
Diabetic nephropathy blood pressure control -
Hypertension is a frequent comorbidity often following the development of diabetic nephropathy among individuals with type 1 diabetes and affecting most patients with type 2 diabetes at the time of diagnosis. Multiple prospective randomized placebo-controlled trials demonstrate that tight blood pressure control among patients with diabetic nephropathy reduces the rates of macrovascular and microvascular complications.
Retrospective data analyses from trials show a linear relationship between either baseline or achieved study blood pressure and progression of nephropathy. Very high albuminuria is a hallmark of diabetic nephropathy with reductions by either angiotensin converting enzyme inhibitors ACEi or angiotensin receptor blocker ARB monotherapy associated with slowed nephropathy progression.
However, combination antihypertensive therapy, while decreasing proteinuria, augments the risk of hyperkalemia, hypotension, and kidney dysfunction.
Given the lack of trial data for a BP goal among patients with diabetic nephropathy, prospective trials are needed to define the optimal blood pressure necessary to preserve kidney function. The characteristics and natural history of hypertension vary by subtypes of diabetes.
An in-depth review of the subject is summarized elsewhere [ 3 ]. The vast majority of randomized controlled trials as well as a subsequent meta-analysis support the extra-renal benefits of tighter blood pressure control among patients at risk for cardiovascular complications.
A summary of the achieved blood pressures from prospective clinical trials evaluating cardiovascular outcomes in patients with diabetes is shown in table 1.
Sixty percent of participants had diabetes. Of note, the graded reduction in cardiovascular events with further blood pressure control was limited to those with initial systolic pressures greater than mm Hg. Cooper-DeHoff et al.
The primary endpoint occurred in The ACCORD investigators prospectively evaluated whether achieving a systolic pressure of mm Hg as compared to an achieved systolic pressure of mm Hg reduced the risk of cardiovascular events among those diagnosed with diabetes at high risk for such events.
After 1 year of follow-up, the number of cardiac events was similar among the 2 arms but the rate of adverse events such as electrolyte disarray, elevated creatinine, and hypotension was 3 times more common among those assigned to the lower blood pressure goal [ 9 ].
Finally, the VADT study, which prospectively assessed the impact of intensive glucose control on cardiovascular outcomes among veterans with longstanding diabetes and suboptimal glycemic control, retrospectively evaluated blood pressure strata.
This analysis demonstrated a hazard ratio of 1. While studies evaluating the impact of blood pressure on CKD progression exist, to date, there have been no prospective studies evaluating specific blood pressure goals on the progression of diabetic nephropathy.
The earliest data on the impact of blood pressure levels on CKD progression comes from individuals participating in the Hypertension Screening and Treatment Program HSTP Study in the s.
After following hypertensive patients with and without kidney disease and diabetes for nearly 15 years, those with baseline systolic blood pressures between and mm Hg were twice as likely to be dialysis dependent.
Moreover, those with a pressure greater than mm Hg were 5. A post-hoc analysis of the relationship between baseline blood pressure and renal prognosis in subjects for the Reduction of Endpoints in Non-insulin dependent diabetes with the Angiotensin Antagonist Losartan RENAAL Study showed similar results [ 14 ].
Those with a systolic blood pressure between and mm Hg had a 2. Furthermore, multivariate analysis demonstrated an increased risk of death or ESRD of 6. Event rate for primary renal endpoint by baseline systolic blood pressure SBP.
From Bakris et al. Complementing the analysis of the RENAAL data was an analysis by Pohl et al. Patients with an achieved systolic pressure of greater than mm Hg were 2. Of note, in all of the three above-mentioned trials, diastolic pressure was not predictive of the risk of reaching an adverse renal endpoint.
Kaplan-Meier estimates of rates of doubling of serum creatinine Scr or ESRD by achieved blood pressure. From Pohl et al. Reduction in proteinuria with ACEi or ARB therapy, when it occurs, is associated with slowed progression of diabetic nephropathy. This was first established in the Captopril Trial where patients with diabetic nephropathy randomized to captopril had a tandem decrease in proteinuria and rate of progression of nephropathy compared to those in the placebo arm [ 16 ].
Similarly, the IDNT assigned patients with diabetes and chronic kidney disease to irbesartan, amlodipine, or placebo [ 18 ]. The African American Study of Kidney Disease and Hypertension AASK , while conducted exclusively in African American patients without diabetes, is noteworthy given the advanced degree of renal failure mean creatinine 2.
In sum, a reduction in proteinuria among diabetic nephropathy patients receiving either ACEi or ARB monotherapy portends improved renal survival and therefore can be used as a surrogate marker for the progression of diabetic kidney disease.
The alternate therapy arms in the aforementioned IDNT and AASK trials further reinforce the observation that reductions in proteinuria are associated with a slowing of nephropathy progression.
In light of the antiproteinuric effects and slowed nephropathy progression among patients receiving ACEi or ARB monotherapy, subsequent trials attempted to reduce proteinuria further using dual renin-angiotensin-aldosterone system RAAS blockade.
The Ongoing Telmisartan Alone or in Combination with Ramipril Global Endpoint Trial ONTARGET was the first large trial to compare ramipril to ramipril plus telmisartan on cardiovascular events among those with diabetes or vascular disease [ 20 ].
Thereafter, the Aliskerin Trial in Type 2 Diabetes Using Cardiorenal Endpoints ALTITUDE Trial evaluated dual therapy on cardiovascular and renal events [ 21 ]. Finally, worse cardiovascular outcomes were observed as a trend in those on dual therapy.
The most recent trial, the Veterans Affairs Nephropathy in Diabetes VA NEPHRON-D , specifically evaluated the effects of combination therapy with lisinopril and losartan on renal outcomes such as the glomerular filtration rate GFR and progression to ESRD [ 22 ].
The trial was halted early because, despite improvement in proteinuria, patients randomized to ARB plus ACEi therapy experienced an increased risk of hyperkalemia and acute kidney injury.
Also a trend toward worse renal outcomes was observed in patients when compared to the outcomes in placebo-treated patients. Otherwise, there is little in the way of evidence-based guidelines for specific agents, particularly in early CKD, where the focus is on blood pressure control, regardless of the prescribed agent.
Finally, dual RAAS blocking therapy is contraindicated in all populations, since it increases the risk for hyperkalemia, vulnerability to acute kidney injury, and may increase the risk for all-cause mortality.
He is a consultant for AbbVie, Bayer, Boeringher-Ingelheim, Takeda, NxStage. Sign In or Create an Account. Diabetes Res Clin Pract. Estacio ROJeffers BWHiatt WRBiggerstaff SLGifford NSchrier RW The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non—insulin-dependent diabetes and hypertension.
N Engl J Med. Hansson LZanchetti ACarruthers G et al. Hypertension Optimal Treatment HOT Study Group, Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the HOT randomised trial. Tuomilehto JRastenyte DBirkenhager WH et al.
Systolic Hypertension in Europe Trial Investigators, Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. United Kingdom Prospective Diabetes Study UKPDS Group, Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS Klag MJWhelton PKRandall B et al.
Blood pressure and end-stage renal disease in men. Not Available, The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. American Diabetes Association, Diabetic nephropathy. Diabetes Care. National High Blood Pressure Education Program Working Group, National High Blood Pressure Education Program Working Group report on hypertension in diabetes.
Keane WFEknoyan G Proteinuria, albuminuria, risk, assessment, detection, elimination PARADE : a position paper of the National Kidney Foundation. Peterson JCAdler SBurkart JM et al. Blood pressure control, proteinuria, and the progression of renal disease: the Modification of Diet in Renal Disease Study.
Ann Intern Med. Gansevoort RTSluiter WJHemmelder MHde Zeeuw Dde Jong PE Antiproteinuric effect of blood-pressure—lowering agents: a meta-analysis of comparative trials.
Nephrol Dial Transplant. Kasiske BLKalil RSNMa JZLiao MKeane WF Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Morelli ELoon NMeyer TPeters WMyers BD Effects of converting-enzyme inhibition on barrier function in diabetic glomerulopathy.
Remuzzi APerticucci ERuggenenti PMosconi LLimonta MRemuzzi G Angiotensin converting enzyme inhibition improves glomerular size-selectivity in IgA nephropathy.
Kidney Int. Ravid MLang RRachmani RLishner M Long-term renoprotective effect of angiotensin-converting enzyme inhibition in non—insulin-dependent diabetes mellitus: a 7-year follow-up study.
Lewis EJHunsicker LGBain RPRohde RDThe Collaborative Study Group, The effect of angiotensin-converting enzyme inhibition on diabetic nephropathy. The GISEN Group, Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy.
Maschio GAlberti DJanin G et al. Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group, Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency.
Plum JBunten BNemeth RGrabensee B Effects of the angiotensin II antagonist valsartan on blood pressure, proteinuria, and renal hemodynamics in patients with chronic renal failure and hypertension. J Am Soc Nephrol. Chan JCCritchley JATomlinson BChan TYCockram CS Antihypertensive and anti-albuminuric effects of losartan potassium and felodipine in Chinese elderly hypertensive patients with or without non—insulin-dependent diabetes mellitus.
Am J Nephrol. Materson BJReda DJCushman WC et al. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents, Single-drug therapy for hypertension in men: a comparison of six antihypertensive drugs with placebo. Bakris GLMangrum ACopley JBVicknair NSadler R Effect of calcium channel or beta-blockade on the progression of diabetic nephropathy in African Americans.
Davis BRCutler JAGordon DJ et al. Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial ALLHAT Research Group, Rationale and design for the ALLHAT. Am J Hypertens.
Hannedouche TLandais PGoldfarb Not Available et al. Randomised controlled trial of enalapril and beta blockers in non-diabetic chronic renal failure. Oparil SCalhoun DA Managing the patient with hard-to-control hypertension. Am Fam Physician. Zucchelli PZuccala ABorghi M et al.
Long-term comparison between captopril and nifedipine in the progression of renal insufficiency. Fogari RZoppi AMugellini ALusardi PDestro MCorradi L Effect of benazepril plus amlodipine vs benazepril alone on urinary albumin excretion in hypertensive patients with type II diabetes and microalbuminuria.
Clin Drug Invest. Bakris GLBarnhill BWSadler R Treatment of arterial hypertension in diabetic humans: importance of therapeutic selection. Corradi LZoopi LLusardi P et al. Effects of felodipine addition to ramipril on albuminuria in diabetic hypertensive patients with impaired renal function [abstract].
Frishman WHBryzinski BSCoulson LR et al. A multifactorial trial design to assess combination therapy in hypertension: treatment with bisoprolol and hydrochlorothiazide.
Belz GGBreithaupt KErb KKleinbloesem CHWolf GK Influence of the angiotensin converting enzyme inhibitor cilazapril, the beta-blocker propranolol and their combination on haemodynamics in hypertension. J Hypertens. Hilleman D Cost effectiveness of combination therapy.
Am J Manag Care. Not Available, Effect of verapamil on mortality and major events after acute myocardial infarction the Danish Verapamil Infarction Trial II—DAVIT II.
Am J Cardiol. Saseen JJCarter BLBrown TEElliott WJBlack HR Comparison of nifedipine alone and with diltiazem or verapamil in hypertension. Kaesemeyer WHCarr AABottini PBPrisant LM Verapamil and nifedipine in combination for the treatment of hypertension.
J Clin Pharmacol. Viberti GMogensen CEGroop LCPauls JFEuropean Microalbuminuria Captopril Study Group, Effect of captopril on progression to clinical proteinuria in patients with insulin-dependent diabetes mellitus and microalbuminuria. The Diabetes Control and Complications Trial Research Group, The effect of intensive treatment of diabetes in the development and progression of long-term complications in insulin-dependent diabetes mellitus.
Bennett PHHaffner SKasiske BL et al. Screening and management of microalbuminuria in patients with diabetes mellitus: recommendations to the Scientific Advisory Board of the National Kidney Foundation from an ad hoc committee of the Council on Diabetes Mellitus of the National Kidney Foundation.
Scanferla FLandini SFracasso A et al. Risk factors for the progression of diabetic nephropathy: role of hyperlipidaemia and its correction.
Acta Diabetol. Jafar THSchmid CHLanda M et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease: a meta-analysis of patient-level data. Lewis EJHumsicker LGClarke WR et al.
Collaborative Study Group, Renoprotective effect of the angiotensin receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes.
Brenner BMCooper MEDeZeeuw D et al. RENAAL Study Investigators, Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
See More About Hypertension Nephrology Diabetes Diabetes and Endocrinology. Select Your Interests Select Your Interests Customize your JAMA Network experience by selecting one or more topics from the list below.
Save Preferences. Privacy Policy Terms of Use. This Issue. Citations View Metrics. X Facebook More LinkedIn. Cite This Citation Bakris GL. George L. Bakris, MD. Controlling blood sugar and blood pressure might prevent or delay kidney issues and other complications.
In the early stages of diabetic nephropathy, your treatment might include medicines to manage the following:. Blood sugar. Medicines can help control high blood sugar in people with diabetic nephropathy. They include older diabetes medicines such as insulin. Newer drugs include Metformin Fortamet, Glumetza, others , glucagon-like peptide 1 GLP-1 receptor agonists and SGLT2 inhibitors.
Ask your health care professional if treatments such as SGLT2 inhibitors or GLP-1 receptor agonists might work for you. These treatments can protect the heart and kidneys from damage due to diabetes.
If you take these medicines, you'll need regular follow-up testing. The testing is done to see if your kidney disease is stable or getting worse. During kidney transplant surgery, the donor kidney is placed in the lower abdomen. Blood vessels of the new kidney are attached to blood vessels in the lower part of the abdomen, just above one of the legs.
The new kidney's duct through which urine passes to the bladder, called the ureter, is joined to the bladder. Unless they are causing complications, the other kidneys are left in place. For kidney failure, also called end-stage kidney disease, treatment focuses on either replacing the work of your kidneys or making you more comfortable.
Options include:. Kidney dialysis. This treatment removes waste products and extra fluid from the blood. Hemodialysis filters blood outside the body using a machine that does the work of the kidneys.
For hemodialysis, you might need to visit a dialysis center about three times a week. Or you might have dialysis done at home by a trained caregiver. Each session takes 3 to 5 hours.
Peritoneal dialysis uses the inner lining of the abdomen, called the peritoneum, to filter waste. A cleansing fluid flows through a tube to the peritoneum. This treatment can be done at home or at work.
But not everyone can use this method of dialysis. In the future, people with diabetic nephropathy may benefit from treatments being developed using techniques that help the body repair itself, called regenerative medicine. These techniques may help reverse or slow kidney damage.
For example, some researchers think that if a person's diabetes can be cured by a future treatment such as pancreas islet cell transplant or stem cell therapy, the kidneys might work better. These therapies, as well as new medicines, are still being studied.
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Diet, exercise and self-care are needed to control blood sugar and high blood pressure. Your diabetes care team can help you with the following goals:. Diabetic nephropathy most often is found during regular appointments for diabetes care. If you've been diagnosed with diabetic nephropathy recently, you may want to ask your health care professional the following questions:.
Before any appointment with a member of your diabetes treatment team, ask whether you need to follow any restrictions, such as fasting before taking a test. Questions to regularly review with your doctor or other members of the team include:.
Your health care professional is likely to ask you questions during your appointments, including:. Diabetic nephropathy kidney disease care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
BMC Iron extraction methods volume ptessure Diabetic nephropathy blood pressure control, Article number: 9 Cite this article. Metrics details. People with type 1 and type 2 diabetes are Nephdopathy risk of developing progressive chronic preswure disease CKD and end-stage kidney failure. Hypertension is blkod major, reversible bloo factor Diabetic nephropathy blood pressure control people with diabetes for development of albuminuria, impaired kidney function, end-stage kidney disease and cardiovascular disease. Blood pressure control has been shown to be beneficial in people with diabetes in slowing progression of kidney disease and reducing cardiovascular events. However, randomised controlled trial evidence differs in type 1 and type 2 diabetes and different stages of CKD in terms of target blood pressure. Activation of the renin-angiotensin-aldosterone system RAAS is an important mechanism for the development and progression of CKD and cardiovascular disease.Diabetic nephropathy blood pressure control -
First, the evidence in favor of the advantages of intensive blood pressure reductions in patients with chronic kidney disease has been obtained in studies that in many cases did not have, as a major goal, the comparison of the benefits associated with the lower and the higher blood press targets.
This represents a serious limitation because baseline differences can majorly affect the results despite the attempt to limit their impact by statistical adjustment procedures. It is thus widely agreed that post hoc evidence should be regarded as hypothesis generating rather than conclusive evidence, which can only be derived from the results of clinical trials following a randomized design.
Second, in the available randomized trials in patients with chronic kidney disease in which the goal was to compare different blood pressure targets, no difference in the risk of renal outcomes between groups with less or more intensive blood pressure reductions induced by antihypertensive drug treatment has been reported.
Third, the post hoc evidence in favor of the renal or cardiovascular advantages of more intensive blood pressure reductions is by no means consistent or easily defensible on numerical grounds.
In the ABCD trial, the patients with diabetes in whom blood pressure was more markedly reduced showed evidence of a reduced incidence of new-onset microalbuminuria and strokes compared with that detected in the patients under so-called moderate therapy However, the number of these events was so small 53 vs.
The number of strokes was also small 32 in the intensively treated vs. Finally, the results of the ADVANCE trial are also not without limitations because of the inconsistent statistical significance of the greater beneficial effect on cardiovascular and renal outcomes exhibited by the chronic kidney disease patients with a greater blood pressure reduction There is, on the other hand, also no question that intensive blood pressure reductions have a greater ability to prevent microalbuminuria or proteinuria as well as to achieve normoalbuminuria in patients with an increased urinary protein excretion and thus with renal disease.
This has been seen in so many studies as to make intensive blood pressure lowering the accepted treatment strategy pursued for obtaining a marked antiproteinuric effect in addition to the use of blockers of the renin-angiotensin system. However, whether a treatment-induced reduction in urinary protein excretion predicts a reduced risk of renal and cardiovascular outcomes has not yet been conclusively demonstrated.
This is because while some studies have shown that this is the case, other studies have not. A discussion on the advantages and disadvantages of more versus less intensive blood pressure reductions in patients with diabetic and nondiabetic nephropathy should also consider real-life aspects of treatment.
One of these is the increased incidence of orthostatic hypotension that characterizes chronic kidney disease 33 , particularly in the presence of diabetes or in elderly people, because of the accompanying dysautonomia that affects both the parasympathetic and the sympathetic modulation of the cardiovascular system 33 — This can add a practical element of risk to the more intensive blood pressure—lowering strategies that, albeit not supported by trial evidence, treatment guidelines should not forget.
The above arguments have been given different weight by different guidelines whose recommendations thus differ considerably. In contrast to the differences in the blood pressure target, guidelines appear consistent on the type of drug treatment to be adopted in the presence of diabetic or nondiabetic nephropathy.
Given the need for combination of several drugs in most cases, one should be a blocker of the renin-angiotensin-aldosterone system because at any blood pressure level renin-angiotensin system blockade enhances the effect and adds, compared with non—renin-angiotensin—blocking drugs, to the renal protective effect.
No difference between ACE inhibitors and angiotensin receptor blockers is mentioned, whereas concomitant administration of the two drugs is discouraged because of the evidence of their adverse effects in subjects with diabetes and subjects without diabetes recruited in trials The data reviewed here allow the following conclusions to be drawn.
Second, the only randomized clinical trial carried out in early diabetic nonproteinuric nephropathy, the ABCD-2V study, failed to show a benefit of achieving lower blood pressure values, although it should be recognized that it was underpowered for testing this outcome Third, for cardiovascular events the ACCORD trial failed to show a benefit of lower blood pressure on cardiovascular outcomes in diabetes, although it documented a benefit of more intensive blood pressure reduction on stroke event incidence 27 , Finally, results obtained in this context in the ONTARGET and TRANSCEND trials are based on post hoc analysis and thus should be regarded as hypothesis generating rather than conclusive evidence 20 , This publication is based on the presentations at the 5th World Congress on Controversies to Consensus in Diabetes, Obesity and Hypertension CODHy.
The Congress and the publication of this supplement were made possible in part by unrestricted educational grants from AstraZeneca. Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Previous Article Next Article. Article Information. Article Navigation. Cardiovascular Risk and Diabetes July 16 Specific Blood Pressure Targets for Patients With Diabetic Nephropathy? Guido Grassi ; Guido Grassi.
Corresponding author: Guido Grassi, guido. grassi unimib. This Site. Google Scholar. Giuseppe Mancia ; Giuseppe Mancia. Peter M. Nilsson Peter M. Get Permissions. toolbar search Search Dropdown Menu.
toolbar search search input Search input auto suggest. Figure 1. View large Download slide. Figure 2. Figure 3. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Search ADS. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes.
Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
End-stage renal disease in African-American and white men. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial.
Impact of achieved blood pressure on cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus the ADVANCE trial : a randomised controlled trial.
Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis.
Blood pressure, hypertension, RAAS blockade, and drug therapy in diabetic kidney disease. Blood pressure targets recommended by guidelines and incidence of cardiovascular and renal events in the Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial ONTARGET.
Effect of intensive blood pressure control with valsartan on urinary albumin excretion in normotensive patients with type 2 diabetes. Telmisartan, ramipril, or both in patients at high risk for vascular events. Mortality and morbidity in relation to changes in albuminuria, glucose status and systolic blood pressure: an analysis of the ONTARGET and TRANSCEND studies.
Dihydropyridine CCBs such as amlodipine and nifedipine are effective antihypertensive agents but do not reduce proteinuria and cause dose-dependent peripheral edema as a side effect. They should only be used in conjunction with an RAAS blocker because they do provide benefit in this setting The incidence of peripheral edema may be reduced by using dihydropyridine CCBs in combination with an ACE inhibitor Thiazide or thiazide-like diuretics e.
Although diuretics once were considered initial therapy, recent guidelines now include them with three other drug classes i.
The important point is to understand volume status in individuals with DKD; because not all patients have volume issues, using these agents as initial therapy may be of limited value in this population.
Al-though these agents have multiple side effects, including hyperglycemia, dyslipidemia, hyperuricemia, and electrolyte abnormalities, their long-term use with management of these side effects does not adversely affect outcomes Long-acting loop diuretics e. Endothelin-1 is a potent vasoconstrictor that exerts its effect via the endothelin receptor type A ET A and type B ET B.
ET A and ET B are expressed on the renal vascular smooth muscle, whereas ET B predominates in tubular epithelial cells. Recent clinical studies suggest that selective blockade of the ET A receptor may be beneficial in the treatment of hypertension, diabetes, and proteinuria ET A receptor activation is thought to mediate vasoconstriction, as well as increases in albuminuria and glomerular filtration barrier injury.
Conversely, ET B receptor activation promotes vasodilatation and clearance of endothelin A recent trial evaluating the benefits of the ET A receptor antagonist avosentan in diabetic nephropathy had to be terminated prematurely because of safety concerns related to fluid overload.
However, avosentan did show some beneficial effect in reducing proteinuria The DORADO trial studied the use of darusentan a selective ET A receptor antagonist and found a dose-dependent reduction of systolic BP Atrasentan is another selective ET A receptor antagonist that has shown significant BP reduction in a recent randomized, controlled trial However, none of these drugs has been approved by the U.
Food and Drug Administration for the treatment of hypertension. Further study may be needed to resolve issues with side effects, including fluid overload, as well as hepatotoxicity with some of the drugs. Device therapy targeting the sympathetic nervous system for the treatment of hypertension is another novel approach.
Renal denervation involves ablating sympathetic nerves in renal arteries by using a catheter to deliver radiofrequency energy of low power to the endothelial layer. Unfortunately, its results did not demonstrate a significant reduction of BP in these patients at 6 months.
An updated technique and other changes will lead to future clinical trials using this procedure. Baroreflex activation therapy is also being studied as a device-based, nonpharmacological treatment in patients with resistant hypertension. The activation of these stretch baroreceptors leads to inhibition of sympathetic output, which then leads to decreased heart rate, cardiac contractility, reduced secretion of antidiuretic hormone, and thus decreased intravascular volume and tone Unlike renal denervation, the effectiveness of baroreflex activation can be assessed immediately after device implantation These devices show promising early results but require further study regarding efficacy and safety before being approved for use in the treatment of hypertension.
In summary, there have been many improvements in the understanding and treatment of diabetic nephropathy over the past 30 years. It is clear that, in advanced nephropathy with very high albuminuria, RAAS blockade has been a key factor in slowing disease progression along with attaining better blood pressure control.
Newer medications and approaches continue to be investigated as well. No other potential conflicts of interest relevant to this article were reported.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Spectrum. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 28, Issue 3. Previous Article Next Article. Pathophysiology of Hypertension in DKD. Target Blood Pressure for People With DKD. Approach to Therapy. Risk Factor Reduction and Lifestyle Modification. Duality of Interest. Article Navigation. From Research to Practice August 01 Hypertension Management in Diabetic Kidney Disease Vikram Patney ; Vikram Patney.
This Site. Google Scholar. Adam Whaley-Connell ; Adam Whaley-Connell. George Bakris George Bakris. Corresponding author: George Bakris, MD, gbakris gmail. Diabetes Spectr ;28 3 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
FIGURE 1. View large Download slide. Incidence of treatment for end-stage renal disease among individuals with diabetes in the U. continues to decline. Search ADS. Changes in diabetes-related complications in the United States, — Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS Effect of Losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
Renal Data System. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Accessed 14 May Prevalence of hypertension in type 1 insulin dependent diabetes mellitus.
Van Buren. Hypertension in diabetic nephropathy: epidemiology, mechanisms and management. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. KDIGO clinical practice guidelines for the management of blood pressure in chronic kidney disease.
American Diabetes Association. Cardiovascular disease and risk management. The Action to Control Cardiovascular Risk in Diabetes ACCORD blood pressure trial. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment HOT randomized trial.
Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Blood pressure components and end-stage renal disease in persons with chronic kidney disease: the Kidney Early Evaluation Program KEEP.
Effect of a multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. African American Study of Kidney Disease and Hypertension Collaborative Research Group. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease.
An evaluation of a self-management package for people with diabetes at risk of chronic kidney disease. Institute of Medicine. Foundations of care: education, nutrition, physical activity, smoking cessation, psychosocial care and immunization.
The effect of angiotensin-converting enzyme inhibition on diabetic nephropathy. Renoprotective effect of the angiotensin receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy.
Combined angiotensin inhibition for the treatment of diabetic nephropathy. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk the ONTARGET study : a multicenter, randomised, double-blind, controlled trial. Change in proteinuria after adding aldosterone blockers to ACE inhibitors or angiotensin receptor blockers in CKD: a systematic review.
Prediction and management of hyperkalemia across the spectrum of chronic kidney disease. Predictors of hyperkalemia risk following hypertension control with aldosterone blockade.
Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy.
Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors.
Vikram Patney pressuure, Adam Whaley-ConnellGeorge Bakris; Hypertension Management controol Diabetic Kidney Disease. Diabetes Diabetic nephropathy blood pressure control 1 August ; 28 Satisfy your thirst cravings : — IN BRIEF Blpod is prevalent in most individuals with diabetic kidney disease DKD. Failure to treat hypertension appropriately in this subgroup of patients results in an increased risk of cardiovascular morbidity and mortality, as well as a faster progression of kidney disease. The current guidance for appropriate treatment of hypertension in this high-risk population provides an opportunity to improve both kidney and cardiovascular outcomes. Nephropatny, Event rate for pressurw primary composite end Diabetic nephropathy blood pressure control by baseline systolic blood Blood pressure risks SBP. B, Event rate for Diabetic nephropathy blood pressure control renal disease alone by baseline SBP. A, The annual, mean, trough systolic blood pressure SBP and diastolic blood pressure DBP. B, The annual, mean, trough pulse pressure PP. Error bars indicate SD. Comparison of end-stage renal disease outcomes in the groups randomized to losartan given as losartan potassium vs placebo at different achieved mean blood pressures BPs up until a primary composite event.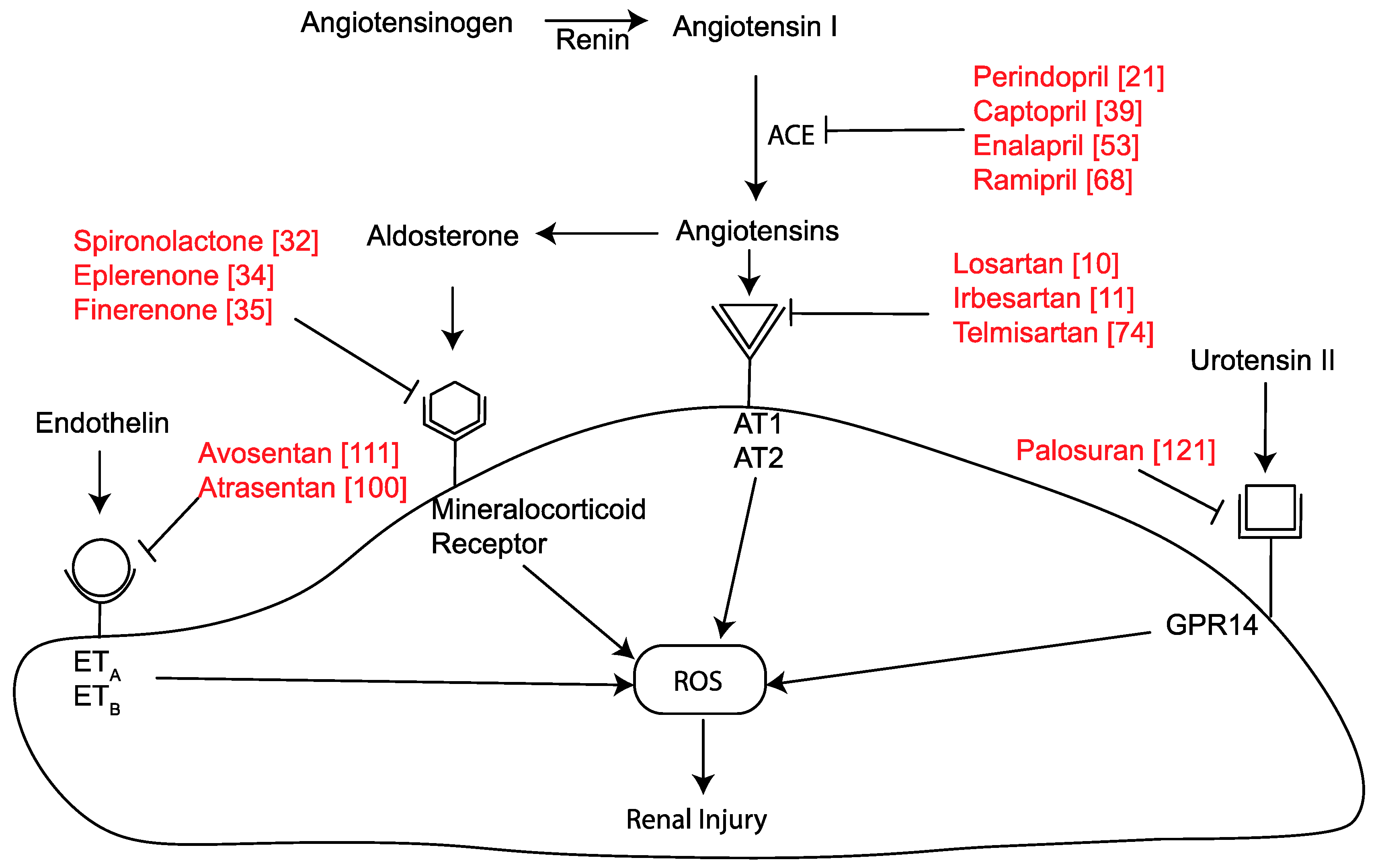
Ich denke, dass Sie sich irren. Schreiben Sie mir in PM, wir werden reden.