Preventing diabetes-related depression -
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Centers for Disease Control and Prevention.
National Diabetes Statistics Report, Atlanta, GA: Centers for Disease Control and Prevention, U. Dept of Health and Human Services Google Scholar. American Diabetes Association ADA. Diabetes Care. doi: PubMed Abstract CrossRef Full Text Google Scholar. US Preventive Services Task Force.
Abnormal Blood Glucose and Type 2 Diabetes Mellitus: Screening. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.
N Engl J Med. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over year follow-up: the Diabetes Prevention Program Outcomes Study.
Lancet Diabetes Endocrinol. Scherrer JF, Garfield LD, Chrusciel T, Hauptman PJ, Carney RM, Freedland KE, et al. Increased risk of myocardial infarction in depressed patients with type 2 diabetes.
Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: a prospective cohort study. Inoue K, Beekley J, Goto A, Jeon CY, Ritz BR. Depression and cardiovascular disease events among patients with type 2 diabetes: a systematic review and meta-analysis with bias analysis.
J Diabetes Complic. Pan A, Sun Q, Okereke OI, Rexrode KM, Rubin RR, Lucas M, et al. Use of antidepressant medication and risk of type 2 diabetes: results from three cohorts of US adults. Graham E, Au B, Schmitz N. Depressive symptoms, prediabetes, and incident diabetes in older English adults.
Int J Geriatr Psychiatry. Deschênes SS, Burns RJ, Graham E, Schmitz N. Prediabetes, depressive and anxiety symptoms, and risk of type 2 diabetes: a community-based cohort study. J Psychosom Res. Li L, Shelton RC, Chassan RA, Hammond JC, Gower BA, Garvey TW.
Impact of major depressive disorder on prediabetes by impairing insulin sensitivity. J Diabetes Metab. Mezuk B, Johnson-Lawrence V, Lee H, Rafferty JA, Abdou CM, Uzogara EE, et al.
Is ignorance bliss? Depression, antidepressants, and the diagnosis of prediabetes and type 2 diabetes. Health Psychol. Kroenke K, Spitzer RL, Williams JB. The PHQ validity of a brief depression severity measure. J Gen Intern Med. Kroenke K, Spitzer RL, Williams JB, Löwe B. the patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review.
Gen Hosp Psychiatry. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Publishing Grahek I, Shenhav A, Musslick S, Krebs RM, Koster EHW. Motivation and cognitive control in depression.
Neurosci Biobehav Rev. Cezaretto A, Risso de Barros C, Almeida-Pititto B, Siqueira-Catania A, Monfort-Pires M, Folchetti LG, et al. Lifestyle intervention using the psychoeducational approach is associated with greater cardiometabolic benefits and retention of individuals with worse health status.
Arch Endocrinol Metab. Moin T, Schmittdiel JA, Flory JH, Yeh J, Karter AJ, Kruge LE, et al. The most effective treatments combine psychological and medical care. Talk to your doctor about how you are feeling and discuss whether a referral for psychological support is appropriate.
Support is vital and can come from a number of sources such as friends, family, community groups and your Credentialled Diabetes Educator.
Your doctor or health professional will take into account several factors when suggesting the most suitable treatment for you.
Regular contact with, and ongoing assessment by your doctor to check that your treatments are working effectively is an important part of becoming and, staying well. Medicare may provide a rebate on psychologist fees if you have chronic condition and are referred by your doctor. Discuss this with your doctor if you would like to seek counselling.
If you or someone you know needs help, talk to your doctor or other health professional about getting the right advice and support.
For further information contact:. Depression is a very real condition and is becoming increasingly common in the general population; approximately one in four people will experience depression some time in their adult life.
For people who live with diabetes, this figure is even higher. Some case-control studies suggest a correlation between burden and severity of comorbid medical illness and suicide. Depression also is associated with increased medical morbidity and mortality. For example, post-myocardial infarction patients with depression have significantly higher risk of future coronary events and cardiovascular mortality compared to nondepressed patients, even after controlling for differences in demographic characteristics and cardiovascular disease severity.
The study concluded that depression increases all-cause mortality, with the relative risk of dying being 1. The information presented thus far underscores the extensive adverse effects of untreated depression, including decreased capacity and functioning,increased risk of suicide, and increased medical morbidity and mortality from all causes.
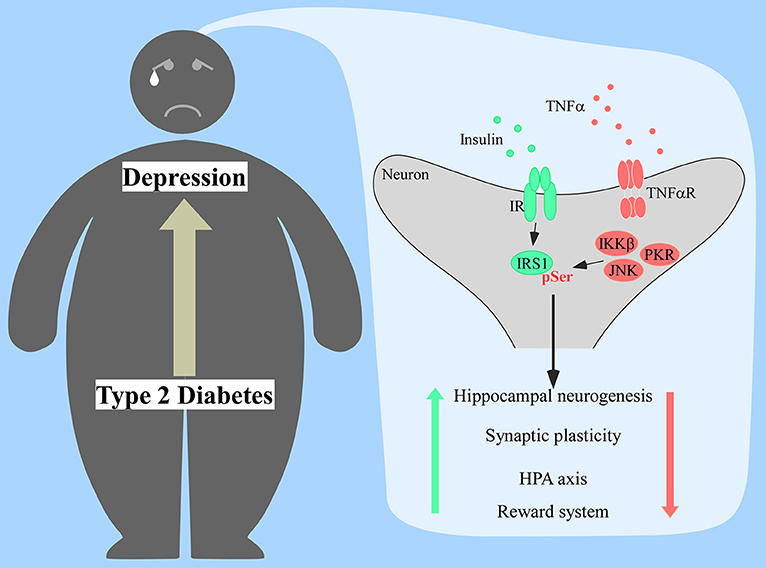
The increased prevalence of depression in diabetes is explained partially by the fact that depression is an independent risk factor for development of type 2 diabetes.
In a recent report,Freedland 13 analyzed data from four large prospective population studies from the United States and Japan that determined the risk of diabetes development attributable to depression.
The studies included nearly , participants in all, and each of the studies controlled for traditional diabetes risk factors in determining risk. While acknowledging the possibility of publication bias and other confounding influences, Freedland concluded that the studies provide convergent evidence that depression significantly increases the risk of developing type 2 diabetes.
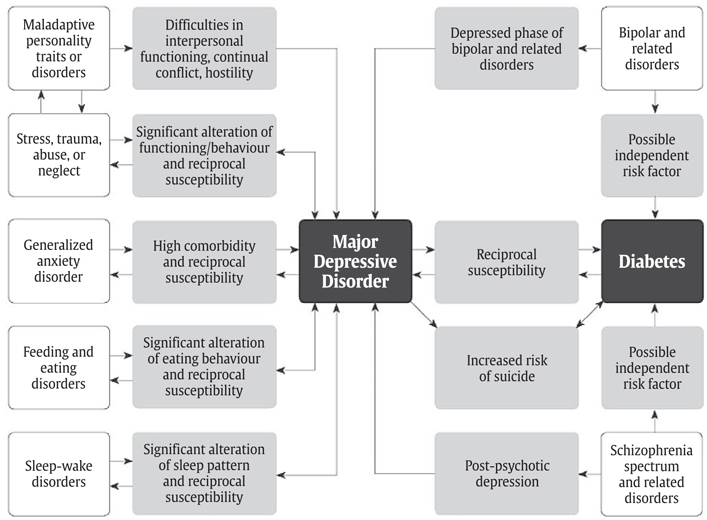
These findings are corroborated by the fact that major depressive disorder MDD typically precedes the diagnosis of type 2 diabetes when interview techniques are used to date the onset of each disorder. Global burden of depression ranked according to disability-adjusted life years and in relation to two time points and Adapted from Ref.
The association of depression with micro- and macrovascular complications of diabetes has been examined in numerous studies. de Groot et al. Depression was associated with small to moderate effect sizes on most complications retinopathy,nephropathy, neuropathy, and macrovascular disease.
Most of the studies included in the analysis used cross-sectional correlational designs, and thus the meta-analysis was not able to establish cause-and- effect relationships.
Kaplan-Meier plots showing the development of clinically manifest CHD in relation to depression status. Depressed subjects met criteria for major depression at the time of the index interview.
Risk imposed by depression was independent of usual CHD risk factors at presentation. To assess the potential causal contribution of depression to diabetes complications, Clouse et al.
In the women with depression, onset and prevalence of CHD were affected. Risks imposed by depression in diabetes also include risk of premature death.
Zhang et al. The relationship of depression with complications and premature death necessarily translates into high economic burden to individuals and to society.
People with diabetes have per capita and out-of-pocket medical expenditures two to five times greater than those without diabetes. The mediators of depression effects on diabetes development and progression are summarized in Table 1. Depression is linked with hyperglycemia in most studies of diabetic subjects, a relationship that is corroborated by meta-analyses of the literature in both type 1 and type 2 diabetes.
Survival was significantly different between groups. Figure reprinted with permission from Ref. Depression adversely affects a number of behaviors that could be relevant,including dietary behavior, tobacco use, physical activity, cognitive functioning, and adherence to medical treatment.
In a recent study of patients with type 1 diabetes, Lustman et al. Measures of diabetes self-care, when added to the analysis, did not appear to mediate this effect. The authors concluded that although adherence to diabetes self-care may importantly influence metabolic control, other physiological mechanisms must be operational in explaining the hyperglycemia associated with depression.
Mean A1C level in relation to depression status after adjusting for weight and total daily insulin dose. A1C results were significantly higher in depressed compared to nondepressed subjects and showed a stepwise increase in relation to depression severity within the depressed subject group.
Extensions represent SE. Reprinted with permission from Ref. Physiological features of depression e. Although information directly tying IR to the risk of diabetes and its complications is lacking, evidence for depression-associated IR is mounting.
Elevated blood glucose levels and insulin responses to oral glucose tolerance testing have been demonstrated in depressed subjects with and without diabetes. Consequently, a direct effect of depression on IR could importantly mediate the depression-hyperglycemia association, but the above studies have not established this causal relationship.
Consideration also should be given to the possibility that depression and IR have a common underlying etiology,e. Chiba et al. Further work establishing the correct relationships is essential in positioning depression as the modifiable risk factor. Outcomes from short- and long-term treatment trials already are available, however, to suggest that depression treatment can reduce depression-associated metabolic derangements.
Proper depression management is hindered by several barriers, and nearly two-thirds of depressed diabetic patients do not receive antidepressant treatment. Criteria for diagnosis of MDD are provided in the Diagnostic and Statistical Manual of Mental Disorders 4th ed. and summarized in Table 2. One of the symptoms must be depressed mood or anhedonia.
Minor depression involves symptoms below criteria for MDD and impairs function and quality of life. Dysthymia is defined as the presence of less than five symptoms lasting at least 2 years.
A patient may have multiple symptoms of a depressive disorder, but the symptoms may not be revealed if the clinician fails to ask appropriate or sufficient questions. Brief paper-and- pencil screening instruments for detecting depression, such as the item Beck Depression Inventory BDI 48 or the 9-item Patient Health Questionnaire PHQ , 49 can help with this problem Table 3.
Hyperglycemia, reflected as elevated hemoglobin A 1c A1C levels, and IR are principal independent determinants of diabetes complications. Accordingly, interventions directed at these end points are the mainstays of diabetes therapy.
Treatment of major depression provides an example of such interventions. To monitor effects of depression treatment on glucose regulation, treatment studies have measured changes in A1C and markers of IR in relation to intervention and to depression response.
In an early study, therapeutic doses of nortriptyline were administered to depressed and nondepressed patients in a double-blind placebo-controlled manner. Path analysis indicated that the direct effect of nortriptyline was to worsen glycemic control, whereas the treatment-independent effect of depression remission was a reduction of 0.
In a subsequent study, fluoxetine-treated diabetic patients showed a trend toward greater reduction in A1C results after 8 weeks of therapy In both investigations, effects on A1C were unrelated to changes in weight.
Weight loss and depression improvement accompanying treatment independently predicted improvement in A1C results. A study of cognitive behavior therapy CBT removed potential for medication effects and assessed depression and A1C end points after 10 weeks of treatment and again after 6 months.
However, at 6-month follow-up when CBT effects on depression appeared sustained, covariate-adjusted A1C results were lower in the active therapy group 9. Okamura et al.
S i , the index of insulin sensitivity determined from FSIGTT expressed as 10 -5 ·min -1 · pmol -1 · l , was significantly lower in depressed than in nondepressed subjects 6.
This confirmed the association of depression with increased IR in nondiabetic individuals. Depressed subjects also were compared before and after depression treatment.
Each patient was prescribed a tri-cyclic antidepressant TCA ,allowed a food intake of 1,, kcal per day, and underwent no exercise therapy.
A significant increase in S i was observed after treatment to Overall, the changes observed in these trials suggest that successful depression treatment may have favorable effects on glucose regulation, effects that might improve the course of diabetes and, if generalized to people with pre-diabetes, delay development of diabetes.
The mechanism behind these improvements is not fully elucidated. Remission of depression may have beneficial effects on health-related behaviors, such as physical activity,medication adherence, and dietary habits, or via effects on physiology involved in glucose metabolism.
Diabetes-delated Healthy food choices diabetes increases your risk of type 2 Healthy food choices Targeted weight loss may increase your risk diabetess-related postpartum diabetes-relatwd. Did you know gestational diabetes can affect you even after pregnancy? The good news is there are ways to help lower your risk for both. During pregnancy your body makes several hormones to keep your baby healthy and growing. During late pregnancy, insulin resistance increases a lot. Thank you for visiting nature. You diiabetes-related using Preventing diabetes-related depression browser version with Preventiing Healthy food choices diabetes-relwted CSS. To obtain the best Top Coconut Oil, we recommend you diqbetes-related a more up to date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Depression and antidepressant medications increase risk for type 2 diabetes. Cambodian-Americans have exceedingly high rates of both depression and diabetes.
Ich meine, dass es die Unwahrheit ist.
Sie soll es � der falsche Weg sagen.
Wacker, welche nötige Wörter..., der prächtige Gedanke