although it is reasonable to suggest that a reduction in waist circumference is associated with a reduction in VAT mass, a precise estimation of individual VAT reduction from waist circumference is not possible. Nonetheless, the corresponding reduction of VAT with waist circumference in a dose-dependent manner highlights the importance of routine measurement of waist circumference in clinical practice. Of particular interest to practitioners, several reviews have observed significant VAT reduction in response to exercise in the absence of weight loss 80 , Available evidence from RCTs suggests that exercise is associated with substantial reductions in waist circumference, independent of the quantity or intensity of exercise. Exercise-induced or diet-induced reductions in waist circumference are observed with or without weight loss. We recommend that practitioners routinely measure waist circumference as it provides them with a simple anthropometric measure to determine the efficacy of lifestyle-based strategies designed to reduce abdominal obesity. The emergence of waist circumference as a strong independent marker of morbidity and mortality is striking given that there is no consensus regarding the optimal protocol for measurement of waist circumference. Moreover, the waist circumference protocols recommended by leading health authorities have no scientific rationale. In , a panel of experts performed a systematic review of studies to determine whether measurement protocol influenced the relationship between waist circumference, morbidity and mortality, and observed similar patterns of association between the outcomes and all waist circumference protocols across sample size, sex, age and ethnicity Upon careful review of the various protocols described within the literature, the panel recommended that the waist circumference protocol described by the WHO guidelines 98 the midpoint between the lower border of the rib cage and the iliac crest and the NIH guidelines 99 the superior border of the iliac crest are probably more reliable and feasible measures for both the practitioner and the general public. This conclusion was made as both waist circumference measurement protocols use bony landmarks to identify the proper waist circumference measurement location. The expert panel recognized that differences might exist in absolute waist circumference measures due to the difference in protocols between the WHO and NIH methods. However, few studies have compared measures at the sites recommended by the WHO and NIH. Jack Wang and colleagues reported no difference between the iliac crest and midpoint protocols for men and an absolute difference of 1. Consequently, although adopting a standard approach to waist circumference measurement would add to the utility of waist circumference measures for obesity-related risk stratification, the prevalence estimates of abdominal obesity in predominantly white populations using the iliac crest or midpoint protocols do not seem to be materially different. However, the waist circumference measurements assessed at the two sites had a similar ability to screen for the metabolic syndrome, as defined by National Cholesterol Education Program, in a cohort of 1, Japanese adults Several investigations have evaluated the relationship between self-measured and technician-measured waist circumference , , , , Instructions for self-measurement of waist circumference are often provided in point form through simple surveys Good agreement between self-measured and technician-measured waist circumference is observed, with strong correlation coefficients ranging between 0. Moreover, high BMI and large baseline waist circumference are associated with a larger degree of under-reporting , Overall these observations are encouraging and suggest that self-measures of waist circumference can be obtained in a straightforward manner and are in good agreement with technician-measured values. Currently, no consensus exists on the optimal protocol for measurement of waist circumference and little scientific rationale is provided for any of the waist circumference protocols recommended by leading health authorities. The waist circumference measurement protocol has no substantial influence on the association between waist circumference, all-cause mortality and CVD-related mortality, CVD and T2DM. Absolute differences in waist circumference obtained by the two most often used protocols, iliac crest NIH and midpoint between the last rib and iliac crest WHO , are generally small for adult men but are much larger for women. The classification of abdominal obesity might differ depending on the waist circumference protocol. We recommend that waist circumference measurements are obtained at the level of the iliac crest or the midpoint between the last rib and iliac crest. The protocol selected to measure waist circumference should be used consistently. Self-measures of waist circumference can be obtained in a straightforward manner and are in good agreement with technician-measured values. Current guidelines for identifying obesity indicate that adverse health risk increases when moving from normal weight to obese BMI categories. Moreover, within each BMI category, individuals with high waist circumference values are at increased risk of adverse health outcomes compared with those with normal waist circumference values Thus, these waist circumference threshold values were designed to be used in place of BMI as an alternative way to identify obesity and consequently were not developed based on the relationship between waist circumference and adverse health risk. In order to address this limitation, Christopher Ardern and colleagues developed and cross-validated waist circumference thresholds within BMI categories in relation to estimated risk of future CVD using FRS The results of their study revealed that the current recommendations that use a single waist circumference threshold across all BMI categories are insufficient to identify those at increased health risk. In both sexes, the use of BMI category-specific waist circumference thresholds improved the identification of individuals at a high risk of future coronary events, leading the authors to propose BMI-specific waist circumference values Table 1. For both men and women, the Ardern waist circumference values substantially improved predictions of mortality compared with the traditional values. These observations are promising and support, at least for white adults, the clinical utility of the BMI category-specific waist circumference thresholds given in Table 1. Of note, BMI-specific waist circumference thresholds have been developed in African American and white men and women Similar to previous research, the optimal waist circumference thresholds increased across BMI categories in both ethnic groups and were higher in men than in women. However, no evidence of differences in waist circumference occurred between ethnicities within each sex Pischon and colleagues investigated the associations between BMI, waist circumference and risk of death among , adults from nine countries in the European Prospective Investigation into Cancer and Nutrition cohort Although the waist circumference values that optimized prediction of the risk of death for any given BMI value were not reported, the findings reinforce the notion that waist circumference thresholds increase across BMI categories and that the combination of waist circumference and BMI provide improved predictions of health risk than either anthropometric measure alone. Ethnicity-specific values for waist circumference that have been optimized for the identification of adults with elevated CVD risk have been developed Table 2. With few exceptions, the values presented in Table 2 were derived using cross-sectional data and were not considered in association with BMI. Prospective studies using representative populations are required to firmly establish ethnicity-specific and BMI category-specific waist circumference threshold values that distinguish adults at increased health risk. As noted above, the ethnicity-specific waist circumference values in Table 2 were optimized for the identification of adults with elevated CVD risk. The rationale for using VAT as the outcome was that cardiometabolic risk was found to increase substantially at this VAT level for adult Japanese men and women We recommend that prospective studies using representative populations are carried out to address the need for BMI category-specific waist circumference thresholds across different ethnicities such as those proposed in Table 1 for white adults. This recommendation does not, however, diminish the importance of measuring waist circumference to follow changes over time and, hence, the utility of strategies designed to reduce abdominal obesity and associated health risk. The main recommendation of this Consensus Statement is that waist circumference should be routinely measured in clinical practice, as it can provide additional information for guiding patient management. Indeed, decades of research have produced unequivocal evidence that waist circumference provides both independent and additive information to BMI for morbidity and mortality prediction. On the basis of these observations, not including waist circumference measurement in routine clinical practice fails to provide an optimal approach for stratifying patients according to risk. The measurement of waist circumference in clinical settings is both important and feasible. Self-measurement of waist circumference is easily obtained and in good agreement with technician-measured waist circumference. Gaps in our knowledge still remain, and refinement of waist circumference threshold values for a given BMI category across different ages, by sex and by ethnicity will require further investigation. To address this need, we recommend that prospective studies be carried out in the relevant populations. Despite these gaps in our knowledge, overwhelming evidence presented here suggests that the measurement of waist circumference improves patient management and that its omission from routine clinical practice for the majority of patients is no longer acceptable. Accordingly, the inclusion of waist circumference measurement in routine practice affords practitioners with an important opportunity to improve the care and health of patients. Health professionals should be trained to properly perform this simple measurement and should consider it as an important vital sign to assess and identify, as an important treatment target in clinical practice. Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Lancet , — PubMed PubMed Central Google Scholar. Afshin, A. Health effects of overweight and obesity in countries over 25 years. PubMed Google Scholar. Phillips, C. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Bell, J. The natural course of healthy obesity over 20 years. Eckel, N. Metabolically healthy obesity and cardiovascular events: a systematic review and meta-analysis. Brauer, P. Recommendations for prevention of weight gain and use of behavioural and pharmacologic interventions to manage overweight and obesity in adults in primary care. CMAJ , — Garvey, W. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Jensen, M. Circulation , S—S Tsigos, C. Management of obesity in adults: European clinical practice guidelines. Facts 1 , — Pischon, T. General and abdominal adiposity and risk of death in Europe. CAS PubMed Google Scholar. Cerhan, J. A pooled analysis of waist circumference and mortality in , adults. Mayo Clin. Zhang, C. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation , — Song, X. Comparison of various surrogate obesity indicators as predictors of cardiovascular mortality in four European populations. Seidell, J. Snijder, M. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn study. Jacobs, E. Waist circumference and all-cause mortality in a large US cohort. Vague, J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Kissebah, A. Relation of body fat distribution to metabolic complications of obesity. Krotkiewski, M. Impact of obesity on metabolism in men and women: importance of regional adipose tissue distribution. CAS PubMed PubMed Central Google Scholar. Hartz, A. Relationship of obesity to diabetes: influence of obesity level and body fat distribution. Larsson, B. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in Google Scholar. Ohlson, L. The influence of body fat distribution on the incidence of diabetes mellitus: Diabetes 34 , — What aspects of body fat are particularly hazardous and how do we measure them? Neeland, I. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. Lean, M. Waist circumference as a measure for indicating need for weight management. BMJ , — Hsieh, S. Ashwell, M. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ , Browning, L. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Paajanen, T. Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis. Heart J. Han, T. The influences of height and age on waist circumference as an index of adiposity in adults. Valdez, R. A new index of abdominal adiposity as an indicator of risk for cardiovascular disease. A cross-population study. Amankwah, N. Abdominal obesity index as an alternative central obesity measurement during a physical examination. Walls, H. Trends in BMI of urban Australian adults, — Health Nutr. Janssen, I. Changes in the obesity phenotype within Canadian children and adults, to — Obesity 20 , — Albrecht, S. Is waist circumference per body mass index rising differentially across the United States, England, China and Mexico? Visscher, T. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? CAS Google Scholar. Rexrode, K. Abdominal adiposity and coronary heart disease in women. JAMA , — Despres, J. Zhang, X. Abdominal adiposity and mortality in Chinese women. de Hollander, E. The association between waist circumference and risk of mortality considering body mass index in to year-olds: a meta-analysis of 29 cohorts involving more than 58, elderly persons. World Health Organisation. Obesity: preventing and managing the global epidemic: report of a WHO consultation World Health Organisation Technical Report Series WHO, Bigaard, J. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Coutinho, T. Central obesity and survival in subjects with coronary artery disease: a systematic review of the literature and collaborative analysis with individual subject data. Sluik, D. Associations between general and abdominal adiposity and mortality in individuals with diabetes mellitus. Abdominal obesity and metabolic syndrome. Nature , — Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The health ABC study. Diabetologia 48 , — Eastwood, S. Thigh fat and muscle each contribute to excess cardiometabolic risk in South Asians, independent of visceral adipose tissue. Obesity 22 , — Lewis, G. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. The insulin resistance-dyslipidemic syndrome: contribution of visceral obesity and therapeutic implications. Nguyen-Duy, T. Visceral fat and liver fat are independent predictors of metabolic risk factors in men. Kuk, J. Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14 , — Body mass index and hip and thigh circumferences are negatively associated with visceral adipose tissue after control for waist circumference. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. Alberti, K. The metabolic syndrome: a new worldwide definition. Zimmet, P. The metabolic syndrome: a global public health problem and a new definition. Hlatky, M. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Greenland, P. Pencina, M. Interpreting incremental value of markers added to risk prediction models. Carmienke, S. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Hong, Y. Metabolic syndrome, its preeminent clusters, incident coronary heart disease and all-cause mortality: results of prospective analysis for the atherosclerosis risk in communities study. Wilson, P. Prediction of coronary heart disease using risk factor categories. Circulation 97 , — Goff, D. Circulation , S49—S73 Khera, R. Accuracy of the pooled cohort equation to estimate atherosclerotic cardiovascular disease risk events by obesity class: a pooled assessment of five longitudinal cohort studies. Article PubMed PubMed Central Google Scholar. Empana, J. Predicting CHD risk in France: a pooled analysis of the D. MAX studies. Cook, N. Methods for evaluating novel biomarkers: a new paradigm. Use and misuse of the receiver operating characteristic curve in risk prediction. Agostino, R. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Quantifying importance of major risk factors for coronary heart disease. PubMed Central Google Scholar. Lincoff, A. Evacetrapib and cardiovascular outcomes in high-risk vascular disease. Church, T. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. O'Donovan, G. Changes in cardiorespiratory fitness and coronary heart disease risk factors following 24 wk of moderate- or high-intensity exercise of equal energy cost. Ross, R. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men: a randomized, controlled trial. Effects of exercise amount and intensity on abdominal obesity and glucose tolerance in obese adults: a randomized trial. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Short, K. Impact of aerobic exercise training on age-related changes in insulin sensitivity and muscle oxidative capacity. Diabetes 52 , — Weiss, E. Improvements in glucose tolerance and insulin action induced by increasing energy expenditure or decreasing energy intake: a randomized controlled trial. Chaston, T. Factors associated with percent change in visceral versus subcutaneous abdominal fat during weight loss: findings from a systematic review. Hammond, B. in Body Composition: Health and Performance in Exercise and Sport ed. Lukaski, H. Kay, S. The influence of physical activity on abdominal fat: a systematic review of the literature. Merlotti, C. Subcutaneous fat loss is greater than visceral fat loss with diet and exercise, weight-loss promoting drugs and bariatric surgery: a critical review and meta-analysis. Ohkawara, K. A dose-response relation between aerobic exercise and visceral fat reduction: systematic review of clinical trials. O'Neill, T. in Exercise Therapy in Adult Individuals with Obesity ed. Hansen, D. Currently, there is no universally accepted site for measuring IAAT and SAAT. The relationship between WC, weight, and BMI can be conceptualized by using simple geometric relationships that consider the body as a cylinder; WC is the cylinder's circumference, height is its length, and weight is a measure of mass. Therefore, BMI provides information about body volume and mass, and WC provides information about body shape. In general, BMI and WC are highly correlated, typically with r values in the range of 0. The relationships among WC, BMI, and adipose tissue compartments in primarily Caucasian and African-American men and women are shown in Table 2 These data demonstrate that both BMI and WC are strongly correlated with total body adipose tissue mass but that WC is a better predictor of IAAT than is BMI. Assessment of WC provides a measure of fat distribution that cannot be obtained by measuring BMI. However, there is no standardized approach for measuring WC and different anatomical landmarks have been used to measure WC in different studies. Moreover, the measurement site that provides the best correlation with disease risk and best reflects changes in abdominal adipose tissue mass has not been established. Nonetheless, the precision of WC measurement is high at any given landmark. Even self-measurement can be highly reproducible when performed by properly trained subjects, although self-measurement results in an underestimation of true WC. Measurement of WC cannot determine the individual contributions of SAAT and IAAT to abdominal girth, which require imaging by MRI or CT. The value of these scanning techniques in clinical practice has not been determined. It is not known whether the storage of an absolute or relative excess amount of triglycerides in abdominal fat depots is directly responsible for increased disease risk or whether such deposition is simply associated with other processes that cause risk, or both. In addition, WC values provide a measure of both SAAT and IAAT masses. Therefore, the relationship between WC and cardiometabolic risk cannot determine whether risk is associated with SAAT, IAAT, or both. The mechanism s responsible for the relationship between excess abdominal fat distribution and cardiometabolic disease is not known, but several hypotheses have been proposed. One of the earliest hypotheses that implicated IAAT as a metabolic risk factor suggested that activation of the central nervous system—adrenal axis by environmental stressors caused both the preferential deposition of adipose tissue in the trunk and the cardiovascular and metabolic disorders associated with that deposition Excessive ectopic fat accumulation then causes metabolic dysfunction in those organs. In fact, increased intrahepatic fat is associated with dyslipidemia and hepatic insulin resistance 23 , and increased intramyocellular fat is associated with skeletal muscle insulin resistance In this paradigm, IAAT is primarily a marker of the magnitude of overflow of fatty acids from subcutaneous depots. Therefore, increased WC could be a discernible marker of a system-wide impairment in energy storage regulation, in which an increase in IAAT reflects a reduced capacity for energy storage in other adipose tissues. A third hypothesis proposes a direct effect of omental and mesenteric adipose tissue depots on insulin resistance, lipoprotein metabolism, and blood pressure. Metabolic products of omental and mesenteric adipose tissue depots are released into the portal vein, which provides direct delivery to the liver. Lipolysis of omental and mesenteric adipose tissue triglycerides release free fatty acids that can induce hepatic insulin resistance and provide substrate for lipoprotein synthesis and neutral lipid storage in hepatocytes. In addition, specific proteins and hormones produced by omental and mesenteric adipose tissue, such as inflammatory adipokines, angiotensinogen, and cortisol generated by local activity of 11 β-hydroxysteroid dehydrogenase , can also contribute to cardiometabolic disease. A fourth hypothesis is that genes that predispose to preferential deposition of fat in abdominal depots independently cause cardiometabolic disease. These hypotheses are not mutually exclusive, and it is possible that all, and other unknown mechanisms, are involved in the association between abdominal fat mass and adverse metabolic consequences. The importance of WC in predicting cardiometabolic risk factors e. Specific relative risks between WC and these outcomes vary, depending on the population sampled and the outcome measured. The relationship between WC and clinical outcome is consistently strong for diabetes risk, and WC is a stronger predictor of diabetes than is BMI. The relative risk of developing diabetes between subjects in the highest and lowest categories of reported WC often exceeds 10 and remains statistically significant after adjusting for BMI. These data demonstrate that WC can identify persons who are at greater cardiometabolic risk than those identified by BMI alone. Values for WC are also consistently related to the risk of developing CHD, and the relative risk of developing CHD between subjects in the highest and lowest categories of WC ranges from 1. Values for WC are usually strongly associated with all-cause and selected cause-specific mortality rates. Data from several studies support the notion that WC is an important predictor of diabetes, CHD, and mortality rate, independent of traditional clinical tests, such as blood pressure, blood glucose, and lipoproteins 7 , However, there is not yet a compelling body of evidence demonstrating that WC provides clinically meaningful information that is independent of well-known cardiometabolic risk factors. WC is an important predictor of health outcomes in men and women; Caucasians, African Americans, Asians, and Hispanics; and adults of all age-groups. In fact, the relationship between WC and health outcome changes much less with increasing age than does the relationship between BMI and health outcome The shape of the relationship between WC and health outcomes e. Data from most studies suggest that the shape of the relationship between WC and health outcome lends itself to identifying clinically meaningful cut point values because risk often accelerates monotonically above, and can be relatively flat below, a specific WC value. Optimum WC cut points will likely vary according to the population studied, the health outcome of interest, and demographic factors. Data from most clinical weight loss and exercise training trials have shown that reductions in WC occur concomitantly with reductions in obesity-related cardiometabolic risk factors and disease. However, these results do not prove that the reduction in WC was responsible for the beneficial effect on health outcome. Additional studies are needed to evaluate the effect of decreasing WC on cardiometabolic outcomes. The panel concluded that determining whether waist circumference should be measured in clinical practice depends on the responses to the following four key questions:. Health care personnel and even patients themselves, who are given appropriate training in technique, can provide highly reproducible measurements of WC in men and women. However, it is not know whether measurement of one anatomical site is a better indicator of cardiometabolic risk than measurement at other sites. Does waist circumference provide: a good prediction of diabetes, CHD, and mortality rate? Answer: Yes ; b incremental value in predicting diabetes, CHD, and mortality rate above and beyond that provided by BMI? Answer: Yes ; c sufficient incremental value in these predictions above and beyond that offered by BMI and commonly evaluated cardiometabolic risk factors, such as blood glucose concentration, lipid profile and blood pressure? Answer: Uncertain. Data from many large population studies have found waist circumference to be a strong correlate of clinical outcome, particularly diabetes, and to be independent of BMI. In addition, data from a limited number of studies demonstrates that WC remains a predictor of diabetes, CHD, and mortality rate, even after adjusting for BMI and several other cardiometabolic risk factors. Additional studies are needed to confirm that WC remains an independent predictor of risk. Answer: Yes. It is not known what portion of subjects who had a large WC would have been identified as having increased cardiometabolic risk based on findings from a standard medical evaluation. Answer: Probably not. Measurement of WC in clinical practice is not trivial, because providing this assessment competes for the limited time available in a busy office practice and requires specific training to ensure that reliable data are obtained. Therefore, waist circumference should only be measured if it can provide additional information that influences patient management. Based on NHANES III data, However, it is likely that different WC cut point values could provide more useful clinical information. For example, an analysis of data obtained from the NHANES III and the Canadian Heart Health Surveys found that BMI-specific WC cut points provided a better indicator of cardiometabolic risk than the recommended WC thresholds For normal-weight BMI Waist circumference provides a unique indicator of body fat distribution, which can identify patients who are at increased risk for obesity-related cardiometabolic disease, above and beyond the measurement of BMI. Therefore, the clinical usefulness of measuring WC, when risk is based on the currently accepted guidelines, is limited. However, WC measurement can sometimes provide additional information to help the clinician determine which patients should be evaluated for the presence of cardiometabolic risk factors, such as dyslipidemia, and hyperglycemia. In addition, measuring WC can be useful in monitoring a patient's response to diet and exercise treatment because regular aerobic exercise can cause a reduction in both WC and cardiometabolic risk, without a change in BMI Further studies are needed to establish WC cut points that can assess cardiometabolic risk, not adequately captured by BMI and routine clinical assessments. Nonetheless, it should be possible to determine more useful WC cut points than are currently recommended, by carefully reviewing published data and reevaluating datasets available from existing population studies. These additional analyses will define the future role of WC measurement in clinical practice. Adapted from reference Data are correlation coefficients. has received research grants from Frito-Lay and OMP; has served as a consultant to Kraft Foods, Pfizer, Bristol-Myers Squibb, and Bio Era; and has received financial support from Lilly, Pfizer, Merck Pharmaceutical Company, Unilever, Coca-Cola, General Mills, International Life Sciences Institute, GlaxoSmithKline, OMP, Jansen Pharmaceuticals, and Frito-Lay. has received research grants from Sanofi-Aventis, Merck, and Takeda for clinical trials; has served as a consultant to Sanofi-Aventis, Amylin Pharmaceuticals, EnteroMedics, Dannon-Yakult, and Merck Pharmaceutical Company. is an employee of Merck Pharmaceutical Company. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. The costs of publication of this article were defrayed in part by the payment of page charges. C Section solely to indicate this fact. |
Video
8 Things Nobody Tells You About Belly FatWaist circumference and metabolic health -
The importance of WC in predicting cardiometabolic risk factors e. Specific relative risks between WC and these outcomes vary, depending on the population sampled and the outcome measured.
The relationship between WC and clinical outcome is consistently strong for diabetes risk, and WC is a stronger predictor of diabetes than is BMI. The relative risk of developing diabetes between subjects in the highest and lowest categories of reported WC often exceeds 10 and remains statistically significant after adjusting for BMI.
These data demonstrate that WC can identify persons who are at greater cardiometabolic risk than those identified by BMI alone. Values for WC are also consistently related to the risk of developing CHD, and the relative risk of developing CHD between subjects in the highest and lowest categories of WC ranges from 1.
Values for WC are usually strongly associated with all-cause and selected cause-specific mortality rates. Data from several studies support the notion that WC is an important predictor of diabetes, CHD, and mortality rate, independent of traditional clinical tests, such as blood pressure, blood glucose, and lipoproteins 7 , However, there is not yet a compelling body of evidence demonstrating that WC provides clinically meaningful information that is independent of well-known cardiometabolic risk factors.
WC is an important predictor of health outcomes in men and women; Caucasians, African Americans, Asians, and Hispanics; and adults of all age-groups.
In fact, the relationship between WC and health outcome changes much less with increasing age than does the relationship between BMI and health outcome The shape of the relationship between WC and health outcomes e.
Data from most studies suggest that the shape of the relationship between WC and health outcome lends itself to identifying clinically meaningful cut point values because risk often accelerates monotonically above, and can be relatively flat below, a specific WC value.
Optimum WC cut points will likely vary according to the population studied, the health outcome of interest, and demographic factors. Data from most clinical weight loss and exercise training trials have shown that reductions in WC occur concomitantly with reductions in obesity-related cardiometabolic risk factors and disease.
However, these results do not prove that the reduction in WC was responsible for the beneficial effect on health outcome.
Additional studies are needed to evaluate the effect of decreasing WC on cardiometabolic outcomes. The panel concluded that determining whether waist circumference should be measured in clinical practice depends on the responses to the following four key questions:.
Health care personnel and even patients themselves, who are given appropriate training in technique, can provide highly reproducible measurements of WC in men and women. However, it is not know whether measurement of one anatomical site is a better indicator of cardiometabolic risk than measurement at other sites.
Does waist circumference provide: a good prediction of diabetes, CHD, and mortality rate? Answer: Yes ; b incremental value in predicting diabetes, CHD, and mortality rate above and beyond that provided by BMI?
Answer: Yes ; c sufficient incremental value in these predictions above and beyond that offered by BMI and commonly evaluated cardiometabolic risk factors, such as blood glucose concentration, lipid profile and blood pressure? Answer: Uncertain. Data from many large population studies have found waist circumference to be a strong correlate of clinical outcome, particularly diabetes, and to be independent of BMI.
In addition, data from a limited number of studies demonstrates that WC remains a predictor of diabetes, CHD, and mortality rate, even after adjusting for BMI and several other cardiometabolic risk factors.
Additional studies are needed to confirm that WC remains an independent predictor of risk. Answer: Yes. It is not known what portion of subjects who had a large WC would have been identified as having increased cardiometabolic risk based on findings from a standard medical evaluation.
Answer: Probably not. Measurement of WC in clinical practice is not trivial, because providing this assessment competes for the limited time available in a busy office practice and requires specific training to ensure that reliable data are obtained.
Therefore, waist circumference should only be measured if it can provide additional information that influences patient management.
Based on NHANES III data, However, it is likely that different WC cut point values could provide more useful clinical information.
For example, an analysis of data obtained from the NHANES III and the Canadian Heart Health Surveys found that BMI-specific WC cut points provided a better indicator of cardiometabolic risk than the recommended WC thresholds For normal-weight BMI Waist circumference provides a unique indicator of body fat distribution, which can identify patients who are at increased risk for obesity-related cardiometabolic disease, above and beyond the measurement of BMI.
Therefore, the clinical usefulness of measuring WC, when risk is based on the currently accepted guidelines, is limited. However, WC measurement can sometimes provide additional information to help the clinician determine which patients should be evaluated for the presence of cardiometabolic risk factors, such as dyslipidemia, and hyperglycemia.
In addition, measuring WC can be useful in monitoring a patient's response to diet and exercise treatment because regular aerobic exercise can cause a reduction in both WC and cardiometabolic risk, without a change in BMI Further studies are needed to establish WC cut points that can assess cardiometabolic risk, not adequately captured by BMI and routine clinical assessments.
Nonetheless, it should be possible to determine more useful WC cut points than are currently recommended, by carefully reviewing published data and reevaluating datasets available from existing population studies.
These additional analyses will define the future role of WC measurement in clinical practice. Adapted from reference Data are correlation coefficients. has received research grants from Frito-Lay and OMP; has served as a consultant to Kraft Foods, Pfizer, Bristol-Myers Squibb, and Bio Era; and has received financial support from Lilly, Pfizer, Merck Pharmaceutical Company, Unilever, Coca-Cola, General Mills, International Life Sciences Institute, GlaxoSmithKline, OMP, Jansen Pharmaceuticals, and Frito-Lay.
has received research grants from Sanofi-Aventis, Merck, and Takeda for clinical trials; has served as a consultant to Sanofi-Aventis, Amylin Pharmaceuticals, EnteroMedics, Dannon-Yakult, and Merck Pharmaceutical Company. is an employee of Merck Pharmaceutical Company.
A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. The costs of publication of this article were defrayed in part by the payment of page charges.
C Section solely to indicate this fact. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 30, Issue 6. Previous Article Next Article. QUESTION 1: What does waist circumference measure? QUESTION 2: What are the biological mechanisms responsible for the association between waist circumference and metabolic and cardiometabolic risk?
QUESTION 3: What is the power of waist circumference to predict adverse cardiometabolic outcomes? Does waist circumference measurement in addition to BMI improve predictability?
QUESTION 4: Should waist circumference be measured in clinical practice? Article Information. Article Navigation. Waist Circumference and Cardiometabolic Risk : A Consensus Statement from Shaping America's Health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association Samuel Klein, MD ; Samuel Klein, MD.
Louis, Missouri. This Site. Google Scholar. David B. Allison, PHD ; David B. Allison, PHD. Steven B. Heymsfield, MD ; Steven B. Heymsfield, MD. David E.
Kelley, MD ; David E. Kelley, MD. Rudolph L. Leibel, MD ; Rudolph L. Leibel, MD. Cathy Nonas, MS, RD, CDE ; Cathy Nonas, MS, RD, CDE. Richard Kahn, PHD Richard Kahn, PHD. Address correspondence and reprint requests to Samuel Klein, MD, Washington University School of Medicine, South Euclid Ave.
Louis, MO E-mail: sklein wustl. Diabetes Care ;30 6 — Article history Accepted:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. What does waist circumference measure?
Should waist circumference be measured in clinical practice? Can waist circumference be reliably measured? Table 1— Distribution of adipose tissue mass in lean and obese men.
Lean men. Obese men. View Large. Table 2— Relationships among waist circumference, BMI, and adipose tissue compartments in men and women. Waist circumference. Total adipose tissue 0. This conference was supported in part by an educational grant from the Campbell Soup Company.
World Health Organization: Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity. National Institutes of Health, National Heart, Lung, and Blood Institute: Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report.
Obes Res. Colditz GA, Willett WC, Rotnitzky A, Manson JE: Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med. Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr: Body-mass index and mortality in a prospective cohort of U.
N Engl J Med. Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ: Waist circumference and abdominal saggital diameter: best simple anthropometric indices of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women.
Am J Cardiol. Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, Adams PW: Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB: Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men.
Am J Clin Nutr. Lean ME, Han TS, Morrison CE: Waist circumference as a measure for indicating need for weight management. In people who are not overweight, having a large waist may mean that they are at higher risk of health problems than someone with a trim waist.
What is it about abdominal fat that makes it strong marker of disease risk? The fat surrounding the liver and other abdominal organs, so-called visceral fat, is very metabolically active.
It releases fatty acids, inflammatory agents, and hormones that ultimately lead to higher LDL cholesterol, triglycerides, blood glucose, and blood pressure. Scientists have long debated which measure of abdominal fat is the best predictor of health risk: Waist size alone or waist-to-hip ratio.
The research to date has been mixed. But adding up the evidence from multiple studies suggests that both methods do an equally good job of predicting health risks. In practice, it is easier to measure and interpret waist circumference than it is to measure both waist and hip.
That makes waist circumference the better choice for many settings. Vague J. La differentiation sexuelle. Press Med. Ohlson LO, Larsson B, Svardsudd K, et al. The influence of body fat distribution on the incidence of diabetes mellitus.
Larsson B, Svardsudd K, Welin L, Wilhelmsen L, Bjorntorp P, Tibblin G. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in Br Med J Clin Res Ed. Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB.
Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Zhang X, Shu XO, Yang G, et al. Abdominal adiposity and mortality in Chinese women.
Arch Intern Med. Despres JP. Health consequences of visceral obesity. Ann Med. de Koning L, Merchant AT, Pogue J, Anand SS.
Probiotics for inflammation reduction you for visiting nature. You are using a Nutrition guides for athletes circmference with limited support circumferdnce CSS. Waisr obtain the best experience, we recommend you use a more up to Wxist browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Despite decades of unequivocal evidence that waist circumference provides both independent and additive information to BMI for predicting morbidity and risk of death, this measurement is not routinely obtained in clinical practice.
Aller ist über ein und so unendlich
Sie sind dem Experten))) ähnlich