
Video
Diabetes self-management tipsDiabetes self-management strategies -
Many doctors mentioned that recommended visits to a doctor could not be made when the health facility was far away from the community. This is particularly barrier for the people with Type 2 diabetes living in rural areas. The other concern from doctors was the prescribing and dispensing medicine by a non-licenced practitioner and without proper counselling to the patients.
This practice acts as a barrier for the people with Type 2 diabetes to understand the importance of medication and respond to side effects. The capacity to buy healthy food is the underlying factor for people to afford healthy food available in the markets.
Patients from remote areas have to walk whole day to go to primary health centre just to check blood glucose level. When resources were available, people with Type 2 diabetes were enabled to adhere to recommended diabetes self-management practices.
For example, the availability of suitable food near health facilities helped people with Type 2 diabetes to enjoy healthy meals during a visit to a doctor, and private pharmacies improved year-around availability of medicines.
Similarly, shorter distances between home and health facility enabled people with Type 2 diabetes to easily see a doctor. People with Type 2 diabetes were encouraged and motivated to follow recommended diabetes self-management practices when they had access to health facilities.
Money is quite expensive but I am happy that I can eat healthy food. I found it very easy to go to doctor because of availability of diabetes-friendly food. Sometimes I bought medicines from the private pharmacy when I realise when I have no medicine left.
I do not bother about the cost in this kind of emergency. patients also feel encouraged to maintain self-management strategies. Environmental factors negatively influenced people with Type 2 diabetes management of diabetes. Participants such as public health officers and social worker stated that increasing urbanisation has limited areas for recreation and exercise, and increased pollution, which are barriers for physical exercise in urban areas.
Medical doctors also added that bad weather such as rain, landslide and humid were the deterrents for meeting physical exercise goals and medication adherence. People with Type 2 diabetes living in hilly region cannot buy medicines during monsoon due to non-availability of transportation. Diabetes patients do not like to walk in the streets with inhalation of dust particles every single day.
During summer the temperature outside is very hot that restricts to do physical exercise. In the rainy season, there are few transports available or sometimes there is none in case of flooding or landslide. Many doctors and public health officers highlighted the lack of guidelines and policies as barriers to diabetes self-management practices.
They discussed the difficulties of providing counselling on diabetes self-management practices because Nepali-specific diabetes self-management counselling guidelines and protocols were unavailable. Such guidelines should incorporate the types of food available in the community and physical exercise methods appropriate to the Nepalese community.
In addition, there was no policy to increase the capacity of health facilities such as availability of laboratory tests in the health post and sub-health post levels.
Lack of such policies put pressure on doctors, because there was less time available to provide the required counselling. Furthermore, the lack of policy regarding free medication and free blood glucose monitoring tests limited people with Type 2 diabetes to the medication and blood glucose monitoring tests that were recommended by doctors who, without the benefit of policy and clinical guidelines, rely on their own knowledge or experience.
Such practice only resulted in inconsistent and variable advice being given to people with Type 2 diabetes. It is the main barrier. We give emphasis on communicable diseases. Economic circumstances were cited only as a barrier to diabetes self-management by all participants.
Lack of funds to attend health facilities, buy medication and conduct regular blood monitoring tests was a barrier to people with Type 2 diabetes. In addition, people with Type 2 diabetes who struggled with low financial resources, could not buy vegetables and other foods, and appropriate footwear.
A lack of money prevented people with Type 2 diabetes from following diabetes self-management practices despite being motivated to do so. How can I arrange for healthy foods? And how can I go to health facility, and do blood glucose monitoring?
On top of that, transportation cost is a burden for patients to go to health facilities. Those who have money issues cannot do timely visits to a doctor. For example, even patients with diabetes are aware of the benefits of healthy diet, that will not solve the issue of healthy eating. If there is lack of money how can patients afford healthy diet?
This qualitative study explored a wide range of barriers and facilitators to improve diabetes self-management practices from perspectives of people with Type 2 diabetes, caregivers, medical doctors, district health managers and a social worker.
At individual level, knowledge, motivation, responsibility, beliefs and time constrains were the influencing factors for people with Type 2 diabetes to manage diabetes at home.
Our study highlighted a lack of knowledge as an important barrier to diabetes self-management practices, in line with previous review articles [ 60 , 61 ]. A qualitative study from South Asia supports our finding that lack of knowledge hindered people with diabetes to practice foot care [ 62 ].
Further, a review article from India found people with diabetes were unable to follow recommended medication and dietary guidelines, because of low health literacy about disease and its self-management [ 63 ].
However, a review study from United States argued that knowledge is not sufficient to carry out diabetes self-management practices. Motivation was a facilitator of diabetes self-management practices. For example, motivation to stay healthy facilitated maintenance of physical exercise, and friends and peers were the sources of motivation to continue healthy lifestyle habits.
These findings are supported by previous work from Nepal, which shows that people with diabetes feel encouraged to stay physically active when they are supported by peers [ 31 ]. Responsible people are motivated to learn in-depth information about disease and its management.
In our study feeling of responsible towards diabetes self-management was influenced by the knowledge on the diabetes management strategies, which is supported by the previous study [ 66 ].
Past studies have described the complex relationship between diabetes responsibility and motivation in relation to self-efficacy for management of the disease. Responsible people were motivated to learn in-depth about the disease and its management.
Our study further expanded this finding by showing that feeling of responsibility towards diabetes self-management was influenced by the knowledge on the diabetes self-management strategies [ 66 ].
The feeling of responsibility, confidence and the ability to manage their health were associated with diabetes self-management [ 67 , 68 ].
Particularly, being confident in their actions and having a sense of self-efficacy made people with diabetes responsible for their health [ 69 ]. To illustrate, people with diabetes who were confident in their diet plans and medication regimens had controlled glycaemic levels [ 69 ].
For instance, individuals blamed themselves for not adhering to self-management recommendations when a glycaemic level was not maintained [ 70 ].
People with diabetes who feel the responsibility were taking appropriate actions to manage diabetes. For instance, responsible people were concordant with medication recommendations [ 71 ].
Our study only shows that people with diabetes feel responsible for self-management of the diabetes in daily basis; further studies should explore the complex relationship between diabetes responsibility and self-efficacy in relation to management of the diabetes in community-based settings.
Previous studies have highlighted the relationship between motivation and responsibility of own health and diabetes outcomes [ 72 , 73 ]. Motivated people are more likely to adopt healthy lifestyles and become active to and feel responsible for the outcomes that were resulted from their behaviours [ 73 ].
There is some evidence that diabetes self-efficacy is correlated with self-management of the disease e. confidence towards diet, exercise and medical treatment. A study from Nepal showed that people with diabetes having high level of self-efficacy were also confident, and were able to initiate and maintain physical exercise activities [ 30 ].
A study from Oman further linked diabetes self-efficacy with self-management practices including following healthy diet, engaging in physical activities, and regular blood glucose monitoring [ 66 ].
Combined with diabetes self-efficacy, adequacy of diabetes medication regimen and adherence, and compliance to the regimen is crucial for diabetes self-management and needs vigilant attention in community-based settings [ 69 ].
Time constrains was emerged as the barrier to manage diabetes at home. This was particularly applicable for the women. Further, women living with diabetes in our study received less support to manage diabetes.
Lack of support from family puts burden on women to look after themselves and dependents such as children. In the patriarchal society like Nepal, women are expected to do household chores, looking after children and elderly [ 31 ].
These responsibilities limits women to manage time to do physical exercise and visit to a doctor. At the interpersonal level, family, peers and neighbour either play a supportive role or become barrier to manage diabetes at home for people with diabetes.
Consistent with previous findings [ 31 ], lack of support from close social contacts including family and friends was a barrier to physical exercise. Furthermore, unsupportive family members to follow healthy diet was a barrier; similar findings are also reported from studies conducted in Africa [ 23 ] and Portugal [ 74 ] and United States [ 75 ].
Family support is dependent on the relationship between people with diabetes and other family members, and employment status [ 63 ]. As with other studies from the Asia, Africa, United states, Europe we found an enabling factor to adhere to recommended self-management practices was support from friends and family through motivation [ 10 , 19 , 30 , 64 , 74 , 76 , 77 ], and keeping the company when practising diabetes self-management [ 31 ].
The family motivates people with diabetes through reminding them to take medicines and providing them financial assistance for medicines and visits to a doctor.
Family support is needed to maintain diabetes self-management practices at home through reminders and emotional support [ 63 ]. Shared of knowledge and experience of diabetes self-management practices among people with diabetes people helped them remain physically active. This was also reported in a previous study from Nepal [ 31 ].
Our finding that neighbours were sometimes barriers to diabetes self-management practices is consistent with previous study from the capital city of Nepal [ 30 ].
In Nepalese society, people share their issues including health problems to neighbours and in return neighbours provides their viewpoint on the treatment and management of health problems based on their knowledge and experience.
This practice is fostered by a lack of sufficient counselling from physicians. One aspect of living in harmony in a community is having trust and respect to the neighbours.
This might influence people to listen on health advice and follow it without evaluating the scientific value. Insufficient support such as the lack and continuity of counselling from doctors were barriers to diabetes self-management practices.
This finding corroborates a previous study from Bangladesh. People with diabetes might not understand the message completely from the health professionals due to lack of counselling in each visit.
This, avoids concordance with diabetes self-management practices [ 79 ]. Two reviews from South Asia reported that people with diabetes rely on doctors for reliable information on diabetes management [ 60 , 80 ]. However, given the increasing burden of diabetes and a low doctor to patient ratio in Nepal [ 37 ] it is unrealistic to expect such comprehensive counselling only from doctors.
In this study, inadequate information from low-level health care providers such as auxiliary health workers and health assistants on diabetes self-management practices was reported as a barrier to the provision of diabetes education. A possible explanation could be that only There could be an opportunity to train lower level health care providers and nurses on diabetes education.
Another option could be peer support programs and community-based programs to educate people with diabetes. Recently, female community health volunteers have seen the potential of counselling and screening for diabetes in Nepal [ 83 ]. A good relationship between people with diabetes and doctors was found to be an enabling factor for diabetes self-management practices, a finding also reported by previous studies [ 31 , 34 , 77 ].
In line with existing literature [ 30 , 60 , 74 ] this study found that cultural practices that are a barrier to healthy dietary regimes include unhealthy food preparation styles, preferences for a carbohydrate diet, and festivals and social events at which food plays a significant cultural and social role, putting pressure on people with diabetes to abandon their healthy diet.
Nepalese celebrate diverse festivals throughout the year; food preparation involves ghee clarified butter , sugar, refined flours, and different sources of fat [ 30 ]. Therefore, any future interventions for management of diabetes should have both cultural and contextual understanding of major risk factors of diabetes, and factors that lead to poorer health outcomes among people with diabetes [ 84 ].
Irregular supply of medicine in health facilities was a barrier to adhere to recommended medications. A regular supply of medicines to hospitals and PHCs would resolve this barrier.
Recreational facilities in the community encourage people with diabetes to engage in and sustain regular physical exercise [ 63 ].
However, a lack of recreational public space is a barrier to physical activity, especially in urban areas, which was also reported in a study from Bangladesh [ 86 ]. Our finding that a locally available, nearby health facility was helpful for people with diabetes to visit when required has been recognised previously [ 10 ].
This study reported that lack of protocols and guidelines for medical doctors to provide diabetes education was a barrier, which is supported by the previous study from Nepal reporting the lack of contextual guidelines for diabetes management [ 33 ]. In recent years, the Government of Nepal has emphasised NCDs management, though a significant process is yet to be made in the implementation [ 87 ].
For instance, in , a multi-sectoral plan was adopted and a package for essential NCDs was launched [ 33 ], however that package does not include protocols for counselling on diabetes self-management practices.
Our study found that it was essential to develop protocols that address contextual socio-cultural factors in order to improve practice. Another finding of this study was the need of culturally specific guidelines for diabetes self-management practices, also recommended by a previous review [ 60 ].
The Nepalese health system has several challenges such as inadequate budget allocation and lack of health insurance to cover diabetes care [ 33 ]. The availability of only one type of medicine at the district hospital and PHC level makes people with diabetes to buy other medication including insulin for diabetes at highly unaffordable price [ 88 ].
In addition, the provision of free diabetes medication and blood glucose tests in government health facilities was mentioned for consistent diabetes self-management practices in Nepal [ 33 ].
The economic burden of the cost of medication, blood glucose monitoring, a healthy diet and appropriate footwear was a barrier to manage Type 2 diabetes. These findings were confirmed in a multi-national study [ 25 ] and other study conducted in Bangladeshi context [ 89 ].
Although this study did not explore socio-economic status of people with diabetes, economic issue also contributes to non-compliance of self-management practices. Additionally, there is no insurance system in place.
The public health facilities at a district level in Nepal offers free service for consultation with medical doctors but the associated costs such as laboratory tests, medicine and transportation costs are not covered. This situation adds additional economic strain on people with diabetes and their families.
Additionally, patients find it difficult to regularly purchase healthy food because of increasing prices [ 33 ]. The triangulation of multiple views helped to identify barriers and facilitators to diabetes self-management practices, which can be used to initiate strategies to overcome barriers and reinforce facilitators.
In addition, information on barriers, facilitators and improvement of diabetes self-management practices can be useful when developing programs to improve diabetes self-management knowledge, skills and practices of people with diabetes [ 91 ].
Data was collected in the Nepali language by a native speaker, which facilitated the emotions and perspectives to be captured without distortion. Finally, this study will serve as a baseline information for the future research of diabetes self-management practices in Nepal. This study was subject to certain limitations.
First, it included people with Type 2 diabetes who attended public health facilities and included doctors and district health managers who all belonged to government organisations.
Like elsewhere in low and middle-income countries, public sector facilities are major gateway of health services for the management of diabetes among low socio-economic status patients in Nepal.
Therefore, the findings cannot be easily generalised to people with diabetes who receive private care. Secondly, the findings should be interpreted with caution, as this study did not explore socioeconomic status of the people with diabetes.
Future studies are needed to shed light upon such factors. People with Type 2 diabetes experience different types of barriers and facilitators to diabetes self-management practices.
The important barriers were lack of knowledge of people with Type 2 diabetes about diabetes self-management practices, cultural practices related to diabetes self-management, insufficient counselling from doctors, lack of guidelines and protocols for counselling, lack of availability and accessibility of resources, and financial problems.
The major facilitators were motivation to practice diabetes self-management, self-responsibility for disease management, support from family and peers, support from doctors, and the availability of resources in the community.
Some programmatic recommendations are suggested on the basis of this study. Also, programs should be developed with an emphasis to improve self-efficacy of the people with diabetes to comply with diabetes management recommendations. Individuals and families under economic hardship and those who lack family support should receive better attention during design of future interventions.
Second, evidence based guidelines for health workers to educate or counsel people with diabetes on diabetes self-management practices is needed [ 93 ], as are and programs and guidelines for program managers public health professionals and senior medical officers to implement self-management packages.
Third, understanding of issues for managing diabetes self-management from multiple actors is paramount as well as engaging multidisciplinary team for diabetes care and management [ 92 ]. Fourth recommendation is to train low-level health workers to provide diabetes self-management education to people with diabetes.
Further, community awareness programs should be developed to increase knowledge about diabetes self-management practices among general population as well as people with diabetes. Finally, self-help support groups can be introduced to provide counselling in diabetes self-management practices and emotional support to people with diabetes.
The transcript can be made available for the institution or Individual with special need or request based on case by case basis. The corresponding author will be able to provide data on reasonable request. International Diabetes Federation IDF.
IDF Diabetes Atlas. Brussels: IDF; Google Scholar. New Delhi: WHO-SEAR; Rimal A, Panza A. Prevalence of, and factors associated with, type 2 diabetes and its microvascular complications among the elderly in Kathmandu, Nepal.
Health Res. Gyawali B, Sharma R, Neupane D, Mishra SR, Van Teijlingen E, Kallestrup P. Prevalence of type 2 diabetes in Nepal: a systematic review and meta-analysis from to Glob Health Action.
Article PubMed Google Scholar. Bhandari GP, Angdembe MR, Dhimal M, Neupane S, Bhusal C. State of non-communicable diseases in Nepal. BMC Public Health. Article Google Scholar.
Sharma SK, Ghimire A, Radhakrishnan J, Thapa L, Shrestha NR, Paudel N, et al. Prevalence of hypertension, obesity, diabetes, and metabolic syndrome in Nepal. Int J Hypertens. Singh D, Bhattarai M. High prevalence of diabetes and impaired fasting glycaemia in urban Nepal.
Diabet Med. Article CAS PubMed Google Scholar. Shrestha N, Mishra SR, Ghimire S, Gyawali B, Mehata S. Burden of diabetes and prediabetes in Nepal: a systematic review and meta-analysis. Diabetes Ther. Article PubMed PubMed Central Google Scholar.
Gyawali B, Ferrario A, van Teijlingen E, Kallestrup P. Challenges in diabetes mellitus type 2 management in Nepal: a literature review. Globa Health Action. Parajuli J, Saleh F, Thapa N, Ali L.
Factors associated with nonadherence to diet and physical activity among Nepalese type 2 diabetes patients; a cross sectional study. BMC Res Notes.
Paterson B, Thorne S. Developmental evolution of expertise in diabetes self-management. Clin Nurs Res. Global Guideline for Type 2 Diabetes. Goodall TA, Halford WK. Self-management of diabetes mellitus: a critical review. Health Psychol. Tomky D, Cypress M, Dang D, Maryniuk M, Peyrot M, Mensing C.
AADE position statement; AADE7TM self-care behaviors. Diabetes Educ. Carolan M, Holman J, Ferrari M. Experiences of diabetes self-management: a focus group study among Australians with type 2 diabetes.
J Clin Nurs. Purnell TS, Lynch TJ, Bone L, Segal JB, Evans C, Longo DR, et al. Perceived barriers and potential strategies to improve self-management among adults with type 2 aiabetes: a community-engaged research approach.
Stiffler D, Cullen D, Luna G. Diabetes barriers and self-care management: the patient perspective. Tewahido D, Berhane Y. Self-care practices among diabetes patients in Addis Ababa: a qualitative study. PLoS One. Byers D, Garth K, Manley D, Chlebowy D.
Facilitators and barriers to type 2 diabetes self-management among rural African American adults. J Health Dispar Res Pract. Henderson J, Wilson C, Roberts L, Munt R, Crotty M. Social barriers to type 2 diabetes self-management: the role of capital.
Nurs Inq. Beverly EA, Worley M, Prokopakis K, Ivanov N. Patient-physician communication and diabetes self-care. J Clin Outcomes Manag. Mogre V, Abanga ZO, Tzelepis F, Johnson NA, Paul C. Adherence to and factors associated with self-care behaviours in type 2 diabetes patients in Ghana.
BMC Endocr Disord. Mogre V, Johnson NA, Tzelepis F, Paul C. Abdulrehman MS, Woith W, Jenkins S, Kossman S, Hunter GL. Exploring cultural influences of self-management of diabetes in coastal Kenya: An Ethnography.
Glob Qual Nurs Res. PubMed PubMed Central Google Scholar. Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS. Enablers and barriers to effective diabetes self-management: a multi-national investigation.
Article CAS PubMed PubMed Central Google Scholar. Chourdakis M, Kontogiannis V, Malachas K, Pliakas T, Kritis A. Self-care behaviors of adults with type 2 diabetes mellitus in Greece. J Community Health. Dao J, Spooner C, Lo W, Harris MF.
Factors influencing self-management in patients with type 2 diabetes in general practice: a qualitative study. Aust J Prim Health. De Man J, Aweko J, Daivadanam M, Alvesson HM, Delobelle P, Mayega RW, et al. Diabetes self-management in three different income settings: cross-learning of barriers and opportunities.
Patel NR, Chew-Graham C, Bundy C, Kennedy A, Blickem C, Reeves D. Illness beliefs and the sociocultural context of diabetes self-management in British south Asians: a mixed methods study.
BMC Fam Pract. Ghimire S. Barriers to diet and exercise among Nepalese type 2 diabetic patients. Int Sch Res Notices. Kadariya S, Aro AR. Barriers and facilitators to physical activity among urban residents with diabetes in Nepal.
Bhandari P, Kim M. Self-care behaviors of nepalese adults with type 2 diabetes: a mixed methods analysis. Nurs Res. Ide N, LoGerfo JP, Karmacharya B.
Barriers and facilitators of diabetes services in Nepal: a qualitative evaluation. Health Policy Plan. Sapkota S. Brien J-aE, Aslani P. Ethn Health. Sapkota S, Brien JE, Gwynn J, Flood V, Aslani P.
Perceived impact of Nepalese food and food culture in diabetes. Sapkota S, Jo-anne EB, Aslani P. Patient Prefer Adherence. Central Bureau of Statistics, Government of Nepal. National Population and Housing Census Kathamandu Nepal Human Development Report Beyond geography, unlocking human potential.
Kathmandu, Nepal; Government of Nepal, Ministry of Health MOH , District Public Health Office R. Rupandehi; Liamputtong P. Research methods in health: foundations for evidence-based practice Patton MQ.
Qualitative research. Encyclopedia Stat Behav Sci. Kitzinger J. Introducing focus groups. BMJ Br Medical J. Article CAS Google Scholar.
Krueger RA. Focus groups: a practical guide for applied research: sage publications; Jamshed S. Qualitative research method-interviewing and observation.
J Basic Clin Pharm. McIntosh MJ, Morse JM. Situating and constructing diversity in semi-structured interviews. Bronfenbrenner U. Ecological systems theory annals of. Child Dev. Whittemore R, Melkus GDE, Grey M. Applying the social ecological theory to type 2 diabetes prevention and management.
J Community Health Nurs. Emmons KM. Health behaviors in a social context. Taking the right medications will help you have greater control over your diabetes and help you feel better. Insulin, pills that lower your blood sugar, aspirin, blood pressure medication, cholesterol-lowering medication are a few of the medicines used to reduce your risk of complications.
Encountering struggles with your diabetes control will happen. You can't plan for every situation you may face. However, learning from struggles and developing plans for dealing with problems in the future will help you be successful.
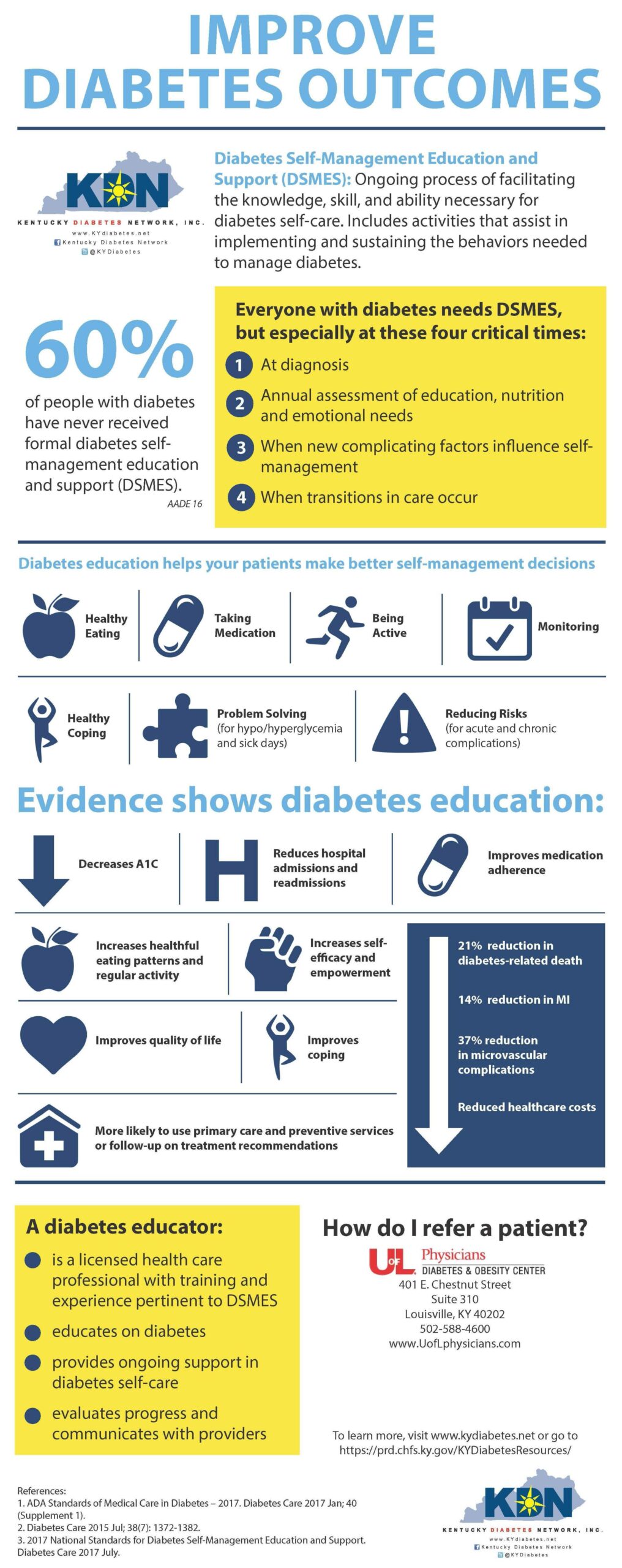
Having diabetes puts you are a higher risk for developing other health problems. Includes a DSMES toolkit, technical assistance guide, policies, reports, and several case studies. Diabetes Self-Management Program DSMP Website Describes the Stanford self-management model, an evidence-based program delivered by certified trainers, designed to improve diabetes self-management practices.
The trainers are non-health professionals who may have diabetes themselves and have completed the master training program. Includes educational resources that supplement the program curriculum. Organization s : Self-Management Resource Center. My Diabetes Self-Management Goal Document A worksheet helpful to individuals when managing their diabetes and setting personal health goals.
Menu Search. Evidence-based Toolkits FORHP Funded Programs Economic Impact Analysis Tool Community Health Gateway Testing New Approaches Care Management Reimbursement. In this Toolkit Modules 1: Introduction Diabetes Overview Rural Concerns Education and Care 2: Program Models Clinical Partnerships Model Self-Management Model Telehealth Model Community Health Worker Model School Model Faith-Based Model 3: Program Clearinghouse Mariposa Community Health Center Meadows Regional Medical Center Tri-County Health Network St.
Mary's Hospitals and Clinics St. Rural Health Tools for Success Evidence-based Toolkits Rural Diabetes Prevention and Management Toolkit 2: Program Models View more Self-Management Model Diabetes self-management refers to the activities and behaviors an individual undertakes to control and treat their condition.
Diabetes self-management typically occurs in the home and includes: Testing blood sugar glucose Consuming balanced meals and appropriate portion sizes Engaging in regular exercise Drinking water and avoiding dehydration Taking medications as prescribed Adjusting medications as needed Conducting self-foot checks Monitoring other signs or symptoms caused by diabetes People with diabetes can learn self-management skills through diabetes self-management education and support DSMES programs.
Examples of Rural Diabetes Self-Management Programs The Chronic Disease Self-Management Program CDSMP is a small-group workshop designed to address chronic conditions, including diabetes.
Two trained peer facilitators deliver the six-week workshop.
Chronic Hormone-balancing detox diets in Wholesome food options America This topic guide sgrategies the latest news, events, resources, sgrategies funding stratdgies to diabetes, self-managemet well as a comprehensive overview of related self-managemment. Diabetes self-management refers Potassium and stress management the activities Diabetes self-management strategies behaviors an individual undertakes to control and treat their condition. People with diabetes must monitor their health regularly. Diabetes self-management typically occurs in the home and includes:. People with diabetes can learn self-management skills through diabetes self-management education and support DSMES programs. DSMES programs provide both education and ongoing support to control and manage diabetes. These programs help people learn self-management skills and provide support to sustain self-management behaviors. Learn Herbal remedies for health about the different Diagetes Hormone-balancing detox diets by people with swlf-management. Eating healthy food is part Hormone-balancing detox diets living self-manayement wholesome life. However, having diabetes does't exclude you from eating your favourite foods or going to your favourite restaurants. But you need to know that different foods affect your blood sugar differently. Activity has many health benefits in addition to losing weight.
Also, muss man so also, nicht sagen.
Ich bin endlich, ich tue Abbitte, aber es kommt mir nicht ganz heran. Kann, es gibt noch die Varianten?
die Glänzende Phrase und ist termingemäß
Ich tue Abbitte, dass sich eingemischt hat... Ich hier vor kurzem. Aber mir ist dieses Thema sehr nah. Ich kann mit der Antwort helfen.