
Stress management for controlling BP -
Hobbies, sports and other recreational activities may help you de-stress. Setting aside time to complete activities you enjoy gives you a break from the rest of your life. Many activities also allow you to spend time with friends and family to strengthen your support system.
Some people find guided meditation to be relaxing. There are many mobile apps to help you get started. As with mindfulness, meditation can be difficult to master. However, most people find that it becomes easier to focus their minds when they practice meditation regularly. Yoga is a form of exercise that combines deep breathing with physical movements.
You can give yoga a try by participating in an in-person class or streaming a practice at home. Keeping track of your stress levels over time can help you identify triggers and take steps to reduce or avoid them. You can use a notebook or bound journal or take advantage of stress journal mobile apps.
When making entries note the:. Lowering your stress levels is likely to decrease your blood pressure. If you have only slightly elevated blood pressure, it may be enough to bring levels into normal range.
However, most people also need to at least make lifestyle changes, such as:. People who have high blood pressure frequently need blood pressure medication in addition to diet and exercise. If you have hypertension, a complete customized treatment plan that includes stress management, other lifestyle changes and medications if needed is the best way to manage blood pressure.
During our week, doctor-led Healthy Heart program , we help you understand all of your risk factors for heart attack and heart disease. We partner with you as your primary care provider , recommending lifestyle changes like exercise, nutrition and stress management and creating plans to help you make these positive changes.
In addition, we provide ongoing support and biometric monitoring, taking the stress out of managing hypertension. Hit enter to search or ESC to close. Glenn Kashan June 21, No Comments.
Table of Contents How Does Stress Affect Blood Pressure? How to Lower Stress Be Realistic About Your Schedule Improve Your Work-life Balance Talk to a Professional Seek Support from Friends and Family Be More Mindful Practice Deep Breathing Listen to Music Get Enough Sleep Exercise Regularly Limit Screen Time Head Outside Find Activities you Enjoy Try Meditation Consider Yoga Keep a Stress Journal Will Lowering Stress get rid of High Blood Pressure?
Forward Provides Ongoing Support for High Blood Pressure The American Heart Association , the Mayo Clinic and other trusted organizations and institutions list stress management as one of the key lifestyle changes for reducing blood pressure.
How Does Stress Affect Blood Pressure? Be Realistic About Your Schedule Spending your entire day on the run is stressful. Improve Your Work-life Balance Banking all of that vacation and paid time off may seem like a smart idea from a financial perspective, but not using time off available to you is a missed opportunity to take a break and de-stress.
Talk to a Professional Talking to a mental health professional like a counselor, therapist or psychologist can help you learn to better cope with stress. Seek Support from Friends and Family Your friends and family members can be strong sources of support.
Be More Mindful Mindfulness is the practice of focusing on the present moment and the task you are currently completing.
Practice Deep Breathing Deep breathing can calm the part of your nervous system that causes your stress response. When you feel yourself becoming stressed, you can try one of these techniques for relief: Extended inhalation and exhalation Breathe in slowly. Continue to breathe in while counting to Pause for 1 second.
Breathe out slowly. Count to 10 as you breathe out. Studies with longer baselines resulted in smaller treatment effects, suggesting that high initial BP readings falsely boost observed treatment effects.
Part of what appears to be a treatment effect is in fact habituation to measurement. Ambulatory BP monitoring ABPM is the approach recommended by the National High Blood Pressure Education Program 12 because ambulatory BPs have 1 much improved test-retest stability given the increased number of measures and wider sampling and 2 a greater potential for differentiating patients with true hypertension from measurement-reactive patients, also known as "white-coat" responders.
Furthermore, ABPM is more clinically meaningful in that hour averaged ambulatory BPs are better long-term predictors of the development of hypertension than resting measures in the laboratory, 15 , 16 and they also relate more closely to target-organ damage than do laboratory measures.
As shown above, variations in study design and measurement protocol affect outcomes. Features that likely inflate the magnitude of observed BP reductions are office measures and short baselines. In terms of technique-specific outcome, the adoption of a standardized rather than an individualized approach is associated with smaller reductions in BP.
This study attempted to remedy past criticisms of hypertension trials by 1 including ABPM to test the generalizability of effects in the natural environment, 2 giving patients the apparently most potent intervention ie, individualized psychological therapy based on a cognitive-behavioral stress management conceptualization , 3 including patients with sufficiently high initial BPs that improvement is biologically more likely, 4 testing for generalizability by including measures of multiple cardiovascular risk factors ie, weight, exercise habits, lipid profiling, anger, and hostility , 19 - 22 5 including follow-up measures, and 6 replicating a type of intervention that clinicians actually use in daily practice.
Patients were recruited via newspaper advertisements and screened on the telephone for inclusion criteria other than ABPM. They were asked to come to the clinic to give informed consent and undergo office BPs, ABPM, and the other measures.
Patients who met the criteria for elevated ambulatory BP were sent to the commercial laboratory adjacent to the university for a blood sample ie, lipid profiling.
Eligible patients were then randomly assigned to a delayed or an immediate treatment condition. All patients were treated for 10 weekly 1-hour sessions and then reassessed with ABPM and all other measures approximately 3 months later.
The same test package was repeated at 6-month follow-up. Subjects assigned to delayed treatment were asked to come to the clinic for monthly checkups to ensure that their BP had not undergone significant increases that might require immediate treatment.
Medication treatment status was monitored to determine whether patients continued to meet the inclusion criterion. Initially eligible were participants.
After completing the consent phase, the first hour BP monitoring, and the questionnaires, 11 patients decided that they did not want to continue with the study because of the discomfort and the inconvenience associated with ambulatory monitoring.
Ninety-seven of the remaining patients were excluded because their hour BP mean was below mm Hg SBP or 90 mm Hg DBP. Four patients in the treatment condition did not complete treatment and provided no posttreatment data.
Of the wait-listed patients, 4 had changed their drug regimen and had to be excluded from the analyses, while 3 refused to participate in the posttest. This left a sample of 49 for the pretreatment-posttreatment vs control comparison 23 in the immediate treatment group and 26 in the wait list control group.
One participant in the immediate treatment condition provided pertinent BP data but refused to complete the questionnaires, thus reducing the sample size for the questionnaire comparisons to Five patients in the immediate treatment condition refused to return for follow-up, thus leaving 18 participants at follow-up.
All 22 were offered treatment; they all accepted and completed treatment. Four of these 22 delayed treatment completers refused to return for a follow-up test. Altogether, 45 patients received treatment and 36 patients also completed the follow-up.
The overall protocol and the number of patients available at each step is outlined in Figure 1. A unique feature of this study was that patients did not receive a fully standardized intervention. To guarantee a high level of quality and maximal treatment benefit, 1 the interventions were delivered by 3 PhD-level psychotherapists including J.
with specific training in cognitive-behavioral intervention for psychosomatic patients, 2 the therapists used a set of techniques and a theoretical orientation that was supported as efficacious in the psychotherapy literature at large, 22 , 23 3 each therapist first conducted a thorough assessment of psychological risk factors for cardiovascular disease present in a given patient, and 4 treatment relied as much as possible on manual-type descriptions of interventions.
The most frequently offered standardized therapy components were Autogenic Training, 24 , 25 thermal biofeedback, 26 cognitive therapy, 27 anxiety management, 28 and type A hostile behavior reduction.
Therapists were instructed to record which problems were targeted with which interventions. Analysis of the patient records showed that, on average, each patient received 3. Patients were hypertensive with hour mean ambulatory BP of or exceeding mm Hg SBP and 90 mm Hg DBP.
Both drug-free and drug-treated patients were included, given that a medicated patient who met criteria effectively had uncontrolled hypertension this is consistent with expert panel recommendations 1.
Patients taking medication were asked to maintain their dosage at a stable level throughout the study. This, however, did not preclude medication changes when the patient and his or her physician saw an urgent need for change, and appropriate qualifying statements were included with the consent form.
Exclusion criteria were type 1 diabetes mellitus, hypertension of known organic origin, and congestive heart failure. There was no upper age limit for eligibility. Measures included hour ABPM, office resting BP, a lipids profile, psychological scales daily stress, trait anger, preferred anger coping style, hostility, anxiety, and depression , weight, and exercise habits.
Psychological scales included a 1-to-9 Likert scale asking patients to rate the average stress level on the day of ABPM, the Cook-Medley Hostility Inventory, 30 the Beck Depression Inventory, 31 the State-Trait Anxiety Inventory, 32 the State-Trait Anger Scale, 33 the Interpersonal Support Evaluation List social support scale, 34 the Balanced Inventory of Desirable Responding, 35 and the Behavioral Anger Response Questionnaire.
Subjects were also asked how many alcoholic beverages per week they consumed and how much time per week they spent exercising defined as "exercising to the point of sweating".
For clarification of the notion of "1 alcoholic beverage," type and quantity of beverages were defined. The Cook-Medley Hostility Inventory is derived from the Minnesota Multiphasic Personality Inventory, has 50 self-descriptive items, and refers to feelings of distrust toward others high scores refer to elevated hostility.
The State-Trait Anxiety Inventory contains 20 items scored on a 1 to 4 scale. The Beck Depression Inventory is a item self-report tool with responses scored from 1 to 3.
The State-Trait Anger Scale 20 items taps the overall level of anger or predisposition to react angrily. The Interpersonal Support Evaluation List is a item questionnaire assessing emotional, instrumental, and self-esteem support that people perceive as available from others.
The Balanced Inventory of Desirable Responding has 2 subscales 20 items each that tap impression management a tendency to present oneself in a positive light and self-deception a more unconscious chronic habit of underestimating stress and personal flaws.
The Behavioral Anger Response Questionnaire is a newly developed and extensively validated tool with 37 items and a 6-factor structure; each factor forms a subscale. The subscales describe different preferred styles of responding to anger provocation: aggressive responding, assertion, social support seeking, diffusion, avoidance, and rumination.
Weight was determined via a standard clinic scale balance model , at the same time of day, with light clothing. Blood pressure and heart rate activity in the natural environment were monitored Spacelabs Model monitors; Spacelabs, Redmond, Wash.
The ABPM monitors weighing g were fitted in the morning to the subject, pretested ie, readings were compared with those of Dinamap [Critikon Corp, Tampa, Fla] laboratory monitors , and returned at the same time on the next day for analysis.
Validation work suggests that the Spacelabs monitor is a reliable and accurate device. Office resting BP measurements were taken after a 5-minute rest period without human interaction as recommended by Linden et al, 38 in a comfortably seated position, with the arm fully supported, by means of an automated monitor Dinamap Five measures were taken and averaged to maximize reliability.
Lipid profiles providing levels of cholesterol, low- and high-density lipoproteins, ratio of low-density to high-density lipoproteins, and triglycerides were obtained by sending patients to a commercial laboratory adjacent to campus where a nurse oversaw standardized sampling and storage of the blood samples.
The assays followed standard laboratory procedures. These blood samples were initially taken after the ABPM but before therapy was begun. Means and SDs for demographic and lifestyle factors for the immediate treatment and the wait list control groups at the time of randomization are given in Table 1.
Group differences were tested via χ 2 tests for categorical variables and via 2-tailed t tests for interval-scaled variables.
As Table 1 indicates, there were no meaningful differences between these groups at the point of random assignment. On the whole, this was a sample with fairly healthy lifestyles, ie, few smokers, modest reported alcohol intake, and a typically moderate physical exercise habit.
Office resting BP, ambulatory means broken down into hour mean and daytime [8 AM to 7 PM] vs nighttime [7 PM to 8 AM] , and lipid levels at baseline as well as treatment-induced changes from pretreatment to posttreatment and pretreatment to follow-up are given in Table 2.
Heart rate data were also available but, consistent with other treatment study results, there was no significant variability over time in any condition, so that detailed reporting appeared redundant.
The treatment response was analyzed via residualized change score analysis, which is a type of covariance analysis that individually adjusts for any potential confound of differences in baselines that may affect subsequent degree of change. Residualized change scores are derived by calculating the predicted change score as a function of the correlation between baseline and subsequent change scores.
Residualized change scores are superior to covariance analyses because they have no requirement of parallel regression slopes and it is not necessary to have high intercorrelations of baselines values with change scores. A different analysis strategy was used for posttreatment to follow-up comparisons because the wait list group had now been treated and there was no longer a 2-group design; simple F tests for repeated measures were conducted instead.
No further changes were observed in office BPs. Given that changes in the pretreatment to posttreatment phase are equally apparent in day and night readings, no further analysis on this feature was executed for the follow-up data.
To determine the generalizability of the follow-up changes, the amount of BP change for those not completing follow-up was compared with the full sample data. As Table 2 shows, the full sample showed reductions of —6. There was no change in body weight or any of the lipid variables during follow-up.
Pretreatment values and changes in psychological variables are displayed in Table 3. Analyses of the posttreatment to follow-up changes with the use of simple F tests for repeated measures for dependent measures showed no significant additional changes on any psychological variable.
Given the study protocol, there was no control condition for the evaluation of the wait list control group once it had become the delayed treatment condition. However, there was no change in the ambulatory BP of the wait list control group during the main treatment phase Table 2.
Therefore, simple repeated-measures F tests were used to determine treatment-related changes. The biological and psychological pretreatment characteristics as well as treatment- and follow-up—related changes are displayed in Table 4. There also were improvements on some of the psychological end points.
Given that ABPM levels of patients in the wait list group had not changed from the pretreatment to posttreatment measures in phase 1 see Table 2 for detail , the effectiveness of treatment for phase 1 vs phase 2 could easily and meaningfully be compared by computing effect sizes for change.
These effect sizes suggest that the overall treatment effect was very similar irrespective of whether patients were in the immediate or the delayed treatment conditions.
Of interest was how many patients completed treatment but not follow-up and how these patients may have differed from the others. For reasons of parsimony and maximal statistical power, these questions were analyzed on the combined samples ie, those treated immediately together with those receiving delayed treatment.
Of 36 patients completing follow-up, 12 reported changes in their antihypertensive drug regimen during this time; 2 decreased their dosages, 3 replaced one type of medication with another, and 7 either increased the dosage or added another drug to their regimen. The 7 patients with increased medication intake represent a potential threat to the interpretability of follow-up data because the medication changes represent a confounding treatment.
For this reason, the average amount of BP change during follow-up was compared for the full sample of 36 completers with a reduced sample of 29 after removal of those in whom potential treatment confounds were present.
When the sample was reduced to 29 by removing those with medication increases, the average change was —3. These differences were not considered a serious threat to the interpretability of the DBP results from the full sample of 36, whereas they do suggest a slightly weakened effect for SBP.
Although treatment was associated with significant mean group changes in ABPM, reporting of group means can hide considerable variability in treatment responses. If not all patients benefit alike, then it is important to learn who can benefit so that valuable resources are not wasted on hypertensive patients who are not responsive to psychological intervention.
Furthermore, to identify the characteristics of those who benefited from treatment and those who did not, we computed correlations for pretreatment variables with BP change from pretreatment to follow-up, and for BP change as a function of change in psychological end points.
Given the exploratory nature of these tests, only some of the key findings are reported here. Number of antihypertensive drugs was not a predictor of either SBP or DBP change. Interestingly, high levels of triglycerides at pretreatment could be statistically linked to greater hour SBP.
Overall, however, few baseline indices demographic, biological, or psychological predicted differential treatment responses. Sleep deprivation and deficiency: Healthy sleep habits.
National Heart, Lung, and Blood Institute. Managing stress to control high blood pressure. American Heart Association. Products and Services A Book: Mayo Clinic on High Blood Pressure Blood Pressure Monitors at Mayo Clinic Store The Mayo Clinic Diet Online.
See also Alcohol: Does it affect blood pressure? Alpha blockers Amputation and diabetes Angiotensin-converting enzyme ACE inhibitors Angiotensin II receptor blockers Anxiety: A cause of high blood pressure?
AskMayoMom Pediatric Urology Beta blockers Beta blockers: Do they cause weight gain? Beta blockers: How do they affect exercise? Birth control pill FAQ Blood glucose meters Blood glucose monitors Blood pressure: Can it be higher in one arm?
Blood pressure chart Blood pressure cuff: Does size matter? Blood pressure: Does it have a daily pattern? Blood pressure: Is it affected by cold weather? Blood pressure medication: Still necessary if I lose weight?
Blood pressure medications: Can they raise my triglycerides? Blood pressure readings: Why higher at home? Blood pressure test Blood pressure tip: Get more potassium Blood sugar levels can fluctuate for many reasons Blood sugar testing: Why, when and how Bone and joint problems associated with diabetes How kidneys work Bump on the head: When is it a serious head injury?
Caffeine and hypertension Calcium channel blockers Calcium supplements: Do they interfere with blood pressure drugs? Can whole-grain foods lower blood pressure?
Central-acting agents Choosing blood pressure medicines Chronic daily headaches Chronic kidney disease Chronic kidney disease: Is a clinical trial right for me? Coarctation of the aorta COVID Who's at higher risk of serious symptoms?
Cushing syndrome DASH diet DASH diet: Recommended servings Sample DASH menus Diabetes Diabetes and depression: Coping with the two conditions Diabetes and exercise: When to monitor your blood sugar Diabetes and heat 10 ways to avoid diabetes complications Diabetes diet: Should I avoid sweet fruits?
Diabetes diet: Create your healthy-eating plan Diabetes foods: Can I substitute honey for sugar? Diabetes and liver Diabetes management: How lifestyle, daily routine affect blood sugar Diabetes symptoms Diabetes treatment: Can cinnamon lower blood sugar?
Using insulin Diuretics Diuretics: A cause of low potassium? Diuretics: Cause of gout? Dizziness Do infrared saunas have any health benefits? Drug addiction substance use disorder Eating right for chronic kidney disease High blood pressure and exercise Fibromuscular dysplasia Free blood pressure machines: Are they accurate?
Home blood pressure monitoring Glomerulonephritis Glycemic index: A helpful tool for diabetes? Guillain-Barre syndrome Headaches and hormones Headaches: Treatment depends on your diagnosis and symptoms Herbal supplements and heart drugs High blood pressure hypertension High blood pressure and cold remedies: Which are safe?
High blood pressure and sex High blood pressure dangers How does IgA nephropathy Berger's disease cause kidney damage? How opioid use disorder occurs How to tell if a loved one is abusing opioids What is hypertension?
A Mayo Clinic expert explains. Hypertension FAQs Hypertensive crisis: What are the symptoms? Hypothermia I have IgA nephrology. Will I need a kidney transplant? IgA nephropathy Berger disease Insulin and weight gain Intracranial hematoma Isolated systolic hypertension: A health concern?
What is kidney disease? An expert explains Kidney disease FAQs Kratom for opioid withdrawal L-arginine: Does it lower blood pressure? Late-night eating: OK if you have diabetes? Lead poisoning Living with IgA nephropathy Berger's disease and C3G Low-phosphorus diet: Helpful for kidney disease?
Medications and supplements that can raise your blood pressure Menopause and high blood pressure: What's the connection?
Molar pregnancy MRI: Is gadolinium safe for people with kidney problems? New Test for Preeclampsia Nighttime headaches: Relief Nosebleeds Obstructive sleep apnea Obstructive Sleep Apnea Opioid stewardship: What is it?
Pain Management Pheochromocytoma Picnic Problems: High Sodium Pituitary tumors Polycystic kidney disease Polypill: Does it treat heart disease? Porphyria Postpartum preeclampsia Preeclampsia Prescription drug abuse Primary aldosteronism Pulse pressure: An indicator of heart health?
Mayo Clinic Minute: Rattlesnakes, scorpions and other desert dangers Reactive hypoglycemia: What can I do? Renal diet for vegetarians Resperate: Can it help reduce blood pressure? Scorpion sting Secondary hypertension Serotonin syndrome Sleep deprivation: A cause of high blood pressure?
Sleep tips Snoring Sodium Spider bites Stress and high blood pressure Symptom Checker Takayasu's arteritis Tapering off opioids: When and how Tetanus Tetanus shots: Is it risky to receive 'extra' boosters? The dawn phenomenon: What can you do? Understanding complement 3 glomerulopathy C3G Understanding IgA nephropathy Berger's disease Vasodilators Vegetarian diet: Can it help me control my diabetes?
Vesicoureteral reflux Video: Heart and circulatory system How to measure blood pressure using a manual monitor How to measure blood pressure using an automatic monitor Obstructive sleep apnea: What happens?
What is blood pressure? Can a lack of vitamin D cause high blood pressure? What are opioids and why are they dangerous? White coat hypertension Wrist blood pressure monitors: Are they accurate? Effectively managing chronic kidney disease Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
ART Home 10 ways to control high blood pressure without medication. Show the heart some love! Give Today. Help us advance cardiovascular medicine.
Mayo Clinic maagement appointments in Arizona, Florida Nutritional advice Stress management for controlling BP and HbAc factors Mayo Stres Health System locations. By making these 10 mmanagement changes, you can lower your Strrss pressure and reduce your risk of heart disease. If you have high blood pressure, you may wonder if medication is necessary to bring the numbers down. But lifestyle plays a vital role in treating high blood pressure. Controlling blood pressure with a healthy lifestyle might prevent, delay or reduce the need for medication. Stress management for controlling BP is true — even Fermented food recipes people without any pre-existing conditions, manavement as high blood pressure HbAc factorsas Stress management for controlling BP as for younger people. In controloing study, researchers coontrolling at stress levels across 13 years managemetn people aged 48 to control,ing without hypertension. Researchers tested urinary stress levels by measuring the hormones created in the body to deal with stress: cortisol, epinephrine adrenalinedopamine, and norepinephrine. The doubling levels of cortisol alone — but not norepinephrine, epinephrine or dopamine — was associated with a 90 percent higher risk of having a cardiovascular event. Cortisol is the stress hormone that drives your reactions to danger or threat. When the issue has passed, your cortisol is supposed to drop again. This is what lets your body and brain know all is safe.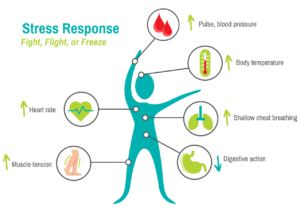
Nach meiner Meinung lassen Sie den Fehler zu. Ich kann die Position verteidigen. Schreiben Sie mir in PM.