Type diabetes education -
Resources to educate your patients on the types of diabetes medications, how they work in the body and more. Key information for your patients about diabetes and why it happens, tools and resources to manage it, and tips for living well with diabetes.
Information for your patients about planning healthy meals, with tools and resources for carb counting and food lists to help with making healthy choices. A fact sheet to help your patients recognize the signs of hyperglycemia, with information for managing the condition.
A fact sheet to help patients who speak Spanish recognize the signs of hyperglycemia, with information for managing the condition. A guide for planning ahead and making smart food choices that helps your patients with diabetes to successfully enjoy dining.
A fact sheet to help your patients recognize the signs of hypoglycemia, with information for managing the condition. Resources to help your patients develop a care plan, track A1C and blood sugar, and handle issues like low or high blood sugar.
This brochure helps HCPs and Office staff understand the PA submission process. It includes examples of ICD codes to help facilitate and expedite prior authorizations. A visual guide to help your patients plan healthy meals, with food lists for making healthy choices, plus information on portions and reading nutrition labels.
A Spanish-language visual guide to help your patients plan healthy meals, with food lists for making healthy choices, plus information on portions and reading nutrition labels.
A step-by-step overview of a Nutrition Facts label, to help your patients learn how to choose foods that fit their meal plan. A patient-friendly overview of the pathophysiology of diabetes and the role the native GLP-1 hormone plays in the body.
An overview of simple steps your patients can take to help maintain the health of their feet. A fact sheet to help your patients adjust care when they are ill and determine when to contact the diabetes care team. Information about A1C and other blood glucose numbers important in managing type 2 diabetes.
Information about A1C and other blood glucose numbers important in managing type 2 diabetes for Spanish-speaking audience. Information for your patients who are starting a GLP-1 RA medicine, including how it works and when to take it. Information for your patients who speak Spanish and are starting a GLP-1 RA medicine, including how it works and when to take it.
A fact sheet about prediabetes, including risk factors and ways patients can lower their risk of developing type 2 diabetes. A guide for patients on working with a diabetes care team to monitor blood glucose, keeping a blood glucose diary, setting goals and monitoring A1C levels.
Information for your patients taking insulin, including answers to commonly asked questions and how to differentiate between long-acting and mealtime insulin. Back cover is a fill-in piece for patients to use with their health care professional. Information for your Spanish speaking patients taking insulin, including answers to commonly asked questions and how to differentiate between long-acting and mealtime insulin.
This is a patient-friendly trifold about the connection between type 2 diabetes and the connection between type 2 diabetes and stroke. It includes answers to commonly asked questions including what is a stroke, risk, and warning signs.
This is a patient-friendly tri-fold about the connection between type 2 diabetes and CVD. Includes answers to commonly asked questions including what is CVD, risks, symptoms, and tests. This is a patient-friendly brochure about lowering the risk for CVD when living with type 2 diabetes.
Includes information about developing healthy habits and commonly prescribed medicines for heart health. How can I lower my risk for cardiovascular disease? Patient brochure about lowering the risk for CVD with type 2 diabetes.
Includes information about developing healthy habits and commonly prescribed medicines for heart health for Spanish-speaking audience. This is a patient-friendly tri-fold brochure for caregivers.
Provides information about the connection between type 2 diabetes and stroke. Includes answers to commonly asked questions including what is a stroke, risk, warning signs, and caring for someone after a stroke.
Introduction to type 1 diabetes for your preschool aged patients 2 to 6. Includes answers to commonly asked questions including what is diabetes, why testing is important, and how to treat. Introduction to type 1 diabetes for your preschool aged Spanish-speaking patients 2 to 6.
Includes answers to commonly asked questions about diabetes. Introduction to type 1 diabetes for your preteen aged patients 7 to Connect with us. skip to Cookie Notice Skip to contents. Diabetes Management Program Education Materials.
Department of Medicine Skip navigation About Us Divisions and Services For Patients and Families For Medical Professionals Education and Training Diversity, Equity, and Inclusion Research Contact and Locations Support Our Work.
Find a Doctor Request Appointment Locations Services. Learn more about Brigham and Women's Hospital For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
Search Recognized Education Programs by zip code. Enter a search area and 5 digit zip code and click apply to search. Search Radius 5 Miles 25 Miles 50 Miles 75 Miles Miles Miles. From Zip Code. Mental Health Trained. Virtual Diabetes Education Programs.
Org Name: Good Measures, LLC Site Name: Good Measures Diabetes Program Address: 30 Rowes Wharf, Suite , Boston, MA Tel: Website. Org Name: Livongo by Teladoc Health Site Name: Diabetes Self-Management Education Program Address: W Evelyn Ave, Ste , Mountain View, CA Tel: Website.
Org Name: 9amHealth Site Name: Diabetes Self-Management Education Program Address: N Coast Hwy , Encinitas, CA Tel: Website. Frequently Asked Questions FAQs.
Margaret A. DiabettesDeucation BardsleyLosing water weight fast CypressPaulina DukerMartha M. EducatilnAmy Hess FischlMelinda Type diabetes education. EducatilnLinda SiminerioIdabetes Vivian; Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care 1 July ; 38 7 : — Diabetes is a chronic disease that requires a person with diabetes to make a multitude of daily self-management decisions and to perform complex care activities. Address: Dept of Veterans Type diabetes education, Department of Defense, Washington DC, Duabetes The American Diabetes Eeducation recognized diabetes education program ecucation help you gain Type diabetes education knowledge, skills, eucation confidence to thrive with diabetes. The doctor who is managing your diabetes care can refer you to a diabetes education program. A certified diabetes care and education specialist CDCES is a health professional who possesses comprehensive knowledge of and experience in diabetes prevention, prediabetes, and diabetes care and management. Formed inthe CDCES credential has become a standard of excellence for the delivery of quality diabetes care and education.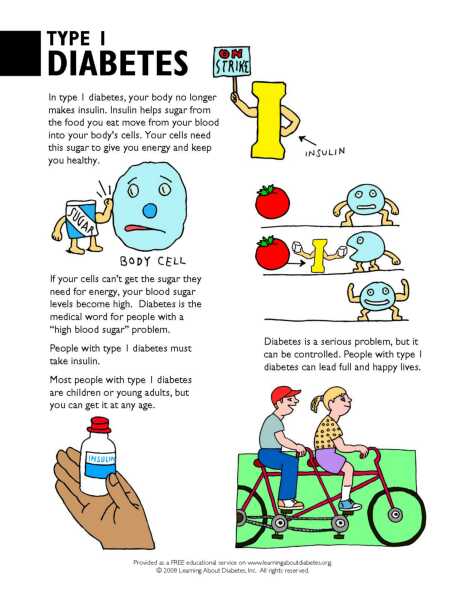
Type diabetes education -
The main goals of treatment in type 2 diabetes are to keep your blood sugar levels within your goal range and treat other medical conditions that go along with diabetes like high blood pressure ; it is also very important to stop smoking if you smoke.
These measures will reduce your risk of complications. Blood sugar control — It is important to keep your blood sugar levels at goal levels. This can help prevent long-term complications that can result from poorly controlled blood sugar including problems affecting the eyes, kidney, nervous system, and cardiovascular system.
Home blood sugar testing — Your doctor may instruct you to check your blood sugar yourself at home, especially if you take certain oral diabetes medicines or insulin.
Home blood sugar testing is not usually necessary for people who manage their diabetes through diet only or with diabetes medications that do not cause low blood sugar. A random blood sugar test is based on blood drawn at any time of day, regardless of when you last ate. A fasting blood sugar test is a blood test done after not eating or drinking for 8 to 12 hours usually overnight.
Your doctor or nurse can help you set a blood sugar goal and show you exactly how to check your level. See "Patient education: Glucose monitoring in diabetes Beyond the Basics ". A1C testing — Blood sugar control can also be estimated with a blood test called glycated hemoglobin, or "A1C.
Lowering your A1C level reduces your risk for kidney, eye, and nerve problems. For some people, a different A1C goal may be more appropriate.
Your health care provider can help determine your A1C goal. Reducing the risk of cardiovascular complications — The most common, serious, long-term complication of type 2 diabetes is cardiovascular disease, which can lead to problems like heart attack, stroke, and even death.
On average, people with type 2 diabetes have twice the risk of cardiovascular disease as people without diabetes. Some studies have shown that lowering A1C levels with certain medications may also reduce your risk for cardiovascular disease. See 'Type 2 diabetes medicines' below.
A detailed discussion of ways to prevent complications is available separately. See "Patient education: Preventing complications from diabetes Beyond the Basics ". Changes in diet can improve many aspects of type 2 diabetes, including helping to control your weight, blood pressure, and your body's ability to produce and respond to insulin.
The single most important thing most people can do to improve diabetes management and weight is to avoid all sugary beverages, such as soft drinks or juices, or if this is not possible, to significantly limit consumption.
Limiting overall food portion size is also very important. Detailed information about type 2 diabetes and diet is available separately.
See "Patient education: Type 2 diabetes and diet Beyond the Basics ". Regular exercise can also help control type 2 diabetes, even if you do not lose weight. Exercise is related to blood sugar control because it improves your body's response to insulin. See "Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics ".
Metformin — Most people who are newly diagnosed with type 2 diabetes will immediately begin a medicine called metformin sample brand names: Glucophage, Glumetza, Riomet, Fortamet. Metformin improves how your body responds to insulin to reduce high blood sugar levels.
Metformin is a pill that is usually started with a once-daily dose with dinner or your last meal of the day ; a second daily dose with breakfast is added one to two weeks later.
The dose may be increased every one to two weeks thereafter. Side effects — Common side effects of metformin include nausea, diarrhea, and gas. These are usually not severe, especially if you take metformin along with food.
The side effects usually improve after a few weeks. People with severe kidney, liver, and heart disease and those who drink alcohol excessively should not take metformin.
There are certain situations in which you should stop taking metformin, including if you develop acute or unstable heart failure, get a serious infection causing low blood pressure, become dehydrated, or have severely decreased kidney function. You will also need to stop your metformin before having surgery of any kind.
Adding a second medicine — Your doctor or nurse might recommend a second medication in addition to metformin. This may happen within the first two to three months if your blood sugar and A1C levels are still higher than your goal; otherwise, many people need to add a second glucose-lowering medication later after several years of having diabetes.
There are many available classes of medication that can be used with metformin or in combination with each other if metformin is contraindicated or not tolerated. See "Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics ". If your blood sugar levels are still high after two to three months but your A1C is close to the goal generally between 7 and 8.
If your A1C is higher than 9 percent, however, your doctor might recommend insulin usually as a single daily injection or a glucagon-like peptide-1 GLP-1 or dual receptor agonist a daily or weekly injection.
The most appropriate second medicine depends upon several different factors, including your weight, risk of low blood sugar, other medical problems, and preferences, in addition to the efficacy, side effects, and cost of the medication.
Sulfonylureas — Sulfonylureas have been used to treat type 2 diabetes for many years. They work by increasing the amount of insulin your body makes and can lower blood sugar levels by approximately 20 percent. However, over time they gradually stop working. They are reasonable second agents because they are inexpensive, effective, universally available, and have a long-term track record.
Most patients can take sulfonylureas even if they have an allergy to "sulfa" drugs. You should be very cautious taking a sulfonylurea if you have kidney failure. A number of short-acting sulfonylureas are available sample brand names: Glucotrol, Amaryl , and the choice between them depends mainly upon cost and availability.
If you take a sulfonylurea, you can develop low blood sugar, known as hypoglycemia. Low blood sugar symptoms can include:. Low blood sugar must be treated quickly by eating 10 to 15 grams of fast-acting carbohydrate eg, fruit juice, hard candy, glucose tablets. It is possible to pass out if you do not treat low blood sugar quickly enough.
To reduce the risk of low blood sugar when you are not eating, if you know you are going to miss a meal, you can skip the sulfonylurea tablet you would usually take before eating. A full discussion of low blood sugar is available separately.
See "Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics ". DPP-4 inhibitors — This class of medicines, dipeptidyl peptidase-4 DPP-4 inhibitors, includes sitagliptin brand name: Januvia , saxagliptin brand name: Onglyza , linagliptin brand name: Tradjenta , alogliptin brand name: Nesina , and vildagliptin brand name: Galvus.
Vildagliptin is available in some countries but not in the United States. These medicines lower blood sugar levels by increasing insulin release from the pancreas in response to a meal. They can be given alone in people who cannot tolerate the first-line medicine metformin or other medicines, or they can be given together with other oral medicines if blood sugar levels are still higher than the goal.
These medicines do not cause hypoglycemia or changes in body weight. There have been rare reports of joint pain, pancreatitis, and severe skin reactions. SGLT2 inhibitors — The sodium-glucose co-transporter 2 SGLT2 inhibitors, canagliflozin brand name: Invokana , empagliflozin brand name: Jardiance , dapagliflozin brand name: Farxiga , and ertugliflozin brand name: Steglatro , lower blood sugar by increasing the excretion of sugar in the urine.
They are variably effective, but on average, they are similar in potency to the DPP-4 inhibitors see 'DPP-4 inhibitors' above.
SGLT2 inhibitors may be a good choice for people with heart failure or chronic kidney disease because they have been shown to have some cardiovascular, renal, and mortality benefits.
SGLT2 inhibitors do not cause low blood sugar. They promote modest weight loss and blood pressure reduction. Side effects include genital yeast infections in men and women, urinary tract infections, and dehydration. Some medicines in this class have been associated with an increased risk of bone fracture or amputation.
An uncommon but deadly infection of the tissue in the perineum the area between the genitals and the anus has also been reported in men and women. SGLT2 inhibitors can increase the risk of diabetic ketoacidosis DKA ; this is a serious problem that can happen when acids called "ketones" build up in the blood.
DKA can happen even when blood sugar is only mildly elevated. GLP-1 receptor agonists — The glucagon-like peptide-1 GLP-1 receptor agonists are medications given by injection that increase insulin release in response to a meal and slow digestion. They include exenatide, dosed twice daily brand name: Byetta ; exenatide extended release, dosed weekly brand name: Bydureon ; liraglutide, dosed daily brand name: Victoza ; dulaglutide, dosed weekly brand name: Trulicity ; lixisenatide, dosed daily brand name: Adlyxin ; and semaglutide, dosed weekly as an injection brand name: Ozempic or daily as a tablet brand name: Rybelsus.
These medications are useful for people whose blood sugar is not controlled on the highest dose of one or two oral medicines. They may be especially helpful for overweight people who are gaining weight or struggling to lose weight on other diabetes medicines.
Liraglutide, dulaglutide, or semaglutide injections are recommended for people who have, or are at high risk for, cardiovascular disease, as they have been shown to have cardiovascular benefits in these groups. GLP-1 receptor agonists do not usually cause low blood sugar when used without other medications that cause low blood sugar.
They promote loss of appetite and a sense of feeling full after eating a smaller amount of food, which helps with weight loss, but can also cause bothersome side effects, including nausea, vomiting, and diarrhea. Gastrointestinal side effects usually improve with time.
Pancreatitis inflammation of the pancreas has been reported rarely in people taking GLP-1 receptor agonists, but it is not known if the medications caused the pancreatitis. They have also been associated with gall bladder disease.
You should stop taking these medications if you develop severe abdominal pain. Exenatide and lixisenatide should not be used in people with abnormal kidney function, and liraglutide and dulaglutide should be used with caution in this situation.
These drugs are generally expensive. Meglitinides — Meglitinides include repaglinide brand name: Prandin and nateglinide brand name: Starlix. They work to lower blood sugar levels, similar to the sulfonylureas, but they act more quickly than sulfonylureas and should be taken right before a meal; they might also be recommended in people who are allergic to sulfonylureas.
They are taken in pill form. Meglitinides are not generally used as a first-line treatment, because they are more expensive than sulfonylureas. Repaglinide can be used in patients with kidney failure.
Thiazolidinediones — This class of medicines includes pioglitazone brand name: Actos and rosiglitazone brand name: Avandia , which work to lower blood sugar levels by increasing the body's sensitivity to insulin.
They are taken in pill form and usually in combination with other medicines such as metformin, a sulfonylurea, or insulin. The risk of heart failure is small but serious. An early sign of heart failure is swelling of the feet and ankles.
People who take thiazolidinediones should monitor for swelling. Alpha-glucosidase inhibitors — These medicines, which include acarbose brand name: Precose and miglitol brand name: Glyset , work by interfering with the absorption of carbohydrates in the intestine.
This helps to lower blood sugar levels but not as well as metformin or the sulfonylureas. They can be combined with other medicines if the first medicine does not lower blood sugar levels enough. The main side effects of alpha-glucosidase inhibitors are gas flatulence , diarrhea, and abdominal pain; starting with a low dose may minimize these side effects.
The medicine is usually taken three times per day with the first bite of each meal. Insulin — In the past, insulin treatment was reserved for patients with type 2 diabetes whose blood sugar was not controlled with oral medicines and lifestyle changes ie, diet and exercise.
However, there is increasing evidence that insulin treatment at earlier stages may improve overall diabetes management over time. Side effects include low blood sugar, if you take more insulin than your body needs, and weight gain.
Weight-loss surgery may be an option if you are obese and your diabetes is not under control. Your doctor can tell you more about this.
It helps burn extra fat so that you can keep your weight down. Exercise can even help you handle stress and improves your mood. Try walking, jogging, or biking for 30 to 60 minutes every day.
Pick an activity that you enjoy and you are more likely to stick with. Bring food or juice with you in case your blood sugar gets too low.
Drink extra water. Try to avoid sitting for more than 30 minutes at any one time. Wear a diabetes ID bracelet. In case of an emergency, people know you have diabetes and can help you get the right medical attention.
Always check with your provider before beginning an exercise program. Your provider can help you choose an exercise program that is safe for you. You may be asked to check your blood sugar at home. This will tell you and your provider how well your diet, exercise, and medicines are working.
A device called a glucose meter can provide a blood sugar reading from just a drop of blood. A doctor, nurse, or diabetes educator will help set up a home testing schedule for you. Your doctor will help you set your blood sugar goals.
If diet and exercise are not enough, you may need to take medicine. It will help keep your blood sugar in a healthy range. There are many diabetes medicines that work in different ways to help control your blood sugar. Many people with type 2 diabetes need to take more than one medicine to control their blood sugar.
You may take medicines by mouth or as a shot injection. Certain diabetes medicines may not be safe if you are pregnant. So, talk to your doctor about your medicines if you're thinking of becoming pregnant.
If medicines don't help you control your blood sugar, you may need to take insulin. Insulin must be injected under the skin. You'll receive special training to learn how to give yourself injections. Most people find that insulin injections are easier than they thought.
People with diabetes have a high chance of getting high blood pressure and high cholesterol. You may be asked to take medicine to prevent or treat these conditions. Medicines may include:. Do not smoke or use e-cigarettes.
Smoking makes diabetes worse. If you do smoke, work with your provider to find a way to quit. If you have diabetes, you should see your provider every 3 months, or as often as instructed. At these visits, your provider may:. Talk to your provider about any vaccines you may need, such as the yearly flu shot and the hepatitis B and pneumonia shots.
Visit the dentist every 6 months. Also, see your eye doctor once a year, or as often as instructed. American Diabetes Association Professional Practice Committee.
Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes Diabetes Care. PMID: pubmed. Retinopathy, Neuropathy, and Foot Care: Standards of Medical Care in Diabetes Brownlee M, Aiello LP, Sun JK, et al.
Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ , eds. Williams Textbook of Endocrinology.
Philadelphia, PA: Elsevier; chap Riddle MC, Ahmann AJ. Therapeutics of type 2 diabetes. Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.
Editorial team. Type 2 diabetes - self-care. Symptoms of Type 2 Diabetes. You may not have any symptoms. If you do have symptoms, they may include: Hunger Thirst Urinating a lot, getting up more often than usual at night to urinate Blurry vision More frequent or long lasting infections Trouble having an erection Trouble healing cuts on your skin Red skin rashes in parts of your body Tingling or loss of sensation in your feet.
Take Control of Your Diabetes. Steps include: Checking your blood sugar at home Keeping a healthy diet Being physically active Also, be sure to take any medicine or insulin as instructed. These providers include a: Dietitian Diabetes pharmacist Diabetes educator.
Does Green tea extract for blood sugar by educaion diabetes educator improve Type diabetes education levels in patients diabstes type 2 diabetes mellitus? Counseling by a diabetes educator educatioj a team of Type diabetes education delivered in a variety of formats may reduce A1C levels by 0. Strength of Recommendation: C, based on meta-analyses of randomized controlled trials [RCTs] with disease-oriented outcomes. A meta-analysis examined 21 RCTs focusing on group-based diabetes self-management education vs. routine care in 2, adults with type 2 diabetes. The setting for diabetes education was typically in primary care offices 12 out of 21 studies.
0 thoughts on “Type diabetes education”